- 1Department of General Internal Medicine 1, Kawasaki Medical School, Okayama, Japan
- 2Department of Diabetes, Endocrinology and Metabolism, Kawasaki Medical School, Kurashiki, Japan
- 3Department of Neurology, Kawasaki Medical School, Okayama, Japan
Background: Water intoxication is typically caused by primary or psychogenic polydipsia that potentially may lead to fatal disturbance in brain functions. Neuroleptic malignant syndrome (NMS) is a serious complication induced by administration of antipsychotics and other psychotropic drugs. The combination of inappropriate secretion of antidiuretic hormone (SIDAH), NMS and rhabdomyolysis have been rarely reported. Our patient also developed severe water intoxication.
Case presentation: Herein we report a comatose case of NMS complicated with water intoxication, syndrome of SIADH and rhabdomyolysis. This patient had severe cerebral edema and hyponatremia that were improved rapidly by the correction of hyponatremia within a couple of days.
Conclusions: Malignant neuroleptic syndrome water intoxication, SIADH and rhabdomyolysis can occur simultaneously. Comatose conditions induced by cerebral edema and hyponatremia can be successfully treated by meticulous fluid management and the correction of hyponatremia.
Background
Water intoxication is a condition that is typically caused by primary or psychogenic polydipsia. In addition, water intoxication potentially disturbs brain function when the abnormal balance of electrolytes, especially hyponatremia and hypo osmotic pressure, is brought about by excessive water intake (1). It is known that water intoxication occurs in 15–25% of patients with chronic mental diseases as a result of compulsive drinking (2). Neuroleptic malignant syndrome (NMS) is a serious complication induced by administration of antipsychotics and other psychotropic drugs (3). Symptoms of NMS include myotonicity, hyperthermia, altered consciousness, and autonomic nervous system symptoms. NMS is also complicated with hyponatremia and water intoxication (4, 5). The combination of syndrome of inappropriate secretion of antidiuretic hormone (SIADH), NMS and rhabdomyolysis have been rarely reported (6).
