
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Endocrinol., 29 September 2023
Sec. Translational and Clinical Endocrinology
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1120475
With the global epidemic and prevention of the COVID-19, long COVID-19 sequelae and its comprehensive prevention have attracted widespread attention. Long COVID-19 sequelae refer to that three months after acute COVID-19, the test of SARS-CoV-2 is negative, but some symptoms still exist, such as cough, prolonged dyspnea and fatigue, shortness of breath, palpitations and insomnia. Its pathological mechanism is related to direct viral damage, immunopathological response, endocrine and metabolism disorders. Although there are more effective methods for treating COVID-19, the treatment options available for patients with long COVID-19 remain quite limited. Psychophysical therapies, such as exercise, oxygen therapy, photobiomodulation, and meditation, have been attempted as treatment modalities for long COVID-19, which have the potential to promote recovery through immune regulation, antioxidant effects, and neuroendocrine regulation. Neuroendocrine regulation plays a significant role in repairing damage after viral infection, regulating immune homeostasis, and improving metabolic activity in patients with long COVID-19. This review uses oxytocin as an example to examine the neuroendocrine mechanisms involved in the psychophysical therapies of long COVID-19 syndrome and proposes a psychophysical strategy for the treatment of long COVID-19.
The coronavirus disease 2019 (COVID-19) has not only a high morbidity and mortality, but also long-lasting sequelae that affect multiple systems, constitute intense obstacle for normal daily life and work, and impose huge burden to the healthcare system. Many cohort studies have shown that following the acute phase of COVID-19, 40–90% of patients have chronic symptoms that last more than three weeks after recovering from active infection although they exhibit negative test results for SARS-CoV-2 in conventional throat and nose swab COVID test (1–4). If these symptoms last beyond 12 weeks after acquiring the infection, with no alternative diagnosis, the patients are considered as having a long COVID-19 (5, 6). However, the drug therapies administrated in managing the symptoms and rehabilitation of the long COVID-19 sequelae commonly have limited therapeutic effectiveness (7). The non-drug therapies, mainly psychophysical therapies were recently employed for the rehabilitation of long COVID-19. Psychophysical therapy involves various mechanisms, including promotion of cell metabolism, modulation of immune cell activity, anti-oxidation, and neuroendocrine regulation (8, 9). Notably, COVID-19 has been shown to significantly impact neuroendocrine function, with chemosensory dysfunction being one of the most common symptoms observed (10, 11). Based on this fact, we propose that psychophysical therapy utilizing neuroendocrine mechanisms may offer an effective approach to treat long COVID-19.
This article aims to explore the pathological processes and clinical manifestations of long COVID-19, the role and mechanisms of psychophysical therapy, and the potential use of oxytocin as an example of how neuroendocrine hormones can aid in the rehabilitation of long COVID-19 through psychophysical therapy.
People with long COVID-19 involve almost all the organ systems (12). The occurrence of long COVID-19 is closely associated with viral invasion and immunological injury, poor control of complications, cardiopulmonary and cerebral sequelae as well as social stress (13). The factors involving direct and indirect pathogenesis of SARS-CoV-2 and symptoms of long COVID-19 sequelae are summarized in Figure 1.
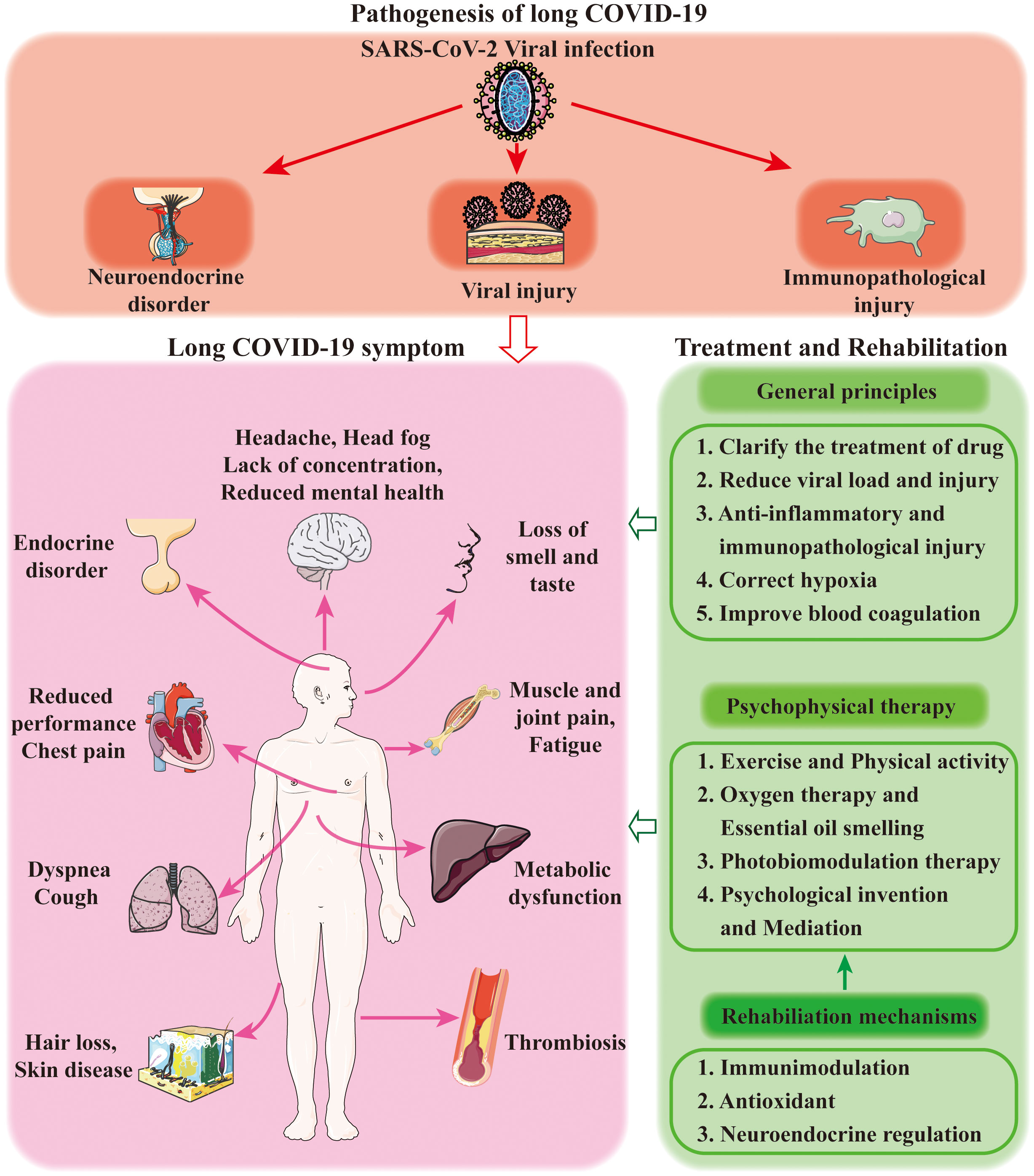
Figure 1 Diagrammatic summary of the common symptoms, pathogenesis and treatments of long COVID-19 sequelae.
