- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Chungbuk National University College of Medicine and Chungbuk National University Hospital, Cheongju, Republic of Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Republic of Korea
- 3Department of Epidemiology and Health Informatics, Korea University, Seoul, Republic of Korea
- 4Department of Biochemistry, Chungbuk National University College of Medicine, Cheongju, Republic of Korea
- 5Division of Pulmonary and Allergy, Department of Internal Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Republic of Korea
- 6Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Republic of Korea
- 7Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Republic of Korea
- 8Department of Internal Medicine, Chonbuk National University Hospital-Chonbuk National University Medical School, Jeonju, Republic of Korea
- 9Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Republic of Korea
Background: Subjects with diabetes are at higher risk of serious influenza-related complications. We aimed to investigate the yearly trend of influenza vaccination and factors associated with being unvaccinated for influenza in subjects with diabetes using a nationwide observational study performed within the recent decade.
Methods: Among 105,732 subjects from the Korea National Health and Nutrition Examination Survey between 2007 and 2019, 8,632 with diabetes were included. We investigated the yearly trend of influenza vaccination and factors associated with being unvaccinated for influenza.
Results: During the study period, the prevalence of influenza vaccination in subjects with diabetes showed a tendency to increase every year, reaching almost 60% in 2019, which was higher than the rate in subjects without diabetes. Younger age (adjusted hazard ratio (aHR) [95% CI] 11.29 [8.63–14.75] for < 50 years; 6.16 [5.21–7.29] for 50–65 years), male (aHR 1.67 [1.52–1.87]), current smoker (aHR 1.31 [1.00–1.72], lower-income status (aHR 1.46 [1.17, 1.84]), and high education level (aHR 1.30 [1.01–1.67]) were associated with being unvaccinated. Also, a poorer glycemic control with HbA1c ≥ 9% was found to be correlated with unvaccinated status (aHR 1.48 [1.15–1.90]).
Conclusion: The influenza vaccination rate is still unsatisfactory in subjects with diabetes. Young age, males, low-income level, high education level, and poor glycemic control were associated with unvaccinated status. Considering the risk-benefits of influenza vaccination in patients with diabetes, physicians should make an effort to increase vaccination rates, especially in low vaccination rate groups.
1 Introduction
Diabetes is a common metabolic disorder affecting the entire body (1). It is one of the top 10 causes leading to mortality and is responsible for over 55.4 million deaths/year worldwide (2). Diabetes increases the susceptibility of infections and worsens their treatment outcomes (3, 4). Of various infections, respiratory infections have been shown to impose a substantially increased risk of morbidity and mortality on subjects with diabetes (5, 6). Thus, preventing respiratory infection in subjects with diabetes would be important to improve the treatment outcomes of diabetes.
Influenza is one of the commonly identified respiratory viruses (7). Influenza can cause serious illness in people with certain underlying chronic conditions including diabetes (8, 9). For example, diabetes triples the risk of influenza-related hospitalization, quadruples the risk of admission to an intensive care unit, and doubles the risk of fatal outcomes (10, 11). Accordingly, subjects with diabetes are strongly recommended to be vaccinated for influenza (12, 13). The significant benefits of influenza vaccination have been well demonstrated in its efficacy to reduce complications, hospitalizations, and death in subjects with diabetes (11, 14).
Information about coverage of influenza vaccination and factors affecting vaccination would be helpful to make health policy to enhance influenza vaccination in subjects with diabetes. However, despite the importance of influenza vaccination in subjects with diabetes (11, 15), few studies addressed this important issue. Hence, we aimed to investigate the yearly trend of influenza vaccination and factors associated with being unvaccinated for influenza in subjects with diabetes using a nationwide observational study performed within the recent decade.
