- 1Department of Thyroid Surgery, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, Shandong, China
- 2Office of Academic Research, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, Shandong, China
- 3Department of Thyroid and Breast Surgery, Changle People’s Hospital Affiliated to Weifang Medical College, Weifang, Shandong, China
Background: Ambulatory thyroid surgery has been increasingly performed in recent years. However, the feasibility of the ambulatory transoral endoscopic thyroidectomy vestibular approach (TOETVA) has not been evaluated. We aimed to evaluate the safety, economy, and mental health outcomes of ambulatory TOETVA.
Methods: We retrospectively reviewed the data of patients who underwent TOETVA between March 2019 and August 2022. The procedure was performed by a skilled surgical team from the Department of Thyroid Surgery of the affiliated Yantai Yuhuangding Hospital of Qingdao University. Patients were enrolled in the ambulatory (n=166) and conventional (n=290) groups, based on their chosen procedure. We analyzed patients’ clinical characteristics, surgical outcomes, Hamilton Anxiety Rating Scale (HAM-A) scores, and hospitalization costs.
Results: Of 456 patients, 166 underwent ambulatory TOETVA and 290 underwent conventional TOETVA. No significant differences were found in clinical and surgical characteristics between the groups, including sex (P=0.363), age (P=0.077), body mass index (P=0.351), presence of internal diseases (P=0.613), presence of Hashimoto’s thyroiditis (P=0.429), pathology (P=0.362), maximum tumor diameter (P=0.520), scope of surgery (P=0.850), or operative time (P=0.351). There were no significant differences in maximum tumor diameter (P=0.349), extrathyroidal tissue invasion (P=0.516), number of retrieved central lymph nodes (P=0.069), or metastatic central lymph nodes (P=0.897) between the groups. No significant differences were found in complications, including transient hypoparathyroidism (P=0.438), transient vocal cord palsy (P=0.876), transient mental nerve injury (P=0.749), permanent mental nerve injury (P=0.926), and other complications (P=1.000). Ambulatory patients had shorter hospital stays (P<0.001) and reduced hospitalization costs (P<0.001). There was no significant difference in HAM-A scores between the groups (P=0.056).
Conclusions: Ambulatory TOETVA is a safe, feasible, and cost-effective procedure for selected patients. This procedure resulted in shorter hospital stays, decreased medical costs, and did not increase patient anxiety. To ensure patient safety, surgical teams must inform patients of the indications, when to seek help, and how to receive the fastest medical attention.
1 Introduction
Transoral endoscopic thyroidectomy vestibular approach (TOETVA) has become one of the most common remote access techniques to avoid visible scarring of the neck since it was first performed by Nakajo et al. and Wang et al. in 2013 (1, 2). Increasing evidence has shown that TOETVA is comparable to open thyroidectomy in terms of safety and efficacy (3, 4), making it acceptable in an increasing number of medical centers in recent years.
Steckler first introduced ambulatory thyroid surgery in 1986 (5). In recent years, improvements in surgical techniques have decreased the incidence of complications in thyroid surgery (6), and the use of ambulatory thyroid surgery has gradually increased. Many international reports have shown the safety and economic benefits of ambulatory thyroid surgery (7, 8). The American Thyroid Association released a consensus statement regarding outpatient thyroid surgery in 2013 (9); however, to the best of our knowledge, there are no such reports for ambulatory TOETVA. Therefore, in this study, we aimed to evaluate the safety, economy, and mental health impact of ambulatory TOETVA.
2 Materials and methods
2.1 Study population
This retrospective study was approved by the Ethics Committee of the Affiliated Yantai Yuhuangding Hospital of Qingdao University. All patients who underwent TOETVA between March 2019 and August 2022 by a single skilled surgical team at the Thyroid Surgery Department of the affiliated Yantai Yuhuangding Hospital of Qingdao University were included in this study. The indications for TOETVA in our department are as follows: (1) patients who were diagnosed with papillary thyroid carcinoma (PTC) with a maximum tumor diameter of ≤1.5 cm in the upper pole or ≤3 cm in other parts of the thyroid and (2) patients diagnosed with benign tumors with a maximum tumor diameter of ≤6 cm. Patients with the following characteristics were excluded: (1) history of neck surgery or neck radiation therapy, (2) lateral cervical or superior mediastinal lymph node metastasis, (3) tumor invasion into extrathyroidal organs. (4) American Society of Anaesthesiology grade of III or higher, (5) inability to receive prompt medical care after discharge for various reasons such as distance from medical facilities, transportation, and education level.
A total of 456 patients underwent TOETVA in our department from March 2019 to August 2022; 166 received ambulatory TOETVA and 290 received conventional TOETVA. Patients were allowed to freely choose between the two procedures, and multimedia materials were provided to patients on multiple occasions to ensure they knew what to watch for, when to seek help, and how to get the fastest medical attention after discharge.
2.2 Preoperative examination
Thyroid ultrasonography, neck computed tomography, and fine needle aspiration cytology were performed to screen patients for indications and rule out contraindications. Preoperative laryngoscopy was performed to assess vocal cord function in patients with tumors in the posterior part of the gland or those with hoarseness. Preoperative examinations of the patients were performed within 7 days before admission in the ambulatory group and 1 to 2 days after admission in the conventional group. The patients in the ambulatory group underwent surgery on the day of admission, whereas the patients in the conventional group underwent surgery after completing all the preoperative examinations, which took approximately 2 days. The surgeon and anesthesiologist jointly evaluated the patients before surgery to rule out contraindications to surgery or anesthesia.
