
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 31 March 2023
Sec. Clinical Diabetes
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1148468
This article is part of the Research Topic Influence of Lifestyle Factors in the Management of Diabetes Mellitus View all 15 articles
 Mayumi Hirosaki1,2*
Mayumi Hirosaki1,2* Tetsuya Ohira1*
Tetsuya Ohira1* Yawei Wu3
Yawei Wu3 Eri Eguchi1
Eri Eguchi1 Kokoro Shirai3
Kokoro Shirai3 Hironori Imano3,4
Hironori Imano3,4 Narumi Funakubo1
Narumi Funakubo1 Hitoshi Nishizawa5
Hitoshi Nishizawa5 Naoto Katakami5
Naoto Katakami5 Iichiro Shimomura5
Iichiro Shimomura5 Hiroyasu Iso3
Hiroyasu Iso3Background: Laughter has been reported to have various health benefits. However, data on the long-term effects of laughter interventions on diabetes are limited. This study aimed to investigate whether laughter yoga can improve glycemic control among individuals with type 2 diabetes.
Methods: In a single-center, randomized controlled trial, 42 participants with type 2 diabetes were randomly assigned to either the intervention or the control group. The intervention consisted of a 12-week laughter yoga program. Hemoglobin A1c (HbA1c), body weight, waist circumference, psychological factors, and sleep duration were evaluated at baseline and week 12.
Results: Intention-to-treat analysis showed that participants in the laughter yoga group experienced significant improvements in HbA1c levels (between-group difference: −0.31%; 95% CI −0.54, −0.09) and positive affect scores (between-group difference: 0.62 points; 95% CI 0.003, 1.23). Sleep duration tended to increase in the laughter yoga group with a between-group difference of 0.4 hours (95% CI −0.05, 0.86; P = 0.080). The mean attendance rate for laughter yoga program was high (92.9%).
Conclusions: A 12-week laughter yoga program is feasible for individuals with type 2 diabetes and improves glycemic control. These findings suggest that having fun could be a self-care intervention. Further studies with larger numbers of participants are warranted to better evaluate the effects of laughter yoga.
Clinical trial registration: http://www.chinadrugtrials.org.cn, identifier UMIN000047164.
Diabetes is a chronic condition that requires lifelong self-management for metabolic control, such as healthy eating, regular physical activity, and self-monitoring of the blood glucose levels, as well as taking medication as prescribed (1, 2). Previous studies have shown that good glycemic control maintenance is important for reducing the risk of diabetes-related complications and mortality (3–5). However, it has been reported that about 40-60% of individuals with type 2 diabetes have not achieved good glycemic control in all regions of the world (6). For example, about 60% of individuals with type 2 diabetes in Japan and about half of those in the US, have not achieved the HbA1c < 7% glycemic target (7, 8). Furthermore, a study has found that despite greater utilization of newly developed glucose-lowering medications, concurrent improvements in overall glycemic control were not shown (9). These findings suggest that existing therapeutic options may not be sufficient for maintaining good glycemic control and investigating new complementary therapeutic approaches would be needed.
Previous studies have also found that individuals with type 2 diabetes had poor adherence to exercise and a healthy diet (10, 11). It would be difficult to sustain lifestyle changes (12), and efforts toward lifestyle modifications have the potential to cause emotional distress. On the other hand, it has been suggested that positive affect experienced during health behaviors facilitates long-term adherence to the behaviors (13). Previous studies have shown that people are more likely to intend to engage in a health behavior and to actually engage in it, when the behavior is seen as enjoyable (14, 15). A systematic review has found that pleasant affect experienced during exercise predicts future physical activity (16). Thus, we expected that enjoyable activities, which boost positive psychological states, would be useful as self-care behavior in individuals with type 2 diabetes.
In this study, we focused on laughter as an enjoyable diabetes self-care intervention. Laughter has been demonstrated to have various health benefits, such as reducing stress (17), enhancing the activities of natural killer cells (17–19), suppressing allergic reactions (20), and inhibiting increases in postprandial blood glucose levels (21). Prospective cohort studies demonstrated that a low frequency of laughter is associated with increased risks of functional disabilities, all-cause mortality, and cardiovascular diseases (22, 23). Additionally, laughter interventions have a positive effect on depression and the well-being of older adults (24).
We previously reported that the combination of laughter and exercise decreased hemoglobin A1c (HbA1c) levels among older adults (25). In that study, we combined watching comedy programs with a general exercise program to increase the participants’ enjoyment and enhance their motivation to attend the intervention. However, making all participants laugh by watching the same comedy programs is difficult. Different individuals have different preferences. In contrast, self-induced laughter, including laughter yoga, which combines simulated laughter with deep breathing, does not require humorous stimuli (26). Additionally, a study that examined the potential benefits of laughter-inducing therapies has suggested that simulated laughter not caused by humor or other stimuli is more effective than spontaneous laughter triggered by humorous stimuli (27). Therefore, we conducted a laughter yoga intervention in this study.
Laughter yoga is now used in many countries (28). Several studies have shown that it improves depressive symptoms (29), decrease the levels of stress hormones (30, 31), and improves heart rate variability (32). Additionally, a study has reported that laughter yoga inhibits increases in postprandial blood glucose levels in individuals with type 2 diabetes (33). However, that study has shown the effect of a single 30-min session of laughter yoga only, and to the best of our knowledge, little is known about the long-term effects of laughter yoga on diabetes.
Therefore, this 12-week randomized controlled trial investigated the effects of laughter yoga on glycemic control and psychological well-being in individuals with type 2 diabetes.
This study was a single-center, two-group, randomized controlled trial designed to evaluate the effects of laughter yoga on individuals with type 2 diabetes. The intervention was conducted at Osaka University from October 2015 to December 2015. The study protocol was approved by the Scientific Ethics Committee of Fukushima Medical University (no. 2028). The Declaration of Helsinki was followed, and reporting in this article is aligned with the Consolidated Standards of Reporting Trials standards. All participants provided oral and written informed consent. This trial was registered at the University Hospital Medical Information Network Clinical Trials Registry (no. UMIN000047164).
