
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 20 February 2023
Sec. Bone Research
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1112534
Introduction: The risk of fragility fractures is increased in patients with type 2 diabetes mellitus (T2DM). Many reports indicate that inflammatory and immune responses are associated with osteoporosis and osteopenia. The monocyte-to-lymphocyte ratio (MLR) is a novel potential marker of inflammatory and immune responses. The present study evaluated the associations between the MLR and osteoporosis in postmenopausal females with T2DM.
Methods: Data were obtained from 281 T2MD postmenopausal females, and divided into three groups: Osteoporosis group, osteopenia group and normal BMD group.
Result: Data analyses revealed that the MLR was significantly lower in T2MD postmenopausal females with osteoporosis than in those with osteopenia and normal BMD. Logistic regression showed that the MLR was an independent protective factor for osteoporosis in postmenopausal females with T2DM (odds ratio [OR]: 0.015, 95% confidence interval [CI]: 0.000–0.772). Based on the receiver operating characteristic (ROC) curve, the MLR for diagnosing osteoporosis in postmenopausal females with T2DM was projected to be 0.1019, an area under the curve of 0.761 (95% CI: 0.685–0.838), a sensitivity of 74.8% and a specificity of 25.9%.
Conclusions: The MLR have a high efficacy in diagnosis for osteoporosis in postmenopausal females with T2DM. MLR have the potential to be used as diagnosis marker for osteoporosis in postmenopausal females with T2DM.
Fractures are a common complication of diabetes mellitus (DM) (1–3), and the risk of hip fracture is increased in patients with type 2 diabetes mellitus (T2DM) (4, 5), particularly in patients with T2DM and poorly controlled blood glucose (6). Research has also shown that patients with type 1 diabetes mellitus (T1DM) have decreased bone mineral density (BMD), and there is an increased risk of fracture in patients with T2DM (7, 8). T2DM is often associated with increased levels of pro-inflammatory cytokines, which have been implicated in the development of T2DM and microvascular and macrovascular complications. Chronic subclinical inflammation plays an important role in insulin resistance, metabolic syndrome and atherosclerosis (9, 10). Peripheral blood monocytes are classic indicators of inflammation, and peripheral blood monocytes are directly involved in osteoclast genesis. The monocyte-to-lymphocyte ratio (MLR) has been identified as a potential marker of inflammation in various conditions (11–13). Yue et al. previously reported that the MLR was an independent risk factor for diabetic retinopathy (14). The mechanism by which T2DM affects osteoporosis in postmenopausal females is unclear. The associations of the MLR and osteoporosis in postmenopausal females with T2DM have not been investigated to date. Therefore, the present study investigated the relationship between the MLR and osteoporosis in postmenopausal females with T2DM to evaluate the related factors influencing osteoporosis in postmenopausal females with T2DM.
The patients were evaluated in the Renmin Hospital of Wuhan University. We assessed a total of 281 postmenopausal patients diagnosed with diabetes. Patients were excluded if they had type 1 diabetes mellitus, any acute inflammation, active infection, cancer, chronic liver diseases, or any diabetic complications except for osteopenia or osteoporosis. This research was approved by the ethics committee, and written informed consent was obtained from all enrolled patients.
All subjects underwent dual energy X-ray bone densitometry to assess the T-score of BMD (DEXA, MEDILINK, France). The participants’ systolic blood pressures (SBP) and diastolic blood pressures (DBP) were measured after a 5-min rest using a sphygmomanometer. Venous blood samples were drawn after an overnight fast. All biochemical analyses were performed in our hospital, including a routine blood test, fasting blood glucose (FPG), fasting insulin (FINS), fasting C-peptide (FC-p), osteocalcin (OC), parathyroid hormone (PTH), serum uric acid (UA), 25-OH vitamin D3 (VitD3), total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), C-terminal telopeptide of type I collagen (β-CTX), high-density lipoprotein cholesterol (HDL-C), and glycosylated hemoglobin A1c (HbA1c), The MLR was calculated as the ratio of monocytes to lymphocytes.
Non-parametric analyses were used to compare non-normally distributed numerical variables, and the results were expressed as the median and interquartile range. Logistic regression was used to analyze Osteoporosis in postmenopausal females with T2DM with risk factors. Receiver operating characteristic (ROC) curve analysis was used to compare the prognostic power of the MLR for Osteoporosis in postmenopausal females with T2DM. The predictive validities were quantified as areas under the ROC curves. The positive predictive value (95% confidence interval (CI)) and negative predictive value (95% CI) were calculated using MedCalc ver. 15.2.2. Other analyses were performed using SPSS 22.0, and p<0.05 was considered statistically significant.
