
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 27 October 2022
Sec. Thyroid Endocrinology
Volume 13 - 2022 | https://doi.org/10.3389/fendo.2022.1041538
 Jiaming Chen1
Jiaming Chen1 Qi Zhong1
Qi Zhong1 Lizhen Hou1
Lizhen Hou1 Hongzhi Ma1
Hongzhi Ma1 Qian Shi1
Qian Shi1 Ling Feng1
Ling Feng1 Shizhi He1
Shizhi He1 Yansong Lin2
Yansong Lin2 Meng Lian1
Meng Lian1 Xixi Shen1
Xixi Shen1 Ru Wang1*
Ru Wang1* Jugao Fang1*
Jugao Fang1*Objective: To investigate the clinicopathological characteristics of papillary thyroid cancer (PTC) and identify risk factors for postoperative recurrence of PTC with recurrent laryngeal nerve (RLN) involvement.
Methods: In total, 171 patients (112 women and 59 men, age: 18–80 years, and 65 patients aged ≥ 55) with T4a PTC with RLN involvement, treated at Beijing Tongren Hospital, Capital Medical University, from January 2006 to December 2020, were retrospectively examined. Clinicopathological characteristics, including voice analysis results, and survival outcomes were assessed. The Mann–Whitney U and Kruskal–Wallis H tests were used to analyze differences in acoustic parameters. The Kaplan–Meier method was used to calculate the overall survival (OS) and recurrence-free (RFS) rates. Univariate and multivariate Cox regression analyses were performed of the clinical data.
Results: The postoperative follow-up period ranged from 12 to 196 months (mean: 66.18 months). Of the 171 patients, 16 had recurrence and 8 died of thyroid-related diseases. The 5-year OS rate was 95.22%. The 5-year RFS rate was 89.38%. Jitter and shimmer were higher and maximum phonation time was shorter in patients with preoperative vocal cord paralysis (VCP) than in those without RLN involvement, and in those with RLN involvement but without preoperative VCP. Acoustic parameters were similar in patients with no preoperative VCP and those without RLN involvement. Voice analysis results did not differ between cases with RLN adhesion and RLN invasion. Univariate analysis showed that age at onset ≥ 55 years, preoperative RLN palsy, and esophageal invasion were risk factors for postoperative recurrence of PTC with RLN involvement. Multivariate analysis showed that onset age ≥ 55 years (OR 4.52, 95% confidence interval: 1.44–14.19, P = 0.010) was an independent risk factor for recurrence.
Conclusions: PTC patients with RLN invasion can achieve good outcomes. Preoperative voice analysis may offer insights into RLN function. Age of onset ≥ 55 years is an independent risk factor for postoperative recurrence in T4a PTC patients.
Thyroid carcinoma is the most common malignant endocrine tumor. In recent years, the morbidity rate of thyroid cancer has gradually increased worldwide. In China, according to the statistics of the Chinese National Cancer Center, the number of newly diagnosed thyroid cancers is estimated to be 220,000 per year, causing it to rank seventh among all malignant tumors (1). Although the incidence of thyroid cancer is high, the associated mortality rate is rather low, mainly because most thyroid cancers are papillary thyroid cancers (PTC), which often have good differentiation and are associated with a better prognosis.
In clinical practice, some PTCs show high invasiveness, spreading to the recurrent laryngeal nerve (RLN) most commonly. It has been reported that, in PTC patients with extrathyroidal invasion, the rate of RLN involvement is 33–61% (2–4). The involvement of RLN not only affects the survival outcomes of patients with PTC, but it also affects their quality of life. Therefore, surgical management of these patients, to resect the tumor while preserving neural functions, has long been a goal. However, identification of RLN involvement using conventional imaging examinations is difficult.
In this study, we retrospectively evaluated PTC patients with RLN invasion and analyzed their clinicopathological characteristics, preoperative acoustic parameters, and survival outcomes, to identify risk factors for postoperative recurrence of PTC with RLN involvement.
This study was approved by the ethics committee of Beijing Tongren Hospital, Capital Medical University.
This retrospective study included PTC patients with RLN invasion at Beijing Tongren Hospital from January 2006 to December 2020. The exclusion criteria were as follows: history of irradiation or of other head and neck cancers; T4b patients according to the American Joint Committee on Cancer’s (AJCC) Staging Manual, 8th edition (5); and distant metastasis. The inclusion flow chart of this study is shown in Figure 1.
In all, 171 patients with T4a PTC with RLN invasion were enrolled in the analysis: stage I, 106 cases (T4aN0M0: 22 cases, T4aN1aM0: 27 cases, T4aN1bM0: 57 cases); stage III, 65 cases (T4aN0M0: 26 cases, T4aN1aM0: 16 cases, T4aN1bM0: 23 cases). Additionally, 116 PTC patients with stage T3 were enrolled as a control group for voice analysis.
