- 1Heilongjiang University of Chinese Medicine, Harbin, China
- 2First Affiliated Hospital, Heilongjiang University of Chinese Medicine, Harbin, China
- 3Heilongjiang Provincial Hospital, Harbin Institute of Technology, Harbin, China
Fertility, a social, cultural, and medical issue, has aroused public attention because of its potential to predict future health. In recent years, the incidence of male infertility has increased significantly, and various risk factors, such as congenital factors, acquired factors, and idiopathic factors, have led to this situation. Male infertility causes substantial psychological and social distress in patients. With the implementation of the two-child policy, male infertility has brought enormous psychological and social pressure and huge economic burden to patients and the healthcare system. This has attracted the attention of not only men of childbearing age but also many male experts. The conventional therapeutic approaches for treating male infertility, including drugs, varicocele surgery, intrauterine insemination, in vitro fertilization, and intracytoplasmic sperm injection, can restore fertility to a certain extent, but their efficacy is far from satisfactory, not to mention some adverse events. Therefore, acupuncture has been chosen by many men to treat their infertility and produced significant effects. In the present paper, the efficacy and mechanism of acupuncture in the treatment of male infertility were analyzed from different perspectives such as regulating hormone secretion, reducing inflammation, and improving semen parameters. The existing literature shows that acupuncture can effectively treat male infertility.
Introduction
Infertility is usually defined as being unable to get pregnant after unprotected intercourse for more than 12 months (1). It is estimated that approximately 15% of couples might suffer from infertility, of which the male factor accounts for nearly 50% (2, 3). Agawal et al. studied the regions and reports of male infertility rate according to the data of female infertility and reported that there are at least 30 million male infertility in the world (4). Although great advancements have been made, the etiology of more than half of male patients with infertility still cannot be determined (5).
Apart from increasing the burden on women, the lack of evaluation of male infertility often leads to neglect of several diseases. Numerous literatures suggest that there is an intimate association between male infertility and some medical conditions, including oncological, cardiovascular, autoimmune, and metabolic disorders, and even mortality (6). Several studies have illustrated that the impaired semen parameters (e.g., semen volume, sperm concentration, sperm motility, and total sperm count) have a positive correlation with the increased risk of sperm mortality (7, 8). Meanwhile, owing to not being covered by essential health insurance, the treatment of infertility imposes a considerable economic burden on patients and the healthcare system. Although the awareness of infertility has increased, its legislation covered by health insurance still needs cooperation from different apartments (9). Therefore, effective measures must be taken to avoid the above situation, especially the early diagnosis and proper management.
The treatment of male infertility needs to be formulated depending on individual etiology and need. Couples better quest for high-quality counseling to acquire proper diagnostic tests and the most appropriate therapy, including pharmacology, surgery, and assisted reproductive technology (10). However, some of the aforementioned methods are still controversial, for instance, the indications and surgical methods for varicocele repair (11). The semen parameter can be improved by varicocele repair in men with varicoceles and abnormal semen quality and quantity. However, current guidelines do not recommend varicocelectomy in infertile men with normal semen analysis or men with sub-clinical varicocele (12). In addition, these therapies also have some shortcomings, such as low live-birth rate, high cost, a long-cycle treatment, and adverse reactions. Complementary and alternative medicine (CAM) encompasses a broad set of practices including the use of acupuncture, natural products, and mind–body therapies, which is defined by the Centers for Disease Control (CDC) as a medical and healthcare system that differs from current conventional medicine (13, 14). Rayner et al. estimated that 29%–91% of fertility patients utilized a CAM method during their treatment (15). During fertility treatment, CAM could increase hope by incorporating cultural traditions of health and fertility (16). Meanwhile, it was also reported that CAM could increase the pregnancy rate and decrease stress and anxiety levels (17).
Acupuncture, a branch of traditional Chinese medicine (TCM), is a therapy that combines meridians, acupuncture points, and acupuncture methods to treat diseases for thousands of years in China (18). TCM believes that there is a network called meridians in the body to connect and coordinate the internal organs and surface tissues (19). During acupuncture treatment, needles are inserted into specific areas of the patient’s body called acupoints, which produces the sensations of soreness, numbness, fullness, or heaviness. These sensations are termed De Qi or Qi arriving, the process of which can regulate and re-balance the flow of Qi and can cure various diseases (20). A large number of studies have reported the efficacy and mechanism of acupuncture in the treatment of male infertility. This article describes acupuncture in treating male infertility from the efficacy to mechanism to provide an evidence-based decision about whether to use acupuncture in the treatment of male infertility.
Search strategies
In the present study, the literature including clinical trials, animal experiment, meta-analysis, and systematic reviews from January 1985 and January 2022 were retrieved from the database of PubMed and CNKI. The search strategy included “male infertility”, “asthenozoospermia”, “oligoasthenozoospermia”, “varicocele”, “erectile dysfunction”, “premature ejaculation”, “genital inflammation”, “acupuncture”, “electroacupuncture”, and “transcutaneous acupoint electrical stimulation”.
Causes of male infertility
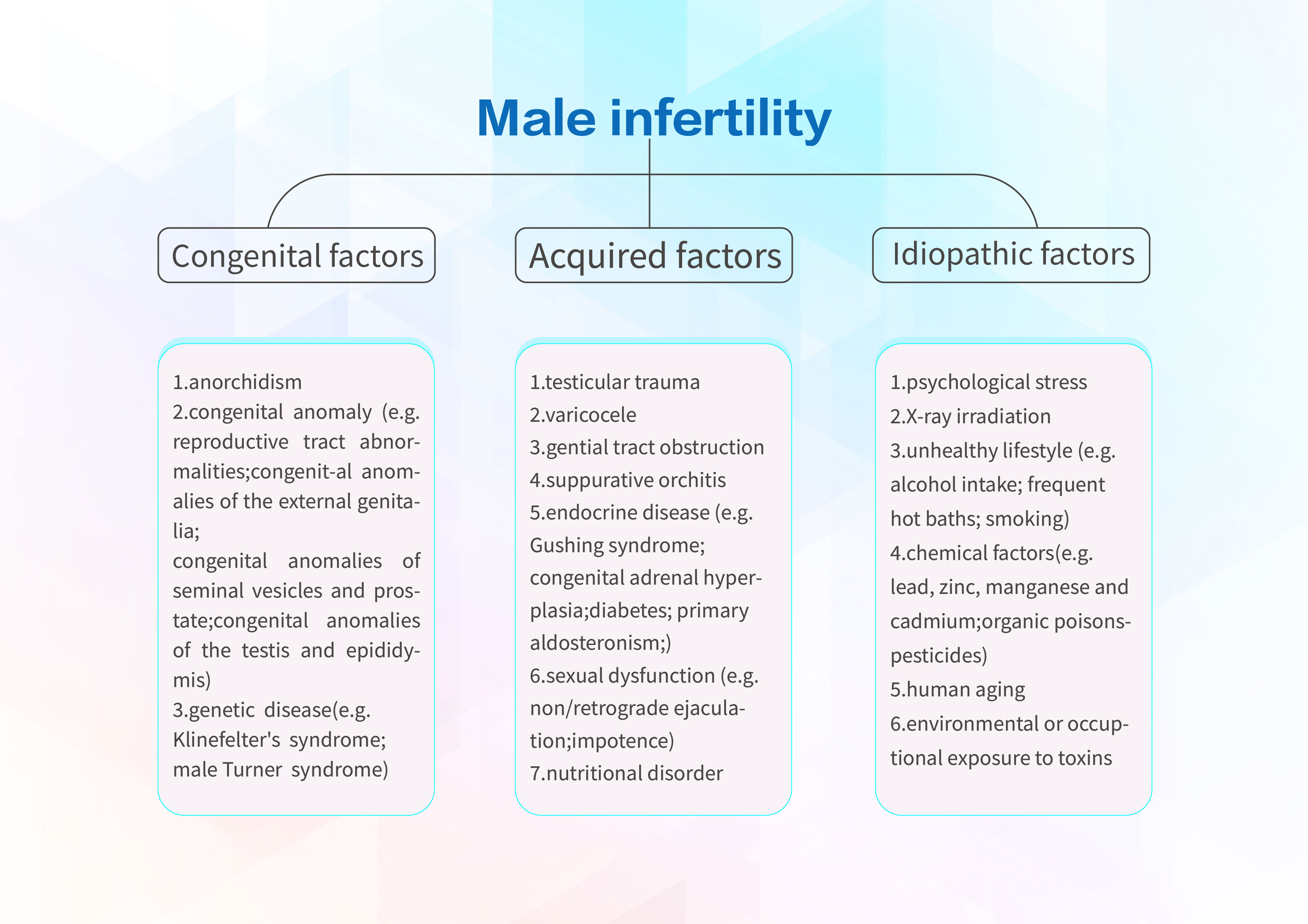
There are many causes of male infertility, which can be mainly categorized into congenital factors, acquired factors, and idiopathic factors. The major congenital causes are divided into anorchia, congenital anomaly (e.g., reproductive tract abnormalities, congenital anomalies of the external genitalia, congenital anomalies of seminal vesicles and prostate, congenital anomalies of the testis, and epididymis), and genetic disease (e.g., Klinefelter’s syndrome, male Turner syndrome) (21). Congenital bilateral absence of the vas deferens is the main cause of infertility caused by reproductive tract abnormalities. It is well known as obstructive azoospermia, which is caused by obstruction of sperm transport during ejaculation, therefore absenting the spermatozoa in the ejaculate (22). Acquired factors include testicular trauma, varicocele, reproductive tract obstruction, suppurative orchitis, endocrine disorders (e.g., gusher syndrome, congenital adrenal hyperplasia, diabetes mellitus, and primary aldosteronism), sexual dysfunction (e.g. non-retrograde ejaculation and impotence), and nutritional disorders. The research conducted by Giorgio Cavallini et al. has found that sperm abnormalities (e.g., poor sperm quality, low sperm counts, and reduced sperm motility) account for nearly 30% of male infertility (23). In addition, nearly 50% of cases do not have a clear pathogenesis and refer to as “idiopathic infertility” (24). Age is one of idiopathic factors, which is the most non-collectable cause of male infertility. Testosterone levels and sperm concentration decrease with age, although some aging men can still be fertile by attempting multiple intercourse (25). In addition, several cases of infertility may potentially be induced by occupational exposure to toxic chemicals and lifestyle factors including tobacco smoking (26) and alcohol intake (27), and psychological stress can cause endocrine disruptions leading to male infertility. Figure 1 shows all the causes and potential risks of male infertility.
