- 1Department of Laboratory Medicine, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Science, Beijing, China
- 2Immune Cells and Antibody Engineering Research Center of Guizhou Province, Key Laboratory of Biology and Medical Engineering, School of Biology and Engineering, Guizhou Medical University, Guiyang, China
- 3Department of Medical Research Center, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing, China
- 4State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Science, Beijing, China
Neuroblastoma breakpoint family, member 1 (NBPF1), appears to be a double-edged sword with regard to its role in carcinogenesis. On the one hand, the tumor-suppressing functions of NBPF1 have been definitively observed in neuroblastoma, prostate cancer, cutaneous squamous cell carcinoma, and cervical cancer. On the other hand, there is evidence that NBPF1 regulates the colony formation, invasion, and maintenance of liver cancer cells and hence functions as an oncogene. The roles of NBPF1 are strictly dependent on the biological context and type of organization. However, a systematic pan-cancer analysis has thus far not been undertaken, and the significance of NBPF1 in the occurrence and progression of many malignancies is uncertain. In this paper, bioinformatics techniques were employed to analyze NBPF1 expression across different cancers and investigate the relationship between NBPF1 and clinical features, prognosis, genetic alteration, and tumor immune microenvironment, respectively. Our results show that NBPF1 is variably expressed in distinct tumor tissues and is also closely linked to clinical outcomes. In particular, compared to other tumor types, there was a strong negative correlation between NBPF1 expression and various components of the tumor microenvironment in adrenocortical carcinoma (ACC). We thus developed an NBPF1-derived immune risk model based on NBPF1-related immune genes; ACC patients with a high-risk score tended to have a poorer prognosis, accompanied by immune hyporesponsiveness. NBPF1 can be used as a prognostic biomarker for multiple cancers. Moreover, anti-NBPF1 immunotherapy may be suitable for treating ACC patients.
Introduction
The increasing sophistication of sequencing technologies, as well as bioinformatics, has allowed us to identify tumor driver genes, molecular subtypes, and other features using large-scale cancer genomics programs, such as The Cancer Genome Atlas (TCGA), the International Cancer Genome Consortium (ICGC), and GENIE. These programs have provided large amounts of tumor genomic and clinical data resources. The structured integration of various multi-omics platforms provides an important opportunity to understand the major genetic alterations that drive cancer development and progression. As genomic and molecular interactions are more reliably described, it is becoming increasingly clear that understanding the characteristics of a unique tissue environment, altered pathways, and immunological features of each cancer and subtype are essential to discern the underlying dynamics of tumorigenesis and to inform diagnosis, prognosis, and treatment.
The neuroblastoma breakpoint family, member 1 (NBFP1) gene was first reported to be disrupted by constitutional translocation in a neuroblastoma patient (1, 2). Subsequently, numerous studies have reported that chromosomal region 1p36, where NBPF1 is located, is broadly deleted in various human malignancies, such as those of hematopoietic, epithelial, and neural origins (3). A meta-analysis based on the Oncomine database showed that levels of NBPF1 were decreased in neuroblastomas that recurred within five years (4). Additionally, in cutaneous squamous cell carcinoma and cervical cancer, NBPF1 inhibits tumor cell proliferation, growth, and cell cycle progression by targeting the PI3K/mTOR and Akt-p53-Cyclin signaling pathways, respectively (5, 6). However, Wu et al. reported that downregulation of NBPF1 in human liver cancer cells strongly inhibits their proliferative capacity (7). Moreover, NBPF1 can form a trimolecular complex with chibby and clusin to engage in critical signaling pathways (such as the Wnt-catenin and NF-kappa-B signaling pathways), which are activated in a disease type-specific manner (8–11). Collectively, previous research has shown that NBPF1 has diverse functions in carcinogenesis and clinical prognosis. However, the expression and prognostic implications of NBPF1 are still unknown, and its probable role in pathological and physiological activities is yet to be thoroughly studied.
Materials and methods
Gene expression
The “Gene_DE” function of the Tumor Immune Estimation Resource, version 2 tool (TIMER2, http://timer.cistrome.org/) was used for observing the NBPF1 transcription differences between 33 tumors and matched noncancerous tissues, including: adrenocortical carcinoma (ACC) (n = 79), bladder urothelial carcinoma (BLCA) (n = 408), breast invasive carcinoma (BRCA) (n = 1,093), cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC) (n = 304), cholangiocarcinoma (CHOL) (n = 36), colon adenocarcinoma (COAD) (n = 457), lymphoid neoplasm diffuse large B cell lymphoma (DLBC) (n = 48), esophageal carcinoma (ESCA) (n = 184), glioblastoma multiforme (GBM) (n = 153), head and neck squamous cell carcinoma (HNSC) (n = 520), kidney chromophobe renal cell carcinoma (KICH) (n = 66), kidney renal clear cell carcinoma (KIRC) (n = 533), kidney renal papillary cell carcinoma (KIRP) (n = 290), acute myeloid leukemia (LAML) (n = 173), brain lower grade glioma (LGG) (n = 516), liver hepatocellular carcinoma (LIHC) (n = 371), lung adenocarcinoma (LUAD) (n = 515), lung squamous cell carcinoma (LUSC) (n = 501), mesothelioma (MESO) (n = 87), ovarian serous cystadenocarcinoma (OV) (n = 303), pancreatic adenocarcinoma (PAAD) (n = 178), pheochromocytoma and paraganglioma (PCPG) (n = 179), prostate adenocarcinoma (PRAD) (n = 497), rectum adenocarcinoma (READ) (n = 166), sarcoma (SARC) (n = 259), skin cutaneous melanoma (SKCM) (n = 103), stomach adenocarcinoma (STAD) (n = 415), testicular germ cell tumors (TGCT) (n = 150), thyroid carcinoma (THCA) (n = 501), thymoma (THYM) (n = 120), uterine corpus endometrial carcinoma (UCEC) (n = 545), uterine carcinosarcoma (UCS) (n = 57), and uveal melanoma (UVM) (n = 80).
Gene expression data were formatted in transcripts per million reads (TPM), and relevant patient records of 33 cancer types were extracted from the TCGA database (http://cancergenome.nih.gov/). Clinical data from the TCGA dataset are shown in Supplementary Tables 1, 2. Microarray datasets with detailed survival data of the ACC cohort, namely, GSE33371 and GSE10927, were acquired from the GEO database (https://www.ncbi.nlm.nih.gov/geo/) and were set as external validation datasets. A total of 47 ACC specimens with accessible prognostic information were included in the external validation dataset.
The limma R package was used to investigate the correlation between clinicopathological features, including pathological stage, TNM stage, and NBPF1 levels.
The TISIDB online tool (http://cis.hku.hk/TISIDB/) was used to analyze NBPF1 expression across different tumor subtypes.
Immunohistochemistry staining
The Human Protein Atlas (HPA; http://www.proteinatlas.org/) was used to obtain IHC images of NBPF1 protein expression.
Survival prognosis analysis of NBPF1
The Gene Expression Profiling Interactive Analysis, version 2 (GEPIA2, https://gepia2.cancer-pku.cn/#analysis) webserver was used to extract survival data relating to NBPF1, including Overall Survival (OS) and Disease-Free Survival (DFS). The median value of NBPF1 expression was set as the expression threshold to determine the high or low expression of NBPF1.
A univariate Cox regression analysis was used to analyze the association between levels of NBPF1 and survival parameters, including OS and disease-specific survival (DSS) in 33 cancers.
Moreover, to determine whether NBPF1 expression could independently predict OS or DSS in patients with ACC, the survival R package was applied to undertake univariate and multivariate logistic regression analysis with NBPF1 expression and various clinical features as variables.
Genetic alteration analysis
The cBioPortal online tool (https://www.cbioportal.org/) was used to assess the frequency of NBPF1 genetic changes among the TCGA tumors. We further analyzed the correlation between survival metrics and NBPF1 DNA copy number amplification and methyltransferase using the GSCA database (http://bioinfo.life.hust.edu.cn/GSCA/).
Correlation between NBPF1 expression and immunological characteristics
The TISIDB online tool was used to assess NBPF1 expression across different immune subtypes and to quantify the linkages between NBPF1 expression and tumor-infiltrating lymphocyte (TIL) abundance. Moreover, we used the TIMER2 web browser to retrieve immune infiltration data for all 33 cancer types. Eight different algorithms, namely, CIBERSORT, CIBERSORT-ABS, EPIC, MCP-counter, quantTIseq, xCell, TIMER, and TIP, were used to estimate immune infiltration.
We downloaded the immune cell infiltration data and immune process score data from the TIP database (12). The gsva R package was employed to conduct ssGSEA analysis for evaluating tumor infiltration fraction, with the generated heatmap showing the correlation between NBPF1 expression levels and the abundance of immune infiltrate cells. The ESTIMATE R package was used to evaluate the stromal and immune scores. Moreover, 122 immunomodulators, including MHC, receptors, chemokines, and immune stimulators, and 47 common immune checkpoint genes were selected from the previously published studies by Charoentong et al. and Chen et al. (13, 14). The Spearman’s correlations between NBPF1 expression levels and immunomodulators and immune checkpoints were calculated in R. PERL scripts were used to evaluate the tumor mutational burden (TMB) of each TCGA tumor case based on the somatic mutation data obtained from the TCGA. The tumor mutation load was calculated as the total number of mutations per megabase sequence in the exon-coding region of a gene (15).
Identification of differentially expressed genes and functional enrichment analysis
The limma R package was used to identify the differentially expressed genes (DEGs) with a |log2(FC)| >1, and the statistical significance of the adjusted P-value was set at<0.05.
To learn more about the probable functions of DEGs, we used the clusterProfiler R package for Gene Ontology (GO)/Kyoto Encyclopedia of Genes and Genomes (KEGG) and GSEA enrichment analysis, the org.Hs.eg.db R package for ID reformation, and the GOplot R package for the z-score calculation. The Zscore was used to determine whether the corresponding entry was positively regulated (zscore >0) or negatively regulated (zscore<0). The generated circle map shows the data of the top five GO terms (including biological process, cellular component, and molecular function) and KEGG functional enrichment of DEGs.
Furthermore, the GSEA R package was used to evaluate the correlation between the marker gene and all other genes contained in the external validation datasets. All genes were then ranked from high to low according to their correlations, and this sorted gene set was used in our analysis. The KEGG signaling pathway set was used as a preset set for the identification of the clusters of biologically related enriched meta-pathways of NBPF1. Statistical significance was set at P<0.05. The enrichment results are presented in Supplementary Table 3.
Establishment of an immune risk score
Evaluation of the Import Shared Database (https://www.immport.org/shared/home) yielded 1,811 immune-related genes (IRGs). The shared immune-related differentially expressed genes (IDEGs) between DEGs and IRGs were identified using the Venn Diagram R program.
We further conducted a univariate Cox regression analysis to screen out the immune-related prognostic genes (IRPGs) with the ability to affect ACC prognosis via the survival R package. Statistical significance was set at P<0.05. The TCGA-ACC cohort was separated into training and validation sets at a 1:1 ratio. Based on the training cohort, LASSO regression analysis was conducted to screen out the optimal candidate IRPGS and establish an immune risk signature in these IRPGS via the glmnet package. According to the prognostic model, the risk score of each sample in the training cohort was calculated, and the median risk score was set as the cut-off value to divide all ACC patients into high- and low-risk groups. We evaluated the effect of the immune risk signature on ACC prognosis between the high- and low-risk groups in the training, testing, and validation cohorts using Kaplan–Meier curves. Subsequently, ROC curves and principal component (PCA) analysis were applied to evaluate the prediction accuracy.