2.3 Surgical procedures and postoperative management
Treatments on the day of surgery were the same in both groups. All patients were required to abstain from food for at least 6 h and water for at least 2 h before surgery. All patients received intravenous cefuroxime sodium and metronidazole 30 min before anesthesia, which was repeated 6 h and 14 h after surgery. All patients were required to use a chlorhexidine gargle before surgery and continued this until 7 days postoperatively. In case of a total thyroidectomy, 600 mg calcium carbonate and 0.25 µg calcitriol would be administered orally twice a day from 2 days before surgery until the day of surgery.
Patients with benign lesions underwent unilateral or total thyroidectomy according to the size and location of the tumor. We can perform TOETVA if the tumor is no larger than 6 cm in size, while surgery is difficult if the tumor is larger than 4 cm in size. So we need to build a larger workspace to increase the mobility of the tumor, and we need to cut the specimen into long strips in the endo-bag before extracting it. On the other hand, patients diagnosed with PTC via fine needle aspiration cytology before surgery or intraoperative frozen pathological examination received unilateral or total thyroidectomy and central lymph node dissection.
The surgical technique was the same in both groups as previously described (10–12). All patients in the two groups underwent TOETVA successfully without conversion to open surgery. Venous blood was collected on the morning of the first postoperative day to measure parathyroid hormone (PTH) levels in the patients who underwent total thyroidectomy. Calcium carbonate 600 mg every 6 h and calcitriol 0.25 µg every 12 h were administered orally if serum PTH levels were lower than 15 pg/ml after surgery. Intravenous calcium supplementation was administered if the patient developed hypocalcemia-related symptoms or if serum calcium levels were lower than 1.8 mmol/L. Postoperative laryngoscopy was performed if the doctors or patients sensed abnormalities in sound. Patients in the ambulatory group were discharged from the ward within 24 h after admission, whereas those in the conventional group on the second postoperative day or later.
2.4 Clinical parameters
The Hamilton Anxiety Rating Scale (HAM-A) was used to assess patients’ mental health on discharge day. We reviewed patient medical records to collect data, including sex, age, body mass index (BMI), presence of internal diseases, presence of Hashimoto’s thyroiditis, pathology, maximum tumor diameter, the scope of surgery, operative time, number of retrieved and metastatic central lymph nodes (for patients diagnosed with PTC), extrathyroidal tissue invasion (for patients diagnosed with PTC), complications, HAM-A score, and hospitalization costs.
2.5 Statistical analyses
Data were analyzed by independent-samples t-tests, Χ2 tests, or Fisher’s exact tests using SPSS software (version 26.0; IBM Corp, Armonk, NY, USA). Differences were considered statistically significant at P-values of <0.05.
3 Results
3.1 Clinical and surgical characteristics
During the study period, 456 patients underwent TOETVA, of whom 166 received ambulatory TOETVA and 290 received conventional TOETVA. No significant differences were observed in the clinical and surgical characteristics between the two groups (Table 1). The percentage of women was 84.9% in the ambulatory group and 87.9% in the conventional group (P = 0.363). The mean age was 33.18 ± 8.13 and 34.58 ± 8.06 years in the ambulatory and conventional groups (P = 0.077), respectively. BMI was 24.46 ± 5.16 kg/m2 in the ambulatory group and 24.89 ± 4.55 kg/m2 in the conventional group (P = 0.351). Four patients in the ambulatory group and five in the conventional group had hypertension, and one of the five hypertensive patients in the conventional group also had coronary heart disease. Coincidentally, no patient in either group had diabetes. Overall, there were no significant differences between the two groups regarding comorbidities (P = 0.613). A total of 49 patients (29.5%) in the ambulatory group and 96 (33.1%) in the conventional group had Hashimoto’s thyroiditis (P = 0.429). A total of 160 patients (96.4%) in the ambulatory group and 274 (94.5%) in the conventional group were diagnosed with PTC (P = 0.362). The maximum tumor diameter was 0.78 ± 0.48 cm in the ambulatory group and 0.75 ± 0.42 cm in the conventional group (P = 0.520). Fourteen patients (8.4%) in the ambulatory group and 23 (7.9%) in the conventional group underwent total thyroidectomy (P = 0.850). Operative time was 160.93 ± 35.82 min and 166.00 ± 38.18 min in the ambulatory and conventional groups, respectively (P = 0.351).
