- 1Department of Ultrasound, Linzi District Maternity and Child Health Care Hospital, Zibo, China
- 2Department of Ultrasound, Chinese PLA General Hospital, Beijing, China
Objective: The aim of this study was to explore the clinical diagnostic value of puncture feeling during fine-needle aspiration (FNA) for non-diagnostic and indeterminate thyroid nodules.
Methods: A retrospective analysis was performed on 176 patients (196 nodules) diagnosed with Bethesda I or III by FNA cytology at the ultrasound department of our hospital between January 2017 and January 2020. Comparisons were made on the differences in puncture feeling (including stiffness and grittiness) between benign and malignant thyroid nodules, and their diagnostic performance was analyzed.
Results: There were significant differences between benign and malignant nodules with respect to the puncture stiffness and puncture grittiness (P < 0.001). The presence of a hard stiffness and grittiness demonstrated comparable levels of diagnostic performance for malignant thyroid nodules, with sensitivities, specificities, accuracies, positive predictive values, and negative predicative values of 55.56% and 63.89%, 87.10% and 78.22%, 75.51% and 72.96%, 71.43% and 63.01%, and 77.14% and 78.86%, respectively. The diagnostic performance was most optimal in the presence of at least one puncture feeling (area under the receiver operating characteristic curve: 0.771), exhibiting a sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of 79.17%, 75.00%, 76.53%, 64.77, and 86.11%%, respectively.
Conclusions: Puncture feeling adds clinical value in the diagnosis of thyroid nodules with indeterminate FNA findings.
Introduction
There has been a significantly gradual rise in the incidence of thyroid cancer over the past few years (1). Fine-needle aspiration (FNA) is a cytopathological technique that plays a crucial role in the diagnosis of thyroid cancer (2, 3). The diagnosis through FNA cytology is reliant on the Bethesda System for Reporting Thyroid Cytopathology (4). However, there are ambiguities in its criteria for cytological diagnosis, and 10-15% false negatives has been reported (5, 6). In particular, Bethesda category I and III nodules are non-diagnostic and indeterminate thyroid nodules prone to misdiagnosis, which inevitably cause repeat aspiration or diagnostic operation.
Molecular pathology including gene mutational panel and comprehensive multigene next-generation sequencing panel can be used to diagnosis thyroid cancer (7). However, the cost is expensive and not universally available. Repeat FNA of non-diagnostic and indeterminate thyroid nodules had a positive impact. However, some cases may remain indeterminate even after repeat aspiration of the nodule (8).During the process of FNA, the operator may detect different sensations as the needle enters the nodule (i.e., puncture feeling), such as stiffness, grittiness, etc. The different sensations indicate different internal composition of the nodules, which may contribute to differential diagnosis. Due to the presence of calcifications and psammoma bodies in papillary thyroid carcinomas, the friction may contribute to the sensation of grittiness during the puncture process (9). In addition, most thyroid cancers appear as hard nodules on elastography (10). At present, research on the significance of puncture feeling to the diagnostic performance of thyroid nodule biopsy is relatively scarce, and it remains unclear which types of puncture feeling can better facilitate the diagnosis of thyroid nodules.
In order to further improve diagnostic accuracy on the basis of cytopathological diagnosis and to provide evidence for decision-making by clinicians and interventional sonographers, this study explored the clinical diagnostic value of puncture feeling during FNA biopsy for non-diagnostic and indeterminate nodules and compared the diagnostic performances of different commonly observed puncture feelings.
Materials and methods
Patients
176 patients (196 nodules) diagnosed with Bethesda category I or III nodules by thyroid nodule FNA cytology at the ultrasound department of Qidu Hospital between January 2017 and January 2020 were enrolled in this retrospective study.
The inclusion criteria were as follows (1): patients with well-defined single or multiple thyroid nodules that were suspicious for malignancy and indicated for FNA biopsy; (2) patients who underwent ultrasound-guided FNA at our department; (3) cytopathological findings indicating Bethesda category I or III nodules; (4) patients who underwent repeat aspiration or surgical treatment after FNA. The exclusion criteria: patients with unclear secondary aspiration or postoperative pathological findings.