The SARS-CoV-2 infection causes prompt and direct damage to the tissues while SARS-CoV-2 RNA has been identified in fecal specimens of patients with COVID-19 during and beyond the acute phase (13). Virus-specific pathological variations specifically affect oxidative stress, immunological function, impaired diffusional O2 conductance and inflammation (14). Many symptoms of long COVID-19 occur or do not recover completely after the acute phase, including pulmonary fibrosis, endothelial damage, microvascular injury, brain fog, cardiac damage, muscle weakness, poor exercise tolerance and reduced sex steroid secretion and infertility (15). Moreover, different organ systems respond to SARS-CoV-2 infection differently. For example, in the cardiovascular system, alongside direct virus-induced injuries, inflammatory plaque instability and plaque rupture can contribute to myocardial infarction-induced long COVID-19 complications. Vascular leakage is related to SARS-CoV-2 induced clot formation in association with activation of Factor XIIa, complements and platelets, endothelial dysfunction, immune cell responses with cytokine-mediated action (16).Viruses and autoantibodies can damage the midbrain sympathetic center and change adrenergic and muscarinic neurotransmission, cause a hyper-adrenergic state and peripheral denervation, and result in blood pooling in the lower extremities and reflex tachycardia (17).In long COVID-19, the olfactory bulbs and taste buds are among the first organs infected by SARS-CoV-2, and thus anosmia and hypogeusia are the typical findings in the patients (18). Notably, anosmia and hypogeusia are also COVID-19-specific anxiety risk factors (19). In addition, long-intensive care syndrome and medical or clinical sequelae can contribute to long COVID-19 (20). Moreover, the reduced hypothalamic neural activity in long COVID-19 patients is likely because of olfactory bulb-mediated viral infection of the hypothalamus (21). It was identified that SARS-CoV-2 infection has significant longitudinal effects on greater changes in global brain structure, and a greater cognitive decline or the loss of sensory input due to anosmia in the patients (22).
Immune system dysregulation can manifest as hyperinflammation, cytokine storm, and immune-mediated multi-system damage. These effects can cause the aggregation of inflammatory cells and the release of pro-inflammatory and pro-fibrotic cytokines/factors (23). The inflammation can also cause secondary hemophagocytic lymphohistiocytosis, arthritis, skin psoriasis, systemic lupus erythematosus, Grave’s diseases, and immune thrombocytopenic purpura (24). Notably, there are at least 14 pentapeptides shared by the SARS-CoV-2 S-protein, thyroid, pituitary, adrenal cortex autoantigens and beta-cells of the islets of Langerhans. They all belong to the immunoreactive epitopes of SARS-CoV-2 and thus account for COVID-19 associated autoimmune endocrinopathies, such as autoimmune thyroid disease and autoimmunity against adrenals (25). In addition, vaccine-induced immunological reactions are also involved in long COVID-19, such as immune thrombotic thrombocytopenia (26). A specific endocrine event in long COVID-19 is the increased angiotensin II (ATII) levels due to the loss of ACE2 in response to SARS-CoV-2 invasion. Increased ATII can cause neutrophil accumulation, vascular hyper-permeability, pulmonary edema, the profibrotic, proapoptotic and proinflammatory signalizations in the lungs and other organs (27). Thus, increased ATII level is also an important etiology of long COVID-19 symptoms. In addition, viruses can also reduce autophagy to influence metabolism and macromolecule recycling processes while causing excessive inflammatory and autoimmune responses, as observed in long COVID-19 patients (28). By contrast, effective control of metabolic complications could prove useful therapeutic targets for combating COVID-19 (29).
Endocrine disorders are a dramatic feature of long COVID-19. Angiotensin converse enzyme 2 (ACE2) is the primary receptor of SARS-CoV-2. The expression of ACE2 in the hypothalamus, pituitary, pancreas, thyroid, adrenal glands, testes, and ovaries makes these endocrine organs become a target for viral injury. As a result of SARS-CoV-2 attacks, there are significant decreases in hypothalamic metabolism (30), cortisol and adrenocorticotropic hormone (31), total triiodothyronine and thyroid stimulating hormone (TSH) (18), testosterone (32), and estrogen (33) levels. The extensive damage to the whole endocrine system in turn worsens immunological and metabolic disorders, such as insulin resistance and hyperglycemia in COVID-19 patients (34). In addition, histamine and histamine H2 receptor signaling is likely essential for spike protein to induce ACE2 internalization in endothelial cells and cause endothelial dysfunction (35). These endocrine problems can extend into the long COVID-19, such as hyperthyroidism, hyperglycemia and adrenal insufficiency (32). SARS-CoV-2 infection can shift cellular metabolism from oxidative phosphorylation to glycolysis and decrease ATP generation. ATP depletion contributes not only to the multiple organ failure during the acute phase, but also to elevating the susceptibility of patients with diabetes to this virus, involving immune cells and alleviating therapeutic effectiveness against SARS-CoV-2 infection (36).
According to the above changes, the sequelae of the long COVID-19 may consider as a syndrome based on damage after virus infection and neuroendocrine, immune and other disorders (37).
Currently, most long COVID-19 patients are mainly treated by general practitioners. The physiological and psychological rehabilitation and treatments are considered primarily to treatment of most frequently seen symptoms of fatigue, reduced performance, poor and loss of smell and taste, or lack of concentration and so on in long COVID-19 (38).
Long COVID-19 requires multidisciplinary rehabilitation, including pulmonary, cardiac, sport and exercise medicine, psychological, musculoskeletal, neurological rehabilitation and general medical management (39). In the actual practice of managing long COVID-19 sequelae, psychological and physical therapies are increasingly recognized, with a focus on combating mental, respiratory and neuromuscular dysfunctions.
Six major therapeutic goals for long COVID-19 therapy based on the pathogenic mechanisms of SARS-CoV-2 should be considered (40). The first goal is determining the indicators of testing and therapy for COVID-19 patients, such as the COVID-19 molecular biomarkers and symptoms, and oxygen saturation (41). The second goal is correction of the COVID-19 patient’s hypoxia (42). The third goal is to reduce the viral load of SARS-CoV-2 by using an oral antiviral agent at early stage of COVID-19, such as molnupiravir and paxlovid pill (43). The fourth goal is to identify and address the hyperinflammation phase for those with fever and elevated C-reactive protein. Low-dose dexamethasone therapy can be an effective treatment (44). The fifth goal is to identify and address the hypercoagulability phase seen in many hospitalized COVID-19 patients with a marked increase in d-dimer and prothrombin time and a decrease in fibrinogen. Low molecular weight heparin is preferred in COVID-19 patients (45). The last goal is prophylaxis of persons without infection by using of supplements of vitamin D, vitamin C, resveratrol, and zinc (46).
