- 1Diabetes Unit, Rashid Hospital, Dubai, United Arab Emirates
- 2Internal Medicine, Setif University Hospital, Setif, Algeria
- 3Research and Scientific Centre, Sultan Bin Abdulaziz Humanitarian City, Riyadh, Saudi Arabia
- 4University of the Witwatersrand, Netcare Union and Clinton Hospitals, Alberton, South Africa
- 5Endocrinology and Metabolism, Erciyes University Faculty of Medicine, Kayseri, Turkey
- 6Endocrinology Division, Rafik Hariri University Hospital, Beirut, Lebanon
- 7Medical Affairs Department, AstraZeneca Middle East and Africa, Luton, United Kingdom
- 8Medical Affairs Department, AstraZeneca Algeria, Algiers, Algeria
Background: We evaluated the prevalence of vascular complications and associated risk factors in individuals with type 2 diabetes mellitus (T2DM) initiating second-line glucose-lowering therapy from the Middle East and Africa (MEA) cohort of the 3-year prospective DISCOVER study involving 15,992 patients in 38 countries.
Methods: Baseline cross-sectional data collected from healthcare settings were used to assess micro and macrovascular complications prevalence as crude and age- and sex-standardised. The multi‐variable analysis assessed factors associated with these complications.
Results: Of 3,525 enrolled patients (mean age: 54.3 ± 10.8 years), >40% had hypertension and hyperlipidaemia. Metformin monotherapy was the first-line therapy in 56.5%, followed by metformin+sulphonylurea (20.3%). Crude and standardised prevalence of microvascular complications were 17.7% and 16.9% (95% confidence interval [CI], 16.77‐16.98) and macrovascular complications were 10.7% and 8.7% (95% CI, 8.59–8.76). Factors significantly (p<0.05) associated with micro and macrovascular complications (odds ratios [95% CI]) were age (1.24 [1.12–1.39] and 1.58 [1.35–1.84]), male sex (1.33 [1.04‐1.70] and 1.71 [1.22–2.40]), hyperlipidaemia (1.33 [1.07-1.65] and 1.96 [1.46-2.63]) and hypertension (1.75 [1.40–2.19] and 2.84 [2.07-3.92]).
Conclusion: A substantial burden of vascular complications with prominent risk factors in the MEA cohort calls for early preventive interventions.
Introduction
Diabetes has seen exponential growth over the last two decades transcending all the socioeconomic and national boundaries to become a truly global epidemic (1). There has been a steady increase in the prevalence of diabetes with International Diabetes Federation (IDF) Middle East and North Africa (MENA) region having the highest age-adjusted comparative prevalence of diabetes (12.2%) in people aged 20 to 79 years with country-specific prevalence varying from 5.4% in Yemen to 22.1% in Sudan (2). MENA region has also reported the second-highest rate of rise, the highest‐adjusted mortality from non‐communicable disease and the highest diabetes-related disability‐adjusted life years (3).
In Africa, despite the lowest Age-adjusted diabetes prevalence and the highest proportion of undiagnosed diabetes among all IDF regions, South Africa registered a prevalence of 12.7% (2).
The most common form, type 2 diabetes mellitus (T2DM) is associated with various micro and macrovascular complications that negatively impact the quality of life and increase morbidity and mortality and account for the majority of the social and economic disease burden (4–8). T2DM remains underdiagnosed and is often detected incidentally. Therefore, the discovery of vascular complications is common at the time of diagnosis (9). Thus, the American Diabetes Association as well as the European Society of Cardiology and the European Association for the Study of Diabetes now advocate screening for co‐morbidities at diagnosis of T2DM and assessment of cardiovascular risk in individuals with diabetes and pre‐diabetes (10, 11).
A comprehensive understanding of the impact of patients’ characteristics, risk factors and management patterns in terms of clinical outcomes and T2DM progression is needed to improve the quality of interventions and reduce the burden of T2DM. In Middle East and Africa (MEA) countries as in many regions, such data remain scarce (12, 13). Thus, the DISCOVER (DISCOVERing Treatment Reality of Type 2 Diabetes in Real World Settings) study was conducted with an aim to address these knowledge gaps by providing real-world observational data on patient characteristics, disease management patterns and clinical outcomes over 3 years in individuals with T2DM who are initiating a second-line glucose-lowering therapy (GLT).
Considering the paucity of data in MEA countries on the prevalence of T2DM-related vascular complications at an early stage of the disease, we report the data from the MEA cohort of the DISCOVER study on the prevalence of microvascular and macrovascular complications and associated factors in individuals with T2DM, using a standardised methodology. Data from the DISCOVER overall population has been published earlier (14).
Methods
Study design
DISCOVER is a 3-year observational, prospective, longitudinal study carried out across 38 countries (ClinicalTrials.gov identifiers: DISCOVER in 37 countries [NCT02322762] and J‐DISCOVER in Japan [NCT02226822]). The methods and statistical analysis have been described in detail elsewhere (14–16). The study was approved by the relevant ethical committee of each country and the Institutional Review Board of each site and was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation of Good Clinical Practice and other applicable clinical guidelines.
We present the baseline cross-sectional analysis of 12 countries (Algeria, Bahrain, Egypt, Jordan, Kuwait, Lebanon, Oman, Saudi Arabia, South Africa, Tunisia, Turkey and United Arab Emirates [UAE]) representing the DISCOVER-MEA cohort.
Patients with T2DM, recruited from primary and specialist healthcare settings, initiating a second-line GLT after a first-line oral monotherapy or combination (dual or triple) therapy were enrolled in routine clinical practice. Patients were excluded if they had type 1 diabetes, were pregnant or using an injectable agent as first-line treatment. Informed consent was obtained from all the patients participating in the study at each site. The eligibility criteria are detailed in Supplementary Table S1. Patients meeting the inclusion/exclusion criteria were consecutively recruited in the study (site selection in terms of types and investigators’ specialties was made to achieve representativeness of the way T2DM is managed in each participating country). The patients underwent clinical assessments and receive standard medical care as determined by their treating physicians. No investigational treatment or experimental intervention was provided as a part of the study.
The reporting of results in the manuscript is as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (17).
Data collection
Baseline data were collected using a standardized electronic case report form at the initiation of second‐line GLT and later transferred to a central database through a web-based data capture system. In addition to investigators’ characteristics, patients’ data regarding demographics, socioeconomic characteristics, physiological variables (blood pressure, pulse rate, body mass index [BMI]), laboratory parameters (glycated haemoglobin [HbA1c], total cholesterol, high‐density lipoproteins, low-density lipoproteins), duration of T2DM, first-line GLTs (received by patients before study baseline), second-line GLTs (prescribed at study baseline) and reason(s) for change in anti-diabetic therapy were collected at initiation of second-line therapy, co-medications, medical history and presence of comorbidities (including existing diabetes-related vascular complications) (14, 15).
Given the observational nature of the study, information with regard to clinical variables was collected as measured in routine clinical practice at each site, according to the local standard of care. Diagnosis and classification of complications relied on the judgement of investigators and there was no external independent adjudication of events.