2 Methods
2.1 Study population
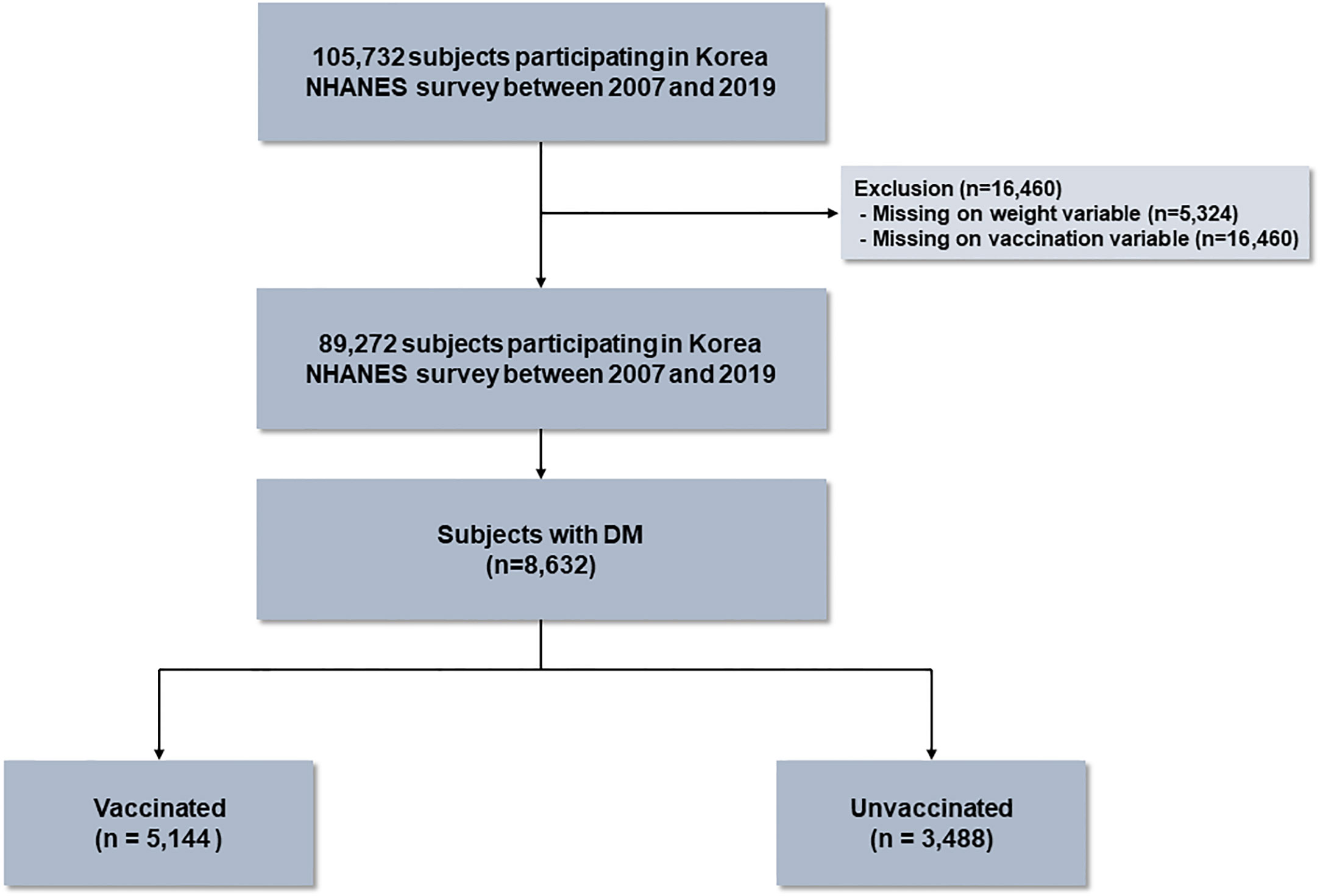
The Korea National Health and Nutritional Survey (NHANES) is a population-based nationwide survey to assess the health and nutritional status of the noninstitutionalized population of Korea, and conducted by Korea Disease Control and Prevention (KCDC). We used data from the Korea NHANES IV (2007–2009), V (2010–2012), VI (2014–2015), VII (2016-2018), and VIII (2019). The data from Korea NHANES V (2013) was excluded because the vaccination data was not available. The study population was investigated based on a stratified multi-stage sampling method. During the 13 years, there were 105,732 participants. Of these, participants with missing on survey weight variable (n = 5,324) or vaccination variable (n = 16,460) were excluded, and 89,272 subjects were included in this study. Of the eligible participants, 8,632 (9.7%) subjects had diabetes, who were classified into two groups based on influenza vaccination status: vaccinated (n = 5,144) and unvaccinated (n = 3,488) (Figure 1). The study protocol was approved by the Institutional Review Board of Chungbuk National University Hospital (application no.2022-03-003).
2.2 Exposure: Diabetes
The main exposure of this study was diabetes. Diabetes was defined as any presence of the following criteria: 1) history of physician-diagnosis of diabetes. 2) fasting glucose level ≥ 126 mg/dL, 3) hemoglobin A1c (HbA1c) ≥ 6.5% (16), or 4) participants who reported taking oral hypoglycemic agents or administering insulin were classified as having diabetes (17).
2.3 Outcomes: Influenza vaccination
The main outcomes of our study were to evaluate the trend of influenza vaccination and to explore factors associated with influenza vaccination in patients with diabetes. Influenza vaccination was investigated using the following question: “Have you ever been vaccinated against influenza in the past year?”
2.4 Measurements
Available data on age, sex, body mass index (BMI), smoking history, marital status, income, education, respiratory symptom physical activity, and the EuroQoL five dimensions questionnaire (EQ-5D) index values were obtained from the Korea NHANES database. Regular walking was defined as a person who walked at least five times a week for more than 30 minutes at a time. The EQ-5D index values, used to measure the quality of life, range between 0 (worst imaginable health state) and 1 (best imaginable health state). Comorbidities of pulmonary tuberculosis, cardiovascular disease including myocardial infarction or angina, stroke, and chronic kidney disease were self-reported based on previous physician diagnosis (18, 19). Hypertension was defined as a self-reported physician diagnosis, the use of antihypertensive medication, a systolic blood pressure ≥ 140 mmHg, or a diastolic blood pressure ≥ 90 mmHg (20, 21). Dyslipidemia was defined as a self-reported physician diagnosis, the use of lipid-lowering medication, total cholesterol ≥ 240 mg/dL, or fasting triglyceride ≥ 200 mg/dL (19, 21). The data of HbA1c was obtained from a general health examination.
2.5 Statistical analysis
All analysis was performed using survey commands in STATA 15.1 version (StataCorp LP, College Station, TX, USA) to account for the complex sampling design and survey weights. All data are presented as a weighted percentage with standard errors (SE). The data were compared using Student’s t-test for continuous and Pearson’s χ2 test for categorical variables. To evaluate factors associated with influenza vaccination status in patients with diabetes, both univariable and multivariable logistic regression analyses were performed. Multivariable analysis was adjusted for age, sex, BMI, smoking status, marital status, income, regular walking, respiratory symptoms, physical limitation, EQ-5D, HbA1c and comorbidities (pulmonary tuberculosis, hypertension, dyslipidemia, chronic kidney disease, cardiovascular disease, and stroke). All tests were two-sided, and p-values < 0.05 were considered statistically significant differences.
