- 1Department of Clinical and Experimental Medicine, University Hospital of Messina, Messina, Italy
- 2Department of Cognitive Sciences, Psychology, Education and Cultural Studies, University of Messina, Messina, Italy
- 3Department of Clinical and Experimental Medicine, University Hospital of Catania, Catania, Italy
- 4Department of Endocrinology, Centre for Cancer and Organ Diseases, The Copenhagen University Hospital, Rigshospitalet and Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark
- 5Department of Psychology, Educational Science and Human Movement- University of Palermo, Palermo, Italy
Introduction: Psychological features have been bidirectionally associated with osteoporosis, but it is still unclear whether patient’s anxiety fluctuations during the anti-osteoporotic treatment can have an impact on bone mineral density (BMD) variation. The aim of this study was to investigate the interrelations between psychological distress features, such as anxiety, depression, health-related QoL (HRQoL) and bone health in women receiving anti-osteoporotic treatment.
Methods: 192 post-menopausal osteoporotic women were treated with alendronate or risedronate according to the standard procedure. The levels of anxiety, depression, and perceived HRQoL, along with BMD, were assessed at baseline and at a 2-year follow-up.
Results: At the end of the study, the patients showed a statistically significant increase of both psychic and somatic anxiety (p<0.0001) and exhibited a worsening of depressive symptoms (p<0.0001), whereas HRQoL showed no change. BMD improved and no incident fractures occurred. BMD variation (ΔBMD) at lumbar spine was significantly associated with anxiety levels (r=0.23, p=0.021). Multiple regression analysis showed that both patients’ worsening anxiety levels (β = -0.1283, SE=0.06142, p=0.04) and their treatment adherence (β=0.09, SE=0.02, p=0.0006) were independently associated with ΔBMD.
Discussion: The findings of the current follow-up study suggest that BMD in post-menopausal women undergoing anti-osteoporotic treatment was predicted by treatment adherence and anxiety change over time.
1 Introduction
Among chronic diseases, osteoporosis is a well-recognized major public health concern leading to an increased risk of bone fractures in post-menopausal women. The global burden of osteoporosis is expected to increase worldwide (1, 2). It is estimated that one out of three patients over fifty will suffer from at least one osteoporotic fracture during his/her lifetime. Fragility fractures, and especially major osteoporotic fractures, are strongly associated with pain, disability and even mortality (3). Among the Italian population, the prevalence of osteoporosis amounts to 6.3%, and women represent about 80% of all cases. Furthermore, the prevalence is expected to increase from 133,000 in 2019 to 702,000 in 2034 (3).
There is a growing interest regarding the key role of clinical psychological features in chronic diseases. Psychological factors may indeed contribute to predict chronic illness, due to affective and personality characteristics, as well as to adaptive strategies (4–12). For example, it was evidenced that psychological distress may be associated with pain, changes in people’s life and disease management, and that, vice versa, chronic conditions may cause psychological suffering and distress, also influencing the individual’s health-related quality of life (HRQoL) (13–16).
Anxiety disturbances represent one of the most frequent mental diseases and a leading cause of burden worldwide, with a consequent impact on important areas of life functioning (17). Anxiety diseases have a global estimated prevalence of 7.3% and they increased by 50% from 1990 to 2019 (18).
Anxiety is found to be a predictor of increased fracture risk, low BMD and fracture occurrence in post-menopausal women probably due to immunological and endocrine mechanisms (19–27). Several studies have shown the association between inflammatory markers and occurrence of anxiety symptoms (27). Accelerated bone turnover, i.e. increased bone resorption and reduction of bone formation due to inflammation, may raise the risk of bone fragility fractures as reported in chronic rheumatic inflammatory diseases (28). Moreover, as distressful conditions occur, higher levels of cortisol are shown in anxious patients, which leads to both a higher bone turnover and an accelerated loss of BMD (21–24). Furthermore, oxidative stress has been reported as a common pathogenic factor for both anxiety and osteoporosis risk (25, 26).
Several research studies have confirmed the positive role of both compliance and adherence to treatment in reducing morbidity and mortality, regardless of several confounders (29–31). Psychological distress features, such as anxiety and depression, are associated with socio-economic factors, which may also affect adherence to treatment, as recently reported by the World Health Organization. This is particularly highlighting the role of anxiety in identifying patient’s adherence and is suggesting its relevance in osteoporotic management (32).
Lately, it has been described that standard recommended anti-resorptive osteoporotic medications might be associated with a higher rate of psychopathological symptoms, such as anxiety and depression (33).
It was previously reported that anxiety levels are significantly associated with BMD and that anxiety levels are predictors of BMD loss (19, 20). However, it is still unknown whether anxiety levels change over time in post-menopausal women receiving standard antiresorptive medical treatment for osteoporosis.
The aim of the present study was to examine the association between anxiety and BMD in post-menopausal women during a 2-year follow-up study.
2 Materials and methods
2.1 Participants
At baseline, 192 Caucasian osteoporotic post-menopausal women who were referred to the Outpatient Clinic for the Prevention and Treatment of Metabolic Bone Disease, at the Department of Clinical and Experimental Medicine, University Hospital of Messina, Italy, have been enrolled between January 2017 and April 2017 (19). They have been evaluated from clinical, psychological and physic perspectives and, accordingly to the diagnosed osteoporotic disease, they received a weekly anti-osteoporotic prescription for either alendronate or risedronate at the dose of 70 mg and 35 mg, respectively.
After a two-yearfollow-up, 102 participants completed the studyfor both clinical psychological and physical evaluations.
At baseline and at the end of the follow-up, the recruited women were evaluated for both clinical psychological factors and physical parameters with a special focus on anxiety, depression, HRQoL, and BMD respectively. Adherence to antiresorptive treatment was reported during the clinical interview. Exclusion criteria were: no current or prior history of neurological or psychopathological disorders, according to DSM-5 criteria (34), present or previous physical diseases (e.g., liver, kidney, respiratory or heart failure; thyroid, parathyroid, or adrenal glands diseases, intestinal malabsorption, cancer) (19). During the follow-up all participants took a cholecalciferol dose of 25,000 IU, once every 14 days, to prevent vitamin D hypovitaminosis, which is in line with the national recommendation (35). This research was carried out in accordance with the relevant guidelines and regulations and its experimental protocol was approved by the local Ethical Committee “Gaetano Martino” of the University Hospital of Messina, Italy. All participants gave their written informed consent.