Acupuncture
TCM has been utilized to treat and prevent various diseases for thousands of years. Acupuncture originated about 3,000 years ago in China. In ancient China, it was found that stimulating specific areas of the body can relieve pain. Afterward, during the Neolithic period, people utilized sharpened stones and bones as appliances for drawing blood or lancing abscesses, which might be associated with the origin of acupuncture (28). In the following centuries, with the development of smelting technology, various types of needles came into being and were used to treat diseases. The Yellow Emperor’s Classic of Internal Medicine (Huang Dei Nei Jing), the first comprehensive and specific acupuncture system, mentioned that the needling sensation is essential in operation (19). Needling sensation, also known as obtaining qi, is the feeling when the needles are punctured into acupoints and manipulated, as the patients usually feel numbness, pain, soreness, etc. The curative effect is usually better in patients who have these sensations than those who do not (29). Guided by meridian and acupoint theory, acupuncturists regard human as entirety and employ acupuncture to treat and prevent diseases. TCM believes that meridians are a network of pathways in the human body that connect and coordinate with the internal organs and surface tissues (30). Diseases are usually caused by interruptions in the flow of “Qi” and “blood” in the meridians. Inserting needles or stimulating acupoints using acupressure can regulate Qi and blood and, therefore, can be used to treat diseases because, according to this theory, diseases are usually caused by interruptions of Qi and “blood” flow in the meridians. Stimulating acupoints by acupuncture needles or acupressure can regulate Qi and blood and can treat diseases.
Acupuncture has been used for more than 1,000 years worldwide. Japan was the first country to incorporate acupuncture into its medical system. In the seventeenth century, Christian missionaries brought acupuncture to Europe (31). In the nineteenth century, Louis Berlioz, a French doctor, first proposed the idea of electroacupuncture (EA), which is a modern treatment derived from traditional acupuncture, and by doing so, he has added electrical stimulation to the acupuncture science and increased the stimulation methods (32). Ultimately, Zhu Longyu invented the first EA instrument in the 1950s and applied it to the clinic. Numerous clinical studies have shown that the combination of needle and electric stimulation could augment the stimulus and enhance therapeutic effects on diseases (33, 34). Transcutaneous acupoint electrical stimulation (TAES) is another extension of acupuncture, in which electrodes are placed on acupoints to stimulate them through electric current to exert analgesia or other therapeutic effects (35). In addition, acupoint injection, catgut embedding, auricular acupuncture, and laser acupuncture are also invented in acupuncture science.
Up to now, there are 103 countries around the world that approved the use of acupuncture, of which 29 have formulated corresponding laws or regulations, and even several countries have covered this treatment in their medical insurance system (36). It is an invasive technique with ultra-micro-trauma and is usually regarded as low risk if operated by experienced personnel (37). In addition, the adverse effects of acupuncture were substantially lower than those of drugs or other conventional medical procedures under identical conditions (38). The World Health Organization has announced the range of conditions treated by acupuncture in the respiratory, circulatory, alimentary, urinary, endocrine, nervous, cardio-cerebral, reproductive systems, etc. (39–41). Acupuncture treatment of male infertility has been recorded in many ancient classics. In recent years, a growing number of clinical and animal studies have been conducted to study the treatment of male infertility with acupuncture to observe its efficacy and explore the mechanism.
The overview of acupuncture in the treatment of male infertility
In China, the treatment of acupuncture for male infertility has a long history, which can be traced back to the classic A–B Classic of Acupuncture and Moxibustion (Zhen Jiu Jia Yi Jing) in the Western Jin Dynasty, nearly 2,000 years ago. The earliest study of acupuncture for male infertility in Western countries was conducted by Riegler et al. in 1984. They investigated the correlation between the effect of acupuncture on male fertility and psychological effects (42). The efficacy of treatment was evaluated by subjective parameters, namely, written psychological tests, and objective parameters, including concentration, volume, and motility of sperm before and after acupuncture. The result showed that apart from volume, the other sperm parameters increased significantly. Due to the fact that psychological test showed no change, it was suggested that the effect of acupuncture on improving sperm quality is not triggered by placebo mechanisms. This is the first report on the effectivity of acupuncture in treating male infertility in Western countries. In the following years, many countries around the world carried out studies on acupuncture treatment of male infertility and have reached similar conclusions (43–47). It was not until 2009 that Stefan Dieterle et al. designed the first prospective, randomized, single-blind, placebo-controlled trial of acupuncture for infertile patients with severe oligoasthenozoospermia based on the principles of TCM (48). A total of 57 patients were randomly assigned to receive either acupuncture or placebo acupuncture twice weekly for 6 weeks totally. The results showed that the percentage of motile sperm in the acupuncture arm is significantly higher than that in the placebo arm, which supports the significance of acupuncture in men with severe oligoasthenozoospermia.