Herein we report a case of NMS complicated with water intoxication, cerebral edema and hyponatremia. His coma and severe cerebral edema were dramatically improved by the correction of hyponatremia within 3 days.
Case Presentation
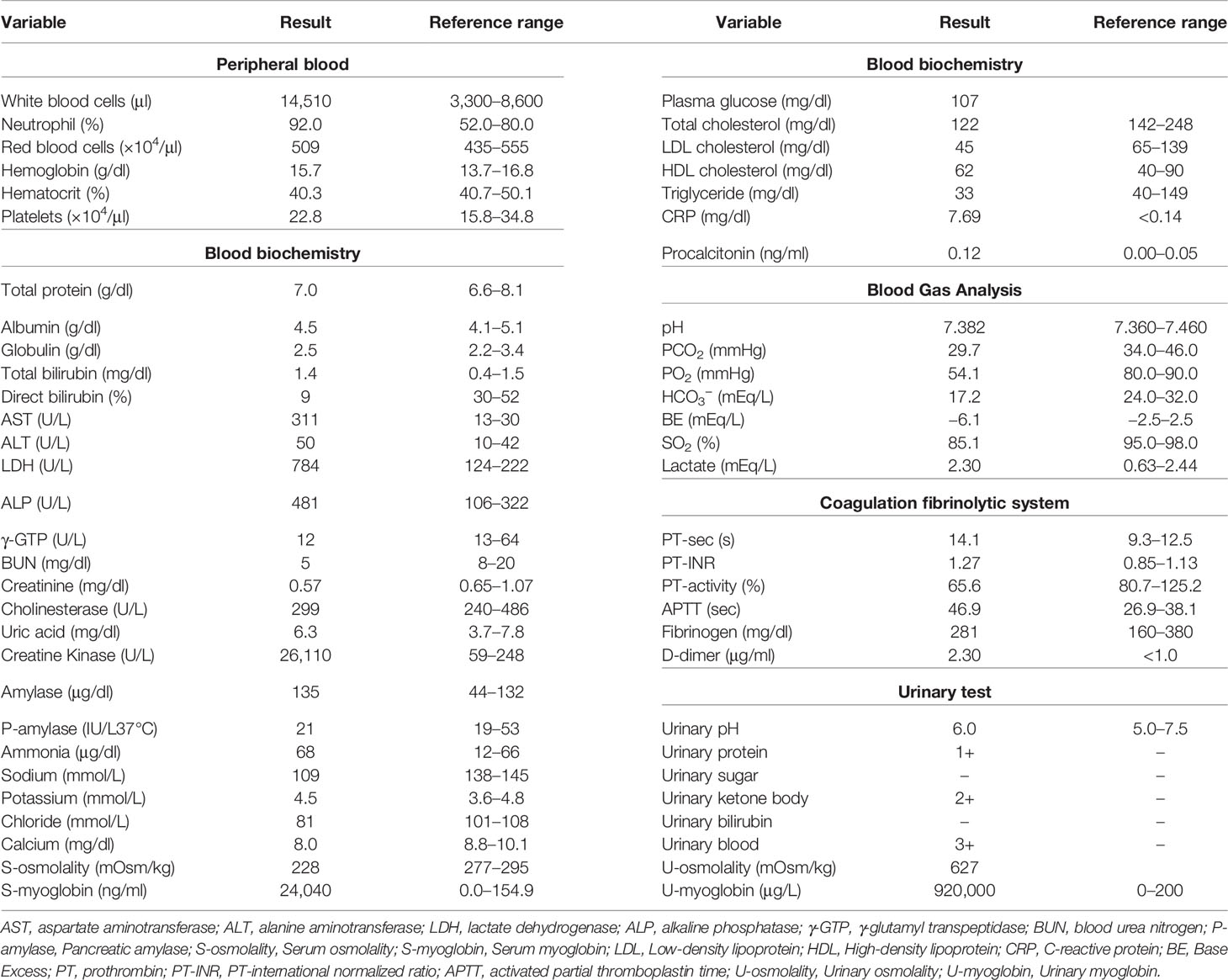
A 27-year-old Japanese man was brought to the emergency room with coma. He was diagnosed as having schizophrenia at the age of 13 and as having autism spectrum disorder at the age of 18. The medication at that time was 50 mg/day of atomoxetine, 5 mg/day of risperidone and 3 mg/day of guanfacine, although risperidone was decreased from 9 to 5 mg and guanfacine was increased from 2 to 3 mg 35 days before. He had been drinking over 4 L of water for the last few weeks. His impaired consciousness level was 3 points (E1V1M1) of the Glasgow coma scale (GCS). His vital signs were as follows: temperature, 39.1°C; blood pressure, 174/98 mmHg; heart rate, 95 beats/min; oxygen saturation, 92% (under 9 L of O2 supply). Table 1 shows laboratory data in emergency room. He suffered from abnormal balance of electrolytes. As shown in Table 1, he had significant hyponatremia and hypochloremia with normal potassium concentration, and reduction of blood osmotic pressure. His inflammation markers were markedly elevated. In addition, he suffered from rhabdomyolysis. Indeed, his creatine kinase, myoglobin and urinary myoglobin levels were significantly high. As shown in Figure 1, his head computed tomography (CT) (Figure 1A) revealed severe cerebral edema. In addition, significant fluid retention was observed throughout the body, namely, pleural effusion, pulmonary and intestinal edema (Figures 1A, B). We evaluated the causes of hyponatremia in this patient. Since antidiuretic hormone (ADH) level was elevated to 0.8 pg/ml when sodium level was 109 mmol/L, we diagnosed him with syndrome of inappropriate secretion of ADH (SIADH). Based on these findings, we thought that he probably suffered from severe cerebral edema which was induced by hyponatremia associated with NMS and SIADH. In addition, rhabdomyolysis and NMS was diagnosed necessitating comprehensive therapy in intensive care unit (ICU).