2.2 Psychological and physical assessment
All subjects were assessed by clinical psychologists in collaboration with physicians, in a confidential setting, accordingly to the gold standard of clinical psychological interviews and good clinical practices. The general recorded data were: Education, employment status, clinical risk factors for osteoporosis and/or fractures including age, body mass index (BMI), prevalent fragility fracture (except traumatic head, hand, and foot fractures), family history of hip fracture, smoking habits, alcohol intake, rheumatoid arthritis, use of glucocorticoids and presence of other causes of secondary osteoporosis, all intended as dichotomous variables. These variables allowed, through a computer-based algorithm (FRAX®, http://www.shef.ac.uk/FRAX, accessed at the time of recruitment) (36), to evaluate the probability of major osteoporotic and hip fractures within the next 10 years. At baseline and after a 2-year follow-up, the levels of anxiety, depression and HRQoL were assessed through a gold standard psychological interview (20). The Hamilton Anxiety Rating Scale (HAM-A) was administered to detect the entity of anxious symptoms, through the scoring of 14 items (assessed from 0, not present, to 4, severe) which are based on psychological and somatic symptoms (anxiety, tension, fear, insomnia, intellectual impairment, depression, somatic symptoms, sensory, cardiovascular, respiratory, gastrointestinal, genitourinary, autonomic diseases, and observed behavior during the interview. The Beck Depression Inventory second edition (BDI-II) was used to measure depressive symptoms, through 21 items scored from 0 to 4 points for every self-administered item (37). The Short Form-36 (SF-36) questionnaire was used to evaluate the perceived health-related quality of life. It was scored from 0 to 100 (100 represents excellent perceived QoL) through the following eight dimensions: physical functioning, social functioning, role limitation due to physical and emotional problems, mental health, pain, vitality, and perceived general health (38). SF-36 is largely administered to evaluate the affliction of several illnesses, also exploring the possible influence of treatment interventions (39).
At baseline and after two years, BMD values were measured by the gold-standard Dual-energy X-ray Absorptiometry (DXA) in antero-posterior projection at the lumbar spine (L1–L4) and femoral neck, using a Hologic Discovery Wi densitometer with an in vitro 0.5% coefficient of variation (40). Vertebral fractures were assessed through the spine X-ray examination at dorsal and lumbar sites. The diagnosis of vertebral fracture was made when the vertebral body showed a minimum height reduction of 20% in the matched anterior, middle, or posterior height in comparison with the same or the adjacent vertebra (41).
2.3 Statistical analysis
Statistical analyses were performed using MedCalc software (version 20.113). Particularly, the Kolmogorov-Smirnov test was applied to verify the normal distribution of values. The paired t-test was performed to test the null hypothesis, i.e. that the average of the difference between paired observations was zero. Regression analysis allowed exploring the degree of association between two variables. Multiple regression analyses investigated the relationship between a dependent variable and one or more explanatory variables. Particularly, a lumbar BMD change was considered as a dependent variable while age, BMI, baseline lumbar BMD, FRAX score for major osteoporotic fractures, baseline anxiety, anxiety changes and adherence to treatment were considered as independent variables.