Instruments and methods
Thyroid examination was performed using the Mindray Resona 7 (Mindray, Shenzhen, Guangdong, China) color Doppler ultrasound system equipped with an L14-5 probe, and the settings were adjusted for thyroid examination (frequency: 5–14 MHz). In accordance with the classification criteria of the American College of Radiology (ACR) Thyroid Imaging, Reporting and Data System (TI-RADS) (2), the thyroid nodules that met the ACR criteria or 2012 Chinese Medical Association Guidelines (11) were recommended for FNA. Prior to the biopsy, informed consent was obtained in writing from the patients and their family members. FNA was performed using 25G × 50 mm biopsy needles (Hakko Co., Ltd., Chikum-Shi, Nagano, Japan).
All FNA procedures were performed by a sonographer with more than 10 years of interventional experience. During the procedure, patients were placed in a supine position, and the puncture site was covered with fenestrated drapes after undergoing disinfection. The sonographer sat at the patient’s cranial end. Using the freehand FNA technique, the needle was inserted at the midpoint on the side of the probe. Under ultrasound guidance, the needle tip entered the nodule without negative pressure, and 10–20 needle passes were made in multiple directions. The assistant observed whether bleeding occurred at the end of the needle and prompted the sonographer to stop if bleeding occurred to prevent excessive blood in the biopsy specimen. The puncture feeling was dictated and documented by the operator. Grittiness was defined as a sensation of sandpaper-like friction during the needle insertion, and its presence or absence was recorded. In addition, the stiffness encountered when the needle tip entered the nodule was compared with that entering normal thyroid parenchyma. Nodules with a higher stiffness than normal thyroid parenchyma were defined as hard. Otherwise, they were defined as soft. Once FNA was completed, rapid smear preparation was performed with the cooperation of the assistant, and the specimens were fixed using 95% alcohol for 20 s. The operator then selected 2–3 smears based on visual judgement of the specimen quality for cytopathological examination in the pathology department. The pathological findings were classified according to the Bethesda System for Reporting Thyroid Cytopathology (12). Patients with nodules classified as category I or category III were recommended for repeat aspiration or surgical treatment, as appropriate.
The medical records of patients with thyroid nodules stored in the ultrasound department were reviewed. Screening was performed using the clinical data and pathological records to select the patients with Bethesda category I or III nodules. The patients’ parameters were recorded, which included sex, age, maximum nodule diameter, nodule volume (superior-inferior diameter × left-right diameter × anterior-posterior diameter × 0.52), initial FNA findings and final pathological findings. Comparisons were performed to determine whether the presence/absence of grittiness and nodule puncture texture was associated with the final pathological findings (benign vs. malignant). In addition, we evaluated the clinical value of applying the two types of puncture feelings alone or combined in the diagnosis of thyroid nodules.
Statistical methods
All statistical analyses were performed using SPSS (version 26.0). Measurement data are expressed as the mean ± standard deviation, whereas the count data are expressed as the number of cases and percentage. Comparisons of differences were performed using the chi-squared test or Fisher’s exact test. The diagnostic performance of puncture feeling for thyroid nodules was evaluated using its sensitivity, specificity, accuracy, positive predictive value (PPV), negative predictive value (NPV), receiver operating characteristic (ROC) curve and area under the ROC curve (AUROC). P < 0.05 was used to indicate statistical significance.
