
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 29 July 2022
Sec. Obesity
Volume 13 - 2022 | https://doi.org/10.3389/fendo.2022.922312
This article is part of the Research TopicAssociation of Novel Anthropometric Indexes with Metabolic Syndrome and Beyond, volume IIView all 16 articles
 Ming-Shyan Lin1,2,3
Ming-Shyan Lin1,2,3 Huang-Shen Lin2,4
Huang-Shen Lin2,4 Ming-Ling Chang5
Ming-Ling Chang5 Ming-Horng Tsai6
Ming-Horng Tsai6 Yung-Yu Hsieh7
Yung-Yu Hsieh7 Yu-Sheng Lin1,2
Yu-Sheng Lin1,2 Meng-Shu Tsai1
Meng-Shu Tsai1 Chia-Ling Yang1
Chia-Ling Yang1 Mei-Yen Chen1,3,8*
Mei-Yen Chen1,3,8*Background: The serum aminotransferase elevation in metabolic syndrome (MetS) reflected hepatosteatosis, but there is a conflict with the coexistence of viral hepatitis, especially for the hepatitis B virus (HBV). Thus, this study aimed to investigate the relationship between the alanine aminotransferase (ALT)/aspartate aminotransferase (AST) ratio, MetS, and HBV infection in a rural Taiwanese population.
Methods: We conducted a cross-sectional analysis in southern Taiwan between March and December 2019. Multivariable logistic regression analyses adjusted for demographics, education, dietary behaviors, irregular exercise, substance use, and viral markers were performed to investigate the association between the ALT/AST ratio and MetS.
Results: Altogether, 2,416 participants (891 men and 1,525 women; mean age, 64.1 ± 14.9 years) were enrolled. Of the participants, 22.7% (n = 519) were seropositive for viral hepatitis. In the multivariable analysis, age [odds ratio (OR) 1.02, 95% CI 1.01–1.03, p < 0.001], ALT/AST ratio >1 (OR 2.63, 95% CI 2.15–3.21, p < 0.001), education (OR 0.96, 95% CI 0.94–0.98, p < 0.001), and HBV seropositivity (OR 0.70, 95% CI 0.52–0.95, p = 0.021) were associated with the risk of MetS. The area under the curve of the ALT/AST ratio was 0.62 (95% CI 0.60–0.64, p < 0.001), and the cutoff value was >0.852 for the Youden index.
Conclusion: An ALT/AST ratio >1 could be a simple index for MetS prediction during community checkups. In contrast to age and betel nut chewing, HBV seropositivity and higher education might be inversely associated with MetS. Aggressive health promotion for MetS prevention has emerged as essential in participants without HBV and with lower education levels. Further large-scale, longitudinal studies are needed to unlink these correlations.
Metabolic syndrome (MetS) is hypervalent (13.6% to 30.1%) in southern Taiwan (1), which is also a viral hepatitis endemic area. Twelve percent to 15% of the adult population infected with hepatitis B virus (HBV) remains hepatitis B surface antigen (HBsAg)-positive (2), and the prevalence of hepatitis C virus (HCV) seropositivity is remarkably high (overall 2%–4% in Taiwan). Although HCV independently increases the MetS burden (1, 3), the association between HBV and MetS is diverse (4–7). Central obesity and fatty liver have emerged as significant components of MetS, while steatohepatitis increases the mortality risk in the population (8, 9). Both viral hepatitis and fatty liver could induce abnormal alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels (3, 7), the data of which can be obtained from community checkups. Moreover, the predictive effect of aminotransferases on MetS may be influenced by viral hepatitis and lifestyle factors, including diet, exercise, and personal habits.
Serum aminotransferases increase along with being overweight [body mass index (BMI) ≥ 25 kg/m2] or obese (BMI ≥ 30 kg/m2), although this is more prominent for ALT than for AST. After complete viral suppression in patients infected with HBV, ALT elevation indicated high BMI [adjusted odds ratio (OR) 1.78; 95% confidence interval (CI) 1.02–3.11] (10), and ALT levels were significantly higher in chronic HBV infection with MetS (7). In contrast to the De Ritis ratio (AST/ALT ratio > 2.0) for alcoholic hepatitis and >1.0 for cirrhosis/fibrosis (11), and ALT/AST ratio >1 could be independently associated with MetS (12, 13) and fatty liver disease (14, 15). The index might offer more predictive power when considering more confounders, including lifestyle variables and viral hepatitis.
Although aminotransferase can be easily checked during routine examinations, whether the ALT/AST ratio has a predictive impact on MetS in viral hepatitis endemic areas remains unknown. Thus, we aimed to investigate the relationship between the ALT/AST ratio, MetS, and HBV infection in a rural Taiwanese population.