These goals are essential for the prevention of long COVID-19 sequelae. For example, there was a dramatic improvement in disease severity, radiology, and pulmonary function following corticosteroids and concurrent exercise training (39). In patients who received steroid treatment, there is a mean relative increase in transfer factor following treatment of 31.6% and forced vital capacity of 9.6%, with significant symptomatic and radiological improvement (47). To correct disseminated intravascular coagulation-like phase, anticoagulation therapy with unfractionated heparin is preferred, particularly in COVID-19 patients with acute kidney injuries. Anticoagulation therapy can markedly increase d-dimer and prothrombin time with a decrease in fibrinogen. In addition, cell therapy with mesenchymal stem cells or resident lung epithelial stem/progenitor cells has been developed to prevent long-acute sequelae of COVID-19, with both pros and cons (48).
In general, outpatient rehabilitation of long COVID-19 includes exercise therapy, respiratory rehabilitation, photobiomodulation (PBM) therapy, psychological support such as meditation. Other rehabilitation includes essential oil smelling, activities of daily living and gait training, education, traditional Chinese medicine, and cognitive and vocational rehabilitation (49, 50). Some patients need medications to address problems such as dizziness or headaches, and others need a referral to a heart or lung specialist for further treatment. Still, others receive mental health treatment for anxiety, depression or insomnia, like physical therapy, speech therapy, rehabilitation psychology, vocational rehabilitation and social work.
Exercise programs and physical activities are well-known modulators of the clinical manifestations and prognosis of many chronic diseases. Regular exercise in resistance and cardiopulmonary training methods may improve many of these symptoms of long COVID-19 (51). For instance, aerobic training exercises can improve muscle strength, kinesiophobia and quality of life measures in long COVID-19 sarcopenia, particularly low-intensity aerobic training (52). The recovery of the musculoskeletal system using musculoskeletal physical therapy is able to resume a long COVID-19 woman’s daily physical activities (53). Increasing the aerobic capacity can decrease psychological problems commonly seen in people with long COVID-19 and increase immune functions by modulating the levels of glucocorticoid, oxytocin, insulin, and thyroid hormones (54). A short running exercise significantly increased the level of salivary oxytocin (55). Similarly, running wheel in mice for six weeks significantly increases oxytocin levels in the brain and serum (female only) (56).
The effect of exercise can be achieved through the following mechanisms. Exercise could stimulate the immune system and induce mitochondrial adaptations, cell generation and immune surveillance. It can also treat pulmonary complications effectively by relieving dyspnea and fatigue. Exercise can also improve cardiovascular health by enhancing mitochondrial biogenesis and function, restoring and improving vasculature, and the release of myokines from skeletal muscle. At last, stimulate brain plasticity and increases psychological well-being by improving the quality of life, controlling depression and anxiety (51).
Oxygen therapy stresses on daily monitoring, non-invasive ventilation and continuous positive airways pressure delivery, pronation and longural changes to improve oxygenation, reconditioning with leg/arm cranking and exercises, initial and final patients’ functional assessment by short-physical performance battery and 1-minute sit-to-stand test to evaluate the long COVID-19 patient’s motor conditions and exercise-induced oxygen desaturation (57). Over the course of the long COVID-19 patient’s rehabilitation, exertional dyspnea, 6-min walking distance, 3-min sit-to-stand test, hyperventilation syndrome prevalence and quality of life significantly improved (58). Correspondingly, corticosteroids have been used extensively in the alleviation of acute and chronic syndromes of COVID-19 while physical therapy can decrease oxygen therapy and corticosteroid requirements during rehabilitation (59), suggesting recovery of adrenal functions and corticosteroid secretion.
Hypothalamic oxytocin neurons receive excitatory inputs from the olfactory bulbs (OBs) and the accessory OBs. Intranasally-applied oxytocin can activate oxytocin neurons by the mediation of lateral olfactory tracts (60). By contrast, olfaction deficits correlate with negative symptoms and low social drive (61), which can account for the aberrant mental activity in long COVID with anosmia. Thus, by acting on the OBs, odorants can extensively modulate brain activity, at least partially by changing hypothalamic oxytocin neuronal activity.
Studies in humans and animals have demonstrated that many odorants can increase oxytocin secretion. For example, salivary oxytocin concentrations increase significantly after exposure to aroma of certain essential oils, including lavender, neroli, jasmine absolute, roman chamomile, clary sage, and Indian sandalwood than after exposure to the control odor in postmenopausal women (62). Consistently, inhalation of lavender essential oil can ameliorate the depression-like behavior, and increase the dendritic complexity of immature neurons in the hippocampus and the subventricular zone under high corticosterone conditions (63). These effects are associated with increased oxytocin in serum (64). Rosemary extract can significantly increase central oxytocin and its receptor expressions, attenuate stress-induced changes in serum corticosterone and decrease depressive- and anxiety-like behavior in mice (65). Together with the fact that essential oils have anti-inflammatory, immunomodulatory, bronchodilatory, and antiviral properties (66), these essential oils are readily applicable for promoting the rehabilitation of long COVID directly and by increasing oxytocin secretion indirectly.
Recent studies on the therapeutic effects of PBM therapy in humans and animals indicate that it plays a pivotal role in long COVID-19 rehabilitation (67). LED illumination can improve skin diseases, arthritis, and osteoporosis, promote wound healing repair, participate in immune regulation (67), and increase neuroendocrine hormone secretion (68). The red and near-infrared radiation can reduce the lethality of COVID-19 (69) and this effect is associated with its reducing lung inflammation and accelerating the regeneration of damaged tissues (70). Importantly, red and near-infrared illumination through LED devices can be used to directly mobilize hormone secretion and improve pathological conditions.
So far, PBM therapy has been applied in clinical trials. It has shown good curative effect in the prevention, early treatment and the recovery of the symptoms of COVID-19 (71, 72). Clinical experimental studies have confirmed that PBM has shown good curative effects in pulmonary function rehabilitation, breathing regulation, and taste rehabilitation (73). Different studies use different wavelengths such as notably blue, red, and near-infrared light. The mechanism of PBM in treating COVID-19 is mainly manifested in the regulation of inflammatory factors, anti-oxidation and regulation of endocrine hormones (74, 75). Furthermore, topical methylene blue photodynamic virus inactivation (MB-PDI) administered in the oral and nasal cavity, combined with oral methylene blue (MB) and photobiomodulation, exerts systemic antiviral effects in patients with long-standing COVID-19 sequelae (76). The combined application of PBM and microneedle can also improve the hair loss symptoms of long-term COVID-19 syndrome (77).
A “Recovering from COVID” course of 7-week virtual rehabilitation takes a whole system, biopsychosocial approach to understanding COVID-19 and long-viral fatigue and is delivered by an interdisciplinary team. The course focuses on understanding long-viral fatigue, sleep optimization, nutrition, swallowing, activity management, energy conservation, stress management, breathing optimization, managing setbacks, and sign longing to appropriate resources and services. Rehabilitation is effective in reversing some of the problems faced by people living with long COVID-19 (78). In the management of anxiety in COVID-19, the general approach focuses on compassionate, similar to that during trauma or disaster, with efforts focused on instilling a sense of hope and resilience (19).
