- 1Division of Endocrinology, Diabetes and Metabolism, Virginia Commonwealth University Health System, Richmond, VA, United States
- 2Division of Endocrinology, Diabetes and Metabolism, University of Arkansas Medical Center, Little Rock, AR, United States
- 3Joslin Diabetes Center, Harvard Medical School, Boston, MA, United States
About 1 in 10 adults worldwide are estimated to have diabetes mellitus. They are at risk of developing life-threatening complications resulting in reduced quality of life, increased mortality and higher healthcare costs. The ability to prevent or delay type 2 diabetes mellitus (T2DM) by modifying some of its risk factors has been hypothesized for decades. The long and often gradual time-course of increasing dysglycemia prior to diabetes diagnosis suggests that interventions during that period could be effective in preventing T2DM. In addition to lifestyle modifications, certain drugs prevent or slow development of hyperglycemia. Recently, drugs used for obesity management were shown to prevent T2DM. In this review, we discuss various pharmacotherapeutic options for preventing T2DM.
Introduction
The epidemic of diabetes mellitus and its complications pose major global health threat. The global prevalence of diabetes and impaired glucose tolerance (IGT) quadrupled in the past three decades. This pace of change in diabetes prevalence in many countries has been heightened by rapid urbanization (1, 2). The global prevalence of diabetes was estimated to be 463 million (9.3% of adults 20–79 years of age) and this estimate is projected to rise to 700 million by 2045 (3). Over 90% of diabetes mellitus cases are type 2 diabetes mellitus (T2DM) (4). T2DM is also associated with increased health care cost; estimated to be $850 billion globally (5). The enormous human and financial costs that accompany T2DM, and the challenge of treating it effectively once it is diagnosed, make it an ideal target for prevention.
The ability to prevent or delay T2DM by modifying some of its risk factors has been hypothesized for decades. The long and gradual time-course of increasing dysglycemia prior to T2DM diagnosis suggests that interventions during that period could be effective in prevention of the disease. Substantial progress has been made in recent years in evaluating effective preventive strategies. In addition to lifestyle modifications, certain drugs were shown to prevent or delay development of hyperglycemia. Recently, drugs targeting obesity, have also been studied for T2DM prevention.
In this review, we discuss various pharmacotherapeutic options for preventing T2DM and discuss the evidence behind them as summarized in Tables 1, 2.
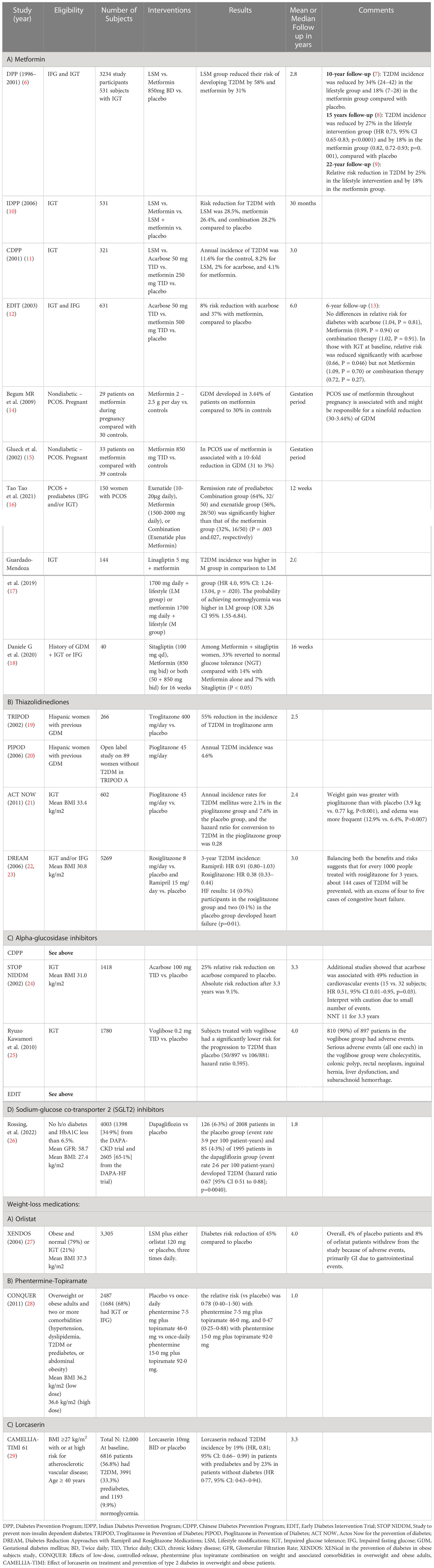
Table 1 Summary of clinical trials on T2DM prevention with glucose lowering drugs and weight-loss medications.