This cross-sectional study included adult patients who participated in annual checkups from March to December 2019 in rural communities in southern Taiwan. We collected patient data on personal health habits, laboratory results, and viral markers of hepatitis. All participants signed an informed consent form and completed a questionnaire. After excluding those with incomplete data, 2,416 participants were enrolled in the final analysis (Figure 1). This study was approved by the Institutional Review Board and Ethics Committee of Chang Gung Memorial Hospital (IRB No. 201900222A3). According to a previous study reporting the correlation between the presence/absence of MetS and the ALT/AST ratio, the mean (standard deviation) ALT/AST ratio was 1.29 (0.42) and 1.09 (0.41) in men with and without MetS, respectively (16). The mean (standard deviation) ALT/AST ratio was 1.10 (0.35) and 0.87 (0.35) in women with and without MetS, respectively (16). Considering a type I error rate of 1% and power of 99%, a minimum sample size of 418 men and 226 women was required.
The questionnaire on lifestyle and demographic characteristics, including sex, age, and educational level (number of years of education received), were included. Participants were asked the following questions regarding three substances and four healthy habits: “Do you smoke cigarettes, chew betel nuts, and regularly consume alcohol or alcohol-related beverages?” Participants were classified as “non-users” if they reported having never smoked, chewed, or drunk and “current/former users” if they reported being current users or previous users who had ceased chewing or smoking. Regarding diet, they were asked the following: “How often do you consume three portions of vegetables (1.5 bowls)? Two portions of fruit (one bowl)? Water intake of at least 1,500 ml per day?” and “How often do you have exercise, for at least >30 min, three times per week?” Responses were categorized as “never,” “seldom,” “usually,” or “always.” For the evaluation, four responses were categorized into two-level frequencies: no—never/seldom and yes—usually/always.
Waist circumference was measured using a soft tap and defined at the umbilical level while standing without stress for a moment (17). For blood pressure measurements, all participants underwent two measurements via anthropometric equipment in the sitting position after 10 min of rest, and the mean arterial pressure (systolic and diastolic) was recorded (18).
Blood samples were obtained after fasting for 12 h and tested in the laboratory of the CGMH Hospital. Biochemical tests included serum AST, ALT, TG, LDL-C, HDL-C, TC (Roche Diagnostics, Cobas6000, C501, Germany), and HbA1c (Trinity Biotech, Premier, HB9210, USA). Hepatitis B surface antigen (HBsAg) was detected using routine standard ELISA (General Biological Corp., Hsinchu, Taiwan), and the anti-HCV antibody was evaluated using SP-NANBASE C-96 3.0 plate (General Biological Corp).
MetS was diagnosed based on the modified qualitative criteria of the International Diabetes Federation definition (19), requiring the presence of three or more of the following five criteria: 1) waist circumference >90 cm in men or >80 cm in women for Asians, 2) TG >150 mg/dl, 3) HDL-C <40 mg/dl in men or <50 mg/dl in women, 4) blood pressure >130/85 mmHg or current use of antihypertensive medications, and 5) glycohemoglobin (HbA1c) >5.7 or use of oral antidiabetic agents or insulin.
The demographic characteristics of the participants with different HBV and HCV statuses (none, HBV only, HCV only, and co-infection) were compared using the chi-square test for categorical variables and the independent sample t-test for continuous variables. Pairwise comparisons using the Bonferroni correction were performed when the overall test results were significant. We also compared the demographic characteristics between the MetS and non-MetS groups using the chi-square test for categorical variables and the independent sample t-test for continuous variables. Using the demographics/characteristics as explanatory variables, a series of univariate logistic regression analyses were performed to initially screen the potentially associated factors of MetS. The multivariable logistic regression model further included variables with significance levels <0.15 (20). Among the indicators of liver function (AST, ALT, and ALT/AST ratio > 1), ALT/AST ratio >1 was selected in the multivariable model to prevent multicollinearity. Finally, a receiver operating characteristic (ROC) curve analysis was conducted to evaluate the ability of the ALT/AST ratio to discriminate the presence of MetS. All tests were two-tailed, and a p-value <0.05 was considered significant. Data analyses were performed using SPSS version 25 (IBM SPSS Inc., Chicago, IL, USA).
Table 1 presents the demographics and characteristics of the 2,416 participants who completed the health examination and the questionnaire. The mean age of the participants was 64.1 years [standard deviation (SD) 14.9 years], with 56.1% being >65 years. Women were predominant (63.1%). Nearly one-fourth of the participants (n = 548, 22.7%) were seropositive for viral hepatitis, of whom 213 (8.8%) had HBV, 306 (12.7%) had HCV, and 29 (1.2%) were co-infected with HBV and HCV. Approximately 70% of the participants did not exercise regularly, and the distribution difference among all subgroups was insignificant. Compared to HCV patients, those with HBV seropositivity were younger (61.1 ± 12.3 vs. 70.8 ± 10.0 years), had lower education levels (7.7 vs. 3.9 years), and had more alcoholic drinking but less betel nut chewing. Half of the participants (n = 1,262, 52.2%) had MetS. The HBV seropositive patients had fewer MetS components and a lower risk of MetS than HCV seropositive patients (41.8% vs. 58.8%). The participants with co-infection had higher ATL and AST levels than the other subgroups (p < 0.001), whereas the proportion of patients with an ALT/AST ratio >1 was slightly lower in the HCV subgroup.