Results
Clinical and pathological data
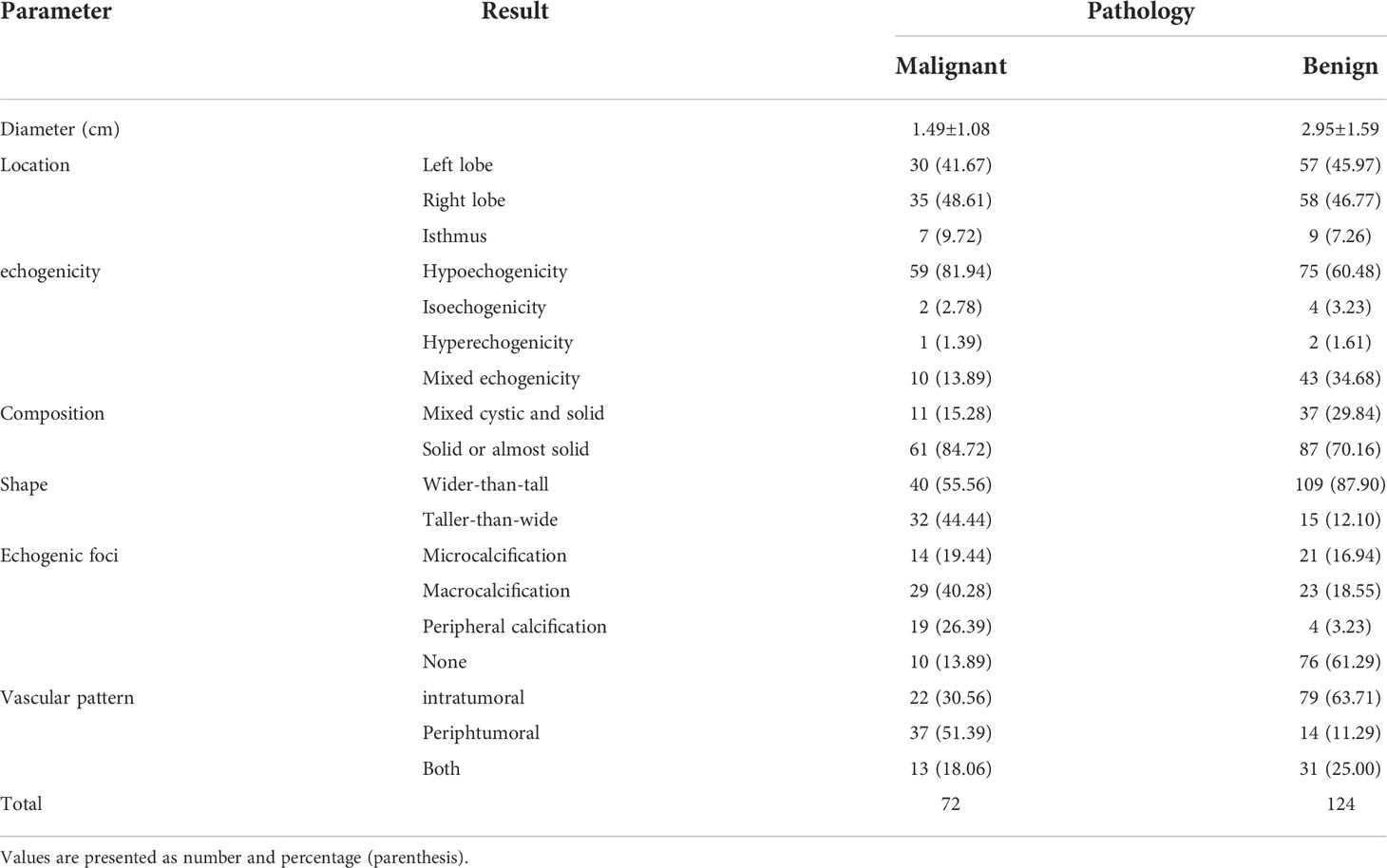
A total of 176 patients with 196 nodules were enrolled, including 21 males (11.9%) and 155 females (88.1%), and the patients had a mean age of 43.48 ± 11.39 years (20–72 years). The maximum nodule diameter was 2.42 ± 1.59 cm (0.5–6.6 cm), and the nodule volume was 7.78 ± 2.01 (0.065–66.25 cm3). The initial FNA findings indicated that 115 (58.7%) were Bethesda category III nodules and 81(41.3%) were category I nodules. The final pathological confirmation indicated that 124 were benign nodules, including 61 (49.2%) nodular goiter, 5 (4.0%) subacute thyroiditis, 40 (32.3%) thyroid adenoma and 18 (14.5%) localized Hashimoto’s thyroiditis; whereas 72 were malignant nodules, including 70 (97.2%) papillary thyroid carcinoma and 2 (2.8%) follicular thyroid carcinoma. Of all the nodules enrolled in our study, their tumor size, location and ultrasound characteristics were displayed in Table 1.