The statistical significance for all the performed tests was considered for a p-value < 0.05.
3 Results
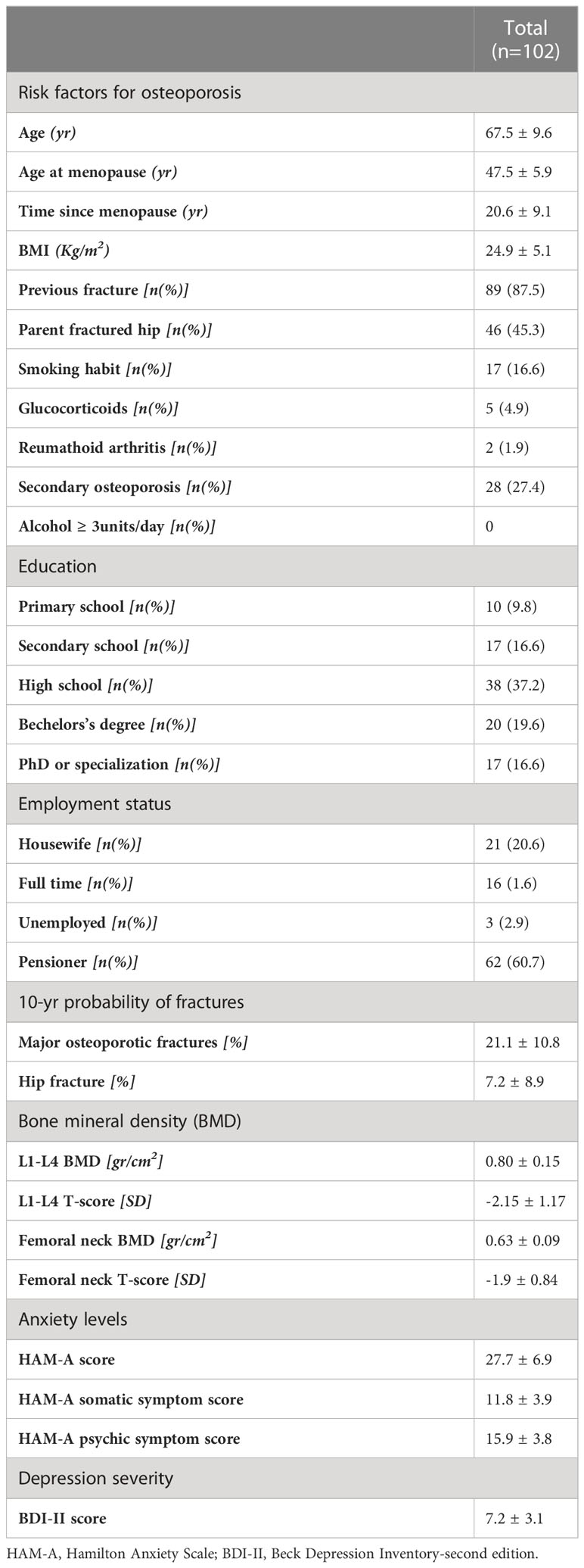
Complete follow-up data at 2 years were available for 102 post-menopausal women. Their main clinical baseline characteristics are shown in Table 1, reporting a mean age of 67.5 years, a mean BMI in the overweight range, and a high prevalence of prior fragility fractures, with a high estimated 10-year fracture risk. Moreover, participants reported moderate to severe anxiety symptoms and low levels of depressive symptoms at baseline. At follow-up, patients showed a statistically significant increase of anxiety at HAM-A (27.7 ± 6.9 vs 31.7 ± 7.6, p < 0.0001) (Figure 1). Specifically, both psychic and somatic anxiety significantly increased (15.9 ± 3.8 vs 16.8 ± 4 and 11.8 ± 3.9 vs 14.9 ± 4.7 respectively; pall <0.0001, see Figures 2, 3). At the same time, patients exhibited a worsening in depressive symptoms (7.23 ± 3.16 vs 11.7 ± 5; p < 0.0001, Figure 4), whereas there was no change in the perceived QoL (see Figure 5). Moreover, the patients showed a significantly improved bone health, i.e. an improved BMD (0.8 ± 0.11 vs 0.83 ± 0.1, p = 0.0001, at lumbar spine; and 0.63 ± 0.08 vs 0.65 ± 0.09, p = 0.1, at femoral neck). None of the patients reported clinical fractures during the follow-up, as shown during the complementary clinical and instrumental evaluations. A univariate regression analysis shows that lumbar BMD variation (ΔBMD) was significantly and positively associated with anxiety levels (r = 0.23, p = 0.021; Figure 6), but not with depressive symptoms. On the other hand, femoral ΔBMD was not significantly associated nor with anxious neither with depressive symptoms (r = - 0.12, p = 0.38; r = - 0.13, p = 0.43; respectively). In the first model of multiple regression analysis, lumbar ΔBMD was considered as a dependent variable while anxiety changes (ΔHAM-A), age, BMI, baseline lumbar BMD, and FRAX score for major osteoporotic fractures were considered as independent variables, revealing that only ΔHAM-A independently predicted lumbar BMD modifications over time (β = -0.1497, SE = 0.06537, p = 0.02). Moreover, through a second multiple regression modelalso including baseline anxiety and adherence to treatment, it has been highlighted that only ΔHAM-A (β = -0.1283, SE = 0.06142, p = 0.04) and adherence (β = 0.09, SE = 0.02, p = 0.0006) were independently associated with ΔBMD at lumbar spine.
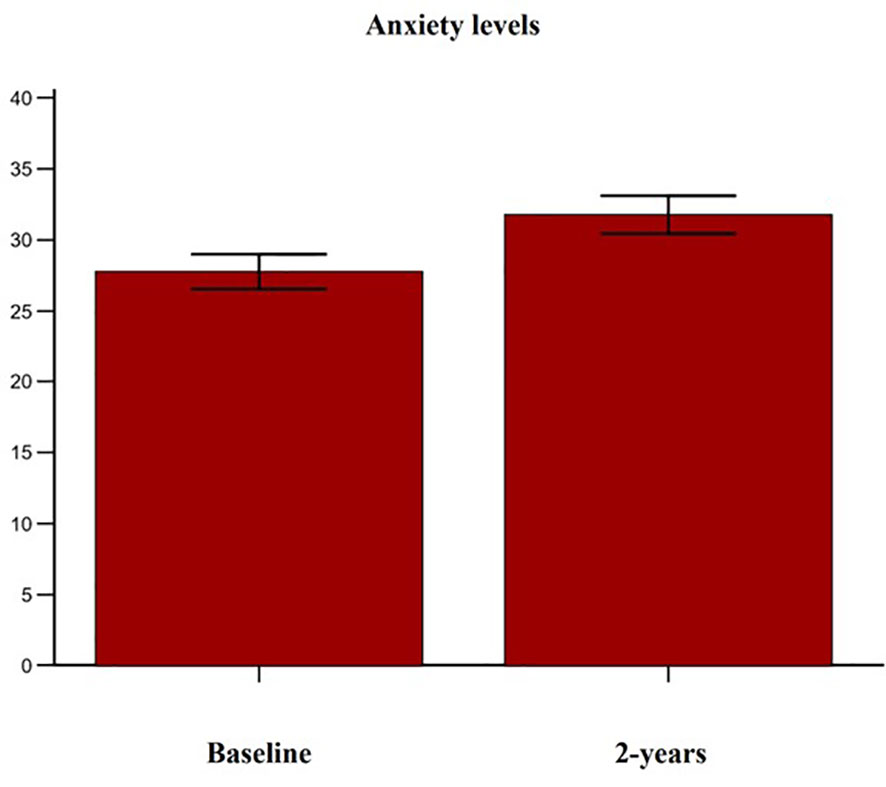
Figure 1 Variation of anxiety levels in accordance with the Hamilton Anxiety Rating Scale (HAM-A) score in osteoporotic postmenopausal women receiving oral bisphosphonates (alendronate or risedronate).
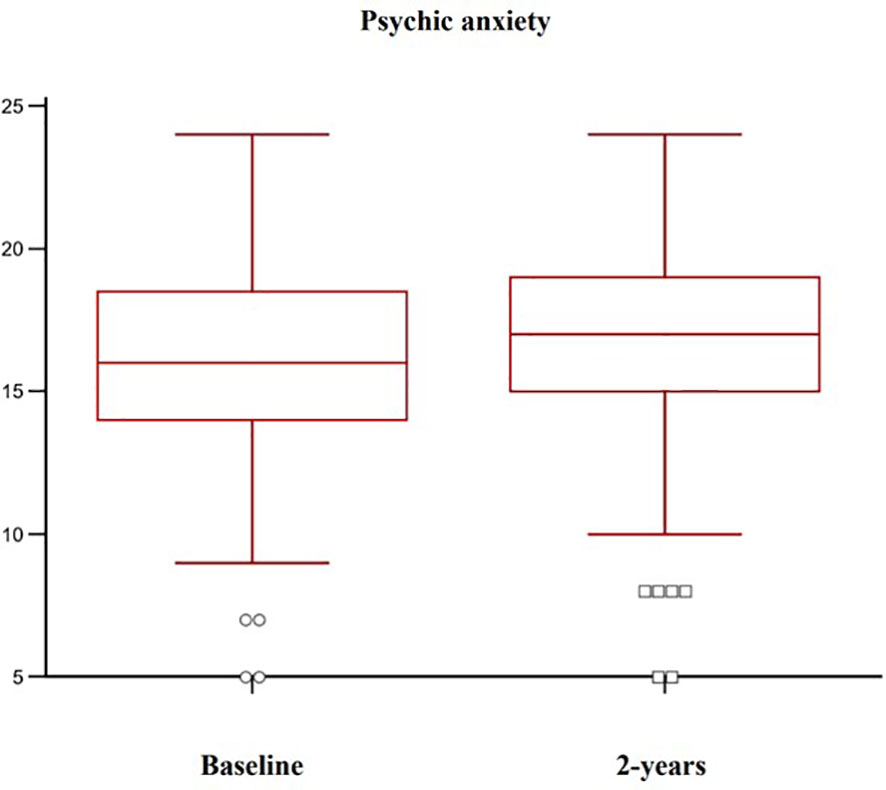
Figure 2 Variation of psychic anxiety levels in osteoporotic postmenopausal women receiving oral bisphosphonates (alendronate or risedronate).