3 Results
3.1 Baseline characteristics
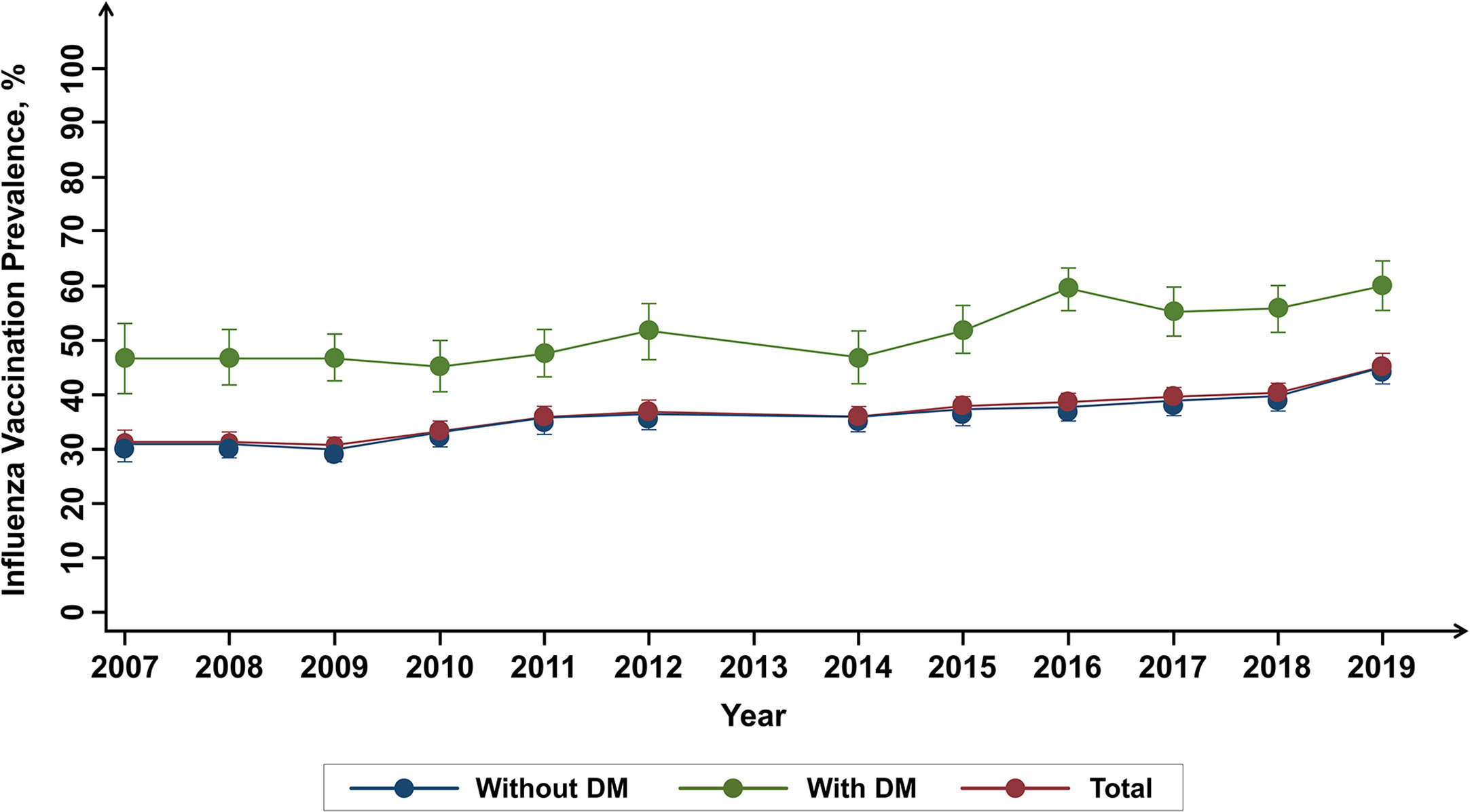
The baseline characteristics of the study population are presented in Table 1. Of 8,632 participants, about 60% of participants were vaccinated (vaccinated group) and 40% were unvaccinated (unvaccinated group). Compared with vaccinated group, unvaccinated group was younger (mean 53.2 years vs. 65.2 years), had a lower proportion of female (36.7 vs. 53.5%), and a higher proportion of overweight or obesity (52.9 vs. 49.4%) and current smoker (31.5 vs. 16.3%) (P < 0.001 for all variables). Fasting plasma glucose and HbA1c levels were significantly higher in unvaccinated group compared with vaccinated group (148.9 vs. 137.3 mg/dL and 7.4 vs. 7.1%, respectively) (P < 0.001 for both). Regarding comorbidities, vaccinated group had a higher proportion of hypertension (67.6 vs. 51.0%), cardiovascular disease (8.3 vs. 3.9%), stroke (6.9 vs. 3.5%), and chronic kidney disease (15.6 vs. 5.8%) compared with unvaccinated group (P < 0.001 for all). The proportion of individuals with dyslipidemia was similar in both groups (77.0 vs. 78.0%, P = 0.392).
3.2 Influenza vaccination trend
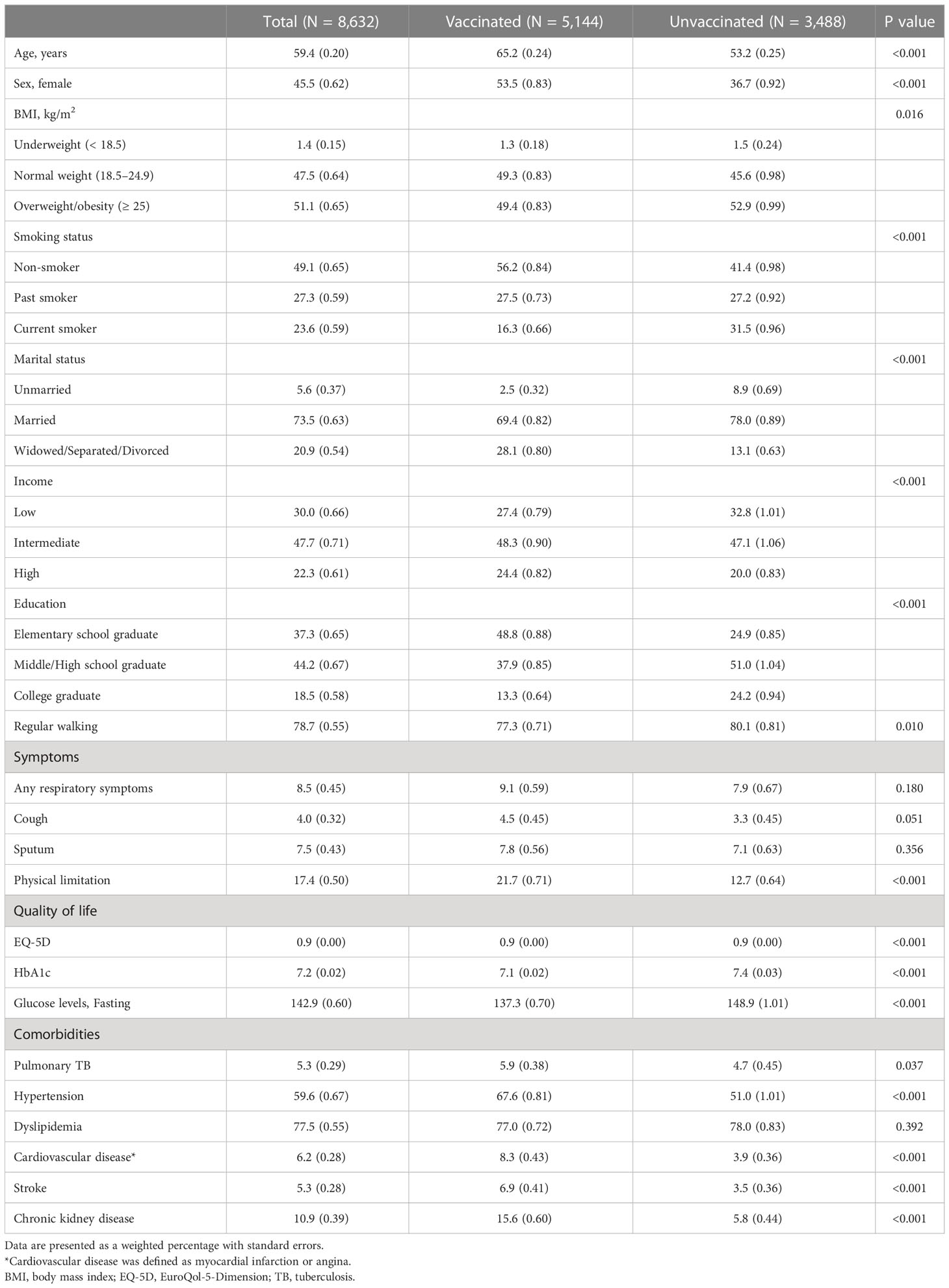
The 13-year trend of influenza vaccination according to diabetes is summarized in Figure 2. Regardless of diabetes, increasing tendency was observed (from 30.9% in 2007 to 45.8% in 2019 for total population; from 46.54% in 2007 to 59.9% in 2019 for participant with diabetes; from 29.8% in 2007 to 44.1% in 2019 for participants without diabetes). Individuals with diabetes showed a significantly higher prevalence of influenza vaccination compared to those without diabetes (P < 0.001).