The data on vascular complications included:
● Microvascular complications – nephropathy (presence of chronic kidney disease and/or albuminuria), retinopathy (history of retinopathy or retinal laser photocoagulation) and neuropathy (autonomic neuropathy, peripheral neuropathy and erectile dysfunction)
● Macrovascular complications – coronary artery disease (CAD) (history of CAD, angina, myocardial infarction [MI], percutaneous coronary intervention and coronary artery bypass grafting), cerebrovascular disease (stroke, transient ischaemic attack, carotid artery stenting and carotid endarterectomy), peripheral artery disease (history of peripheral artery disease including revascularisation procedures, diabetic foot and amputation), heart failure and implantable cardioverter-defibrillator use.
Patients who had experienced either micro or macrovascular disease prior to their T2DM diagnosis were not excluded. The overall and country-specific prevalence of micro and macrovascular complications and associated risk factors were evaluated.
Statistical methods
The statistical analysis conducted was similar to that of the DISCOVER global cohort‐Vascular complications manuscript (14). Multi‐variate Imputation by Chained Equations (MICE) R package was used to perform the missing value imputation. All statistical analyses were carried out using the RStudio (Boston, MA, USA). The descriptive data (sex, tobacco smoking, co‐morbidities, co‐medications and first-line GLTs) were presented as numbers and percentages for categorical variables; mean (standard deviation [SD]) values were reported for continuous variables. Crude prevalence rates of micro and macrovascular diseases and those standardised for age and sex using a regression model are reported.
A multi‐variate analysis using a modified Poisson model determined the odds ratios (ORs) for the factors that were associated with micro and macrovascular complications. Variables included in the analysis were: age (per 10-year increment), sex, smoking status, HbA1c, duration of T2DM (per 1-year increment), hyperlipidaemia, and hypertension; p<0.05 was considered to be statistically significant.
Results
Baseline characteristics
The sociodemographic characteristics and clinical data of 3,525 patients included in the MEA cohort are presented in Table 1. About half (52.5%) were males; the mean age of patients was 54.3 ± 10.8 years for the overall MEA cohort with comparatively higher age in patients recruited from Lebanon (59.2 ± 10.3 years); it was lower in Oman (41.8 ± 8.5 years). The mean duration of T2DM since diagnosis was 6.2 ± 5.4 years with the highest duration reported in Kuwait (10.9 ± 7.3 years) and the lowest in Egypt (4.1 ± 3.7 years). The baseline mean HbA1c for the overall MEA cohort was 8.7% ± 1.7 (median 8.3% [interquartile range: 7.6% to 9.4%]). Baseline HbA1c did not vary significantly across the countries (mean HbA1c range 8.3% to 9.0%). Among co‐morbidities, hypertension was reported in 43.2% (n=1,523) and hyperlipidaemia in 40.1% (n=1,413) of the patients in the overall MEA cohort. Bahrain and South Africa had a comparatively higher percentage of patients with hypertension (68.6% and 67.2%) while Kuwait (82.4%), Oman (77.4%), Bahrain (70.0%) and UAE (63.2%) had a higher percentage of patients with hyperlipidaemia compared to the overall cohort. Statins (42.3% [n=1,492]), angiotensin-converting enzyme inhibitors (ACEi; 33.6% [n=1,185]) and aspirin (22.4% [n=790]) were the most frequent co‐medications in the overall MEA cohort.
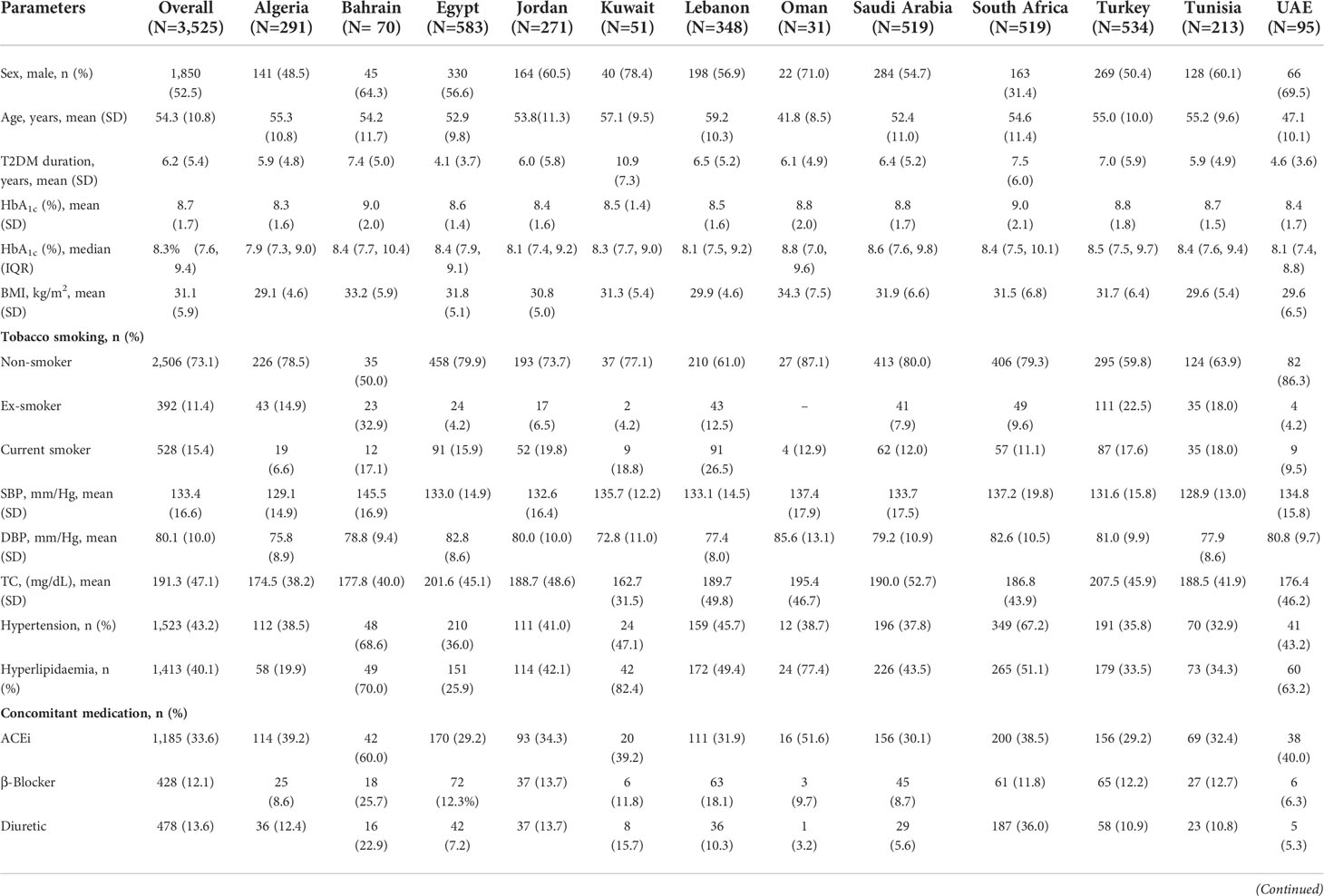
Table 1 Patient Demographics, Baseline Characteristics and Treatment Patterns, Overall and Country-wise.