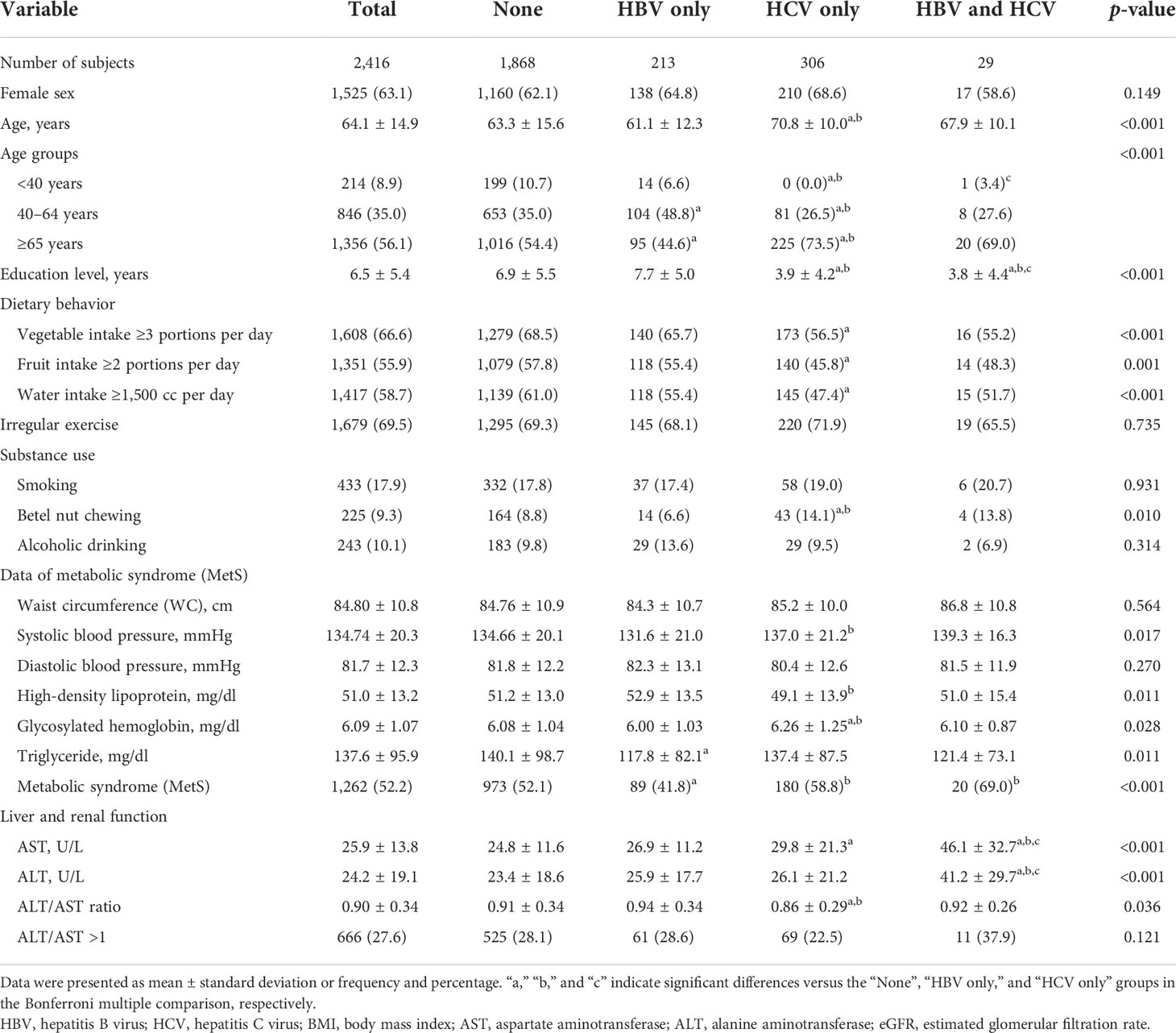
Table 1 Demographics and characteristics of the study subjects according to the HBV and HCV status (N = 2,416).
Table 2 presents the demographics and characteristics of participants with and without MetS. Compared to the patients without MetS, those with MetS were older (67.0 ± 12.8 vs. 61.0 ± 16.4 years, p < 0.001), had lower education levels (5.5 ± 5.1 vs. 7.7 ± 5.6 years, p < 0.001), had less fruit intake at ≥2 portions per day (53.2% vs. 58.9%, p = 0.004), were more likely to do betel nut chewing (11.1% vs. 7.4%, p = 0.002), had significantly positive data of individual MetS components, and had higher AST (27.4 ± 15.8 vs. 24.2 ± 11.0, p < 0.001) and ALT levels (27.1 ± 21.0 vs. 21.0 ± 16.2 U/L, p < 0.001). The MetS group had a significantly higher ALT/AST ratio >1 (34.2% vs. 20.4%, p < 0.001) and higher proportion of HCV seropositivity (14.3% vs. 10.9%) than the non-MetS group. Meanwhile, the prevalence of HBV seropositivity was higher in the non-MetS group than in the MetS group (10.7% vs. 7.1%).