Of all the 72 malignant nodules, 9 of them (12.5%) were presence with psamoma on histology. And tumor variant results showed 2(2.8%) medullary carcinoma, 3(4.2%) follicular papillary carcinoma, 15(20.8%) micro-carcinoma and 52(72.2%) classical papillary carcinoma. 64(88.9%) received surgery and 8(11.1%) received ultrasound guided thermal ablation. Of the 64 patients who underwent surgery, the results of the T-staging showed 59(92.2%) T1, three (4.7%) T2 and two (3.1%) T4. Their N-staging showed 27(42.2%) N1 and 37(57.8%) N0. Occult cancers were detected in 12(18.8%) cases. The 8 patients who underwent ablation were all confirmed as classical papillary carcinoma by CNB before ablation, and the ablation was successfully completed, with more than 1 year’s follow-up. No tumor recurrence and lymph node metastasis were detected in the 8 ablation cases.
Diagnostic performance of puncture feeling in thyroid nodules with indeterminate FNA findings
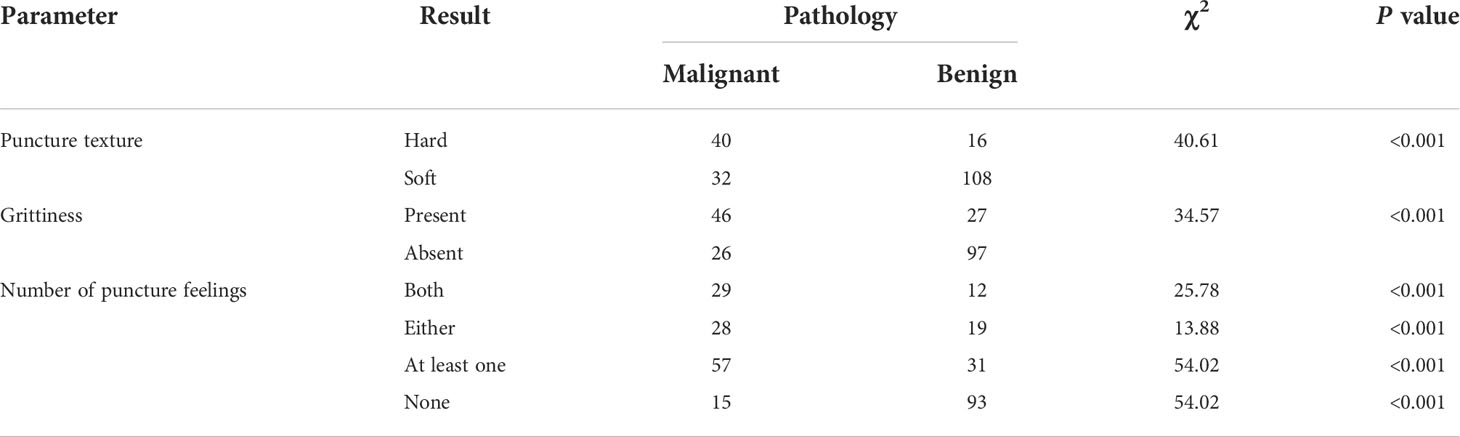
As shown in Table 2, there were significant differences between benign and malignant nodules with respect to the nodule texture (hard vs. soft) (P < 0.001) and presence of grittiness (P < 0.001) during the puncture.
As shown in Table 3, the puncture stiffness exhibited a diagnostic sensitivity of 55.56%, specificity of 87.10%, accuracy of 75.51%, PPV of 71.43%, and NPV of 77.14% in the diagnosis of benign and malignant thyroid nodules; while the puncture grittiness exhibited a diagnostic sensitivity of 63.89%, specificity of 78.22%, accuracy of 72.96%, PPV of 63.01%, and NPV of 78.86% in the differential diagnosis of benign and malignant thyroid nodules.