The postmenopausal females with T2DM were divided into three groups: Osteoporosis group, osteopenia group and normal BMD group. The clinical characteristics of the study population are shown in Table 1. The MLR were significantly lower in the osteoporosis group than those in the osteopenia group and the BMD normal group (Table 1). However, there was no significant difference in MLR between the osteopenia group and the normal BMD group. Age, menopausal years, β-CXT and OC were significantly higher in the osteoporosis group than those in the osteopenia group and the normal BMD group (Table 1). And the β-CTX in the osteopenia group was higher than that in the normal BMD group, but there was no statistical difference (p=0.087). Correlation analysis showed that MLR was positively correlated with hip and lumbar BMD, and β-CTX was negatively correlated with hip and lumbar BMD (Figure 1). Logistic regression analysis showed that the MLR was an independent protective factor for Osteoporosis in postmenopausal females with T2DM, while age and menopausal years were independent risk factor for Osteoporosis in postmenopausal females with T2DM. However, β-CTX was not an independent risk factor for Osteoporosis in postmenopausal females with T2DM (Table 2). ROC analysis showed that MLR had high diagnosis efficacy T2DM with osteoporosis in postmenopausal, with a cut-off value of 0.1019. Additionally, the area under ROC (AUC) of the MLR was 0.761 (95% CI: 0.685–0.838), the sensitivity and specificity were 74.8% and 25.9% respectively (Figure 2). The diagnostic efficacy of β-CTX is inferior to that of MLR, with a cut-off value of 637.3, an area under the curve of 0.710 (95% CI: 0.544–0.875), a sensitivity of 60.0% and a specificity of 13.0% (Figure 3).
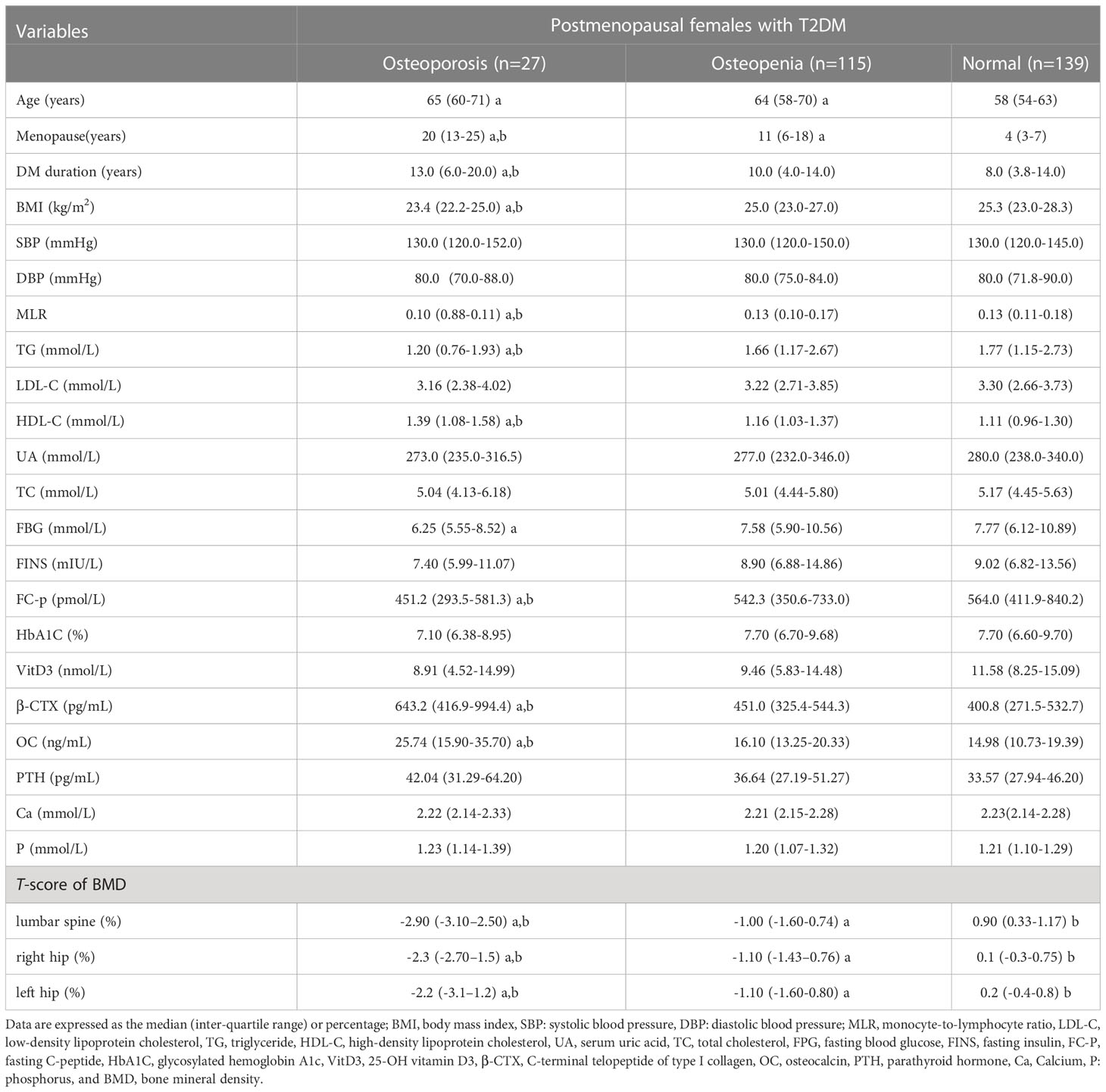
Table 1 Clinical characteristics in postmenopausal females with T2DM. vs.normal a, vs. Osteopenia b,.