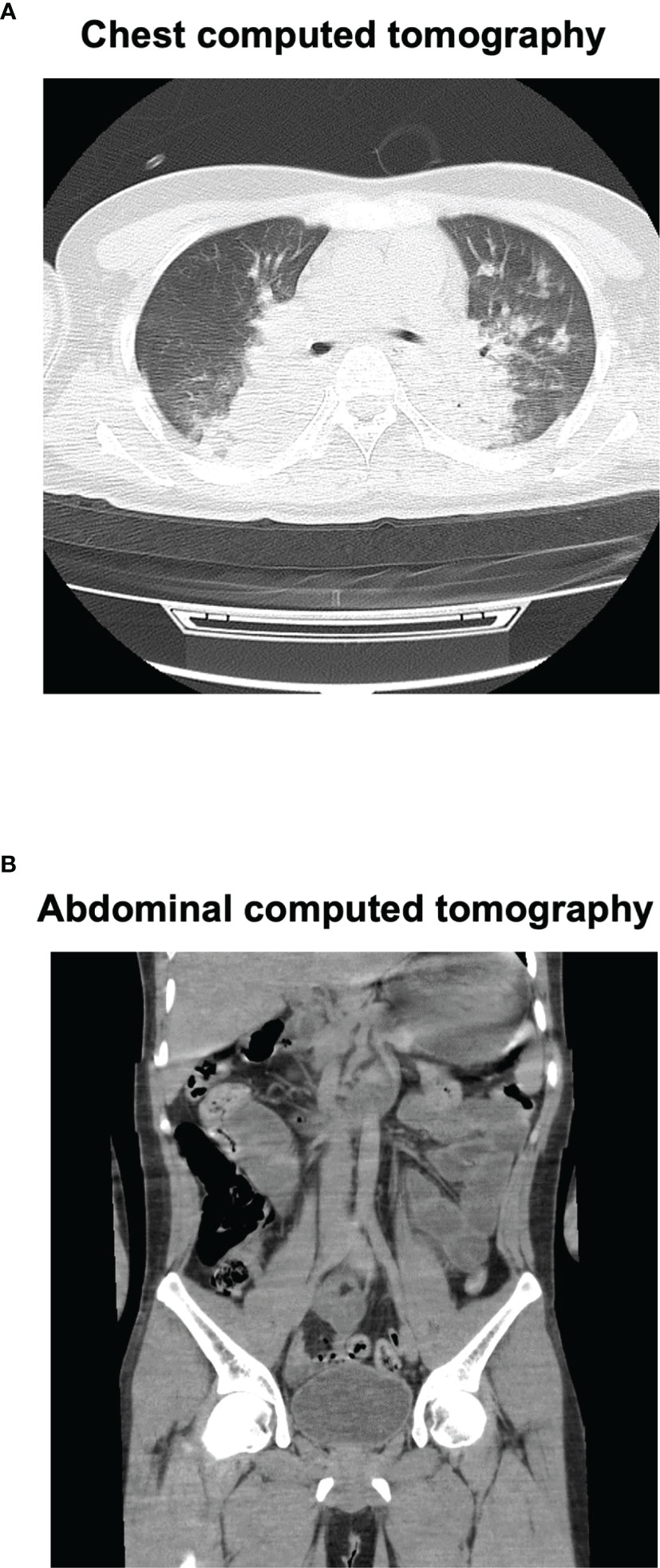
Figure 1 Chest and abdominal computed tomography (CT) on admission. Chest CT (A) revealed marked pleural effusion and pulmonary edema. Abdominal CT (B) revealed marked intestinal edema.