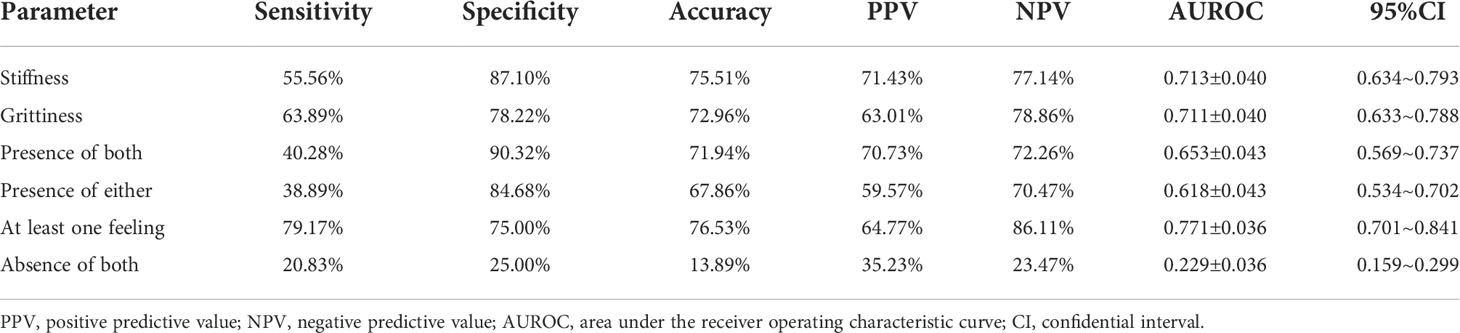
Table 3 Diagnostic performance of puncture feeling for thyroid nodules with indeterminate FNA findings.
In the differential diagnosis of benign and malignant thyroid nodules with indeterminate FNA findings, the presence of stiffness produced an AUROC of 0.713, while the presence of grittiness produced an AUROC of 0.711. When at least one of the both feelings were present, we can get the highest sensitivity, accuracy, NPC and AUROC of 0.778, 0.811, 0.853 and 0.764; when both hard texture and grittiness were present, the AUROC was 0.653 with the highest specificity of 90.32%. The diagnostic ROC curves are shown in Figure 1.
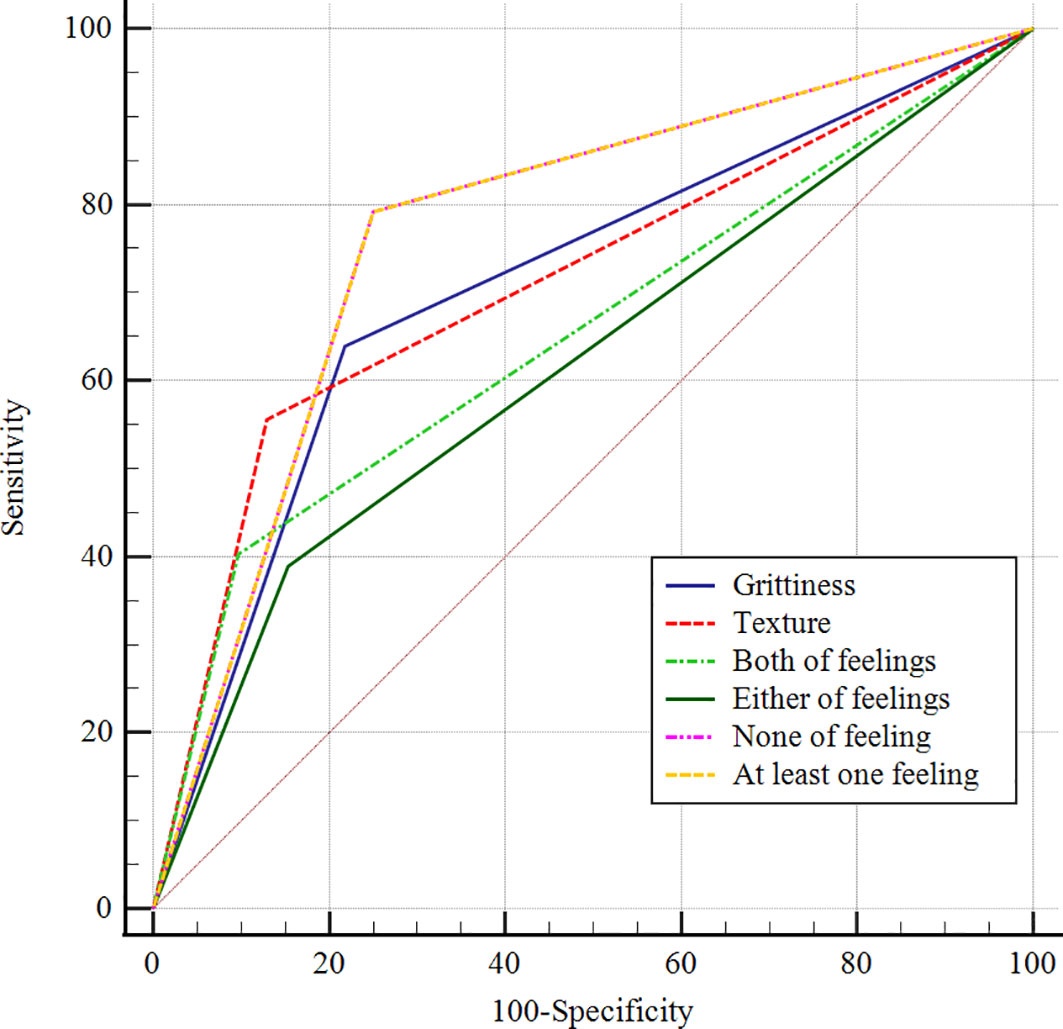
Figure 1 ROC curves for puncture feeling in the differential diagnosis of benign and malignant thyroid nodules with indeterminate FNA findings.