All patients underwent preoperative high-resolution ultrasound (US) evaluation of thyroid nodules and potential metastatic lymph nodes (LNs) in the neck. When the tumor size was > 4 cm or when there were suspicious metastatic LNs and potential extrathyroidal lesions, computed tomography (CT) or magnetic resonance imaging (MRI) was also performed. A laryngoscopic examination was performed to evaluate the RLN function of each patient.
Some patients also underwent preoperative voice assessment using the multi-dimensional voice program (Version 3.3.0, Key Pentax, Tokyo, Japan). The acoustic parameters included fundamental frequency (F0), percentage of jitter (%), percentage of shimmer (%), and maximum phonation time (MPT). The voice of each patient was recorded three times, and the average of each parameter was used for further analysis.
According to the 2015 American Thyroid Association (ATA) risk scoring system (6), all patients in this study were assigned to the high-risk group, and total thyroidectomy was recommended. For some patients who strongly refused total thyroidectomy, and whose RLNs were mildly invaded, hemithyroidectomy was performed. For LN dissection, prophylactic central neck LN dissection was performed routinely, and lateral neck LN dissection was only performed in patients with high suspicion of lateral LN metastasis on CT and MRI or with biopsy-confirmed nodal metastases.
Preoperative RLN function assessment and intraoperative observation are vital for the treatment of invaded RLNs. When the tumors mildly invaded or adhered to the nerve, the tumor tissue was meticulously peeled off the nerve under magnification using surgical loupes. However, when there was vocal cord paralysis (VCP) preoperatively, or if there was extensive infiltration, the nerve was usually sacrificed (7, 8). Intraoperative nerve monitoring (IONM) was performed in this group. In addition, it should be noted that when bilateral RLN injury was confirmed, tracheotomy was usually performed intraoperatively.
Based on the pathological results, patients underwent radioactive iodine (RAI) with 150–200 mCi at 4–8 weeks after surgery.
Continuous variables were expressed as median and range or mean ± standard deviation, and categorical variables were expressed as numbers and percentages. The Mann–Whitney U test and Kruskal–Wallis H test were used to determine the differences in acoustic parameters between groups. To evaluate the associations between clinicopathological characteristics and recurrence, the χ2 test or Fisher’s exact test was utilized. Univariate and multivariate Cox proportional hazards models were also used to determine the risk factors for recurrence. Variables with P < 0.1 in the univariate analysis were subsequently included in the multivariable model. The Kaplan–Meier method was used to estimate overall survival (OS) and recurrence-free survival (RFS), and differences were analyzed using the log-rank test. Statistical differences were defined as P < 0.050.
From January 2006 to December 2020, 2,782 PTC patients underwent surgery at Beijing Tongren Hospital. Among them, 171 (6.15%) were confirmed to have RLN invasion. There were 112 females and 59 males, aged between 18 and 80 years. Twelve patients had PTC size > 4 cm. Eighty-five patients presented with multifocal lesions. Preoperative laryngoscopy revealed VCP in 60 patients. Thirty-five patients had laryngeal or tracheal invasion, while 29 had esophageal involvement.
When we investigated the RLN invasion condition more closely, we found that the RLNs of 33 patients were invaded by metastatic LNs. RLN invasion occurred in the recurrent laryngeal nerve inlet zone in 22 patients. In 82 patients, the RLN adhered to the tumor, while the RLNs of the other 89 patients were directly invaded by the tumor.
A total of 150 patients underwent total thyroidectomy and 85 patients underwent lateral neck LN dissection. Intraoperative tracheotomy was performed in 16 patients, and among them, 3 patients had bilateral RLN invasion. Finally, 14 patients had their tracheostomy tubes removed, and the average time to removing the tubes was 149.79 ± 102.97 days. A total of 4 patients were treated with endoscopic laser-assisted medial arytenoidectomy. Of the patients that had the RLN spared surgically, 73 patients were treated with separation or partial layer resection. Among these patients, seven patients suffered from transient VCP one week after surgery, while no patients developed permanent vocal cord paralysis one year after surgery. The remaining 98 patients underwent resection of the RLN. Immediate RLN reconstructions were performed in 33 patients, of which 13 patients had direct RLN anastomosis and 21 patients underwent ansa cervicalis nerve-to-RLN anastomosis. At one year after surgery, we found that the 33 patients who received immediate RLN reconstructions recovered their RLN function with varying degrees, while the other 65 patients who did not have RLN reconstructions all presented with VCP.
Pathological results indicated that seven patients had tall cell variant PTC and one patient had follicular variant PTC, while the remaining 163 patients had classic variant PTC. All patients had negative resection margins. A total of 125 patients had LN metastasis. Of these, 33 patients had five or more central metastatic LNs and 80 had lateral metastatic LNs. Seventeen patients were diagnosed with Hashimoto thyroiditis. In total, 126 patients underwent postoperative RAI therapy.