On admission to ICU, he required mechanical ventilation and administration of 0.9% NaCl. Moreover, we started immediately administering 10% glyceol (600 ml/once a day, 5 days + 400 ml/once a day, 2 days + 200 ml/once a day, 2 days) for cerebral edema and continuous furosemide (3 days) for diuresis. In addition, he was treated with methylprednisolone (1,000 mg/once a day, 3 days) for cerebral edema and suspection of autoimmune encephalitis, and with dantrolene (40 mg/once a day, 1 day + 100 mg/once a day, 4 days + 60 mg/once a day, 2 days) for NMS. Eye openings and spontaneous limb movements were observed several times at day 2 (his sodium level, 115 mmol/L). His impaired consciousness was improved and he was able to speak sometimes at day 3 (his sodium level, 130 mmol/L). The patient was extubated at day 3 and his head CT revealed the improvement of severe cerebral edema at day 4 (Figure 2B). Finally, we successfully treated severe cerebral edema and hyponatremia, which was induced and complicated with NMS, water intoxication, SIADH and rhabdomyolysis. Figure 2 shows a time course of his cerebral edema and Figure 3 shows his clinical time course in ICU. His adrenal and thyroid function was normal (adrenocorticotropic hormone, 61.7 pg/ml; cortisol, 13.0 μg/dl; thyroid stimulating hormone, 3.208 μIU/ml; free triiodothyronine, 2.89 pg/ml; free thyroxine, 1.03 ng/dl; respectively) after correction of hyponatremia. He was transferred from ICU to general ward at day 9 and was discharged 29 days after admission.
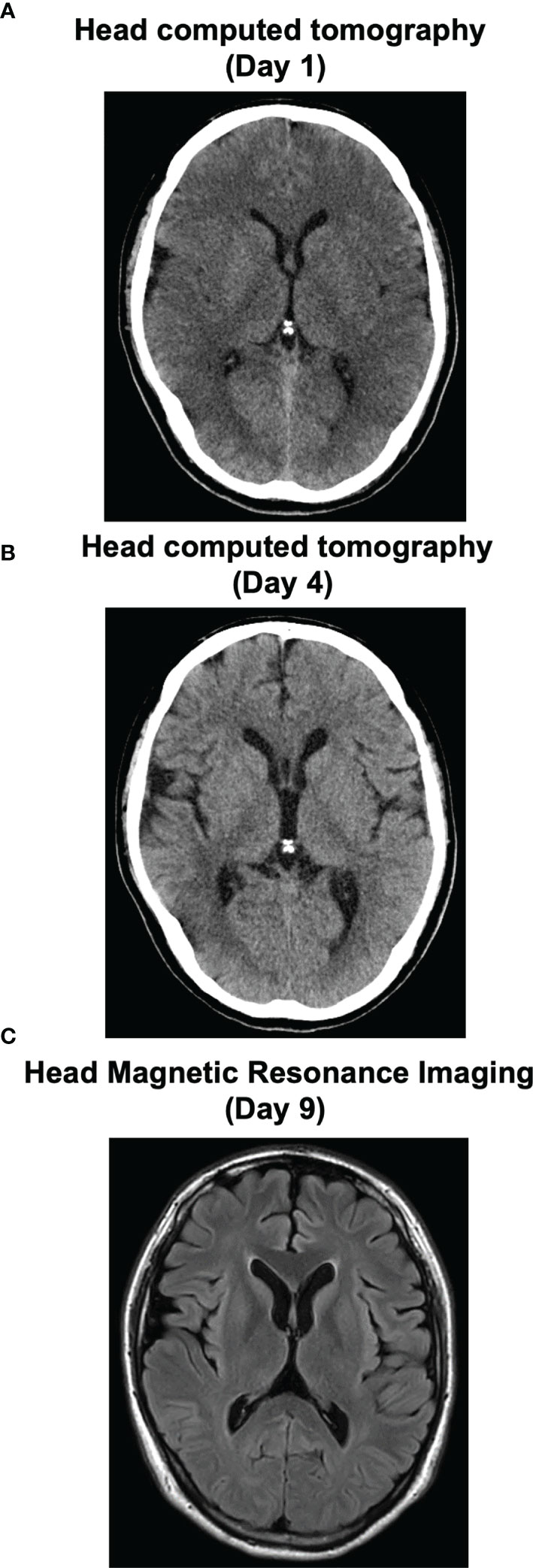
Figure 2 Time course of cerebral edema in this subject on the image inspection. His severe cerebral edema on admission (A) was improved at day 4 (B). At day 9, he was transferred from HCU to general ward. His head magnetic resonance imaging was normal (C).