After univariate and multivariate Cox analyses, the overall survival rates of each patient at 1, 2, and 3 years were predicted using a nomogram that integrated ACC clinical features and immune risk signatures. The corresponding calibration curve was used to estimate the prediction accuracy of the nomogram. The heatmap package was used to draw a heatmap of the clinical features and IRS RNA expression.
Since the IRS was built based on IDEGs, we evaluated the correlation of the immune risk signature with immunological characteristics among high- and low-risk populations in the TCGA-ACC cohort. First, the CIBERSORT algorithm and LM22 feature matrix were applied to calculate the composition of immune cells between the two risk groups. Second, the ESTIMATE R package, which generates an ESTIMATEScore inferring tumor purity, was used to evaluate the difference in ESTIMATEScore between high- and low-risk ACC patients. Third, the TIDE algorithm helped us separate ACC patients into non-responder and responder groups according to their clinical response to immunotherapy. Statistical significance was set at P<0.05. Fourth, the expressive variability of immune checkpoints among high- and low-risk populations was determined.
Assessment of drug sensitivity
The Corrplot R package was used to measure the correlations between IRPG expression levels and drug sensitivity using the NCI-60 analysis tools in CellMiner (https://discover.nci.nih.gov/cellminer/). Statistical significance was set at P<0.05. The scatter diagrams generated showed significant correlations with a Pearson correlation coefficient (Cor) >0.6 and a p-value<0.05.
Statistical analysis
The Kruskal–Wallis (KW) test, one-way ANOVA, and Wilcoxon rank sum test were used to analyze NBPF1 expression among 33 TCGA cancers with distinct pathological phases and TNM. Then, Spearman’s method was applied to calculate the correlation between two variables, and statistical significance was set at P<0.05. The R version used was 3.6.3.
Results
Analysis of NBPF1 expression across multiple cancer types
Details of this analysis are shown in Figure 1. First, we used the TIMER database to ascertain the mRNA expression of NBPF1 in multiple cancers and corresponding noncancerous tissues, which revealed that NBPF1 was differentially expressed in various cancers. As shown in Figure 2A, NBPF1 tended to be significantly downregulated in most cancer types, including BRCA, COAD, KICH, KIRC, KIRP, LUSC, PCPG, READ, THCA, and UCEC, suggesting that NBPF1 has an essential anti-cancer role in these cancers, whereas it is overexpressed in CHOL, LIHC, and STAD. In addition to transcription, we investigated the protein expression of NBPF1 in the HPA database since only 12 types of cancer, namely, cervical, colorectal, endometrial, liver, lung, pancreatic, prostate, renal, skin, stomach, testis, and thyroid cancers, were available with normal tissues as controls. We found that, compared with the corresponding normal tissue, NBPF1 was differentially expressed in colorectal, endometrial, liver, renal, stomach, and thyroid cancers (Figure 2B). However, the expression in the other six tumors did not differ from that in normal tissues.
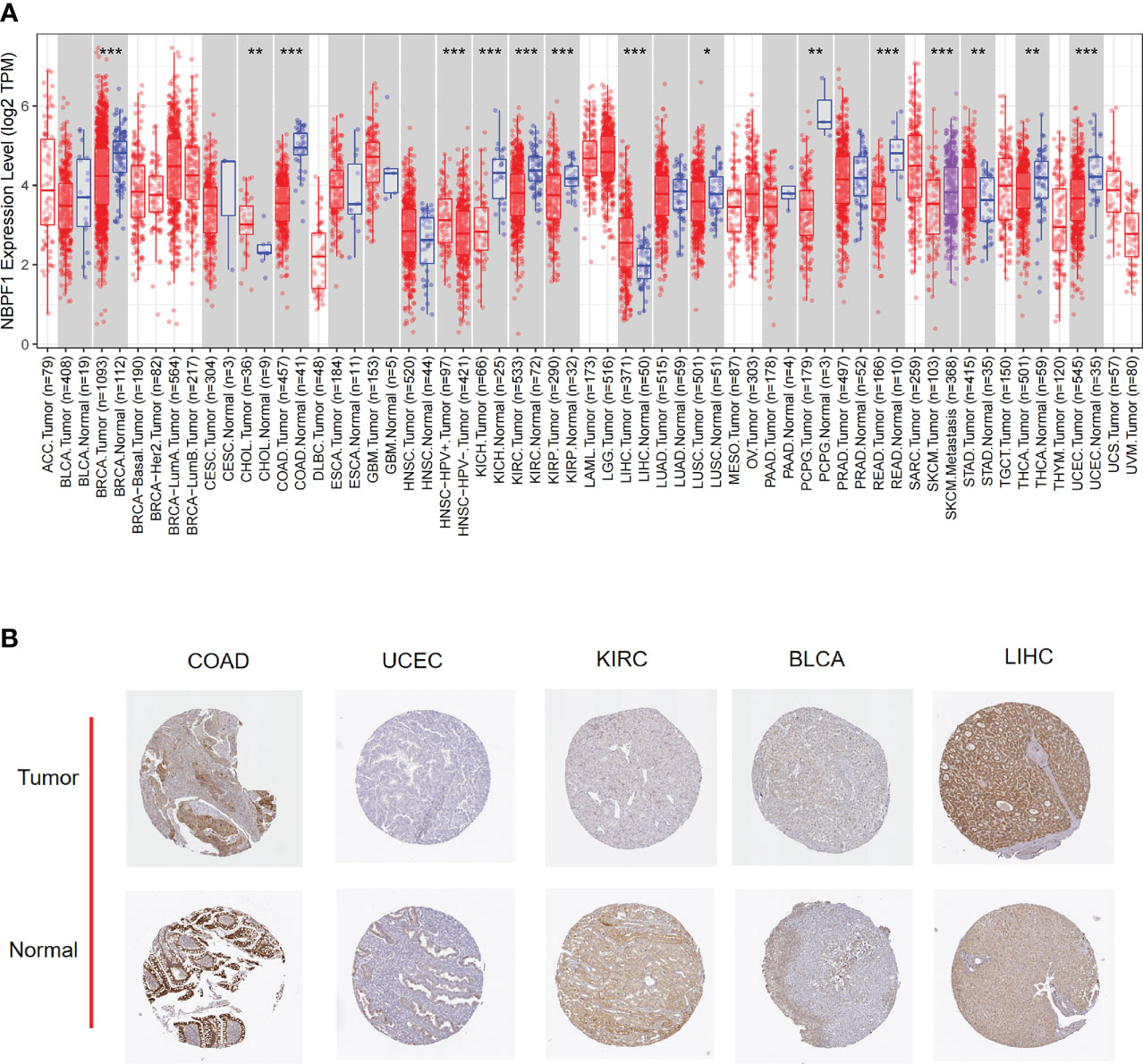
Figure 2 The expression of NBPF1 in human cancers. (A) The expression status of the NBPF1 gene in normal tissues and tumors taken from the TIMER2 database. (B) NBPF1 protein expression based on immunohistochemistry staining taken from the Human Protein Atlas database. (*P<0.05; **P < 0.01; ***P < 0.001).
Next, we examined the expression profile of NBPF1 in tumors of various pathological stages and cancer subtypes, which indicated that low expression of NBPF1 generally predicted late pathological stage in KIRC and LUAD, larger tumor size in KIRC and LUAD, more lymph node metastases in KIRC, and more distant metastases in LUAD. However, an exception to the rule was found in ACC, where overexpression of NBPF1 predicted a greater possibility of lymph node involvement (Figures 3A–F). Additionally, there were discrepancies in the expression levels of NBPF1 in diverse cancer subtypes (Supplementary Figure 1). For example, NBPF1 expression was found to be higher in the CIMP-high ACC subtype.
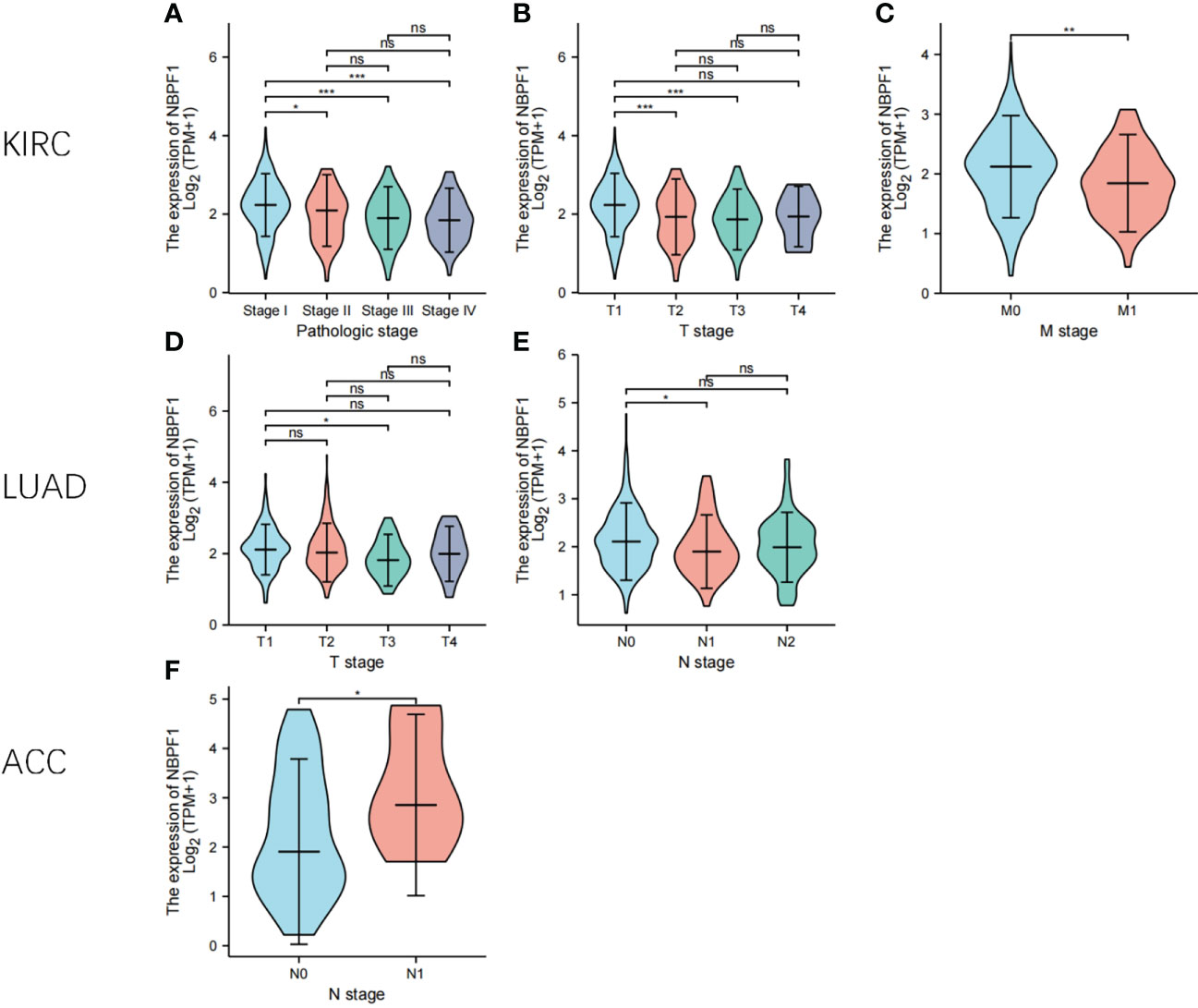
Figure 3 The expression levels of NBPF1 in tumors with different pathological stages. (A–F) The pathological stage-dependent expression levels of NBPF1 (*P < 0.05; **P < 0.01; ***P < 0.001) ns, no significant difference.