Due to the inflammatory processes can affect the feeling of stiffness and grittiness, we perform an analysis between the inflammatory lesion and malignant thyroid nodules. The puncture stiffness exhibited a diagnostic sensitivity of 55.56%, specificity of 86.96%, accuracy of 63.16%, PPV of 93.02%, and NPV of 38.46%; while the puncture grittiness exhibited a diagnostic sensitivity of 63.89%, specificity of 78.26%, accuracy of 67.37%, PPV of 90.20%, and NPV of 41.86% in the differential diagnosis of inflammatory and malignant thyroid nodules.
Discussion
FNA is one of the most reliable techniques for the diagnosis of thyroid malignancies and selection of treatment methods and has been recommended by numerous guidelines published in China and abroad (2, 13, 14). However, due to the ambiguities in the FNA findings, nodules with indeterminate pathological reports will often require patients to undergo repeat biopsy. In this study, we demonstrated that puncture feeling had some value in assisting the diagnosis of thyroid nodules with indeterminate pathological findings. Thus, reporting the puncture feeling can provide clinicians with auxiliary diagnostic evidence in cases with indeterminate pathological diagnosis.
Our findings revealed that the sensations of nodule texture perceived during puncture can serve as an auxiliary diagnostic method. Previous studies have demonstrated that malignant tumors exhibited a loss of normal orderly arrangement and an increase in density (15). Furthermore, the presence of proliferative stromal fibrosis in thyroid cancer tissues contributes to tumor hardening. In addition, the presence of calcifications, especially macrocalcifications, in malignant thyroid tumors can also increase their stiffness. Studies using ultrasound elastography have demonstrated that malignant thyroid tumors exhibit a significant higher stiffness than benign tumors (16). However, sonoelastography is more operator-dependent and may be subjected to some interfering factors (17). Moreover, the instrumentation requirements of this technique are not conducive to its widespread promotion in primary care settings. Despite the lack of an objective indicator for evaluating nodule stiffness in this study, the use of puncture feeling to determine the nodule stiffness was more direct. Therefore, this indicator can exclude patients with benign tumors more effectively, which in favor of reducing unnecessary repeat aspirations and diagnostic operation.
Our findings also indicate that puncture grittiness has clinical significance in aiding the diagnosis. The feeling of grittiness encountered during puncture may result from the friction between the nodule calcifications and the needle tip, while nodule microcalcifications are one of the distinct manifestations of malignant thyroid tumors, especially papillary thyroid carcinomas (18). According to histopathological studies, microcalcifications chiefly manifest as psammoma bodies. Psammoma bodies are currently defined as round concentric lamellar calcifications observed in the stroma of papillary carcinomas, and the exact mechanisms underlying their pathogenesis are poorly understood (19). However, they are detected in more than 50% of all papillary thyroid carcinomas (20). Owing to its unique nature, the puncture feeling of grittiness obtained good agreement among experienced operators (8), which also served as a basis for its reliability. In addition, compared with puncture texture, grittiness demonstrated a higher sensitivity, which enabled the more-effective screening of suspicious patients, thereby reducing a missed diagnosis in cases of an indeterminate pathological diagnosis.