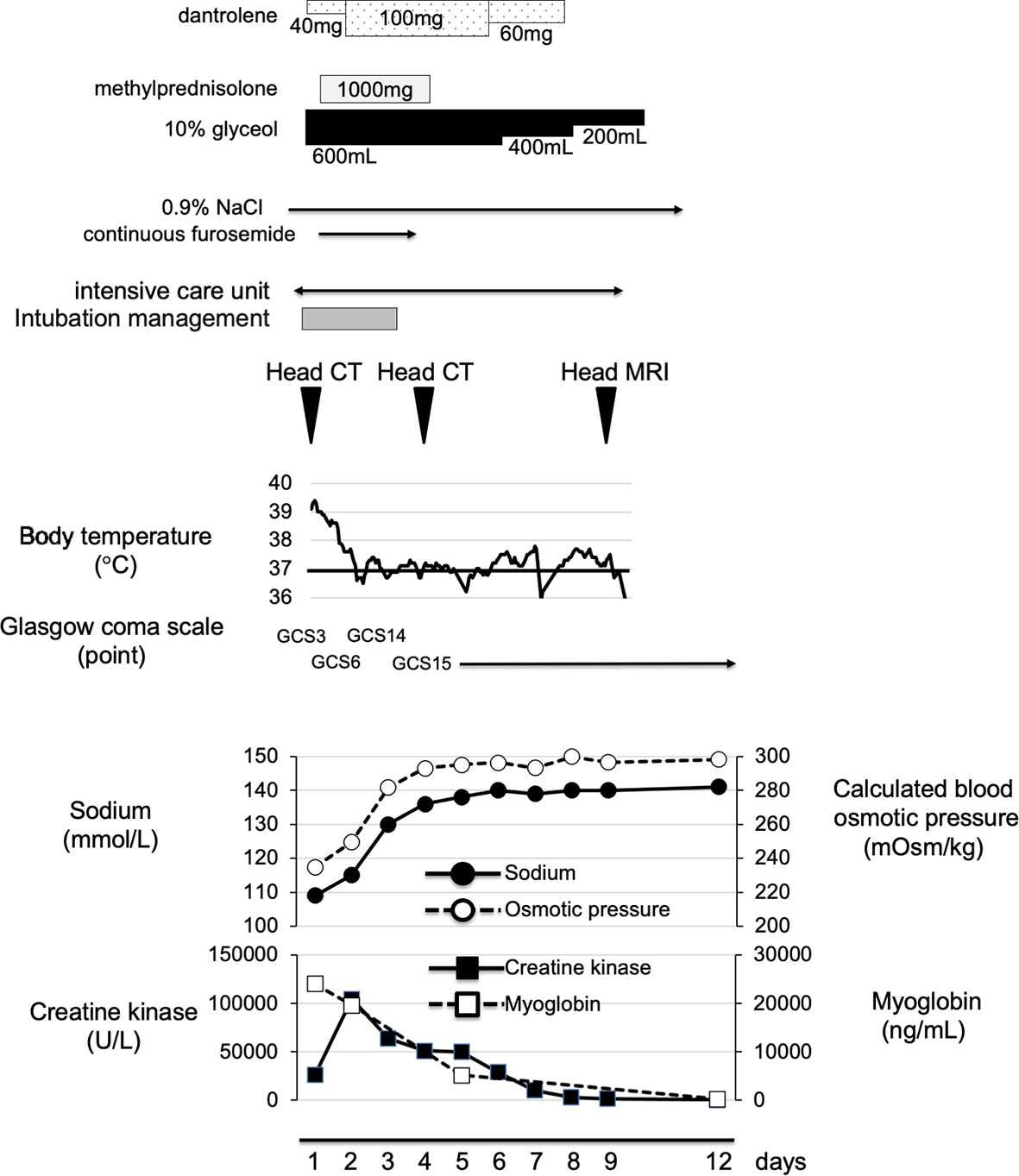
Figure 3 Time course of clinical parameters in this subject. On admission, we started fluid management, by using 10% glyceol and methylprednisolone for cerebral edema and dantrolene for NMS. His body temperature and coma were improved together with correction of hyponatremia and cerebral edema. He was transferred from HCU to general ward at day 9.