Participants were recruited at the Diabetes Center of Osaka University Hospital, between August 2015 and September 2015. Three diabetologists evaluated their outpatients for study eligibility and approached patients meeting the eligibility criteria. Eligible patients received a flyer and the study was explained. Patients were recruited in order of their visit until the number of participants reached the target sample size. The inclusion criteria were outpatients aged 40 years or older with type 2 diabetes, HbA1c levels ranging from 6.1% to 7.9%, and changes in HbA1c levels < 1.0% during the last 3 months before baseline measurements. The glycemic control target is set at HbA1c <7.0% in Japan and modification of treatment (including intensive pharmacotherapy or insulin treatment) is needed when HbA1c level exceeded 8% (34). In addition, it would be difficult to determine whether the change in HbA1c level is due to the laughter yoga intervention or other factors in patients with originally large HbA1c fluctuations (unstable diabetes) before the laughter yoga intervention. Therefore, we included patients with HbA1c level changes of <1.0% during the last 3 months before baseline measurements (with stable treatment status). Patients with active coronary heart disease or stroke were excluded to reduce the risk of adverse events due to the intervention (e.g., a cardiac event during physical activity). Additionally, patients who could participate in light to moderate–intensity exercises were included, and those with other vascular complications and severe illness were excluded.
Before randomization, the participants were informed that similar laughter yoga sessions would be held after the study period for those who were allocated to the control group to reduce the reporting bias.
All participants continued to receive standard therapy for diabetes as they received before the study began. The control group continued the standard therapy and the intervention group received the standard therapy plus the laughter yoga program. Standard therapy included taking oral hypoglycemic medications, receiving advice from the doctor in charge of dietary modifications and physical activity in accordance with the “Treatment Guide for Diabetes” in Japan (35). Three participants received insulin therapy (one participant in the intervention group and two in the control group); the other participants received oral hypoglycemic agents. The control group was instructed to spend the study period as usual.
The participants in the intervention group received laughter yoga program once a week during the first 4 weeks and then every other week during the last 8 weeks. In total, eight sessions over 12 weeks were provided. The duration of laughter yoga intervention in previous studies ranged from 4 weeks to 8 weeks (28). However, a systematic review assessing the effects of yoga intervention on cardiovascular disease risk factors reported that the effects were most prominent in randomized controlled trials with 12 weeks of intervention duration (36). Therefore, we considered 12 weeks of intervention as appropriate. Every session began with a lecture of approximately 30 min on laughter and health, followed by a 60-min laughter yoga session. The laughter yoga session was based on the standardized laughter yoga program and the mini-lecture was added. The purpose of the lecture was to relax the participants and create a friendly atmosphere before the laughter yoga. Laughter yoga sessions were group-based interventions and guided by certified laughter yoga trainers from the Japan Laughter Yoga Association. All sessions were delivered by the same laughter yoga trainers to unify the contents of the intervention.
Laughter yoga is a kind of exercise consisting of deep breathing and voluntary laughter in a sitting or standing position. Each laughter yoga session consisted of warm up exercises, deep-breathing exercise, laughter exercise, and calming activity. At the beginning, the participants were asked to clap their hands along with saying the phrase “Ho, Ho, Ha, Ha, Ha,” as a warm up exercises. Then, deep breathing with laughter were performed. Subsequently, the participants were asked to participate in voluntary laughing imaging in a variety of situations, including 5-min break. For example, when doing the “milkshake laughter,” participants were asked to imagine that they have a glass of milk in their right hand and a glass of their favorite fruit juice in their left hand. They pretended to pour the milk from one glass into the other and pour it back into the first glass (to mix them). Then, they pretended to drink the milkshake, with a laugh. Finally, the participants were asked to close their eyes and relax.
The primary outcome was changes in HbA1c levels from the baseline to the 12-week follow-up measurement. Exploratory outcomes included changes in body weight, waist circumference, body mass index (BMI), positive affect, negative affect, subjective stress, and sleep duration from baseline to the 12-week follow-up. Physical examination and self-administered questionnaire were assessed on weeks 0 and 12.
HbA1c levels were measured in capillary whole blood, collected by finger prick, using the COBAS b101 point-of-care system (Roche Diagnostics International Ltd, Rotkreuz, Switzerland). Body weights were measured using a UC-322 weighing scale (A&D Co. Ltd., Tokyo, Japan), and BMIs were calculated as follows: weight (kg)/height squared (m2). Waist circumference was measured halfway between the lower border of the ribs and the iliac crest using a measuring tape.
The following data were obtained via a self-administered questionnaire: height; lifestyle factors, such as smoking and drinking habits, sleep duration, and physical activity; and psychological factors. Positive and negative affects were assessed using the Japanese version of the 15-item Geriatric Depression Scale (GDS-15) (37). Most study participants were at least 65 years old. Thus, the GDS-15 was used for the assessment of psychological status. The GDS-15 is widely used to screen depression among older adults. Although the factor structure of the GDS-15 varies across study populations and language groups, a meta-analysis showed that the positive mood factor, including five items (Are you basically satisfied with your life? Are you in good spirits most of the time? Do you feel happy most of the time? Do you think it is wonderful to be alive now? and Do you feel full of energy)? is the most similar across languages (38). In this study, we used the 5 items as an indicator of positive affect and another 10 items as an indicator of negative affect. In a previous study, the Cronbach’s alpha value was 0.72 for the 5 positive affect items and 0.82 for the 10 negative affect items in community-dwelling older adults in Japan (39). All GDS-15 items were assessed in a “yes/no” format. We calculated the sum of the presence of the positive affect and that of the negative affect (yes = 1, no = 0), respectively. In this study, positive (0–5) and negative (0–10) affect summary scores were created. Subjective stress was assessed using a single item (“Do you feel stressed at work or in daily life?”) with four response options: very much = 4, quite a lot = 3, a little = 2, and not at all = 1. In addition, we took attendance in every session and calculated the attendance rate.
A previous study reporting that laughter can decrease HbA1c levels in older adults without diabetes (25) revealed a 0.19% difference in HbA1c changes between the intervention and control groups. A meta-analysis reported that low to moderate–intensity resistance exercises reduced HbA1c levels by 0.23% in individuals with type 2 diabetes (40). Therefore, we assumed a 0.2% difference in the mean decrease in HbA1c levels between the intervention and control groups (standard deviation of 0.2). A sample size of 44 participants (22 in each group) was sufficient to detect the difference of 0.2% between groups using a two-tailed t-test of the difference between means with 90% power and a 5% significant level. The required sample size was 48, considering a dropout rate of 10%.
After baseline measurements were completed, the participants were stratified according to sex and randomly allocated to either the intervention (laughter yoga program and standard therapy) or control (standard therapy only) group in a 1:1 ratio according to a computer-generated sequence. All randomization was carried out by a researcher who was not involved with participant enrollment. Participants were informed of their group assignment after consent and baseline measurements. Outcome assessors were blinded to group allocation.