3.3 Prevalence of influenza vaccination according to age, sex, and smoking status in participants with diabetes
Comparison of prevalence of influenza vaccination according to clinical characteristics in patients with diabetes is shown in Figure 3. Subjects with age between 50 and 65 showed the highest prevalence, and those under 50 noted the lowest prevalence of vaccination. Male patients were a higher rate of vaccination than females. Regarding smoking status, the vaccination rate tended to decrease in the order of non-smoker, past smoker, and current smoker.
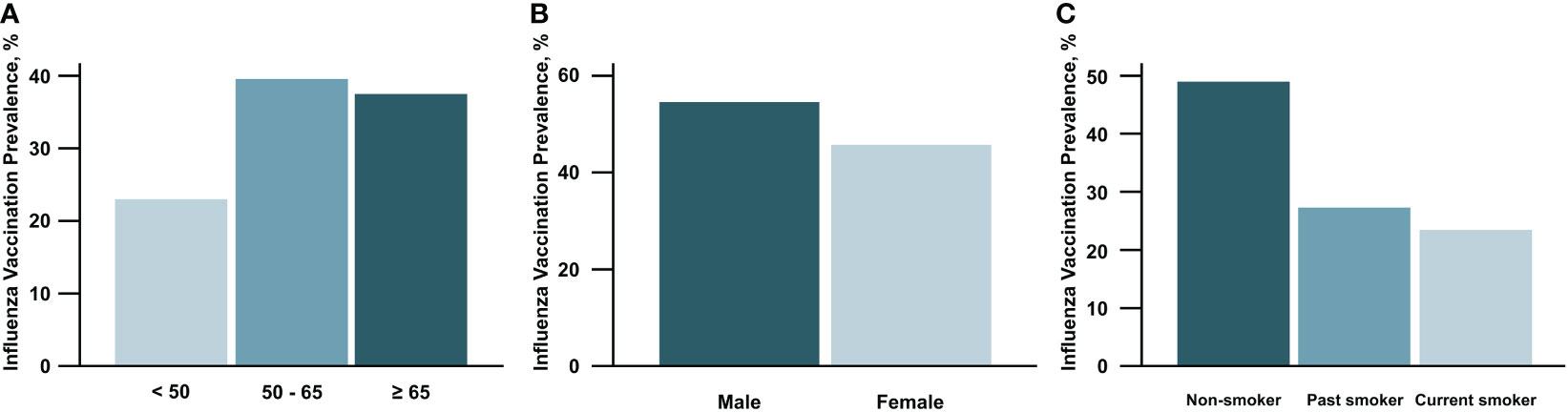
Figure 3 Prevalence of influenza vaccination according to age (A), sex (B), and smoking status (C) in participants with diabetes mellitus.
3.4 Prevalence of influenza vaccination according to glycemic control in participants with diabetes
Figure 4 summarizes the prevalence of influenza vaccination according to glycemic control in patients with diabetes. Relatively higher prevalence was observed in patients with HbA1c between 6.0% and 7.5%. The patients with HbA1c ≥ 9% showed the lowest prevalence of influenza vaccination (P < 0.001).
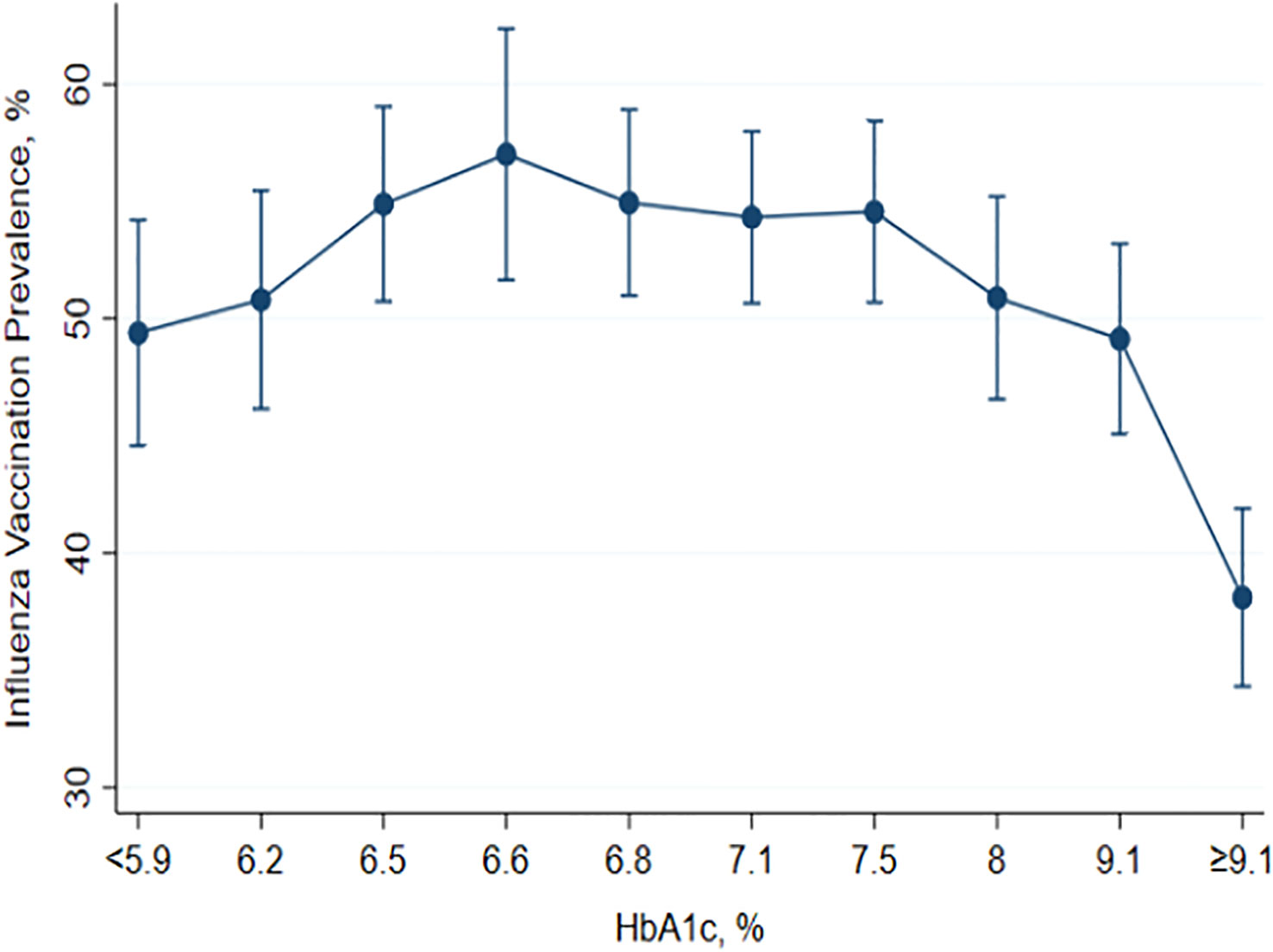
Figure 4 Prevalence of influenza vaccination according to glycemic control in participants with diabetes mellitus.