Analysis of the prognostic significance of NBPF1 across multiple cancer types
Based on the typical expression values of NBPF1 in 33 types of cancer, patients were separated by median into NBPF1-high and NBPF1-low transcription groups. The correlation between NBPF1 transcription and survival metrics, including OS and DFS, was estimated via Kaplan–Meier survival curves. In patients with ACC, LGG, and LIHC, increased NBPF1 transcription was a risk factor for poorer OS and DFS, while increased NBPF1 expression corresponded with better OS and DFS in patients with KIRC and LUAD (Figures 4A, B).
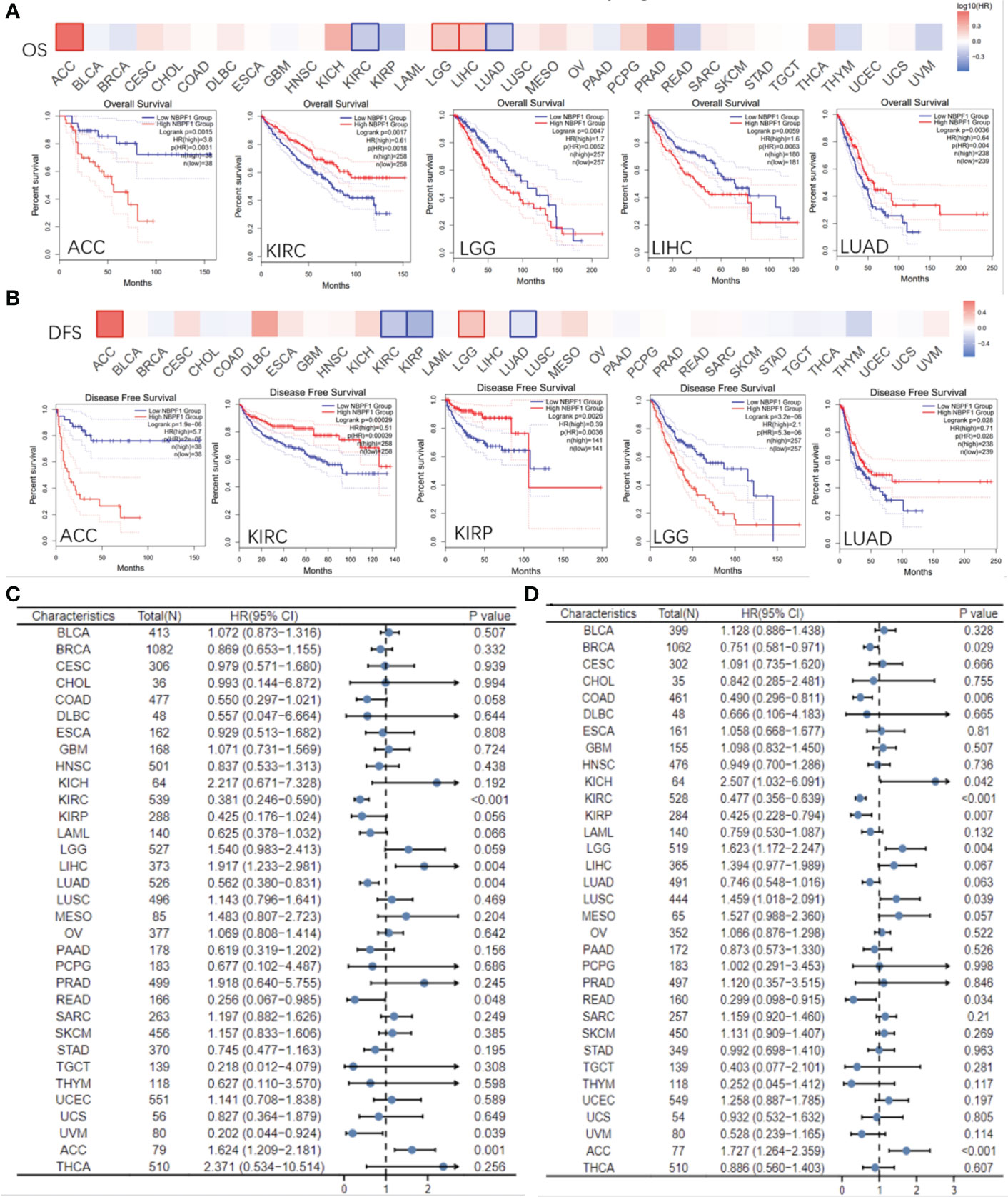
Figure 4 Prognostic value of NBPF1 in human cancers. KM curves and heatmap showing the relationship between NBPF1 gene expression levels and (A) overall survival and (B) disease-free survival taken from the GEPIA2 database. Forest plots of pan-cancer univariate Cox regression analyses of (C) overall survival and (D) disease-specific survival.
Reduced NBPF1 mRNA expression was also associated with shorter OS in KIRC and LUAD according to univariate Cox regression analysis. In contrast, increased NBPF1 expression was correlated with unfavorable OS in ACC and LIHC. We also noticed that NBPF1 expression had a protective influence on DSS in BRCA, COAD, KICH, KIRC, and KIRP. On the other hand, NBPF1 expression was found to be a risk factor for poor DSS in ACC, LGG, and LUSC patients (Figures 4C, D).
These results indicate that NBPF1 is a reliable prognostic biomarker, especially for ACC. We then conducted univariate and multivariate Cox regression analyses to evaluate whether clinical parameters and the expression of NBPF1 were independent prognostic factors for OS and DSS in ACC patients. Tables 1, 2 show that NBPF1 was an appropriate independent prognostic tool for patients with ACC (OS: univariate: HR = 1.624, 95% CI = 1.209–2.181, P = 0.001; multivariate: HR = 1.431, 95% CI = 1.031–1.986, P = 0.032); (DSS: univariate: HR = 1.727, 95% CI = 1.264–2.359, P<0.001; multivariate: HR = 1.489, 95% CI = 1.060–2.091, P = 0.022).
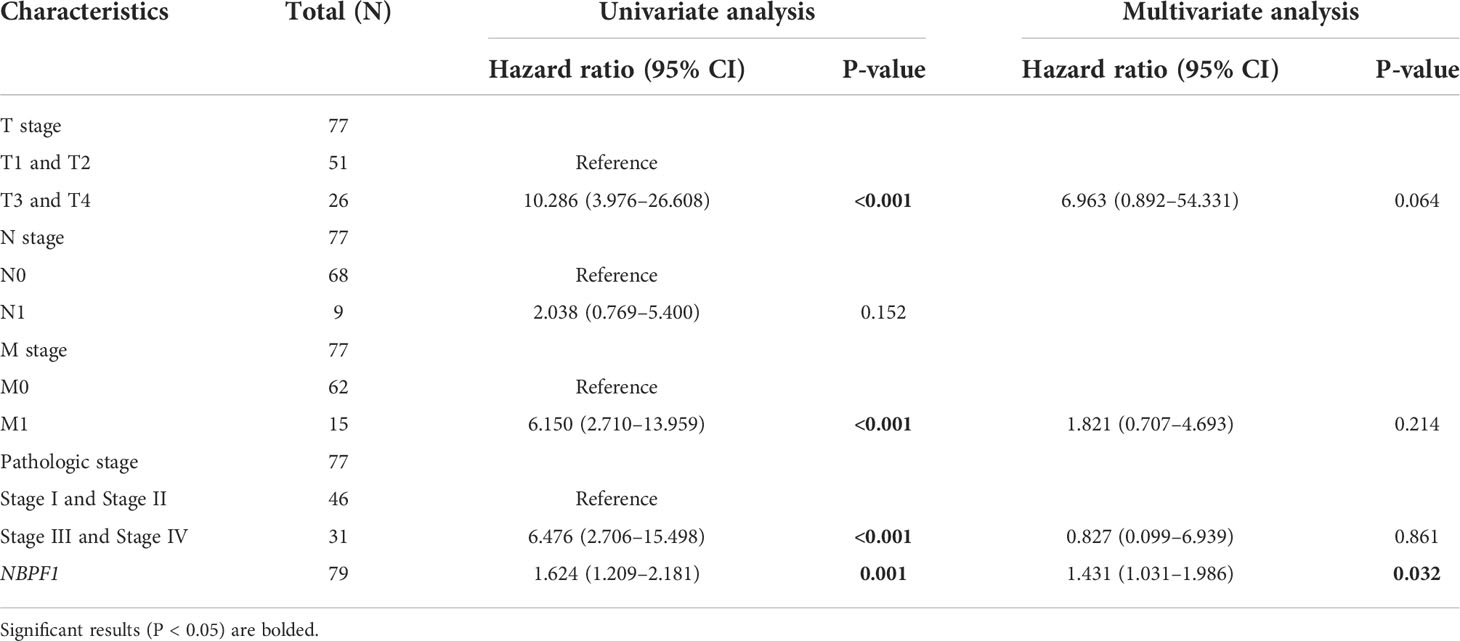
Table 1 Univariate and multivariate Cox regression analyses of clinical characteristics associated with OS of ACC.
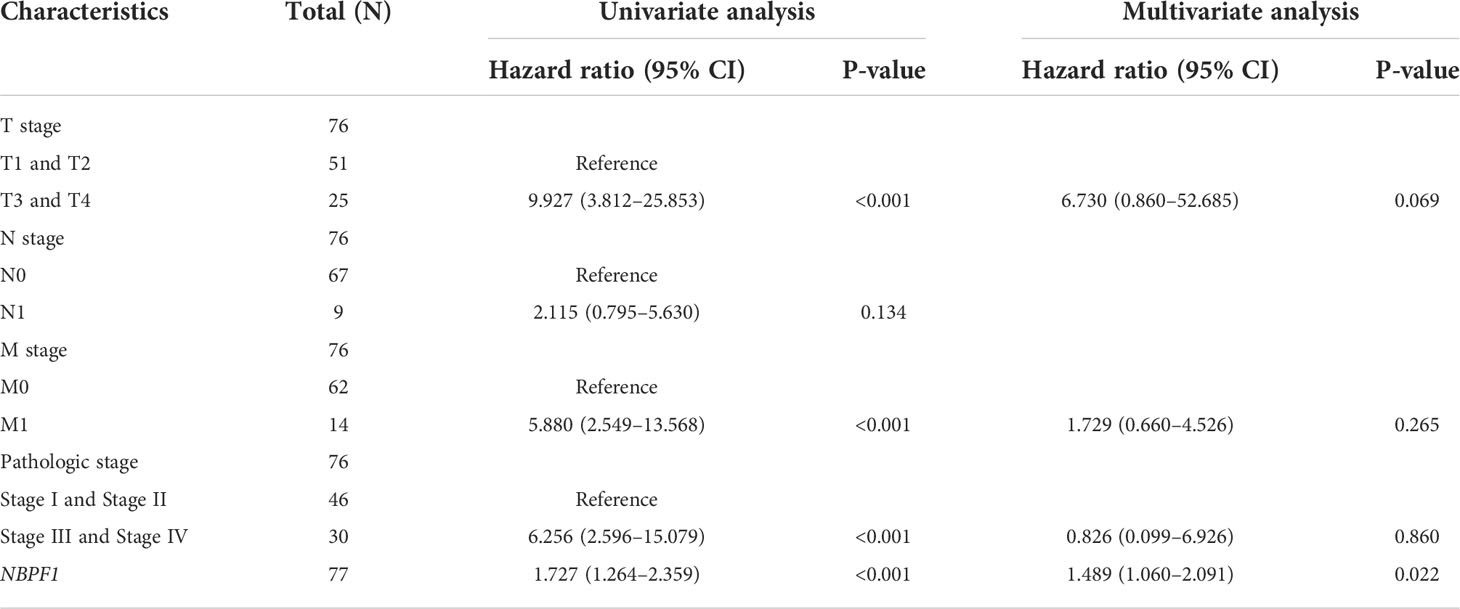
Table 2 Univariate and multivariate Cox regression analyses of clinical characteristics associated with DSS of ACC.