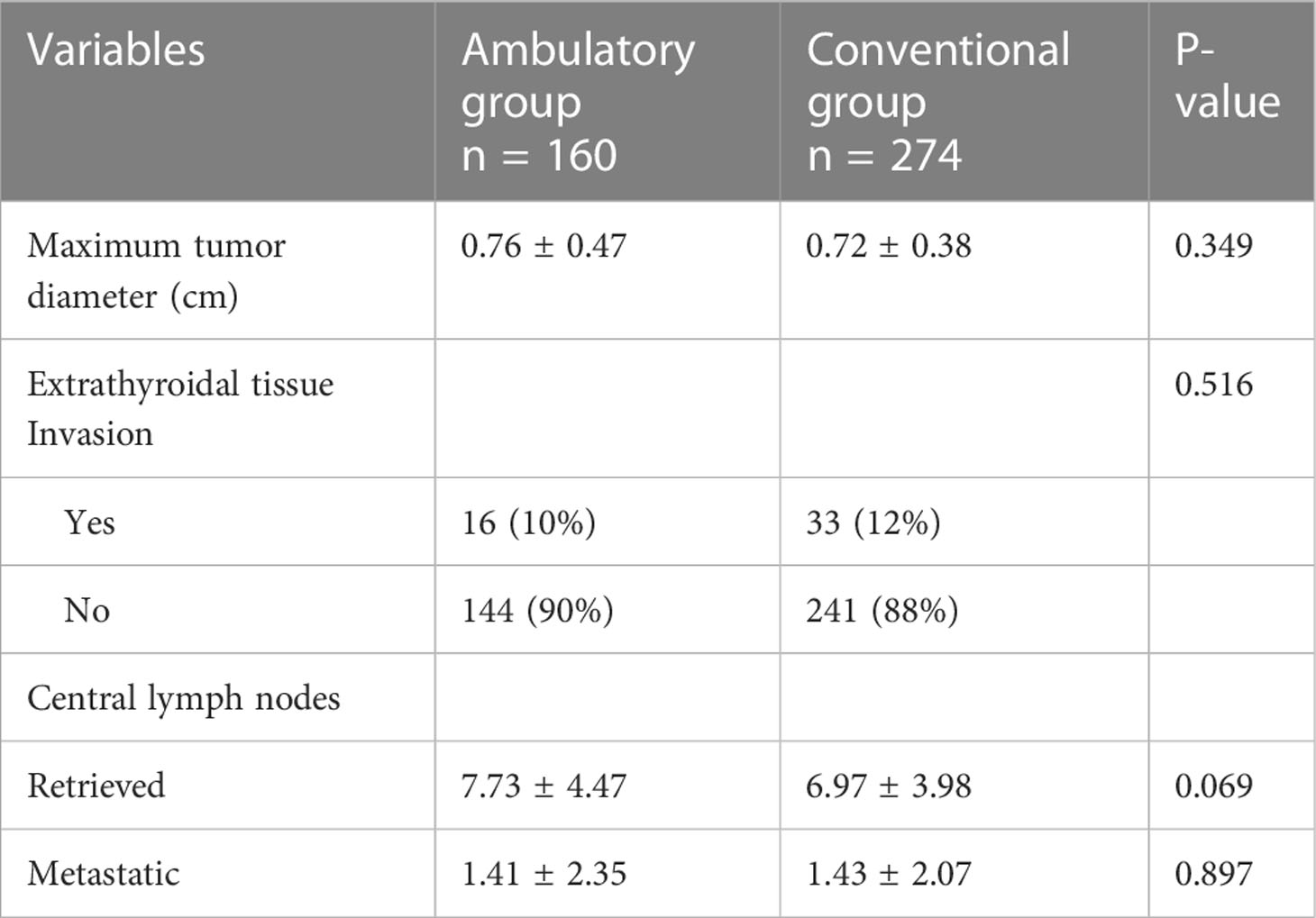
A subgroup analysis of the pathological results was performed for patients with PTC in both groups to ensure a similar surgical difficulty between the two groups (Table 2). There were no significant differences between the PTC subgroups in maximum tumor diameter (ambulatory, 0.76 ± 0.47 cm vs. conventional, 0.72 ± 0.38 cm, P = 0.349), extrathyroidal tissue invasion (P = 0.516), number of retrieved central lymph nodes (ambulatory, 7.73 ± 4.47 vs. conventional, 6.97 ± 3.98, P = 0.069), and number of metastatic central lymph nodes (ambulatory, 1.41 ± 2.35 vs. conventional, 1.43 ± 2.07, P = 0.897).