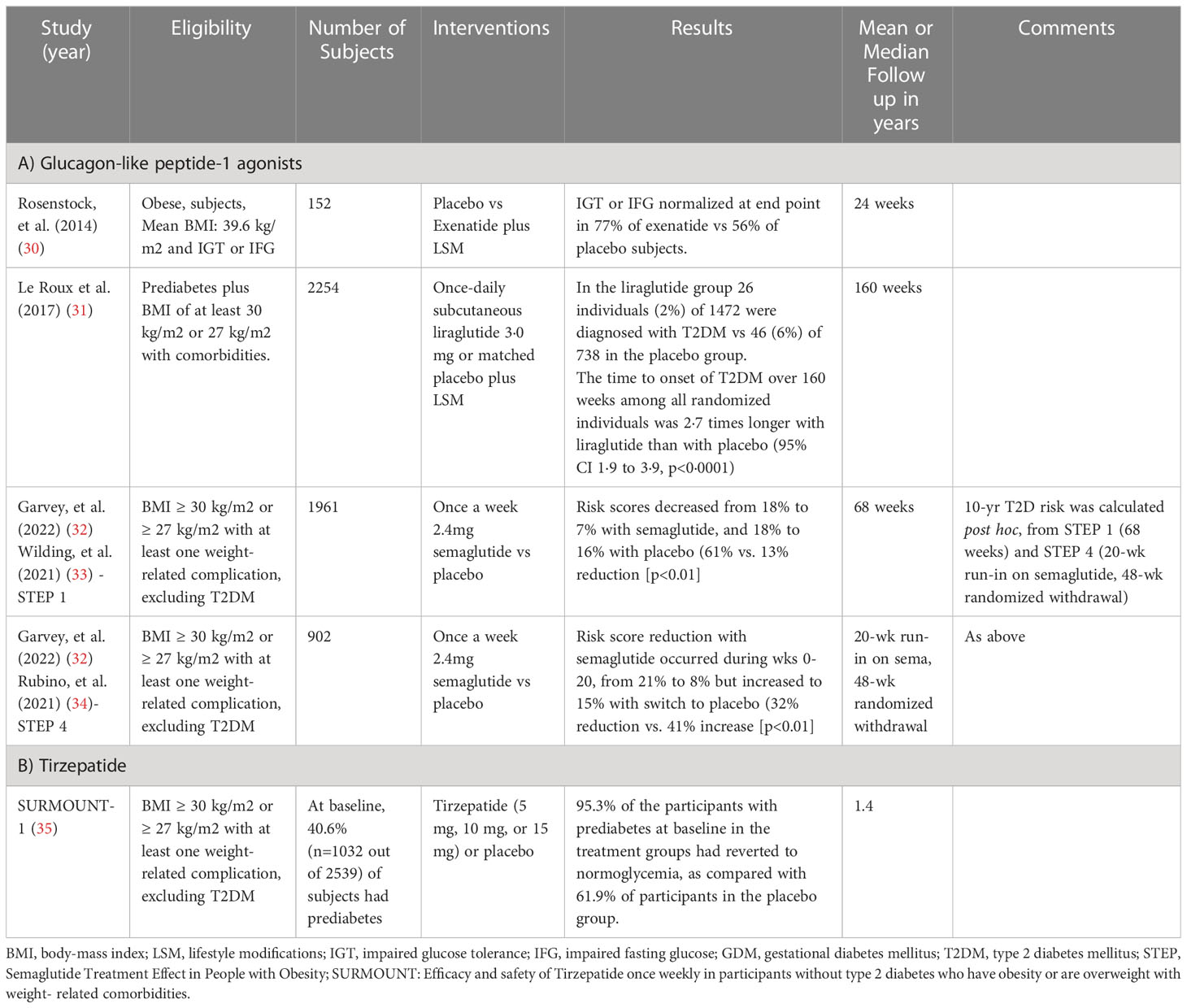
Table 2 Summary of evidence on T2DM prevention with medications promoting both glucose-lowering and weight-loss.
Glucose-lowering medications
Metformin
Metformin, a biguanide, primarily decreases hepatic glucose production by inhibiting gluconeogenesis. It enhances peripheral insulin sensitivity in the skeletal muscle by increasing insulin receptor tyrosine kinase activity and glucose transporter (GLUT)-4 translocation to the cell membrane (36). Metformin also improves beta-cell responsiveness to a glucose load through correction of glucotoxicity (37).
The Diabetes Prevention Program (DPP) study was a multi-center trial which enrolled 3,234 subjects with prediabetes and randomized them to either intensive lifestyle intervention (intended to achieve 7% body weight loss), metformin (850mg twice daily) or standard lifestyle recommendations (38). Participants in the study were overweight or obese (mean BMI 34 kg/m2), mostly middle-aged adults with IGT or impaired fasting glucose (IFG) with values between 95-126 mg/dL. In the ensuing 2.8 years, T2DM incidence was reduced by 58% with lifestyle intervention and by 31% with metformin compared to placebo (6). It is interesting to note that genome-wide association studies in the DPP cohort revealed novel ethnic-specific associations with metformin response and may have implications for individualized therapy (39).
A secondary analysis of the DPP study was performed in subjects with history of gestational diabetes (GDM). Women with history of GDM were compared with women with previous live birth but without GDM history. It was found that progression to T2DM is more common among women with history of GDM compared with those without it, despite equivalent degrees of IGT at baseline. Both lifestyle modifications (LSM) (53% reduction in T2DM incidence) and metformin (50% reduction in T2DM incidence) were highly effective in delaying T2DM in women with IGT and history of GDM (40).
Eighty-eight percent of the surviving DPP cohort enrolled in a long-term follow up study, the Diabetes Prevention Program Outcomes Study (DPPOS). During the DPPOS, unmasked metformin was continued as a study intervention in the original metformin group. T2DM incidence was reduced by 34% in the lifestyle group and 18% in the metformin group compared to placebo in the following 10 years (7). Significant reduction in T2DM incidence persists in the metformin group at 15-year (relative risk reduction/RRR 18%; p=0. 001) (8) and 22-year follow up (RRR 18%) (9).
Similarly, The Indian Diabetes Prevention Program (IDPP) randomized 531 Asian Indian subjects with IGT (mean BMI 25.8 kg/m2) to 4 groups: LSM or metformin (250-500mg twice daily) or LSM plus metformin or control group (standard healthcare advice). The median follow-up period was 30 months. The 3-year cumulative incidences of diabetes were 39.3%, 40.5%, 39.5% and 55.0%, respectively. The RRR was 26.4% with metformin (95% CI 19.1–35.1, p=0.029) and 28.2% with LSM plus metformin (95% CI 20.3–37.0, p=0.022), as compared to the control group (10).
The Chinese Diabetes Prevention Program (CDPP) evaluated the preventive effect of lifestyle intervention with diet and exercise, acarbose, and metformin on T2DM progression in 321 subjects with IGT. Annual T2DM incidence was 11.6, 8.2, 2.0, and 4.1% in the control, lifestyle intervention, acarbose, and metformin groups, respectively (11).