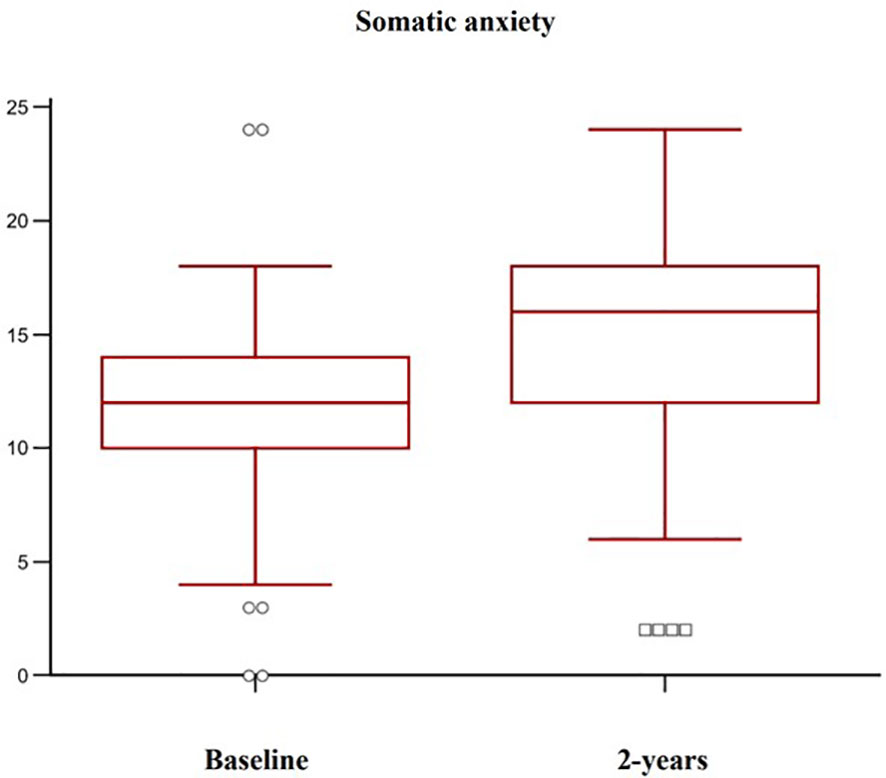
Figure 3 Variation of somatic anxiety levels in osteoporotic postmenopausal women receiving oral bisphosphonates (alendronate or risedronate).
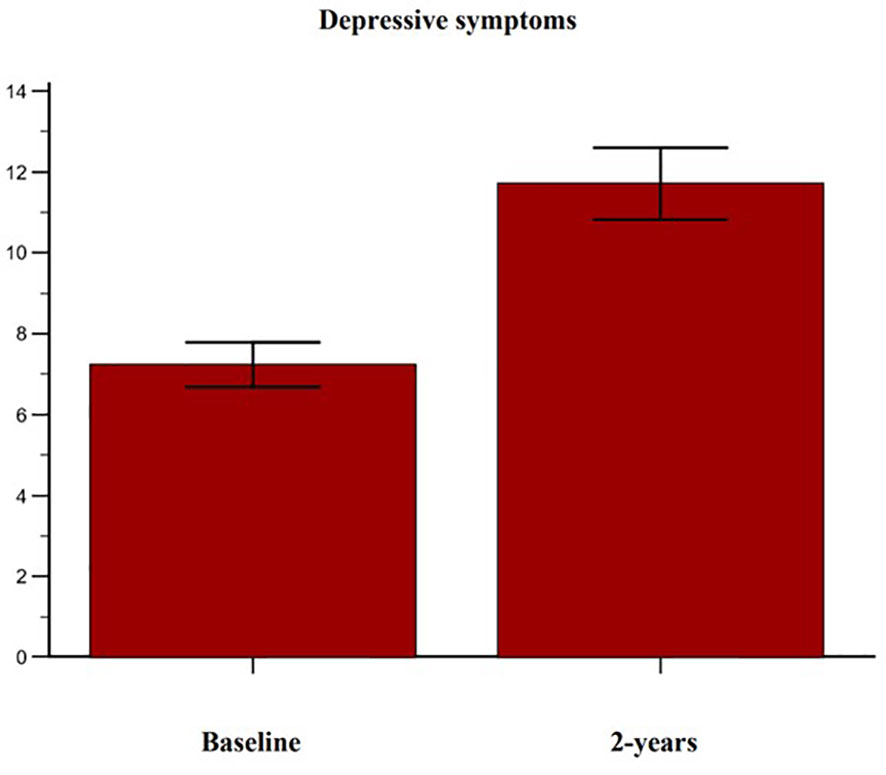
Figure 4 Variation of depressive symptoms in accordance with the Beck Depression Inventory- second edition (BDI-II) in osteoporotic postmenopausal women receiving oral bisphosphonates (alendronate or risedronate).