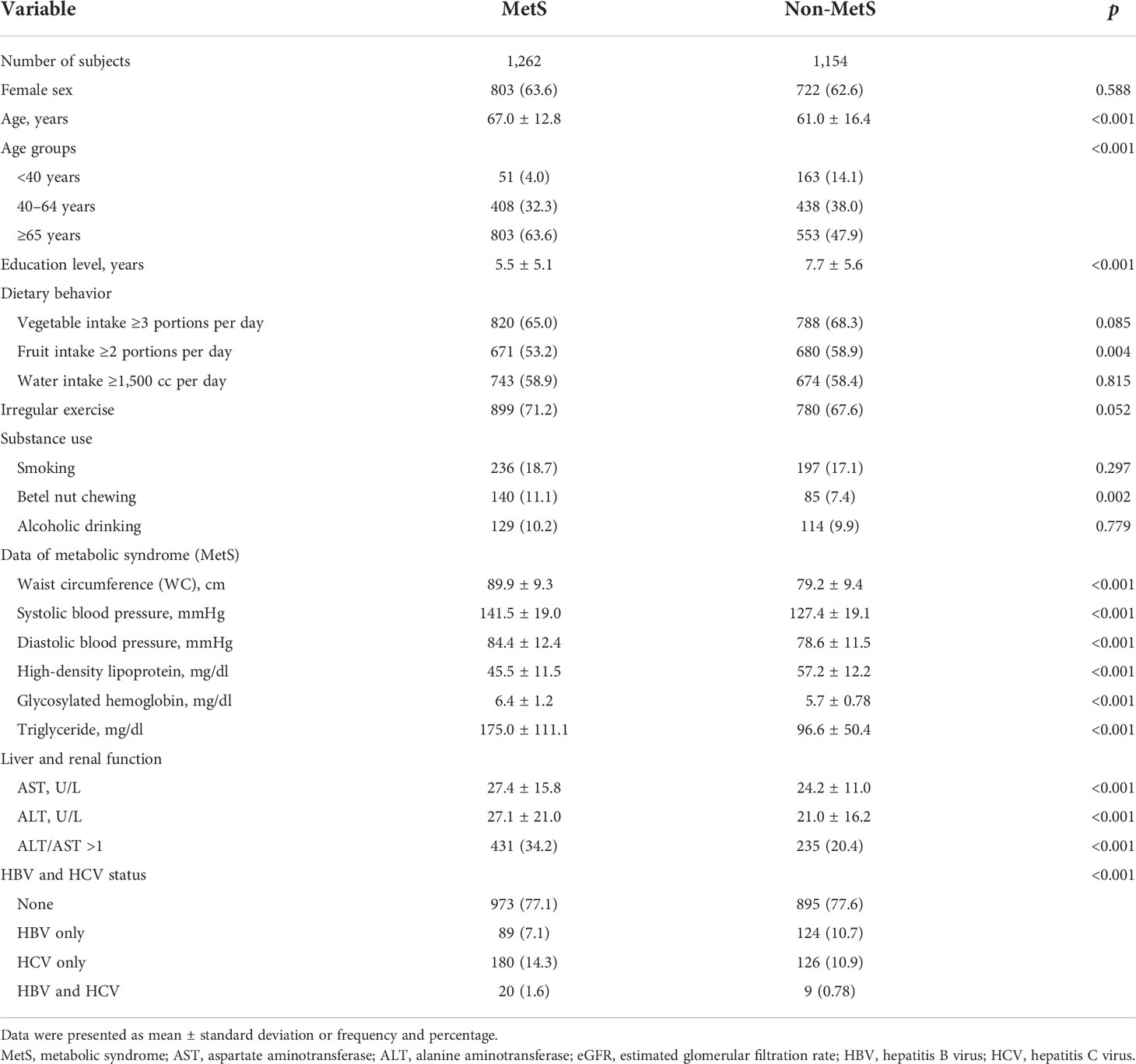
Table 2 Demographics and characteristics of the study subjects according to the status of MetS (N = 2,416).
The univariate logistic regression analyses revealed that the following covariates might be associated with MetS: age, education level, fruit intake, betel nut chewing, AST level, ALT level, ALT/AST ratio >1, and seropositivity to HBV and HCV (Table 3). After incorporating the variables whose significant levels were <0.15 in the univariate analyses, the multivariable model identified that older age (OR 1.02, 95% CI 1.01–1.03) and the presence of ALT/AST ratio >1 (OR 2.63, 95% CI 2.15–3.21) were significantly associated with a greater risk of MetS. By contrast, a high education level (OR 0.96, 95% CI 0.94–0.98) and HBV seropositivity (OR 0.70, 95% CI 0.52–0.95) were also significantly inversely related to the risk of MetS. Additionally, betel nut chewing was associated with a higher risk of MetS (OR 1.41, 95% CI 1.05–1.90).