As first-line GLTs, more than half (56.5% [n=1,990]) of the patients received metformin monotherapy, followed by dual therapy of metformin+sulphonylurea (SU) in 20.3% (n=714). In a country-wise analysis of first-line GLT, except for Oman (29.0%) and Kuwait (21.6%), metformin monotherapy was commonly prescribed as first-line GLT (range: 40.2% to 87.1%). In Oman and Kuwait, dual therapy of metformin+SU was the most prescribed treatment (58.1% and 33.3%) as first-line GLT, respectively. Except for Egypt, metformin+SU was the second most common GLT (range: 10.0% to 58.1%). In Egypt, SU monotherapy was the second most commonly prescribed (33.2%) GLT.
Prevalence of microvascular complications
The crude prevalence of microvascular complications in the overall MEA cohort was 17.7%; the age- and sex-standardised prevalence was 16.9% (95% confidence interval [CI], 16.77‐16.98) (Table 2). The country-wise crude prevalence of microvascular complications is shown in Supplementary Table S2 and the age- and sex-standardized prevalence are shown in Table 3. The age- and sex-standardized prevalence of microvascular disease was highest in Kuwait 28.6% (95% CI, 23.65-34.15), closely followed by Oman 28.0% (95% CI, 21.16‐35.97) and was lowest in Jordan 7.9% (95% CI, 7.50-8.37). Peripheral neuropathy was the most prevalent microvascular complication in the overall MEA cohort (crude prevalence: 8.2%; age- and sex-standardised prevalence: 7.8% [95% CI, 7.72‐7.87]). It was the most prevalent complication in Egypt (13.3%), Turkey (10.9%), Saudi Arabia (10.4%), Algeria (8.6%), South Africa (2.9%) and Jordan (2.8%). In Kuwait and Bahrain, retinopathy (15.0% and 4.3%) was the most prevalent complication. albuminuria (28.0%, 9.9% and 5.6%) in Oman, Tunisia and Lebanon respectively, while chronic kidney disease (CKD; 3.2%) in UAE, were the most prevalent.
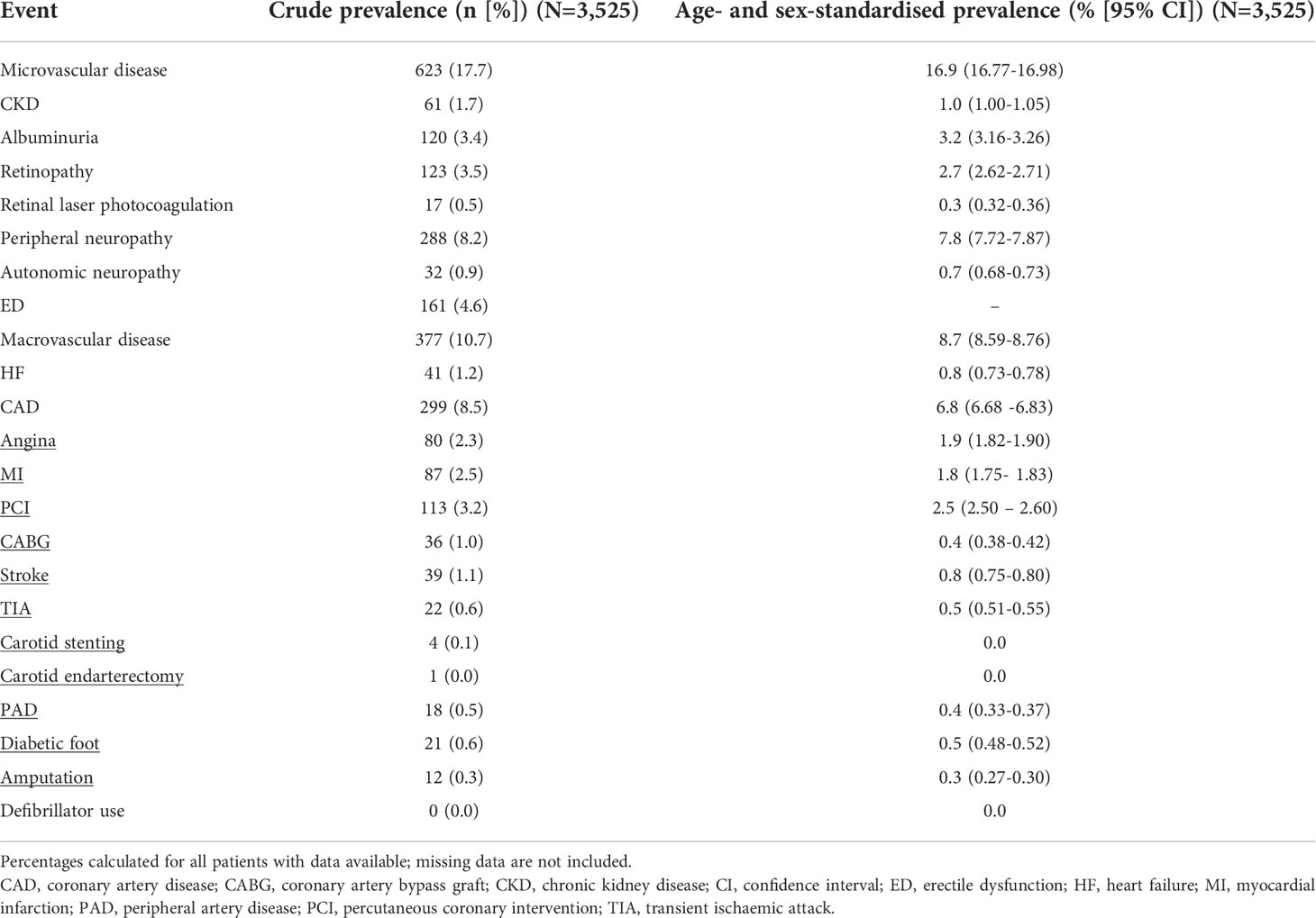
Table 2 Crude and Age- and Sex-Standardised Prevalence of Microvascular and Macrovascular Complications and Related Procedures at Baseline in Overall Cohort.
Prevalence of macrovascular complications
In the overall MEA cohort, for macrovascular complications, the crude prevalence was 10.7% and the age- and sex- standardized was 8.7% (95% CI, 8.59‐8.76) (Table 2). The crude as well as age- and sex-standardized prevalence was the highest for CAD (8.5% and 6.8% [95% CI, 6.68 to 6.83]) in the overall MEA cohort. The crude country-wise prevalence of macrovascular complications is shown in Supplementary Table S2 and the age- and sex-standardized prevalence are shown in Table 3. The age- and sex-standardized prevalence of macrovascular complications was the highest in Turkey at 14.4% (95% CI, 14.16‐14.71). CAD was the most prevalent complication in all countries (range: 2.7%‐11.6%).