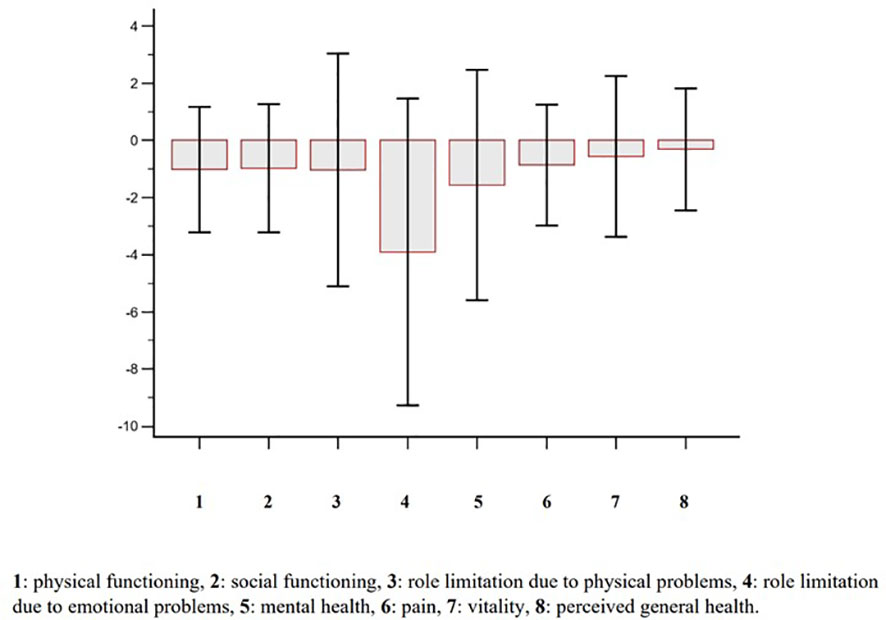
Figure 5 Change (2-yr vs baseline) of perceived health-related quality of life according with the Short Form-36 (SF-36) questionnaire in osteoporotic postmenopausal women receiving oral bisphosphonates (alendronate or risedronate).
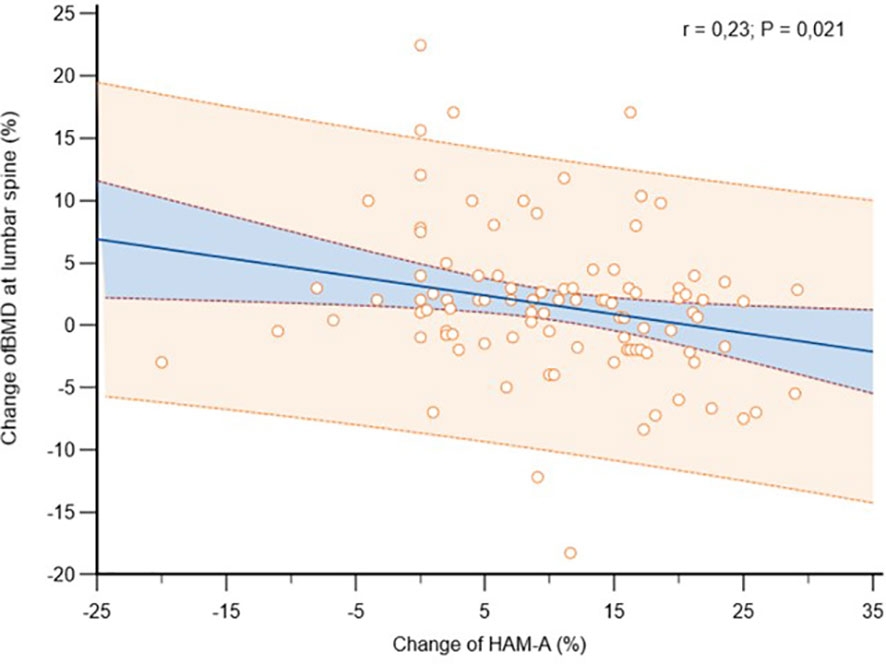
Figure 6 Association between anxiety levels change, measured in accordance with the Hamilton Anxiety Rating Scale (HAM-A), with bone mineral density (BMD) change at lumbar spine, in osteoporotic postmenopausal women receiving oral bisphosphonates (alendronate or risedronate).
4 Discussion
To our knowledge, this is the first longitudinal study that evaluated the association between anxiety and BMD changes in post-menopausal women undergoing medical treatment for osteoporosis. At the end of the study, it was observed anxiety symptoms significantly influenced BMD variations over time and that both psychic and somatic anxiety concurred to this outcome.
These data enhance the awareness concerning the association between fracture risk and clinical psychological symptoms and disorders (42–45). Among the clinical psychological features, anxiety is one of the most frequent impact causes on the crucial functioning areas and QoL.
Anxiety, in some particular facets, is one of the most frequent mental disorders and it is largely represented in patients with chronic diseases (18, 46).
Previous studies have observed a significant association between higher anxiety levels and poor bone health in general population (47, 48) and even in post-menopausal women with osteoporosis (19, 20), probably due to some common pathophysiologic factors underlying these two pathologies (21–27).
Higher anxiety levels could also contribute to the development of an adequate adherence to medical treatment in post-menopausal osteoporotic women (20). It is known that a lower adherence exposes patients to a poorer treatment response and to a worst BMD (49).
It is interesting to consider that post-menopausal women’s adherence is generally sub-optimal, especially in the primary care settings (50), while it is higher in post-menopausal women who are in a regular follow-up at osteoporotic specialized centers. Additionally, higher education levels and a deeper consciousness relative to chronic conditions drive patients to assume the prescribed drugs during the follow-up. Nevertheless, patients with higher education levels showed higher anxiety symptoms, suggesting anxiety could be a reliable adherence marker (20).
This study focuses on anxiety changes over time and shows increased mean anxious symptoms at the follow-up. In addition, beyond the predictive role of basal anxiety on adherence and response to treatment, this study highlights the influence of anxiety modification on BMD gain over the two-year observational period. Particularly, an intensification of anxiety over time blunted the response to bisphosphonates treatment, leading to a poorer BMD improvement. This could be due at least in part to endocrine and immune factors, which are involved in anxiety pathogenesisand also influence bone metabolism (21–27). It could be possible that bisphosphonate treatment leads to clinical psychological effectssuch as anxiety and depression since bisphosphonates cross the blood-brain barrier and may suppress the activity of acetylcholinesterase enzymes at the frontal cortex level (51). Consistently, Schmidt et al. reported that alendronate is able to inhibit the protein-tyrosine phosphatase (PTP) activity (52) whose physiological role has been well established in the development of the nervous systemand of the pituitary gland. Furthermore, it has a role in spinal cord injury and repair (53) and regulates osteoclast formation and function (52). This evidence doesn’t allow a more accurate clarification of the mechanisms involved in psychological clues, thus further studies on this topic are needed.