Data were analyzed according to an intention to treat principle, with the baseline value carried forward for missing data. The differences in baseline characteristics between the two groups were tested using independent samples t tests for continuous variables and chi-square tests for categorical variables. Mann-Whitney U tests were used when the continuous variables were not normally distributed. The changes in measurements between the baseline and the 12-week follow-up in both groups were compared using paired-samples t tests. Unadjusted differences of changes from baseline to the 12-week follow-up between the two groups were analyzed using the independent samples t tests. Differences in changes between the two groups adjusting for age, BMI and each dependent variable value at baseline were analyzed using analysis of covariance. As a further check, per-protocol analyses excluding dropouts were conducted. Attendance rates for laughter yoga program were calculated by dividing the number of sessions attended by the number of sessions prescribed (41). All analyses were conducted using Statistical Package for the Social Sciences (IBM Corporation, Armonk, NY, USA). P-values of less than 0.05 were used to denote statistical significance.
Forty-five eligible participants were enrolled in the study, and 42 agreed to participate in this study and underwent baseline measurements. Twenty-one participants were assigned to the laughter yoga group and 21 participants were assigned to the control group (Figure 1). One person in each group dropped out because of personal reasons. Both groups had high retention rates of 95%. The mean attendance rate for the laughter yoga program was 92.9%. No serious adverse events occurred. No changes in the content of the medical treatment occurred in either group during the study period.
The baseline characteristics of the 42 participants stratified by groups are shown in Table 1. No significant differences in baseline characteristics were observed between the two groups. The Cronbach’s alpha value was 0.70 for the positive affect items and 0.51 for the negative affect items.
Table 2 presents the changes from baseline to 12th week follow-up. The mean HbA1c levels changed from 7.07% to 6.82% in the laughter yoga group and from 7.19% to 7.26% in the control group. The unadjusted difference between the two groups was statistically significant (−0.31%; 95% confidence interval [CI]: −0.54% to −0.09%; P = 0.008). The adjusted difference (adjustment for age, BMI and HbA1c level at baseline) was also significant (P = 0.002). The positive affect score significantly increased in the laughter yoga group (between-group difference: 0.62 points; 95% CI 0.003 to 1.23; P = 0.049), although the adjusted between-group difference (adjustment for age, BMI and positive affect score at baseline) was not statistically significant (P = 0.139). A trend toward an increase in sleep duration was observed in the laughter yoga group with a between-group difference of 0.4 hours (unadjusted: 95% CI −0.05 to 0.86; P = 0.080), and the adjusted difference was marginally significant (P = 0.054). No significant differences in body weight, BMI, waist circumference, negative affect, and subjective stress were found between groups. Per-protocol analyses excluding dropouts and missing data in the follow-up questionnaire revealed a very similar pattern of results for all outcomes (Table 3).
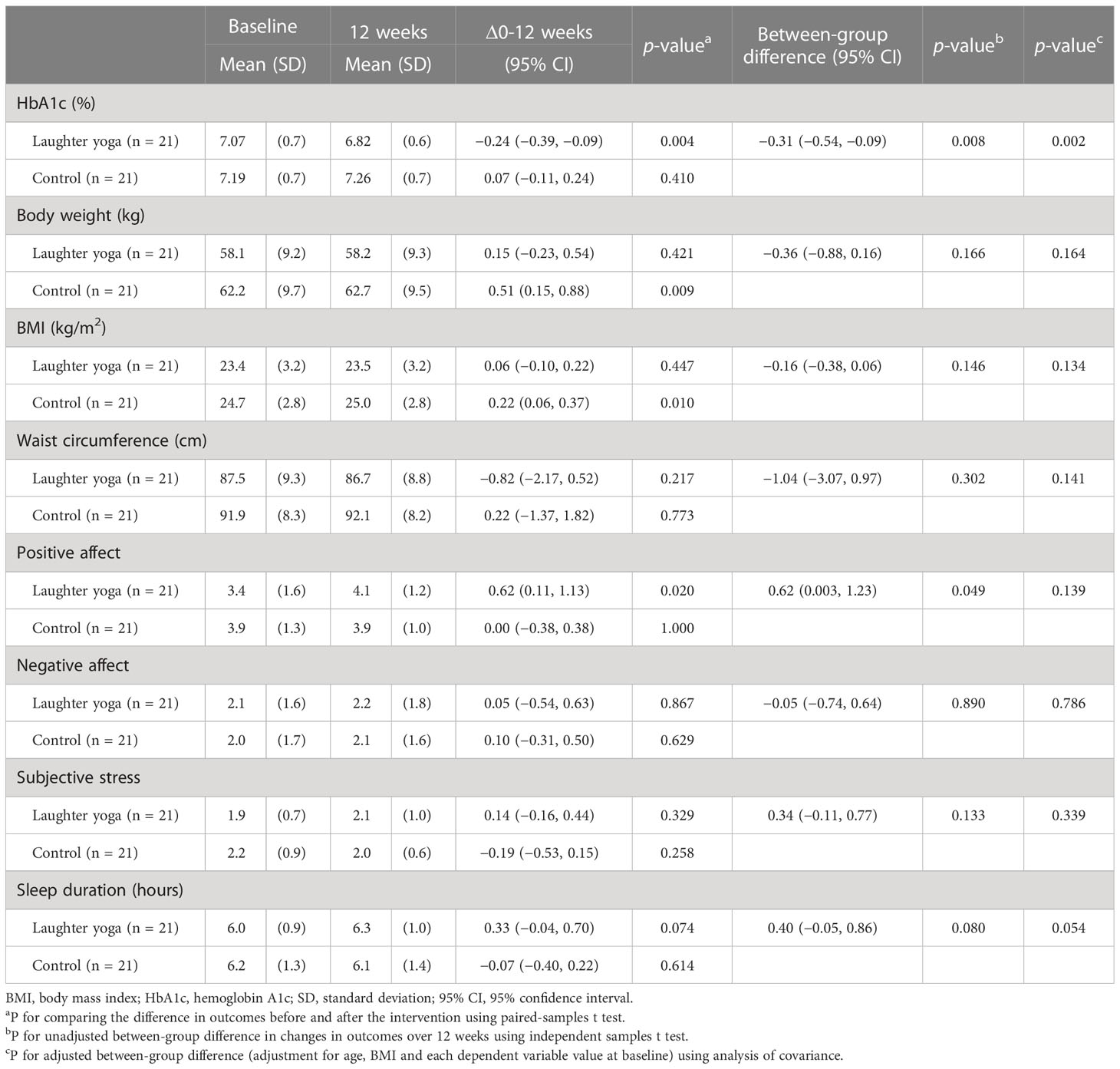
Table 2 Physiological and psychological changes during the intervention in the laughter yoga and control groups.