Analysis of genetic alteration in NBPF1 across multiple cancer types
We observed the genetic alteration status of NBPF1 in 33 types of cancer in the TCGA cohort. These consisted primarily of mutation status, copy number alterations (CNA), and methylation. Here, the mutation frequency was higher in UCEC and CHOL than in the other cancers. Additionally, the genomic alteration frequency of NBPF1 was less than 2% in ACC, where the “amplification” type of CNA was the main alteration (Figure 5A). Copy number alterations of NBPF1 were associated with the clinical survival prognosis of ACC patients (Figure 5A–E). In particular, for patients had copy number amplification of NBPF1, their disease-free interval (DFI) and progression-free survival (PFS) rate was worse than those without NBPF1 alteration or those with copy number deletion alterations (Figure 5D–E). Furthermore, a strong negative correlation was found between NBPF1 transcription and DNA methylation in 14 types of cancers (Supplementary Figure 2), and we also observed that patients with ACC with higher DNA methylation of NBPF1 showed a better prognosis in PFS. According to the above data, NBPF1 may be highly expressed in the ACC by underlying DNA copy number amplification or methylation variants, resulting in worse survival (Figures 5B, C).
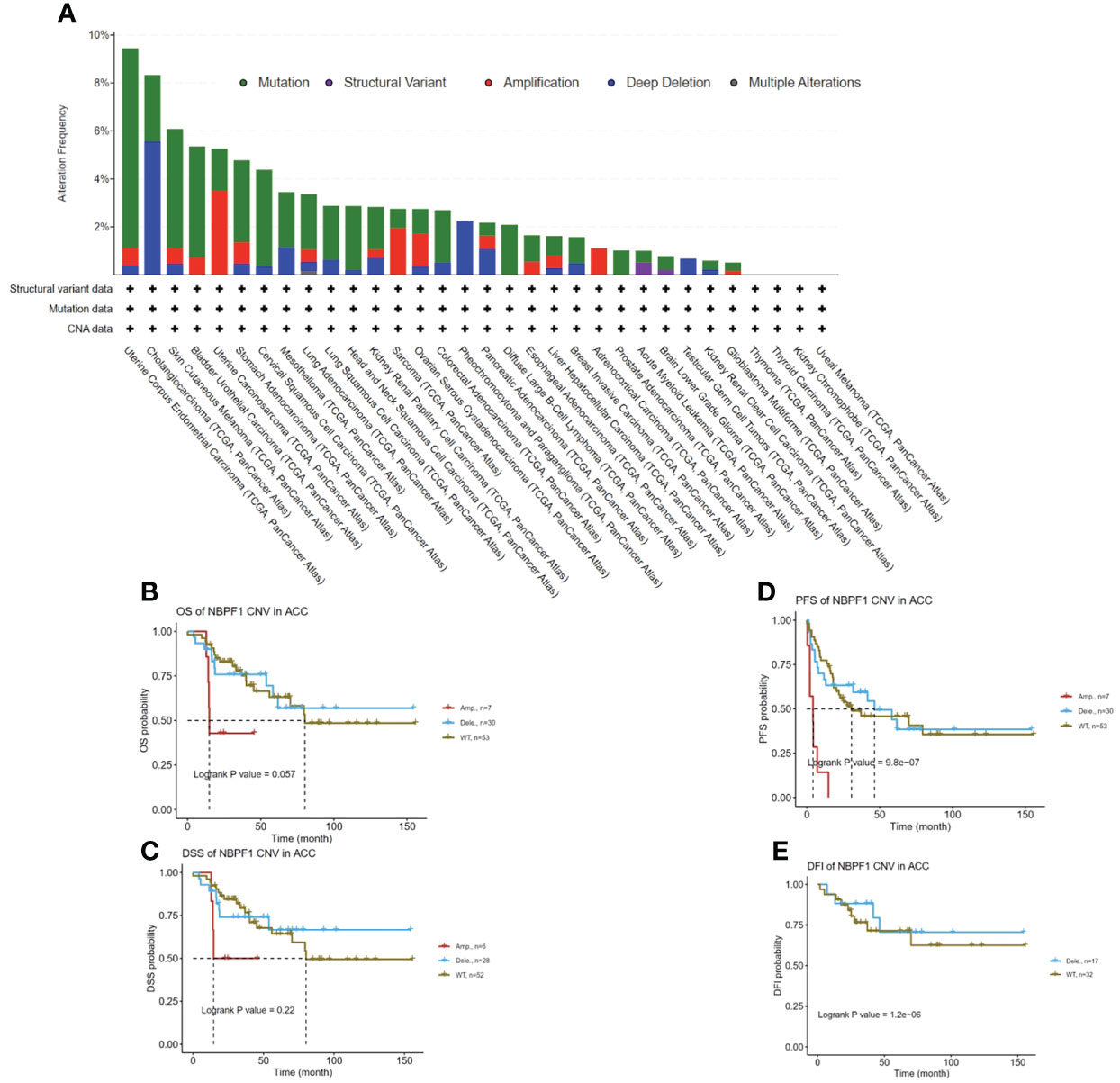
Figure 5 Genetic alteration of NBPF1 in TCGA tumors. (A) Alteration frequency and mutation type of NBPF1. (B–E) Correlation between mutation status and OS, DSS, PFS, and DFI in ACC patients.
The immunological role of NBPF1 across multiple cancer types
Tumorigenesis is an outcome of the complex interactions between tumor cells and their microenvironment. We further explored the possible molecular mechanisms of action of NBPF1 in tumorigenesis and progression by analyzing the association between NBPF1 and tumor immunity in various cancers. The immunophenotype spans traditional anatomical classifications and reflects the integrated regulatory network of immune cells (16), which is closely related to immune features as well as clinical outcomes. We observed different trends of up and downregulation of NBPF1 expression in different immune subtypes of a given cancer type, suggesting the potential immunological role of NBPF1 in certain tumors (Supplementary Figure 3). We further analyzed the correlation between NBPF1 transcription and tumor-infiltrating lymphocytes (TIL) abundance using the TISIDB database (Supplementary Figure 4A). Interestingly, NBPF1 was negatively associated with most immune cells in 30 cancer types, except for KIHC and PAAD, with the negative correlation being particularly evident in ACC. We also observed that the transcription of NBPF1 in patients with ACC seemed to be adversely linked with stromal, immunologic, and ESTIMATE scores (Supplementary Figure 4B). To prevent computational mistakes caused by using a single method and different sets of TIL-tagged genes, we used eight algorithms to calculate the potential association between NBPF1 transcription and infiltrating stromal and immune cells. Although there was some variation in the results obtained by the eight different algorithms, we noted that at least seven algorithms—CIBERSORT (Figure 6A), MCP-counter (Supplementary Figure 5A), CIBERSORT-ABS (Supplementary Figure 5B), quantTIseq (Supplementary Figure 5C), TIP (Supplementary Figure 5D), xCell (Supplementary Figure 6A), EPIC (Supplementary Figure 6B), and TIMER (Supplementary Figure 6C)—produced calculations indicating that the proportions of CD8 T cell and macrophage recruitment in ACC patients were adversely linked to NBPF1 expression. We also observed a positive correlation between NBPF1 transcription and mast cell infiltration in BRCA (Supplementary Figures 7A–I), LUAD (Supplementary Figures 7J–L), and KIRC (Supplementary Figures 7M–O).
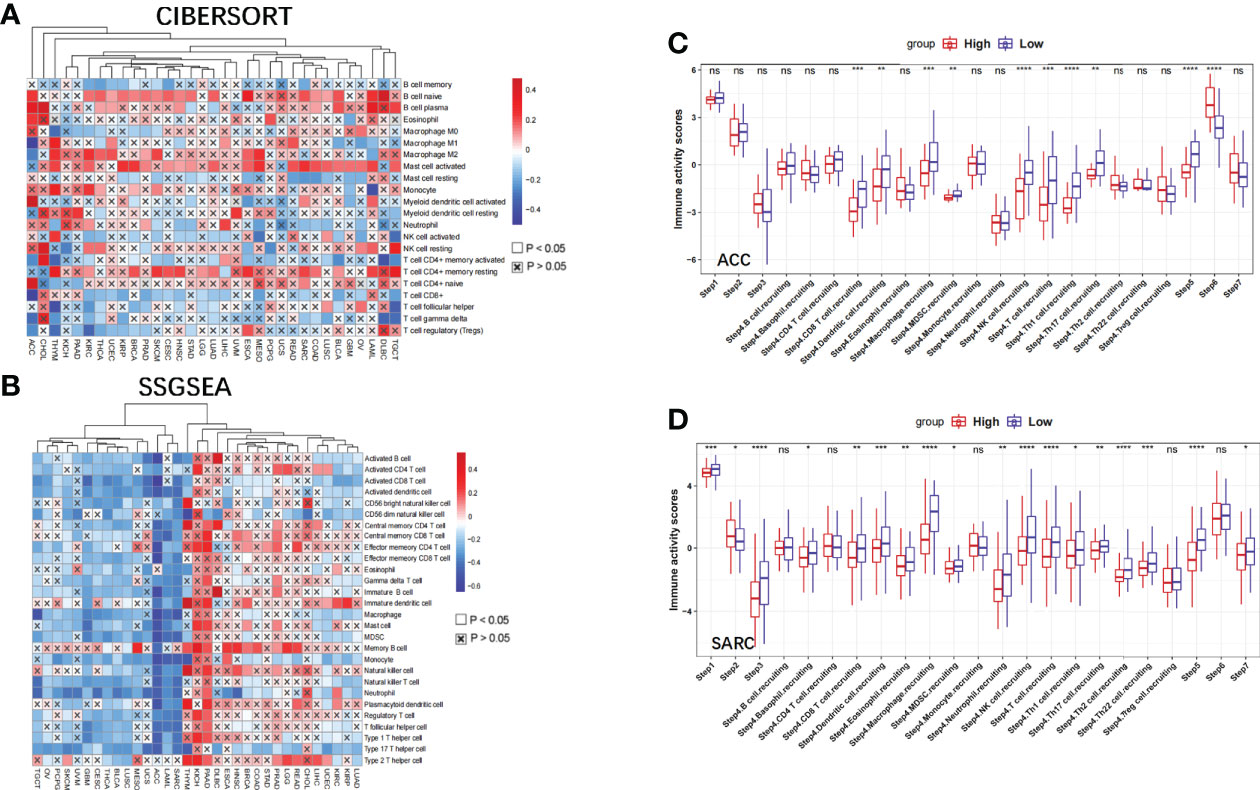
Figure 6 The effect of NBPF1 on immunological status in human cancers. (A) Correlation analysis between NBPF1 expression and the abundance of tumor-infiltrating lymphocytes in human cancers using the CIBERSORT algorithm. (B) Correlation between NBPF1 and 28 tumor-associated immune cells using the ssGSEA algorithm. (C, D) Comparison between groups with high and low NBPF1 expression in the various stages of the cancer immune cycle in ACC and SARC (*P < 0.05; **P < 0.01; ***P < 0.001; ****p < 0.0001; ns, no significant difference).