Multi‐variable analysis
Table 4 and Figures 1A, B show the factors associated with micro and macrovascular complications. In the multi‐variable analysis, similar factors were associated with a higher prevalence of both micro and macrovascular complications. The factors significantly associated (p<0.05) were age per 10-year increment (microvascular: OR 1.24 [95% CI, 1.12‐1.39], macrovascular: OR 1.58 [95% CI, 1.35‐1.84]); male sex (microvascular: OR 1.33 [95% CI, 1.04‐1.70], macrovascular: OR 1.71 [95% CI, 1.22‐2.40]), history of hyperlipidaemia (microvascular: OR 1.33 [95% CI, 1.07‐1.65], macrovascular: OR 1.96 [95% CI, 1.46‐2.63]) and history of hypertension (microvascular: OR 1.75 [95% CI, 1.40‐2.19], macrovascular: OR 2.84 [95% CI, 2.07-3.92]). Apart from these factors, current smokers (OR 1.52 [95% CI, 1.01‐2.26]) and ex-smokers (OR 2.50 [95% CI, 1.72 to 3.61]) showed significant association with macrovascular complications (both p<0.05) compared with non-smokers. A multi‐variable analysis was not performed for individual countries due to small sample size.
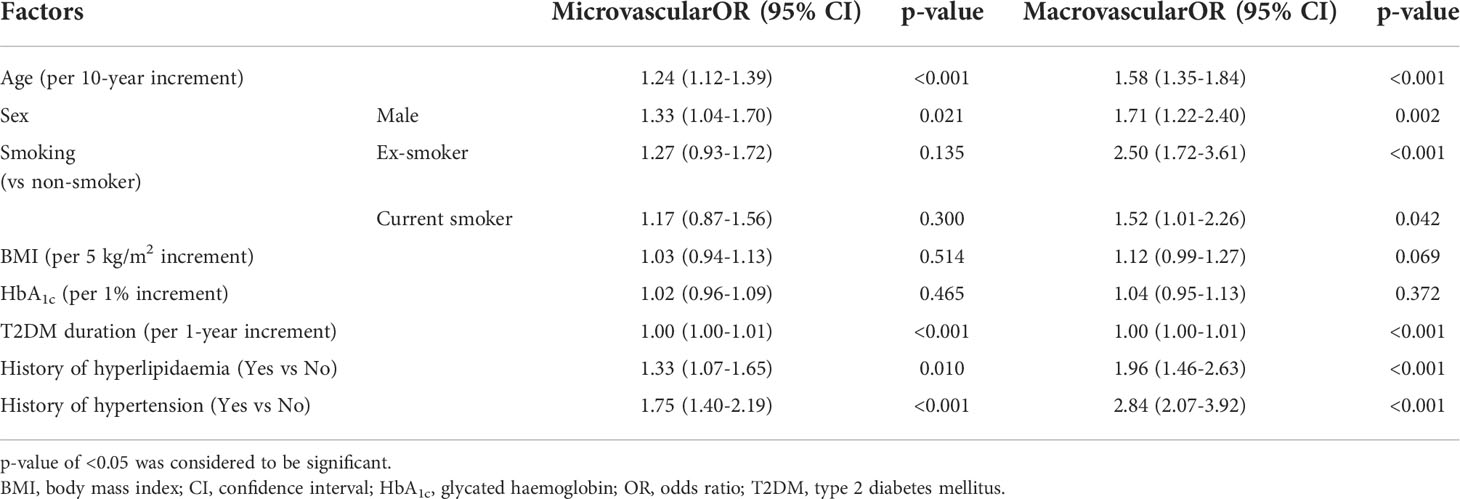
Table 4 Multi‐variable Analysis for Factors Associated With Microvascular and Macrovascular Complications.
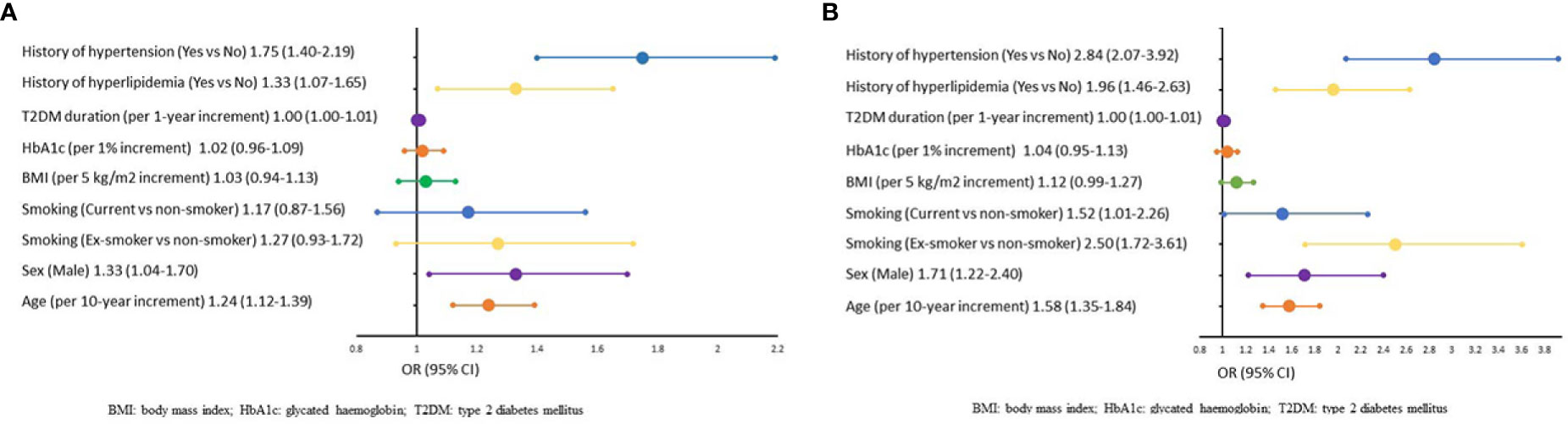
Figure 1 (A), Multi‐variable Analysis of Factors Associated With Microvascular Complications. BM, body mass index; HbA1c, glycated haemoglobin; T2DM, type 2 diabetes mellitus. (B), Multi‐variable Analysis of Factors Associated With Macrovascular Complications BMI, body mass index; HbA1c, glycated haemoglobin; T2DM, type 2 diabetes mellitus.
Discussion
This analysis focused on the prevalence of vascular complications and their potentially associated factors in individuals with T2DM initiating a second-line GLT in the MEA cohort of the DISCOVER study. We found the overall crude prevalence of microvascular and macrovascular complications to be 17.7% and 10.7%. The age- and sex-standardised prevalence of microvascular and macrovascular complications was 16.9% (95% CI, 16.77‐16.98) and 8.7% (95% CI, 8.59‐8.76), respectively. The prevalence varied markedly across the countries in MEA (Table 3A and Table 3B). Among microvascular complications, peripheral neuropathy was the most prevalent one with age- and sex-standardised prevalence of 7.8% (95% CI, 7.72‐7.87). CAD was the most prevalent macrovascular complication with age- and sex-standardised prevalence of 6.8% (95% CI, 6.68 to 6.83).