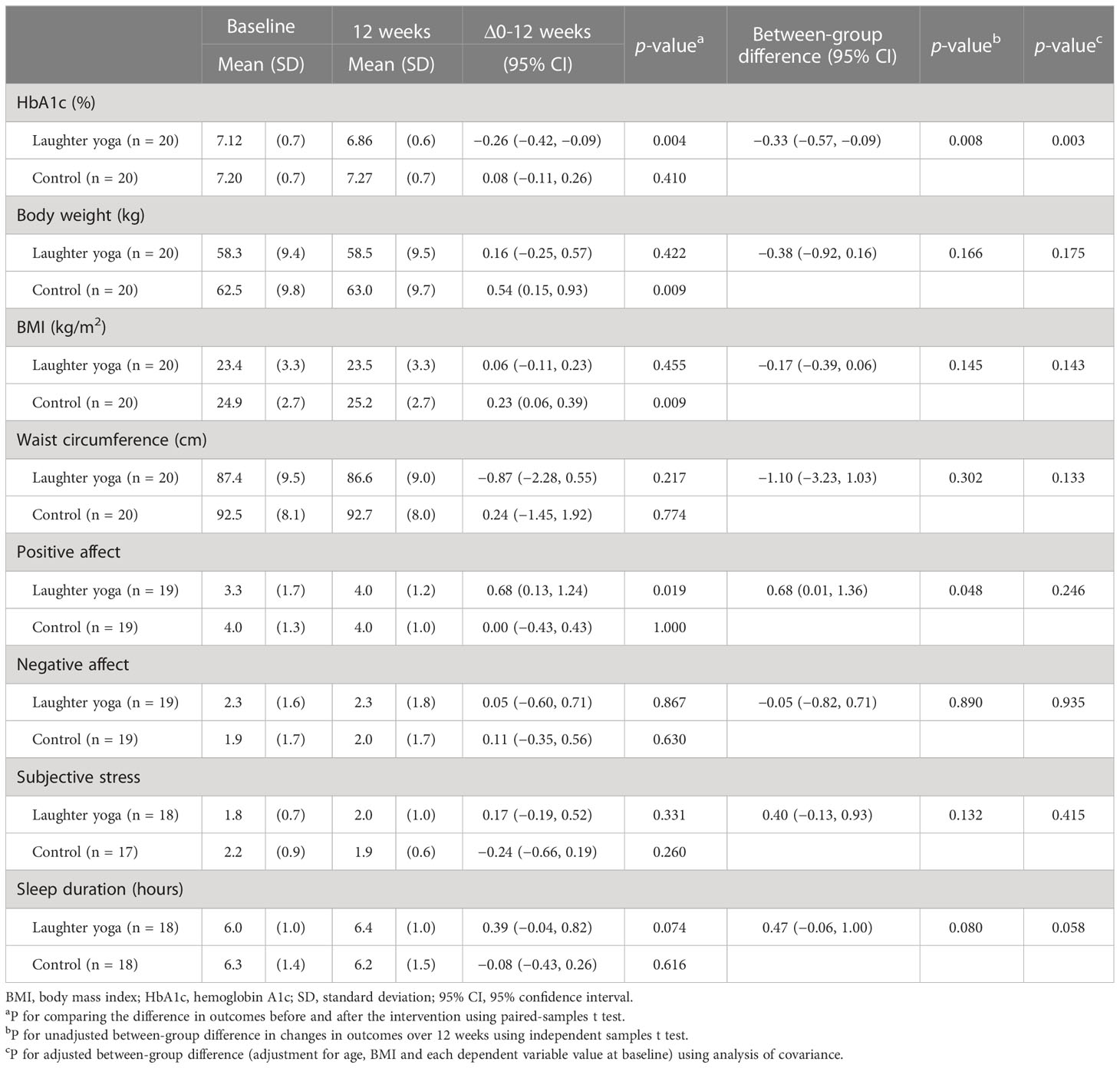
Table 3 Physiological and psychological changes during the intervention in the laughter yoga and control groups using per-protocol analyses.
At baseline and 12-week follow-up, 14 (66.7%) and 19 (90.5%) individuals in the laughter yoga group, and 10 (47.6%) and 8 (38.1%) individuals in the control group reported having exercise at least twice a week, respectively. The number of individuals with exercise habits increased in the laughter yoga group but with no statistical significance. However, the adjusted between-group difference of HbA1c remained statistically significant after adding the change in exercise habits as a covariate. The mean change in HbA1c was 0% in the five participants who reported increased exercise habits and −0.32% in the 16 participants without exercise habit changes. Additionally, the number of individuals who reported eating until full and skipping breakfast was not significantly different between the two groups at baseline and 12-week follow-up (data not shown). The number of individuals who reported eating until full and skipping breakfast remained from baseline to 12-week follow-up in both groups.
The results of this study showed that laughter yoga program for 12 weeks decreased HbA1c levels in individuals with type 2 diabetes. Additionally, the high attendance rate suggests that the program is feasible for the participants. To the best of our knowledge, this is the first randomized controlled trial that has evaluated the long-term effects of laughter yoga on glycemic control in individuals with type 2 diabetes.
The findings of the current study are consistent with previous studies demonstrating that laughter by watching a comedy show for 40 min (21) or a single 30-min session of laughter yoga (33) inhibits the increase in postprandial glucose levels in individuals with type 2 diabetes. The findings are also consistent with our previous study showing that the combination of laughter by watching comedy shows and exercise for 10 weeks decreased HbA1c levels among older adults (25).
The mean HbA1c levels changed from 7.07% to 6.82% in the laughter yoga group. Recent study has shown that maintaining HbA1c levels at <7% over 5 years is associated with significant reductions in the odds of being diagnosed with diabetes-related complications (3). Another study found that the secondary structure of hemoglobin in individuals with good glycemic control (HbA1c < 7.0%) was not significantly altered although elevated HbA1c levels contribute to hemoglobin structural modifications, which are associated with pathological complications in type 2 diabetes mellitus (42). A previous meta-analysis reported that every 1% increase in HbA1c is associated with a 15% increase in the hazard of all-cause mortality, a 25% increase in cardiovascular disease mortality, a 17% increase in cardiovascular diseases, and an 11% increase in stroke, and suggested a positive dose-response trend between HbA1c levels and cardiovascular outcomes in people with type 2 diabetes (5). A recent study in the USA also demonstrated that a 1% reduction in HbA1c is associated with a 13% reduction in diabetes-related total healthcare costs, resulting in an annual cost savings of $736 (43). Thus, changes in HbA1c in this study might be clinically significant in patients with type 2 diabetes.