3.2 Complications
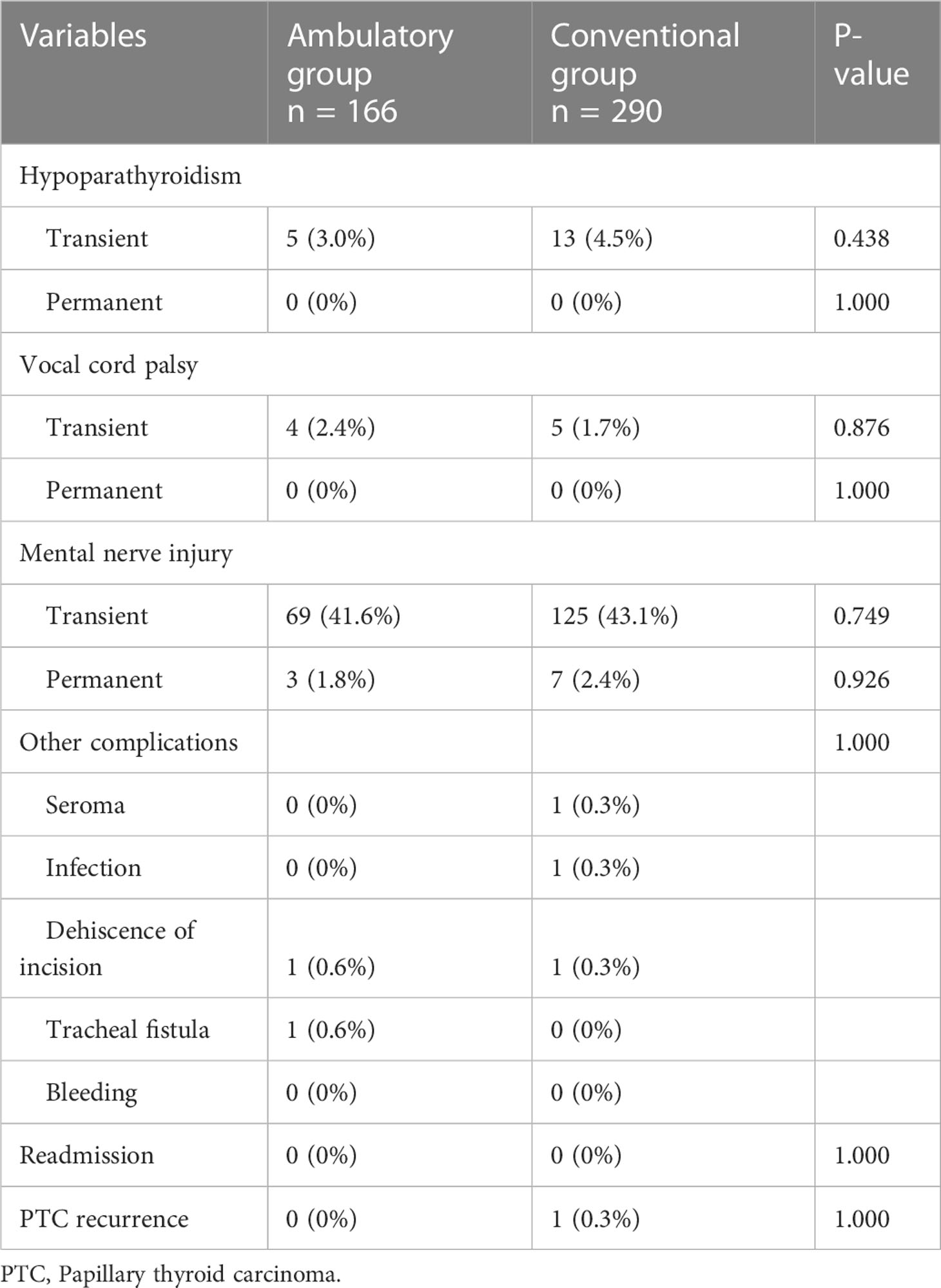
Postoperative complications are shown in Table 3. Five patients (3.0%) in the ambulatory group and 13 (4.5%) in the conventional group experienced transient hypoparathyroidism (P = 0.438). All the 18 patients who developed transient hypoparathyroidism underwent total thyroidectomy and central neck dissection, and the incidence of hypoparathyroidism in patients who underwent total thyroidectomy and central neck dissection was 48.6% (18/37). Only 2 of the 18 patients with temporary hypoparathyroidism had hypocalcemia-related symptoms on the day of surgery, and their symptoms were rapidly relieved after receiving one dose of intravenous calcium. None of the patients had serum calcium levels of <1.8 mmol/L. Four patients (2.4%) in the ambulatory group and five (1.7%) in the conventional group developed transient vocal cord palsy (P = 0.876). All patients with transient hypoparathyroidism or vocal cord palsy recovered within 3 months. No patients in either group had permanent hypoparathyroidism or vocal cord palsy. Patients who experienced numbness around the jaw area were considered to have sustained mental nerve injury, and those whose condition did not recover in six months after surgery were considered to have permanent mental nerve injury. No significant differences were observed in the percentage of patients with transient (ambulatory, 41.6% vs. conventional, 43.1%, P = 0.749) or permanent (ambulatory, 1.8% vs. conventional, 2.4%, P = 0.926) mental nerve injury between the groups.
In the conventional group, one patient developed a seroma and recovered after two ultrasound-guided needle aspiration. One patient who had neck pain and fever was diagnosed with an infection of the surgical site and recovered after intravenous administration of cefoperazone sulbactam for 2 days. One patient who developed partial dehiscence of the intraoral incision recovered within 1 week without re-suturing. In the ambulatory group, intraoral incision dehiscence occurred in one patient on the first day after surgery and healed well without infection after re-suturing. One patient developed subcutaneous emphysema owing to tracheal injury, which healed after intravenous administration of cefoperazone sulbactam and high negative pressure drainage for 13 days. No readmission or postoperative bleeding occurred in either group. The median follow-up was 18 months (range: 3–44 months). Only one patient with PTC in the conventional group experienced recurrence in the contralateral lobe 15 months after the initial surgery. We performed contralateral lobectomy and central neck dissection using a gasless trans-axillary approach, without complications.