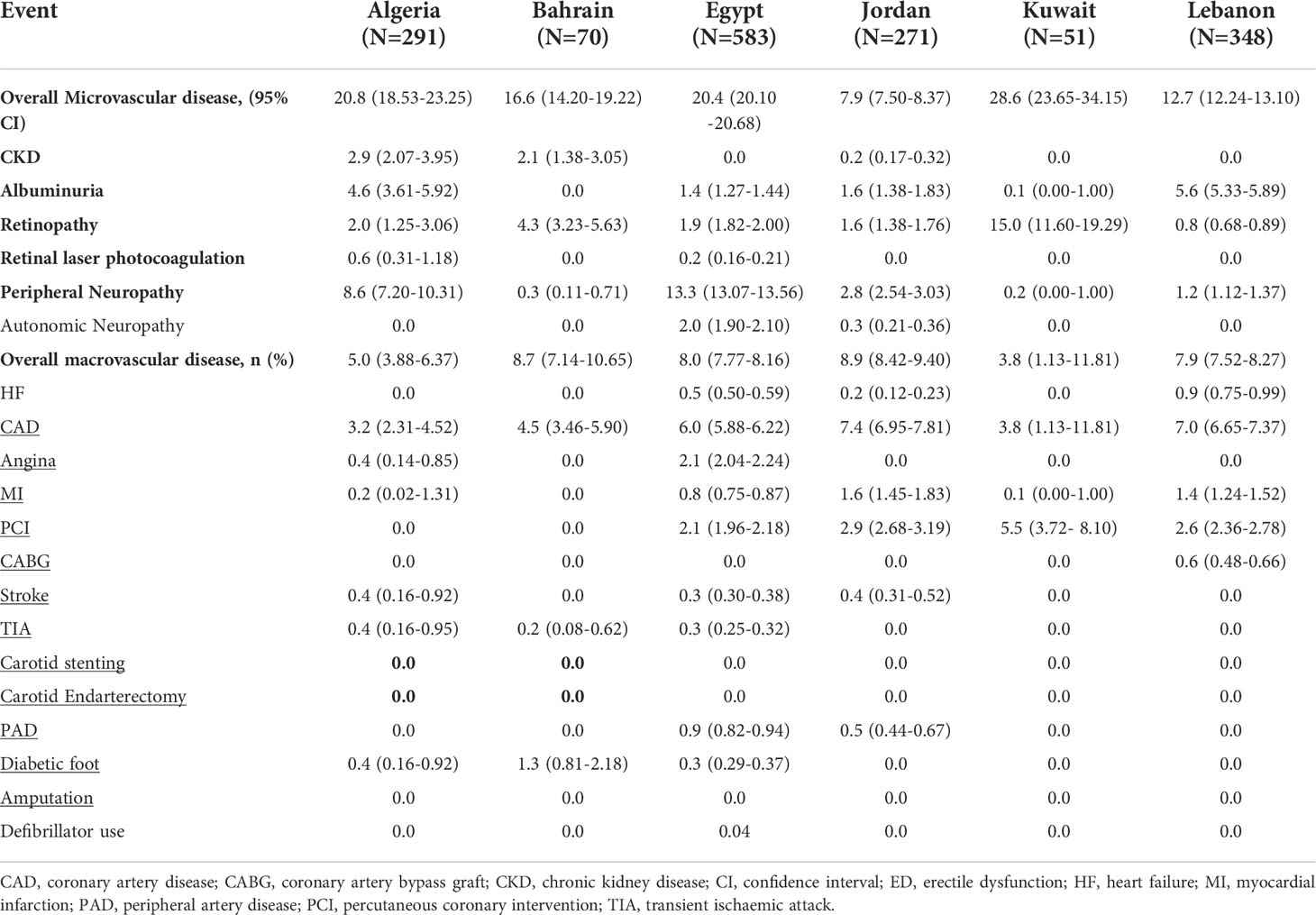
Table 3A Age- and Sex-standardised Prevalence of Microvascular and Macrovascular Complications, Country-wise.
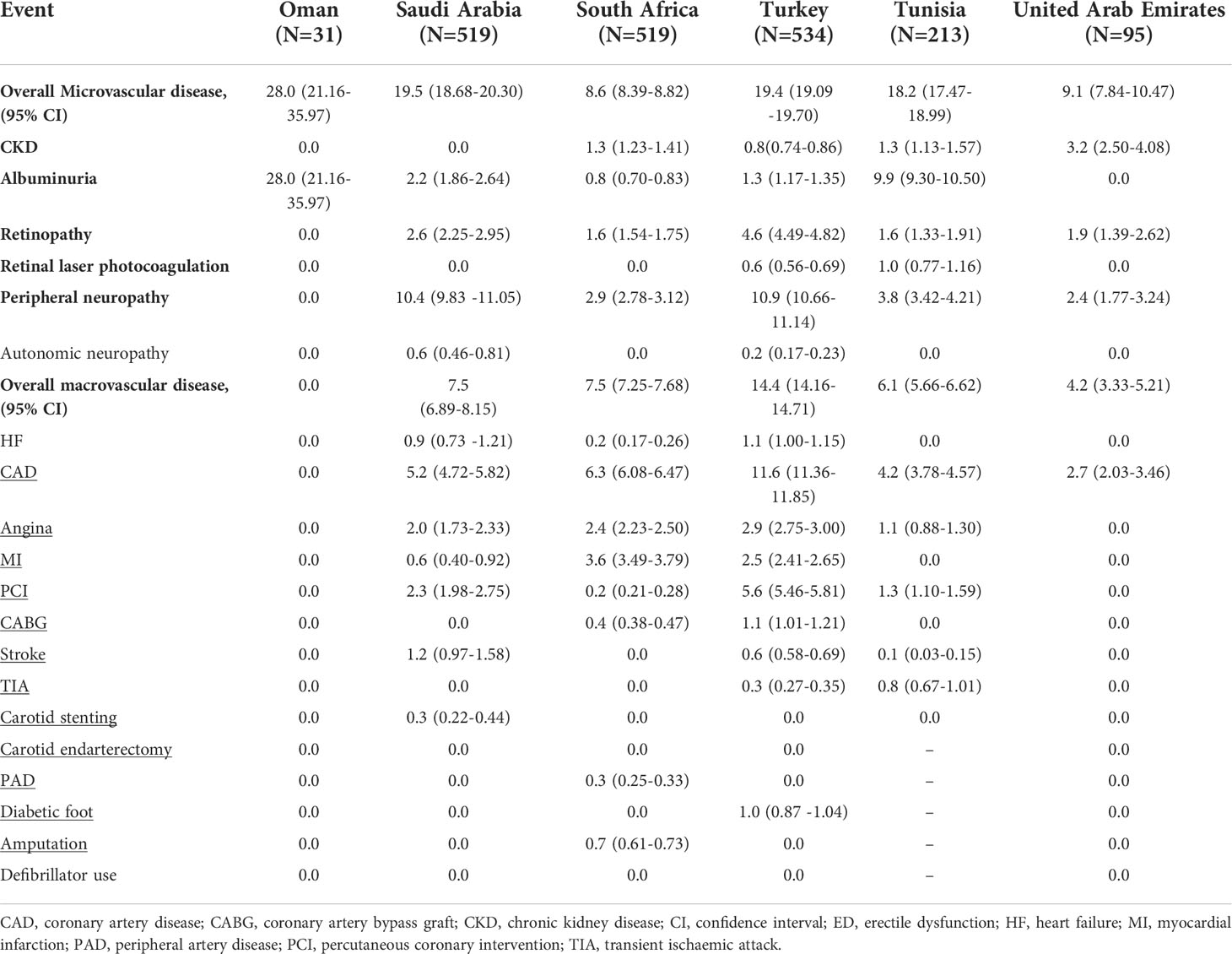
Table 3B Age- and Sex-Standardised Prevalence of Microvascular and Macrovascular Complications, Country-wise.