The AYUSH system proposed by the Indian government includes yoga and natural remedies to relieve post-COVID symptoms, improve lung function, improve quality of life and reduce stress (79). Mindfulness meditation is practiced widely to promote physical and mental health through cognitive performance. Observations have verified its improvements of anxiety, depression and pain scores with low-cost as well as its feasibility to practice during COVID-19 pandemic (80). It can be practiced in combination with Yogic breathing to reduce symptoms and COVID-19-associated anxiety in patients receiving dialysis. In the college population, individuals who participated in a 4-week online centering intervention showed improved of stress levels and trait mindfulness over time (81). It is also identified that mindfulness-based training can effectively mitigate the negative psychological consequences of the COVID-19 outbreak, help restore well-being in the most vulnerable individuals and have psychological well-being among nurses working for COVID-19 patients (82). All these source effects can be mediated by increasing central oxytocin actions (83).
These psychophysical therapies presented above are closely related to the inherent immunity (84) and metabolism as well as neuroendocrine activities in patients with long COVID-19 (85). Analyzing the mechanisms underlying psychophysical therapies for long COVID-19 reveals that changes in neuroendocrine activity underlie the effectiveness of these therapies. We propose a neuroendocrine mechanism for psychophysical therapies in the rehabilitation of long COVID-19. Specifically, we introduce the role of hormones, using oxytocin as an example, in the neuroendocrine mechanism of psychophysical therapies for the treatment of long COVID-19.
Endocrine disorders can cause physical and mental problems, whereas oxytocin can exert such functions directly and indirectly by modulating the activity of other endocrine activities. By contrast, oxytocin has antiviral effects and anti-inflammation without the long-term side-effect of corticosteroids. Thus, oxytocin can inhibit hypothalamic–pituitary–adrenal (HPA) axis activity while reserving immune-protective effects (86). Thus, the application of oxytocin at different stages of long COVID-19 in males and females can exert the effect of prevention and/or treatment of long COVID-19 sequelae. In females, oxytocin may prevent the occurrence of COVID-19 by increasing estrogen release and decreasing ACE2 expression; in males, oxytocin can reduce inflammation-evoked injury by increasing androgen release and suppressing humoral immunity (87). Although it is unclear how oxytocin affects HPA axis activity under pathological conditions, the inhibitory role of oxytocin may improve long COVID-19 sequelae of Grave’s disease that has an overproduction of thyroid hormones (88). In addition, oxytocin can reduce norepinephrine levels and thus possibly weaken stress reactions and hypertension in long COVID-19 sequelae (89). Oxytocin can increase insulin secretion by directly innervating the islets of Langerhans in the pancreas (90), maintaining β-cell adaptation reactivity (91) and increasing vagal activity (92), thereby promoting metabolic hemostasis, particularly helping control hyperglycemia in long COVID-19 (93). Metabolic disorders are important etiology of long COVID-19 sequelae alongside mitochondrial dysfunction (94). Oxytocin can compensate for tryptophan insufficiency-associated long COVID-19 sequelae (94). Together with the other reviews (95, 96), these findings indicate that oxytocin can improve long COVID-19 sequelae by regulating the activity of the endocrine system.
Pathogenesis underlying long COVID-19 sequelae at different organ systems vary dramatically. Oxytocin can exert protective effects through various approaches, such as promoting tissue repairs and regeneration. Oxytocin may help clear residual or hidden SARS-CoV-2 by inducing antiviral immune cell responses, as shown in the effect of Carbetocin and by blocking the interaction between SARS-CoV-2 spike protein and ACE2 (97). In pediatric patients, the long COVID-19 symptoms mainly exhibit difficulties with sustained auditory attention and divided attention while most of these patients have preexisting attention and/or mood concerns and some have elevated depression and anxiety symptoms (98). By exerting this function, oxytocin can also alleviate pain reactions in long COVID-19 (99). In addition, oxytocin can increase the expression of pulmonary surfactants, promote angiogenesis and regeneration of infarcted cardiomyocytes, prevent atherosclerosis and coronary artery disease, and many other complications associated with long COVID-19, thereby becoming a strong candidate hormone to improve long COVID-19 sequelae (95). Immune system dysregulation causes tissue damages through hyperinflammation, cytokine storm syndrome, and immune-mediated multi-system damage. It is well known that Oxytocin treatment can weaken the neuroinflammatory process (100). Oxytocin inhibits LPS-induced inflammation and attenuates microglial activation in LPS-treated mice (101), which provides long-term neuroprotection and likely alleviates brain neurological symptoms in long COVID-19 (102).
Long COVID-19 is the sequelae in COVID-19 survivors and significantly influences the healthcare system (103). However, current understandings of the pathogenesis and rehabilitation strategy remain quite limited (104). By analyzing the underlying mechanisms of psychophysical therapies for long COVID-19, a common involvement of neuroendocrine activity is revealed (Figure 1). In view of the diverse clinical manifestations of COVID-19 and long COVID-19, it is recommended that individualized treatment should be considered in both inpatient treatment (community hospitals and general hospitals) and out-of-hospital treatment (family treatment) during psychophysical therapies (105). At the same time, it is recommended to use ICF (International Classification of Functioning, Disability and Health), a method proposed by WHO in 1996 to describe the health status of patients based on biological, psychological and social perspectives, to accurately evaluate the effect of psychophysical therapy and choose physical psychotherapy methods on the sequelae of long COVID-19.
QM and WS contributed equally to this work and wrote the first manuscript. QM, WS, LC, FMZ, and YFW contributed to the critical revision of the manuscript. FMZ, and YFW conceived the study and edited the text. All authors approved the submitted version.