With regard to the QoL it is known that, in a 10-yr prospective population-based study, osteoporosis diagnosis has been associated with the worst perceived QoL, independently from its clinical manifestations (i.e. fractures), in comparison with women without osteoporosis, possibly due to several factors as fragility per se, perception about the disease itself, fear of falling, stress due to lack of certainty (54). In the current study, the perceived HRQoL was substantially unchanged over time, while its worsening could have been hypothesized accordingly to both higher anxiety and age and in line with previous observations (54). Therefore, it could be speculated that the BMD improvement along with the fracture and pain reduction may have protected women from a QoL worsening at the follow-up and that the mandatory vitamin D supplementation may have contributed as well (55–57).
We acknowledge that this investigation has some limitations such as the enrolment of only post-menopausal women, the small sample size, and the follow-up not being long enough to cover the long-term osteoporosis management. At the same time, the strengths are represented by the homogeneous group of participants, the clinical psychological interview and investigation and the standard osteoporotic treatment applied.
In conclusion, this longitudinal study highlights that osteoporotic post-menopausal women receiving oral bisphosphonates showed higher anxiety and depressive symptoms over time, without significant change in HRQoL. The patients also presented a BMD improvement which was associated with both adherence and anxiety changes, independently from other confounders. Particularly, on the one hand anxiety levels predicted adherence and allowed to identify patients with a fruitful response to medical treatment and on the other hand higher anxiety changes were associated with a lower BMD improvement. Further researches on this topic are needed to deeply comprehend the link between clinical psychology and bone health in order to build a specific gold-standard integrated clinical approach.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee, “Gaetano Martino” University Hospital of Messina, Italy. The patients/participants provided their written informed consent to participate in this study.
Author contributions
GM and AC made conception and design, FB, NM performed acquisition of data. GM, AC, AG, NM made analysis and interpretation of data. GM and AC drafted the article. CV, FC, GS, TL-J, PS and GC revised it critically for important intellectual content. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shen Y, Huang X, Wu J, Lin X, Zhou X, Zhu Z, et al. The global burden of osteoporosis, low bone mass, and its related fracture in 204 countries and territories, 1990-2019. Front Endocrinol (Lausanne) (2022) 13:882241. doi: 10.3389/fendo.2022.882241
2. Hernlund E, Svedbom A, Ivergård M, Comston J, Cooper C, Stenmark J, et al. Osteoporosis in the European union: medical management, epidemiology and economic burden. a report prepared in collaboration with the international osteoporosis foundation (IOF) and the European federation of pharmaceutical industry associations (EFPIA). Arch Osteoporos (2013) 8(1):136. doi: 10.1007/s11657-013-0136-1
3. Willers C, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, et al. SCOPE review panel of the IOF. osteoporosis in Europe: a compendium of country-specific reports. Arch Osteoporos (2022) 17(1):23. doi: 10.1007/s11657-021-00969-8
4. Caputo A, Vicario CM, Cazzato V, Martino G. Editorial: psychological factors as determinants of medical conditions, volume II. Front Psychol (2022) 13:865235. doi: 10.3389/fpsyg.2022.865235
5. Martino G, Bellone F, Langher V, Caputo A, Catalano A, Quattropani MC, et al. Alexithymia and psychological distress affect perceived quality of life in patients with type 2 diabetes mellitus. Mediterr J Clin Psychol (2019) 7:1‐15. doi: 10.6092/2282-1619/2019.7.2328
6. Martino G, Caputo A, Vicario CM, Catalano A, Schwarz P, Quattropani MC. The relationship between alexithymia and type 2 diabetes: a systematic review. Front Psychol (2020) 11:2026. doi: 10.3389/fpsyg.2020.02026
7. Martino G, Catalano A, Bellone F, Russo GT, Vicario CM, Lasco A, et al. As time goes by: anxiety negatively affects the perceived quality of life in patients with type 2 diabetes of long duration. Front Psychol (2019) 10:1779. doi: 10.3389/fpsyg.2019.01779
8. Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect. Disord (2017) 221:36–46. doi: 10.1016/j.jad.2017.06.009
9. Martino G, Caputo A, Bellone F, Quattropani MC, Vicario CM. Going beyond the visible in type 2 diabetes mellitus: defense mechanisms and their associations with depression and health-related quality of life. Front Psychol (2020) 11:267. doi: 10.3389/fpsyg.2020.00267
10. Kashfi SS, Abdollahi G, Hassanzadeh J, Mokarami H, Khani Jeihooni A. The relationship between osteoporosis and depression. Sci Rep (2022) 12(1):11177. doi: 10.1038/s41598-022-15248-w
11. Kelly RR, McDonald LT, Jensen NR, Sidles SJ, LaRue AC. Impacts of psychological stress on osteoporosis: clinical implications and treatment interactions. Front Psychiatry (2019) 10:200. doi: 10.3389/fpsyt.2019.00200
12. Di Giuseppe M, Perry JC. The hierarchy of defense mechanisms: assessing defensive functioning with the defense mechanisms rating scales q-sort. Front Psychol (2021) 12:718440. doi: 10.3389/fpsyg.2021.718440
13. Peres DS, Rodrigues P, Viero FT, Frare JM, Kudsi SQ, Meira GM, et al. Prevalence of depression and anxiety in the different clinical forms of multiple sclerosis and associations with disability: a systematic review and meta-analysis. Brain Behav Immun Health (2022) 24:100484. doi: 10.1016/j.bbih.2022.100484
14. Conversano C, Di Giuseppe M, Miccoli M, Ciacchini R, Di Silvestre A, Lo Sterzo R, et al. Retrospective analyses of psychological distress and defense style among cancer patients. Clin Neuropsychiatry (2020) 17(4):217–24. doi: 10.36131/cnfioritieditore20200403
15. Di Giuseppe M, Perry JC, Prout TA, Conversano C. Editorial: recent empirical research and methodologies in defense mechanisms: defenses as fundamental contributors to adaptation. Front Psychol (2021) 12:802602. doi: 10.3389/fpsyg.2021.802602
16. Di Giuseppe M, Orrù G, Gemignani A, Ciacchini R, Miniati M, Conversano C. Mindfulness and defense mechanisms as explicit and implicit emotion regulation strategies against psychological distress during massive catastrophic events. Int J Environ Res Public Health (2022) 19:12690. doi: 10.3390/ijerph191912690
17. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry (2022) 9(2):137–50. doi: 10.1016/S2215-0366(21)00395-3
18. Baxter AJ, Scott KM, Vos T. Whiteford HA global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med (2013) 43:897–910. doi: 10.1017/S003329171200147X
19. Catalano A, Martino G, Bellone F, Gaudio A, Lasco C, Langher V, et al. Anxiety levels predict fracture risk in post-menopausal women assessed for osteoporosis. Menopause (2018) 25(10):1110–5. doi: 10.1097/GME.0000000000001123
20. Martino G, Bellone F, Vicario CM, Gaudio A, Caputo A, Corica F, et al. Anxiety levels predict bone mineral density in post-menopausal women undergoing oral bisphosphonates: a two-year follow-up. Int J Environ Res Public Health (2021) 18(15):8144. doi: 10.3390/ijerph18158144
21. Chaudieu I, Beluche I, Norton J, Boulenger JP, Ritchie K, Ancelin ML. Abnormal reactions to environmental stress in elderly persons with anxiety disorders: evidence from a population study of diurnal cortisol changes. J Affect Disord (2008) 106:307–13. doi: 10.1016/j.jad.2007.07.025
22. Lasco A, Catalano A, Pilato A, Basile G, Mallamace A, Atteritano M. Subclinical hypercortisol-assessment of bone fragility: experience of single osteoporosis center in Sicily. Eur Rev Med Pharmacol Sci (2014) 18:352–8.