The standardised prevalence of vascular complications in MEA was similar to DISCOVER global data, which reported a prevalence of microvascular complications at 17.9% (95% CI, 17.3‐18.6) and macrovascular complications at 9.2% (95% CI, 8.7‐9.7) that varied across the regions (14).
This manuscript explored the crude prevalence of cardiovascular disease (CVD) in the MEA region, which is less than what has been observed in western countries as shown by global data, warranting further explanation (14). Of the 38 countries participating in the DISCOVER study, the MEA cohort comprised 12 countries accounting for almost one-fifth (22.1%) of the total DISCOVER population. Overall, the baseline characteristics and patients’ sociodemographics were similar across all the countries. Oman had a younger population (41.8 ± 8.5 years) compared with the MEA cohort (54.3 ± 10.8 years) as well as the global DISCOVER cohort (57.2 ± 12.0 years). The duration of T2DM was of 6.2 years, which was comparatively higher than the DISCOVER global data (5.6 years) (14). The duration of T2DM was the highest in Kuwait (10.9 ± 7.3 years) and lowest in Egypt (4.1 ± 3.7 years).
In line with the global data and as expected in patients who were moving to second-line therapy, mean HbA1c was above the target of 7.0% recommended by international (11, 18–20) as well as local guidelines (21–23). Based on the median HbA1c (8.3% [interquartile range: 7.6% to 9.4%]) values, more than 50% of patients for whom HbA1c was reported had levels above 8.0%, and >25% had a measurement higher than 9.0%. This suggests suboptimal glycaemic control and delayed treatment intensification increasing the risk of vascular complications.
More than 40% of patients in the MEA cohort had hyperlipidaemia and hypertension and most of them were prescribed statins and ACEis. A similar prevalence of hypertension and hyperlipidaemia was observed in cross-sectional studies from Saudi Arabia, Turkey and Jordan (24–27). In the VISION study, the prevalence of hypertension and dyslipidaemia in patients initiating insulin in the MEA region were 42.9% and 43.5% (28). In South Africa, analysis using medicine claims data reported a prevalence of 35.0% and 45.6% for hyperlipidaemia and hypertension respectively (29). All these studies confirm the high prevalence of two major risk factors for CVD in individuals with T2DM – hypertension and dyslipidaemia.
The prevalence of micro and macrovascular complications in people with T2DM has been evaluated in several studies. In the international, open-label, observational A1chieve study in more than 66,000 individuals with T2DM initiated on insulin across 28 countries from 4 continents (Asia, Africa, Europe and South America), the overall prevalence of micro and macrovascular complications was 53.5% and 27.2%, respectively compared with 65.8% and 28.7% for micro and macrovascular complications in the Middle East subgroup (30). Also, the Middle East cohort had younger patients with micro and macrovascular complications compared with the global A1chieve cohort. In a review of prevalence studies and cross‐sectional surveys published between 2007 to 2017, estimating the prevalence of CVDs in individuals with T2DM, though the prevalence of CVD in the MENA region was lower than global data (26.9% vs 32.2%), the prevalence of CAD (27.4% vs 21.2%) and MI (11.4% vs 10.0%) was higher (31). In the CAPTURE study evaluating the prevalence of CVD in individuals with T2DM, the prevalence of CVD were 18.0% in Saudi Arabia and 31.2% in Turkey (32).
In a retrospective cohort study in the United States reporting the prevalence of micro and macrovascular complications in 135 199 patients with newly diagnosed T2DM, the prevalence of CKD was 12.3%, peripheral neuropathy was 3.8% and composite CVD was 3.3% at diagnosis (33). A study from Italy in patients with newly diagnosed T2DM reported CVD in 11.2%, neuropathy in 18.6%, CKD in 8.8% and albuminuria in 13.2% of cases (34). In our MEA cohort, though the prevalence of CKD was not more than 1.0%, albuminuria was reported in 3.2% of patients. The prevalence of albuminuria was the highest in Oman (27.9%); however, due to the small sample size from Oman (n=31), the generalisation of this data is limited. Studies from the Middle East, Gulf and Africa region are limited; however, data from South Africa published in 1997 reported a prevalence of 15.6% for proliferative and preproliferative retinopathy, 27.6% for peripheral neuropathy and 36.7% for microalbuminuria after a mean diabetes duration of 8 years (35). Results from Saudi National Diabetes Registry reported a prevalence of 10.8% for nephropathy and 19.7% for retinopathy (36, 37). In the Gulf DiabCare survey conducted in Saudi Arabia, Kuwait and the UAE, from 1,290 individuals with T2DM, 34.9% of patients had neuropathy, 29.9% of patients had retinopathy, and <10% of patients had CVD and end-stage renal failure (38). In a study from Qatar, the prevalence of microvascular complications was 48.4% (500 of 1,034 patients) with 13.5% of patients presenting with more than one complication (39). Individuals with complications had lower age of onset, higher duration of T2DM and higher HbA1c compared with individuals without complications (all p<0.0001).
Results of our correlation analysis revealed a relationship between vascular complications and patients’ characteristics – age, male sex, smoking status, BMI, HbA1c, history of hyperlipidaemia and hypertension but the association was only significant with higher age, male sex, current/ex-smoking status, and history of hyperlipidaemia and hypertension (p<0.05). Micro and macrovascular complications were positively and significantly associated with the same risk factors but the ORs were higher for macrovascular complications. Additionally, we found that BMI and HbA1c were not significantly associated with either micro and macrovascular complications similar to that reported for the global DISCOVER study population macrovascular analysis but contrasts with microvascular one where HbA1c was found to be significantly associated (14). In a study from Qatar, similar risk factors for microvascular complications were reported along with other factors like family history, time in formal education, oral GLTs and hypertension (39).
In the A1chieve study, a multi‐variate analysis of the factors positively associated with micro and macrovascular complications were age, BMI, diabetes duration, total cholesterol, triglycerides and systolic blood pressure. High-density lipoproteins were negatively associated with macrovascular complications (30).
DISCOVER-MEA is the first prospective real-world study in this region evaluating the prevalence and risk factors for vascular disorders in patients with T2DM who have progressed to second-line therapy. Although the prevalence of micro and macrovascular disorders was similar to DISCOVER global data, the increasing prevalence of T2DM in the MEA region should be accounted for, for future strategies for the holistic management of T2DM. Outcomes-driven management of T2DM is needed for decreasing the risk of vascular complications.
The limitations of our study are those of real-world observational studies. The diagnosis of vascular disorders was not standardised across countries and thus, bias might have been introduced due to judgment by treating physicians. Also, small sample sizes for some countries did not allow for the exact interpretation of age- and sex-standardised prevalence and a multi‐variable analysis. Healthcare utilization is dependent on socioeconomic status which may impact access and hence reporting of vascular complications; however, this analysis was not undertaken for this manuscript because of limited data from most of the participating countries.