This work was supported by the National Key Research and Development Program of China (2022YFB3604705, FMZ). The work was supported by the grant of the Russian Science Foundation, N# 22-15-00113, https://rscf.ru/project/22-15-00113/ accessed on 13 May 2022.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA (2020) 324(6):603–5. doi: 10.1001/jama.2020.12603
2. Huang L, Yao Q, Gu X, Wang Q, Ren L, Wang Y, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet (2021) 398(10302):747–58. doi: 10.1016/S0140-6736(21)01755-4
3. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet (2021) 397(10270):220–32. doi: 10.1016/S0140-6736(20)32656-8
4. Osmanov IM, Spiridonova E, Bobkova P, Gamirova A, Shikhaleva A, Andreeva M, et al. Risk factors for post-COVID-19 condition in previously hospitalised children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur Respir J (2022) 59(2):2101341. doi: 10.1183/13993003.01341-2021
5. Montani D, Savale L, Noel N, Meyrignac O, Colle R, Gasnier M, et al. Post-acute COVID-19 syndrome. Eur Respir Rev (2022) 31(163):210185. doi: 10.1183/16000617.0185-2021
6. Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol (2023) 21(3):133–46. doi: 10.1038/s41579-022-00846-2
7. Adeloye D, Elneima O, Daines L, Poinasamy K, Quint JK, Walker S, et al. The long-term sequelae of COVID-19: an international consensus on research priorities for patients with pre-existing and new-onset airways disease. Lancet Respir Med (2021) 9(12):1467–78. doi: 10.1016/S2213-2600(21)00286-1
8. Mahalakshmi B, Maurya N, Lee SD, Bharath Kumar V. Possible neuroprotective mechanisms of physical exercise in neurodegeneration. Int J Mol Sci (2020) 21(16):5895. doi: 10.3390/ijms21165895
9. Carvalho GF, Schwarz A, Szikszay TM, Adamczyk WM, Bevilaqua-Grossi D, Luedtke K. Physical therapy and migraine: musculoskeletal and balance dysfunctions and their relevance for clinical practice. Braz J Phys Ther (2020) 24(4):306–17. doi: 10.1016/j.bjpt.2019.11.001
10. Esmaeilzadeh A, Elahi R, Siahmansouri A, Maleki AJ, Moradi A. Endocrine and metabolic complications of COVID-19: lessons learned and future prospects. J Mol Endocrinol (2022) 69(3):R125–R50. doi: 10.1530/JME-22-0036
11. Caretta A, Mucignat-Caretta C. Are multiple chemosensory systems accountable for COVID-19 outcome? J Clin Med (2021) 10(23):5601. doi: 10.3390/jcm10235601
12. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis (2022) 22(4):e102–e7. doi: 10.1016/S1473-3099(21)00703-9
13. Merad M, Blish CA, Sallusto F, Iwasaki A. The immunology and immunopathology of COVID-19. Sci (New York NY) (2022) 375(6585):1122–7. doi: 10.1126/science.abm8108
14. Dotan A, David P, Arnheim D, Shoenfeld Y. The autonomic aspects of the post-COVID19 syndrome. Autoimmun Rev (2022) 21(5):103071. doi: 10.1016/j.autrev.2022.103071
15. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. Bmj (2021) 374:n1648. doi: 10.1136/bmj.n1648
16. Veluswamy P, Wacker M, Stavridis D, Reichel T, Schmidt H, Scherner M, et al. The SARS-coV-2/receptor axis in heart and blood vessels: A crisp update on COVID-19 disease with cardiovascular complications. Viruses (2021) 13(7):1346. doi: 10.3390/v13071346
17. Ståhlberg M, Reistam U, Fedorowski A, Villacorta H, Horiuchi Y, Bax J, et al. Post-COVID-19 tachycardia syndrome: A distinct phenotype of post-acute COVID-19 syndrome. Am J Med (2021) 134(12):1451–6. doi: 10.1016/j.amjmed.2021.07.004
18. de Melo GD, Lazarini F, Levallois S, Hautefort C, Michel V, Larrous F, et al. COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci Transl Med (2021) 13(596):eabf8396. doi: 10.1126/scitranslmed.abf8396
19. Uzunova G, Pallanti S, Hollander E. Presentation and management of anxiety in individuals with acute symptomatic or asymptomatic COVID-19 infection, and in the post-COVID-19 recovery phase. Int J Psychiatry Clin Pract (2021) 25(2):115–31. doi: 10.1080/13651501.2021.1887264
20. Yong SJ, Liu S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev Med Virol (2022) 32(4):e2315. doi: 10.1002/rmv.2315
21. Pascual-Goñi E, Fortea J, Martínez-Domeño A, Rabella N, Tecame M, Gómez-Oliva C, et al. COVID-19-associated ophthalmoparesis and hypothalamic involvement. Neurol Neuroimmunol Neuroinflamm (2020) 7(5):e823. doi: 10.1212/NXI.0000000000000823
22. Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature (2022) 604(7907):697–707. doi: 10.1038/s41586-022-04569-5
23. Huang WJ, Tang XX. Virus infection induced pulmonary fibrosis. J Transl Med (2021) 19(1):496. doi: 10.1186/s12967-021-03159-9
24. Utrero-Rico A, González-Cuadrado C, Chivite-Lacaba M, Cabrera-Marante O, Laguna-Goya R, Almendro-Vazquez P, et al. Alterations in circulating monocytes predict COVID-19 severity and include chromatin modifications still detectable six months after recovery. Biomedicines (2021) 9(9):1253. doi: 10.3390/biomedicines9091253
25. Churilov LP, Normatov MG, Utekhin VJ. Molecular mimicry between SARS-coV-2 and human endocrinocytes: A prerequisite of post-COVID-19 endocrine autoimmunity? Pathophysiology (2022) 29(3):486–94. doi: 10.3390/pathophysiology29030039
26. Perry RJ, Tamborska A, Singh B, Craven B, Marigold R, Arthur-Farraj P, et al. Cerebral venous thrombosis after vaccination against COVID-19 in the UK: a multicentre cohort study. Lancet (2021) 398(10306):1147–56. doi: 10.1016/S0140-6736(21)01608-1
27. Sahu S, Patil CR, Kumar S, Apparsundaram S, Goyal RK. Role of ACE2-Ang (1-7)-Mas axis in post-COVID-19 complications and its dietary modulation. Mol Cell Biochem (2022) 477(1):225–40. doi: 10.1007/s11010-021-04275-2
28. Williams CG, Jureka AS, Silvas JA, Nicolini AM, Chvatal SA, Carlson-Stevermer J, et al. Inhibitors of VPS34 and fatty-acid metabolism suppress SARS-CoV-2 replication. Cell Rep (2021) 36(5):109479. doi: 10.1016/j.celrep.2021.109479
29. Mahrooz A, Muscogiuri G, Buzzetti R, Maddaloni E. The complex combination of COVID-19 and diabetes: pleiotropic changes in glucose metabolism. Endocrine (2021) 72(2):317–25. doi: 10.1007/s12020-021-02729-7