During follow-up, recurrence was observed in 16 of 171 patients (9.36%). Among these, recurrence involved the thyroid lobe and the surgical bed in three patients; larynx, trachea, or esophagus in five patients; and neck LNs in eight patients. Nine patients underwent a second operation, and one patient received targeted therapy. Eight patients died of thyroid-related disease. The average follow-up was 66.18 months, with a median of 58 months. As shown in Figure 2, the 5-year OS rate was 95.22% and the 5-year RFS rate was 89.38%.
The differences in acoustic parameters between PTC patients with different RLN conditions are presented in Tables 1 and 2. The results showed that patients with preoperative VCP had higher jitter, shimmer, and shorter MPT than patients without RLN involvement, as well as patients with RLN involvement but without preoperative VCP. Patients with RLN involvement and those without preoperative VCP showed no differences in acoustic parameters as compared to patients without RLN involvement.
In addition, the F0 of female patients with VCP was significantly higher than that of those without RLN involvement (P = 0.029) and those without VCP (P = 0.038), whereas there was no evident difference in males.
When the severity of RLN invasion differed among the patients, we also attempted to determine the association between acoustic parameters and the extent of RLN invasion. Thus, patients with direct RLN invasion (n = 57) and simple adhesions (n = 59) were enrolled. Table 3 presents the results. There were no significant differences between the two groups.
Among the investigated clinicopathological characteristics, only age ≥ 55 years (P = 0.001) and esophageal invasion (P = 0.021) differed significantly in terms of recurrence. Other characteristics (such as sex, multifocal tumors, and tumor size) were not associated with recurrence (Table 4).
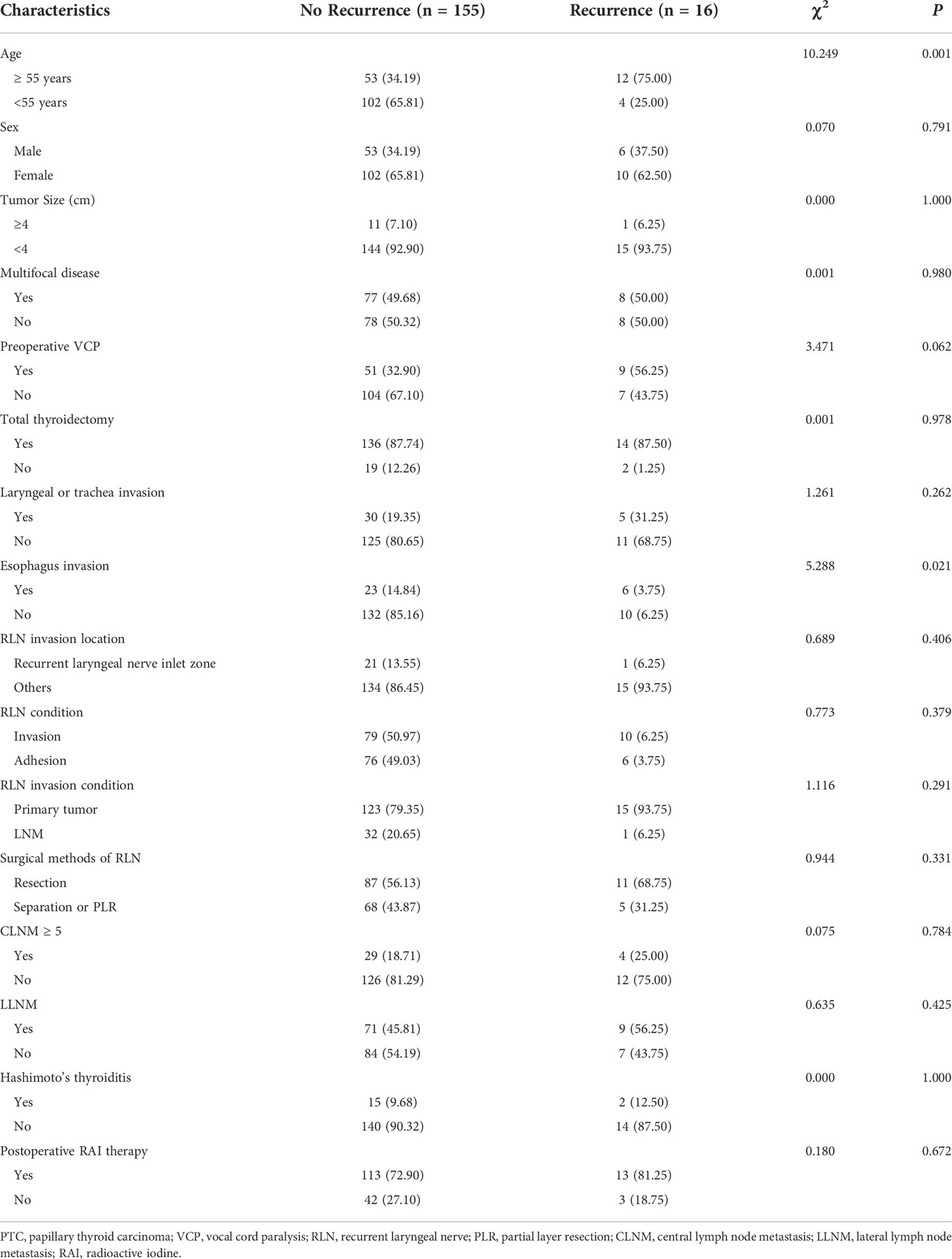
Table 4 Association between clinicopathological characteristics and recurrence in PTC patients with RLN invasion (n, %).