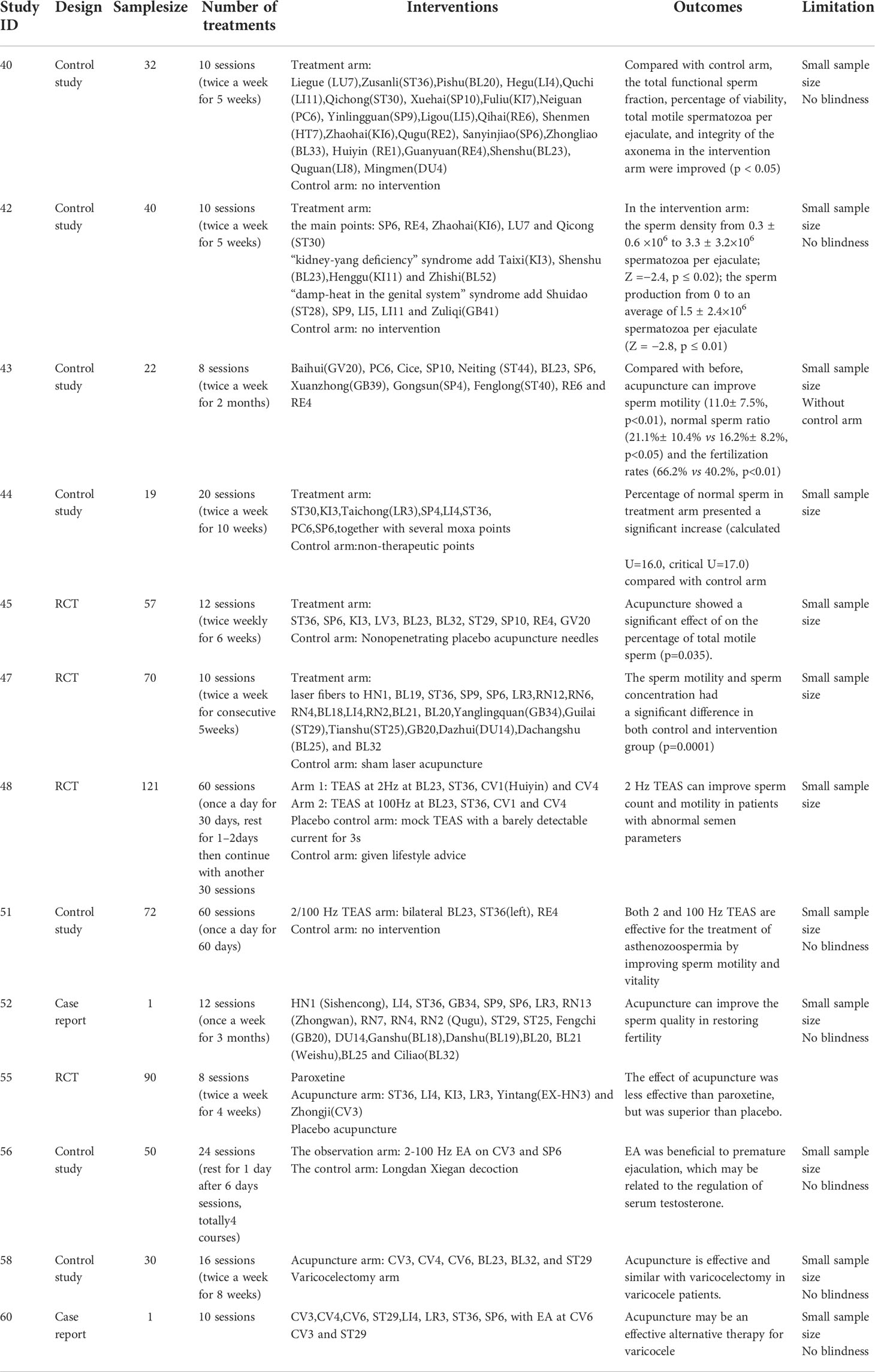
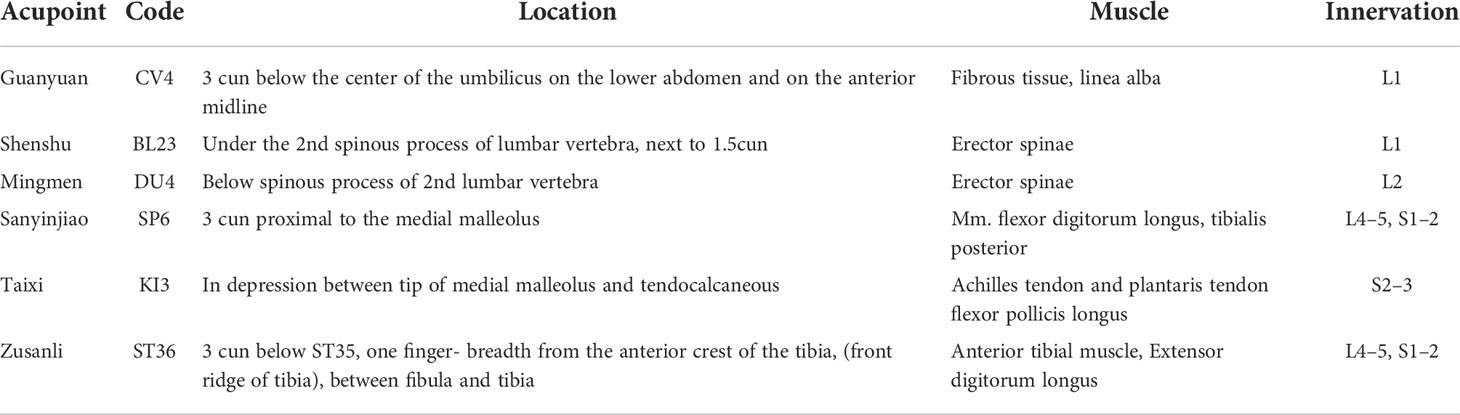
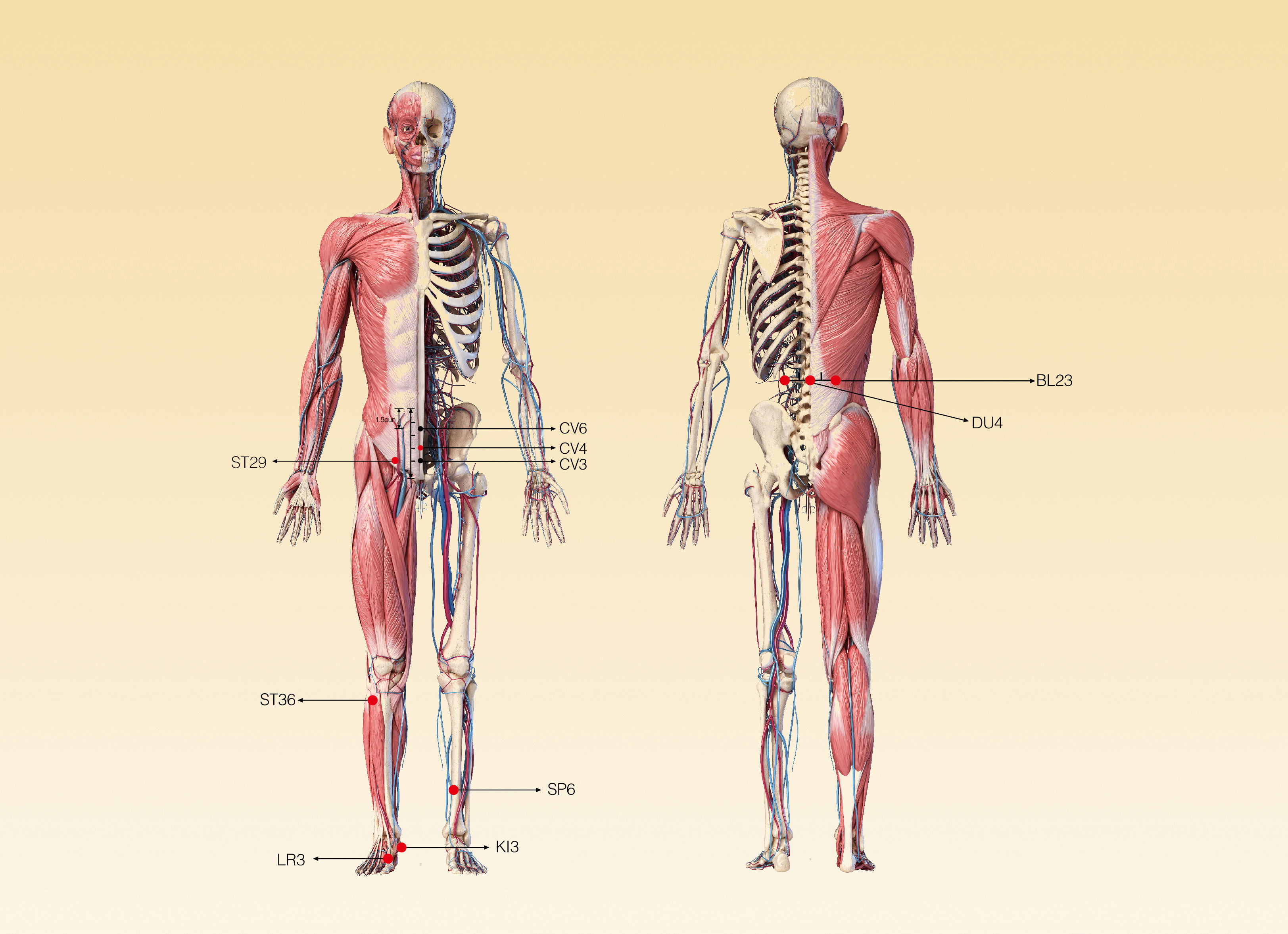
Many scholars in the world have carried out in-depth study on acupuncture and created many new acupuncture therapies, such as the ones combining modern science and technology with traditional acupuncture that have been widely used. Cakmak et al. (49) has performed a prospective, randomized study to clarify the effect of the short-term EA on testicular blood flow (TBF) in men. This is the first study to show a point- and frequency-specific effects of EA on TBF, namely, a significant increase in TBF at 10 Hz within 5 min upon stimulation of Guilai (ST-29). More recently, a clinical trial on semen parameters in infertile patients with oligospermia has demonstrated that compared with the sham laser acupuncture group, the motility and concentration of sperm had a significant increase in the laser acupuncture group (p=0.0001) (50). In addition, since the laser probe is only in contact with the body surface, it is minimally invasive; therefore, it is safer, more convenient, and better tolerated by patients. A study evaluating the effect of transcutaneous electrical acupuncture point stimulation (TEAS) on sperm parameters found that 2 Hz TEAS can improve sperm count and motility in patients with abnormal semen parameters (51). With the increasing number of male infertility patients, there are more and more studies on acupuncture treatment of male infertility. In 2015, some scholars from Chengdu University of Traditional Chinese Medicine and Gansu University of Chinese Medicine in China searched and analyzed Chinese literature on acupuncture for male infertility (52). By analyzing the included 94 studies, they noticed that a total of 69 acupoints can be needled to treat male infertility, including 3 extra-meridian acupoints, 18 auricular acupoints, and 3 scalp acupoints. Among them, there are 15 acupoints with a frequency of more than 10 times, and CV4 (Guanyuan), BL23 (Shenshu), DU4 (Mingmen), SP6 (Sanyinjiao), KI3 (Taixi), and ST36 (Zusanli) are used as the basic acupoints for the clinical treatment of male infertility (the location of these acupoints are shown in Figure 1). Furthermore, some acupoints can be added or subtracted according to different TCM patterns. Meanwhile, several meta-analyses on whether acupuncture performed to improve male fertility was effective and safe have been published. Among them, the one conducted by Fang You et al. (53) has systematically assessed the effect of acupuncture on men with oligoasthenozoospermia. Based on the included 12 randomized controlled trials with 1,088 participants, acupuncture or acupuncture together with another intervention was effective in improving the semen quality. The efficacy of acupuncture on the treatment of male infertility is introduced further as follows.
Clinical effect and mechanism of acupuncture on male infertility
Semen parameters
Semen quality is usually considered to be a surrogate measure of fecundity in male fertility and pregnancy assessments. Abnormal semen parameters were found in approximately 50% of men evaluated for infertility (54). A comprehensive meta-regression analysis report demonstrated that during the past half a century, the number of sperm and other sperm parameters have shown a significant decline trend (55). Apart from oligoasthenospermia, other diseases that cause male infertility due to semen quality include oligospermia, asthenozoospermia, and teratozoospermia (56). In 1997, Siterman et al. (43) conducted a prospective controlled study to evaluate the effect of acupuncture on men who suffered from subfertility due to sperm impairment. After the treatment, all semen parameters of the 16 acupuncture-treated subfertile patient semen parameters such as total functional sperm fraction, percentage of viability, total motile spermatozoa per ejaculate, and integrity of the axonema were increased significantly compared with control group (p ≤ 0.05). Jin ZiRun et al. (57) investigated the effect of TEAS in the treatment of asthenozoospermia by needling acupoints BL23 bilaterally, left ST36, and CV4 once a day for 60 days. Compared with the sperm motility and vitality in baseline, TEAS treatment, either 2 or 100 Hz, significantly increased sperm motility and the percentage of grade a+b sperm in the asthenozoospermic patients. A Macedonian young infertile couple received acupuncture treatment in Skopje, Macedonia. After the treatment, the sperm quality of the man and ovarian function of the woman were restored, and their endocrine system was balanced (58). A prospective, controlled, and blind study was conducted by Gurfinkel, Edson et al. (47) to assess the effect of acupuncture and moxibustion on the semen quality in patients with semen abnormalities. After the treatment, compared with the control arm who received acupuncture and moxibustion at non-therapeutic acupoints, the ratio of the normal form sperm increased significantly in the treatment group.