30. Guedj E, Million M, Dudouet P, Tissot-Dupont H, Bregeon F, Cammilleri S, et al. (18)F-FDG brain PET hypometabolism in post-SARS-CoV-2 infection: substrate for persistent/delayed disorders? Eur J Nucl Med Mol Imaging (2021) 48(2):592–5. doi: 10.1007/s00259-020-04973-x
31. Alzahrani AS, Mukhtar N, Aljomaiah A, Aljamei H, Bakhsh A, AlSudani N, et al. The impact of COVID-19 viral infection on the hypothalamic-pituitary-adrenal axis. Endocr Pract (2021) 27(2):83–9. doi: 10.1016/j.eprac.2020.10.014
32. Al-Kuraishy HM, Al-Gareeb AI, Faidah H, Alexiou A, Batiha GE. Testosterone in COVID-19: an adversary bane or comrade boon. Front Cell Infect Microbiol (2021) 11:666987. doi: 10.3389/fcimb.2021.666987
33. Al-Lami RA, Urban RJ, Volpi E, Algburi AMA, Baillargeon J. Sex hormones and novel corona virus infectious disease (COVID-19). Mayo Clin Proc (2020) 95(8):1710–4. doi: 10.1016/j.mayocp.2020.05.013
34. Ilias I, Diamantopoulos A, Pratikaki M, Botoula E, Jahaj E, Athanasiou N, et al. Glycemia, beta-cell function and sensitivity to insulin in mildly to critically ill covid-19 patients. Med (Kaunas) (2021) 57(1):68. doi: 10.3390/medicina57010068
35. Raghavan S, Leo MD. Histamine potentiates SARS-coV-2 spike protein entry into endothelial cells. Front Pharmacol (2022) 13:872736. doi: 10.3389/fphar.2022.872736
36. Miller L, Berber E, Sumbria D, Rouse BT. Controlling the burden of COVID-19 by manipulating host metabolism. Viral Immunol (2022) 35(1):24–32. doi: 10.1089/vim.2021.0150
37. França K, Lotti TM. Psycho-neuro-endocrine-immunology: A psychobiological concept. Adv Exp Med Biol (2017) 996:123–34. doi: 10.1007/978-3-319-56017-5_11
38. Schrimpf A, Braesigk A, Lippmann S, Bleckwenn M. Management and treatment of long COVID symptoms in general practices: An online-based survey. Front Public Health (2022) 10:937100. doi: 10.3389/fpubh.2022.937100
39. Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med (2020) 54(16):949–59. doi: 10.1136/bjsports-2020-102596
40. Stratton CW, Tang YW, Lu H. Pathogenesis-directed therapy of 2019 novel coronavirus disease. J Med Virol (2021) 93(3):1320–42. doi: 10.1002/jmv.26610
41. Les Bujanda I, Loureiro-Amigo J, Bastons FC, Guerra IE, Sánchez JA, Murgadella-Sancho A, et al. Treatment of COVID-19 pneumonia with glucocorticoids (CORTIVID): a structured summary of a study protocol for a randomised controlled trial. Trials (2021) 22(1):43. doi: 10.1186/s13063-020-04999-4
42. Mortaz E, Malkmohammad M, Jamaati H, Naghan PA, Hashemian SMR, Tabarsi P, et al. Correction to: Silent hypoxia: higher NO in red blood cells of COVID-19 patients. BMC Pulm Med (2020) 20(1):294. doi: 10.1186/s12890-020-01326-0
43. Couzin-Frankel J. Antiviral pills could change pandemic's course. Sci (New York NY) (2021) 374(6569):799–800. doi: 10.1126/science.acx9605
44. Hasan SS, Kow CS, Mustafa ZU, Merchant HA. Does methylprednisolone reduce the mortality risk in hospitalized COVID-19 patients? A meta-analysis of randomized control trials. Expert Rev Respir Med (2021) 15(8):1049–55. doi: 10.1080/17476348.2021.1925546
45. Castillo-Perez M, Jerjes-Sanchez C, Castro-Varela A, Paredes-Vazquez JG, Vazquez-Garza E, Ramos-Cazares RE, et al. Differences between surviving and non-surviving venous thromboembolism COVID-19 patients: a systematic review. Thromb J (2021) 19(1):101. doi: 10.1186/s12959-021-00346-y
46. Di Matteo G, Spano M, Grosso M, Salvo A, Ingallina C, Russo M, et al. Food and COVID-19: preventive/co-therapeutic strategies explored by current clinical trials and in silico studies. Foods (2020) 9(8):1036. doi: 10.3390/foods9081036
47. Myall KJ, Mukherjee B, Castanheira AM, Lam JL, Benedetti G, Mak SM, et al. Persistent post-COVID-19 interstitial lung disease. An observational study of corticosteroid treatment. Ann Am Thorac Soc (2021) 18(5):799–806. doi: 10.1513/AnnalsATS.202008-1002OC
48. Zhao F, Ma Q, Yue Q, Chen H. SARS-coV-2 infection and lung regeneration. Clin Microbiol Rev (2022) 35(2):e0018821. doi: 10.1128/cmr.00188-21
49. Thomas P, Baldwin C, Beach L, Bissett B, Boden I, Cruz SM, et al. Physiotherapy management for COVID-19 in the acute hospital setting and beyond: an update to clinical practice recommendations. J Physiother (2022) 68(1):8–25. doi: 10.1016/j.jphys.2021.12.012
50. Webber SC, Tittlemier BJ, Loewen HJ. Apparent discordance between the epidemiology of COVID-19 and recommended outcomes and treatments: A scoping review. Phys Ther (2021) 101(11):pzab155. doi: 10.1093/ptj/pzab155
51. Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz Martínez BJ, et al. Post-COVID-19 syndrome and the potential benefits of exercise. Int J Environ Res Public Health (2021) 18(10):5329. doi: 10.3390/ijerph18105329
52. Nambi G, Abdelbasset WK, Alrawaili SM, Elsayed SH, Verma A, Vellaiyan A, et al. Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia: A randomized controlled trial. Clin Rehabil (2022) 36(1):59–68. doi: 10.1177/02692155211036956
53. Santos S, Flores JA. Musculoskeletal physiotherapy in physical sequelae of SARS-CoV-2 infection: A case report. Physiother Res Int (2022) 27(2):e1938. doi: 10.1002/pri.1938
54. Amro M, Mohamed A, Alawna M. Effects of increasing aerobic capacity on improving psychological problems seen in patients with COVID-19: a review. Eur Rev Med Pharmacol Sci (2021) 25(6):2808–21. doi: 10.26355/eurrev_202103_25443
55. Jong TR, Menon R, Bludau A, Grund T, Biermeier V, Klampfl SM, et al. Salivary oxytocin concentrations in response to running, sexual self-stimulation, breastfeeding and the TSST: The Regensburg Oxytocin Challenge (ROC) study. Psychoneuroendocrinology (2015) 62:381–8. doi: 10.1016/j.psyneuen.2015.08.027
56. Yüksel O, Ateş M, Kızıldağ S, Yüce Z, Koç B, Kandiş S, et al. Regular aerobic voluntary exercise increased oxytocin in female mice: the cause of decreased anxiety and increased empathy-like behaviors. Balkan Med J (2019) 36(5):257–62. doi: 10.4274/balkanmedj.galenos.2019.2018.12.87
57. Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil (2020) 99(9):769–74. doi: 10.1097/PHM.0000000000001505