As shown in Table 5, among the various clinicopathological characteristics, age ≥ 55 years, preoperative VCP, and esophageal invasion were associated with an increased risk of PTC recurrence in univariate analyses (P < 0.100). However, only age ≥ 55 years was confirmed in the multivariable analysis (hazard ratio 4.52, 95% confidence interval: 1.44–14.19, P = 0.010).
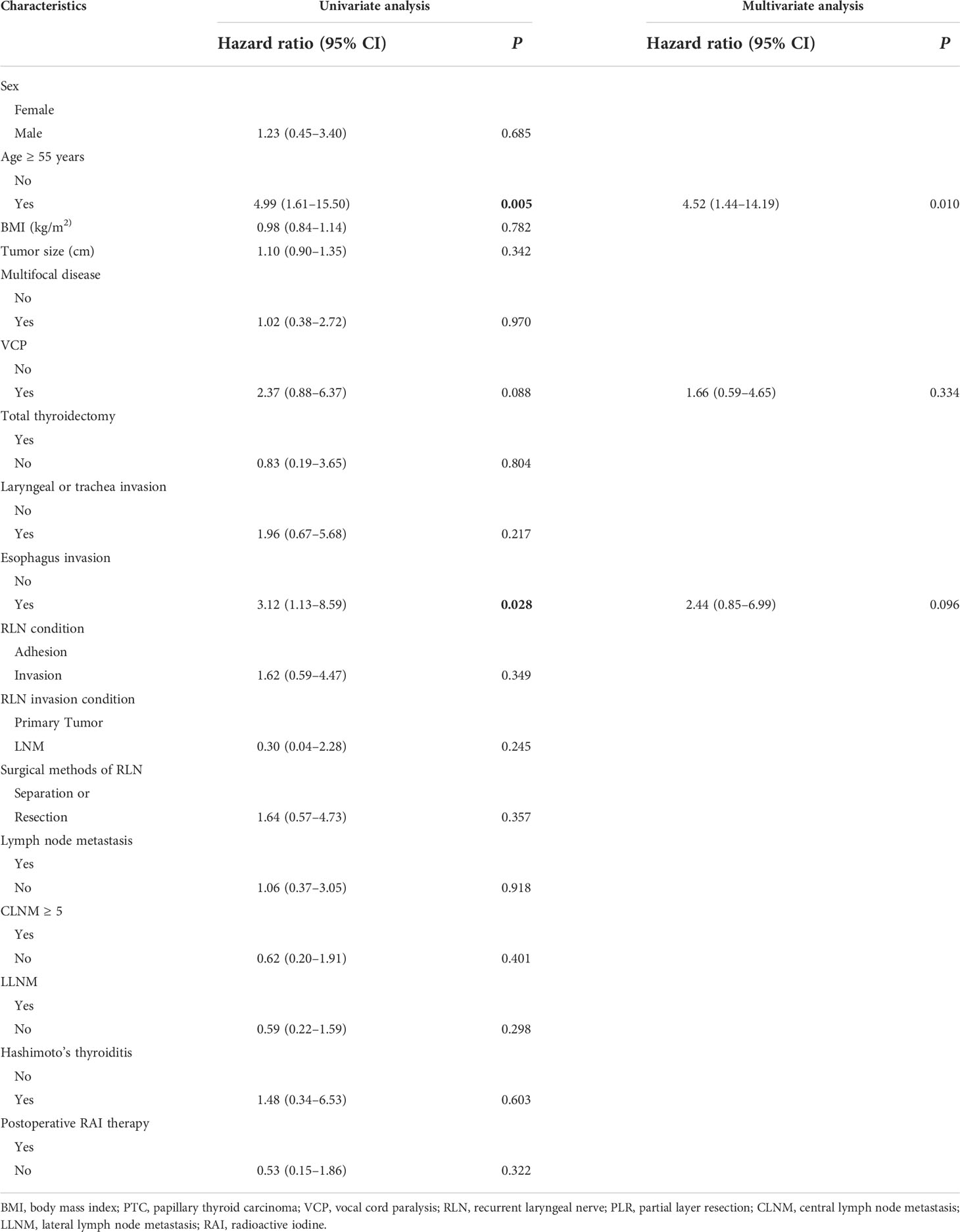
Table 5 Univariable and multivariable Cox proportional hazards regression analyses of the risk of recurrence.
