- 1Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
- 2Haas School of Business, University of California Berkeley, Berkeley, CA, United States
- 3The Netherlands Cancer Institute (NKI), Amsterdam, Netherlands
- 4Feinberg Cardiovascular and Renal Research Institute, Northwestern University, School of Medicine, Chicago, IL, United States
- 5Endocrinology and Metabolism Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
- 6Heller School for Social Policy and Management, Brandeis University, Waltham, MA, United States
- 7Institute for Clinical Research and Health Policy Studies, Tufts Medical Center, Boston, MA, United States
Aims: To investigate the journey of patients with diabetes in the healthcare system using nationally-representative patient-reported data.
Methods: Participants were recruited using a machine-learning-based sampling method based on healthcare structures and medical outcome data and were followed up for three months. We assessed the resource utilization, direct/indirect costs, and quality of healthcare services.
Results: One hundred fifty-eight patients with diabetes participated. The most utilized services were medication purchases (276 times monthly) and outpatient visits (231 times monthly). During the previous year, 90% of respondents had a laboratory fasting blood glucose assessment; however, less than 70% reported a quarterly follow-up physician visit. Only 43% had been asked about any hypoglycemia episodes by their physician. Less than 45% of respondents had been trained for hypoglycemia self-management. The annual average health-related direct cost of a patient with diabetes was 769 USD. The average out-of-pocket share of direct costs was 601 USD (78.15%). Medication purchases, inpatient services, and outpatient services summed up 79.77% of direct costs with a mean of 613 USD.
Conclusion: Healthcare services focused solely on glycemic control and the continuity of services for diabetes control was insufficient. Medication purchases, and inpatient and outpatient services imposed the most out-of-pocket costs.
Introduction
Diabetes mellitus (hereafter diabetes) is one of the most significant global public health concerns causing 916 Disability-Adjusted Life-Years (DALYs) per 100,000 population in 2019 worldwide (1). Despite the previous efforts, diabetes remains the second most significant cause of reduced healthy life expectancy (2). The International Diabetes Federation (IDF) estimated that unless effective prevention methods are employed, the prevalence of diabetes will increase by 54% in 2045 (3). On the national scale, the prevalence of diabetes has risen roughly 30% in Iran in the last decade, which is alarmingly higher than the global estimations (4).
The presence of diabetes is associated with increased mortality from infections, cardiovascular diseases, stroke, chronic kidney diseases, chronic liver diseases, and cancers (5). Uncontrolled diabetes can impose high direct and indirect costs on patients and healthcare systems. The annual costs attributable to diabetes were estimated to be US$1.31 trillion worldwide or 1.8% of the global gross domestic product (GDP), two-thirds of which were direct medical costs, and the one-third were indirect costs (6). In the meantime, diabetes costs are expected to grow considerably, disproportionately affecting low- and middle-income countries, where 80% of patients with diabetes live (7).
Delivery of essential medications, blood glucose management, cardiometabolic risk factors elimination, and early screening for complications via well-organized care reduce acute and chronic complications and extends healthy life expectancy among patients with diabetes (8, 9). Nevertheless, the comprehensive, evidence-based diabetes care delivery is suboptimal even in well-resourced health systems (10). Notably, multicomponent quality improvement programs have been beneficial in achieving diabetes care goals (11). In this sense, investigating healthcare quality and costs for diabetes is essential to make evidence-based decisions to lower the costs and increase the quality of care.
Thus, the objective of this study was to investigate the journey of patients with diabetes in the healthcare system via assessing the healthcare utilization, quality, and costs on a national level in Iran based on the results of the Iran Quality of Care in Medicine Program (IQCAMP). IQCAMP is a series of longitudinal surveys focusing on seven high-prevalence and high-cost diseases, including chronic obstructive pulmonary disease, congestive heart failure, diabetes mellitus, end-stage renal failure, major depressive disorder, myocardial infarction, and stroke (12). We believe this study serves as guidance on assessing the care for diabetes at the national level in a minimal but sufficient way, particularly in countries with a similar context. It could also shed light on the likely scenarios of diabetic patients go through where the healthcare system resembles Iranian healthcare architecture.
Materials and methods
Overview
The current demonstration study is part of a nationally representative IQCAMP survey generating patient-centered real-world data on the utilization, costs, and quality of care for seven high-prevalence and high-cost diseases in Iran from 2016 to 2018. This study reports first-hand data on patient experience regarding healthcare utilization, costs, and quality of care for diabetes.
Study protocol
The patients in the IQCAMP study were selected using a novel sampling method, the details of which are provided elsewhere (12). A machine-learning-based sampling method was used to divide the 31 provinces into eight clusters considering their similarity in healthcare structure and outcome data. One province from each cluster was selected for data collection. Simulation analysis of the sampling revealed an efficiency of up to 70% (12). In the selected clusters, patients with diabetes (13) were selected from the participants with diabetes from the STEPwise Approach to NCD Risk Factor Surveillance (STEPS) 2016 study, a national cross-sectional survey carried out by the Non-Communicable Diseases Research Center (NCDRC). Participants of the STEPS survey were selected via multistage cluster sampling, and they were representative of the general population aged ≥18 years living in urban and rural areas in all provinces of Iran. A detailed description of the study population and the sampling method of the STEPS survey has been published elsewhere (14). Diabetes was defined as the presence of fasting plasma glucose > 7 mmol/L or A1C > 6.5% or a past medical history of confirmed diabetes that is under treatment. All patients with diabetes who were aware of their disease were invited to participate in the study. Trained nurses called the patients and gave them detailed instructions on the study objectives and their right to leave the study at any time. All participants provided written informed consent. We collected the data through the phone. The initial interview included the participants’ current and past medical history. Then, three monthly follow-up interviews were held to collect information on service utilization, quality indicators, and the cost of healthcare services received. Tehran Medical Science University’s ethics committee and the National Institute of Medical Research Development (NIMAD) approved the patient recruitment protocol.