Conclusion
Despite having a short duration of T2DM, the MEA cohort had a substantial burden of vascular complications in patients mainly treated but suboptimally controlled with metformin and metformin+SUs. This increasing burden should be considered for formulating the strategies to manage T2DM. Early assessment of risk factors, cardiovascular risk status and preventive strategies should be adopted for effective management of T2DM in the MEA region.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was reviewed and approved by the relevant ethical committee of each country and the Institutional Review Board of each site and was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation of Good Clinical Practice, and other applicable clinical guidelines. The patients/participants provided their written informed consent to participate in this study.
Author contributions
The general content of the manuscript was agreed upon by all authors. All authors approved the final version of the manuscript before its submission. An AstraZeneca team reviewed the manuscript during its development and was allowed to make suggestions. The final content was determined by all the authors. The precise role of each author is as follows • Conceptualization: KH, RM, KR, AK, FB, AE, VR, AH • Data curation: KH, RM, KR, AK, FB, AE, VR, AH • Investigation: KH, RM, KR, AK, FB, AE • Methodology: KH, RM, KR, AK, FB, AE, VR, AH • Validation: KH, RM, KR, AK, FB, AE, VR, AH • Visualization, Writing, Review & editing: KH, RM, KR, AK, FB, AE, VR, AH.
Funding
The DISCOVER study program is funded by AstraZeneca. DISCOVER is a non‐interventional study and no drugs were supplied or funded.
Acknowledgments
The authors would like to thank all investigators and patients who participated in the DISCOVER study program. Medical writing support was provided by Prajakta Nachane, LabCorp Scientific Services & Solutions Pvt. Ltd, and was funded by AstraZeneca.
Conflict of interest
KH has received speaker fees and research support from AstraZeneca, Boehringer Ingelheim, Servier, Sanofi, Merck & Co., Novartis, Novo Nordisk, Pfizer, and Eli Lilly. RM has received honoraria as a speaker and a board member from Novo Nordisk, Sanofi, Eli Lilly, AstraZeneca, Merck, Novartis and Hikma. FB reports speaker honoraria and travel sponsorship from Bilim Ilaç, Abbott, Novo Nordisk, Sanofi Genzyme, Pfizer, and Eczacibasi Ilaç, and advisory board and consultancy fees from Novo Nordisk, Sanofi Genzyme, Abbott, Pfizer, and Bilim Ilaç. AE has received advisory board fees from AstraZeneca, Boehringer Ingelheim, Merck, and Novo Nordisk, and speaker fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Merck, Novartis, Novo Nordisk, and Sanofi. AK has received speaker and advisory board fees from Novo Nordisk, AstraZeneca, Merck & Co., Eli Lilly, Aspen Pharma, Sanofi, Boehringer Ingelheim, Cipla, Mylan, Pharmadynamics, Adcock Ingram, and Pfizer. AH and VR are employees of AstraZeneca.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This study received funding from AstraZeneca. AstraZeneca as funder had the following involvement with the study: study design, study management as per ICH GCP Sponsor responsibilities guidelines, decision to publish and the preparation of the manuscript. The data collection was performed by local CROs contracted by AstraZeneca and Data analysis was carried out by an independent academic centre (Mid America Heart Institute).
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.940309/full#supplementary-material
References
1. Standl E, Khunti K, Hansen TB, Schnell O. The global epidemics of diabetes in the 21st century: Current situation and perspectives. Eur J Prev Cardiol (2019) 26(2_suppl):7–14. doi: 10.1177/2047487319881021
2. International Diabetes Federation. IDF diabetes atlas. 9th edn. Brussels, Belgium: IDF Diabetes Atlas (2019). Available at: https://www.diabetesatlas.org.
3. El-Kebbi IM, Bidikian NH, Hneiny L, Nasrallah MP. Epidemiology of type 2 diabetes in the middle East and north Africa: Challenges and call for action. World J Diabetes (2021) 12:1401–25. doi: 10.4239/wjd.v12.i9.1401
4. Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, Schnell O, et al. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol (2019) 26:25–32. doi: 10.1177/2047487319878371
5. Visaria J, Iyer NN, Raval AD, Kong SX, Hobbs T, Bouchard J, et al. Healthcare costs of diabetes and microvascular and macrovascular disease in individuals with incident type 2 diabetes mellitus: A ten-year longitudinal study. Clin Outcomes Res CEOR (2020) 12:423–34. doi: 10.2147/CEOR.S247498
6. Mohammedi K, Woodward M, Marre M, Colagiuri S, Cooper M, Harrap S, et al. Comparative effects of microvascular and macrovascular disease on the risk of major outcomes in patients with type 2 diabetes. Cardiovasc Diabetol (2017) 16:95. doi: 10.1186/s12933-017-0574-y
7. Low Wang CC, Hess CN, Hiatt WR, Goldfine AB. Atherosclerotic cardiovascular disease and heart failure in type 2 diabetes – mechanisms, management, and clinical considerations. Circulation (2016) 133:2459–502. doi: 10.1161/CIRCULATIONAHA.116.022194
8. Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet Lond Engl (2006) 368:29–36. doi: 10.1016/S0140-6736(06)68967-8
9. Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J (2013) 34:2436–43. doi: 10.1093/eurheartj/eht149
10. American Diabetes Association. 4. comprehensive medical evaluation and assessment of comorbidities: Standards of medical care in diabetes-2020. Diabetes Care (2020) 43(Suppl 1):S37–47. doi: 10.2337/dc20-S004
11. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J (2020) 41:255–323. doi: 10.1093/eurheartj/ehz486
12. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
13. Farmanfarma KHK, Ansari-Moghaddam A, Zareban I, Adineh HA. Prevalence of type 2 diabetes in middle–East: Systematic review& meta-analysis. Prim Care Diabetes (2020) 14:297–304. doi: 10.1016/j.pcd.2020.01.003
14. Kosiborod M, Gomes MB, Nicolucci A, Pocock S, Rathmann W, Shestakova MV, et al. Vascular complications in patients with type 2 diabetes: prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc Diabetol (2018) 17:150. doi: 10.1186/s12933-018-0787-8
15. Ji L, Bonnet F, Charbonnel B, Gomes MB, Kosiborod M, Khunti K, et al. Towards an improved global understanding of treatment and outcomes in people with type 2 diabetes: Rationale and methods of the DISCOVER observational study program. J Diabetes Complications (2017) 31:1188–96. doi: 10.1016/j.jdiacomp.2017.03.011
16. Katakami N, Mita T, Takahara M, Hashigami K, Kawashima M, Shimomura I, et al. Rationale and design for the J-DISCOVER study: DISCOVERing the treatment reality of type 2 diabetes in a real-world setting in Japan-a protocol. Diabetes Ther Res Treat Educ Diabetes Relat Disord (2018) 9:165–75. doi: 10.1007/s13300-017-0351-7
17. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Stuart J Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Int J Surg (2014) 12:1500–24. doi: 10.1016/j.ijsu.2014.07.014
18. Association AD. 6. glycemic targets: Standards of medical care in diabetes–2021. Diabetes Care (2021) 44(Supplement 1):S73–84. doi: 10.2337/dc21-S006
19. Qaseem A, Barry MJ, Humphrey LL, Forciea MA, Fitterman N, Horwitch C, et al. Oral pharmacologic treatment of type 2 diabetes mellitus: A clinical practice guideline update from the American college of physicians. Ann Intern Med (2017) 166:279–90. doi: 10.7326/M16-1860
20. Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingroneet G, et al. Management of hyperglycaemia in type 2 diabetes, 2018. a consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetologia (2018) 61:2461–98. doi: 10.1007/s00125-018-4729-5
21. Shera AS, Basit A, Fawwad A. Middle East and north Africa region guidelines for the management of type 2 diabetes. J Diabetol (2019) 10:134–9. doi: 10.4103/jod.jod_43_18
22. Alawadi F, Abusnana S, Afandi B, Aldahmani KM, Alhajeri O, Aljaberi K, et al. Emirates Diabetes society consensus guidelines for the management of type 2 diabetes mellitus – 2020. Dubai Diabetes Endocrinol J (2020) 26:1–20. doi: 10.1159/000506508
23. Turkish Endocrinology And Metabolism Association. Guides. Available at: https://temd.org.tr/yayinlar/kilavuzlar (Accessed September 20, 2021).