Kaplan–Meier analysis showed that the RFS rate was significantly lower in patients aged ≥ 55 years than in those aged < 55 years (P = 0.002). Patients with esophageal invasion also had significantly lower RFS (P = 0.021). In addition, patients with preoperative VCP seemed to have a worse RFS than those without VCP, although this did not reach statistical significance (P = 0.078) (Figure 3). Other clinical characteristics were also suspected to be related to recurrence, such as the surgical scope and postoperative RAI therapy. To figure out their relationship with recurrence, we also performed Kaplan–Meier analysis. The results showed that there were no differences between patients who underwent total thyroidectomy and those who had a hemithyroidectomy (P=0.805) or patients who received or did not receive postoperative RAI (P=0.314) (Figure 4).
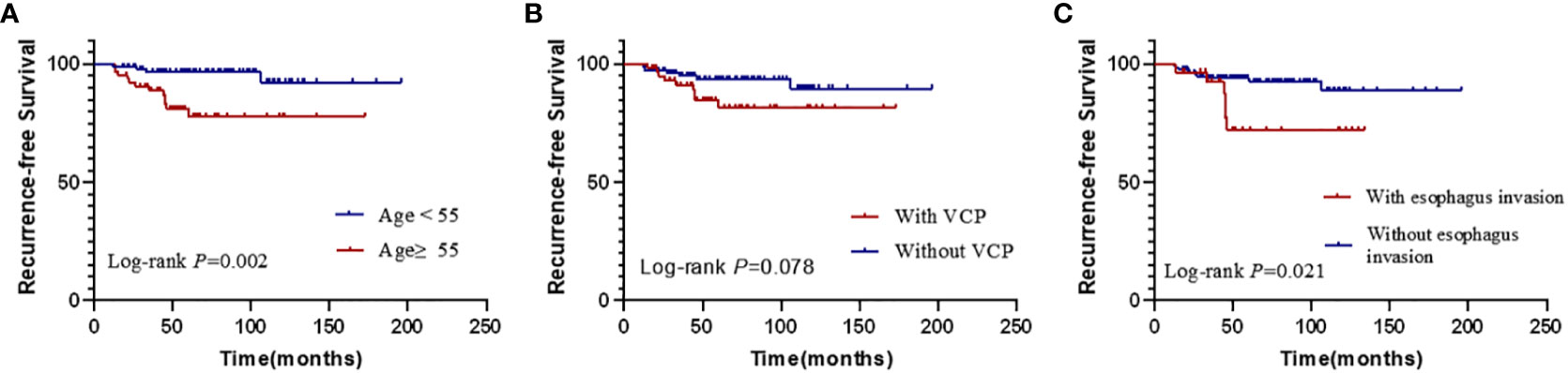
Figure 3 Kaplan–Meier curves for the recurrence-free survival according to different risk factors of univariable analysis. (A) the differences of RFS according to age (B) the differences of RFS according to the preoperative condition of the vocal cords. (C) the differences of RFS according to the status of esophagus. (VCP, vocal cord paralysis).
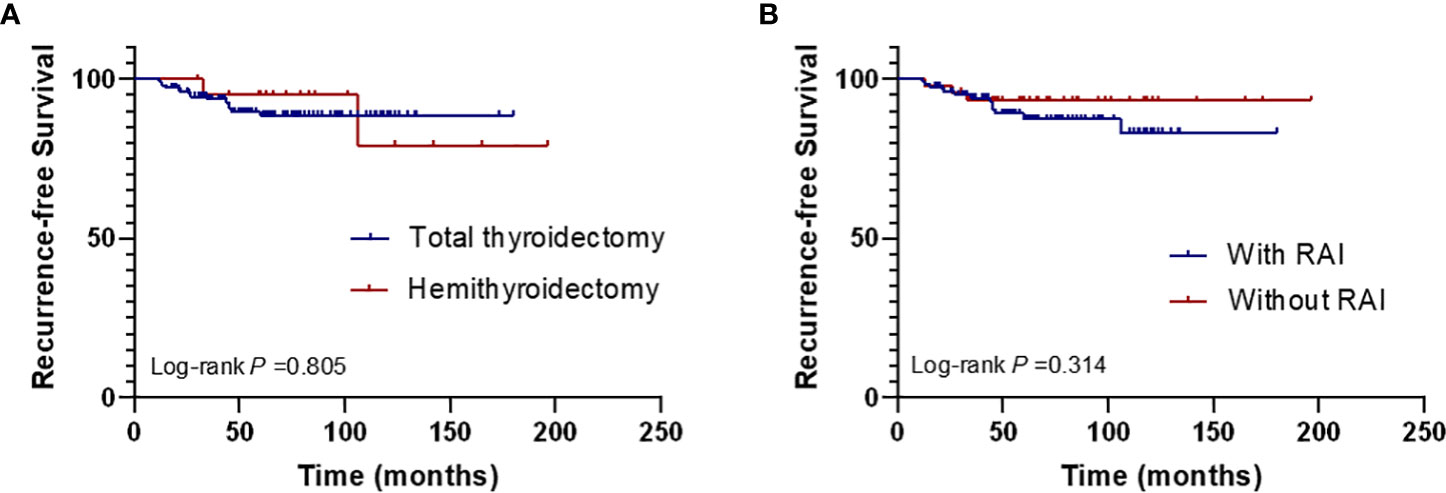
Figure 4 Kaplan–Meier curves for the recurrence-free survival according to the surgical scope of thyroid (A) and the postoperative RAI therapy (B). (RAI, radioactive iodine).