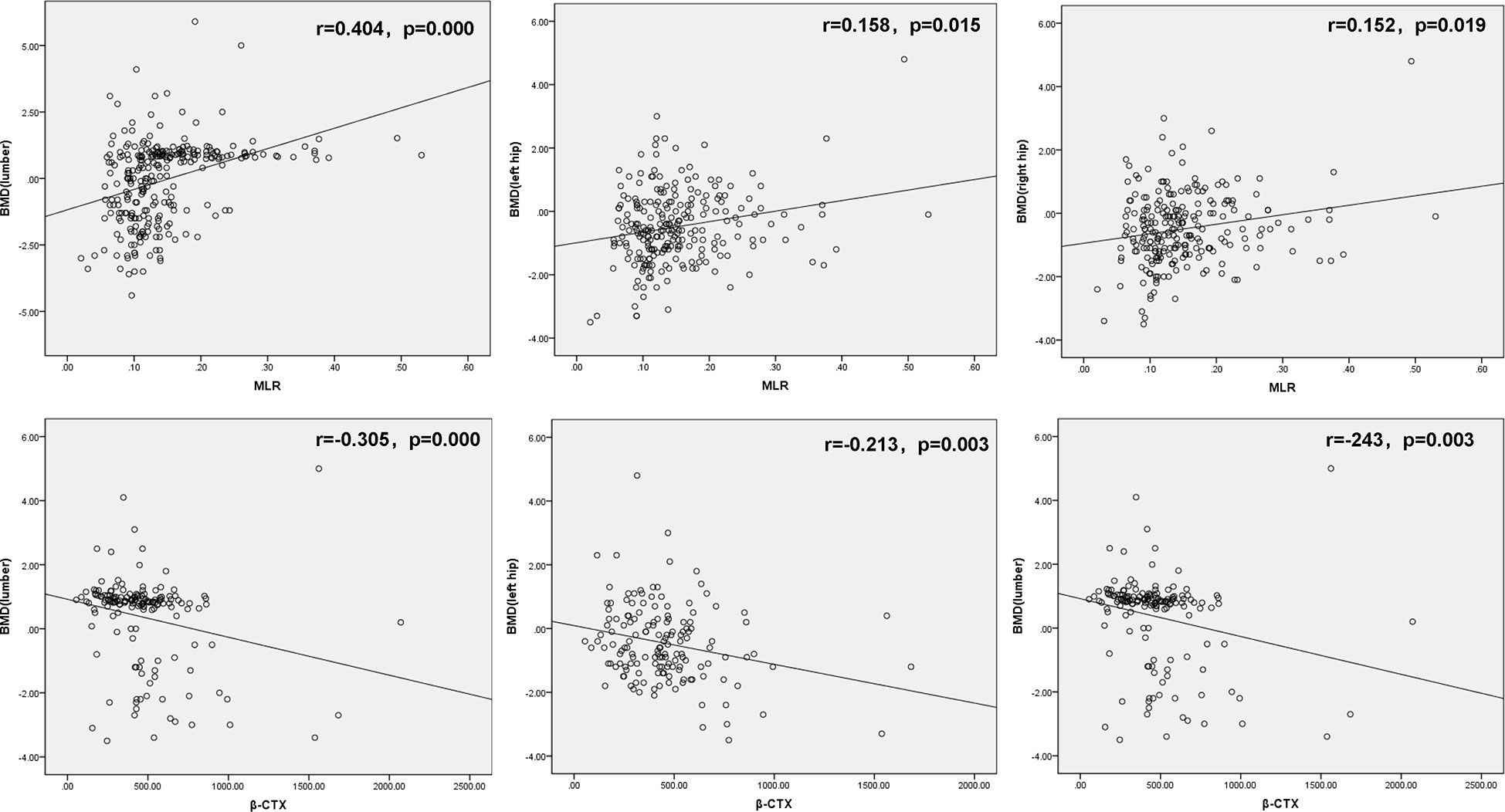
Figure 1 Correlation analysis of MLR with hip and lumbar BMD (up); Correlation analysis of MLR with hip and lumbar BMD (down). MLR, monocyte-to-lymphocyte ratio, β-CTX, C-terminal telopeptide of type I collagen and BMD, bone mineral density.