The Early Diabetes Intervention Trial (EDIT) analyzed the effects of metformin and acarbose in T2DM prevention in 631 subjects with IFG. At three years, there was an 8% risk reduction with acarbose and 37% with metformin, compared to placebo (12) but there was no difference in the relative risk for T2DM at six-year of follow-up. For patients with IGT at baseline, the RRR was significant with acarbose (0.66) but not with metformin (1.09), suggesting different effects of different therapies in subjects with IGT and IFG (13).
A study by Begum et al. (2009) showed that occurrence of GDM among women with polycystic ovarian syndrome (PCOS) was significantly lower in the metformin treatment group with only one subject (3.44%) vs nine of the 30 pregnancies (30%) without metformin (14). Similarly, Glueck et al. (2002) reported the odds ratio for GDM in women with metformin vs those without metformin was 0.093 (95% CI: 0.011 to 0.795) (15).
Recent studies showed promising effects of metformin in combination with glucagon-like peptide-1 (GLP-1) receptor agonists (16) and dipeptidyl peptidase 4 (DPP-4) inhibitors (17, 18) for T2DM prevention.
According to the American Diabetes Association (41), metformin should be considered for T2DM prevention in adults with BMI ≥35 kg/m2, age ≤ 60 years, higher fasting plasma glucose (≥ 110 mg/dL), and higher A1C (≥ 6.0%), and in women with prior GDM.
Thiazolidinediones
Thiazolidinediones (TZDs) are insulin sensitizers. They activate gamma isoform of peroxisome proliferator-activated receptor (PPAR γ), enhance glucose uptake by skeletal muscles and adipocytes, improve insulin sensitivity and consequently improve pancreatic beta-cell function (42, 43).
The Troglitazone in Prevention of Diabetes (TRIPOD) study (19) compared Troglitazone with placebo in 266 nondiabetic Hispanic women (mean age 34.6 years; mean BMI 30.5 kg/m2) with previous GDM, about 70% of whom had IGT at entry into the trial. Troglitazone treated group had a 55% reduction in the incidence of T2DM over 2.5 years. The drug was recalled before the planned study-end because of reports of hepatic failure.
The Pioglitazone in Prevention of Diabetes (PIPOD) study (20) was an open-label follow-up of 89 women from TRIPOD who had not developed diabetes (A1C <7%). These participants showed an average rate of diabetes of 4.6% per year during treatment with pioglitazone for three years, which was much lower compared with the rate of 12.1% per year that was observed during placebo treatment in the TRIPOD study.
Actos Now for the Prevention of Diabetes (ACT NOW) study (21) was an RCT conducted to examine the effectiveness of pioglitazone in preventing T2DM among 602 subjects (mean age 52 years; mean BMI 34 kg/m2) with IGT. The annual rate of T2DM was 7.6% in placebo-treated vs. 2.1% in pioglitazone treated subjects (HR 0.28, p<0.0001) over 2.4 years.
Concerns over adverse effects of TZDs has dampened the enthusiasm to use pioglitazone for T2DM prevention. Undesirable effects of TZDs include fluid retention, increased risk of heart failure, weight gain and loss of bone density increasing fracture risk.
Alpha-glucosidase inhibitors
These drugs act by competitively inhibiting alpha- glucosidase enzyme and decreasing carbohydrate absorption from the small intestine, thus reducing postprandial glucose levels (44).
The Study TO Prevent Non-Insulin Dependent Diabetes Mellitus (STOP-NIDDM) (24) evaluated the effects of acarbose in delaying progression of IGT to T2DM in 1429 subjects. Over the 3.3-year follow-up period, there was a 25% reduction in the incidence of T2DM in the acarbose group compared to placebo. Furthermore, acarbose significantly increased the regression of IGT to normal glucose tolerance (HR 1.42, 95% CI 1.24–1.62; p<0·0001). About one-quarter of the cohort did not complete the study, and this was attributed to the gastrointestinal side effects of acarbose.
Kwawamori et al., randomized 1780 Japanese subjects with IGT to either receiving voglibose 0.6 mg/day or placebo. At the end of the study (11 months; ended early due to efficacy) the T2DM hazard ratio (voglibose vs. placebo) was 0.60 (95% CI 0.43–0.82) (25).
Sodium-glucose co-transporter-2 inhibitors
The SGLT2 is expressed in the proximal tubule and mediates reabsorption of approximately 90 percent of the filtered glucose load to the kidneys. SGLT2 inhibitors promote renal excretion of glucose and thereby modestly lower elevated blood glucose levels (45).
Pre-specified pooled analysis (26) of the DAPA-CKD and DAPA-HF trials suggests that dapagliflozin (10 mg daily) may reduce new-onset T2DM compared with placebo (HR 0·67 [95% CI 0·51–0·88]). In pooled analysis of selected 4,003 participants who had no previous diagnosis of T2DM (mean age 63 years, mean A1C 5.7%), dapagliflozin reduced new-onset T2DM incidence (defined as having A1C ≥6.5% on two consecutive follow-up visits, or a clinical diagnosis of T2DM that led to initiation of a glucose-lowering agent) by approximately one-third. The overall incidence of new-onset T2DM was 2.6 events per 100 patient-years in the dapagliflozin group vs 3.9 events per 100 patient-years in the placebo group (HR 0.67; 95% CI 0.51–0.88; p=0.0040). Treatment was predominantly beneficial in participants with prediabetes. Possible mechanisms include protection of pancreatic beta-cells from glucotoxicity, weight loss, and improvement in hepatic insulin sensitivity. Improvement in CKD and heart failure may have contributed to insulin sensitivity (26). A prospective RCTs is needed to confirm whether dapagliflozin truly prevents T2DM.