A meta-analysis found that, in individuals with type 2 diabetes, low-to-moderate-intensity resistance exercise reduced HbA1c levels by 0.23%, and high-intensity resistance exercise reduced HbA1c levels by 0.61% (40). The 0.24% reduction in HbA1c levels in this study is similar to the effects of low-to-moderate-intensity resistance exercise. Another meta-analysis reported a 0.33% reduction in HbA1c levels in a psychological treatment group compared with a control group, and greater improvements in participants with higher baseline HbA1c levels (44). Similarly, a systematic review of healthcare interventions reported a 0.34% reduction in HbA1c levels, and subgroup analysis showed that populations with baseline HbA1c levels > 9.5% exhibited more reduction in HbA1c (0.58%) than populations with baseline HbA1c levels < 9.5% (0.17%) (45). Considering that the average baseline HbA1c level in our study was 7.1%, laughter yoga may be effective as an adjunctive therapy for the management of type 2 diabetes.
Although the mechanisms remain unclear, there are several possibilities for the effect of laughter yoga on diabetes. First, it has been reported that laughter upregulates genes related to natural killer cell activity in individuals with type 2 diabetes, which may ameliorate glucose intolerance (18). Second, laughter could influence glycemic control through the effects of positive affect that accompanies laughter. Positive psychological constructs such as positive affect, optimism and self-efficacy have been suggested to increase adherence to health behaviors (46), which may benefit individuals with type 2 diabetes. A longitudinal cohort study has also reported that positive affect such as enjoyment of life predicts lower risk of mortality in older adults with diabetes (47). In the present study, positive affect significantly increased from baseline to the 12-week follow-up in the laughter yoga group, which might be beneficial for glycemic control. In addition, laughter might have a stress-buffering effect. It has been reported that diabetes-related distress predicts poor glycemic control and poor medication adherence (48). Laughter yoga could attenuate cortisol stress response (30), which might buffer against the negative impact of stress. Third, increased energy expenditure during laughter might be beneficial for glycemic control. A study has suggested that 10–15 min of voiced laughter (by viewing a humorous film) could increase energy expenditure by 10–40 kcal (49). Laughter yoga may increase energy expenditure more than laughter during watching a humorous film, although no studies have examined energy expenditure during laughter yoga.
It has been reported that when people experience positive affect during a specific behavior, they are more likely to continue that behavior (14). The positive affect experienced through laughter yoga may have led to the high attendance rate in the laughter yoga program. Although most health behaviors are difficult to sustain, continuing laughter yoga as a habit may be relatively easy.
In this study, sleep duration tended to improve. This finding is consistent with previous studies reporting that laughter has favorable effects on sleep quality or insomnia. One study has shown that 1 h of laughter therapy once a week for 4 weeks improves insomnia and sleep quality among older individuals (50). Another study has reported that a 30-min laughter yoga session twice weekly for 8 weeks improves sleep quality in patients undergoing hemodialysis (51). Additionally, a significant correlation was observed between changes in sleep duration and HbA1c levels in the laughter yoga group (r = −0.47; P = 0.050). It has been reported that short sleep durations (less than 4.5–6 h/night) are associated with increased HbA1c levels in individuals with type 2 diabetes (52). Thus, the increase in sleep duration in the laughter yoga group might be associated with better glycemic control.
Laughter yoga combines simulated laughter with yoga breathing techniques. The effects of laughter and the effects of yogic breathing are difficult to distinguish because laughter also consists of mixed patterns of expiration, inspiration, and interval pauses (53). It has been reported that voiced laughter causes a 10%–20% increase in energy expenditure and heart rate compared with resting values (49), and may activate sympathetic activity (54). In contrast, most yogic breathing practices result in a parasympathetic shift of autonomic nervous system activity (55). Laughter may have effects similar to exercise, and yogic breathing may enhance the effects of relaxation. However, this study did not measure the heart rate. Further studies are needed to assess the effects of laughter yoga on the autonomic nervous system.
This study conducted a 12-week laughter yoga intervention. In a systematic review of the effects of laughter-inducing interventions, the duration of most laughter yoga interventions ranged 4 to 8 weeks and one study conducted a 12-week laughter yoga intervention (28). Another systematic review of the effects of laughter yoga in older adults reported that the duration of interventions ranged from 4 to 6 weeks (26). To our best knowledge, little is known about the effects of longer-term laughter yoga interventions and it remains unclear which duration of intervention is most effective. It is possible that longer-term intervention is more effective. On the other hand, a systematic review on yoga for type 2 diabetes reported that the duration of yoga intervention ranged one week to 26 weeks (a median of 12 weeks) (56). Additionally, a meta-analysis assessing the effects of yoga intervention on cardiovascular disease risk factors reported that the effects were most prominent in randomized controlled trials with 12 weeks of intervention duration, and fewer effects were found in shorter or longer interventions (36). More studies with various duration of laughter yoga intervention including especially longer-term interventions are needed to examine the most effective intervention duration.
In this study, we did not assess the sustainability of the effects of the intervention after the study period. Further follow-up studies are needed to examine how long the effects of laughter yoga are maintained. A meta-analysis showed that improved physical activity through behavioral change interventions is generally not sustained after the intervention (57). Motivating participants to continue laughter yoga beyond intervention termination would be important (e.g., introducing laughter yoga class in the local community or recommending making a new laughter yoga group).