3.5 Factors associated with influenza unvaccinated status
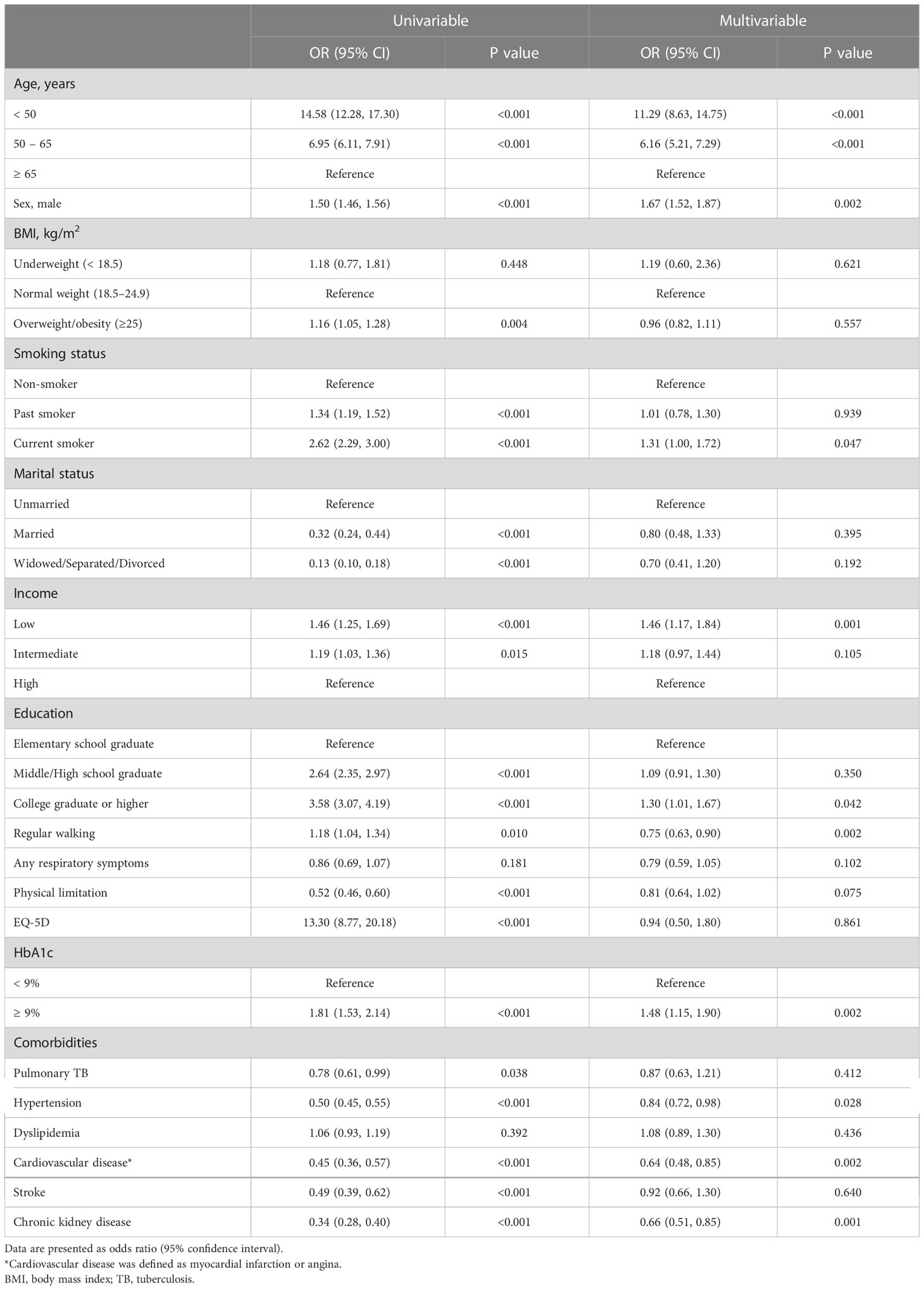
To evaluate the factors associated with influenza vaccination status, a multivariable logistic regression analysis was performed (Table 2). Younger age was found to be associated with influenza unvaccinated status (adjusted hazard ratio (aHR) [95% CI] for age 11.29 [8.63–14.75] for < 50 years; 6.16 [5.21–7.29] for 50–65 years). Male (aHR 1.67 [1.52–1.87]), current smoker (aHR 1.31 [1.00–1.72]), and lower-income status (aHR 1.46 [1.17–1.84]) showed a significant association with unvaccinated status. A poorer glycemic control with HbA1c ≥ 9% was found to be correlated with unvaccinated status (aHR 1.48 [1.15–1.90]). In contrast, a higher education level (aHR 1.30 [1.01–1.67] for college graduate or higher) and comorbidities such as hypertension (aHR 0.84 [0.72–0.98]), cardiovascular disease (aHR 0.64 [0.48–0.85]), and chronic kidney disease (aHR 0.66 [0.51– 0.85]) showed a negative association with unvaccinated status.