Although empagliflozin did not demonstrate significant benefit for T2DM prevention among patients with heart failure and prediabetes in EMPEROR-Preserved study (46) (HR: 0.84; 95% CI 0.65–1.07) and EMPEROR-Reduced study (47) (HR: 0.86; 95% CI 0.62–1.19), the hazard ratios were consistent with potential benefit. A recent meta-analysis of four RCTs showed that SGLT2 inhibitors (empagliflozin and dapagliflozin) were significantly associated with a lower risk of new-onset diabetes (relative risk, 0.79; 95% CI, 0.68-0.93) (48). This meta-analysis included 5655 participants with pre-diabetes. The relative risks of new-onset diabetes in dapagliflozin and empagliflozin were 0.68 (95% CI, 0.52-0.89) and 0.87 (95% CI, 0.72-1.04), respectively.
Weight-loss medications
Orlistat
Orlistat acts by reversibly inhibiting gastric and pancreatic lipases (49). It also increases postprandial glucagon-like peptide 1 (GLP-1) levels. In a pooled analysis by Heymsfield et al. (50) orlistat compared to placebo, reduced 2-year cumulative diabetes incidence by 61% (7.6% in the placebo group vs. 3.0% in the orlistat group) among those with IGT. However, due to the side effects of orlistat, only 69% of the participated subjects completed the study.
Xenical in the Prevention of Diabetes in Obese Subjects (XENDOS) study (27) was a 4-year, double-blind, prospective study where 3,305 obese subjects with prediabetes were randomized to either lifestyle intervention plus orlistat 120 mg or plus placebo. It showed that the cumulative incidence of T2DM was 9.0% with placebo and 6.2% with orlistat, corresponding to a risk reduction of 37.3% (p=0.0032). Independent of orlistat or placebo treatment, the relative risk of developing T2DM was greater in patients with IGT, men, older subjects, and subjects with a higher BMI.
Phentermine/topiramate
Phentermine is a sympathomimetic drug, which stimulates norepinephrine release in the hypothalamus, suppresses appetite and increases satiety. Topiramate’s action is not well understood but hypothesized to work on alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors and kainite receptors to reduce food cravings, and on Gamma-aminobutyric acid (GABA) receptors to increase energy expenditure (51).
The CONQUER study evaluated the efficacy of phentermine/topiramate combination as an adjunct to LSM for weight loss and metabolic risk reduction in individuals who are overweight and obese, with two or more risk factors (28). They enrolled 84% of subjects without T2DM at baseline. In this population, development of T2DM was less in phentermine 15 mg/topiramate ER 92 mg group compared to placebo after 56 weeks of intervention (1.7% versus 3.6%; HR, 0.47; 95% CI, 0.25–0.88).
In the long-term follow up study, SEQUEL, a total of 78.1% of subjects in the original CONQUER study continued to take blinded medication over 108 weeks. The annual incidence rates for progression to T2DM were 0.9% in high dose phentermine/topiramate group and 3.7% in the placebo group (P=0.008) (52). These studies were not performed to assess prevention of T2DM as a primary outcome.
A subgroup analysis of the CONQUER study including subjects with prediabetes and/or metabolic syndrome at baseline showed that the annual incidence of T2DM was 1.3% for high dose phentermine/topiramate and 6.1% in placebo (53).
Naltrexone/bupropion
Bupropion is a norepinephrine and dopamine reuptake inhibitor which stimulates proopiomelanocortin (POMC) neurons in the hypothalamus, with a downstream effect of increased satiety. Naltrexone prevents rebound inhibition of POMC neurons by β-endorphin, and synergistically works with bupropion to increase satiety (51).
There were four Contrave Obesity Research (COR) studies looked at the weight loss effects of Naltrexone/Bupropion (NB): the COR-I, COR-II, COR-BMOD (behavior modification), COR-Diabetes (54–57). None of these studies were designed to analyze progression of IGT to T2DM, but COR-I study (54) showed significant decrease in fasting plasma glucose in response to naltrexone SR 32 mg/bupropion SR 16 mg combination treatment. COR-Diabetes study (57) including subjects with T2DM reported improvements in glucose homeostasis, resulting in A1C reduction of 0.6% in the NB group, and the A1C goal of ¾7% was achieved in 44% in NB group vs 26% in placebo group.
Further longer-term studies are needed to establish the effect of this medication in T2DM prevention.
Drugs promoting glucose-lowering and weight-loss
Glucagon-like peptide 1 receptor agonists
Glucagon-like peptide 1 receptor agonists (GLP-1 RA) mimic the action of endogenous GLP-1 in enhancing glucose-dependent insulin secretion and suppress glucagon production from pancreatic alpha cells and thus used to treat T2DM. Apart from glycemic control, they are also thought to reduce neuroinflammation, promote nerve growth, improve cardiac function, suppress appetite, delay gastric emptying, regulate lipid metabolism and reduce fat deposition (58).
In a study (30) of 152 obese patients (mean age 46 years; mean BMI 39.6 kg/m2) with and without prediabetes (IGT or IFG), blood glucose was normalized in 77% and 56% after exenatide and placebo, respectively. There was a significantly higher weight loss with exenatide of 5.1 kg vs 1.6 kg with placebo.
In the SCALE study Obesity and Prediabetes trial (31), 2,254 adults with prediabetes and BMI ≥30 kg/m2 or ≥27 kg/m2 with comorbidities (mean age 47 years, mean BMI 39 kg/m2) were randomized to receive liraglutide 3mg/day vs a matched placebo, as an adjunct to LSM. Time to onset of diabetes in the treatment group was 2.7 times longer with liraglutide compared to placebo (95% CI 1·9 to 3·9, p<0·0001; HR 0.21, 95% CI 0.13–0.34). However, about half the participants withdrew from the study. Based on an analysis imputing the missing data, T2DM incidence was reduced by 66% (HR 0.34, 95% CI 0.22–0.53) with liraglutide vs 36% with placebo.