58. Bouteleux B, Henrot P, Ernst R, Grassion L, Raherison-Semjen C, Beaufils F, et al. Respiratory rehabilitation for Covid-19 related persistent dyspnoea: A one-year experience. Respir Med (2021) 189:106648. doi: 10.1016/j.rmed.2021.106648
59. Bordas-Martínez J, Luzardo-González A, Arencibia A, Tormo F, Matéu L, Vicens-Zygmunt V, et al. Effects of early physical therapy and follow-up in acute severe coronavirus disease 2019 pneumonia: A retrospective observational study. Front Med (Lausanne) (2022) 9:866055. doi: 10.3389/fmed.2022.866055
60. Yeomans DC, Hanson LR, Carson DS, Tunstall BJ, Lee MR, Tzabazis AZ, et al. Nasal oxytocin for the treatment of psychiatric disorders and pain: achieving meaningful brain concentrations. Transl Psychiatry (2021) 11(1):388. doi: 10.1038/s41398-021-01511-7
61. Woolley JD, Lam O, Chuang B, Ford JM, Mathalon DH, Vinogradov S. Oxytocin administration selectively improves olfactory detection thresholds for lyral in patients with schizophrenia. Psychoneuroendocrinology (2015) 53:217–22. doi: 10.1016/j.psyneuen.2014.12.018
62. Tarumi W, Shinohara K. The effects of essential oil on salivary oxytocin concentration in postmenopausal women. J Altern Complement Med (2020) 26(3):226–30. doi: 10.1089/acm.2019.0361
63. Cavanagh HM, Wilkinson JM. Biological activities of lavender essential oil. Phytother Res (2002) 16(4):301–8. doi: 10.1002/ptr.1103
64. Sánchez-Vidaña DI, Po KK, Fung TK, Chow JK, Lau WK, So PK, et al. Lavender essential oil ameliorates depression-like behavior and increases neurogenesis and dendritic complexity in rats. Neurosci Lett (2019) 701:180–92. doi: 10.1016/j.neulet.2019.02.042
65. Sasaki K, Ferdousi F, Fukumitsu S, Kuwata H, Isoda H. Antidepressant- and anxiolytic-like activities of Rosmarinus officinalis extract in rodent models: Involvement of oxytocinergic system. BioMed Pharmacother (2021) 144:112291. doi: 10.1016/j.biopha.2021.112291
66. Asif M, Saleem M, Saadullah M, Yaseen HS, Al Zarzour R. COVID-19 and therapy with essential oils having antiviral, anti-inflammatory, and immunomodulatory properties. Inflammopharmacology (2020) 28(5):1153–61. doi: 10.1007/s10787-020-00744-0
67. Enwemeka CS, Bumah VV, Masson-Meyers DS. Light as a potential treatment for pandemic coronavirus infections: A perspective. J Photochem Photobiol B (2020) 207:111891. doi: 10.1016/j.jphotobiol.2020.111891
68. Ciosek J, Drobnik J. Function of the hypothalamo-neurohypophysial system in rats with myocardial infarction is modified by melatonin. Pharmacol Rep (2012) 64(6):1442–54. doi: 10.1016/S1734-1140(12)70942-8
69. Fernandes AB, de Lima CJ, Villaverde A, Pereira PC, Carvalho HC, Zângaro RA. Photobiomodulation: shining light on COVID-19. Photobiomodul Photomed Laser Surg (2020) 38(7):395–7. doi: 10.1089/photob.2020.4882
70. Nejatifard M, Asefi S, Jamali R, Hamblin MR, Fekrazad R. Probable positive effects of the photobiomodulation as an adjunctive treatment in COVID-19: A systematic review. Cytokine (2021) 137:155312. doi: 10.1016/j.cyto.2020.155312
71. Vetrici MA, Mokmeli S, Bohm AR, Monici M, Sigman SA. Evaluation of adjunctive photobiomodulation (PBMT) for COVID-19 pneumonia via clinical status and pulmonary severity indices in a preliminary trial. J Inflammation Res (2021) 14:965–79. doi: 10.2147/JIR.S301625
72. Williams RK, Raimondo J, Cahn D, Williams A, Schell D. Whole-organ transdermal photobiomodulation (PBM) of COVID-19: A 50-patient case study. J Biophotonics (2022) 15(2):e202100194. doi: 10.1002/jbio.202100194
73. De Marchi T, Frâncio F, Ferlito JV, Weigert R, de Oliveira C, Merlo AP, et al. Effects of photobiomodulation therapy combined with static magnetic field in severe COVID-19 patients requiring intubation: A pragmatic randomized placebo-controlled trial. J Inflammation Res (2021) 14:3569–85. doi: 10.2147/JIR.S318758
74. Kitchen LC, Berman M, Halper J, Chazot P. Rationale for 1068 nm photobiomodulation therapy (PBMT) as a novel, non-invasive treatment for COVID-19 and other coronaviruses: roles of NO and hsp70. Int J Mol Sci (2022) 23(9):5221. doi: 10.3390/ijms23095221
75. Aguida B, Pooam M, Ahmad M, Jourdan N. Infrared light therapy relieves TLR-4 dependent hyper-inflammation of the type induced by COVID-19. Commun Integr Biol (2021) 14(1):200–11. doi: 10.1080/19420889.2021.1965718
76. Garcez AS, Delgado MGT, Sperandio M, Dantas ESFT, de Assis JSR, Suzuki SS. Photodynamic therapy and photobiomodulation on oral lesion in patient with coronavirus disease 2019: A case report. Photobiomodul Photomed Laser Surg (2021) 39(6):386–9. doi: 10.1089/photob.2020.4977
77. Gentile P. Preliminary investigation on micro-needling with low-level LED therapy and growth factors in hair loss related to COVID-19. J Clin Med (2022) 11(19):5760. doi: 10.3390/jcm11195760
78. Harenwall S, Heywood-Everett S, Henderson R, Godsell S, Jordan S, Moore A, et al. Post-covid-19 syndrome: improvements in health-related quality of life following psychology-led interdisciplinary virtual rehabilitation. J Prim Care Community Health (2021) 12:21501319211067674. doi: 10.1177/21501319211067674
79. Tillu G, Salvi S, Patwardhan B. AYUSH for COVID-19 management. J Ayurveda Integr Med (2020) 11(2):95–6. doi: 10.1016/j.jaim.2020.06.012
80. Bursky M, Kosuri M, Walsh Carson K, Babad S, Iskhakova A, Nikulina V. The utility of meditation and mindfulness-based interventions in the time of COVID-19: A theoretical proposition and systematic review of the relevant prison, quarantine and lockdown literature. Psychol Rep (2023) 126(2):557–600. doi: 10.1177/00332941211048734
81. Dorais S, Gutierrez D. The effectiveness of a centering meditation intervention on college stress and mindfulness: A randomized controlled trial. Front Psychol (2021) 12:720824. doi: 10.3389/fpsyg.2021.720824
82. Matiz A, Fabbro F, Paschetto A, Cantone D, Paolone AR, Crescentini C. Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. Int J Environ Res Public Health (2020) 17(18):6450. doi: 10.3390/ijerph17186450