This study has several limitations. First, the number of participants was small, and the study was conducted in a single center. Multicenter studies with larger sample sizes are needed to better understand the intervention’s efficacy and generalizability. The study participants were all Japanese living in an urban area and outpatients of the university hospital with relatively good glycemic control. Our findings may not apply to different populations, including other ethnic groups, those living in rural areas, and those with poorly controlled type 2 diabetes. Further studies are needed to evaluate the effects of laughter yoga on glycemic control in different populations. In contrast, the effects of laughter yoga on mental health have been reported worldwide (Asia, the Middle East, Australia, and United States) and in different clinical settings (28, 58). Therefore, this intervention could be applied to various populations. Second, changes in unknown psychosocial or lifestyle factors that were not assessed in this study might have affected glycemic outcomes. Additionally, group activity participation might have beneficial effects. Communicating with other participants and developing a sense of community could improve their motivation to attend the intervention. Third, diabetes-related distress was not assessed in this study. Further study is needed to assess distress using validated questionnaires. Fourth, positive and negative affect was measured using items from GDS-15. The Cronbach’s Alpha value in this study was acceptable for the positive affect items, however the value was relatively low for the negative affect items. The Cronbach’s Alpha value is influenced by the number of items, item inter-relatedness, and dimensionality, and a small number of items will underestimate the reliability (59). A study has suggested that a value of 0.50 is satisfactory when the items are fewer than 20 (60). However, using the ten items as one factor may not be suitable for this study population. Negative affect has various types. The factor structure of the GDS-15 has been reported to vary depending on the study population (38). For example, a study among community-dwelling older Japanese reported three factors: depressed mood, positive affect, and energy loss (61). Another study that included home-dwelling poststroke patients in Japan reported two factors: the positive affect and the depressed mood, including lack of energy (62). In addition, although the GDS-15 includes components of positive and negative affect, they might not represent pure positive and negative affect. Fifth, comorbid psychological conditions were not considered in the exclusion criteria. In terms of depression, no individuals received treatment for depression after confirming the medication status, and the baseline scores of the GDS-15 did not indicate depression in any participants. Sixth, sleep duration was self-reported, which might have affected the reliability of the data.
In conclusion, laughter yoga for 12 weeks decreased HbA1c levels in individuals with type 2 diabetes, and the program is feasible with a high attendance rate. The importance of psychological well-being in individuals with diabetes has been gradually recognized, and positive psychological interventions have been recommended (63). We propose that having fun could be a self-care intervention. Although further studies with larger numbers of participants are warranted to better evaluate the beneficial effects, laughter yoga may be applied as an easy, enjoyable, and effective option for self-managing type 2 diabetes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Scientific Ethics Committee of Fukushima Medical University. The patients/participants provided their written informed consent to participate in this study.
MH analyzed and interpreted data, and wrote the manuscript. MH, TO, and YW conducted the study and contributed to data acquisition. TO, EE, KS, HIm, NF, HN, NK, IS, and HIs contributed to the concept and design of the study and participated in critical revision of the manuscript. HN, NK and IS recruited participants and interpreted the diabetes-related outcome measures. MH and TO are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
This research was supported by the Health Science Research Fund by the Ministry of Health, Labour and Welfare (H25-Junkanki-Ippan008) and the Japan Agency for Medical Research and Development under Standard Agreement (15ek0210003h00031 and 22rea522104h0001) and Japan Society for the Promotion of Science (JSPS) KAKENHI under Grant Agreement Nos. 18K19688, 19H03901, and 20K21719.
The authors are grateful to Ms. Yoshiko Takada (chairperson of the Japanese Laughter Yoga organization), Ms. Seiko Ikegawa, and all other staff for their continuous support of the laughter yoga program. Also, we thank all participants involved and staff at Osaka University Hospital and Osaka University for their assistance with the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, et al. Japanese Clinical practice guideline for diabetes 2019. J Diabetes Invest (2020) 11(4):1020–76. doi: 10.1111/jdi.13306
2. DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers (2015) 1:15019. doi: 10.1038/nrdp.2015.19
3. Boye KS, Thieu VT, Lage MJ, Miller H, Paczkowski R. The association between sustained HbA1c control and long-term complications among individuals with type 2 diabetes: A retrospective study. Adv Ther (2022) 39(5):2208–21. doi: 10.1007/s12325-022-02106-4
4. Gebregziabher M, Egede LE, Lynch CP, Echols C, Zhao Y. Effect of trajectories of glycemic control on mortality in type 2 diabetes: A semiparametric joint modeling approach. Am J Epidemiol (2010) 171(10):1090–8. doi: 10.1093/aje/kwq070
5. Zhang Y, Hu G, Yuan Z, Chen L. Glycosylated hemoglobin in relationship to cardiovascular outcomes and death in patients with type 2 diabetes: A systematic review and meta-analysis. PloS One (2012) 7(8):e42551. doi: 10.1371/journal.pone.0042551
6. Blonde L, Aschner P, Bailey C, Ji L, Leiter LA, Matthaei S, et al. Gaps and barriers in the control of blood glucose in people with type 2 diabetes. Diabetes Vasc Dis Res (2017) 14(3):172–83. doi: 10.1177/1479164116679775
7. Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med (2021) 384(23):2219–28. doi: 10.1056/NEJMsa2032271
8. Tajima N, Nishimura R, Izumi K, Hayashino Y, Origasa H, Noda M, et al. A large-scale, observational study to investigate the current status of diabetes complications and their prevention in Japan: Research outline and baseline data for type 2 diabetes-JDCP study 1. Diabetol Int (2015) 6:243–51. doi: 10.1007/s13340-015-0223-1
9. Lipska KJ, Yao X, Herrin J, McCoy RG, Ross JS, Steinman MA, et al. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006-2013. Diabetes Care (2017) 40(4):468–75. doi: 10.2337/dc16-0985
10. Al-Salmi N CP, D'Souza MS. Diet adherence among adults with type 2 diabetes mellitus: A concept analysis. Oman Med J (2022) 37(2):e361. doi: 10.5001/omj.2021.69
11. da Rocha RB, Silva CS, Cardoso VS. Self-care in adults with type 2 diabetes mellitus: A systematic review. Curr Diabetes Rev (2020) 16(6):598–607. doi: 10.2174/1573399815666190702161849
12. Schmidt SK, Hemmestad L, MacDonald CS, Langberg H, Valentiner LS. Motivation and barriers to maintaining lifestyle changes in patients with type 2 diabetes after an intensive lifestyle intervention (The U-TURN trial): A longitudinal qualitative study. Int J Environ Res Public Health (2020) 17(20). doi: 10.3390/ijerph17207454
13. Van Cappellen P, Rice EL, Catalino LI, Fredrickson BL. Positive affective processes underlie positive health behaviour change. Psychol Health (2018) 33(1):77–97. doi: 10.1080/08870446.2017.1320798
14. Kiviniemi MT, Voss-Humke AM, Seifert AL. How do I feel about the behavior? the interplay of affective associations with behaviors and cognitive beliefs as influences on physical activity behavior. Health psychology: Off J Division Health Psychology Am Psychol Assoc (2007) 26(2):152–8. doi: 10.1037/0278-6133.26.2.152
15. Lawton R, Conner M, McEachan R. Desire or reason: Predicting health behaviors from affective and cognitive attitudes. Health psychology: Off J Division Health Psychology Am Psychol Assoc (2009) 28(1):56–65. doi: 10.1037/a0013424
16. Rhodes RE, Kates A. Can the affective response to exercise predict future motives and physical activity behavior? a systematic review of published evidence. Ann Behav medicine: A Publ Soc Behav Med (2015) 49(5):715–31. doi: 10.1007/s12160-015-9704-5
17. Bennett MP, Zeller JM, Rosenberg L, McCann J. The effect of mirthful laughter on stress and natural killer cell activity. Altern therapies Health Med (2003) 9(2):38–45.