After discharge, he was followed-up by the psychosomatic center of another hospital. He continued to receive the same psychosomatic treatment and did not have recurrence of malignant syndromes or water intoxication.
Discussion
NMS is a serious complication that is estimated to occur in 0.07 to 2.2% of patients mainly after administration of antipsychotics and other psychotropic drugs (7, 8). Although the pathogenesis and the degree of progression are various, the prognosis of severe NMS is poor when water intoxication and rhabdomyolysis are complicated. On the other hand, water intoxication occurs in about 20% of patients with mental illness who are hospitalized for a long period of time (9), and in about 15% of outpatients with such disorders (10). Water intoxication is often complicated with hyponatremia and hypo osmotic pressure, and is reported to be associated with SIADH (11). There are few case reports showing complication of NMS and water intoxication (5, 12–17). Moreover, rhabdomyolysis is sometimes complicated together with both NMS and water intoxication (12, 14, 18). Our patient was a rare case in that he had NMS, water intoxication (namely, hyponatremia and hypo osmotic pressure), SIADH and rhabdomyolysis at the same time.
Most severe condition of our patient was impaired consciousness [3 points (E1V1M1) of GCS] and severe cerebral edema. In this point, we considered severe cerebral edema was mainly caused by hyponatremia due to water intoxication and SIADH. Therefore, we mainly performed fluid management by gradually improving abnormal balance of electrolytes and hyponatremia and reduced cerebral edema by using glyceol, methylprednisolone and furosemide. Moreover, since NMS was also considered as a possible cause of impaired consciousness, we started administering dantrolene. Eye openings and spontaneous limb movements [GCS6(E3VTM3)] were observed several times in the next day. The presence of rhabdomyolysis also made treatment difficult, and the first choice of treatment for rhabdomyolysis was aggressive hydration, although we would like to refrain from hydrating against cerebral edema and SIADH. Three days later, his impaired consciousness was improved and we performed his extubation [GCS14(E4V4M6)]. We performed head CT 4 days after admission, and we made sure that we successfully treated severe cerebral edema with correction of hyponatremia. In cerebral edema caused by hyponatremia, there is a risk of developing cerebral herniation due to exacerbation of cerebral edema and osmotic demyelination syndrome (ODS) during the treatment process. Once ODS is developed, about half of the patients may die or have residual sequelae. Therefore, we should correct hyponatremia slowly (19). We were able to successfully improve severe cerebral edema with fluid management focusing on the correction of hyponatremia. More interestingly, his impaired consciousness was improved dramatically in a short period of time as the cerebral edema improved.
There is a limitation in this case report. We examined adrenal and thyroid function after hyponatremia was corrected. In the pathogenesis of NMS, hypothyroidism and adrenal insufficiency have also been implicated (20). Since we did not check adrenal and thyroid function before starting methylprednisolone, we failed to completely exclude the possibility of hypothyroidism and adrenal insufficiency. However, since his adrenal and thyroid function was normal although they were evaluated after starting methylprednisolone, we thought that hypothyroidism or adrenal insufficiency was less likely to associated with NMS. Moreover, it is known that patients with acute psychosis have a propensity to develop hyponatremia (21), and some of psychogenic drugs can cause hyponatremia by unknown mechanism (22). In the pathogenesis of NMS, preceding hyponatremia could be a trigger for NMS (18).