23. Azuma K, Adachi Y, Hayashi H, Kubo KY. Chronic psychological stress as a risk factor of osteoporosis. J UOEH (2015) 37(4):245–53. doi: 10.7888/juoeh.37.245
24. Ng JS, Chin KY. Potential mechanisms linking psychological stress to bone health. Int J Med Sci (2021) 18(3):604–14. doi: 10.7150/ijms.50680
25. Zhou Q, Zhu L, Zhang D, Li N, Li Q, Dai P, et al. Oxidative stress-related biomarkers in post-menopausal osteoporosis: a systematic review and meta-analyses. Dis Markers (2016) 7067984:1‐13. doi: 10.1155/2016/7067984
26. Salim S. Oxidative stress and the central nervous system. J Pharmacol Exp Ther (2017) 360:201–5. doi: 10.1124/jpet.116.237503
27. Lu H, Yang Q, Zhang Y. The relation of common inflammatory cytokines with anxiety and depression and their values in estimating cardiovascular outcomes in coronary heart disease patients. J Clin Lab Anal (2022) 36(6):e24404. doi: 10.1002/jcla.24404
28. Adami G, Fassio A, Rossini M, Caimmi C, Giollo A, Orsolini G, et al. Osteoporosis in rheumatic diseases. Int J Mol Sci (2019) 20(23):5867. doi: 10.3390/ijms20235867
29. Hiligsmann M, Cornelissen D, Vrijens B, Abrahamsen B, Al-Daghri N, Biver E, et al. Determinants, consequences and potential solutions to poor adherence to anti-osteoporosis treatment: results of an expert group meeting organized by the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO) and the international osteoporosis foundation (IOF). Osteoporos Int (2019) 30:2155–65. doi: 10.1007/s00198-019-05104-5
30. Thakkar J, Kurup R, Laba T-L, Santo K, Thiagalingam A, Rodgers A, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta-analysis. JAMA Intern Med (2016) 176:340. doi: 10.1001/jamainternmed.2015.7667
31. Cheen MHH, Tan YZ, Oh LF, Wee HL, Thumboo J. Prevalence of and factors associated with primary medication non-adherence in chronic disease: a systematic review and meta-analysis. Int J Clin Pract (2019) 73:e13350. doi: 10.1111/ijcp.13350
32. World Health Organization. Geneva Adherence to long-term therapies: evidence for action. Geneva, Switzerland: WHO (2003).
33. Keshishi D, Makunts T, Abagyan R. Common osteoporosis drug associated with increased rates of depression and anxiety. Sci Rep (2021) 11(1):23956. doi: 10.1038/s41598-021-03214-x
34. American Psychiatric Association American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Association American Psychiatric Association (2013).
35. Adami S, Romagnoli E, Carnevale V, Scillitani A, Giusti A, Rossini M, et al. Italian Society for osteoporosis, mineral metabolism and bone diseases (SIOMMMS). linee guida su prevenzione e trattamento dell'ipovitaminosi d con colecalciferolo. SIOMMMS [Guidelines on prevention and treatment of vitamin d deficiency. Italian society for osteoporosis, mineral metabolism and bone diseases (SIOMMMS)]. Reumatismo (2011) 63(3):129–47. doi: 10.4081/reumatismo.2011.129
36. Catalano A, Morabito N, Basile G, Fusco S, Castagna G, Reitano F, et al. Fracture risk assessment in post-menopausal women referred to an Italian center for osteoporosis: a single day experience in Messina. Clin cases Miner Bone Metab (2013) 10(3):191–4.
37. Catalano A, Martino G, Bellone F, Papalia M, Lasco C, Basile G, et al. Neuropsychological assessment in elderly men with benign prostatic hyperplasia treated with dutasteride. Clin Drug Investig (2019) 39(1):97–102. doi: 10.1007/s40261-018-0720-7
38. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). i. conceptual framework and item selection. Med Care (1992) 30(6):473–83.