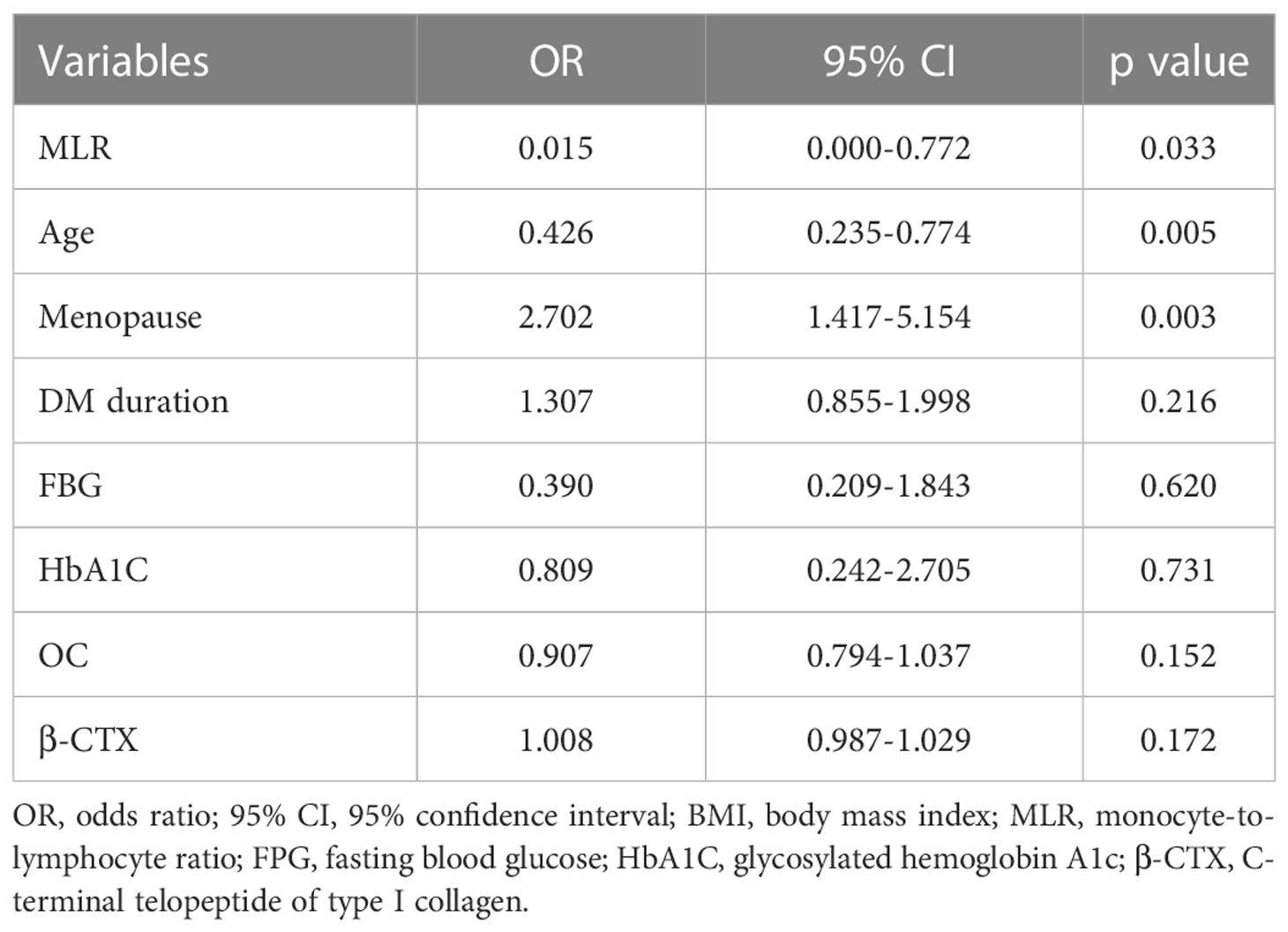
Table 2 Logistic regression analysis showing independent predictors of Osteoporosis in postmenopausal females with T2DM.