18. Hayashi T, Tsujii S, Iburi T, Tamanaha T, Yamagami K, Ishibashi R, et al. Laughter up-regulates the genes related to NK cell activity in diabetes. Biomed Res (2007) 28(6):281–5. doi: 10.2220/biomedres.28.281
19. Takahashi K, Iwase M, Yamashita K, Tatsumoto Y, Ue H, Kuratsune H, et al. The elevation of natural killer cell activity induced by laughter in a crossover designed study. Int J Mol Med (2001) 8(6):645–50. doi: 10.3892/ijmm.8.6.645
20. Kimata H. Effect of humor on allergen-induced wheal reactions. Jama (2001) 285(6):738. doi: 10.1001/jama.285.6.738
21. Hayashi K, Hayashi T, Iwanaga S, Kawai K, Ishii H, Shoji S, et al. Laughter lowered the increase in postprandial blood glucose. Diabetes Care (2003) 26(5):1651–2. doi: 10.2337/diacare.26.5.1651
22. Sakurada K, Konta T, Watanabe M, Ishizawa K, Ueno Y, Yamashita H, et al. Associations of frequency of laughter with risk of all-cause mortality and cardiovascular disease incidence in a general population: Findings from the yamagata study. J Epidemiol (2020) 30(4):188–93. doi: 10.2188/jea.JE20180249
23. Tamada Y, Takeuchi K, Yamaguchi C, Saito M, Ohira T, Shirai K, et al. Does laughter predict onset of functional disability and mortality among older Japanese adults? the JAGES prospective cohort study. J Epidemiol (2021) 31(5):301–7. doi: 10.2188/jea.JE20200051
24. Gonot-Schoupinsky FN, Garip G. Laughter and humour interventions for well-being in older adults: A systematic review and intervention classification. Complement Ther Med (2018) 38:85–91. doi: 10.1016/j.ctim.2018.04.009
25. Hirosaki M, Ohira T, Kajiura M, Kiyama M, Kitamura A, Sato S, et al. Effects of a laughter and exercise program on physiological and psychological health among community-dwelling elderly in Japan: Randomized controlled trial. Geriatr Gerontol Int (2013) 13(1):152–60. doi: 10.1111/j.1447-0594.2012.00877.x
26. Kuru Alici N, Arikan Donmez A. A systematic review of the effect of laughter yoga on physical function and psychosocial outcomes in older adults. Complement Ther Clin Pract (2020) 41:101252. doi: 10.1016/j.ctcp.2020.101252
27. van der Wal CN, Kok RN. Laughter-inducing therapies: Systematic review and meta-analysis. Soc Sci Med (2019) 232:473–88. doi: 10.1016/j.socscimed.2019.02.018
28. Stiwi K, Rosendahl J. Efficacy of laughter-inducing interventions in patients with somatic or mental health problems: A systematic review and meta-analysis of randomized-controlled trials. Complement Ther Clin Pract (2022) 47:101552. doi: 10.1016/j.ctcp.2022.101552
29. Bressington D, Mui J, Yu C, Leung SF, Cheung K, Wu CST, et al. Feasibility of a group-based laughter yoga intervention as an adjunctive treatment for residual symptoms of depression, anxiety and stress in people with depression. J Affect Disord (2019) 248:42–51. doi: 10.1016/j.jad.2019.01.030
30. Meier M, Wirz L, Dickinson P, Pruessner JC. Laughter yoga reduces the cortisol response to acute stress in healthy individuals. Stress (2021) 24(1):44–52. doi: 10.1080/10253890.2020.1766018
31. Tanaka A, Tokuda N, Ichihara K. Psychological and physiological effects of laughter yoga sessions in Japan: A pilot study. Nurs Health Sci (2018) 20(3):304–12. doi: 10.1111/nhs.12562
32. Dolgoff-Kaspar R, Baldwin A, Johnson MS, Edling N, Sethi GK. Effect of laughter yoga on mood and heart rate variability in patients awaiting organ transplantation: A pilot study. Altern Ther Health Med (2012) 18(5):61–6.
33. Čokolič M, Herodež Š, Sternad S, Krebs S. The inhibitory effect of laughter yoga on the increase in postprandial blood glucose in type2 diabetic patients. Diabetol Croat (2013) 42(2):54–8.
34. Araki E, Haneda M, Kasuga M, Nishikawa T, Kondo T, Ueki K, et al. New glycemic targets for patients with diabetes from the Japan diabetes society. Diabetol Int (2016) 7(4):327–30. doi: 10.1007/s13340-016-0297-4
36. Cramer H, Lauche R, Haller H, Steckhan N, Michalsen A, Dobos G. Effects of yoga on cardiovascular disease risk factors: A systematic review and meta-analysis. Int J Cardiol (2014) 173(2):170–83. doi: 10.1016/j.ijcard.2014.02.017
37. Niino N, Imaizumi T, Kawakami N. A Japanese translation of the geriatric depression scale. Clin Gerontologist (1991) 10:85–7.