Furthermore, our findings suggest that, for nodules with heterogenous texture, the lesion sites were often located in areas with hard texture and grittiness. Hence, focusing the biopsy to such areas can also improve the accuracy of FNA. In addition, providing timely remarks on the puncture feeling or suspicions in ultrasound diagnosis can also facilitate a targeted cytological diagnosis by pathologists, thereby reducing the risk of misdiagnosis.
The diagnostic performance of combining the two types of puncture feelings was also validated in this study. In the presence of both puncture feelings, the diagnostic specificity was 90.32%, which essentially reduced erroneous diagnosis of thyroid cancer, and reduced the pain and medical expenses caused by repeat aspiration. In the presence of at least one puncture feeling, the sensitivity was 79.17%, which reduced misdiagnosis and can serve as an indication for clinicians to arrange for a repeat aspiration promptly or switch to histological biopsy. Li has reported FNA combined with puncture feeling in the diagnosis of thyroid nodules (21). The result showed that the puncture feeling had a good PPV and NPV, which was similar to our result. However, their study included nodules with all Bethesda categories. 74% of them were classified as category V and VI and only 14% of them were classified as category I and III. In contrast, only non-diagnostic and indeterminate thyroid nodules were included in our study. Therefore, the results of our study are more valuable for the diagnosis of such nodules.
There are several limitations to this study. First, the subjectivity of the evaluation indicator (puncture feeling) may lead to significant disparities among different operators. We did not evaluate the concordance among physicians with different puncture experiences, which can be further explored in subsequent studies. Second, the puncture feeling produced in this study cannot be confirmed using objective indicators at present. Finally, this was a single-center retrospective study with a relatively small sample size, and it also did not include rare malignancies (e.g., undifferentiated carcinoma, metastatic carcinoma, etc.). Thus, the sample size should be further increased and prospective studies should be performed in the future.
In conclusion, puncture feeling during FNA may assist the diagnosis of thyroid nodules with indeterminate cytopathological findings, thereby providing the basis for reducing unnecessary repeat aspirations or preventing missed diagnoses. Hence, it has potential value in clinical application.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee of the Linzi Maternal and Child Health Care Hospital (Qidu Hospital). The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Acknowledgments
We are grateful to the patients who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Welch HG, Doherty GM. Saving thyroids - overtreatment of small papillary cancers. N Engl J Med (2018) 379:310–2. doi: 10.1056/NEJMp1804426
2. Tessler F, Middleton W, Grant E, Hoang J, Berland L, Teefey S, et al. ACR thyroid imaging, reporting and data system (TI-RADS): White paper of the ACR TI-RADS committee. J Am Coll Radiol JACR (2017) 14:587–95. doi: 10.1016/j.jacr.2017.01.046
3. Tanaka A, Hirokawa M, Suzuki A, Higuchi M, Kanematsu R, Yamao N, et al. Clinical significance and cytological detection of tracheal puncture following thyroid fine-needle aspiration: A retrospective study. Diagn Cytopathol (2021) 49:1116–21. doi: 10.1002/dc.24826
4. Cibas ES, Ali SZ. The 2017 Bethesda system for reporting thyroid cytopathology. Thyroid Off J Am Thyroid Assoc (2017) 27(11):1341–6. doi: 10.1089/thy.2017.0500
5. Kulstad R. Do all thyroid nodules >4 cm need to be removed? An evaluation of thyroid fine-needle aspiration biopsy in large thyroid nodules Endocr Pract. (2016) 22(7):791–8. doi: 10.4158/EP151150
6. Yoon JH, Moon HJ, Kim EK, Kwak JY. Inadequate cytology in thyroid nodules: should we repeat aspiration or follow-up? Ann Surg Oncol (2011) 18:1282–9. doi: 10.1245/s10434-011-1605-7
7. Poller DN, Glaysher S. Molecular pathology and thyroid FNA. CYTOPATHOLOGY (2017) 28:475–81. doi: 10.1111/cyt.12492
8. Saieg MA, Barbosa B, Nishi J, Ferrari A, Costa F. The impact of repeat FNA in non-diagnostic and indeterminate thyroid nodules: A 5-year single-centre experience. Cytopathology (2018) 29(2):196–200. doi: 10.1111/cyt.12508
9. Luo J, Zhang C, Huang F, Chen J, Sun Y, Xu K, et al. Risk of malignancy in thyroid nodules: predictive value of puncture feeling of grittiness in the process of fine-needle aspiration. Sci Rep (2017) 7:13109. doi: 10.1038/s41598-017-13391-3
10. Hu L, Liu X, Pei C, Xie L, He N. Assessment of perinodular stiffness in differentiating malignant from benign thyroid nodules. Endocr Connect (2021) 10:492–501. doi: 10.1530/EC-21-0034
11. Teng W, Liu Y, Gao M, Huang G, Zhao J, Shan Z, et al. China Anti-cancer associatio head and neck tumor proffessional committee. management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Chin J Pract Surg (2011) 31:908–14.