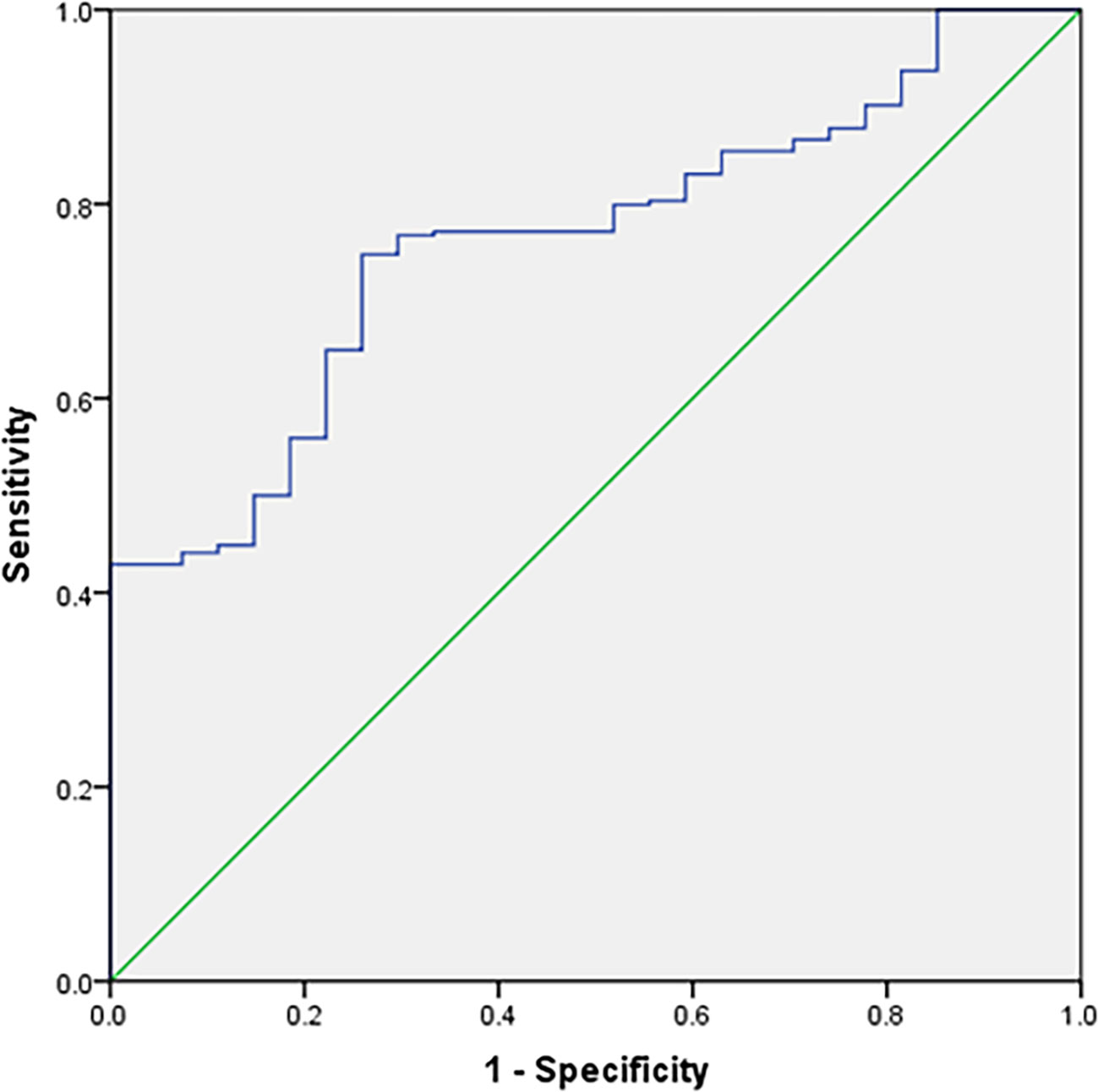
Figure 2 Receiver–operating characteristic (ROC) curve analysis for the monocyte-to-lymphocyte ratio as a predictor of Osteoporosis in postmenopausal females with T2DM (The sensitivity and specificity were 74.8% and 25.9%, respectively).
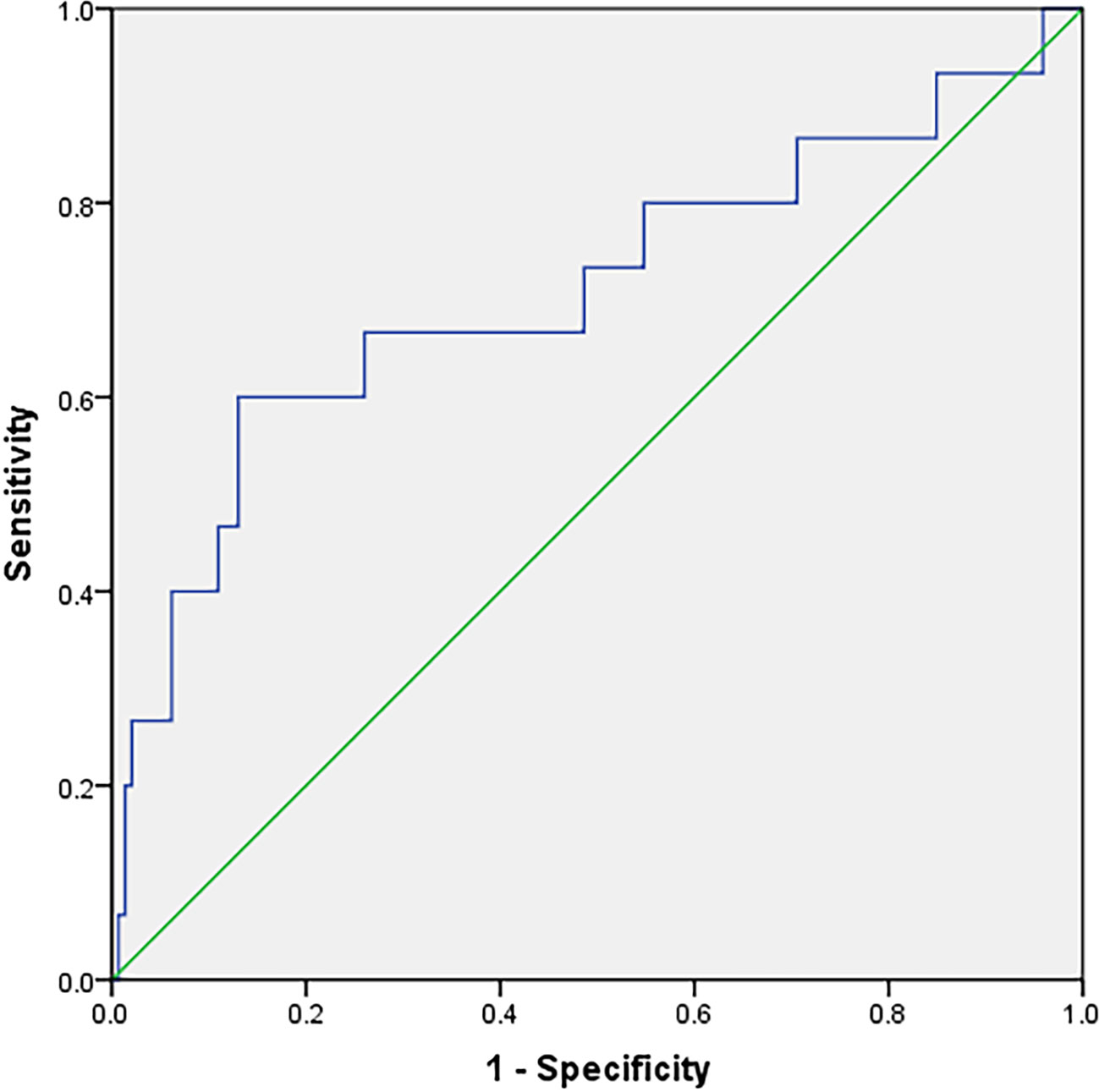
Figure 3 Receiver–operating characteristic (ROC) curve analysis for the β-CTX as a predictor of osteoporosis in postmenopausal females with T2DM (The sensitivity and specificity were 60.0% and 13.0%, respectively).
The MLR has been studied in many subjects, this was the first time the MLR was used as a marker of the relationship between the MLR and osteoporosis in postmenopausal females with T2DM. Our results indicate that the MLR is significantly higher in non-osteoporosis than osteoporosis in postmenopausal females with T2DM, and the MLR was an independent protective factor for osteoporosis with T2DM in postmenopausal females.
T2DM is associated with impaired bones, it is possible that bone microvascular disease impairs the mechanotactic function of osteocytes, bone turnover and collagen properties (15). The cytokines TNF and IL-6 are increased in patients with obesity and metabolic syndrome, and in hyperglycemic states, tissues exposed to inflammatory cytokines, such as IL-1, IL-6 and TNF, produce reactive oxygen species (ROS) that directly affects the differentiation and survival of osteoclasts, osteoblasts and osteocytes (16). TNF also stimulates osteoclast genesis and inhibits osteoblast genesis (17). Counts of white blood cells and their subtypes are important inflammatory markers associated with the pathophysiologic process of many diseases. In addition, many findings have revealed the predictive effects of the platelet-to-lymphocyte ratio (PLR) and neutrophil-to-lymphocyte ratio (NLR), particularly in DM, acute coronary syndromes, and various cancers (18–20). The MLR is an important marker of inflammation and the immune response and is related to tumor prognosis (21) and the MLR is also an independent risk factor for diabetic retinopathy (14). Because monocytes and lymphocytes play a crucial role in the induction and maintenance of an immune response, the MLR is used as a maker to measure vaccine efficacy in malaria (11). RANK and