4 Discussion
As a result of analyzing the prevalence of influenza vaccination for 13 years in participants with diabetes using data from Korea NHANES, the vaccination rate showed a tendency to increase every year, reaching almost 60% in 2019, which was higher than the rate in participants without diabetes. However, vaccination rates were significantly lower in certain groups of younger age, male sex, current smokers, low income-level, and high education level. Notably, poorer glycemic control (HbA1c ≥ 9%) showed a significant association with unvaccinated status.
It is well-known that diabetes is a risk factor for higher susceptibility to bacterial, viral, or fungal infection (22). Furthermore, patients with diabetes showed poor infection outcomes such as hospitalization and mortality (23, 24). Influenza is one of the most common respiratory viruses resulting in annual epidemics. Influenza infection causes substantial mortality in some subjects, especially in elderly or chronic diseases such as diabetes (6). Previous studies have shown that patients with diabetes have higher infection-related morbidity and mortality during influenza infection than those without diabetes (22, 25). In another study, a higher risk of admission to the intensive care unit was observed in patients with diabetes during the influenza pandemic (10). Therefore, several guidelines including American Diabetic Association, the European Association for the Study of Diabetes, and Korean Diabetes Association recommend that patients with diabetes ≥ 6 months of age who do not have a contraindication should receive the influenza vaccination annually (13, 26, 27).
As shown in the previous studies, our study showed that influenza vaccination rate is higher in subjects with diabetes compared with those without diabetes (28). Extending the previous findings, our study provided a long-term trend of vaccination rates in patients with diabetes. Although the prevalence of vaccination rate steadily increased during the observation period, the most recent rate of vaccination (2019) in patients with diabetes was 59.8%, suggesting there is still unmet need to increase influenza vaccination rate in this population. The World Health Organization (WHO) recommends a vaccination coverage rate of at least 75% in the vulnerable population for effective prevention against influenza (29). From this view, the clinical relevance of our study is that we revealed various factors associated with unvaccinated status, which might be helpful for physicians and health policy managers to make some enhanced strategies to increase vaccination rate in subjects with diabetes.
Our study showed younger age, male sex, current smoker, low-income status, and high education level showed significant factors affecting vaccination. Some previous studies evaluated the association between clinical characteristics and influenza vaccination coverage in patients with diabetes. In a study performed in the United States, a low vaccination rate was reported in some vulnerable sociodemographic groups such as younger adults (18−64 years), non-Hispanic Black adults, individuals without insurance, those from low-income families, and individuals lacking access to usual care (30). Another study conducted in Thailand also showed similar results: a different vaccination rate was shown according to age, sex, and comorbidities (31). Other studies in Korea reported that age and economic activity were associated with influenza vaccination (2, 28). Our findings are consistent with recent studies that decrease in vaccine coverage rates are related to young age and lower-income levels. Besides these factors, our study showed that males and current smokers are important factors associated with unvaccinated status. Considering that these two factors are significant predictors of poor outcomes of influenza (32, 33), substantial efforts are needed to increase influenza vaccination rate in these groups. Considering that education levels are generally correlated with income levels, it is very interesting that high education level was associated with unvaccinated status in patients with diabetes. Previous studies have consistently demonstrated similar results (34–36). The results from a recent study conducted in Korea also showed that a lower education level was associated with higher influenza vaccination coverage (37). It might be that people with low education levels have the need for preventive management because they have more possibility to work in fields that require more physical activities and less social support. This may partly explain the reasons for the results seen in our study. Since the reasons why high education levels are associated with low vaccination rates are still unclear, future studies are needed to improve the vaccination rate in this subpopulation.
For the first time to the best of our knowledge, it is noteworthy that our study analyzed the prevalence of influenza vaccination according to glycemic control in patients with diabetes. Although not fully elucidated, several factors have been suggested to explain the underlying mechanisms of increased risk of infection in patients with diabetes. Chronic inflammatory conditions associated with obesity, hyperlipidemia, and insulin resistance in diabetes are thought to be relevant (38, 39). Moreover, it is well-known that poor glycemic control was associated with an increased risk of infection-related morbidity and mortality in patients with diabetes (40, 41). Thus, influenza vaccination would be more important in patients with poor glycemic control. However, in our study, the patients with poor glycemic control, referred to as higher HbA1c, showed lower vaccination rates. Since our study is observational, the reason for this phenomenon is not fully explainable. We carefully suggest that low compliance to medical advice, often found in patients with poor glycemic control, might be an explanation for the lower vaccination rate in this population.
During the COVID-19 pandemic, a pattern of decreased influenza transmission has been observed worldwide. However, as social distancing relaxes and people do not wear face masks, the transmission of both influenza and COVID-19 can be expected to increase (42). Accordingly, increasing influenza and COVID-19 vaccinations carry heightened importance to minimize the tremendously harmful effects of these viruses on patients with diabetes.
One of the strengths of this study is the inclusion of a large population in the analysis because of the use of Korea NHANES data, which were taken from a nationwide survey sample showing a high response rate. In addition, the investigation was focused on glycemic control, which is an important factor in patients with diabetes. However, there are some limitations to this study. First, we did not classify type of diabetes due to the absence of information in Korea NHNES. Since Korea NHANES is a representative study designed to select samples that can represent the overall Korean population, both type 1 and type 2 diabetes subjects are thought to be enrolled in this study. However, since the prevalence of type 1 diabetes is very low (< 0.1%) in Korea (43), most of our study subjects are thought to have type 2 diabetes. Second, the potential recall bias might have affected our results because of self-reported influenza vaccination information in this database, which may underestimate or overestimate the true prevalence of influenza vaccination. Third, it is challenging to validate the causality due to cross-sectional data. Fourth, the influenza vaccination policies may differ by country. For example, in Korea, free influenza vaccination has been provided for all subjects aged 65 or older since 2005. Thus, our study results might not be applicable to other countries with different influenza vaccination policies.