Recently, the effect of semaglutide in T2DM prevention was assessed in comparison to placebo in overweight or obese individuals in the Semaglutide Treatment Effect in People with Obesity (STEP) studies. In a post-hoc analysis (32) of the STEP 1 (33) (68 weeks) and STEP 4 (34) (20-week run-in on semaglutide, 48-week randomized withdrawal) trials, it was shown that semaglutide 2.4 mg could reduce the 10-year risk of progression to T2DM by 61%, regardless of the initial glycemic status (vs 13% reduction in the placebo group (p<0.01). In this analysis, the 10-year risk of T2DM was calculated using Cardiometabolic Disease Staging (CMDS). Most of the risk reduction occurred during the initial weeks (0-20 weeks), from 21% to 11%. Risk scores further decreased with continued semaglutide (weeks 20-68) but increased with switch to placebo (32% reduction vs. 41% increase, p<0.01).
Dual glucose-dependent insulinotropic polypeptide and GLP-1 receptor agonist
Tirzepatide, the dual GIP/GLP-1 receptor agonist was recently approved by the FDA in May 2022 for treatment of T2DM. In the 72-week SURMOUNT-1 trial (35), 40.6% of the patients had prediabetes at baseline. At the end of the trial, 95.3% of those participants reverted back to normoglycemia, as compared with 61.9% of participants in the placebo group. There was also a notable decrease in the fasting insulin levels in the treatment groups. This is probably attributed to the significant weight loss that was seen in association with tirzepatide (15-20.9% weight loss), however future dedicated studies are still needed to confirm the role of tirzepatide for T2DM prevention.
Other medications
Renin angiotensin aldosterone system blockade
Various trials (23, 59–65) suggested that RAAS inhibition may reduce the incidence of new onset T2DM in patients with or without hypertension or at high risk of T2DM. The risk reduction was explained by hemodynamic effects such as improved delivery of insulin and glucose to the peripheral skeletal muscle, non-hemodynamic effects, including direct effects on glucose transport and insulin signaling pathways, which collectively decrease insulin resistance.
A meta-analysis (66) of new-onset T2DM in select comparative outcome trials involving the use of RAAS blockade vs non-RAS blockade showed a lower risk ratio (RR 0.78; 95% CI 0.74-0.88). However, most of these trials did not include T2DM incidence as the pre-specified end point.
Vitamin D
The Vitamin D and Type 2 Diabetes (D2d) Study (67), randomly assigned 2,423 adults with prediabetes to receive 4,000 units of vitamin D3 per day or placebo, regardless of their baseline vitamin D status. After a median follow-up of 2.5 years, T2DM occurred in 293 participants in the vitamin D group, and 323 in the placebo group (9.39 and 10.66 events per 100 person-years, respectively). The hazard ratio for vitamin D compared with placebo was 0.88 (95% CI, 0.75 to 1.04; p=0.12), failing to show a significant decrease in T2DM incidence among the study population.
However, subsequent meta-analyses of studies in patients with pre-diabetes demonstrated that vitamin D supplementation at moderate to high doses significantly reduced the incidence risk of T2DM (68, 69). A secondary analysis of the D2d study showed that participants who maintained higher intratrial serum vitamin D levels during follow-up had a reduced risk of diabetes (70).
Testosterone
Men who are overweight frequently have low serum testosterone (T) concentrations, which is in turn associated with increased risk of T2DM (71).
T4DM (72) was a randomized, placebo-controlled trial, which included 1,007 men who were enrolled in lifestyle intervention program and randomly assigned to receive T or placebo. At 2 years, 21% of the subjects in the placebo group failed OGTT vs 12% in the T group (RR 0.59, CI 0.43-0.80, p=0.007). Treatment effect was independent of baseline serum testosterone level. So far, testosterone use is not approved for T2DM prevention or treatment.
Conclusion
The rates of T2DM have been rising, parallel to the rates of obesity, largely due to sedentary lifestyle and increased access to highly obesogenic foods. T2DM is one of the leading risk factors for cardiovascular mortality.
Trials involving lifestyle therapies (38, 73, 74) have shown that 5-10% weight loss in obese and overweight individuals with prediabetes is effective in preventing or delaying development of T2DM. Bariatric surgery (75) is particularly effective in preventing T2DM. However, majority of patients are unable to sustain lifestyle changes (76) or accept bariatric surgery as a preventive tool. Appropriate pharmacotherapy is an attractive option to prevent or delay development of T2DM. Metformin should be considered for T2DM prevention in adults with BMI ≥35 kg/m2, age ≤ 60 years, higher fasting plasma glucose (≥ 110 mg/dL), and higher A1C (≥ 6.0%), and in women with prior GDM (41).
Newer therapies like GLP-1 receptor agonists or dual GIP/GLP-1 receptor agonists have unique ability to suppress appetite, and improve pancreatic insulin production, resulting in profound weight loss, improved insulin sensitivity. Although there are several emerging data to show benefits of these therapies in preventing T2DM, further randomized prospective studies are required.
Author contributions
PM and FO contributed to the conception and design of the manuscript. PM and FO wrote the first draft of the manuscript. DE and OH wrote sections of the manuscript. OH edited the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer GW declared a past collaboration with the author PM to the handling editor.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gassasse Z, Smith D, Finer S, Gallo V. Association between urbanisation and type 2 diabetes: an ecological study. BMJ Glob Health (2017) 2(4):e000473. doi: 10.1136/bmjgh-2017-000473
2. Thanikachalam M, Fuller CH, Lane KJ, Sunderarajan J, Harivanzan V, Brugge D, et al. Urban environment as an independent predictor of insulin resistance in a south Asian population. Int J Health Geogr (2019) 18(1):5. doi: 10.1186/s12942-019-0169-9
3. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
4. Holman N, Young B, Gadsby R. Current prevalence of type 1 and type 2 diabetes in adults and children in the UK. Diabetes Med (2015) 32(9):1119–20. doi: 10.1111/dme.12791
5. Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract (2018) 138:271–81. doi: 10.1016/j.diabres.2018.02.023
6. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med (2002) 346(6):393–403. doi: 10.1056/NEJMoa012512
7. Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, et al. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet (2009) 374(9702):1677–86. doi: 10.1016/S0140-6736(09)61457-4
8. Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the diabetes prevention program outcomes study. Lancet Diabetes Endocrinol (2015) 3(11):866–75. doi: 10.1016/S2213-8587(15)00291-0
9. American Diabetes Association. New data from diabetes prevention program outcomes study shows persistent reduction of type 2 diabetes development over 22-year average follow-up (2020). Available at: https://www.diabetes.org/newsroom/press-releases/2020/new-data-from-diabetes-prevention-program-outcomes-study-shows-persistent-reduction-of-t2d-development-over-22-year-average-follow-up.
10. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian diabetes prevention programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia (2006) 49(2):289–97. doi: 10.1007/s00125-005-0097-z
11. Wenying Y, Lixiang L, Jinwu Q, Zhiqing Y, Haicheng P, Guofeng H, et al. The preventive effect of acarbose and metformin on the progression to diabetes mellitus in the IGT population: A 3-year multicenter prospective study. Chin J Endocrinol Metab (2001) 17:131–6. doi: 10.3760/cma.j.issn.0366-6999.2001.09.108
12. Holman RR, North BV, Tunbridge FK. Possible prevention of type 2 diabetes with acarbose or metformin. Diabetes (2000) 49 Suppl 1:A111. doi: 10.1042/cs098013Pc
13. Holman RR, Blackwell L, Stratton IM, Manley SE, Tucker L, Frighi V. Six-year results from the early diabetes intervention trial. Diabetes Med (2003) 20 Suppl 2:15.
14. Begum MR, Khanam NN, Quadir E, Ferdous J, Begum MS, Khan F, et al. Prevention of gestational diabetes mellitus by continuing metformin therapy throughout pregnancy in women with polycystic ovary syndrome. J Obstet Gynaecol Res (2009) 35(2):282–6. doi: 10.1111/j.1447-0756.2008.00876.x
15. Glueck CJ, Wang P, Kobayashi S, Phillips H, Sieve-Smith L. Metformin therapy throughout pregnancy reduces the development of gestational diabetes in women with polycystic ovary syndrome. Fertil Steril. (2002) 77(3):520–5. doi: 10.1016/s0015-0282(01)03202-2
16. Tao T, Zhang Y, Zhu YC, Fu JR, Wang YY, Cai J, et al. Exenatide, metformin, or both for prediabetes in PCOS: A randomized, open-label, parallel-group controlled study. J Clin Endocrinol Metab (2021) 106(3):e1420–32. doi: 10.1210/clinem/dgaa692
17. Guardado-Mendoza R, Salazar-López SS, Álvarez-Canales M, Farfán-Vázquez D, Martínez-López YE, Jiménez-Ceja LM, et al. The combination of linagliptin, metformin and lifestyle modification to prevent type 2 diabetes (PRELLIM). A random. Clin trial. Metab (2020) 104:154054. doi: 10.1016/j.metabol.2019.154054
18. Daniele G, Tura A, Dardano A, Bertolotto A, Bianchi C, Giusti L, et al. Effects of treatment with metformin and/or sitagliptin on beta-cell function and insulin resistance in prediabetic women with previous gestational diabetes. Diabetes Obes Metab (2020) 22(4):648–57. doi: 10.1111/dom.13940
19. Buchanan TA, Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk hispanic women. Diabetes (2002) 51(9):2796–803. doi: 10.2337/diabetes.51.9.2796
20. Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, Ochoa C, et al. Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes (2006) 55(2):517–22. doi: 10.2337/diabetes.55.02.06.db05-1066
21. Defronzo RA, Tripathy D, Schwenke DC, Banerji M, Bray GA, Buchanan TA, et al. Prevention of diabetes with pioglitazone in ACT NOW: Physiologic correlates. Diabetes (2013) 62(11):3920–6. doi: 10.2337/db13-0265
22. DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators, Gerstein HC, Yusuf S, Bosch J, Pogue J, Sheridan P, et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: A randomised controlled trial. Lancet (2006) 368(9541):1096–105. doi: 10.1016/S0140-6736(06)69420-8
23. DREAM Trial Investigators, Bosch J, Yusuf S, Gerstein HC, Pogue J, Sheridan P, et al. Effect of ramipril on the incidence of diabetes. N Engl J Med (2006) 355(15):1551–62. doi: 10.1056/NEJMoa065061
24. Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, et al. Acarbose for prevention of type 2 diabetes mellitus: The STOP-NIDDM randomised trial. Lancet (2002) 359(9323):2072–7. doi: 10.1016/S0140-6736(02)08905-5
25. Kawamori R, Tajima N, Iwamoto Y, Kashiwagi A, Shimamoto K, Kaku K, et al. Voglibose for prevention of type 2 diabetes mellitus: A randomised, double-blind trial in Japanese individuals with impaired glucose tolerance. Lancet (2009) 373(9675):1607–14. doi: 10.1016/S0140-6736(09)60222-1
26. Rossing P, Inzucchi SE, Vart P, Jongs N, Docherty KF, Jhund PS, et al. Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. Lancet Diabetes Endocrinol (2022) 10(1):24–34. doi: 10.1016/S2213-8587(21)00295-3
27. Torgerson JS, Hauptman J, Boldrin MN, Sjöström L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: A randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care (2004) 27(1):155–61. doi: 10.2337/diacare.27.1.155
28. Gadde KM, Allison DB, Ryan DH, Peterson CA, Troupin B, Schwiers ML, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): A randomised, placebo-controlled, phase 3 trial. Lancet (2011) 377(9774):1341–52. doi: 10.1016/S0140-6736(11)60205-5