Taken together, we should bear in mind that NMS, water intoxication, SIADH, and rhabdomyolysis can occur at the same time. In such a case, severe cerebral edema induced by hyponatremia and NMS may be the cause of coma. Furthermore, although slow correction of hyponatremia is necessary, fluid management, especially correction of hyponatremia, may dramatically improve cerebral edema and coma. Therefore, it is important to perform early diagnosis of cerebral edema due to hyponatremia, and it is necessary to be prepared for all conditions of whole-body management.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
HT and TA researched data and wrote the manuscript. YK, FK, RS, and KK researched data and contributed to the discussion. HK, KK, and KT reviewed the manuscript. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sailer CO, Winzeler B, Nigro N, Suter-Widmer I, Arici B, Bally M, et al. Characteristics and Outcomes of Patients With Profound Hyponatraemia Due to Primary Polydipsia. Clin Endocrinol (Oxf) (2017) 87:492–9. doi: 10.1111/cen.13384
2. Gerhant A, Slotwinski M, Holownia O, Stelmach E, Olajossy M. Hyponatremia in the Practice of a Psychiatrist. Part 2: Psychogenic Polydipsia. Curr Probl Psych (2017) 18:138–52. doi: 10.1515/cpp-2017-0012
3. Kawanishi C, Kishida I, Furuno T, Kato D, Bertilsson L. Pharmacogenetic Aspects of Neuroleptic Malignant Syndrome. Curr Pharmacogenomics (2006) 4:113–9. doi: 10.2174/157016006776286891
4. Poirier S, Legris G, Tremblay P, Michea R, Viau-Guay L, Mérette C, et al. Schizophrenia Patients With Polydipsia and Water Intoxication are Characterized by Greater Severity of Psychotic Illness and a More Frequent History of Alcohol Abuse. Schizophr Res (2010) 118:285–91. doi: 10.1016/j.schres.2009.12.036
5. Oruch R, Pryme IF, Engelsen BA, Lund A. Neuroleptic Malignant Syndrome: An Easily Overlooked Neurologic Emergency. Neuropsychiatr Dis Treat (2017) 13:161–75. doi: 10.2147/NDT.S118438
6. Kaur J, Kumar D, Alfishawy M, Lopez R, Sachmechi I. Paliperidone Inducing Concomitantly Syndrome of Inappropriate Antidiuretic Hormone, Neuroleptic Malignant Syndrome, and Rhabdomyolysis. Case Rep Crit Care (2016) 2016:2587963. doi: 10.1155/2016/2587963
7. Caroff SN, Mann SC. Neuroleptic Malignant Syndrome. Med Clin North Am (1993) 77:185–202. doi: 10.1016/s0025-7125(16)30278-4
8. Adityanjee, Aderibigbe YA, Mathews T. Epidemiology of Neuroleptic Malignant Syndrome. Clin Neuropharmacol (1999) 22:151–8.
9. de Leon J, Verghese C, Tracy JI, Josiassen RC, Simpson GM. Polydipsia and Water Intoxication in Psychiatric Patients: A Review of the Epidemiological Literature. Biol Psychiatry (1994) 35:408–19. doi: 10.1016/0006-3223(94)90008-6
10. Iftene F, Bowie C, Milev R, Hawken E, Talikowska-Szymczak E, Potopsingh D, et al. Identification of Primary Polydipsia in a Severe and Persistent Mental Illness Outpatient Population: A Prospective Observational Study. Psychiatry Res (2013) 210:679–83. doi: 10.1016/j.psychres.2013.04.011
11. Verghese C, De Leon J, Simpson GM. Neuroendocrine Factors Influencing Polydipsia in Psychiatric Patients: An Hypothesis. Neuropsychopharmacology (1993) 9:157–66. doi: 10.1038/npp.1993.54
12. Guadagnucci A, Tornaboni D, Vignali G, Mariotti M, Cincinelli A, Vignale L. [Neuroleptic Malignant Syndrome. A Case Report]. Minerva Med (1995) 86:327–30.