Moreover, we demonstrated that NBPF1 expression in ACC and SARC was adversely associated with the recruitment of immune cells (Figure 6B) involved in the anti-cancer immune response, and the seven steps of the anti-cancer immune response were differentially suppressed in patients with high expression of NBPF1 (Figures 6C, D). Considering the impact of different pathological stages on the tumor microenvironment, we compared the level of immune cell infiltration between the high- and low-NBPF1 expression groups in patients with ACC with early- (N0) and late-stage (N1) tumors. Supplementary Figure 8 shows that high expression of NBPF1 is associated with suppression of immune cell infiltration in patients with early-stage tumors as taken from the ssGSEA algorithm, which is consistent with our previous findings. However, it is not feasible for us to perform the aforementioned analysis on ACC patients with advanced tumors due to the small number of patients with stage N1 ACC (N = 9) and the fact that only one of them was assigned to the NBPF1-low expression group.
Additionally, NBPF1 was found to be negatively correlated with numerous immunomodulators (MHC, chemokines, receptors, and immunostimulators) (Supplementary Figure 9) in ACC, SARC, and THCA, which are crucial for the activities of the cancer immunity cycle.
Given the association between NBPF1 and tumor immunity, we explored the role of NBPF1 in tumor immunotherapy. We found that the expression of NBPF1 was mutually exclusive of several immune checkpoints in ACC and SARC (Supplementary Figure 10). Likewise, TMB has been identified as a marker of immune checkpoint inhibition (ICI) in the therapeutic response (17); NBPF1 was negatively correlated with TMB in ACC, THYM, and THCA (Supplementary Figure 11). Thus, high levels of NBPF1 expression may predict unsatisfactory immunotherapeutic outcomes when targeting immune checkpoint genes in these cancers.
Analysis of the biological functions of NBPF1 in ACC
Our observations thus far have revealed substantial links between NBPF1 expression and the prognosis and immunological response of ACC patients. We subsequently identified DEGs between NBPF1 groups with elevated or lowered expression levels. According to our generated volcano plot, there were 510 DEGs identified between the elevated/low expression ACC groups, including 235 elevated genes and 275 dysregulated genes (Figure 7A). We then conducted GO/KEGG enrichment analysis based on DEGs; DEGs were abundant in cellular components, including the myosin filament, external side of the plasma membrane, myosin complex, transmembrane transporter complex, and muscle myosin complex. We also observed that the DEGs were involved in certain molecular functions such as cytokine activity, cytokine receptor binding, chemokine activity, chemokine receptor binding, and receptor–ligand activity. The GO analysis of the biological processes revealed that DEGs were recruited for T-cell activation, regulation of T-cell activation, lymphocyte differentiation, calcium ion homeostasis, and positive regulation of cytosolic calcium ion concentration (Figure 7B).
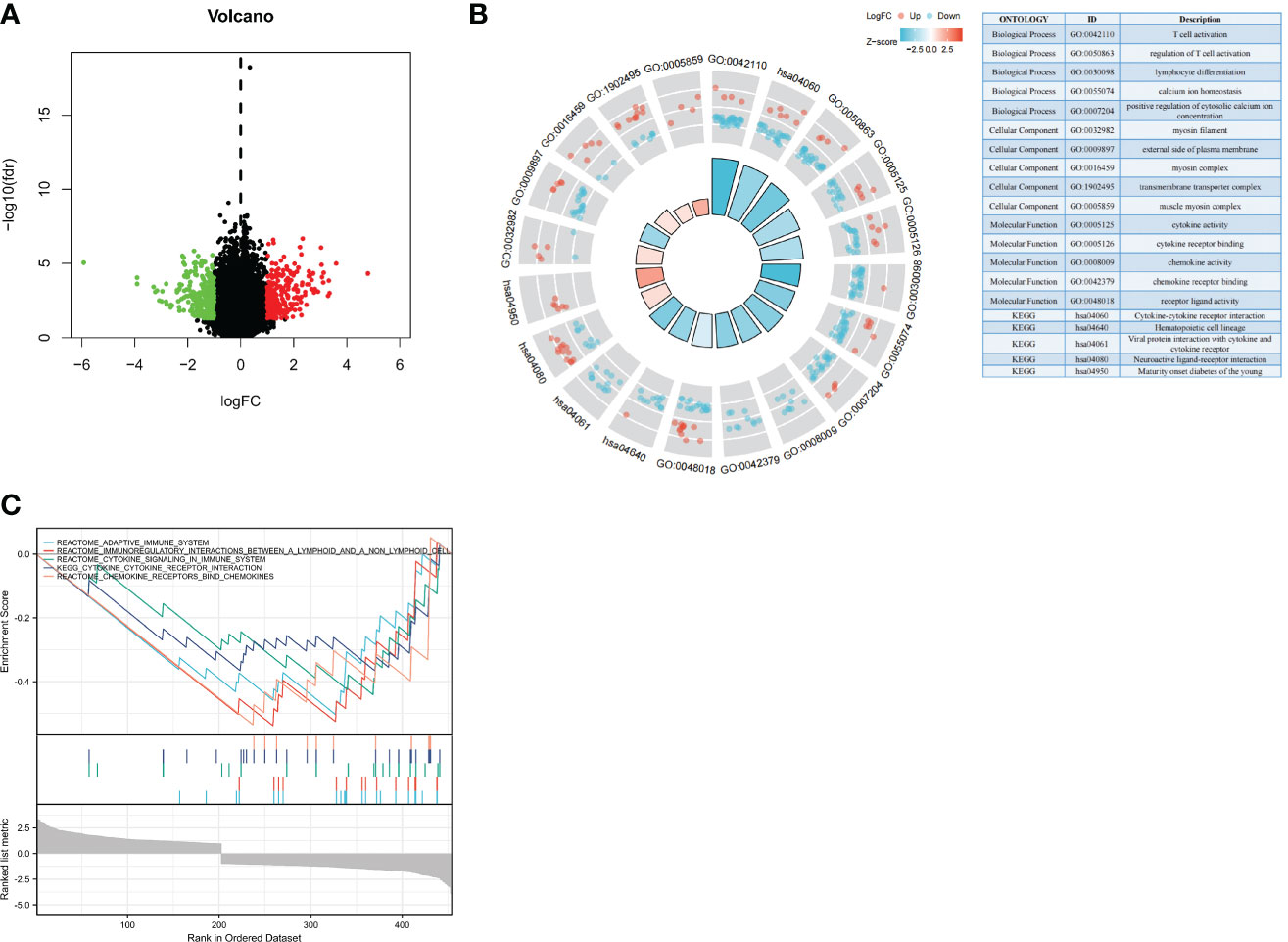
Figure 7 Biological functions of NBPF1 in ACC. (A) Volcano plot showing differentially expressed genes of high- and low-NBPF1 expression groups. (B) GO/KEGG enrichment analysis. (C) GSEA enrichment analysis.
Through GSEA analysis, we also found that DEGs were mainly involved in the regulation of immune responses in ACC patients, including that of the adaptive immune system, immunoregulatory interactions, cytokine signaling, cytokine–receptor interactions, and chemokine receptor binding (Figure 7C). This is also in line with our previous findings that NBPF1 plays a vital role in ACC by reducing the immunological response of the TME. Meanwhile, GSEA analysis was carried out to confirm the putative signaling pathways of NBPF1 in the external (GEO) dataset, and the results suggested that genes relevant to NBPF1 were negatively associated with cytokine–cytokine receptor interactions, primary immunodeficiency, and the toll-like receptor signaling pathway (Supplementary Figure 12). The particular enrichment results have been included in Supplementary Table 4.
Construction and validation of an IRS
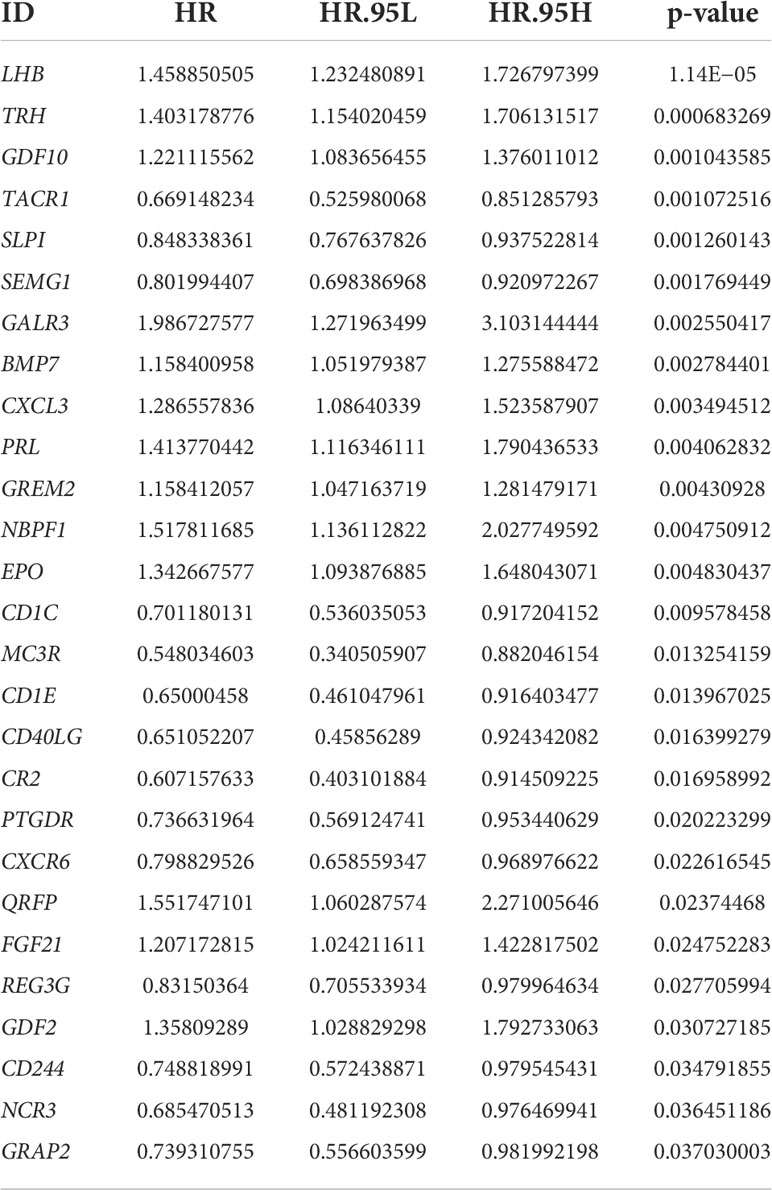
Using Venn analysis, we identified 65 common IDEGs (Supplementary Figure 13), and a univariate Cox regression assessment was used to yield 27 differentially expressed IRPGS (Table 3), which were found to be highly linked to overall survival among ACC samples (P<0.05). A LASSO regression assessment was then performed on these 27 IRPGS, and 13 significant IRPGS were employed to build an IRS based on the training cohort.