PTC is the most common type of malignant endocrine tumor. Although the majority are generally well-differentiated and demonstrate a favorable outcome, PTC is highly invasive in some patients, with the tumor directly invading into the surrounding tissue and structures. The RLN is usually located in the tracheoesophageal groove, and when the thyroid tumor penetrates the latter thyroid capsule or when the LNs of this region are metastatic, the RLN may become involved, and the function of the nerve may be impacted. Research on these patients’ survival outcomes and risk factors for recurrence can provide a scientific basis for the precise management of patients with PTC.
Assessment of RLN invasion includes preoperative and intraoperative observations. Because the RLN is typically located deep in the neck, it is difficult to estimate the condition of the RLN using routine imaging examinations. Some studies have reported that the preoperative assessment of RLN condition using CT, MRI or US. These imaging examinations may have given surgeons hints about the possibility of RLN invasion, however the sensitivity and accuracy were not satisfactory (9–11). Laryngoscopic examination is routinely recommended, but some patients with RLN invasion are still asymptomatic. In this study, only 60 patients experienced preoperative VCP and were identified using laryngoscopy. Other studies have reported that approximately 50–60% of invaded RLNs presented with normal preoperative nerve function (12, 13). Alexandre Dahan et al. reported that even in PTC patients whose RLNs were encased by thyroid tumors, preoperative VCP was present in 16/52 cases (30%) (14). It is more difficult to identify patients with RLN invasion without preoperative VCP. Since the preoperative assessment of RLN condition is often difficult, numerous guidelines now focus more on intraoperative RLN assessment, suggesting that intraoperative neural monitoring (IONM) is necessary for the optimal management of RLN invaded by thyroid tumor (3, 7, 15). As voice analysis continues to be refined and improved, it may provide new ideas and approaches for assessing the RLN preoperatively and noninvasively. Voice analysis is often used to evaluate voice quality in diverse dimensions. Several studies have performed voice analysis in PTC patients postoperatively and found that surgery has side effects on voice quality (16–18). To the best of our knowledge, no previous study had investigated the association between RLN condition and preoperative voice analysis findings. We found that in cases with RLN invasion, jitter and shimmer increased significantly, while MPT decreased significantly, indicating that the stability of the vocal cords worsened. Similarly, in patients with VCP, the jitter and shimmer increased significantly, and the MPT decreased significantly. These findings indicate that preoperative voice analysis can provide efficient and effective information regarding RLN conditions.
The association between age and the prognosis of thyroid cancer has long been a concern. In a previous study, Shah et al. reported that age was a key predictor of response to therapy and disease-specific survival in ATA high-risk thyroid cancer patients (19). Other studies have also indicated that age plays an important role in the survival of patients with ATA high-risk thyroid cancer (20–22). These findings indicated that it was appropriate to use age 55 years as the cut-off when considering tumor stage.
According to the AJCC Cancer Staging Manual, 8th edition, PTC patients with RLN invasion are assigned to stage T4a. In many cases, patients often suffer not only invasion of the RLN, but also of other structures, such as the trachea, larynx, and esophagus. There is still some debate regarding the influence of RLN invasion on survival. Indeed, several retrospective studies have found that PTC patients with only RLN invasion seem to have a better prognosis than patients with other extrathyroidal invasions (23, 24). Thus, some researchers have called for downstaging of patients with invasion of only the RLN. However, some previous studies have also shown that even though there was only RLN invasion, the OS and RFS rates were still lower than those in patients without any extrathyroidal invasion (25–27). In this study, we found that patients with esophageal invasion had significantly lower RFS than those without esophageal invasion, and that the RFS of patients with preoperative VCP tended to be lower than that of patients without preoperative VCP, although that difference was not statistically significant. These findings emphasize the need to actively manage these patients. The actual role of RLN invasion in the survival prognosis of patients requires further in-depth studies.