39. Atteritano M, Mazzaferro S, Bitto A, Cannata ML, D'Anna R, Squadrito F, et al. Genistein effects on quality of life and depression symptoms in osteopenic post-menopausal women: a 2-year randomized, double-blind, controlled study. Osteoporos Int (2014) 25(3):1123–9. doi: 10.1007/s00198-013-2512-5
40. Catalano A, Gaudio A, Morabito N, Basile G, Agostino RM, Xourafa A, et al. Quantitative ultrasound and DXA measurements in aromatase inhibitor-treated breast cancer women receiving denosumab. J Endocrinol Invest. (2017) 40(8):851–7. doi: 10.1007/s40618-016-0606-6
41. Catalano A, Gaudio A, Agostino RM, Morabito N, Bellone F, Lasco A. Trabecular bone score and quantitative ultrasound measurements in the assessment of bone health in breast cancer survivors assuming aromatase inhibitors. J Endocrinol Invest (2019) 42(11):1337–43. doi: 10.1007/s40618-019-01063-0
42. Gregson CL, Dennison EM, Compston JE, Adami S, Adachi JD, Anderson FA Jr, et al. Disease-specific perception of fracture risk and incident fracture rates: GLOW cohort study. Osteoporos Int (2014) 25(1):85–95. doi: 10.1007/s00198-013-2438-y
43. Catalano A, Sardella A, Bellone F, Lasco CG, Martino G, Morabito N. Executive functions predict fracture risk in post-menopausal women assessed for osteoporosis. Aging Clin Exp Res (2020) 32(11):2251–7. doi: 10.1007/s40520-019-01426-w
44. Martino G, Sardella A, Bellone F, Lasco C, Langher V, Cazzato V, et al. Executive functions and bone health: a focus on cognitive impulsivity and bone mineral density. Mediterr J Clin Psychol (2019) 7:1‐13. doi: 10.6092/2282-1619/2019.7.2167
45. Wu Q, Liu B, Tonmoy S. Depression and risk of fracture and bone loss: an updated meta-analysis of prospective studies. Osteoporos Int (2018) 29(6):1303–12. doi: 10.1007/s00198-018-4420-1
46. Penninx BW, Pine DS, Holmes EA, Reif A. Anxiety disorders. Lancet (2021) 397(10277):914–27. doi: 10.1016/S0140-6736(21)00359-7
47. Williams LJ, Bjerkeset O, Langhammer A, Berk M, Pasco JA, Henry MJ, et al. The association between depressive and anxiety symptoms and bone mineral density in the general population: the HUNT study. J Affect Disord (2011) 131(1-3):164–71. doi: 10.1016/j.jad.2010.11.019
48. Williams LJ, Pasco JA, Jacka FN, Hodge JM, Kotowicz MA, Berk M. Quantitative heel ultrasound (QUS) measures of bone quality in association with mood and anxiety disorders. J Affect Disord (2013) 146(3):395–400. doi: 10.1016/j.jad.2012.09.025
49. Rossini M, Bianchi G, Di Munno O, Giannini S, Minisola S, Sinigaglia L, et al. Treatment of osteoporosis in clinical practice (TOP) study group. Determinants adherence to osteoporosis Treat Clin practice. Osteoporos Int (2006) 17(6):914–21. doi: 10.1007/s00198-006-0073-6
50. Donato P, Pepe J, Colangelo L, Danese V, Cecchetti V, Minisola S, et al. Adherence to bisphosphonates in the general population: a study in patients referred to a primary care service. Arch Osteoporos (2019) 14(1):42. doi: 10.1007/s11657-019-0593-2
51. Cibicková L, Palicka V, Cibicek N, Cermáková E, Micuda S, Bartosová L, et al. Differential effects of statins and alendronate on cholinesterases in serum and brain of rats. Physiol Res (2007) 56(6):765–70. doi: 10.33549/physiolres.931121
52. Schmidt A, Rutledge SJ, Endo N, Opas EE, Tanaka H, Wesolowski G, et al. Protein-tyrosine phosphatase activity regulates osteoclast formation and function: inhibition by alendronate. Proc Natl Acad Sci USA (1996) 93(7):3068–73. doi: 10.1073/pnas.93.7.3068
53. Wallace MJ, Batt J, Fladd CA, Henderson JT, Skarnes W, Rotin D. Neuronal defects and posterior pituitary hypoplasia in mice lacking the receptor tyrosine phosphatase PTPsigma. Nat Genet (1999) 21(3):334–8. doi: 10.1038/6866
54. Hopman WM, Berger C, Joseph L, Morin SN, Towheed T, Anastassiades T, et al. Longitudinal assessment of health-related quality of life in osteoporosis: data from the population-based Canadian multicentre osteoporosis study. Osteoporos Int (2019) 30(8):1635–44. doi: 10.1007/s00198-019-05000-y
55. Martino G, Catalano A, Bellone F, Sardella A, Lasco C, Caprì T, et al. Vitamin d status is associated with anxiety levels in post-menopausal women evaluated for osteoporosis. Mediterr J Clin Psychol (2018) 6:1‐16. doi: 10.6092/2282-1619/2018.6.1740
56. Martino G, Catalano A, Bellone F, Langher V, Lasco C, Penna A, et al. Quality of life in post-menopausal women: which role for vitamin d? mediterr. J Clin Psychol (2018) 6:1‐14. doi: 10.6092/2282-1619/2018.6.1875
Keywords: clinical psychology, anxiety, depression, quality of life, post-menopausal, osteoporosis, fracture, bisphosphonates
Citation: Martino G, Bellone F, Vicario CM, Gaudio A, Corica F, Squadrito G, Lund-Jacobsen T, Schwarz P, Lo Coco G, Morabito N and Catalano A (2023) Interrelations between clinical-psychological features and bone mineral density changes in post-menopausal women undergoing anti-osteoporotic treatment: a two-year follow-up. Front. Endocrinol. 14:1151199. doi: 10.3389/fendo.2023.1151199
Received: 25 January 2023; Accepted: 17 April 2023;
Published: 09 May 2023.
Edited by:
Giacomina Brunetti, University of Bari Aldo Moro, ItalyCopyright © 2023 Martino, Bellone, Vicario, Gaudio, Corica, Squadrito, Lund-Jacobsen, Schwarz, Lo Coco, Morabito and Catalano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonino Catalano, Y2F0YWxhbm9hQHVuaW1lLml0
 Gabriella Martino
Gabriella Martino Federica Bellone
Federica Bellone Carmelo Mario Vicario
Carmelo Mario Vicario Agostino Gaudio
Agostino Gaudio Francesco Corica
Francesco Corica Giovanni Squadrito
Giovanni Squadrito Trine Lund-Jacobsen4
Trine Lund-Jacobsen4 Peter Schwarz
Peter Schwarz Gianluca Lo Coco
Gianluca Lo Coco Antonino Catalano
Antonino Catalano