The risk score of each sample in the training cohort was calculated according to the prognostic model, and the median risk score in the training cohort was set as the cut-off value (8.5) to divide the ACC training patients into high- and low-risk groups. Km analysis revealed that the high-risk group had a shorter OS (5.051e−05) than the low-risk group. ROC curves demonstrated that the immune risk signature provided an excellent level of prediction accuracy for ACC prognosis in the training group (Figures 8A–E). Next, the same coefficients and cut-off values were applied to the test group. The same pattern was shown by the generated Km curves, and the ROC curve also confirmed the high prediction accuracy of the risk score for ACC prognosis in the testing group (Supplementary Figure 14). However, disappointingly, accurate prediction could not be achieved (Supplementary Figure 15) when we used the same cut-off value in the validation cohort
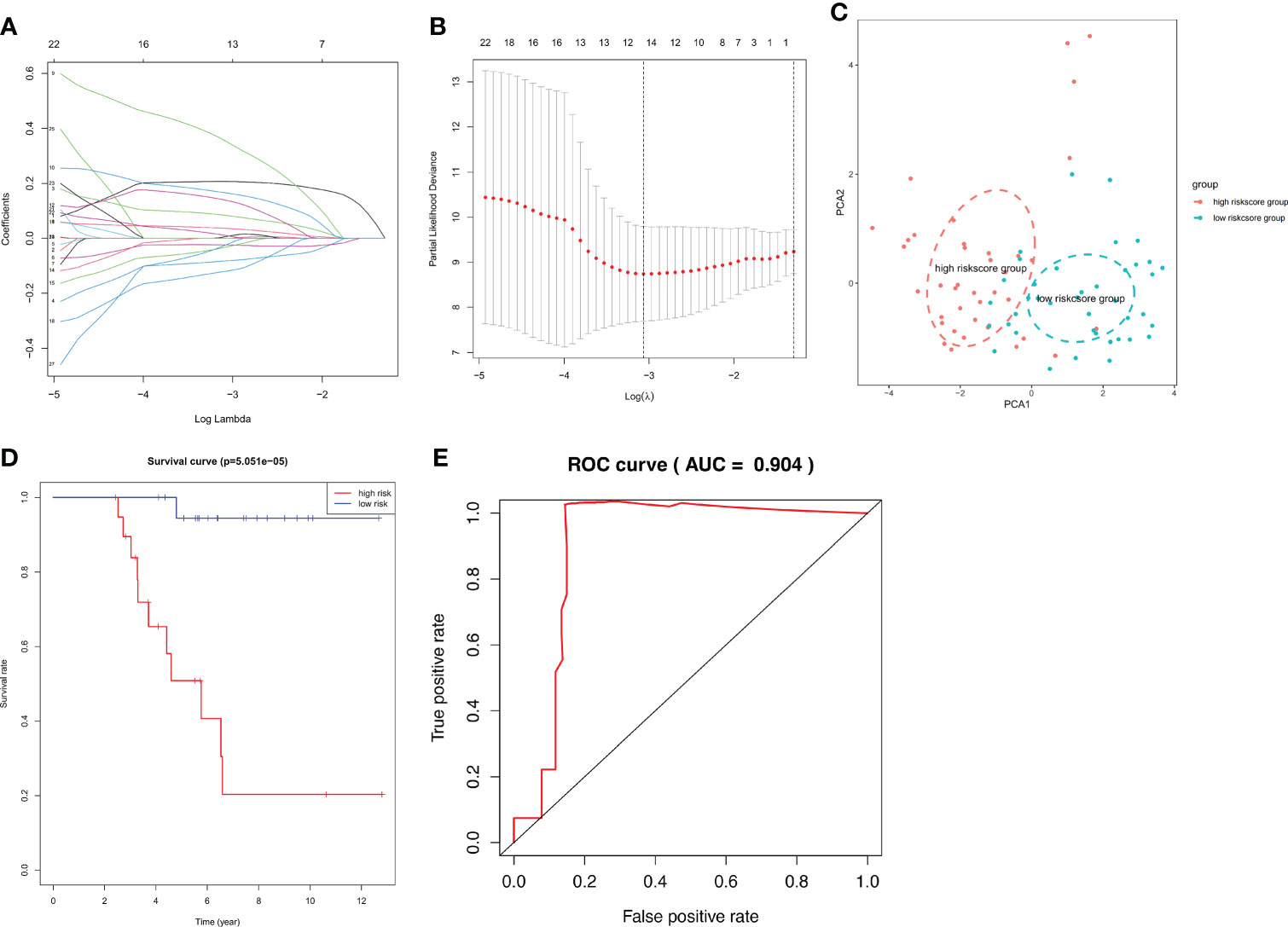
Figure 8 IRS RNA-expression profiles. (A, B) LASSO coefficient spectrum of the 13 selected genes from the TCGA training cohort. (C) Principal Component Analysis (PCA) stratification of TCGA-ACC patients into low- and high-risk groups. (D) Kaplan–Meier curve showing that the survival rate of the low-risk group was significantly greater than the high-risk group in the TCGA training cohort. (E) ROC curve showing the predictive efficiency of the risk scores.
The clinical prognostic monitoring of patients with ACC depends largely on various factors, such as clinicopathological characteristics. Our univariate combined multivariate regression analysis showed that the risk score is an independent indicator, so we inserted the immune risk signature into our ACC prognostic analysis and constructed a nomogram to predict the overall survival rate of an individual at 1, 2, and 3 years. The calibration plots showed that the nomogram performed well in predicting the 1-, 2-, and 3-year OS compared with an ideal model. Moreover, the heatmap showed that high-risk signatures were significantly associated with undesirable clinicopathological status, including pathological stage and high T classification (Figures 9A–E).
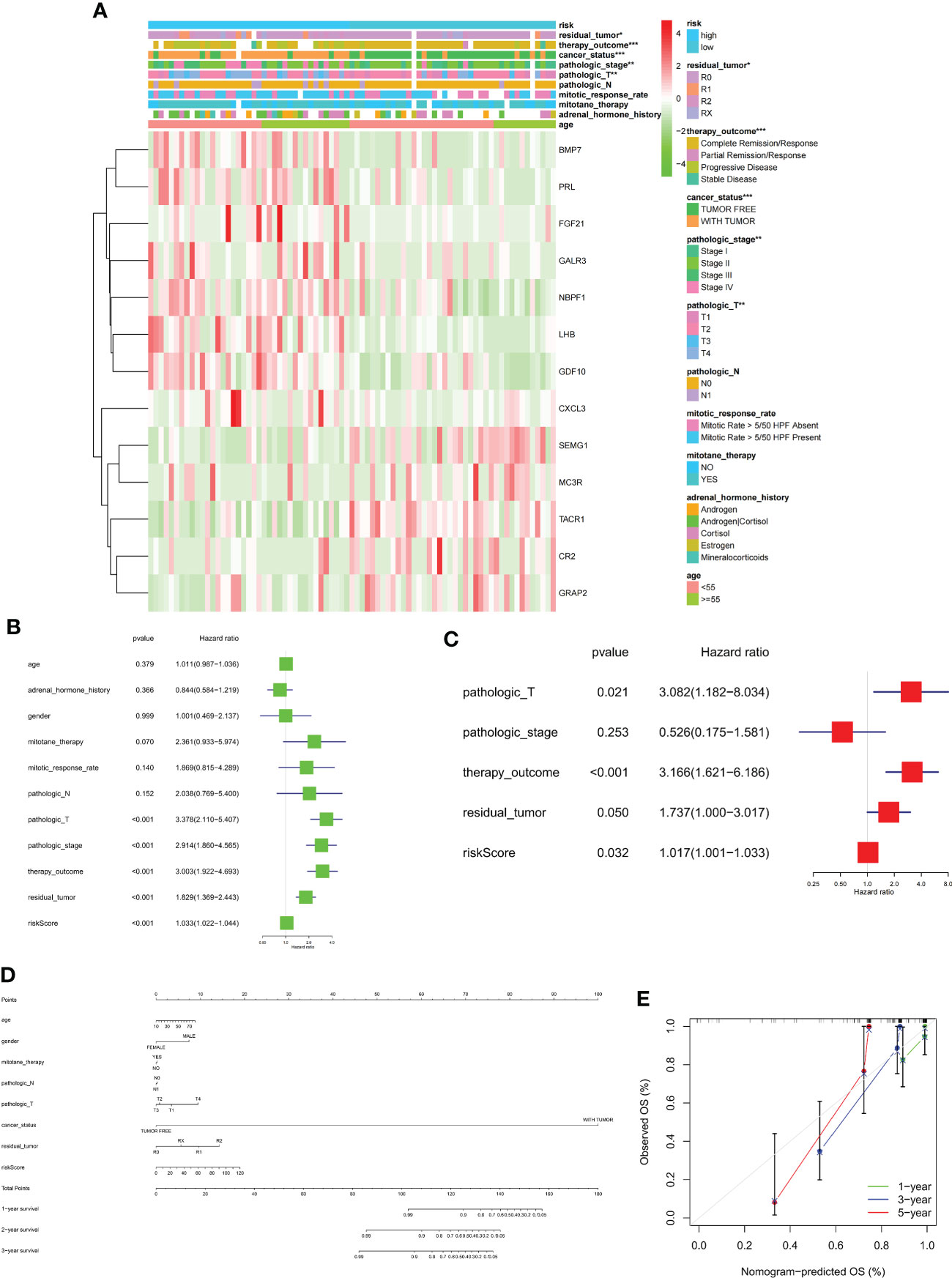
Figure 9 (A) Heatmap comparison of several clinical factors between low- and high-risk groups. (B, C) Univariate Cox regression (green) and multivariate Cox regression (red) showing that the risk signature is an independent prognostic factor for ACC patients. (D) Normogram and (E) calibration curve prediction of the probability of 1-,2-,3-years OS for ACC patients (*p < 0.05, **p < 0.01, ***p < 0.001).
Association between IRS and immunological characteristics
In addition to its prognostic value, the NBPF1-derived immune risk signature is highly associated with TME in TCGA-ACC patients. As shown in Figure 10A, high immune risk can facilitate infiltration of M1 macrophages and resting mast cells while reducing levels of M0 macrophages and activated dendritic cells compared to the low-risk group. Additionally, stromal, immune, and ESTIMATE scores were significantly lower in the high IRS group, suggesting that the process of immune infiltration and the formation of multiple components were significantly inhibited in the high-risk population (Figures 10B–E). Remarkably, we noticed that the clinical response to immunotherapy was stronger in the low IRS population of the TCGA-ACC cohort. It was found that the expression levels of several immune checkpoints, such as PDCD1LG2, CTLA4, CD274, and CD86, were significantly lower in the high-risk population than in the low-risk population (Figures 10F, G).