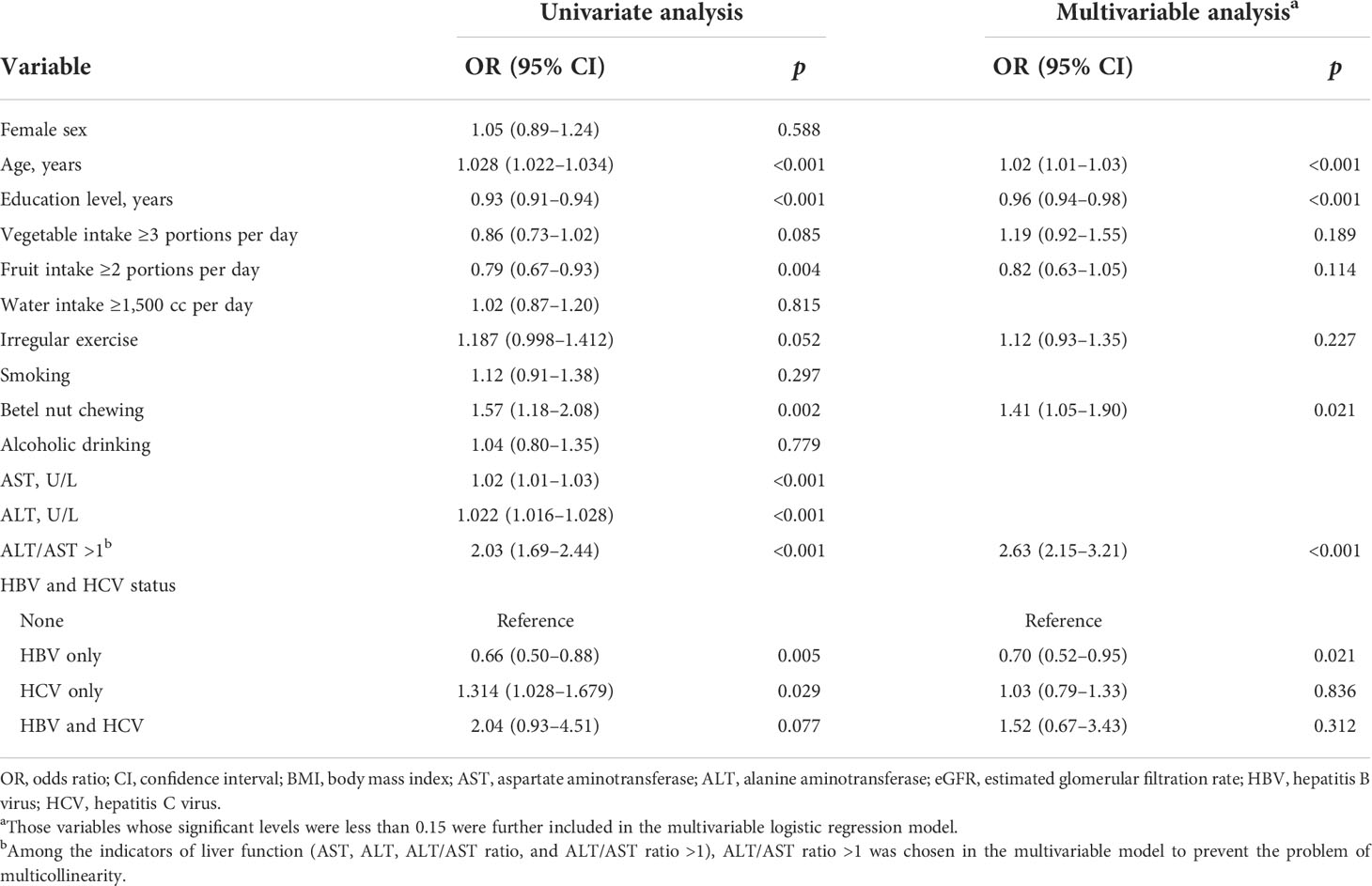
Table 3 Association between demographics/characteristics and the risk of metabolic syndrome (N = 2,416).
Due to the presence of an ALT/AST ratio >1 as an associated factor for MetS, we assessed its ability to discriminate the presence of MetS. The results revealed a modest discrimination performance with an area under the ROC curve of 61.8% (95% CI 59.5%–64.0%). The derived optimal cutoff determined by the Youden index was >0.852, with a sensitivity of 56.7% (95% CI 53.9%–59.4%) and a specificity of 62% (95% CI 59.1%–64.8%) (data not shown).
This community-based participatory research investigates MetS-related factors, including diet, exercise, and education, and uses the ALT/AST ratio as a predictive index for MetS. Our findings suggest that an ALT/AST ratio >1 might increase the risk of MetS (OR 2.63), whereas high education and HBV seropositivity are inversely associated with MetS. The effects of the ALT/AST ratio and HBV seropositivity on MetS prediction differed. High ALT levels were significantly associated with MetS in women (21) and reflected central obesity with advanced steatohepatitis. In this study, an ALT/AST ratio >1 could be a simple index to predict MetS by considering all dietary content, healthy behaviors, and education, especially in viral hepatitis endemic areas. The diverse effects of the ALT/AST ratio and HBV seropositivity might exhibit unlinked pathophysiologies, such as hepatosteatosis or hepatic fibrosis in MetS.