The endocrine system is the main regulator of female and male reproductive function (59). The hypothalamic–pituitary-gonadal axis (HPGA), the regulatory center of reproductive endocrine activities, plays a role in maintaining normal reproductive function. The gonadotropin-releasing hormone (GnRH) secreted by the hypothalamus promotes the secretion of follicle stimulating hormone (FSH) and luteinizing hormone (LH) in the anterior pituitary. In men, FSH stimulates the Sertoli cells (SCs) to produce androgen binding protein (ABP), which formats the barrier of the blood–testis (60). FSH could increase the number of SCs and promote spermatogonial maturation by action on SC receptors. LH could act on interstitial Leydig cell, which is in synergism with the action of FSH on SCs (61), to aid in steroidogenesis and production of testosterone, thereby taking part in the appropriate regulation of spermatogenesis and consistency in semen quality. The abnormal level of FSH and LH would decrease testosterone synthesis. Testosterone, an androgenic steroid, is essential for the continuation of the normal spermatogenesis cycle and plays an integral role in spermatogenesis, sperm maturation, and sperm release. Whatever the reason, low levels of testosterone in the testes could reduce sperm production, leading to reduced fertility and even infertility.
The increased level of FSH and LH in low-fertility men are related to the damage of spermatogenic epithelium and stromal cells in testicular seminiferous tubules (62). A study conducted by Liu et al. found that EA can effectively reduce FSH and LH levels of adenine-induced spermatogenesis dysfunction model rats (63). Another study has shown that needling “Zhibian (BL54) through Shuidao (ST28)” and acupuncture on BL23 for 28 days can significantly reduce the level of LH in rats (64). Interestingly, other studies have also reached similar conclusion that acupuncture could significantly reduce the level of FSH and LH in patients with oligoasthenospermia (65, 66), which suggests that acupuncture may help reduce the damage of testicular seminiferous epithelium and mesenchymal cells caused by abnormal levels of FSH and LH, thereby improving male fertility. Acupuncture can also increase androgen levels in infertile men. Zeng et al. carried out a study on the effects of EA on cytochrome P450 side-chain lyase (P450scc) and steroid growth factor-1 (SF-1) in the testis of middle-aged and elderly rats with partial androgen deficiency syndrome (PADAM). The results showed that acupuncture on BL23 and CV4 could significantly increase the level of total testosterone and free testosterone in PADAM rats and improve the pathological manifestations of Leydig cells and SCs in the testis (67). Furthermore, Ren et al. also reached the same conclusion (68). Compared with PADAM rats, the levels of serum TT and FT were significantly increased; the protein and mRNA expression of P450scc, 17β-hydrox-ysteroid dehydrogenase 3 (17β-HSD3) and SF-1 were significantly increased in PADAM+EA rats. Therefore, the mechanism of acupuncture regulating androgen expression may be related to P450scc, SF-1, and 17β-HSD3.
It has been indicated that the poor sperm parameters are related to the changes in calcium and integrin-binding protein 1 (CIB1) and cell cycle regulator cyclin-dependent kinase 1 (CDK1). The imbalance of CDK1 or other cell cycle regulators can interfere with the normal interval of SC proliferation, resulting in the disproportion between SCs and germ cells, which increases germ cell apoptosis and leads to spermatogenesis defects (69). A clinical experimental study conducted by Yu Yan et al. has suggested that after treatments of TEAS 30 min daily for 30 days, the sperm count and motility in patients with abnormal semen parameters have improved, which is associated with the increased seminal plasma zinc, NAG, and fructose and the upregulation of CIB1 and downregulation of CDK1 (51). SCs, responsible for endocrine and paracrine duties, provide physical and nutritional support to germ cells during spermatogenesis (70). However, both physical and chemical alterations of SCs’ cytoskeleton could severely influence spermatogenesis (71). It has been indicated that after 10 sessions of EA, the sperm count, weight, sperm concentration, and sperm motility have increased. These improvements were connected with disrupted expression of cytoskeletal proteins of SCs and enhanced proliferation of germ cells with reduced apoptosis of germ cells (72). Its mechanism that EA enhances germ cell proliferation by improving the function of SCs facilitates the recovery of spermatogenesis and normal semen parameters in subfertile men (73). The research carried out by Jin ZiRun et al. found a novel mechanism for the pathogenesis of asthenozoospermia. The downregulation of CatSper channel in the sperm might be a contributor or a downstream indicator for asthenozoospermia, while 2 Hz TEAS or EA can be beneficial to recover through inducing the functional upregulation of CatSper channels in the sperm (74).
Varicocele
The debate that varicocele causes male infertility has been going on for more than half a century. Male infertility caused by varicocele is the most easily cured, and even several patients are capable of having children without intervention (75). Varicocele, a kind of vascular disease, is manifested by abnormal dilatation and tortuosity of the pampiniform plexus veins, which can be observed in 35%–44% among men with primary infertility and 45%–81% with secondary infertility (75). Increasing lines of evidence have suggested that varicocele-mediated infertility is not triggered by a factor alone but is the result of the synergy of multiple factors, such as oxidative stress, hypoxia, and nutrient deprivation (76). At present, a large number of studies show that acupuncture can effectively treat male infertility mediated by varicocele. Kucuk et al. (77) conducted a study to compare the effect of the acupuncture with subinguinal microscopic varicocelectomy on sperm parameters and pregnancy rates in patients with primary infertility. They found that the efficacy of acupuncture seems to be equivalent to varicocelectomy in the primary infertile patients with semen abnormalities. Compared to the varicocelectomy arm, the increased sperm concentration was higher in the acupuncture arm (p = 0.039), and the pregnancy rate was the same in both arms (33%). Subsequently, Chen Dong et al. (78) evaluated the curative effect by observing the rheological indices of infertile patients with varicocele after acupuncture. One hundred nine cases in the treatment group received acupuncture, while the other 106 participants were administrated with drugs. After treatment, the diameter of varicocele in patients with grades I and II in the two groups was decrease (p<0.05), and the diameter of varicocele in patients with grade II in the treatment group was more significantly narrowed (p<0.01). Meanwhile, all sperm parameters were improved with longer fluidized time in the treatment group, which were better than those in the control group (p<0.05). A case report about the treatment of acupuncture in varicocele concluded that acupuncture could be an alternative therapy for varicocele (79). The patient received 10 sessions of treatments on acupoints including CV4, Taichong (LR3), ST36, SP6 with manual manipulation, and Zhongji (CV3), Qihai (CV6), and bilateral ST29 with EA; then, the symptom disappeared. The conclusion is acupuncture may be an effective alternative therapy for varicocele.
The exact mechanism of varicocele-induced male infertility is still not fully understood. It is a growing recognition that scrotal hyperthermia, a faulty venous valve causing the reflux of toxic metabolites, elevated hydrostatic pressure in testis, hypoxia, oxidative stress, and Leydig cell dysfunction are the proposed mechanisms for varicocele-induced male infertility (80). Both the overproduction of reactive oxygen species (ROS) and antioxidant deficiency can lead to oxidative stress. Studies have found that ROS levels including malondialdehyde (MDA) in seminal plasma of patients suffering from varicocele are increased, with a significant positive correlation with varicocele degree (81). Furthermore, varicocele is associated with the reduction in local and systemic antioxidant defense, including the reduction in antioxidant substances such as superoxide dismutase (SOD). Extensive research has shown that infertile men have lower levels of antioxidants in their semen (82). Current evidence shows that acupuncture can treat diseases by inhibiting oxidative stress. An animal experiment conducted by Zhang et al. (83) investigated the effect of acupuncture on the antioxidation function of the testis. After needling on CV4 and ST36, the activity of nitric oxide (NO), nitricoxide synthase, SOD, and catalase increased significantly, while the levels of lipid peroxide and MDA decreased markedly in the testis of elderly mice.
In addition, the reduced arterial blood flow of the testis and the reversed pressure gradient between the arterioles and venules might result in testicular hypoxia, thereby aging the testis and impairing spermatogenesis (84, 85). A prospective randomized study by Cakmak et al. (48) found that peak systolic velocity, volume flow, end-diastolic velocity, and the diameter and area of testicular artery were significantly improved after 10 Hz EA for ST29. Based on the results, its possible mechanisms were similarly mediated as a reflex response by the testicular sympathetic nerves controlled by supraspinal pathways. Yu et al. (86) reported a male adolescent patient with varicocele who was treated with an innovative acupuncture therapy, Fu subcutaneous acupuncture (FSN), and found that the patient’s testicular pain, abnormal dilatation, and tortuosity of the spermatic veins were significantly relieved, which might be through the mechanisms of improving relaxation of muscle compression and increasing local blood reperfusion to restore blood flow. Needle pricking therapy stimulates the sympathetic trunk and regulates the function of the gonadal axis and abdominal arteries and veins, which can significantly reduce the blood flow viscosity of varicocele-induced infertility, thereby increasing the testicular blood flow perfusion and oxygen supply and promoting blood circulation to eliminate varicocele (78, 87). In conclusion, acupuncture can enhance blood supply in the testicular artery, decrease the testicular temperature by heat exchange in the pampiniform plexus, and interrupt the perioxidation process, thereby providing a suitable environment for sperm survival, and then increase sperm concentration and improve fertility (88, 89).