This study was limited in that it was a retrospective, single-center study. The long-term voice data were missing, making it hard to compare the voice quality between patients receiving RLN reconstruction or not. It was also subject to the inherent limitations associated with retrospective analyses. Multi-institutional studies with larger sample sizes are needed to confirm the results of our study.
Patients with PTC with RLN invasion are commonly encountered in clinical practice. To achieve optimal survival and vocal outcomes, comprehensive preoperative examinations are necessary. Our study provided novel insights into the use of voice analysis to evaluate RLN function. Moreover, survival analysis demonstrated that age of onset greater ≥ 55 years was an independent risk factor for postoperative recurrence in T4a PTC patients.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
QZ: review and editing (equal). LH, HM, QS: Conceptualization (lead); writing – original draft (lead); formal analysis (lead); writing – review and editing (equal). LF, XS, RW: Software (lead); writing – review and editing (equal). SH, YL, ML: Methodology (lead); writing – review and editing (equal). JF, JC: Conceptualization (supporting); Writing – original draft (supporting); Writing – review and editing (equal). All authors contributed to the article and approved the submitted version.
This study was supported by the National Key R&D Program of China (2020YFB1312805), Capital Health Research and Development of Special (2022–1–2051), Beijing Municipal Administration of Hospitals’ Youth Programme (QMS20210206); Scientific Research Common Program of Beijing Municipal Commission of Education (KM202210025014), Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20180202), Scientific Research and Incubating Fund of Capital Medical University(PYZ21096).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Zheng R, Zhang S, Zeng H, Wang S, Sun K, Chen R, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Center (2022) 2(1):1–9. doi: 10.1016/j.jncc.2022.02.002
2. McCaffrey TV, Bergstralh EJ, Hay ID. Locally invasive papillary thyroid carcinoma: 1940-1990. Head Neck (1994) 16(2):165–72. doi: 10.1002/hed.2880160211
3. Wu C-W, Dionigi G, Barczynski M, Chiang F-Y, Dralle H, Schneider R, et al. International neuromonitoring study group guidelines 2018: Part II: Optimal recurrent laryngeal nerve management for invasive thyroid cancer-incorporation of surgical, laryngeal, and neural electrophysiologic data. Laryngoscope (2018) 128(Suppl 3):S18–27. doi: 10.1002/lary.27360
4. Kowalski LP, Filho JG. Results of the treatment of locally invasive thyroid carcinoma. Head Neck (2002) 24(4):340–4. doi: 10.1002/hed.10058
5. Perrier ND, Brierley JD, Tuttle RM. Differentiated and anaplastic thyroid carcinoma: Major changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin (2018) 68(1):55–63. doi: 10.3322/caac.21439
6. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. American Thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid (2015) 2016:26(1). doi: 10.1089/thy.2015.0020
7. Shindo ML, Caruana SM, Kandil E, McCaffrey JC, Orloff LA, Porterfield JR, et al. Management of invasive well-differentiated thyroid cancer: an American head and neck society consensus statement. AHNS consensus statement. Head Neck (2014) 36(10):1379–90. doi: 10.1002/hed.23619
8. Chiang F-Y, Lin J-C, Lee K-W, Wang L-F, Tsai K-B, Wu C-W, et al. Thyroid tumors with preoperative recurrent laryngeal nerve palsy: clinicopathologic features and treatment outcome. Surgery (2006) 140(3):413–7. doi: 10.1016/j.surg.2006.02.006
9. Takashima S, Takayama F, Wang J, Kobayashi S, Kadoya M. Using MR imaging to predict invasion of the recurrent laryngeal nerve by thyroid carcinoma. AJR Am J Roentgenol (2003) 180(3):837–42. doi: 10.2214/ajr.180.3.1800837
10. Moritani S. Impact of lymph node metastases with recurrent laryngeal nerve invasion on patients with papillary thyroid carcinoma. Thyroid (2015) 25(1):107–11. doi: 10.1089/thy.2014.0152
11. Yamamura N, Fukushima S, Nakao K, Nakahara M, Kurozumi K, Imabun S, et al. Relation between ultrasonographic and histologic findings of tracheal invasion by differentiated thyroid cancer. World J Surg (2002) 26(8):1071–3. doi: 10.1007/s00268-002-6671-3
12. Kamani D, Darr EA, Randolph GW. Electrophysiologic monitoring characteristics of the recurrent laryngeal nerve preoperatively paralyzed or invaded with malignancy. Otolaryngol Head Neck Surg (2013) 149(5):682–8. doi: 10.1177/0194599813504735