Although serum viral load, AST, and ALT levels were independent predictors of histological grade (22), a single ALT or AST test could not offer a strong association between MetS and abnormal liver function, especially in patients with viral hepatitis. Chen et al. have also reported that men had a three times higher risk of MetS than women, who had fewer metabolic abnormalities and elevated ALT levels (12). The ALT/AST ratio is straightforward and feasible for use in community health examinations. The index can be presented as either hepatic fibrosis or steatosis in different studies (13–15). A previous study has reported that a higher ALT/AST ratio is associated with insulin resistance in metabolically unhealthy Korean individuals (13). Moreover, ALT/AST ratio >1 was significantly associated with MetS in the Thai population (16); however, variables correlated with lifestyle and viral hepatitis were absent. Here, the ALT/AST ratio was independently associated with MetS. Zhao et al. have reported that the ALT/AST ratio could predict insulin resistance and MetS among the Chinese population (23), although this was not the case in our study, which had a high proportion of viral hepatitis. A high ALT/AST ratio is associated with fatty liver, a significant component of MetS, hypertriglyceridemia, and steatohepatitis.
Our findings further demonstrate that HBV infection is inversely associated with MetS, which is consistent with the findings of previous studies. Significant hepatic impairment in co-infection with HBV/HCV was observed, but patients with HBV had minor liver dysfunction, were younger, and had a higher education level (7.7 ± 5.0), healthy dietary behavior, and less betelnut chewing. Kuo et al. have reported that HBV infection was inversely associated with MetS only in lean patients (p = 0.002) but not in the general population (1). Joo et al. have reported that HBsAg seropositivity in Korean adults was associated with a lower risk of developing non-alcoholic fatty liver disease (NAFLD), indicating a possible effect of HBV infection on the pathogenesis of NAFLD in a cohort study (24). A body of evidence has also indicated that patients with chronic hepatitis B (CHB) have a lower incidence of NAFLD and steatohepatitis. A possible mechanism is that HBV viral activity might protect against hepatic steatosis and metabolic disturbances. The severity of steatosis was inversely associated with HBV viral load (25, 26). In an animal model, steatosis inhibited HBV replication by reducing HBV DNA and HBV-related antigens (27).
Nevertheless, patients with CHB with coexisting components of MetS are associated with more severe liver diseases. Li et al. have reported that fatty liver was significantly associated with higher HBsAg seroclearance in patients with CHB (28), while concurrent NAFLD might inhibit HBV replication and promote HBsAg seroclearance (29). However, the fatty liver also exacerbates liver fibrosis. Khalili et al. have reported that MetS was prevalent in this HBV group and independently associated with higher ALT levels (7). Moreover, Cai et al. have reported that HBV comorbidity with fibrosis increases the MetS component burden (30), and Yan et al. discovered that cirrhosis is prevalent in HBV with MetS (4.83% vs. 2.93%, compared with non-MetS; p = 0.002) (6). Additionally, Chan et al. revealed that overweight and concurrent fatty liver disease are associated with increased mortality risk and hepatocellular carcinoma in patients with CHB (31). Chien et al. have reported that patients who were unaware of their hepatitis B infection tended to have a higher risk of central obesity, hyperglycemia, insulin resistance, and MetS than those who were aware of their hepatitis B infection (OR 1.85, p < 0.05). In patients without MetS, HBV with MetS has a higher ALT level and ALT/AST ratio, suggesting a prominent hepatic inflammation and a predictor of steatohepatitis.
In addition to health promotion, regular physical exercise, cessation of alcohol or betelnut consumption, good dietary habits, aggressive follow-up, and early detection using the ALT/AST ratio may reduce MetS or steatohepatitis burden in chronic HBV infection/carriers.
This study had several inherent limitations in its cross-sectional design. First, details of the hepatobiliary disease, fatty liver, antiviral therapeutic response, and viral load/activity were unavailable in the research. Nevertheless, the early implementation of HBV vaccination may influence personal lifestyles, behaviors, and insight for disease screening. Second, we lacked the sequential results of aminotransferase levels and detected all the factors influencing liver function. Although the ALT/AST ratio could not reflect an accurate level, the index is a different part of hepatic injury. Third, we could not obtain details of personal health conditions and medications associated with hepatic function. Finally, many non-invasive waist-to-height ratios or echography approaches could be used for predicting MetS (32, 33); however, interoperator variability and infeasible devices in community checkups limit their clinical application.
An ALT/AST ratio >1 is independently associated with MetS after adjusting for age, lifestyle, education level, and viral hepatitis seropositivity. Although HBV seropositivity and higher education are inversely associated with MetS, the ALT/AST ratio remains a reliable predictor of MetS and a simple index for community checkups. Nevertheless, the corresponding biological mechanisms of HBV in MetS remain to be elucidated, and future large-scale studies are needed to survey this association.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author/s.
This study was reviewed and approved by The Institutional Review Board approved the study (IRB NO: 201900222A3). Written informed consent was obtained from individual or guardian participants. The patients/participants provided their written informed consent to participate in this study.
All authors contributed to the statistical analysis and writing of the study. M-SL, H-SL, and M-YC participated in the study design, data acquisition, and critical review and wrote the manuscript. M-LC, M-HT, and Y-YH participated in the analysis and interpretation of data. Y-SL, M-ST, and C-LY collected the data and contributed to the study direction. All authors contributed to the article and approved the submitted version.