Reproductive system infection
Studies have found that 12%–35% of infertile men have had male reproductive system infection (90). Inflammatory damage to the testis, epididymis, and prostate can lead to changes in spermatogenesis, transport, and function. Clinically, many infertile men are usually complicated with prostatitis and epididymitis. Antibiotics are the mainstays of method in clinical practice; however, only one aspect could be relieved and seemed to have similar effects with placebo (91), and the efficacy tends to decline after drug withdrawal. In addition, the increased incidence of adverse events must be taken into consideration if used in the long term (92). Therefore, more and more patients utilize alternative therapies or antibiotics combined with acupuncture. In a study of fertility-related parameters in middle-aged men, normal sperm parameters were significantly reduced in patients with type II and III prostatitis, suggesting that prostatitis can lead to poor semen quality (93). Sun et al. (94) recruited a total of 440 men with prostatitis to receive 8-week acupuncture treatment. The results showed that acupuncture could significantly improve urination symptoms, pain, and sexual function in patients with prostatitis, with an effective rate of 60.6% (95%CI, 53.7%–67.1%). A study conducted by Siterman Shimon et al. (95) to verify whether acupuncture has an effect on the sperm output in patients suffering from inflammation of the genital tract with low sperm density. After treatment, the scrotal skin temperature and sperm concentration were improved, which suggested that acupuncture can be recommended for these men. Other studies have reached similar conclusions, but the reports lack indicators such as sperm motility related to male infertility. Larger randomized controlled clinical trials would be indispensable in the future to provide more convincing evidence for acupuncture in the treatment of male infertility caused by reproductive system infections.
Inflammation could raise the temperature of the testis/scrotum (96). Studies have found that a too high scrotal temperature can result in faster metabolism and increased oxygen consumption and impaired local microcirculation (95). The limited blood flow in the testes is insufficient to satisfy microcirculation, resulting in hypoxia and production of reactive oxygen species (97). The arterial blood flow of the testis decreases with each passing day in a body under oxidative stress. Pressure gradients between venous and arterial blood flow and impaired microcirculation may result in hypoxia of the testis. Testicular arterial blood flow reduction, hypoxia, and other pathological conditions may lead to testicular aging and impaired spermatogenesis. It has been proven in experimental research that the mechanism of acupuncture against aged rats with low testosterone is to reduce the inflammatory factors including NF-κB p65, COX-2, TNFα, and IL1β of Leydig cells, thereby promoting the synthesis of testosterone (98). It has been proven that acupuncture can produce anti-inflammatory effect by inhibiting the synthesis of cyclooxygenase in peripheral and central injurious sites (99). Apart from this, due to the systemic immunoregulatory actions of acupuncture, acupuncture itself might not eliminate pathogenic microorganisms but can be achieved by stimulating the body’s immune response (95, 100).
Male sexual dysfunction
Erectile dysfunction (ED) and premature ejaculation (PE) are the two most common sexual dysfunction in men, which have affected 10%–52% of men in the world, as shown by epidemiological data (101). Sexual dysfunction usually occurs in men of reproductive age, and severe cases can lead to infertility (102). Now, more people seek complementary and alternative method for sexual dysfunction. The current evidence suggests that acupuncture might have beneficial effects on ED and PE. A prospective study conducted by Engelhardt et al. (103) investigated the efficacy of acupuncture in psychogenic erectile dysfunction (pED) patients. Twenty enrolled patients were randomized into the treatment group (acupuncture for ED) and placebo group (acupuncture against headache). After treatment, 68.4% participants in the treatment group received a satisfactory response, whereas 9% in the placebo group (p=0.0017), reaching the conclusion that acupuncture could be an effective option in patients with pED. Sunay, Didem et al. (104) carried out a study to determine the effectiveness of acupuncture in treating PE. Ninety patients were randomized into paroxetine, acupuncture, and sham acupuncture groups. After the treatment for twice a week for 4 weeks, they found the efficacy administrated by paroxetine was significantly better than that of acupuncture (p=0.001). However, the acupuncture had a significant stronger ejaculation-delaying effect than sham acupuncture. Studies have shown that EA can improve the symptoms of premature ejaculation by regulating the level of serum testosterone (105). Although most studies on acupuncture in the treatment of sexual dysfunction have some methodological problems including small sample sizes and lack of blindness, almost all current studies can prove the efficacy of acupuncture in the treatment of sexual dysfunction, at least better than placebo.
The initiation of penile erection is achieved by external stimulation of the somatic and autonomic nerves, and the perineal striated muscle is stimulated by sympathetic postganglionic fibers to maintain normal penile relaxation (106). The autonomic nerve contains sympathetic and parasympathetic fibers and originates from an important branch of the pelvic plexus, the cavernous nerve. The parasympathetic postganglionic fibers are distributed in the penile vascular smooth muscle, cavernous smooth muscle, and cavernous sinus small bundle column smooth muscle, and play a crucial role in the process of penile erection (107). The somatic nerves originating from the pudendal nerve transmit information to the spinal erection center located at the T12-L1 segment and the reflex erection center at S2–S4 to participate in reflex erection. Acupuncture on most acupoints located here can significantly increase the excitability of the spinal erection center, thereby improving the erection state (108). Therefore, its mechanism is related to the modification of sensory afferent impulses at the spinal level (109). For PE, it has been documented that acupuncture can treat PE through changes in central and peripheral neurotransmitters and neurohormones secretion and alter in blood flow regulation (110). It is also possible, although speculative, that acupuncture may alter the secretion of neurotransmitters such as selective serotonin-reuptake inhibitors (SSRIs), as shown in Sunay’s study (104). It has also been demonstrated that acupuncture promotes the release of serotonin, which plays a role in the central regulation of the ejaculatory reflex under the influence of several brain centers (111, 112). Table 1 lists some of the studies mentioned above. The location, regional anatomy, and innervation of acupoints for male infertility mentioned above are described in Table 2 and Figure 2.
The controversy on acupuncture in the treatment of male infertility
In fact, it is not difficult to see that there are many defects in current studies on acupuncture treatment of infertility or improvement of male fertility, such as non-randomized controlled trials, and small sample size, which result in insufficient convincing conclusions of such clinical trials. Some studies have reported that sham acupuncture, placebo acupuncture, etc. used in the control group in acupuncture clinical trials can also produce therapeutic effects (113, 114). There are also studies showing that acupuncture versus placebo acupuncture has no statistically significant effect on in vitro fertilization outcomes (115). In addition, a meta-analysis conducted by Wen Jia et al. (116) suggested that compared with medications or sham acupuncture, acupuncture alone has no clear superiority in improving sperm quality. Although acupuncture may have the similar effect to medications, the considerable clinical heterogeneity and the poor methodological quality among the included studies made the present evidence inadequate to draw a definite conclusion. One crucial matter must be mentioned, that is, in the theory of TCM, the selection of acupoints is usually based on the different TCM syndrome types of diseases depending on the symptoms and signs of patients. However, to facilitate understanding and interpretation, the treatment protocol of the clinical acupuncture trials should be a fixed one, which followed the revised Consolidated Standards for Reporting Trials (CONSORT) statement (117). When the effect of acupuncture is evaluated, the TCM theory would be ignored due to the consideration of randomized controlled trial (RCT). Therefore, this standardization might weaken the effect of acupuncture in individual patients (48). In the future, some larger sample size, prospective, double-blind, placebo-controlled randomized controlled trials are needed to provide more convincing evidence of acupuncture in the treatment of male infertility, or we can spare no effort to update the standards for reporting interventions in controlled trials of acupuncture.
Safety of acupuncture in the treatment of male infertility
In most cases, acupuncture is relatively safe, with few adverse events let alone serious complications (118). Short-term adverse events such as faint, stuck needle, bending of the needle, needle breakage, and hematoma may occur during the treatment if unqualified acupuncturists operate improperly, which can be avoided by careful manipulation. There are few reports on the adverse events of male infertility treated by acupuncture. In an RCT, among all patients, only one patient in the intervention arm reported dizziness and was relieved within 24 h under non-treatments (50). However, in other studies, there were adverse reactions related to acupuncture treatment. An in vitro fertilization (IVF) RCT conducted by Caroline A. Smith et al. reported that among 848 participants, 152 women had mild discomfort or bruises (119). In a prospective observational study enrolled that 229,230 patients to evaluate the safety of acupuncture, 8.6% participants reported experiencing at least one adverse events and 2.2% required treatment (120). Briefly, adverse events do occur during the acupuncture treatment, but to a large extent, they are mostly minor compared with non-acupuncture-related interventions.
Summary
It is estimated that infertility has affected approximately 8%–12% of couples during reproductive age around the world (121). A Global Burden of Disease Survey reported that the age-standardized prevalence of male infertility has increased by 0.291% per year over the past 20 years (122). The current clinical therapy has shortcomings such as unsatisfactory efficacy, high cost, and many adverse reactions. Acupuncture, an adjuvant therapy, has aroused the curiosity of many scholars because of its controversial efficacy and mechanism. The merits of acupuncture in treating male infertility mainly include the following: (1) the advantages of acupuncture for male infertility include no side effects, few adverse effects, and low cost; (2) the combination of acupuncture and conventional therapy can improve the efficacy of male infertility; and (3) from the perspective of TCM, acupuncture can regulate the body as a whole, thereby treating male infertility. Currently, there are still some limitations in the existing studies, such as the lack of rigorous methodology and small sample size. Taken together, the present study not only summarizes the efficacy and mechanism of acupuncture for male infertility but supplies several instructive acupoints for clinic application as well. More high-quality RCTs and basic experiments are needed to provide a more persuasive evidence for the clinical application of acupuncture and more specific mechanism in treating male infertility.