Variable and data collection
The study assessed variables addressing utilization, quality, and costs of healthcare services. Healthcare services were categorized into three major groups: therapeutic, diagnostic, and patient support services. Therapeutic services included inpatient care, ambulatory care, and medication coverage. Lab and imaging services constituted diagnostic services. Rehabilitation could consist of healthcare services such as physiotherapy, occupational therapy, and speech therapy. Data were gathered from the health records of participants who underwent hospitalization and structured questionnaire-based interviews. Domain experts in epidemiology and endocrinology developed the initial draft of the study questionnaire, which patients with diabetes then debriefed. Finally, the study questionnaire was hosted on an android provisioned device and then went through usability testing for the study interviewers. The questionnaire consisted of four cardinal sections, including questions regarding participants’ sociodemographic and health status, frequencies of the utilization of various healthcare services, quality indicators, and healthcare costs.
The sociodemographic section included sex, age, literacy, and household wealth index. Principal Component Analysis (PCA) was applied to derive the household wealth index based on questions on key dwelling characteristics and household ownership, as described in the study protocol. PCA is an approach to statistical analysis in which multiple datasets are combined as orthogonal components (15). The wealth index was used to divide the population into quintiles, whereby the first and fifth quintiles present the least fortunate and wealthiest households, respectively. In the utilization section, participants were asked to declare frequencies of the utilization of any healthcare services throughout the study period. In addition, all medications available in the Iranian Pharmacopoeia were included in the survey.
A selection of pre-defined quality indicators was utilized to assess the quality of provided healthcare services. A panel of medical experts managing patients with diabetes considered different quality indicators using the guidelines of the Ministry of Health and Medical Services of Iran, frameworks utilized in developing countries, and the National Qualification Framework (NQF) designed for the United States (US) (16). The study’s expert panel added several essential indices based on their experience or literature review. The questionnaire was face-validated and then updated after a pilot study with the participation of ten patients.
Hospital invoices and patients’ out-of-pocket share were investigated to calculate the healthcare services’ costs. The related travel and accommodation expenses were added to calculate the direct cost of the disease. Lower income due to diabetes, loss of productivity, and wasted time of the patient and their possible accompanying family members during the doctor-patient appointments were calculated as indirect costs. Questions regarding healthcare diagnostic, therapeutic, and patient-support services were asked to help with out-of-pocket share estimations.
Data analysis
The unit of analysis was defined as person-month. Annual average costs of diabetes were calculated by the average cost of each month multiplied by 12. Purchasing Power Parity (PPP) for 2018 was applied to convert Iranian Rials to US Dollars (USD), 1000 USD equaled 16,773,000 Iranian Rials (17). The number of absent days from work due to diabetes multiplied by the minimum daily wage was calculated the loss due to diabetes. We computed loss of productivity by asking the patients how much less they had earned in a month when they struggled with diabetes complications compared to a normal month. Diabetes care quality was assessed by reporting the percentage of participants meeting the defined quality standards. All quantitative data are reported by mean, standard deviation, number, and percent.
Results
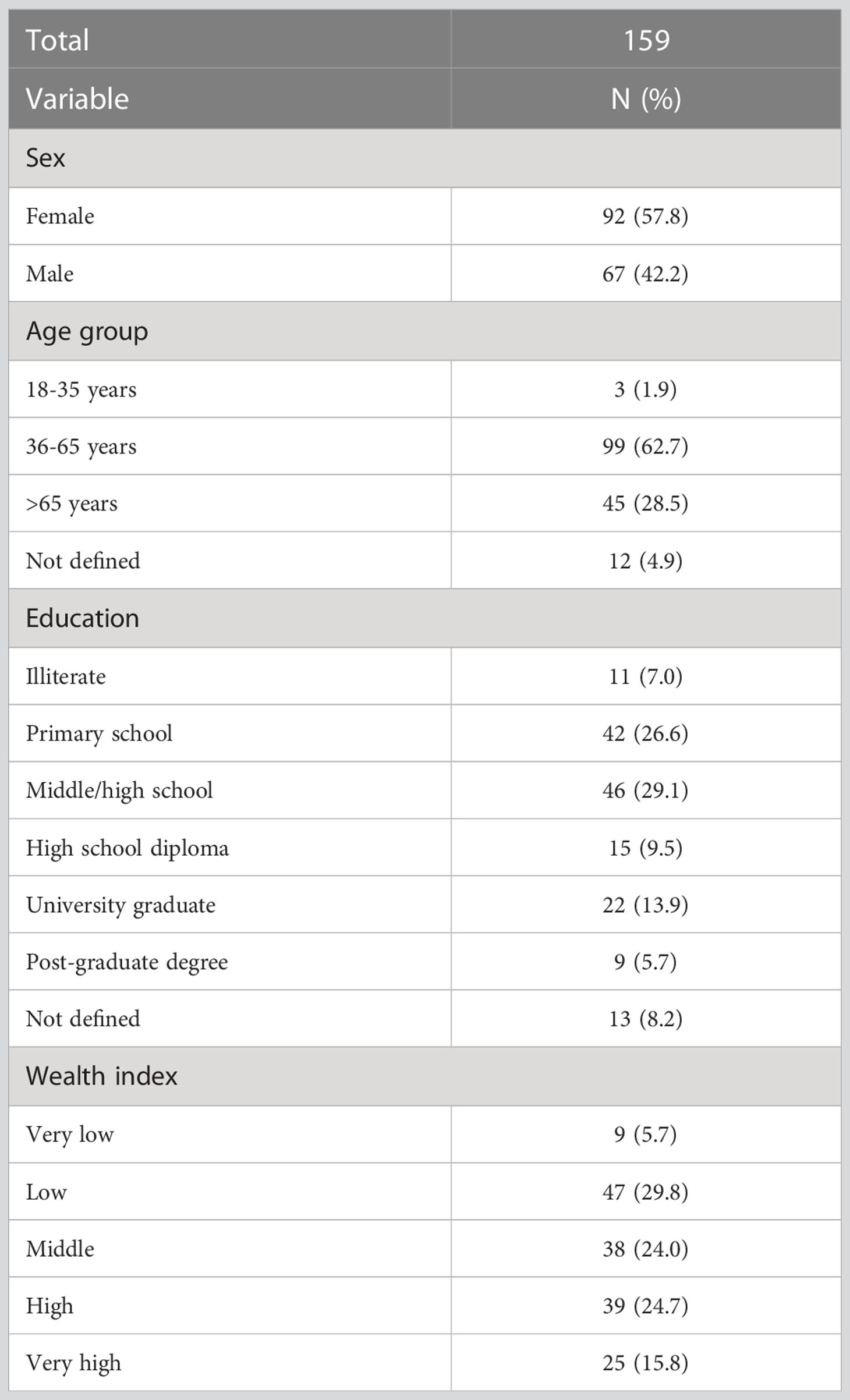
The final sample included 158 patients, among whom 91 (57.6%) were women. All patients underwent three successive monthly follow-ups, summing up to 474 patient months. The sociodemographic characteristics of participants are presented in Table 1.