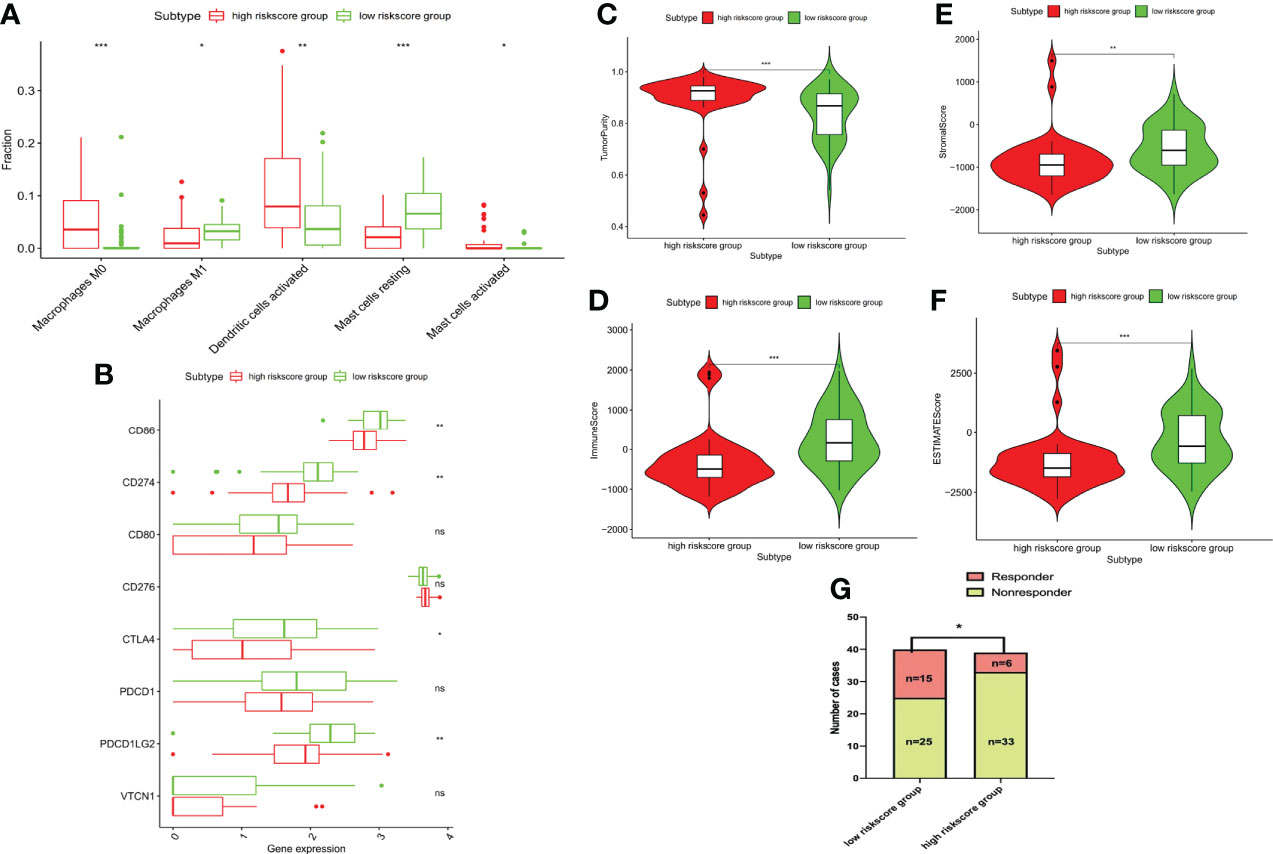
Figure 10 Immune characteristics among different risk groups. (A) Bar chart showing the immune infiltrating cells that are significantly different between the two risk groups. (B) Tumor purity. (C) Immune, (D) stromal, and (E) ESTIMATE scores. (F) Bar chart showing the immune checkpoints that are significantly differentially expressed between the two risk groups. (G) Correlation between risk score and the clinical response to immunotherapy (*P < 0.05, **P < 0.01; ***P < 0.001) ns, no significant difference.
Drug sensitivity
Finally, we assessed the relationship between the 13 IRPGS expression levels and the drug activity of anti-tumor drugs in the NCI-60 cancer cell set and found that, as shown in Figure 11, the sensitivity of nelarabine was increased by GDF10 (Cor = 0.915, p<0.001) and GRAP2 (Cor = 0.855, p<0.001), and the upregulation of GDF10 also enhanced the drug sensitivity of chelerythrine (Cor = 0.617, p<0.001).
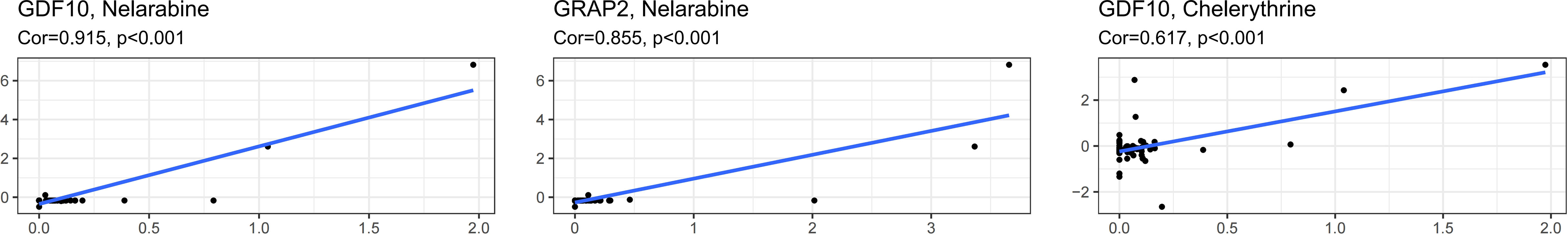
Figure 11 Correlation between IRS RNA-expression and drug sensitivity as derived from the NCI-60 cancer cell set.
Discussion
Our study employed publicly financed cancer genomics programs and archives to decipher the landscape of various tumor types based on NBPF1 expression to determine its likely function in tumorigenesis. In addition to multilevel data comparison of NBPF1 across multiple cancers, we examined the links between NBPF1 expression and clinical manifestations, prognosis, TIME, TMB, immunotherapeutic effectiveness, genetic alteration, function labeling, and enrichment. This comprehensive pan-cancer study revealed the probable biological function of NBPF1 in the development, progression, and clinical prognosis of various human cancers.
In our study, the expression of NBPF1 was significantly downregulated in 10 cancer types in TCGA, while others showed higher expression when compared with paired adjacent normal tissues. This heterogeneity may reflect different underlying functions and mechanisms of NBPF1 across multiple cancer types. Ma et al. reported that Chinese colorectal cancer patients with lower NBPF1 levels showed worse survival rates than those with higher expression levels (18), which is consistent with our finding that NBPF1 is a prognostically relevant protective factor in most tumor types. Interestingly, we found that in a small subset of cancer types, high expression of NBPF1 leads to worse survival outcomes. Notably, both KM analysis and univariate Cox regression assessment suggested that higher expression of NBPF1 was associated with worse survival in patients with ACC. ACC is a rare human malignancy with heterogeneous clinical features and a poor prognosis (19). It has a complex pathogenesis involving multiple aberrant signaling pathways and lacks robust biomarkers to predict the prognosis of patients with ACC. To our knowledge, our study is the first to indicate that NBPF1 expression may be utilized as a prognostic factor in ACC, referring to univariable and multivariable Cox regression. Furthermore, existing research has revealed that NBPF family genes show a high degree of copy number fluctuation in various human diseases, which may be implicated in developmental disorders, craniofacial dysmorphism, and early tumorigenesis of neuroblastoma (20, 21). Subsequently, we further investigated NBPF1 alterations using the cBioPortal database and observed that NBPF1 showed the greatest prevalence of copy number alterations in patients with cholangiocarcinoma. Given the probable role of NBPF family genes in pathological processes, it is worth examining the role of NBPF1 gene variation, particularly copy number alterations, as a cancer sensor in patients with cholangiocarcinoma. We found that amplification was the most prevalent kind of alteration in ACC patients, and, using the GSCA database, we found that NBPF1 expression was shown to be inversely linked with methylation levels in patients with ACC. Moreover, those with hypomethylation of NBPF1 had a worse prognosis. These findings indicate that NBPF1 is a promising prognostic biomarker for ACC and that DNA copy number amplification and methylation may be the two underlying drivers of NBPF1 dysregulation in ACC.
Multiple studies have revealed that the tumor microenvironment not only has a significant impact on tumor development but also plays a key role in immune evasion and treatment resistance. Tumor immune infiltrating cells, an important component of the tumor microenvironment, determine the immune landscape. We employed different methods to evaluate the association between NBPF1 and TIL abundance and observed that NBPF1 gene expression is strongly linked to the degree of mast cell infiltration in patients with LUAD and BRCA. According to a review by Aponte-López et al. (22), high mast cell infiltration has been linked to a better prognosis in non-small cell lung cancer and BRCA in several clinical trials, which is consistent with our prognostic analysis. Therefore, we propose that NBPF1 may work in BRCA and LUAD patients by modulating the number of anti-tumor mast cells in the tumor microenvironment, which further contributes to a better prognosis. In contrast, CD8 T cells were significantly reduced in ACC patients with high NBPF1 expression. Consistent with previous studies, the abundance of CD8+ T cells had an anti-tumor effect and was linked with a positive prognosis, tumor size, and staging in most types of cancers. The anti-cancer immune response can be conceptualized into seven steps: release of cancer cell antigens (Step 1), cancer antigen presentation (Step 2), priming and activation (Step 3), trafficking of immune cells to tumors (Step 4), infiltration of immune cells into tumors (Step 5), recognition of cancer cells by T cells (Step 6), and killing of cancer cells (Step 7) (23). Given the intricacy of the mechanisms underlying the anti-cancer immune response, we assessed immune activation processes and immune infiltration among 33 cancer types and found that NBPF1 may inhibit the activation of anti-tumor immunity, particularly in ACC and SARC. GSEA of NBPF1 also revealed that immune-regulation-relevant pathways were enriched in ACC. In recent years, a growing number of studies have found that decreased TIL levels are associated with higher TNM and AJCC staging and better OS and PFS in patients with ACC (24). Drawing on the findings of the preceding investigation, we hypothesized that NBPF1-mediated inhibition of TIL infiltration might be a prime driver of its oncogenic effect in ACC. Despite the fact that the relationship between TME and immunotherapy efficacy has received comparatively little investigation in ACC, T-cell infiltration is required for successful immunotherapeutic implementation. It has also been found that NBPF1 may regulate the expression of specific immune checkpoint genes. Our study presents evidence for an association between NBPF1 and TMB. These results imply that future research efforts should concentrate on modifying the TME by targeting NBPF1, provide insight into the potential of NBPF1 expression to predict the effect of immunotherapy, and stratify patients for the selection of those who should follow immune checkpoint blockade treatment.