Author contributions
YZ: funding acquisition. JF, HH and YW: conceptualization and writing—original draft preparation. XZ, XYZ, TZ and MZ: editing. XW and YZ: supervision. All authors contributed to the article and approved the version.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82074259), the Project of Cultivation project of outstanding youth fund of Heilongjiang University of Chinese Medicine (grant number 2018jc02), and “Outstanding Young Academic Leaders” scientific research project of Heilongjiang University of Chinese Medicine to YZ.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, De Mouzon J, Sokol R, et al. The international glossary on infertility and fertility care, 2017. Hum Reprod (2017) 32:1786–801. doi: 10.1093/humrep/dex234
2. Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, Sundaram R, et al. Prevalence of infertility in the united states as estimated by the current duration approach and a traditional constructed approach. Fertil Steril (2013) 99:1324–1331.e1. doi: 10.1016/j.fertnstert.2012.11.037
3. Committee P, Society A. Diagnostic evaluation of the infertile female: A committee opinion. Fertil Steril (2015) 103:e44–50. doi: 10.1016/j.fertnstert.2015.03.019
4. Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol (2015) 13:1–9. doi: 10.1186/s12958-015-0032-1
5. Aston KI, Conrad DF. A review of genome-wide approaches to study the genetic basis for spermatogenic defects. Methods Mol Biol (2013) 927:397–410. doi: 10.1007/978-1-62703-38-0_34
6. Choy JT, Eisenberg ML. Male infertility as a window to health. Fertil Steril (2018) 110:810–4. doi: 10.1016/j.fertnstert.2018.08.015
7. Jensen TK, Jacobsen R, Christensen K, Nielsen NC, Bostofte E. Good semen quality and life expectancy: A cohort study of 43,277 men. Am J Epidemiol (2009) 170:559–65. doi: 10.1093/aje/kwp168
8. Eisenberg ML, Li S, Behr B, Cullen MR, Galusha D, Lamb DJ, et al. Semen quality, infertility and mortality in the USA. Hum Reprod (2014) 29:1567–74. doi: 10.1093/humrep/deu106
9. Strasser MO, Dupree JM. Care delivery for male infertility: The present and future. Urol Clin North Am (2020) 47:193–204. doi: 10.1016/j.ucl.2019.12.006
10. Szamatowicz M, Szamatowicz J. Proven and unproven methods for diagnosis and treatment of infertility. Adv Med Sci (2020) 65:93–6. doi: 10.1016/j.advms.2019.12.008
11. Kirby EW, Wiener LE, Rajanahally S, Crowell K, Coward RM. Undergoing varicocele repair before assisted reproduction improves pregnancy rate and live birth rate in azoospermic and oligospermic men with a varicocele: a systematic review and meta-analysis. Fertil Steril (2016) 106:1338–43. doi: 10.1016/j.fertnstert.2016.07.1093
12. Salonia A, Bettocchi C CJ, et al. EAU guidelines on sexual and reproductive health(2020). Available at: https://uroweb.org/wp-content/uploads/EAUGuidelines-on-Sexual-and-Reproductive-Health.
13. Complementary, alternative or integrative health: What’s in a name? Available at: https://nccih.nih.gov/health/integrative-health.
14. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United states, 2007. Natl Health Stat Rep (2008).
15. Rayner JA, Willis K, Burgess R. Women’s use of complementary and alternative medicine for fertility enhancement: A review of the literature. J Altern Complement Med (2011) 17:685–90. doi: 10.1089/acm.2010.0435
16. Read SC, Carrier ME, Whitley R, Gold I, Tulandi T, Zelkowitz P. Complementary and alternative medicine use in infertility: Cultural and religious influences in a multicultural canadian setting. J Altern Complement Med (2014) 20:686–92. doi: 10.1089/acm.2013.0329
17. Aelion A, Barbieri E, Shastri S, Grill E, Chung P, Rosenwaks Z. The use of complementary medicaltherapies (CMT) in infertility patients. Fertil Steril (2009) 92:S33–4. doi: 10.1016/j.fertnstert.2009.07.130
18. Chen H, Yang M, Ning Z, Lam WL, Zhao YKY, et al. A guideline for randomized controlled trials of acupuncture. doi: 10.1142/S0192415X19500010
19. Dong HG, Zhang XR, Chaudhury RRRU. An overview of traditional Chinese medicine. In: Chaudhury RR, Rafei UM (eds), Traditional Medicine in Asia.,” In: Press RO for S-EA, editor. New Delhi (2001), 17–28.
20. Chen T, Zhang WW, Chu YX, Wang YQ. Acupuncture for pain management: Molecular mechanisms of action. Am J Chin Med (2020) 48:793–811. doi: 10.1142/S0192415X20500408
21. Agarwal A, Baskaran S, Parekh N, Cho CL, Henkel R, Vij S, et al. Male infertility. Lancet (2021) 397:319–33. doi: 10.1016/S0140-6736(20)32667-2
22. Carson SA, Kallen AN. Diagnosis and management of infertility: A review. JAMA - J Am Med Assoc (2021) 326:65–76. doi: 10.1001/jama.2021.4788
23. Cavallini G. Male idiopathic oligoasthenoteratozoospermia. Asian J Androl (2006) 8:143–57. doi: 10.1111/j.1745-7262.2006.00123.x
24. Krausz C. Male infertility: Pathogenesis and clinical diagnosis. Best Pract Res Clin Endocrinol Metab (2011) 25:271–85. doi: 10.1016/j.beem.2010.08.006
26. Bundhun PK, Janoo G, Bhurtu A, Teeluck AR, Soogund M, Pursun M. Tobacco smoking and semen quality in infertile males: A systematic review and meta-analysis. J Urol (2019) 202:446. doi: 10.1097/01.JU.0000574400.71886.27
27. Bai S, Wan Y, Zong L, Li W, Xu X, Zhao Y, et al. Association of alcohol intake and semen parameters in men with primary and secondary infertility: A cross-sectional study. Front Physiol (2020) 11:566625. doi: 10.3389/fphys.2020.566625
28. Zhu J, Li J, Yang L, Liu S. Acupuncture, from the ancient to the current. Anat Rec (2021) 304:2365–71. doi: 10.1002/ar.24625
30. Zhang J, Yang L, Du J, Shi N, Song X, Xian T, et al. Research status and development strategies of mox standardization. Zhongguo Zhen Jiu (2020) 40:273–6.
31. Chon TY, Lee MC. Acupuncture. Mayo Clin Proc (2013) 88:1141–6. doi: 10.1016/j.mayocp.2013.06.009
33. Chi YL, Zhang WL, Yang F, Su F, Zhou YK. Transcutaneous electrical acupoint stimulation for improving postoperative recovery, reducing stress and inflammatory responses in elderly patient undergoing knee surgery. Am J Chin Med (2019) 47:1445–58. doi: 10.1142/S0192415X19500745
34. Li X, Dai Q, Shi Z, Chen H, Hu Y, Wang X, et al. Clinical efficacy and safety of electroacupuncture in migraine treatment: A systematic review and network meta-analysis. Am J Chin Med (2019) 47:1755–80. doi: 10.1142/S0192415X19500897
35. Qu F, Li R, Sun W, Lin G, Zhang R, Yang J, et al. Use of electroacupuncture and transcutaneous electrical acupoint stimulation in reproductive medicine: a group consensus. J Zhejiang Univ Sci B (2017) 18:186–93. doi: 10.1631/jzus.B1600437
36. Wen J, Chen X, Yang Y, Liu J, Li E, Liu J, et al. Acupuncture medical therapy and its underlying mechanisms: A systematic review. Am J Chin Med (2021) 49:1–23. doi: 10.1142/S0192415X21500014
37. Franconi G, Manni L, Aloe L, Mazzilli F, Giambalvo Dal Ben G, Lenzi A, et al. Acupuncture in clinical and experimental reproductive medicine: A review. J Endocrinol Invest (2011) 34:307–11. doi: 10.3275/7500
38. Organization WH. Acupuncture: Review and analysis of reports on controlled clinical trials. Parkinsonism Relat Disord (2003), S163. doi: 10.1016/S1353-8020(11)70706-4
39. Jia Y, Xing H LVJ, Shi J, Sun Y, Li X, et al. Regularities of clinical application of hand acupuncture therapy to treatment of various diseases based on data mining. Acupunct Res (2019) 44:220–5. doi: 10.13702/j.1000-0607.180237
40. Qiao L, Guo M, Qian J, Xu B, Gu C, Yang Y. Research advances on acupuncture analgesia. Am J Chin Med (2020) 48:245–58. doi: 10.1142/S0192415X20500135
41. Riegler R, Fischl F, Bunzel B, Neumark J. Korrelation psychischer veränderungen und spermiogrammverbesserungen nch akupunktur [Correlation of psychological changes and spermiogram improvements following acupuncture]. Urologe A (1984) 23:329–33.
42. Riegler R, Fischl F, Bunzel B, Neumark J. Korrelation psychischer veränderungen und spermiogrammverbesserungen nch akupunktur [Correlation of psychological changes and spermiogram improvements following acupuncture]. Urologe A (1984) 23:329–33.
43. Siterman S, Eltes F, Wolfson V, Zabludovsky N, Bartoov B. Effect of acupuncture on sperm parameters of males suffering from subfertility related to low sperm quality. Arch Androl (1997) 39:155–61. doi: 10.3109/01485019708987914
44. Zheng Z. Analysis on the therapeutic effect of combined use of acupuncture and mediation in 297 cases of male sterility. J Tradit Chin Med (1997) 03:190–7. doi: 10.19852/j.cnki.jtcm.1997.03.007
45. Sherman S, Eltes F, Wolfson V, Lederman H, Bartoov B, Gan R. Does acupuncture treatment affect sperm density in males with very low sperm count? A pilot study (2000) 39:31–9.