29. Bohula EA, Scirica BM, Inzucchi SE, McGuire DK, Keech AC, Smith SR, et al. Effect of lorcaserin on prevention and remission of type 2 diabetes in overweight and obese patients (CAMELLIA-TIMI 61): a randomised, placebo-controlled trial. Lancet (2018) 392(10161):2269–79. doi: 10.1016/S0140-6736(18)32328-6
30. Rosenstock J, Klaff LJ, Schwartz S, Northrup J, Holcombe JH, Wilhelm K, et al. Effects of exenatide and lifestyle modification on body weight and glucose tolerance in obese subjects with and without pre-diabetes. Diabetes Care (2010) 33(6):1173–5. doi: 10.2337/dc09-1203
31. le Roux CW, Astrup A, Fujioka K, Greenway F, Lau DCW, Van Gaal L, et al. 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: A randomised, double-blind trial. Lancet (2017) 389(10077):1399–409. doi: 10.1016/S0140-6736(17)30069-7
32. Timothy Garvey W, Holst-Hansen T, Laursen PN, Rinnov AR, Wilkinson LJ. Semaglutide 2.4 mg reduces the 10-year T2D risk in people with Overweight/Obesity. In: Diabetes: American diabetes association (2022) 71(Supplement_1):2–LB. doi: 10.2337/db22-2-LB
33. Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med (2021) 384(11):989–1002. doi: 10.1056/NEJMoa2032183
34. Rubino D, Abrahamsson N, Davies M, Hesse D, Greenway FL, Jensen C, et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: The STEP 4 randomized clinical trial. JAMA (2021) 325(14):1414–25. doi: 10.1001/jama.2021.3224
35. Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med (2022) 387(3):205–16. doi: 10.1056/NEJMoa2206038
36. Goodarzi MO, Bryer-Ash M. Metformin revisited: Re-evaluation of its properties and role in the pharmacopoeia of modern antidiabetic agents. Diabetes Obes Metab (2005) 7(6):654–65. doi: 10.1111/j.1463-1326.2004.00448.x
37. Bailey CJ, Turner RC. Metformin. N Engl J Med (1996) 334(9):574–9. doi: 10.1056/NEJM199602293340906
38. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care (1999) 22(4):623–34. doi: 10.2337/diacare.22.4.623
39. Li JH, Perry JA, Jablonski KA, Srinivasan S, Chen L, Todd JN, et al. Identification of genetic variation influencing metformin response in a multi-ancestry genome-wide association study in the diabetes prevention program (DPP). Diabetes (2022), db220702. doi: 10.2337/db22-0702
40. Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab (2008) 93(12):4774–9. doi: 10.1210/jc.2008-0772
41. American Diabetes Association Professional Practice Committee. 3. prevention or delay of type 2 diabetes and associated comorbidities: Standards of medical care in diabetes-2022. Diabetes Care (2022) 45(Suppl 1):S39–45. doi: 10.2337/dc22-S003
42. Saltiel AR, Olefsky JM. Thiazolidinediones in the treatment of insulin resistance and type II diabetes. Diabetes (1996) 45(12):1661–9. doi: 10.2337/diab.45.12.1661
43. Yki-Järvinen H. Thiazolidinediones. N Engl J Med (2004) 351(11):1106–18. doi: 10.1056/NEJMra041001
44. Akmal M, Wadhwa R. Alpha glucosidase inhibitors, in: StatPearls (2022). StatPearls Publishing. Available at: http://www.ncbi.nlm.nih.gov/books/NBK557848/ (Accessed January 24, 2023).
45. Fonseca-Correa JI, Correa-Rotter R. Sodium-glucose cotransporter 2 inhibitors mechanisms of action: A review. Front Med (Lausanne). (2021) 8:777861. doi: 10.3389/fmed.2021.777861
46. Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med (2021) 385(16):1451–61. doi: 10.1056/NEJMoa2107038
47. Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med (2020) 383(15):1413–24. doi: 10.1056/NEJMoa2022190
48. Mori Y, Duru OK, Tuttle KR, Fukuma S, Taura D, Harada N, et al. Sodium-glucose cotransporter 2 inhibitors and new-onset type 2 diabetes in adults with prediabetes: Systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab (2022) 108(1):221–31. doi: 10.1210/clinem/dgac591
49. Guerciolini R. Mode of action of orlistat. Int J Obes Relat Metab Disord (1997) 21 Suppl 3:S12–23.
50. Heymsfield SB, Segal KR, Hauptman J, Lucas CP, Boldrin MN, Rissanen A, et al. Effects of weight loss with orlistat on glucose tolerance and progression to type 2 diabetes in obese adults. Arch Intern Med (2000) 160(9):1321–6. doi: 10.1001/archinte.160.9.1321
51. Lutz TA, Asarian L. Pharmacotherapy for weight loss, in: Appetite and food intake: Central control (2017). CRC Press/Taylor & Francis (Accessed January 24, 2023).