38. Kim G, DeCoster J, Huang CH, Bryant AN. A meta-analysis of the factor structure of the geriatric depression scale (GDS): The effects of language. Int Psychogeriatr (2013) 25(1):71–81. doi: 10.1017/S1041610212001421
39. Hirosaki M, Ishimoto Y, Kasahara Y, Konno A, Kimura Y, Fukutomi E, et al. Positive affect as a predictor of lower risk of functional decline in community-dwelling elderly in Japan. Geriatr Gerontol Int (2013) 13(4):1051–8. doi: 10.1111/ggi.12008
40. Liu Y, Ye W, Chen Q, Zhang Y, Kuo CH, Korivi M. Resistance exercise intensity is correlated with attenuation of HbA1c and insulin in patients with type 2 diabetes: A systematic review and meta-analysis. Int J Environ Res Public Health (2019) 16(1). doi: 10.3390/ijerph16010140
41. Witlox L, Velthuis MJ, Boer JH, Steins Bisschop CN, Wall EV, Meulen WJTMV, et al. Attendance and compliance with an exercise program during localized breast cancer treatment in a randomized controlled trial: The PACT study. PloS One (2019) 14(5):e0215517. doi: 10.1371/journal.pone.0215517
42. Ye S, Ruan P, Yong J, Shen H, Liao Z, Dong X. The impact of the HbA1c level of type 2 diabetics on the structure of haemoglobin. Sci Rep (2016) 6:33352. doi: 10.1038/srep33352
43. Lage MJ, Boye KS. The relationship between HbA1c reduction and healthcare costs among patients with type 2 diabetes: Evidence from a U.S. claims database. Curr Med Res Opin (2020) 36(9):1441–7. doi: 10.1080/03007995.2020.1787971
44. Winkley K, Upsher R, Stahl D, Pollard D, Kasera A, Brennan A, et al. Psychological interventions to improve self-management of type 1 and type 2 diabetes: A systematic review. Health Technol Assess. (2020) 24(28):1–232. doi: 10.3310/hta24280
45. Murphy ME, Byrne M, Galvin R, Boland F, Fahey T, Smith SM. Improving risk factor management for patients with poorly controlled type 2 diabetes: A systematic review of healthcare interventions in primary care and community settings. BMJ Open (2017) 7(8):e015135. doi: 10.1136/bmjopen-2016-015135
46. Massey CN, Feig EH, Duque-Serrano L, Huffman JC. Psychological well-being and type 2 diabetes. Curr Res Diabetes Obes J (2017) 4(4). doi: 10.19080/crdoj.2017.04.555641
47. Moskowitz JT, Epel ES, Acree M. Positive affect uniquely predicts lower risk of mortality in people with diabetes. Health psychology: Off J Division Health Psychology Am psychol Assoc (2008) 27(1S):S73–82. doi: 10.1037/0278-6133.27.1.S73
48. Aikens JE. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care (2012) 35(12):2472–8. doi: 10.2337/dc12-0181
49. Buchowski MS, Majchrzak KM, Blomquist K, Chen KY, Byrne DW, Bachorowski JA. Energy expenditure of genuine laughter. Int J Obes (2007) 31(1):131–7. doi: 10.1038/sj.ijo.0803353
50. Ko HJ, Youn CH. Effects of laughter therapy on depression, cognition and sleep among the community-dwelling elderly. Geriatr Gerontol Int (2011) 11(3):267–74. doi: 10.1111/j.1447-0594.2010.00680.x
51. Ozer Z, Ates S. Effects of laughter yoga on hemodialysis patients' plasma-beta endorphin levels, pain levels and sleep quality: A randomized controlled trial. Complementary Ther Clin Pract (2021) 43:101382. doi: 10.1016/j.ctcp.2021.101382
52. Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Med Rev (2017) 31:91–101. doi: 10.1016/j.smrv.2016.02.001
53. Miller M, Fry WF. The effect of mirthful laughter on the human cardiovascular system. Med Hypotheses (2009) 73(5):636–9. doi: 10.1016/j.mehy.2009.02.044
54. Sakuragi S, Sugiyama Y, Takeuchi K. Effects of laughing and weeping on mood and heart rate variability. J Physiol Anthropol Appl Hum Sci (2002) 21(3):159–65. doi: 10.2114/jpa.21.159
55. Saoji AA, Raghavendra BR, Manjunath NK. Effects of yogic breath regulation: A narrative review of scientific evidence. J Ayurveda Integr Med (2019) 10(1):50–8. doi: 10.1016/j.jaim.2017.07.008
56. Thind H, Lantini R, Balletto BL, Donahue ML, Salmoirago-Blotcher E, Bock BC, et al. The effects of yoga among adults with type 2 diabetes: A systematic review and meta-analysis. Prev Med (2017) 105:116–26. doi: 10.1016/j.ypmed.2017.08.017
57. McEwan D, Rhodes RE, Beauchamp MR. What happens when the party is over?: Sustaining physical activity behaviors after intervention cessation. Behav Med (2022) 48(1):1–9. doi: 10.1080/08964289.2020.1750335
58. Bressington D, Yu C, Wong W, Ng TC, Chien WT. The effects of group-based laughter yoga interventions on mental health in adults: A systematic review. J Psychiatr Ment Health Nurs (2018) 25(8):517–27. doi: 10.1111/jpm.12491
59. Tavakol M, Dennick R. Making sense of cronbach's alpha. Int J Med Educ (2011) 2:53–5. doi: 10.5116/ijme.4dfb.8dfd
60. Dall'Oglio AM, Rossiello B, Coletti MF, Caselli MC, Rava L, di Ciommo V, et al. Developmental evaluation at age 4: Validity of an Italian parental questionnaire. J Paediatr Child Health (2010) 46(7-8):419–26. doi: 10.1111/j.1440-1754.2010.01748.x
61. Yatomi N. The factor structure and item characteristics of the GDS (Geriatric depression scale) short version in a Japanese elderly sample. Jpn J Geriatr (1994) 16:29–36.
62. Schreiner AS, Morimoto T, Asano H. Depressive symptoms among poststroke patients in Japan: Frequency distribution and factor structure of the GDS. Int J Geriatr Psychiatry (2001) 16(10):941–9. doi: 10.1002/gps.444
Keywords: type 2 diabetes, laughter, laughter yoga, glycemic control, self-care, positive affect
Citation: Hirosaki M, Ohira T, Wu Y, Eguchi E, Shirai K, Imano H, Funakubo N, Nishizawa H, Katakami N, Shimomura I and Iso H (2023) Laughter yoga as an enjoyable therapeutic approach for glycemic control in individuals with type 2 diabetes: A randomized controlled trial. Front. Endocrinol. 14:1148468. doi: 10.3389/fendo.2023.1148468
Received: 20 January 2023; Accepted: 14 March 2023;
Published: 31 March 2023.
Edited by:
Celestino Sardu, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Yukihiro Fujita, Shiga University of Medical Science, JapanCopyright © 2023 Hirosaki, Ohira, Wu, Eguchi, Shirai, Imano, Funakubo, Nishizawa, Katakami, Shimomura and Iso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mayumi Hirosaki, bWF5dW1pMjNnb2dvQHlhaG9vLmNvLmpw; Tetsuya Ohira, ZndnZTExMTlAbmlmdHkuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.