Furthermore, we constructed and validated a novel immune risk signature and demonstrated that it is involved in the prognosis, progression, and TME of patients with ACC. The prognosis of the high-risk population, which is substantially linked to unsatisfactory clinical staging and a higher T classification, is poorer than that of the low-risk population. Although in the external dataset, this cut-off of the risk score that we have established did not distinguish between two different prognostic ACC populations, we believe that this might be the result of batch effects brought on by various sequencing platforms and methodologies. We believe that specific cut-offs should be established for patients with different platforms or laboratory origins. Nomograms integrated with immune risk signatures and clinical features were developed to monitor the survival rates of patients with ACC. The application of the nomogram in clinical practice may provide more detailed information on survival. Additionally, in this study, the risk signature extensively affected the activities of various immune cells in the TME. M0 macrophages can polarize into M1 and M2 macrophages in different environments, and evidence accumulated from many cancer models demonstrated that M1 macrophages possess inflammation-promoting characteristics, which activate cytotoxic anti-tumor mechanisms (25). According to Huang et al., the degree of M0 macrophage infiltration was significantly higher in metastatic ACC than in non-metastatic patients (26). Notably, the immune risk may lead to the suppression of M1 macrophage infiltration and the promotion of M0 infiltration, which suggests that high immune risk may contribute to tumor immune escape and poor prognosis in patients with ACC. In addition, high immune risk can also suppress the expression of immune checkpoint markers and is associated with a failed immunotherapy response. Inspired by the results from other cancer models, the efficacies of the PD-L1 inhibitors pembrolizumab, nivolumab, and avelumab were evaluated in a number of patients with advanced ACC. However, most of these trials have shown a poor therapeutic response to immune checkpoint blockade (24, 27, 28). The immune risk profile identifies molecular alterations among immunotherapy responders and non-responders, which may contribute to improving patient recruitment in future trials.
To the best of our knowledge, this is the first study to explore the specific role of NBPF1 in pan-cancer prognostic relevance and cancer immune regulation, particularly in ACC. However, our study has certain limitations. First, more basic experiments are required to determine the functional mechanisms of NBPF1. Second, all records in our study were collected from public sources and need to be validated further in prospective clinical studies.
Conclusion
Our study explored the role of genetic and epigenetic changes in NBPF1 across generalized carcinoma for the first time. We discovered that NBPF1 expression differed among tumor tissues and was linked to clinical outcomes across different cancers. Particularly in patients with ACC, NBPF1 and related immune risk genes may impact tumorigenesis, the tumor microenvironment, and anti-tumor drug selection. Our study provides a basis for further investigation of the role of NBPF1 in regulating the immune microenvironment and offers novel ideas for developing anti-NBPF1 immunotherapy for patients with ACC.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
LL and YH designed the study and performed the analysis. SC and YT prepared and revised the manuscript. JW and LQ finalized the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The study received support from the Capital’s Funds for Health Improvement and Research (CFH-2020-1-4014) and the Beijing Key Clinical Specialty for Laboratory Medicine-Excellent Project (No. ZK201000).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.950326/full#supplementary-material
References
1. Laureys G, Speleman F, Opdenakker G, Benoit Y, Leroy J. Constitutional translocation T (1,17)(P36;Q12-21) in a patient with neuroblastoma. Genes Chromosomes Cancer (1990) 2(3):252–4. doi: 10.1002/gcc.2870020315
2. Laureys G, Speleman F, Versteeg R, van der Drift P, Chan A, Leroy J, et al. Constitutional translocation T(1;17)(P36.31-P36.13;Q11.2-Q12.1) in a neuroblastoma patient. Establishment of somatic cell hybrids and identification of Pnd/A12m2 on chromosome 1 and Nf1/Scya7 on chromosome 17 as breakpoint flanking single copy markers. Oncogene (1995) 10(6):1087–93.
3. Bagchi A, Mills AA. The quest for the 1p36 tumor suppressor. Cancer Res (2008) 68(8):2551–6. doi: 10.1158/0008-5472.CAN-07-2095
4. Rhodes DR, Kalyana-Sundaram S, Mahavisno V, Varambally R, Yu J, Briggs BB, et al. Oncomine 3.0: Genes, pathways, and networks in a collection of 18,000 cancer gene expression profiles. Neoplasia (2007) 9(2):166–80. doi: 10.1593/neo.07112
5. Qin Y, Tang X, Liu M. Tumor-suppressor gene NBPF1 inhibits invasion and Pi3k/Mtor signaling in cervical cancer cells. Oncol Res (2016) 23(1-2):13–20. doi: 10.3727/096504015X14410238486766
6. Gao Y, Zhu H, Mao Q. Effects of neuroblastoma breakpoint family member 1 (NBPF1) gene on growth and akt-P53-Cyclin d pathway in cutaneous squamous carcinoma cells. Neoplasma (2019) 66(4):584–92. doi: 10.4149/neo_2018_181123N888
7. Wu L, Wei Y, Zhou WB, Zhang YS, Chen QH, Liu MX, et al. Gene expression alterations of human liver cancer cells following borax exposure. Oncol Rep (2019) 42(1):115–30. doi: 10.3892/or.2019.7169
8. Vandepoele K, Staes K, Andries V, van Roy F. Chibby interacts with NBPF1 and clusterin, two candidate tumor suppressors linked to neuroblastoma. Exp Cell Res (2010) 316(7):1225–33. doi: 10.1016/j.yexcr.2010.01.019
9. Takemaru K, Yamaguchi S, Lee YS, Zhang Y, Carthew RW, Moon RT. Chibby, a nuclear beta-Catenin-Associated antagonist of the Wnt/Wingless pathway. Nature (2003) 422(6934):905–9. doi: 10.1038/nature01570
10. Yu F, Yu C, Li F, Zuo Y, Wang Y, Yao L, et al. Wnt/Beta-catenin signaling in cancers and targeted therapies. Signal Transduct Target Ther (2021) 6(1):307. doi: 10.1038/s41392-021-00701-5
11. Zoubeidi A, Ettinger S, Beraldi E, Hadaschik B, Zardan A, Klomp LW, et al. Clusterin facilitates Commd1 and I-kappab degradation to enhance nf-kappab activity in prostate cancer cells. Mol Cancer Res (2010) 8(1):119–30. doi: 10.1158/1541-7786.MCR-09-0277
12. Xu L, Deng C, Pang B, Zhang X, Liu W, Liao G, et al. Tip: A web server for resolving tumor immunophenotype profiling. Cancer Res (2018) 78(23):6575–80. doi: 10.1158/0008-5472.CAN-18-0689
13. Charoentong P, Finotello F, Angelova M, Mayer C, Efremova M, Rieder D, et al. Pan-cancer immunogenomic analyses reveal genotype-immunophenotype relationships and predictors of response to checkpoint blockade. Cell Rep (2017) 18(1):248–62. doi: 10.1016/j.celrep.2016.12.019
14. Chen K, Shen D, Tan L, Lai D, Han Y, Gu Y, et al. A pan-cancer analysis reveals the prognostic and immunotherapeutic value of Alkbh7. Front Genet (2022) 13:822261. doi: 10.3389/fgene.2022.822261
15. Budczies J, Seidel A, Christopoulos P, Endris V, Kloor M, Gyorffy B, et al. Integrated analysis of the immunological and genetic status in and across cancer types: Impact of mutational signatures beyond tumor mutational burden. Oncoimmunology (2018) 7(12):e1526613. doi: 10.1080/2162402X.2018.1526613
16. Thorsson V, Gibbs DL, Brown SD, Wolf D, Bortone DS, Ou Yang TH, et al. The immune landscape of cancer. Immunity (2018) 48(4):812–30.e14. doi: 10.1016/j.immuni.2018.03.023
17. Gao Y, Yang C, He N, Zhao G, Wang J, Yang Y. Integration of the tumor mutational burden and tumor heterogeneity identify an immunological subtype of melanoma with favorable survival. Front Oncol (2020) 10:571545. doi: 10.3389/fonc.2020.571545
18. Ma R, Jing C, Zhang Y, Cao H, Liu S, Wang Z, et al. The somatic mutation landscape of Chinese colorectal cancer. J Cancer (2020) 11(5):1038–46. doi: 10.7150/jca.37017
19. Bilimoria KY, Shen WT, Elaraj D, Bentrem DJ, Winchester DJ, Kebebew E, et al. Adrenocortical carcinoma in the United States: Treatment utilization and prognostic factors. Cancer (2008) 113(11):3130–6. doi: 10.1002/cncr.23886
20. Zhu L, Su X. Case report: Neuroblastoma breakpoint family genes associated with 1q21 copy number variation disorders. Front Genet (2021) 12:728816. doi: 10.3389/fgene.2021.728816
21. Diskin SJ, Hou C, Glessner JT, Attiyeh EF, Laudenslager M, Bosse K, et al. Copy number variation at 1q21.1 associated with neuroblastoma. Nature (2009) 459(7249):987–91. doi: 10.1038/nature08035
22. Aponte-Lopez A, Munoz-Cruz S. Mast cells in the tumor microenvironment. Adv Exp Med Biol (2020) 1273:159–73. doi: 10.1007/978-3-030-49270-0_9
23. Chen DS, Mellman I. Oncology meets immunology: The cancer-immunity cycle. Immunity (2013) 39(1):1–10. doi: 10.1016/j.immuni.2013.07.012
24. Georgantzoglou N, Kokkali S, Tsourouflis G, Theocharis S. Tumor microenvironment in adrenocortical carcinoma: Barrier to immunotherapy success? Cancers (Basel) (2021) 13(8). doi: 10.3390/cancers13081798
25. Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, et al. Macrophage activation and polarization: Nomenclature and experimental guidelines. Immunity (2014) 41(1):14–20. doi: 10.1016/j.immuni.2014.06.008
26. Huang R, Liu Z, Tian T, Song D, Yan P, Yin H, et al. The construction and analysis of tumor-infiltrating immune cells and cerna networks in metastatic adrenal cortical carcinoma. Biosci Rep (2020) 40(3). doi: 10.1042/BSR20200049
27. Habra MA, Stephen B, Campbell M, Hess K, Tapia C, Xu M, et al. Phase ii clinical trial of pembrolizumab efficacy and safety in advanced adrenocortical carcinoma. J Immunother Cancer (2019) 7(1):253. doi: 10.1186/s40425-019-0722-x
Keywords: NBPF1, pan-cancer analysis, adrenocortical carcinoma, immune, biomarker
Citation: Li L, Chen S, Tang Y, Wu J, He Y and Qiu L (2022) Oncogene or tumor suppressor gene: An integrated pan-cancer analysis of NBPF1. Front. Endocrinol. 13:950326. doi: 10.3389/fendo.2022.950326
Received: 22 May 2022; Accepted: 22 July 2022;
Published: 17 August 2022.
Edited by:
Rosa Marina Melillo, University of Naples Federico II, ItalyReviewed by:
Carolina Panis, Universidade Estadual do Oeste do Paraná, BrazilYong Qi, Henan Provincial People’s Hospital, China
Copyright © 2022 Li, Chen, Tang, Wu, He and Qiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Wu, d3VqaWVfcHVtY2hAMTYzLmNvbQ==; Yangzhige He, eXpnX2hlQDE2My5jb20=; Ling Qiu, bGluZ3FpdWJqQDE2My5jb20=
 Lei Li1
Lei Li1 Yangzhige He
Yangzhige He Ling Qiu
Ling Qiu