The study was supported by a grant from Taiwan Formosa Plastic Group (FCRPF6L0011). The authors thank Mr. Alfred Hsing-Fen Lin, M.S., and Mrs. Bing-Yu Chen, Ph.D., for their statistical analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kuo YH, Kee KM, Wang JH, Hsu NT, Hsiao CC, Chen Y, et al. Association between chronic viral hepatitis and metabolic syndrome in southern Taiwan: a large population-based study. Aliment Pharmacol Ther (2018) 48(9):993–1002. doi: 10.1111/apt.14960
2. Liu CJ, Chen PJ. Elimination of hepatitis b in highly endemic settings: Lessons learned in Taiwan and challenges ahead. Viruses (2020) 12(8):815. doi: 10.3390/v12080815
3. Lin MS, Lin HS, Chung CM, Lin YS, Chen MY, Chen PH, et al. Serum aminotransferase ratio is independently correlated with hepatosteatosis in patients with HCV: a cross-sectional observational study. BMJ Open (2015) 5(9):e008797. doi: 10.1136/bmjopen-2015-008797
4. Razi B, Alizadeh S, Omidkhoda A, Imani D, Rezaei R. Association of chronic hepatitis b infection with metabolic syndrome and its components: Meta-analysis of observational studies. Diabetes Metab Syndr (2017) 11 Suppl 2:S939–47. doi: 10.1016/j.dsx.2017.07.020
5. Chien CH, Chen LW, Lin CL, Chang SW, Shyu YC, Chen KF, et al. Unawareness of hepatitis b virus infection confers on higher rate of metabolic syndrome: a community-based study. Sci Rep (2017) 7(1):9869. doi: 10.1038/s41598-017-10029-2
6. Khalili M, Shuhart MC, Lombardero M, Feld JJ, Kleiner DE, Chung RT, et al. Relationship between metabolic syndrome, alanine aminotransferase levels, and liver disease severity in a multiethnic north American cohort with chronic hepatitis b. Diabetes Care (2018) 41(6):1251–9. doi: 10.2337/dc18-0040
7. Yan LB, Liao J, Han N, Zhou LY, Wang XE, Wang YJ, et al. Association between hepatitis b virus infection and metabolic syndrome in southwest China: A cross-sectional study. Sci Rep (2020) 10(1):6738. doi: 10.1038/s41598-020-62609-4
8. Kim HR, Han MA. Association between serum liver enzymes and metabolic syndrome in Korean adults. Int J Environ Res Public Health (2018) 15(8):1658. doi: 10.3390/ijerph15081658
9. Oye-Somefun A, Kuk JL, Ardern CI. Associations between elevated kidney and liver biomarker ratios, metabolic syndrome and all-cause and coronary heart disease (CHD) mortality: analysis of the US national health and nutrition examination survey (NHANES). BMC Cardiovasc Disord (2021) 21(1):352. doi: 10.1186/s12872-021-02160-w
10. Wang K, Lin W, Kuang Z, Fan R, Liang X, Peng J, et al. Longitudinal change of body mass index is associated with alanine aminotransferase elevation after complete viral suppression in chronic hepatitis b patients. J Infect Dis (2019) 220(9):1469–76. doi: 10.1093/infdis/jiz326
11. Botros M, Sikaris KA. The de ritis ratio: the test of time. Clin Biochem Rev (2013) 34(3):117–30.
12. Chen KW, Meng FC, Shih YL, Su FY, Lin YP, Lin F, et al. Sex-specific association between metabolic abnormalities and elevated alanine aminotransferase levels in a military cohort: The CHIEF study. Int J Environ Res Public Health (2018) 15(3):545. doi: 10.3390/ijerph15030545
13. Kwon SS, Lee SG. A high alanine aminotransferase/aspartate aminotransferase ratio determines insulin resistance and metabolically healthy/unhealthy obesity in a general adult population in Korea: The Korean national health and nutritional examination survey 2007-2010. Exp Clin Endocrinol Diabetes (2019) 127(10):677–84. doi: 10.1055/a-0752-0217
14. Zou Y, Zhong L, Hu C, Sheng G. Association between the alanine aminotransferase/aspartate aminotransferase ratio and new-onset non-alcoholic fatty liver disease in a nonobese Chinese population: a population-based longitudinal study. Lipids Health Dis (2020) 19(1):245. doi: 10.1186/s12944-020-01419-z
15. Lu CW, Lin MS, Lin YS, Chang IJ, Tsai MH, Wei KL, et al. Aminotransferase ratio is a useful index for hepatosteatosis in children and adolescents: A cross-sectional observational study. Gastroenterol Nurs (2019) 42(6):486–95. doi: 10.1097/SGA.0000000000000389
16. Homsanit M, Sanguankeo A, Upala S, Udol K. Abnormal liver enzymes in Thai patients with metabolic syndromes. J Med Assoc Thai (2012) 95(3):444–51.