Healthcare utilization
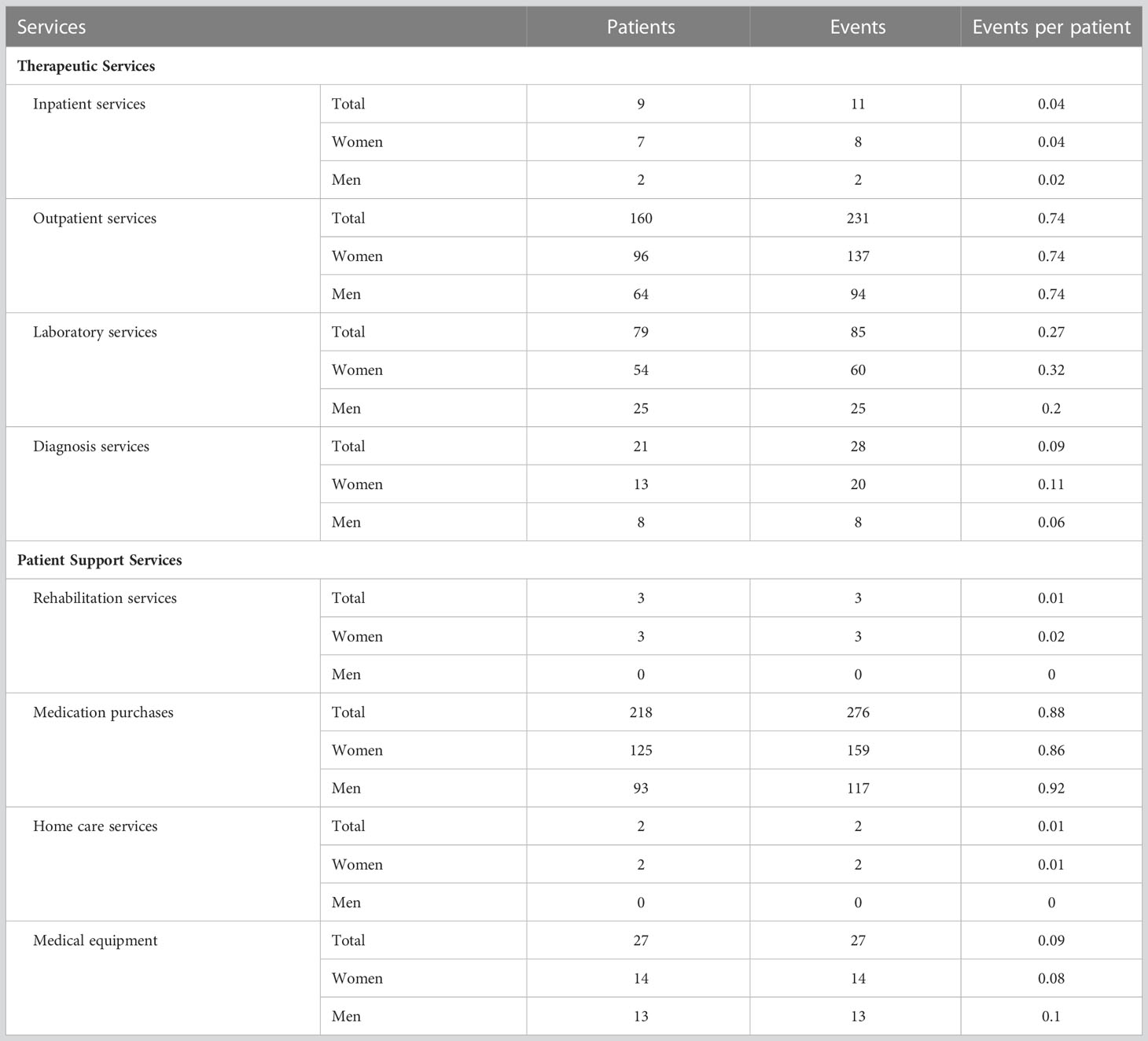
The most utilized services were medication purchase, with times per month (159 times among women and 117 among men). The second most utilized type of healthcare service was outpatient visits with 231 times per month (137 times among women and 94 among men). Table 2 presents the monthly utilization of various diabetes-related services among 474 visits.