46. Zhang M, Huang G, Lu F, Paulus WE, Sterzik K. Influence of acupuncture on idiopathic male infertility in assisted reproductive technology. J Huazhong Univ Sci Technol - Med Sci (2002) 22:228–30. doi: 10.1007/bf02828187
47. Gurfinkel E, Cadenho AP, Yamamura Y, Srougi M. Effects of acupuncture and moxa treatment in patients with semen abnormalities. Asian J Androl (2003) 5:345–8.
48. Dieterle S, Li C, Greb R, Bartzsch F, Hatzmann W, Huang D. A prospective randomized placebo-controlled study of the effect of acupuncture in infertile patients with severe oligoasthenozoospermia. Fertil Steril (2009) 92:1340–3. doi: 10.1016/j.fertnstert.2009.02.041
49. Cakmak YO, Akpinar IN, Ekinci G, Bekiroglu N. Point- and frequency-specific response of the testicular artery to abdominal electroacupuncture in humans. Fertil Steril (2008) 90:1732–8. doi: 10.1016/j.fertnstert.2007.08.013
50. Allameh F, Razzaghi M, Hosseini S, Barati M, Razzaghi Z, Salehi S, et al. The effect of laser acupuncture on semen parameters in infertile men with oligospermia: A randomized clinical trial. J Lasers Med Sci (2021) 12. doi: 10.34172/JLMS.2021.84
51. Yu Y, Bin SS, Zhang B, Guan Q, Liang M, Zhao LG, et al. Effects and mechanism of action of transcutaneous electrical acupuncture point stimulation in patients with abnormal semen parameters. Acupunct Med (2019) 37:25–32. doi: 10.1136/acupmed-2017-011365
52. Qian Z, Wei S, Zhong Z, Jian Z, Yi L. A study on the regular of acupoint selection of acupuncture and moxibustion for male infertility in contemporary literature. J Jiangxi Univ Chin Med (2015) 27:99–101.
53. You F, Ruan L, Zeng L, Zhang Y. Efficacy and safety of acupuncture for the treatment of oligoasthenozoospermia: A systematic review. Andrologia (2020) 52:1–9. doi: 10.1111/and.13415
55. Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, et al. Temporal trends in sperm count: A systematic review and meta-regression analysis. Hum Reprod Update (2017) 23:646–59. doi: 10.1093/humupd/dmx022
56. Nareswari I, Lestari SW, Notonegoro C. Acupuncture therapy for severe oligoasthenoteratozoospermia. Med Acupunct (2021) 33:302–5. doi: 10.1089/acu.2020.1513
57. Jin ZR, Liu BH, Tang WH, Jiang H, Zhang R, Han JS, et al. Transcutaneous electrical acupoint stimulation for asthenozoospermia. Natl J Androl (2017) 23:73–7.
58. Zhu J, Arsovska B, Kozovska K. Acupuncture treatment for fertility. Open Access Maced J Med Sci (2018) 6:1685–7. doi: 10.3889/oamjms.2018.379
60. Dutta S, Sengupta P MS. Male reproductive hormones and semen quality. Asian Pac J Reprod (2019) 8:189–94. doi: 10.4103/2305-0500.268132
61. Czieselsky K, Prescott M, Porteous R, Campos P, Clarkson J, Steyn FJ, et al. Pulse and surge profiles of luteinizing hormone secretion in the mouse. Endocrinology (2016) 157:4794–802. doi: 10.1210/en.2016-1351
62. Ali H, Baig M, Rana MF, Ali M, Qasim R, Khem AK. Relationship of serum and seminal plasma zinc levels and serum testosterone in oligospermic and azoospermic infertile men. J Coll Physicians Surg Pak (2005) 15:671–3.
63. Lu Y, Liu S, He S, Ju Z, Xia YY. Effect of electroacupuncture on serum FSH and LH in a rat model of spermatic abnormalities induced by adenine. Shanghai J Acupunct Moxibustion (2014) 33:70–1. doi: 10.13460/j.issn.1005-0957.2014.01.0070
64. Yunming C, Huizhen J, Jiaru L, Yupeng Y, Jiahong S, Huashan R, et al. Experimental study on' Zhibian (BL54) through shuidao (ST28) ’acupuncture therapy for rats with asthenospermia and oligospermia. J Shanxi Univ Chin Med (2021) 22:26–28+32. doi: 10.19763/j.cnki.2096-7403.2021.01.07
65. Lingkan C, Minyao G. Clinical observation of effects of transcutaneous electrical acupoint stimulation on asthenospermia patients with deficiency of kidney essence. Shanghai J Tradit Chin Med (2016) 50:44–46+66. doi: 10.16305/j.1007-1334.2016.12.014
66. Yiming S, Shida L, Yue L, Li L. Effect of acupuncture on the regulation of hypothalamic pituitary testicular axis dysfunction in the treatment of oligoasthenospermia. J Clin Acupunct Moxibustion (2015) 31:25–7.
67. Tingting Z, Taiwan Y, Xuezhi L, Tang C. Electroacupuncture intervention increases testosterone level of aged rats by activating ERK/Nrf2/HO-1 signaling of leydig cells. Acupunct Res (2019) 44:566–570+582. doi: 10.13702/j.1000-0607.180790
68. Ren Y, Yang X, Zhang Y, Wang Y, Li X. Effects and mechanisms of acupuncture and moxibustion on reproductive endocrine function in male rats with partial androgen deficiency. Acupunct Med (2016) 34:136–43. doi: 10.1136/acupmed-2014-010734
69. Sun W, Guan Q, Wen J, Zhang Q, Yang W, Zhang B, et al. Calcium- and integrin-binding protein-1 is down-regulated in the sperm of patients with oligoasthenozoospermia: CIB1 expression in patients with oligoasthenozoospermia. J Assist Reprod Genet (2014) 31:541–7. doi: 10.1007/s10815-014-0177-4
70. Dimitriadis F, Tsiampali C, Chaliasos N, Tsounapi P, Takenaka A, Sofikitis N. The sertoli cell as the orchestra conductor of spermatogenesis: Spermatogenic cells dance to the tune of testosterone. Hormones (2015) 14:479–503. doi: 10.14310/horm.2002.1633
71. Johnson KJ. Testicular histopathology associated with disruption of the sertoli cell cytoskeleton. Spermatogenesis (2014) 4:e979106. doi: 10.4161/21565562.2014.979106
72. Cui Tw, Qin M, Liu Bx, Gao Yx, Ma Wj, Zhang Xp. Effect of electroacupuncture on spermatogenesis in rats with oligozoospermia of insufficiency of shen (Kidney) essence syndrome. Chin J Integr Med (2019) 25:292–7. doi: 10.1007/s11655-018-2915-9
73. Gao J, Zuo Y, So K-H, Yeung WSB, Ng EHY, Lee K-F. Electroacupuncture enhances spermatogenesis in rats after scrotal heat treatment. Spermatogenesis (2012) 2:53–62. doi: 10.4161/spmg.19282
74. Jin ZR, Fang D, Liu BH, Cai J, Tang WH, Jiang H, et al. Roles of CatSper channels in the pathogenesis of asthenozoospermia and the therapeutic effects of acupuncture-like treatment on asthenozoospermia. Theranostics (2021) 11:2822–44. doi: 10.7150/THNO.51869
75. Jensen CFS, Østergren P, Dupree JM, Ohl DA, Sønksen J, Fode M. Varicocele and male infertility. Nat Rev Urol (2017) 14:523–33. doi: 10.1038/nrurol.2017.98
76. Fang Y, Su Y, Xu J, Hu Z, Zhao K, Liu C, et al. Varicocele-mediated male infertility: From the perspective of testicular immunity and inflammation. Front Immunol (2021) 12:729539. doi: 10.3389/fimmu.2021.729539
77. Kucuk EV, Bindayi A, Boylu U, Onol FF, Gumus E. Randomised clinical trial of comparing effects of acupuncture and varicocelectomy on sperm parameters in infertile varicocele patients. Andrologia (2016) 48:1080–5. doi: 10.1111/and.12541
78. Chen D, He X, Chen Z, Hu L, Zhong J, Hong Y, et al. Effect of needle pricking therapy on rheological indices and efficacy for infertile patients with varicocele. Chin J Integr Tradit West Med (2017) 37:326–30.
79. Zhang Y, Xu H, Wu Y, Chen X. Recurrent varicocele. Explore (NY) (2022) 18:604–7. doi: 10.1016/j.explore.2021.07.001
80. Arya D, Balasinor N, Singh D. Varicocele associated male infertility: cellular and molecular perspectives of pathophysiology. Andrology (2022). doi: 10.1111/andr.13278
81. Pasqualotto FF, Sundaram A, Sharma RK, Borges E, Pasqualotto EB, Agarwal A. Semen quality and oxidative stress scores in fertile and infertile patients with varicocele. Fertil Steril (2008) 89:602–7. doi: 10.1016/j.fertnstert.2007.03.057
82. Barati E, Nikzad H, Karimian M. Oxidative stress and male infertility: current knowledge of pathophysiology and role of antioxidant therapy in disease management. Cell Mol Life Sci (2020) 77:93–113. doi: 10.1007/s00018-019-03253-8
83. Zhang GW, Li YD, Li JN, Zhou YC, Wang X. Influence of acupuncture at zusanli and guanyuan on antioxidation and ultrastructure of testicle tissue in aged mice. Chin J Tissue Eng Res (2006) 27:85–87+193.