17. Ma WY, Yang CY, Shih SR, Hsieh HJ, Hung CS, Chiu FC, et al. Measurement of waist circumference: midabdominal or iliac crest? Diabetes Care (2013) 36(6):1660–6. doi: 10.2337/dc12-1452
18. Nikolic SB, Abhayaratna WP, Leano R, Stowasser M, Sharman JE. Waiting a few extra minutes before measuring blood pressure has potentially important clinical and research ramifications. J Hum Hypertens (2014) 28(1):56–61. doi: 10.1038/jhh.2013.38
19. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome–a new world-wide definition. a consensus statement from the international diabetes federation. Diabetes Med (2006) 23(5):469–80. doi: 10.1111/j.1464-5491.2006.01858.x
20. Heinze G, Wallisch C, Dunkler D. Variable selection - a review and recommendations for the practicing statistician. Biom J (2018) 60(3):431–49. doi: 10.1002/bimj.201700067
21. Wang S, Zhang J, Zhu L, Song L, Meng Z, Jia Q, et al. Association between liver function and metabolic syndrome in Chinese men and women. Sci Rep (2017) 7:44844. doi: 10.1038/srep44844
22. Esmaeelzadeh A, Saadatnia H, Memar B, Mokhtari Amirmajdi E, Ganji A, Goshayeshi L, et al. Evaluation of serum HBV viral load, transaminases and histological features in chronic HBeAg-negative hepatitis b patients. Gastroenterol Hepatol Bed Bench. (2017) 10(1):39–43.
23. Zhao L, Cheng J, Chen Y, Li Q, Han B, Chen Y, et al. Serum alanine aminotransferase/aspartate aminotransferase ratio is one of the best markers of insulin resistance in the Chinese population. Nutr Metab (Lond) (2017) 14:64. doi: 10.1186/s12986-017-0219-x
24. Joo EJ, Chang Y, Yeom JS, Ryu S. Hepatitis b virus infection and decreased risk of non-alcoholic fatty liver disease: A cohort study. Hepatol (2017) 65(3):828–35. doi: 10.1002/hep.28917
25. Hui RWH, Seto WK, Cheung KS, Mak LY, Liu KSH, Fung J, et al. Inverse relationship between hepatic steatosis and hepatitis b viremia: Results of a large case-control study. J Viral Hepat (2018) 25(1):97–104. doi: 10.1111/jvh.12766
26. Zhu L, Jiang J, Zhai X, Baecker A, Peng H, Qian J, et al. Hepatitis b virus infection and risk of non-alcoholic fatty liver disease: A population-based cohort study. Liver Int (2019) 39(1):70–80. doi: 10.1111/liv.13933
27. Hu D, Wang H, Wang H, Wang Y, Wan X, Yan W, et al. Non-alcoholic hepatic steatosis attenuates hepatitis b virus replication in an HBV-immunocompetent mouse model. Hepatol Int (2018) 12(5):438–46. doi: 10.1007/s12072-018-9877-7
28. Li J, Yang HI, Yeh ML, Le MH, Le AK, Yeo YH, et al. Association between fatty liver and cirrhosis, hepatocellular carcinoma, and hepatitis b surface antigen seroclearance in chronic hepatitis b. J Infect Dis (2021) 224(2):294–302. doi: 10.1093/infdis/jiaa739
29. Yang M, Wei L. Impact of NAFLD on the outcome of patients with chronic hepatitis b in Asia. Liver Int (2022). doi: 10.1111/liv.15252
30. Cai S, Ou Z, Liu D, Liu L, Liu Y, Wu X, et al. Risk factors associated with liver steatosis and fibrosis in chronic hepatitis b patient with component of metabolic syndrome. United Eur Gastroenterol J (2018) 6(4):558–66. doi: 10.1177/2050640617751252
31. Chan AW, Wong GL, Chan HY, Tong JH, Yu YH, Choi PC, et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis b. J Gastroenterol Hepatol (2017) 32(3):667–76. doi: 10.1111/jgh.13536
32. Romero-Saldaña M, Tauler P, Vaquero-Abellán M, Lopez-Gonzalez A, Futenes-Jimenez F, Aguilo A, et al. Validation of a non-invasive method for the early detection of metabolic syndrome: a diagnostic accuracy test in a working population. BMJ Open (2018) 8(10):e020476. doi: 10.1136/bmjopen-2017-020476
Keywords: aminotransferase, community-based, education, metabolic syndrome, hepatitis B virus
Citation: Lin M-S, Lin H-S, Chang M-L, Tsai M-H, Hsieh Y-Y, Lin Y-S, Tsai M-S, Yang C-L and Chen M-Y (2022) Alanine aminotransferase to aspartate aminotransferase ratio and hepatitis B virus on metabolic syndrome: a community-based study. Front. Endocrinol. 13:922312. doi: 10.3389/fendo.2022.922312
Received: 17 April 2022; Accepted: 04 July 2022;
Published: 29 July 2022.
Edited by:
Ozra Tabatabaei-Malazy, Tehran University of Medical Sciences, IranReviewed by:
Amir Ali Sohrabpour, Tehran University of Medical Sciences, IranCopyright © 2022 Lin, Lin, Chang, Tsai, Hsieh, Lin, Tsai, Yang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mei-Yen Chen, bWVpeWVuQGd3LmNndXN0LmVkdS50dw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.