Healthcare quality
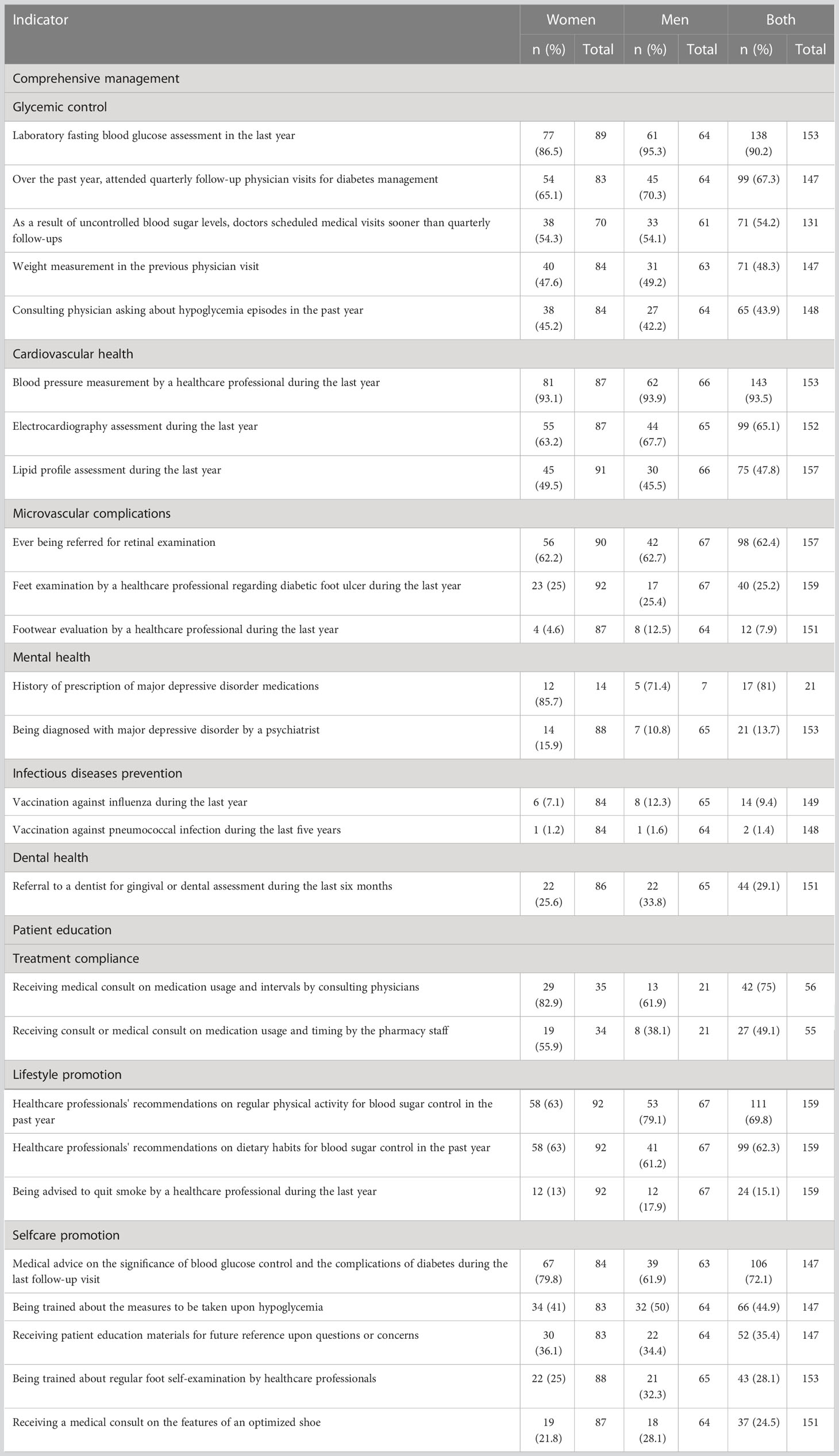
The mean (SD) time from the last laboratory blood sugar assessment was 4.44 (5.33) months, 3.5 (3.05) months among women, and 6.02 (6.51) months among men. While more than 90% of respondents showed a history of laboratory fasting blood glucose assessment in the previous year, less than 70% reported quarterly follow-up physician visits for diabetes management. During the follow-up visits in the last year, 93% of respondents reported that their blood pressure was measured during the office visit. However, less than half of the respondents reported weight measurement by any healthcare professional. While 75% of respondents reported receiving instructions on medication use from their consulting physicians, less than 50% said that pharmacy staff explained the medication use and timing.
Among 129 respondents, 9 (7.0%) had a history of ambulatory care due to hyper or hypoglycemia during the last year: 8 (10.4%) among women and 1 (1.9%) among men. An average of 3.71 (4.04) hypoglycemia episodes resulted in hospital admissions or outpatient visits in the previous year, 4.5 (5.2) among women and 2.67 (1.12) among men. Nevertheless, only 43% the respondents reported being interviewed for hypoglycemia episodes by their consulting physician during the last year. Notably, less than 45% of respondents reported receiving any training about hypoglycemia self-management from their physician or any other healthcare provider. The mean (SD) number of hyperglycemia episodes that have resulted in hospital admission or an outpatient visit in the previous year was 2.26 (1.5), 2.05 (1.4) among women, and 3 (1.7) among men. While 72% of respondents reported receiving medical advice on the significance of blood glucose control during the last follow-up visit, only 54% reported that their physicians had advised them to have more frequent follow-up visits for uncontrolled blood glucose.
Regarding lifestyle modification consults, around 70% of respondents received at least one episode of advice for regular physical activity and 62% for proper dietary habits. Only a quarter of respondents reported undergoing foot examinations by healthcare professionals, and less than 8% said that their shoes had been evaluated for diabetic foot prevention. Regarding diabetic foot prevention, less than 30% of respondents reported being trained for a regular self-foot examination and how to select the correct pair of shoes. Only 35% of respondents said they had received patient education materials for future reference. And finally, less than 10% of respondents reported receiving an influenza vaccine during the previous year, and 1.4% reported vaccination against pneumococcal infection during the last five years (Table 3).