24. Alzaheb RA, Altemani AH. Prevalence and associated factors of dyslipidemia among adults with type 2 diabetes mellitus in Saudi Arabia. Diabetes Metab Syndr Obes Targets Ther (2020) 13:4033–40. doi: 10.2147/DMSO.S246068
25. Bayram F, Kocer D, Gundogan K, Kaya A, Demir O, Coskun R, et al. Prevalence of dyslipidemia and associated risk factors in Turkish adults. J Clin Lipidol (2014) 8:206–16. doi: 10.1016/j.jacl.2013.12.011
26. Ahmed AM, Hersi A, Mashhoud W, Arafah MR, Paula CA, Al Rowaily MA, et al. Cardiovascular risk factors burden in Saudi Arabia: The Africa middle East cardiovascular epidemiological (ACE) study. J Saudi Heart Assoc (2017) 29:235–43. doi: 10.1016/j.jsha.2017.03.004
27. Khader YS, Batieha A, El-Khateeb M, Al Omari M, Ajlouni K. Prevalence of dyslipidemia and its associated factors among Jordanian adults. J Clin Lipidol (2010) 4:53–8. doi: 10.1016/j.jacl.2009.12.004
28. Jabbar A, Abdallah K, Hassoun A, Malek R, Senyucel C, Spaepen E, et al. Patterns and trends in insulin initiation and intensification among patients with type 2 diabetes mellitus in the middle East and north Africa region. Diabetes Res Clin Pract (2019) 149:18–26. doi: 10.1016/j.diabres.2019.01.017
29. Obeng-Kusi M, Lubbe MS, Cockeran M, Burger JR. Time-to-onset of treatment for hypertension and hyperlipidaemia in south African diabetes mellitus patients: A survival analysis using medicine claims data. J Clin Pharm Ther (2019) 44:701–7. doi: 10.1111/jcpt.12844
30. Litwak L, Goh SY, Hussein Z, Malek R, Prusty V, Khamseh ME. Prevalence of diabetes complications in people with type 2 diabetes mellitus and its association with baseline characteristics in the multinational A1chieve study. Diabetol Metab Syndr (2013) 5:57. doi: 10.1186/1758-5996-5-57
31. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol (2018) 17:83. doi: 10.1186/s12933-018-0728-6
32. Mosenzon O, Alguwaihes A, Leon JLA, Bayram F, Darmon P, Davis TME, et al. CAPTURE: a multinational, cross-sectional study of cardiovascular disease prevalence in adults with type 2 diabetes across 13 countries. Cardiovasc Diabetol (2021) 20:154. doi: 10.1186/s12933-021-01344-0
33. An J, Nichols GA, Qian L, Munis MA, Harrison TN, Li Z, et al. Prevalence and incidence of microvascular and macrovascular complications over 15 years among patients with incident type 2 diabetes. BMJ Open Diabetes Res Care (2021) 9(1):e001847. doi: 10.1136/bmjdrc-2020-001847
34. Bonora E, Trombetta M, Dauriz M, Travia D, Cacciatori V, Brangani C, et al. Chronic complications in patients with newly diagnosed type 2 diabetes: prevalence and related metabolic and clinical features: the Verona newly diagnosed type 2 diabetes study (VNDS) 9. BMJ Open Diabetes Res Care (2020) 8:e001549. doi: 10.1136/bmjdrc-2020-001549
35. Levitt NS, Bradshaw D, Zwarenstein MF, Bawa AA, Maphumolo S. Audit of public sector primary diabetes care in cape town, south Africa: high prevalence of complications, uncontrolled hyperglycaemia, and hypertension. Diabetes Med J Br Diabetes Assoc (1997) 14:1073–7. doi: 10.1002/(SICI)1096-9136(199712)14:12<1073::AID-DIA498>3.0.CO;2-9
36. Al-Rubeaan K, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Al-Mutlaq HM, et al. Diabetic nephropathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi national diabetes registry-based study. PloS One (2014) 9:e88956. doi: 10.1371/journal.pone.0088956
37. Al-Rubeaan K, Abu El-Asrar AM, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, et al. Diabetic retinopathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi national diabetes registry-based study. Acta Ophthalmol (Copenh) (2015) 93:e140–147. doi: 10.1111/aos.12532
38. Omar MS, Khudada K, Safarini S, Mehanna S, Nafach J. DiabCare survey of diabetes management and complications in the gulf countries. Indian J Endocrinol Metab (2016) 20:219. doi: 10.4103/2230-8210.176347
Keywords: macrovascular complication, Middle East and Africa, microvascular complications, risk factors, type 2 diabetes, vascular complication
Citation: Hafidh K, Malek R, Al-Rubeaan K, Kok A, Bayram F, Echtay A, Rajadhyaksha V and Hadaoui A (2022) Prevalence and risk factors of vascular complications in type 2 diabetes mellitus: Results from discover Middle East and Africa cohort. Front. Endocrinol. 13:940309. doi: 10.3389/fendo.2022.940309
Received: 10 May 2022; Accepted: 20 July 2022;
Published: 09 August 2022.
Edited by:
Sathish Thirunavukkarasu, Emory University, United StatesReviewed by:
Aswathy Sreedevi, Amrita Institute of Medical Sciences and Research Centre, IndiaMary Chandrika Anton, Sree Balaji Medical College and Hospital, India
Copyright © 2022 Hafidh, Malek, Al-Rubeaan, Kok, Bayram, Echtay, Rajadhyaksha and Hadaoui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Khadija Hafidh, a2hhZGlqYS5oYWZpZGhAZ21haWwuY29t
 Khadija Hafidh
Khadija Hafidh Rachid Malek
Rachid Malek Khalid Al-Rubeaan
Khalid Al-Rubeaan Adri Kok4
Adri Kok4 Ahmed Hadaoui
Ahmed Hadaoui