84. Gat Y, Gornish M, Navon U, Chakraborty J, Bachar GN, Ben-Shlomo I. Right varicocele and hypoxia, crucial factors in male infertility: Fluid mechanics analysis of the impaired testicular drainage system. Reprod BioMed Online (2006) 13:510–5. doi: 10.1016/S1472-6483(10)60638-4
85. Gat Y, Zukerman Z, Chakraborty J, Gornish M. Varicocele, hypoxia and male infertility. fluid mechanics analysis of the impaired testicular venous drainage system. Hum Reprod (2005) 20:2614–9. doi: 10.1093/humrep/dei089
86. Yu X, Li T, Zhuang Z, Li Y, Xie D, Li Z, et al. Treatment of varicocele with fu’s subcutaneous needling: A case report. Med (United States) (2019) 98:4–7. doi: 10.1097/MD.0000000000016983
87. Dong C, Zhong J, Chen S, Xiao Y, Deng L, Zhang Y, et al. Clinical observation on needle pricking therapy for chronic prostatitis with semen abnormality. Chin J Integr Tradit West Med (2012) 32:1139–41.
88. Litscher G. Bioengineering assessment of acupuncture, part 3: Ultrasound. Crit Rev BioMed Eng (2006) 34:295–326. doi: 10.1615/critrevbiomedeng.v34.i4.20
89. Yu Y, Kang J, Shumin D. Clinical studies on treatment of chronic prostatitis with acupuncture and mild moxibustion. (2005) 03:177–81. doi: 10.19852/j.cnki.jtcm.2005.03.005
90. Henkel R, Offor U, Fisher D. The role of infections and leukocytes in male infertility. Andrologia (2021) 53:1–19. doi: 10.1111/and.13743
91. Nickel JC, Krieger JN, McNaughton-Collins M, Anderson RU, Pontari M, Shoskes DA, et al. Alfuzosin and symptoms of chronic prostatitis–chronic pelvic pain syndrome. N Engl J Med (2008) 359:2663–73. doi: 10.1056/NEJMoa0803240
92. Paterson C, Kennedy C. Pharmacological interventions for treating chronic prostatitis/chronic pelvic pain syndrome. Res Nurs Heal (2020) 43:548–9. doi: 10.1002/nur.22027
93. Ausmees K, Korrovits P, Timberg G, Punab M, Mändar R. Semen quality and associated reproductive indicators in middle-aged males: The role of non-malignant prostate conditions and genital tract inflammation. World J Urol (2013) 31:1411–25. doi: 10.1007/s00345-013-1078-3
94. Sun Y, Liu Y, Liu B, Zhou K, Yue Z, Zhang W, et al. Efficacy of acupuncture for chronic prostatitis/chronic pelvic pain syndrome: A randomized trial. Ann Intern Med (2021) 174:1357–66. doi: 10.7326/M21-1814
95. Siterman S, Eltes F, Schechter L, Maimon Y, Hanny Lederman BB. Success of acupuncture treatment in patients with initially low sperm output is associated with a decrease in scrotal skin temperature. Asian J Androl (2009) 11:200–8. doi: 10.1038/aja.2008.4
96. Rew KT, Langan RC, Miriam Hadj-Moussa JJH. Men’s health: Scrotal and testicular conditions. FP Essent (2021) 503:23–7.
97. Ritchie C, Ko EY. Oxidative stress in the pathophysiology of male infertility. Andrologia (2021) 53. doi: 10.1111/and.13581
98. Taiwan Y, Jia L, Xuezhi L, Lin M, Jiapeng W, Xiaofang X, et al. Effect of electroacupuncture on chronic inflammatory reaction of testicular interstitial cells in aged rats with low testosterone. Acupunct Res (2018) 43:163–8. doi: 10.13702/j.1000-0607.170705
99. Lee JH, Jang KJ, Lee YT, Choi YH, Choi BT. Electroacupuncture inhibits inflammatory edema and hyperalgesia through regulation of cyclooxygenase synthesis in both peripheral and central nociceptive sites. Am J Chin Med (2006) 34:981–8. doi: 10.1142/S0192415X06004454
100. Kavoussi B, Ross BE. The neuroimmune basis of anti-inflammatory acupuncture. Integr Cancer Ther (2007) 6:251–7. doi: 10.1177/1534735407305892
101. Tsai MY, Liu CT, Chang CC, Chen SY, Huang ST. Overview of the relevant literature on the possible role of acupuncture in treating male sexual dysfunction. Acupunct Med (2014) 32:406–10. doi: 10.1136/acupmed-2014-010592
102. Lotti F, Maggi M. Sexual dysfunction and male infertility. Nat Rev Urol (2018) 15:287–307. doi: 10.1038/nrurol.2018.20
103. Engelhardt PF, Daha LK, Zils T, Simak R, König K, Pflüger H. Acupuncture in the treatment of psychogenic erectile dysfunction: First results of a prospective randomized placebo-controlled study. Int J Impot Res (2003) 15:343–6. doi: 10.1038/sj.ijir.3901021
104. Sunay D, Sunay M, Aydoǧmuş Y, Baǧbanci S, Arslan H, Karabulut A, et al. Acupuncture versus paroxetine for the treatment of premature ejaculation: A randomized, placebo-controlled clinical trial. Eur Urol (2011) 59:765–71. doi: 10.1016/j.eururo.2011.01.019
105. Lu X, Han H, Zhang Z, Chen H, Huang X, Zhang R. Study on the efficacy of electric acupuncture in the treatment of premature ejaculation based on testosterone level. J Healthc Eng (2022) 2022:3–6. doi: 10.1155/2022/8331688
106. Leisegang K, Finelli R. Alternative medicine and herbal remedies in the treatment of erectile dysfunction: A systematic review. Arab J Urol (2021) 19:323–39. doi: 10.1080/2090598X.2021.1926753
107. Pastuszak AW. Current diagnosis and management of erectile dysfunction. Curr Sex Heal Rep (2014) 6:164–76. doi: 10.1007/s11930-014-0023-9
108. Wang H, Zhao M, Zhang J, Yan B, Liu S, Zhao F, et al. The efficacy of acupuncture on patients with erectile dysfunction: A review. Evidence-Based Complement Altern Med (2022) 2022. doi: 10.1155/2022/4807271
109. Sezai Yaman L, Kilic S, Sarica K, Bayar M, Saygin B. The place of acupuncture in the management of psychogenic impotence. Eur Urol (1994) 26:52–5. doi: 10.1159/000475342
111. Waldinger MD. Contribution of acupuncture to western medical knowledge of premature ejaculation: An intriguing new development. Eur Urol (2011) 59:772–4. doi: 10.1016/j.eururo.2011.02.018
113. Chen H, Lim CED. The efficacy of using acupuncture in managing polycystic ovarian syndrome. Curr Opin Obstet Gynecol (2019) 31:428–32. doi: 10.1097/GCO.0000000000000582
114. Rowe T. Acupuncture and reproduction. J Obstet Gynaecol Canada (2010) 32:1023–4. doi: 10.1016/S1701-2163(16)34704-1
115. Coyle ME, Stupans I, Abdel-Nour K, Ali H, Kotlyarsky M, Lie P, et al. Acupuncture versus placebo acupuncture for in vitro fertilisation: a systematic review and meta-analysis. Acupunct Med (2021) 39:20–9. doi: 10.1177/0964528420958711
116. Jia W, Wang C, Yin Y. Acupuncture for oligospermia and asthenozoospermia: A systematic review and meta-analysis. Med (United States) (2021) 100. doi: 10.1097/MD.0000000000027816
117. Moher D, Schulz KF, DGA. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Lancet (2001) 357:1191–4. doi: 10.1016/S0140-6736(00)04337-3
118. Park J, Sohn Y, White AR, Lee H. The safety of acupuncture during pregnancy: A systematic review. Acupunct Med (2014) 32:257–66. doi: 10.1136/acupmed-2013-010480
119. Smith CA, De Lacey SI, Chapman M, Ratcliffe J, Norman RJ, Johnson NP, et al. Effect of acupuncture VS sham acupuncture on live births among women undergoing in vitro fertilization a randomized clinical trial. JAMA - J Am Med Assoc (2018) 319:1990–8. doi: 10.1001/jama.2018.5336
120. Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: results of a prospective observational study with 229, 230 patients and introduction of a medical information and consent form. Forsch Komplementmed (2009) 16:91–7. doi: 10.1159/000209315
121. Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem (2018) 62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012
Keywords: male infertility, acupuncture, abnormal semen parameters, male sexual dysfunction, varicocele, genital inflammation
Citation: Feng J, He H, Wang Y, Zhang X, Zhang X, Zhang T, Zhu M, Wu X and Zhang Y (2022) The efficacy and mechanism of acupuncture in the treatment of male infertility: A literature review. Front. Endocrinol. 13:1009537. doi: 10.3389/fendo.2022.1009537
Received: 02 August 2022; Accepted: 21 September 2022;
Published: 18 October 2022.
Edited by:
Rossella Cannarella, University of Catania, ItalyReviewed by:
Elena Eugeni, University of Perugia, ItalyFilomena Mottola, University of Campania Luigi Vanvitelli, Italy
Copyright © 2022 Feng, He, Wang, Zhang, Zhang, Zhang, Zhu, Wu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoke Wu, eGlhb2tld3UyMDAyQHZpcC5zaW5hLmNvbQ==; Yuehui Zhang, Y2hpemlzaHVpLTA0QDE2My5jb20=
†These authors have contributed equally to this work
 Jiaxing Feng
Jiaxing Feng Hui He
Hui He Yu Wang2†
Yu Wang2†