Healthcare costs
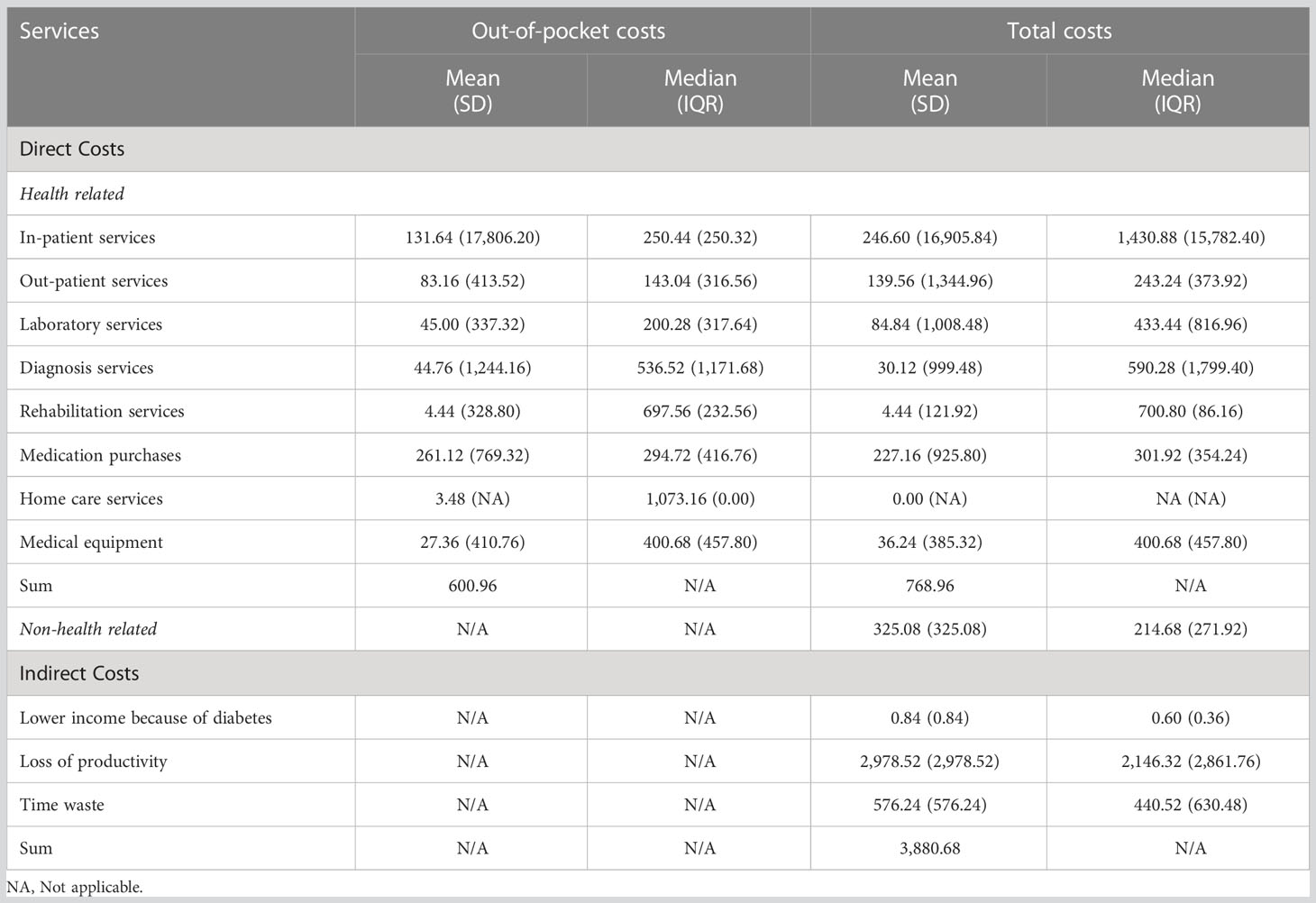
Table 4 conveys the direct and indirect costs of diabetes. The annual average direct health-related cost of a patient with diabetes was 768.96 USD. The average out-of-pocket share of direct health-related costs was 600.96 (78.15%) USD. Medication purchases, inpatient services, and outpatient services summed up 79.77% of direct health-related costs with a mean of 613.4 USD.
Discussion
This study is the first nationally representative research that collects cost and quality information directly from patients at the national level. Medication purchases and outpatient medical visits were the most utilized healthcare services. Most direct costs were for medications and inpatient and outpatient services. Medication purchases and inpatient and outpatient services imposed the most significant proportion of out-of-pocket costs. The healthcare system's primary focus was on glycemic control rather than a fair distribution of services across preventive and therapeutic care according to standard guidelines for diabetes management (18).
Approximately 80% the direct health-related costs of diabetes were for medication purchases, inpatient services, and outpatient services. Similarly, it has been reported that inpatient and medication costs were the most expensive aspects of diabetes care in low- and middle-income countries (19). On average, out-of-pocket share constituted 78% of the total direct costs, primarily due to medication purchases. Evidence shows that change in out-of-pocket share for diabetes medications across various payer policies impacts diabetes medication usage. Patients sharing fewer drug payments tend to have a significantly higher number of months with apparent active medication coverage, a proxy for medication adherence (20).
Continuous medical care is required to achieve optimal glycemic control among patients with diabetes and prevent diabetes complications. The respondents reported receiving inpatient or outpatient healthcare services at least two times during the previous year. While home care could lead to improved diabetes-related outcomes among patients (21), it was among the least utilized services by respondents. It has been reported that some one-third of the inappropriate all-causes hospitalization stays in Iran were due to lack of home care, 35% of which was attributable to diabetes complications (22). Thus, establishing appropriate home care in the health system as well as covering home care expenses by insurance could optimize hospital bed use, reduce costs, decrease readmission rates, and prevent hospital-related complications.
More than half of the respondents said they were not asked about hypoglycemia episodes by their consulting physician during their routine follow-up visits in the last year. Based on patients’ reports, healthcare professionals did not train the patients in self-management of hypoglycemia episodes. Nevertheless, intensive antidiabetic treatments could impose patients at increased risk of hypoglycemia. While hypoglycemia-associated risk factors are yet to be adequately understood (23), the frequency and severity of hypoglycemia could be decreased via structured patient education (24). Telemedicine, as a novel and accessible tool, could be along with proper patient education to monitor blood glucose, thus reducing the risk of hypoglycemia (25).
Despite the clear benefit of weight loss in glycemic management (26), only a tiny percentage of patients with diabetes can maintain substantial weight loss (27). Notably, frequent follow-up visits can better achieve weight management (28). In our study, less than half of the respondents reported that they underwent weight measurement by healthcare professionals during the follow-up visits. However, 70% of respondents had been advised for regular physical activity and 60% for proper dietary habits.
Only a quarter of respondents reported undergoing foot examination by healthcare professionals, and less than one-tenth said their footwear had been evaluated for diabetic foot prevention. Moreover, less than one-third of respondents reported being trained in the regular self-foot examination and the features of an optimized shoe for patients with diabetes. The lifetime incidence of foot ulcers among patients with diabetes could be as high as 25%. There is strong supporting evidence for screening all patients with diabetes to identify those at risk for foot ulceration. High-risk patients could benefit from prophylactic interventions, such as patient education and prescription footwear (29).