CCR6 expressed on monocytes are targets for the regulation of bone resorption in rheumatoid arthritis and osteoporosis (22). Previously reported that under suitable stimulation conditions, monocytes/macrophages can differentiate into osteoclasts (23). Studies have also demonstrated that activated T cells can induce osteoclast genesis by up-regulating the production of inflammatory cytokines (24, 25). Th17 cells are a critical modulator of the pathogenesis of estrogen-deficient osteoporosis (26). Together, these studies indicate that the MLR may be correlated with antibody or T cell responses involved in osteoporosis and osteopenia. Moreover, inflammation and immune responses are involved in the pathological process of osteoporosis and osteopenia, the MLR may be useful as a marker of inflammation in these conditions.
β-CTX is commonly used in clinical evaluation of bone metabolism, but was found in our study using the MLR as a marker to predict osteoporosis in postmenopausal females with T2DM is more reliable than β-CTX. Both MLR and β-CTX showed significant differences in the osteoporosis group compared with the normal BMD group, but β-CTX in the osteopenia group was also significantly higher than that in the normal BMD group, while there was no difference in MLR between the osteopenia group and the normal BMD group, it is suggested that MLR has higher specificity for osteoporosis. The ROC curve also confirmed that the sensitivity and specificity of MLR as a diagnosis of osteoporosis were better than those of β-CTX, therefore MLR was a better predictor of osteoporosis in menopausal females with T2DM than β-CTX and the MLR can be easily measured and cheaper. Although our study showed that the MLR may be an independent protective factor for osteoporosis in postmenopausal females with T2DM, the mechanism for how the MLR impacts osteoporosis in postmenopausal females with T2DM is unclear and warrants further investigation. We also found that the osteoporosis group was older than the normal BMD group and that age was an independent risk factor for osteoporosis in postmenopausal females with T2DM; and the duration of menopause was also significantly higher in the osteoporosis group than in the other two groups, this is consistent with previous research findings.