3.3 Hospital stays, hospitalization cost, and mental health
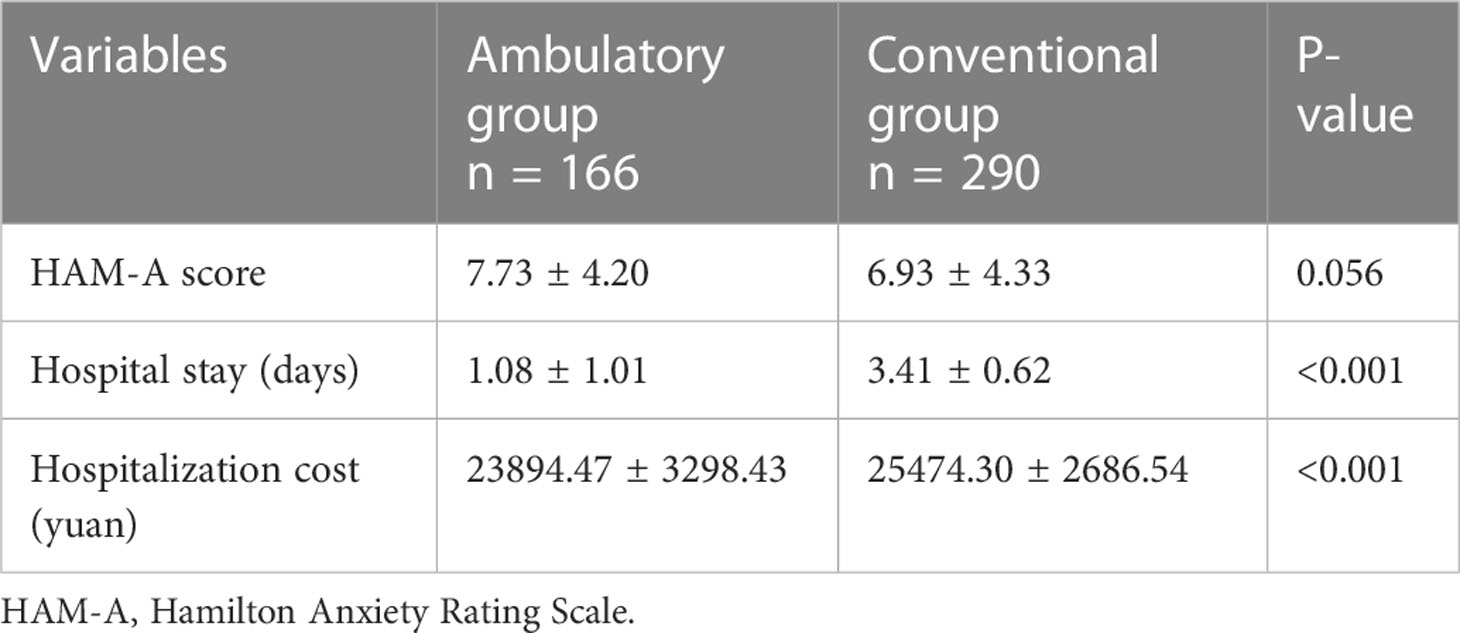
As shown in Table 4, patients in the ambulatory group had shorter hospital stays (1.08 ± 1.01 days vs. 3.41 ± 0.62 days, P < 0.001) and lower hospitalization cost (23,894.47 ± 3298.43 yuan vs. 25,474.30 ± 2686.54 yuan, P < 0.001). The two groups had no significant difference in HAM-A score (7.73 ± 4.20 vs. 6.93 ± 4.33, P = 0.056).
4 Discussion
The incidence of thyroid disease is high worldwide, and increasing healthcare cost is becoming a concern for many medical centers. Moreover, the COVID-19 pandemic has changed many ways we live and work. Unlike in many European and American countries, we are still implementing strategies to prevent the spread of COVID-19 in China. An ambulatory model can reduce hospital exposure and the chance of infectious disease transmission. Many large-sample studies have confirmed the safety of ambulatory thyroid surgery (13–15). In addition, TOETVA is becoming popular worldwide because of its excellent cosmetic effects. In consensus with our previous study (10, 16), many recent studies have reported that TOETVA is comparable in safety and efficacy to conventional open surgery (3, 4, 17). Therefore, the implementation of ambulatory TOETVA is feasible. This is the first study to evaluate the safety, economic, and mental health impact of ambulatory TOETVA.
In this study, we first analyzed the clinical and surgical characteristics of the patients in the two groups and the pathological results of patients diagnosed with PTC in the two groups. No significant differences were found between the two groups. These results suggest that the surgical difficulty of the two groups was the same, and their complications, hospitalization costs, and mental health impact were directly comparable.
Safety is the biggest concern of ambulatory TOETVA. Akritidou et al. reviewed the complications of the TOETVA (18). Serious postoperative complications, such as asphyxia due to hematoma, bilateral recurrent laryngeal nerve (RLN) palsy, and severe hypocalcemia, may occur after TOETVA. These can be life-threatening if the patient does not receive the necessary medical care after discharge. Minor complications include mental nerve injury, injury of the external branch of the superior laryngeal nerve, seroma, hematoma, subcutaneous emphysema, infection, skin injury, pulling sensation, swallowing disorder, and carbon dioxide-related complications. However, in our study, no patient developed serious postoperative complications
Hematoma is a rare but potentially lethal complication of TOETVA. In our study, none of the patients in the two groups developed hematomas, possibly because we used Hem-o-locks to clamp vessels with a diameter of >3 mm, reducing the risk of postoperative bleeding. Previous studies have also reported a very low incidence of hematoma after TOETVA (10–12, 17, 18). Akritidou et al. reported only 0.53% (10/1887) incidence of hematoma after TOETVA (18), and only 2 of the 10 hematoma patients needed repeat surgery (19, 20). Suzuki et al. (21) analyzed 1,123 patients with neck hematoma after thyroidectomy using the Japanese Diagnosis Procedure Combination database. They concluded that 81.9% (920/1123) of the patients developed a hematoma on days 0 and 1 after thyroidectomy. Carvalho et al. (22) reported that 62.5% (35/62) of patients had neck hematoma within 6 h, and only 12.5% (7/62) more than 24 h after thyroidectomy. Although there are no extensive sample reports, we can infer from the occurrence time of hematoma after open thyroid surgery that most hematomas occur shortly after TOETVA.