12. Alhashem MH, Alabidi A, Aly MG. The Bethesda system for reporting thyroid cytopathology: A retrospective review of its diagnostic utility at johns Hopkins aramco healthcare, Saudi Arabia. Am J Otolaryngol (2021) 42:103088. doi: 10.1016/j.amjoto.2021.103088
13. Haugen B, Alexander E, Bible K, Doherty G, Mandel S, Nikiforov Y, et al. American Thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc (2015) 2016:26 1–133. doi: 10.1089/thy.2015.0020
14. Zhou J, Yin L, Wei X, Zhang S, Song Y, Luo B, et al. Chinese Guidelines for ultrasound malignancy risk stratification of thyroid nodules: the c-TIRADS. ENDOCRINE (2020) 2020:70 256–279. doi: 10.1007/s12020-020-02441-y
15. Mahmud F, Siddique AB, Alam F, Siddique MI. Cytologically indeterminate follicular thyroid nodule on fine needle aspiration cytology is an indication for total thyroidectomy. Mymensingh Med J (2019) 28:434–40.
16. Kim H, Kim JA, Son EJ, Youk JH. Quantitative assessment of shear-wave ultrasound elastography in thyroid nodules: diagnostic performance for predicting malignancy. Eur Radiol (2013) 23:2532–7. doi: 10.1007/s00330-013-2847-5
17. Adamczewski Z, Stasiak M, Stasiak B, Adamczewska M, Lewiński A. Interobserver agreement and plane-dependent intraobserver variability of shear wave sonoelastography in the differential diagnosis of ectopic thymus tissue. J Clin Med (2021) 10(2):214. doi: 10.3390/jcm10020214
18. Brophy C, Stewart J, O'Donovan N, McCarthy J, Murphy M, Sheahan P. Impact of microcalcifications on risk of malignancy in thyroid nodules with indeterminate or benign cytology. Otolaryngol Head Neck Surg (2016) 154:46–51. doi: 10.1177/0194599815605326
19. Chernock RD, Lewis JS Jr. Classification of psammoma bodies in the revised college of American pathologists thyroid cancer protocol. Arch Pathol Lab Med (2015) 139:967. doi: 10.5858/arpa.2014-0483-LE
20. Clement KD, Emslie K, Maniam P, Wilson MSJ. What is the operative cost of managing acute appendicitis in the NHS: The impact of stump technique and perioperative imaging. World J Surg (2020) 44:749–54. doi: 10.1007/s00268-019-05306-2
Keywords: Fine needle aspiration (FNA), thyroid nodules, thyroid cancer, puncture feeling, ultrasound
Citation: Wu J, Li Y and Zhang M (2022) Clinical value of FNA puncture feeling in the diagnosis of non-diagnostic and indeterminate thyroid nodules. Front. Endocrinol. 13:1022438. doi: 10.3389/fendo.2022.1022438
Received: 18 August 2022; Accepted: 17 October 2022;
Published: 02 November 2022.
Edited by:
Erivelto Martinho Volpi, Centro de Referencia no Ensino do Diagnóstico por Imagem (CETRUS), BrazilReviewed by:
Qian Xiaoqin, Jiangsu University Affiliated People’s Hospital, ChinaJose Candido Xavier, Salesian University Center of São Paulo, Brazil
Copyright © 2022 Wu, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingbo Zhang, emhhbmdtaW5nYm9AMzAxaG9zcGl0YWwuY29t
 Jintao Wu1
Jintao Wu1 Yingying Li
Yingying Li