There are some limitations of our study. First, by restricting the clinical sample, our study did not include osteoporosis in males with T2DM. Second, the MLR was significantly higher in osteopenia group and normal BMD group, however, monocytes exhibit the potential to differentiate into osteoclasts. The increase of monocyte ratio leads to the increase of BMD, which needs further research to verify.
In conclusion, the MLR was significantly lower in T2DM postmenopausal females with osteoporosis than in those with osteopenia and normal BMD. And the MLR was an independent protective factor for osteoporosis in postmenopausal females with T2DM.
Additionally, the MLR have a high efficacy in diagnosis for osteoporosis in postmenopausal females with T2DM. MLR have the potential to be used as diagnosis marker for osteoporosis in postmenopausal females with T2DM.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Clinical Ethics Committee, Renmin Hospital of Wuhan University. The patients/participants provided their written informed consent to participate in this study.
HL and SW participated in the study design, figures, data interpretation and writing; XiZ, QioZ, QiZ, XuZ. and TX participated in data analysis, data interpretation and writing; HL participated in figures, SW participated in the literature search, figures, study design, data analysis, interpretation and writing. All authors contributed to the article and approved the submitted version.
SW supported by “the Fundamental Research Funds for the Central Universities (No. 2042022kf1120).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Khosla S, Samakkarnthai P, Monroe DG, Farr JN. Update on the pathogenesis and treatment of skeletal fragility in type 2 diabetes mellitus. Nat Rev Endocrinol (2021) 17(11):685–97. doi: 10.1038/s41574-021-00555-5
2. Van Hulten V, Rasmussen N, Driessen JHM, Burden AM, Kvist A, van den Bergh JP. Fracture patterns in type 1 and type 2 diabetes mellitus: A narrative review of recent literature. Curr osteoporos Rep (2021) 19(6):644–55. doi: 10.1007/s11914-021-00715-6
3. Dou J, Wang J, Zhang Q. Differences in the roles of types 1 and 2 diabetes in the susceptibility to the risk of fracture: A systematic review and meta-analysis. Diabetol Metab syndr (2021) 13(1):84. doi: 10.1186/s13098-021-00687-8
4. Compston J. Type 2 diabetes mellitus and bone. J Internal Med (2018) 283(2):140–53. doi: 10.1111/joim.12725
5. Eller-Vainicher C, Cairoli E, Grassi G, Grassi F, Catalano A, Merlotti D, et al. Pathophysiology and management of type 2 diabetes mellitus bone fragility. J Diabetes Res (2020) 2020:7608964. doi: 10.1155/2020/7608964
6. Li CI, Liu CS, Lin WY, Meng NH, Chen CC, Yang SY, et al. Glycated hemoglobin level and risk of hip fracture in older people with type 2 diabetes: A competing risk analysis of Taiwan diabetes cohort study. J Bone miner Res (2015) 30(7):1338–46. doi: 10.1002/jbmr.2462
7. Lekkala S, Taylor EA, Hunt HB, Donnelly E. Effects of diabetes on bone material properties. Curr osteoporos Rep (2019) 17(6):455–64. doi: 10.1007/s11914-019-00538-6
8. Zhu Q, Xu J, Zhou M, Lian X, Xu J, Shi J. Association between type 1 diabetes mellitus and reduced bone mineral density in children: A meta-analysis. Osteoporos Int (2021) 32(6):1143–52. doi: 10.1007/s00198-020-05715-3
9. Tsai JC, Sheu SH, Chiu HC, Chung FM, Chang DM, Chen MP, et al. Association of peripheral total and differential leukocyte counts with metabolic syndrome and risk of ischemic cardiovascular diseases in patients with type 2 diabetes mellitus. Diabetes Metab Res Rev (2007) 23(2):111–8.
10. Lin Q, Zhou W, Wang Y, Huang J, Hui X, Zhou Z, et al. Abnormal Peripheral Neutrophil Transcriptome in Newly Diagnosed Type 2 Diabetes Patients. J Diabetes Res (2020) 2020:9519072.