RLN injury is a common complication of TOETVA. Nine patients (2.0%) in our study developed transient RLN injury, with no significant difference between the groups; however, none of the patients developed permanent RLN injury in either group. Studies have shown post-TOETVA incidence to be 0.5%–5.9% and 0%–2.3% for transient and permanent RLN injuries, respectively (11, 19, 23, 24). All cases of RLN injury in previous studies were unilateral; to the best of our knowledge, there are no reports of bilateral RLN injury after TOETVA. Unilateral RLN injury, which causes hoarseness only, is not potentially life-threatening and does not require hospitalization; therefore, it does not interfere with ambulatory procedures.
As Akritidou et al. reported, the incidence of transient and permanent hypoparathyroidism in TOETVA was 6.11% (range: 0.94%–22.2%) and 0.21% (range: 1.33%–2.22%), respectively (18). However, lobectomy and nodulectomy accounted for most TOETVA operations in the study by Akritidou et al., while total thyroidectomy accounted for only a small proportion. As we reported previously (10), transient hyperparathyroidism occurred in 67.9% of patients with total oral thyroidectomy and bilateral central lymph node dissection. In the current study, the incidence of hypoparathyroidism in patients with total thyroidectomy and central neck dissection was 48.6% (18/37). Therefore, special attention should be paid to calcium supplementation and serum calcium monitoring during the perioperative period to prevent severe hypocalcemia. Mattoo et al. (25) reported a hypocalcemia rate of 54% in patients who underwent total thyroidectomy. They found that the best cut-off serum PTH value was 4.28 pmol/l (39 pg/ml) 20 min after total thyroidectomy because 23% (17/74) of patients required parenteral calcium supplementation when the serum PTH level was below 4.28 pmol/l and only 5.4% (2/37) of patients required parenteral calcium supplementation when the PTH level was above 4.28 pmol/l. In the current study, the incidence of transient hypoparathyroidism was 3% in the ambulatory group and 4.5% in the conventional group. None of the patients had permanent hypoparathyroidism. Only 5.4% (2/37) of the patients who underwent total thyroidectomy developed transient hypocalcemia-related symptoms. This proportion is lower than that reported by Mattoo et al., possibly because of the prophylactic calcium and calcitriol supplements administered during the perioperative period.
Tracheal injury occurred in one patient in the ambulatory group due to a puncture of the tracheal by an ultrasonic scalpel. A primary suture was immediately performed without conversion to open surgery, and the patient developed a large area of subcutaneous emphysema in the neck after coughing on postoperative day 1. This was the only patient in the ambulatory group with delayed hospital discharge. Tracheal injury is also a rare complication of TOETVA. Long et al. (26) reported two cases of tracheal injury: one was closed after conversion to open surgery, and the other was closed transorally. These two patients were discharged on postoperative days 1 and 2.
Other complications included mental nerve injury, seroma, infection, and dehiscence of the incision. Mental nerve injury is a common complication after TOETVA, with reported incidence of 0.7%–78.57%, most of which were transient (10, 12, 19). Mental nerve injury causes sensorimotor abnormalities of the lower lip and jaw, which do not require a prolonged hospital stay. Seroma, infection, and dehiscence of the incision are all rare complications of TOETVA, with incidence of less than 1% in most studies (10, 12, 16, 19, 24, 27).
While overnight observation can ensure the safety of most patients, there is still the possibility of complications after discharge, including hematoma and severe hypocalcemia. Therefore, the surgical team must strictly educate patients to ensure that they know what to watch for, when to seek help, and how to get the fastest medical attention.
In our study, patients in the ambulatory group had a shorter mean hospital stay and lower mean hospitalization cost. Studies on ambulatory surgery have reported different reduced hospitalization cost (28, 29). Shortening hospital stay improves the efficiency of medical resources, reduces economic burden, and enables more patients to receive surgical treatment.
In our study, there was no significant difference in HAM-A scores between the two groups, indicating that patients in the ambulatory group were no more anxious than those in the conventional group. Zeyu-Zhang reported more anxiety among patients in the ambulatory group (30, 31); this may be because we used multimedia to provide patients with a complete understanding of their condition and how to ensure their safety after discharge, thereby reducing anxiety.
Our study has several limitations: First, as this was a retrospective study, patient selection bias and confounding factors were inevitable. Second, most patients in our study were young and had few medical conditions; therefore, this study cannot be used as evidence for ambulatory TOETVA in patients with medical conditions or elderly patients. Third, the sample size in this study was not large enough to assess the impact of rare complications on safety, especially in patients treated with bilateral thyroidectomy. Fourth, the patients were not evaluated for vocal cord paralysis by routine laryngoscopy after surgery, which can lead to an underestimation of vocal cord paralysis. Finally, costs incurred at other medical centers after discharge were not included because they were not available in our system.