Less than 10% of respondents reported receiving an influenza vaccine during the previous year, and only 1.4% said being vaccinated against pneumococcal infection during the last five years. Reasons for low utilization of vaccines among patients could be improper knowledge (30), lack of vaccine recommendations by physicians, mistrust of vaccine safety, inconvenience of vaccination procedure, supply, and accessibility (31).
Neglecting optimal long-term diabetes management can result in a higher prevalence of diabetes complications, reducing the patient’s quality of life and increasing healthcare expenditure. So far, there has been suboptimal diabetes management in the country, as reflected in poor glycemic control (32). Nevertheless, the issue is not specific to Iran, as less than 10% of patients with diabetes in low-income and middle-income countries receive guideline-based comprehensive diabetes treatment (33). Even in countries with well-established economies like the US, improving diabetes control at the national level is a new challenge (34). Part of this challenge is justified by the complicated nature of the patient-provider relationship in setting diabetes control goals when a patient visits the physician (35).
These concerns about diabetes care are a call for concerted efforts toward scaling up the capacity of healthcare systems to follow a complete, integrated care model for the management of diabetes, which provides patient-centered, holistic, and continuous healthcare services for patients with diabetes. Holistic approaches towards diabetes management could consist of multidisciplinary teams (36), close follow-ups (37), regular home visits (38), and medication review (39). Education should become an integral part of diabetes management to empower patients to take control of their disease. Telehealth technology could be utilized for continuous disease monitoring, delivering education materials, and lifestyle promotion as a novel approach. In particular, access to telehealth in addition to in-person visits can promote access to and use of diabetes care and consequently improve health outcomes and quality of life for people with diabetes (40).
The Middle East and North Africa (MENA) region is estimated to have the second-highest global growth rate in the number of affected individuals with diabetes (41). Since 2004, the National Program for Prevention and Control of Diabetes (NPPCD) of Iran has made endeavors toward diabetes prevention and sustained care for patients with diabetes (42, 43). Despite adequate access to core medications for diabetes care, significant heterogeneity remains in comprehensive diabetes management, especially in glycemic control and complications management (44). While 81% of cities in Iran could cover essential diabetes services, 19% could not provide even the lowest coverage level (45). Without a national system for integrated diabetes control, researchers have attempted to provide quality and cost measures of diabetes care with mostly indirect estimations (46–48).
Strengths and limitations
This study presented a patient-centered disease-specific collection of insights on healthcare utilization, quality, and costs of diabetes in Iran. In developing countries, where integrated health record systems do not exist, such surveys usually consist of small samples from limited geographic areas. However, this study delivers information collected from a diverse geographic area of the country using a model-based clustering method to represent the country. The study’s follow-up modules confirmed the self-reported costs with the medical bills. Nevertheless, the small sample of this demonstration study hindered sound subgroup analyses statistically. While self-reports of service utilization and care quality guarantee the patient-centeredness nature of the responses, self-reports always suffer from various biases, such as recall. This study had a small but representative sample from the entire country. It successfully provided a frame of action and a methodological blueprint for a more extensive national-level study of the exact nature with a larger sample in the future, both in developing and developed countries.
Conclusion
Healthcare services have focused on glycemic control, and the comprehensive management of diabetes is compromised by insufficient continuity of services for diabetes control. Medication purchases and outpatient medical services were the most utilized healthcare services among patients with diabetes. The most direct costs were medication purchases and inpatient and outpatient services. Medication purchases and inpatient and outpatient services imposed the most out-of-pocket costs.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation upon request.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Tehran University of Medical Sciences. The patients/participants provided written informed consent to participate in this study.
Author contributions
Conceptualization, SK and SSh. Data curation, FM, MM, NS, YF, SSe, FG, SRa, SK, and SSh. Formal analysis, MA-K, S-HG, NA, YF, MA, SRo, SSe, FG, and SSh. Funding acquisition, SSh. Investigation, MA-K, YF, SSe, NR, SK, and SSh. Methodology, FM, YF, MA, SSe, NR, SK, and SSh. Project administration, FM, YF, SSe, NR, and SSh. Resources, NR and SSh. Software, YF, MA, HZ, MKh, and FG. Supervision, YF, NR, and SSh. Validation, YF, NR, SK, and SSh. Writing – original draft preparation, MA-K, S-HG, and SSh. Writing – review and editing, MA-K, FM, S-HG, MM, NS, NA, YF, MA, SRo, HZ, MKh, SSe, MKe, FG, SRa, NR, SK, and SSh. All authors contributed to the article and approved the submitted version.
Funding
IQCAMP project was supported by Iran National Institute for Medical Research Development (NIMAD), grant number 942936. The funding body had no role in the study's design, analysis, and interpretation of data or in writing the manuscript.