11. Warimwe GM, Fletcher HA, Olotu A, Agnandji ST, Hill AV, Marsh K, et al. Peripheral blood monocyte-to-lymphocyte ratio at study enrollment predicts efficacy of the RTS,S malaria vaccine: Analysis of pooled phase II clinical trial data. BMC Med (2013) 11:184. doi: 10.1186/1741-7015-11-184
12. Xiang J, Zhou L, Li X, Bao W, Chen T, Xi X, et al. Preoperative monocyte-to-Lymphocyte ratio in peripheral blood predicts stages, metastasis, and histological grades in patients with ovarian cancer. Trans Oncol (2017) 10(1):33–9. doi: 10.1016/j.tranon.2016.10.006
13. Gatechompol S, Sophonphan J, Kerr SJ, Ubolyam S, Avihingsanon A, van Leth F, et al. Monocyte-to-lymphocyte ratio as a predictor of TB among people living with HIV. Int J tuberculosis Lung Dis (2021) 25(11):933–8. doi: 10.5588/ijtld.21.0300
14. Yue S, Zhang J, Wu J, Teng W, Liu L, Chen L. Use of the monocyte-to-Lymphocyte ratio to predict diabetic retinopathy. Int J Environ Res Public Health (2015) 12(8):10009–19. doi: 10.3390/ijerph120810009
15. Wongdee K, Krishnamra N, Charoenphandhu N. Derangement of calcium metabolism in diabetes mellitus: negative outcome from the synergy between impaired bone turnover and intestinal calcium absorption. J Physiol Sci JPS (2017) 67(1):71–81. doi: 10.1007/s12576-016-0487-7
16. Manolagas SC. From estrogen-centric to aging and oxidative stress: A revised perspective of the pathogenesis of osteoporosis. Endocr Rev (2010) 31(3):266–300. doi: 10.1210/er.2009-0024
17. Zhou L, Song H, Zhang Y, Ren Z, Li M, Fu Q. Polyphyllin VII attenuated RANKL-induced osteoclast differentiation via inhibiting of TRAF6/c-Src/PI3K pathway and ROS production. BMC musculoskelet Disord (2020) 21(1):112. doi: 10.1186/s12891-020-3077-z
18. Semeniuk-Wojtaś A, Lubas A, Stec R, Syryło T, Niemczyk S, Szczylik C. Neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and c-reactive protein as new and simple prognostic factors in patients with metastatic renal cell cancer treated with tyrosine kinase inhibitors: A systemic review and meta-analysis. Clin genitourinary cancer (2018) 16(3):e685–93. doi: 10.1016/j.clgc.2018.01.010
19. Zheng Q, Liu J, Ji Y, Zhang Y, Chen X, Liu B. Elevated levels of monocyte-lymphocyte ratio and platelet-lymphocyte ratio in adolescents with non-suicidal self-injury. BMC Psychiatry (2022) 22(1):618. doi: 10.1186/s12888-022-04260-z
20. Chang LS, Lin YJ, Yan JH, Guo MM, Lo MH, Kuo HC. Neutrophil-to-lymphocyte ratio and scoring system for predicting coronary artery lesions of Kawasaki disease. BMC pediatr (2020) 20(1):398. doi: 10.1186/s12887-020-02285-5
21. Eo WK, Kwon S, Koh SB, Kim MJ, Ji YI, Lee JY, et al. The lymphocyte-monocyte ratio predicts patient survival and aggressiveness of endometrial cancer. J Cancer (2016) 7(5):538–45. doi: 10.7150/jca.14206
22. Nanke Y, Kobashigawa T, Yago T, Kawamoto M, Yamanaka H, Kotake S. RANK expression and osteoclastogenesis in human monocytes in peripheral blood from rheumatoid arthritis patients. BioMed Res Int (2016) 2016:4874195. doi: 10.1155/2016/4874195
23. Jiang P, Gao W, Ma T, Wang R, Piao Y, Dong X, et al. CD137 promotes bone metastasis of breast cancer by enhancing the migration and osteoclast differentiation of monocytes/macrophages. Theranostics (2019) 9(10):2950–66. doi: 10.7150/thno.29617
24. Yang X, Zhou F, Yuan P, Dou G, Liu X, Liu S, et al. T Cell-depleting nanoparticles ameliorate bone loss by reducing activated T cells and regulating the Treg/Th17 balance. Bioact mater (2021) 6(10):3150–63. doi: 10.1016/j.bioactmat.2021.02.034
25. Fischer V, Haffner-Luntzer M. Interaction between bone and immune cells: Implications for postmenopausal osteoporosis. Semin Cell Dev Biol (2022) 123:14–21. doi: 10.1016/j.semcdb.2021.05.014
Keywords: osteoporosis, T2DM, postmenopausal females, monocyte-to-lymphocyte, retrospective study
Citation: Li H, Zhang X, Zhang Q, Zhang Q, Zhu X, Xie T and Wang S (2023) The relationship between the monocyte-to-lymphocyte ratio and osteoporosis in postmenopausal females with T2DM: A retrospective study in Chinese population. Front. Endocrinol. 14:1112534. doi: 10.3389/fendo.2023.1112534
Received: 30 November 2022; Accepted: 30 January 2023;
Published: 20 February 2023.
Edited by:
Ting Zheng, Hospital for Special Surgery, United StatesReviewed by:
YU-HSIANG HSU, National Cheng Kung University, TaiwanCopyright © 2023 Li, Zhang, Zhang, Zhang, Zhu, Xie and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuo Wang, ZGRkNDU2ODUyQDEyNi5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.