In conclusion, our study evaluated the safety, economic, and mental health impact of ambulatory TOETVA, which had not been reported in previous studies. The results showed that in skilled surgical centers, ambulatory TOETVA is a safe, feasible, and cost-effective procedure for selected patients. The reduction in hospital stay associated with TOETVA did not increase patient anxiety. The surgical team must strictly educate patients to ensure they know what to watch for, when to seek help, and how to get the fastest medical attention to ensure patient safety.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee of The Affiliated Yantai Yuhuangding Hospital of Qingdao University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Study design: HS. Modify the study design: HZ and YC. Data collection: GJZ and HS. Data analysis: HS, YC, and GBZ. Drafting the manuscript: HS. Project supervision: HZ. All authors contributed to the article and approved the submitted version.
Funding
Science and technology project of Shandong Society of Geriatrics (LKJGG2021W128).
Acknowledgments
We thank Editage for English language editing (www.editage.cn).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1116280/full#supplementary-material
Abbreviations
BMI, body mass index; HAM-A, Hamilton Anxiety Rating Scale; PTC, papillary thyroid carcinoma; PTH, parathyroid hormone; RLN, recurrent laryngeal nerve; TOETVA, transoral endoscopic thyroidectomy vestibular approach.
References
1. Nakajo A, Arima H, Hirata M, Mizoguchi T, Kijima Y, Mori S, et al. Trans-oral video-assisted neck surgery (TOVANS). a new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc (2013) 27:1105–10. doi: 10.1007/s00464-012-2588-6
2. Wang C, Zhai H, Liu W, Li J, Yang J, Hu Y, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery (2014) 155:33–8. doi: 10.1016/j.surg.2013.06.010
3. Wang Y, Zhou S, Liu X, Rui S, Li Z, Zhu J, et al. Transoral endoscopic thyroidectomy vestibular approach vs conventional open thyroidectomy: meta-analysis. Head Neck (2021) 43:345–53. doi: 10.1002/hed.26486
4. Wang D, Wang Y, Zhou S, Liu X, Wei T, Zhu J, et al. Transoral thyroidectomy vestibular approach versus non-transoral endoscopic thyroidectomy: a comprehensive systematic review and meta-analysis. Surg Endosc (2022) 36:1739–49. doi: 10.1007/s00464-021-08836-w
5. Steckler RM. Outpatient thyroidectomy: a feasibility study. Am J Surg (1986) 152:417–9. doi: 10.1016/0002-9610(86)90315-6
6. Murray B, Tandon S, Dempsey G. Ambulatory thyroidectomy: an anesthesiologist’s perspective. Local Reg Anesth (2017) 10:31–9. doi: 10.2147/LRA.S111554
7. Orosco RK, Lin HW, Bhattacharyya N. Ambulatory thyroidectomy: a multistate study of revisits and complications. Otolaryngol Head Neck Surg (2015) 152:1017–23. doi: 10.1177/0194599815577603
8. Lee DJ, Chin CJ, Hong CJ, Perera S, Witterick IJ. Outpatient versus inpatient thyroidectomy: A systematic review and meta-analysis. Head Neck (2018) 40:192–202. doi: 10.1002/hed.24934
9. Terris DJ, Snyder S, Carneiro-Pla D, Inabnet WB 3rd, Kandil E, Orloff L, et al. American Thyroid association statement on outpatient thyroidectomy. Thyroid (2013) 23:1193–202. doi: 10.1089/thy.2013.0049
10. Sun H, Wang X, Zheng G, Wu G, Zeng Q, Zheng H. Comparison between transoral endoscopic thyroidectomy vestibular approach (TOETVA) and conventional open thyroidectomy for patients undergoing total thyroidectomy and central neck dissection: A propensity score-matching analysis. Front Oncol (2022) 12:856021. doi: 10.3389/fonc.2022.856021
11. Zheng G, Ma C, Sun H, Wu G, Guo Y, Wu G, et al. Safety and surgical outcomes of transoral endoscopic thyroidectomy vestibular approach for papillary thyroid cancer: A two-centre study. Eur J Surg Oncol (2021) 47:1346–51. doi: 10.1016/j.ejso.2021.01.028
12. Zheng G, Wang X, Wu G, Sun H, Ma C, Zheng H, et al. The sensorimotor changes of the lower lip and chin after transoral endoscopic thyroidectomy vestibular approach. Updates Surg (2021) 73:2283–91. doi: 10.1007/s13304-021-01133-0
13. Compton RA, Simmonds JC, Dhingra JK. Total thyroidectomy as an ambulatory procedure in community practice. OTO Open (2020) 4:2473974X20957324. doi: 10.1177/2473974X20957324
14. Philteos J, Baran E, Noel CW, Pasternak JD, Higgins KM, Freeman JL, et al. Feasibility and safety of outpatient thyroidectomy: A narrative scoping review. Front Endocrinol (2021) 12:717427. doi: 10.3389/fendo.2021.717427
15. Noel CW, Griffiths R, Siu J, Forner D, Urbach D, Freeman J, et al. A population-based analysis of outpatient thyroidectomy: safe and under-utilized. Laryngoscope (2021) 131:2625–33. doi: 10.1002/lary.29816