Acknowledgments
The authors sincerely thank IQCAMP diabetes module interviewers Kobra Alizadeh, Massoumeh Bahrami, Fatemeh Fayazi, Fereshteh Ganji, Aemmeh Hafezi, Azita Homayounfar, Iraj Maleki, Alireza Moezzadeh, Sepideh Nouri, Amir Sadeghi, Narges Shafiei, and Fatemeh Ramezani.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Abbafati C, Machado DB, Cislaghi B, Salman OM, Karanikolos M, McKee M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
2. Chen H, Chen G, Zheng X, Guo Y. Contribution of specific diseases and injuries to changes in health adjusted life expectancy in 187 countries from 1990 to 2013: Retrospective observational study. BMJ (2019) 364:l969. doi: 10.1136/bmj.l969
3. Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract (2018) 138:271–81. doi: 10.1016/j.diabres.2018.02.023
4. Khamseh ME, Sepanlou SG, Hashemi-Madani N, Joukar F, Mehrparvar AH, Faramarzi E, et al. Nationwide prevalence of diabetes and prediabetes and associated risk factors among Iranian adults: Analysis of data from PERSIAN cohort study. Diabetes Ther (2021) 12:2921–38. doi: 10.1007/S13300-021-01152-5/FIGURES/4
5. Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci Rep (2020) 10:1. 2020. doi: 10.1038/s41598-020-71908-9
6. Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol (2017) 5:423–30. doi: 10.1016/S2213-8587(17)30097-9
7. Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besançon S, et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract (2020) 162, 108072. doi: 10.1016/J.DIABRES.2020.108072
8. Jonas DE, Crotty K, Yun JDY, Middleton JC, Feltner C, Taylor-Phillips S, et al. Screening for prediabetes and type 2 diabetes: Updated evidence report and systematic review for the US preventive services task force. JAMA (2021) 326:744–60. doi: 10.1001/JAMA.2021.10403
9. Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, et al. The lancet commission on diabetes: Using data to transform diabetes care and patient lives. Lancet (2020) 396:2019–82. doi: 10.1016/S0140-6736(20)32374-6/ATTACHMENT/FDEC3A23-5EA1-4A0B-925E-D734AEF80FAD/MMC1.PDF
10. Manne-Goehler J, Geldsetzer P, Agoudavi K, Andall-Brereton G, Aryal KK, Bicaba BW, et al. Health system performance for people with diabetes in 28 low- and middle-income countries: A cross-sectional study of nationally representative surveys. PloS Med (2019) 16(3): e1002751. doi: 10.1371/JOURNAL.PMED.1002751
11. Flood D, Hane J, Dunn M, Brown SJ, Wagenaar BH, Rogers EA, et al. Health system interventions for adults with type 2 diabetes in low- and middle-income countries: A systematic review and meta-analysis. PloS Med (2020) 17:e1003434. doi: 10.1371/JOURNAL.PMED.1003434
12. Parsaeian M, Mahdavi M, Saadati M, Mehdipour P, Sheidaei A, Khatibzadeh S, et al. Introducing an efficient sampling method for national surveys with limited sample sizes: Application to a national study to determine quality and cost of healthcare. BMC Public Health (2020) 21(1):1414. doi: 1186/s12889-021-11441-0
13. Goldenberg R, Punthakee Z. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes (2013) 37 Suppl 1:S8–11. doi: 10.1016/J.JCJD.2013.01.011
14. Djalalinia S, Modirian M, Sheidaei A, Yoosefi M, Zokaiee H, Damirchilu B, et al. Protocol design for Large-scale cross-sectional studies of surveillance of risk factors of non-communicable diseases in Iran: STEPs 2016. Arch Iranian Med (2017) 20:608–16.
16. NQF: Measures, reports & tools. [cited 23 Mar 2021]. Available at: https://www.qualityforum.org/Measures_Reports_Tools.aspx.
17. PPP Conversion factor, GDP (LCU per international $). Iran: Islamic Rep. [cited 13 Jan 2023]. Available at: https://data.worldbank.org/indicator/PA.NUS.PPP?locations=IR.
18. Volume 46 Issue Supplement_1 | Diabetes Care | American Diabetes Association. [cited 30 Dec 2022]. Available at: https://diabetesjournals.org/care/issue/46/Supplement_1.
19. Moucheraud C, Lenz C, Latkovic M, Wirtz VJ. The costs of diabetes treatment in low- and middle-income countries: A systematic review. BMJ Global Health (2019) 4:e001258. doi: 10.1136/BMJGH-2018-001258
20. Khorrami P, Sinha MS, Bhanja A, Allen HL, Kesselheim AS, Sommers BD. Differences in diabetic prescription drug utilization and costs among patients with diabetes enrolled in Colorado marketplace and Medicaid plans, 2014-2015. JAMA Network Open (2022) 5:e2140371–e2140371. doi: 10.1001/JAMANETWORKOPEN.2021.40371
21. Nguyen DL, DeJesus RS. Home health care may improve diabetic outcomes among non-English speaking patients in primary care practice: A pilot study. J Immigr Minor Health (2011) 13:967–9. doi: 10.1007/s10903-011-9446-9
22. Siavashi E, Kavosi Z, Zand F, Amini M, Bordbar N. Inappropriate hospital stays and association with lack of homecare services. East Mediterr Health J (2021) 27:656–64. doi: 10.26719/2021.27.7.656
23. Alwafi H, Alsharif AA, Wei L, Langan D, Naser AY, Mongkhon P, et al. Incidence and prevalence of hypoglycaemia in type 1 and type 2 diabetes individuals: A systematic review and meta-analysis. Diabetes Res Clin Practice (2020) 170:108522. doi: 10.1016/J.DIABRES.2020.108522
24. Cryer PE. Minimizing hypoglycemia in diabetes. Diabetes Care (2015) 38:1583–91. doi: 10.2337/DC15-0279
25. Hu Y, Wen X, Wang F, Yang D, Liu S, Li P, et al. Effect of telemedicine intervention on hypoglycaemia in diabetes patients: A systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare (2019) 25:402–13. doi: 10.1177/1357633X18776823
26. Lean ME, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet (2018) 391:541–51. doi: 10.1016/S0140-6736(17)33102-1
27. Norris SL, Zhang X, Avenell A, Gregg E, Bowman B, Serdula M, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: A meta-analysis. Am J Med (2004) 117:762–74. doi: 10.1016/J.AMJMED.2004.05.024
28. Hall KD, Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clinics North Am (2018) 102:183. doi: 10.1016/J.MCNA.2017.08.012
29. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA (2005) 293:217–28. doi: 10.1001/JAMA.293.2.217
30. Ye C, Zhu W, Yu J, Li Z, Hu W, Hao L, et al. Low coverage rate and awareness of influenza vaccine among older people in shanghai, China: A cross-sectional study. Hum Vaccines Immunotherapeutics (2018) 14:2715–21. doi: 10.1080/21645515.2018.1491246
31. Wang Y, Cheng M, Wang S, Wu F, Yan Q, Yang Q, et al. Vaccination coverage with the pneumococcal and influenza vaccine among persons with chronic diseases in shanghai, China, 2017. BMC Public Health (2020) 20:1–9. doi: 10.1186/s12889-020-8388-3
32. Mohseni M, Shams Ghoreishi T, Houshmandi S, Moosavi A, Azami-Aghdash S, Asgarlou Z. Challenges of managing diabetes in Iran: Meta-synthesis of qualitative studies. BMC Health Serv Res (2020) 20:1–12. doi: 10.1186/S12913-020-05130-8/TABLES/2
33. Flood D, Seiglie JA, Dunn M, Tschida S, Theilmann M, Marcus ME, et al. The state of diabetes treatment coverage in 55 low-income and middle-income countries: A cross-sectional study of nationally representative, individual-level data in 680 102 adults. Lancet Healthy Longevity (2021) 2:e340–51. doi: 10.1016/S2666-7568(21)00089-1/ATTACHMENT/F1685BFF-70C4-422D-B5F0-A89DA88C80F2/MMC1.PDF
34. Shahraz S, Pittas AG, Saadati M, Thomas CP, Lundquist CM, Kent DM. Change in testing, awareness of hemoglobin A1c result, and glycemic control in US adults, 2007-2014. JAMA (2017) 318:1825–7. doi: 10.1001/JAMA.2017.11927
35. Shahraz S, Pittas AG, Lundquist CM, Danaei G, Kent DM. Do patient characteristics impact decisions by clinicians on hemoglobin A1c targets? Diabetes Care (2016) 39:e145–6. doi: 10.2337/DC16-0532
36. McGill M, Blonde L, Chan JCN, Khunti K, Lavalle FJ, Bailey CJ. The interdisciplinary team in type 2 diabetes management: Challenges and best practice solutions from real-world scenarios. J Clin Trans Endocrinol (2017) 7:21. doi: 10.1016/J.JCTE.2016.12.001
37. Al-Hamarneh YN, Sauriol L, Tsuyuki RT. After the diabetes care trial ends, now what? A 1-year follow-up of the RxING study. BMJ Open (2015) 5:e008152. doi: 10.1136/BMJOPEN-2015-008152
38. Han L, Ma Y, Wei S, Tian J, Yang X, Shen X, et al. Are home visits an effective method for diabetes management? A quantitative systematic review and meta-analysis. J Diabetes Invest (2017) 8:701. doi: 10.1111/JDI.12630
39. Schindler E, Hohmann C, Culmsee C. Medication review by community pharmacists for type 2 diabetes patients in routine care: Results of the DIATHEM-study. Front Pharmacol (2020) 11:1176. doi: 10.3389/FPHAR.2020.01176
40. Hood KK, Wong JJ. Telehealth for people with diabetes: Poised for a new approach. Lancet Diabetes Endocrinol (2022) 10:8–10. doi: 10.1016/S2213-8587(21)00312-0
41. Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Practice (2014) 103:137–49. doi: 10.1016/j.diabres.2013.11.002
42. Farzadfar F, Murray CJL, Gakidou E, Bossert T, Namdaritabar H, Alikhani S, et al. Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: A nationally representative observational study. Lancet (2012) 379:47–54. doi: 10.1016/S0140-6736(11)61349-4
43. Noshad S, Afarideh M, Heidari B, Mechanick JI, Esteghamati A. Diabetes care in Iran: Where we stand and where we are headed. Ann Global Health (2014) 81:839–50. doi: 10.1016/j.aogh.2015.10.003
44. Esteghamati A, Larijani B, Aghajani MH, Ghaemi F, Kermanchi J, Shahrami A, et al. Diabetes in Iran: Prospective analysis from first nationwide diabetes report of national program for prevention and control of diabetes (NPPCD-2016). Sci Rep (2017) 7(1):13461. doi: 10.1038/s41598-017-13379-z
45. Sharifi A, Farzi Y, Roshani S, Ghamari A, Tabatabaei-Malazy O, Djalalinia S, et al. A new model for optimization of diabetes clinics with the case study in Iran. J Diabetes Metab Disord (2022) 21:817–22. doi: 10.1007/s40200-021-00939-4
46. Javanbakht M, Baradaran HR, Mashayekhi A, Haghdoost AA, Khamseh ME, Kharazmi E, et al. Cost-of-illness analysis of type 2 diabetes mellitus in Iran. PloS One (2011) 6(10):e26864. doi: 10.1371/JOURNAL.PONE.0026864
47. Javanbakht M, Abolhasani F, Mashayekhi A, Baradaran HR, Jahangiri noudeh Y. Health related quality of life in patients with type 2 diabetes mellitus in Iran: a national survey. PloS One (2012) 7(8):e44526. doi: 10.1371/JOURNAL.PONE.0044526
Keywords: patient care continuity, diabetes mellitus, healthcare utilization, patient journey, care quality, care standard
Citation: Abbasi-Kangevari M, Mohebi F, Ghamari S-H, Modirian M, Shahbal N, Ahmadi N, Farzi Y, Azmin M, Roshani S, Zokaei H, Khezrian M, Seyfi S, Keykhaei M, Gorgani F, Rahimi S, Rezaei N, Khatibzadeh S and Shahraz S (2023) Quality and cost of healthcare services in patients with diabetes in Iran: Results of a nationwide short-term longitudinal survey. Front. Endocrinol. 14:1099464. doi: 10.3389/fendo.2023.1099464
Received: 15 November 2022; Accepted: 14 February 2023;
Published: 16 March 2023.
Edited by:
Åke Sjöholm, Gävle Hospital, SwedenReviewed by:
Sudhanshu Kumar Bharti, Patna University, IndiaMansoureh Karimollahi, Ardabil University of Medical Sciences, Iran
Copyright © 2023 Abbasi-Kangevari, Mohebi, Ghamari, Modirian, Shahbal, Ahmadi, Farzi, Azmin, Roshani, Zokaei, Khezrian, Seyfi, Keykhaei, Gorgani, Rahimi, Rezaei, Khatibzadeh and Shahraz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohsen Abbasi-Kangevari, bW9oc2VuLmFiYmFzaUBzYm11LmFjLmly
†These authors share first authorship
 Mohsen Abbasi-Kangevari
Mohsen Abbasi-Kangevari Farnam Mohebi
Farnam Mohebi Seyyed-Hadi Ghamari
Seyyed-Hadi Ghamari Mitra Modirian
Mitra Modirian Nazila Shahbal1
Nazila Shahbal1 Shahin Roshani
Shahin Roshani Mohammad Keykhaei
Mohammad Keykhaei Saral Rahimi
Saral Rahimi Negar Rezaei
Negar Rezaei Shahab Khatibzadeh
Shahab Khatibzadeh Saeid Shahraz
Saeid Shahraz