13. Brooks JA, Abdelhamid Ahmed AH, Al-Qurayshi Z, Kamani D, Kyriazidis N, Hammon RJ, et al. Recurrent laryngeal nerve invasion by thyroid cancer: Laryngeal function and survival outcomes. Laryngoscope (2022) 132(11):2285–92. doi: 10.1002/lary.30115
14. Dahan A, Al Ghuzlan A, Chehab R, Guerlain J, Breuskin I, Garcia C, et al. Pathological analysis of encased resected recurrent nerves in locally invasive thyroid cancer. Cancers (Basel) (2022) 14(12):2961. doi: 10.3390/cancers14122961
15. Scharpf J, Liu JC, Sinclair C, Singer M, Liddy W, Orloff L, et al. Critical review and consensus statement for neural monitoring in otolaryngologic head, neck, and endocrine surgery. Otolaryngol Head Neck Surg (2022) 166(2):233–48. doi: 10.1177/01945998211011062
16. Maeda T, Saito M, Otsuki N, Morimoto K, Takahashi M, Iwaki S, et al. Voice quality after surgical treatment for thyroid cancer. Thyroid (2013) 23(7):847–53. doi: 10.1089/thy.2012.0060
17. Kim S-Y, Kim G-J, Lee D-H, Bae J-S, Lee S-H, Kim J-S, et al. Voice change after thyroidectomy without vocal cord paralysis: Analysis of 2,297 thyroidectomy patients. Surgery (2020) 168(6):1086–94. doi: 10.1016/j.surg.2020.07.055
18. Kletzien H, Macdonald CL, Orne J, Francis DO, Leverson G, Wendt E, et al. Comparison between patient-perceived voice changes and quantitative voice measures in the first postoperative year after thyroidectomy: A secondary analysis of a randomized clinical trial. JAMA Otolaryngol Head Neck Surg (2018) 144(11):995–1003. doi: 10.1001/jamaoto.2018.0309
19. Shah S, Boucai L. Effect of age on response to therapy and mortality in patients with thyroid cancer at high risk of recurrence. J Clin Endocrinol Metab (2018) 103(2):689–97. doi: 10.1210/jc.2017-02255
20. van Velsen EFS, Peeters RP, Stegenga MT, van Kemenade FJ, van Ginhoven TM, Verburg FA, et al. The influence of age on disease outcome in 2015 ATA high-risk differentiated thyroid cancer patients. Eur J Endocrinol (2021) 185(3):421–9. doi: 10.1530/EJE-21-0365
21. Jin M, Ahn J, Lee Y-M, Sung T-Y, Song DE, Kim TY, et al. Clinical implications of age and excellent response to therapy in patients with high-risk differentiated thyroid carcinoma. Clin Endocrinol (Oxf) (2021) 95(6):882–90. doi: 10.1111/cen.14543
22. Trimboli P, Piccardo A, Signore A, Valabrega S, Barnabei A, Santolamazza G, et al. Patient age is an independent risk factor of relapse of differentiated thyroid carcinoma and improves the performance of the American thyroid association stratification system. Thyroid (2020) 30(5):713–9. doi: 10.1089/thy.2019.0688
23. Hotomi M, Sugitani I, Toda K, Kawabata K, Fujimoto Y. A novel definition of extrathyroidal invasion for patients with papillary thyroid carcinoma for predicting prognosis. World J Surg (2012) 36(6):1231–40. doi: 10.1007/s00268-012-1518-z
24. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Prognostic significance of extrathyroid extension of papillary thyroid carcinoma: massive but not minimal extension affects the relapse-free survival. World J Surg (2006) 30(5):780–6. doi: 10.1007/s00268-005-0270-z
25. Song E, Lee Y-M, Oh H-S, Jeon MJ, Song DE, Kim TY, et al. A relook at the T stage of differentiated thyroid carcinoma with a focus on gross extrathyroidal extension. Thyroid (2019) 29(2):202–8. doi: 10.1089/thy.2018.0300
26. Bortz MD, Kuchta K, Winchester DJ, Prinz RA, Moo-Young TA. Extrathyroidal extension predicts negative clinical outcomes in papillary thyroid cancer. Surgery (2021) 169(1):2–6. doi: 10.1016/j.surg.2020.04.003
Keywords: acoustic parameters, recurrence, risk factors, recurrent laryngeal nerve, thyroid neoplasms
Citation: Chen J, Zhong Q, Hou L, Ma H, Shi Q, Feng L, He S, Lin Y, Lian M, Shen X, Wang R and Fang J (2022) Preoperative voice analysis and survival outcomes in papillary thyroid cancer with recurrent laryngeal nerve invasion. Front. Endocrinol. 13:1041538. doi: 10.3389/fendo.2022.1041538
Received: 11 September 2022; Accepted: 17 October 2022;
Published: 27 October 2022.
Edited by:
Frederic Triponez, Hôpitaux universitaires de Genève (HUG), SwitzerlandReviewed by:
Eleonora Lori, Sapienza University of Rome, ItalyCopyright © 2022 Chen, Zhong, Hou, Ma, Shi, Feng, He, Lin, Lian, Shen, Wang and Fang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jugao Fang, ZmFuZ2p1Z2FvMkBjY211LmVkdS5jbg==; Ru Wang, cnV3YW5nMTk4OUAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.