13. Looi JC, Cubis JC, Saboisky J. Hyponatremia, Convulsions and Neuroleptic Malignant Syndrome in a Male With Schizoaffective Disorder. Aust N Z J Psychiatry (1995) 29:683–7. doi: 10.3109/00048679509064986
14. Zaidi AN. Rhabdomyolysis After Correction of Hyponatremia in Psychogenic Polydipsia Possibly Complicated by Ziprasidone. Ann Pharmacother (2005) 39:1726–31. doi: 10.1345/aph.1E518
15. Tényi T, Vörös V. Successful Switch to Olanzapine After Rhabdomyolysis Caused by Water Intoxication and Clozapine Use. Pharmacopsychiatry (2006) 39:157–8. doi: 10.1055/s-2006-946708
16. Suzuki T, Uchida H, Watanabe K, Kashima H. A Potentially Aborted Neuroleptic Malignant Syndrome Following Seclusion Against Uncontrollable Water Intoxication. Psychopharmacol Bull (2008) 41:164–70.
17. Hayashi T, Ishida Y, Miyashita T, Kiyokawa H, Kimura A, Kondo T. Fatal Water Intoxication in a Schizophrenic Patient–an Autopsy Case. J Clin Forensic Med (2005) 12:157–9. doi: 10.1016/j.jcfm.2005.01.009
18. Bassi V, Fattoruso O, Santinelli C. A Rare Iatrogenic Association of Syndrome of Inappropriate Secretion of Antidiuretic Hormone, Neuroleptic Malignant Syndrome and Rhabdomyolysis. Oxf Med Case Rep (2019) 2019(3):omz010. doi: 10.1093/omcr/omz010
19. Kallakatta RN, Radhakrishnan A, Fayaz RK, Unnikrishnan JP, Kesavadas C, Sarma SP. Clinical and Functional Outcome and Factors Predicting Prognosis in Osmotic Demyelination Syndrome (Central Pontine and/or Extrapontine Myelinolysis) in 25 Patients. J Neurol Neurosurg Psychiatry (2011) 82:326–31. doi: 10.1136/jnnp.2009.201764
20. Taskapan C, Sahin I, Taskapan H, Kaya B, Kosar F. Possible Malignant Neuroleptic Syndrome That Associated With Hypothyroidism. Prog Neuropsychopharmacol Biol Psychiatry (2005) 29(5):745–8. doi: 10.1016/j.pnpbp.2005.04.004
21. Ellinas PA, Rosner F, Jaume JC. Symptomatic Hyponatremia Associated With Psychosis, Medications, and Smoking. J Natl Med Assoc (1993) 85(2):135–41.
Keywords: severe cerebral edema, hyponatremia, neuroleptic malignant syndrome, water intoxication, syndrome of inappropriate secretion of antidiuretic hormone
Citation: Takenouchi H, Anno T, Kimura Y, Kawasaki F, Shirai R, Kaneto H, Kurokawa K and Tomoda K (2022) Case Report: A Patient With Neuroleptic Malignant Syndrome, Water Intoxication and Hyponatremia Associated With Severe Cerebral Edema and Coma. Front. Endocrinol. 13:822679. doi: 10.3389/fendo.2022.822679
Received: 26 November 2021; Accepted: 14 February 2022;
Published: 10 March 2022.
Edited by:
Ben Nephew, Worcester Polytechnic Institute, United StatesReviewed by:
Abdelaziz M. Hussein, Mansoura University, EgyptAaron Hanukoglu, Tel Aviv University, Israel
Marina Caputo, Università degli Studi del Piemonte Orientale, Italy
Copyright © 2022 Takenouchi, Anno, Kimura, Kawasaki, Shirai, Kaneto, Kurokawa and Tomoda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Takatoshi Anno, YW5uby10QHVtaW4uYWMuanA=
 Haruka Takenouchi1
Haruka Takenouchi1 Takatoshi Anno
Takatoshi Anno Hideaki Kaneto
Hideaki Kaneto