16. Sun H, Zheng H, Wang X, Zeng Q, Wang P, Wang Y. Comparison of transoral endoscopic thyroidectomy vestibular approach, total endoscopic thyroidectomy via areola approach, and conventional open thyroidectomy: a retrospective analysis of safety, trauma, and feasibility of central neck dissection in the treatment of papillary thyroid carcinoma. Surg Endosc (2020) 34:268–74. doi: 10.1007/s00464-019-06762-6
17. Kang YJ, Cho JH, Stybayeva G, Hwang SH. Safety and efficacy of transoral robotic thyroidectomy for thyroid tumor: A systematic review and meta-analysis. Cancers (2022) 14:4230. doi: 10.3390/cancers14174230
18. Akritidou E, Douridas G, Spartalis E, Tsourouflis G, Dimitroulis D, Nikiteas NI. Complications of trans-oral endoscopic thyroidectomy vestibular approach: A systematic review. Vivo (2022) 36:1–12. doi: 10.21873/invivo.12671
19. Anuwong A, Ketwong K, Jitpratoom P, Sasanakietkul T, Duh QY. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg (2018) 153:21–7. doi: 10.1001/jamasurg.2017.3366
20. Chai YJ, Chae S, Oh MY, Kwon H, Park WS. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): surgical outcomes and learning curve. J Clin Med (2021) 10:863. doi: 10.3390/jcm10040863
21. Suzuki S, Yasunaga H, Matsui H, Fushimi K, Saito Y, Yamasoba T. Factors associated with neck hematoma after thyroidectomy: A retrospective analysis using a Japanese inpatient database. Med (Baltim) (2016) 95:e2812. doi: 10.1097/MD.0000000000002812
22. de Carvalho AY, Gomes CC, Chulam TC, Vartanian JG, Carvalho GB, Lira RB, et al. Risk factors and outcomes of postoperative neck hematomas: An analysis of 5,900 thyroidectomies performed at a cancer center. Int Arch Otorhinolaryngol (2021) 25:e421–7. doi: 10.1055/s-0040-1714129
23. Yu X, Jiang Y, Li Y, He Q, Pan L, Zhu P, et al. Comparison of different mandibular jawlines classifications on transoral endoscopic thyroidectomy for papillary thyroid carcinoma: experiences of 690 cases. Front Endocrinol Lausanne (2022) 13:842148. doi: 10.3389/fendo.2022.842148
24. You JY, Kim HY, Park DW, Yang HW, Kim HK, Dionigi G, et al. Transoral robotic thyroidectomy versus conventional open thyroidectomy: comparative analysis of surgical outcomes using propensity score matching. Surg Endosc (2021) 35:124–9. doi: 10.1007/s00464-020-07369-y
25. Mattoo S, Agarwal A, Mayilvaganan S, Mishra P, Agarwal G, Mishra A, et al. Role of postoperative intact serum PTH as an early predictor of severe post-thyroidectomy hypocalcemia: a prospective study. J Endocrinol Invest (2021) 44:1961–70. doi: 10.1007/s40618-021-01511-w
26. Long SM, Ali K, Tufano RP, Banuchi VE. Airway injury from transoral endoscopic thyroidectomy vestibular approach. Head Neck (2022) 44:E6–E10. doi: 10.1002/hed.26909
27. Ahn JH, Yi JW. Transoral endoscopic thyroidectomy for thyroid carcinoma: outcomes and surgical completeness in 150 single-surgeon cases. Surg Endosc (2020) 34:861–7. doi: 10.1007/s00464-019-06841-8
28. Friedlander DF, Krimphove MJ, Cole AP, Marchese M, Lipsitz SR, Weissman JS, et al. Where is the value in ambulatory versus inpatient surgery? Ann Surg (2021) 273:909–16. doi: 10.1097/SLA.0000000000003578
29. Romero Arenas MA. Appropriate selection of candidates for outpatient thyroidectomy. Curr Opin Endocrinol Diabetes Obes (2021) 28:547–51. doi: 10.1097/MED.0000000000000672
30. Zhang Z, Xia F, Wang W, Jiang B, Yao L, Huang Y, et al. Ambulatory thyroidectomy is safe and beneficial in papillary thyroid carcinoma: randomized controlled trial. Head Neck (2021) 43:1116–21. doi: 10.1002/hed.26557
Keywords: transoral endoscopic thyroidectomy vestibular approach, ambulatory, safety, mental health, hospitalization cost
Citation: Sun H, Chu Y, Zhang G, Zheng G and Zheng H (2023) The ambulatory transoral endoscopic thyroidectomy vestibular approach is safe and economical for patients with thyroid nodules. Front. Endocrinol. 14:1116280. doi: 10.3389/fendo.2023.1116280
Received: 05 December 2022; Accepted: 30 January 2023;
Published: 10 February 2023.
Edited by:
Xinying Li, Xiangya Hospital, Central South University, ChinaReviewed by:
Mehmet Haciyanli, Izmir Katip Celebi University, TürkiyeLei Sheng, Qilu Hospital, Shandong University, China
Copyright © 2023 Sun, Chu, Zhang, Zheng and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haitao Zheng, emhlbmdoYWl0YW8xOTcyQDEyNi5jb20=
†These authors have contributed equally to this work
 Haiqing Sun
Haiqing Sun Yongli Chu
Yongli Chu Guojun Zhang3
Guojun Zhang3 Guibin Zheng
Guibin Zheng