In conclusion, the influenza vaccination rate is low in subjects with diabetes who are younger, males, have low-income levels, have high education levels, and those with poor glycemic control. Considering the risk-benefits of influenza vaccination in patients with diabetes, physicians should recognize the importance of immunization in diabetes and effort to increase vaccination rates in patients with diabetes, especially in low vaccination rate groups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by The study protocol was approved by the Institutional Review Board of Chungbuk National University Hospital (application no.2022-03-003). The ethics committee waived the requirement of written informed consent for participation
Author contributions
Conception or design: HL and SP. Acquisition, analysis, or interpretation of data: BY and SG. Drafting the work or revising: D-HL, BY, SP, and HL. Final approval of the manuscript: D-HL, BY, SG, E-GK, YK, HK, YC, HJ, and SP and HL. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the research grant of the Chungbuk National University in 2022. Also, this work was supported by grants from the National Research Foundation of Korea (2020R1A5A2017476). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Demir S, Nawroth PP, Herzig S, Ekim Ustunel B. Emerging targets in type 2 diabetes and diabetic complications. Adv Sci (Weinh) (2021) 8(18):e2100275. doi: 10.1002/advs.202100275
2. Han AL. Factors associated with influenza vaccine coverage among patients with diabetes: Korea national health and nutrition examination survey 2016-2018. Int J Diabetes Dev Ctries (2021) 42(2):297–304. doi: 10.1007/s13410-021-00977-x
3. Akash MSH, Rehman K, Fiayyaz F, Sabir S, Khurshid M. Diabetes-associated infections: development of antimicrobial resistance and possible treatment strategies. Arch Microbiol (2020) 202(5):953–65. doi: 10.1007/s00203-020-01818-x
4. Eguchi K, Nagai R. Islet inflammation in type 2 diabetes and physiology. J Clin Invest (2017) 127(1):14–23. doi: 10.1172/JCI88877
5. Cavallazzi R, Ramirez JA. Influenza and viral pneumonia. Clinics chest Med (2018) 39(4):703–21. doi: 10.1016/j.ccm.2018.07.005
6. Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet (2018) 391(10127):1285–300. doi: 10.1016/S0140-6736(17)33293-2
7. Lafond KE, Porter RM, Whaley MJ, Suizan Z, Ran Z, Aleem MA, et al. Global burden of influenza-associated lower respiratory tract infections and hospitalizations among adults: A systematic review and meta-analysis. PloS Med (2021) 18(3):e1003550. doi: 10.1371/journal.pmed.1003550
8. Owusu D, Rolfes MA, Arriola CS, Daily Kirley P, Alden NB, Meek J, et al. Rates of severe influenza-associated outcomes among older adults living with diabetes-influenza hospitalization surveillance network (FluSurv-NET), 2012-2017. Open Forum Infect Dis (2022) 9(5):ofac131. doi: 10.1093/ofid/ofac131
9. Al Amad M, Almoayed K. Influenza circulating viruses, positivity rate and risk factors for influenza associated severe acute respiratory infection during 2018/2019 winter season, Yemen. BMC Infect Dis (2022) 22(1):111. doi: 10.1186/s12879-022-07090-2
10. Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza a (H1N1) infection. Diabetes Care (2010) 33(7):1491–3. doi: 10.2337/dc09-2215
11. Goeijenbier M, van Sloten TT, Slobbe L, Mathieu C, van Genderen P, Beyer WEP, et al. Benefits of flu vaccination for persons with diabetes mellitus: A review. Vaccine (2017) 35(38):5095–101. doi: 10.1016/j.vaccine.2017.07.095
12. Remschmidt C, Wichmann O, Harder T. Vaccines for the prevention of seasonal influenza in patients with diabetes: systematic review and meta-analysis. BMC Med (2015) 13:53. doi: 10.1186/s12916-015-0295-6
13. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 4. comprehensive medical evaluation and assessment of comorbidities: Standards of care in diabetes-2023. Diabetes Care (2023) 46(Supplement_1):S49–67. doi: 10.2337/dc23-S004
14. Martínez-Baz I, Navascués A, Portillo ME, Casado I, Fresán U, Ezpeleta C, et al. Effect of influenza vaccination in preventing laboratory-confirmed influenza hospitalization in patients with diabetes mellitus. Clin Infect Dis (2021) 73(1):107–14. doi: 10.1093/cid/ciaa564
15. Dunne JL, Richardson SJ, Atkinson MA, Craig ME, Dahl-Jørgensen K, Flodström-Tullberg M, et al. Rationale for enteroviral vaccination and antiviral therapies in human type 1 diabetes. Diabetologia (2019) 62(5):744–53. doi: 10.1007/s00125-019-4811-7
16. American Diabetes A. 2. classification and diagnosis of diabetes: Standards of medical care in diabetes-2021. Diabetes Care (2021) 44(Suppl 1):S15–33. doi: 10.2337/dc21-S002
17. Lee DH, Jung KY, Park KS, Kim KM, Moon JH, Lim S, et al. Characterization of patients with type 2 diabetes according to body mass index: Korea national health and nutrition examination survey from 2007 to 2011. Endocrinol Metab (Seoul) (2015) 30(4):514–21. doi: 10.3803/EnM.2015.30.4.514
18. Lee H, Rhee CK, Lee BJ, Choi DC, Kim JA, Kim SH, et al. Impacts of coexisting bronchial asthma on severe exacerbations in mild-to-moderate COPD: results from a national database. Int J chronic obstructive pulmonary Dis (2016) 11:775–83. doi: 10.2147/COPD.S95954
19. Lee H, Shin SH, Gu S, Zhao D, Kang D, Joi YR, et al. Racial differences in comorbidity profile among patients with chronic obstructive pulmonary disease. BMC Med (2018) 16(1):178. doi: 10.1186/s12916-018-1159-7
20. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC). J Hypertens (2007) 25(6):1105–87. doi: 10.1097/HJH.0b013e3281fc975a
21. Yang B, Choi H, Lim JH, Park HY, Kang D, Cho J, et al. The disease burden of bronchiectasis in comparison with chronic obstructive pulmonary disease: a national database study in Korea. Ann Trans Med (2019) 7(23):770. doi: 10.21037/atm.2019.11.55
22. Knapp S. Diabetes and infection: is there a link?–a mini-review. Gerontology (2013) 59(2):99–104. doi: 10.1159/000345107