52. Garvey WT, Ryan DH, Look M, Gadde KM, Allison DB, Peterson CA, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): A randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr (2012) 95(2):297–308. doi: 10.3945/ajcn.111.024927
53. Garvey WT, Ryan DH, Henry R, Bohannon NJ, Toplak H, Schwiers M, et al. Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care (2014) 37(4):912–21. doi: 10.2337/dc13-1518
54. Greenway FL, Fujioka K, Plodkowski RA, Mudaliar S, Guttadauria M, Erickson J, et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-i): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet (2010) 376(9741):595–605. doi: 10.1016/S0140-6736(10)60888-4
55. Apovian CM, Aronne L, Rubino D, Still C, Wyatt H, Burns C, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obes (Silver Spring). (2013) 21(5):935–43. doi: 10.1002/oby.20309
56. Wadden TA, Foreyt JP, Foster GD, Hill JO, Klein S, O'Neil PM, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: The COR-BMOD trial. Obes (Silver Spring). (2011) 19(1):110–20. doi: 10.1038/oby.2010.147
57. Hollander P, Gupta AK, Plodkowski R, Greenway F, Bays H, Burns C, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care (2013) 36(12):4022–9. doi: 10.2337/dc13-0234
58. Zhao X, Wang M, Wen Z, Lu Z, Cui L, Fu C, et al. GLP-1 receptor agonists: Beyond their pancreatic effects. Front Endocrinol (Lausanne). (2021) 12:721135. doi: 10.3389/fendo.2021.721135
59. Niklason A, Hedner T, Niskanen L, Lanke J. Captopril prevention project study group. development of diabetes is retarded by ACE inhibition in hypertensive patients–a subanalysis of the captopril prevention project (CAPPP). J Hypertens (2004) 22(3):645–52. doi: 10.1097/00004872-200403000-00029
60. Dahlöf B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the losartan intervention for endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet (2002) 359(9311):995–1003. doi: 10.1016/S0140-6736(02)08089-3
61. ALLHAT Officers, Coordinators for the ALLHAT Collaborative Research Group. The antihypertensive and lipid-lowering treatment to prevent heart attack trial. major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA (2002) 288(23):2981–97. doi: 10.1001/jama.288.23.2981
62. Lithell H, Hansson L, Skoog I, Elmfeldt D, Hofman A, Olofsson B, et al. The study on cognition and prognosis in the elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens (2003) 21(5):875–86. doi: 10.1097/00004872-200305000-00011
63. Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJV, Michelson EL, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: The CHARM-overall programme. Lancet (2003) 362(9386):759–66. doi: 10.1016/s0140-6736(03)14282-1
64. Vermes E, Ducharme A, Bourassa MG, Lessard M, White M, Tardif JC. Enalapril reduces the incidence of diabetes in patients with chronic heart failure: Insight from the studies of left ventricular dysfunction (SOLVD). Circulation (2003) 107(9):1291–6. doi: 10.1161/01.cir.0000054611.89228.92
65. Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: The VALUE randomised trial. Lancet (2004) 363(9426):2022–31. doi: 10.1016/S0140-6736(04)16451-9
66. Jandeleit-Dahm KAM, Tikellis C, Reid CM, Johnston CI, Cooper ME. Why blockade of the renin-angiotensin system reduces the incidence of new-onset diabetes. J Hypertens (2005) 23(3):463–73. doi: 10.1097/01.hjh.0000160198.05416.72
67. Pittas AG, Dawson-Hughes B, Sheehan P, Ware JH, Knowler WC, Aroda VR, et al. Vitamin d supplementation and prevention of type 2 diabetes. N Engl J Med (2019) 381(6):520–30. doi: 10.1056/NEJMoa1900906
68. Zhang Y, Tan H, Tang J, Li J, Chong W, Hai Y, et al. Effects of vitamin d supplementation on prevention of type 2 diabetes in patients with prediabetes: A systematic review and meta-analysis. Diabetes Care (2020) 43(7):1650–8. doi: 10.2337/dc19-1708
69. Barbarawi M, Zayed Y, Barbarawi O, Bala A, Alabdouh A, Gakhal I, et al. Effect of vitamin d supplementation on the incidence of diabetes mellitus. J Clin Endocrinol Metab (2020) 105(8):dgaa335. doi: 10.1210/clinem/dgaa335
70. Dawson-Hughes B, Staten MA, Knowler WC, Nelson J, Vickery EM, LeBlanc ES, et al. Intratrial exposure to vitamin d and new-onset diabetes among adults with prediabetes: A secondary analysis from the vitamin d and type 2 diabetes (D2d) study. Diabetes Care (2020) 43(12):2916–22. doi: 10.2337/dc20-1765
71. Gyawali P, Martin SA, Heilbronn LK, Vincent AD, Taylor AW, Adams RJT, et al. The role of sex hormone-binding globulin (SHBG), testosterone, and other sex steroids, on the development of type 2 diabetes in a cohort of community-dwelling middle-aged to elderly men. Acta Diabetol (2018) 55(8):861–72. doi: 10.1007/s00592-018-1163-6
72. Wittert G, Bracken K, Robledo KP, Grossmann M, Yeap BB, Handelsman DJ, et al. Testosterone treatment to prevent or revert type 2 diabetes in men enrolled in a lifestyle programme (T4DM): a randomised, double-blind, placebo-controlled, 2-year, phase 3b trial. Lancet Diabetes Endocrinol (2021) 9(1):32–45. doi: 10.1016/S2213-8587(20)30367-3
73. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. the da Qing IGT and diabetes study. Diabetes Care (1997) 20(4):537–44. doi: 10.2337/diacare.20.4.537
74. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med (2001) 344(18):1343–50. doi: 10.1056/NEJM200105033441801
75. Carlsson LM, Peltonen M, Ahlin S, Anveden Å, Bouchard C, Carlsson B, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med (2012) 367(8):695–704. doi: 10.1056/NEJMoa1112082
Keywords: type 2 diabetes mellitus, prevention, metformin, prediabetes, remission, pharmacotherapy
Citation: Majety P, Lozada Orquera FA, Edem D and Hamdy O (2023) Pharmacological approaches to the prevention of type 2 diabetes mellitus. Front. Endocrinol. 14:1118848. doi: 10.3389/fendo.2023.1118848
Received: 08 December 2022; Accepted: 13 February 2023;
Published: 09 March 2023.
Edited by:
Elaine Chow, The Chinese University of Hong Kong, ChinaReviewed by:
Anu Grover, Ipca Laboratories (India), IndiaGregory Westcott, Beth Israel Deaconess Medical Center and Harvard Medical School, United States
Natural Chu, The Chinese University of Hong Kong, China
Copyright © 2023 Majety, Lozada Orquera, Edem and Hamdy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Osama Hamdy, T3NhbWEuaGFtZHlAam9zbGluLmhhcnZhcmQuZWR1
 Priyanka Majety
Priyanka Majety Faustina Alejandra Lozada Orquera1
Faustina Alejandra Lozada Orquera1 Dinesh Edem
Dinesh Edem Osama Hamdy
Osama Hamdy