83. Bellosta-Batalla M, Del Carmen Blanco-Gandía M, Rodríguez-Arias M, Cebolla A, Pérez-Blasco J, Moya-Albiol L. Brief mindfulness session improves mood and increases salivary oxytocin in psychology students. Stress Health (2020) 36(4):469–77. doi: 10.1002/smi.2942
84. Dean E, Söderlund A, Gosselink R, Jones AYM, Yu HP, Skinner M. Immuno-modulation with lifestyle behaviour change to reduce SARS-CoV-2 susceptibility and COVID-19 severity: goals consistent with contemporary physiotherapy practice. Physiotherapy (2022) 114:63–7. doi: 10.1016/j.physio.2021.08.006
85. Bottaccioli AG, Bottaccioli F, Minelli A. Stress and the psyche-brain-immune network in psychiatric diseases based on psychoneuroendocrineimmunology: a concise review. Ann N Y Acad Sci (2019) 1437(1):31–42. doi: 10.1111/nyas.13728
86. Imami AS, O'Donovan SM, Creeden JF, Wu X, Eby H, McCullumsmith CB, et al. Oxytocin's anti-inflammatory and proimmune functions in COVID-19: a transcriptomic signature-based approach. Physiol Genomics (2020) 52(9):401–7. doi: 10.1152/physiolgenomics.00095.2020
87. Diep PT. Is there an underlying link between COVID-19, ACE2, oxytocin and vitamin D? Med Hypotheses (2021) 146:110360. doi: 10.1016/j.mehy.2020.110360
88. Korompoki E, Gavriatopoulou M, Hicklen RS, Ntanasis-Stathopoulos I, Kastritis E, Fotiou D, et al. Epidemiology and organ specific sequelae of post-acute COVID19: A narrative review. J Infect (2021) 83(1):1–16. doi: 10.1016/j.jinf.2021.05.004
89. Rabow S, Hjorth U, Schönbeck S, Olofsson P. Effects of oxytocin and anaesthesia on vascular tone in pregnant women: a randomised double-blind placebo-controlled study using non-invasive pulse wave analysis. BMC Pregnancy Childbirth (2018) 18(1):453. doi: 10.1186/s12884-018-2029-1
90. Paiva L, Lozic M, Allchorne A, Grinevich V, Ludwig M. Identification of peripheral oxytocin-expressing cells using systemically applied cell-type specific adeno-associated viral vector. J Neuroendocrinol (2021) 33(5):e12970. doi: 10.1111/jne.12970
91. Gu P, Lin Y, Wan Q, Su D, Shu Q. Oxytocin signal contributes to the adaptative growth of islets during gestation. Endocr Connect (2021) 10(7):694–706. doi: 10.1530/EC-21-0043
92. Tolentino M, Palheta-Junior RC, Silva CMS, Cavalcante AKM, Quetz JDS, Havt A, et al. Role of cholecystokinin and oxytocin in slower gastric emptying induced by physical exercise in rats. Physiol Behav (2021) 233:113355. doi: 10.1016/j.physbeh.2021.113355
93. Reiterer M, Rajan M, Gómez-Banoy N, Lau JD, Gomez-Escobar LG, Ma L, et al. Hyperglycemia in acute COVID-19 is characterized by insulin resistance and adipose tissue infectivity by SARS-CoV-2. Cell Metab (2021) 33(11):2174–88.e5. doi: 10.1016/j.cmet.2021.09.009
94. Ramakrishnan RK, Kashour T, Hamid Q, Halwani R, Tleyjeh IM. Unraveling the mystery surrounding post-acute sequelae of COVID-19. Front Immunol (2021) 12:686029. doi: 10.3389/fimmu.2021.686029
95. Wang SC, Wang YF. Cardiovascular protective properties of oxytocin against COVID-19. Life Sci (2021) 270:119130. doi: 10.1016/j.lfs.2021.119130
96. Li T, Wang P, Wang SC, Wang YF. Approaches mediating oxytocin regulation of the immune system. Front Immunol (2016) 7:693. doi: 10.3389/fimmu.2016.00693
97. Tsegay KB, Adeyemi CM, Gniffke EP, Sather DN, Walker JK, Smith SEP. A repurposed drug screen identifies compounds that inhibit the binding of the COVID-19 spike protein to ACE2. Front Pharmacol (2021) 12:685308. doi: 10.3389/fphar.2021.685308
98. Morrow AK, Ng R, Vargas G, Jashar DT, Henning E, Stinson N, et al. Postacute/long COVID in pediatrics: development of a multidisciplinary rehabilitation clinic and preliminary case series. Am J Phys Med Rehabil (2021) 100(12):1140–7. doi: 10.1097/PHM.0000000000001896
99. Saito H, Hidema S, Otsuka A, Suzuki J, Kumagai M, Kanaya A, et al. Effects of oxytocin on responses to nociceptive and non-nociceptive stimulation in the upper central nervous system. Biochem Biophys Res Commun (2021) 574:8–13. doi: 10.1016/j.bbrc.2021.08.042
100. Reguilón MD, Ferrer-Pérez C, Miñarro J, Rodríguez-Arias M. Oxytocin reverses ethanol consumption and neuroinflammation induced by social defeat in male mice. Horm Behav (2021) 127:104875. doi: 10.1016/j.yhbeh.2020.104875
101. Yuan L, Liu S, Bai X, Gao Y, Liu G, Wang X, et al. Oxytocin inhibits lipopolysaccharide-induced inflammation in microglial cells and attenuates microglial activation in lipopolysaccharide-treated mice. J Neuroinflammation (2016) 13(1):77. doi: 10.1186/s12974-016-0541-7
102. Mairesse J, Zinni M, Pansiot J, Hassan-Abdi R, Demene C, Colella M, et al. Oxytocin receptor agonist reduces perinatal brain damage by targeting microglia. Glia (2019) 67(2):345–59. doi: 10.1002/glia.23546
103. Brown K, Yahyouche A, Haroon S, Camaradou J, Turner G. Long COVID and self-management. Lancet (2022) 399(10322):355. doi: 10.1016/S0140-6736(21)02798-7
104. Scheiber B, Spiegl C, Wiederin C, Schifferegger E, Schiefermeier-Mach N. Post-COVID-19 rehabilitation: perception and experience of Austrian physiotherapists and physiotherapy students. Int J Environ Res Public Health (2021) 18(16):8730. doi: 10.3390/ijerph18168730
Keywords: sequelae, psychophysical therapies, hormone, rehabilitation, long COVID-19
Citation: Meng Q-T, Song W-Q, Churilov LP, Zhang F-M and Wang Y-F (2023) Psychophysical therapy and underlying neuroendocrine mechanisms for the rehabilitation of long COVID-19. Front. Endocrinol. 14:1120475. doi: 10.3389/fendo.2023.1120475
Received: 14 December 2022; Accepted: 11 September 2023;
Published: 29 September 2023.
Edited by:
Alfonso J. Rodriguez-Morales, Fundacion Universitaria Autónoma de las Américas, ColombiaReviewed by:
Tridibesh Tripathy, Lucknow University, IndiaCopyright © 2023 Meng, Song, Churilov, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng-Min Zhang, ZmVuZ21pbnpoYW5nQGVtcy5ocmJtdS5lZHUuY24=; Yu-Feng Wang, MjAyMzEwNTlAemNtdS5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.