23. Kornum JB, Thomsen RW, Riis A, Lervang HH, Schonheyder HC, Sorensen HT. Diabetes, glycemic control, and risk of hospitalization with pneumonia: a population-based case-control study. Diabetes Care (2008) 31(8):1541–5. doi: 10.2337/dc08-0138
24. Magliano DJ, Harding JL, Cohen K, Huxley RR, Davis WA, Shaw JE. Excess risk of dying from infectious causes in those with type 1 and type 2 diabetes. Diabetes Care (2015) 38(7):1274–80. doi: 10.2337/dc14-2820
25. Jimenez-Garcia R, Hernandez-Barrera V, Rodriguez-Rieiro C, Lopez de Andres A, de Miguel-Diez J, Jimenez-Trujillo I, et al. Hospitalizations from pandemic influenza [A(H1N1)pdm09] infections among type 1 and 2 diabetes patients in Spain. Influenza Other Respir Viruses (2013) 7(3):439–47. doi: 10.1111/j.1750-2659.2012.00419.x
26. Hur KY, Moon MK, Park JS, Kim SK, Lee SH, Yun JS, et al. 2021 Clinical practice guidelines for diabetes mellitus of the Korean diabetes association. Diabetes Metab J (2021) 45(4):461–81. doi: 10.4093/dmj.2021.0156
27. Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of hyperglycaemia in type 2 diabetes, 2022. a consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetologia (2022) 65(12):1925–66. doi: 10.1007/s00125-022-05787-2
28. Ko YM, Ko SH, Han K, Park YM, Choi JY, Kim SY, et al. Importance of awareness and treatment for diabetes in influenza vaccination coverage of diabetic patients under 65 years: A population-based study. Diabetes Metab J (2021) 45(1):55–66. doi: 10.4093/dmj.2019.0189
29. Carrillo-Santisteve P, Ciancio BC, Nicoll A, Lopalco PL. The importance of influenza prevention for public health. Hum Vaccin Immunother (2012) 8(1):89–95. doi: 10.4161/hv.8.1.19066
30. Bhugra P, Mszar R, Valero-Elizondo J, Grandhi GR, Virani SS, Cainzos-Achirica M, et al. Prevalence of and sociodemographic disparities in influenza vaccination among adults with diabetes in the united states. J Endocr Soc (2020) 4(11):bvaa139. doi: 10.1210/jendso/bvaa139
31. Thewjitcharoen Y, Butadej S, Malidaeng A, Yenseung N, Nakasatien S, Lekpittaya N, et al. Trends in influenza and pneumococcal vaccine coverage in Thai patients with type 2 diabetes mellitus 2010-2018: Experience from a tertiary diabetes center in Bangkok. J Clin Transl Endocrinol (2020) 20:100227. doi: 10.1016/j.jcte.2020.100227
32. Al-Baadani AM, Elzein FE, Alhemyadi SA, Khan OA, Albenmousa AH, Idrees MM. Characteristics and outcome of viral pneumonia caused by influenza and middle East respiratory syndrome-coronavirus infections: A 4-year experience from a tertiary care center. Ann Thorac Med (2019) 14(3):179–85. doi: 10.4103/atm.ATM_179_18
33. Han L, Ran J, Mak YW, Suen LK, Lee PH, Peiris JSM, et al. Smoking and influenza-associated morbidity and mortality: A systematic review and meta-analysis. Epidemiology (2019) 30(3):405–17. doi: 10.1097/EDE.0000000000000984
34. Bryden GM, Browne M, Rockloff M, Unsworth C. The privilege paradox: Geographic areas with highest socio-economic advantage have the lowest rates of vaccination. Vaccine (2019) 37(32):4525–32. doi: 10.1016/j.vaccine.2019.06.060
35. Dios-Guerra C, Carmona-Torres JM, Lopez-Soto PJ, Morales-Cane I, Rodriguez-Borrego MA. Prevalence and factors associated with influenza vaccination of persons over 65 years old in Spain (2009-2014). Vaccine (2017) 35(51):7095–100. doi: 10.1016/j.vaccine.2017.10.086
36. Grandhi GR, Mszar R, Vahidy F, Valero-Elizondo J, Blankstein R, Blaha MJ, et al. Sociodemographic disparities in influenza vaccination among adults with atherosclerotic cardiovascular disease in the united states. JAMA Cardiol (2021) 6(1):87–91. doi: 10.1001/jamacardio.2020.3978
37. Seo J, Lim J. The impact of free vaccination policies under the Korean influenza national immunization program: Trends in influenza vaccination rates in south Korea from 2010 to 2019. PloS One (2022) 17(1):e0262594. doi: 10.1371/journal.pone.0262594
38. Fisher-Hoch SP, Mathews CE, McCormick JB. Obesity, diabetes and pneumonia: the menacing interface of non-communicable and infectious diseases. Trop Med Int Health (2013) 18(12):1510–9. doi: 10.1111/tmi.12206
39. Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest (2005) 115(5):1111–9. doi: 10.1172/JCI25102
40. Butler SO, Btaiche IF, Alaniz C. Relationship between hyperglycemia and infection in critically ill patients. Pharmacotherapy (2005) 25(7):963–76. doi: 10.1592/phco.2005.25.7.963
41. Critchley JA, Carey IM, Harris T, DeWilde S, Hosking FJ, Cook DG. Glycemic control and risk of infections among people with type 1 or type 2 diabetes in a Large primary care cohort study. Diabetes Care (2018) 41(10):2127–35. doi: 10.2337/dc18-0287
42. Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health (2021) 194:245–51. doi: 10.1016/j.puhe.2021.02.025
43. Song SO, Song YD, Nam JY, Park KH, Yoon JH, Son KM, et al. Epidemiology of type 1 diabetes mellitus in Korea through an investigation of the national registration project of type 1 diabetes for the reimbursement of glucometer strips with additional analyses using claims data. Diabetes Metab J (2016) 40(1):35–45. doi: 10.4093/dmj.2016.40.1.35
Keywords: diabetes mellitus, influenza, vaccination, prevalence, epidemiology
Citation: Lee D-H, Yang B, Gu S, Kim E-G, Kim Y, Kang HK, Choe YH, Jeon HJ, Park S and Lee H (2023) Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database. Front. Endocrinol. 14:1077846. doi: 10.3389/fendo.2023.1077846
Received: 23 October 2022; Accepted: 20 January 2023;
Published: 03 February 2023.
Edited by:
Alok Raghav, Gachon University, Republic of KoreaReviewed by:
Yotsapon Thewjitcharoen, Theptarin Hospital, ThailandZafer Çaliskan, Hacettepe University, Turkey
Copyright © 2023 Lee, Yang, Gu, Kim, Kim, Kang, Choe, Jeon, Park and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyun Lee, bmFtdWhhbmF5ZXlvQGhhbnlhbmcuYWMua3I=; Seungyong Park, Y291Z2hAamJudS5hYy5rcg==
†These authors have contributed equally to this work
‡ORCID: Seungyong Park, orcid.org/0000-0002-3774-4375
Hyun Lee, orcid.org/0000-0002-1269-0913
 Dong-Hwa Lee
Dong-Hwa Lee Bumhee Yang
Bumhee Yang Seonhye Gu3
Seonhye Gu3 Youlim Kim
Youlim Kim Hyun Lee
Hyun Lee