- 1Renal Division, Department of Medicine, Peking University First Hospital, Peking University Institute of Nephrology, Beijing, China
- 2Research Units of Diagnosis and Treatment of Immune-mediated Kidney Diseases, Chinese Academy of Medical Sciences, Beijing, China
- 3Advanced Institute of Information Technology, Peking University, Hangzhou, China
- 4Key Laboratory for Earth Surface Processes of the Ministry of Education, College of Urban and Environmental Sciences, Peking University, Beijing, China
- 5School of Public Health, Peking University, Beijing, China
- 6National Institute of Health Data Science at Peking University, Beijing, China
- 7National Climate Center, China Meteorological Administration, Beijing, China
Background: Accumulated researches revealed that both fine particulate matter (PM2.5) and sunlight exposure may be a risk factor for obesity, while researches regarding the potential effect modification by sunlight exposure on the relationship between PM2.5 and obesity are limited. We aim to investigate whether the effect of PM2.5 on obesity is affected by sunlight exposure among the general population in China.
Methods: A sample of 47,204 adults in China was included. Obesity and abdominal obesity were assessed based on body mass index, waist circumference and waist-to-hip ratio, respectively. The five-year exposure to PM2.5 and sunlight were accessed using the multi-source satellite products and a geochemical transport model. The relationship between PM2.5, sunshine duration, and the obesity or abdominal obesity risk was evaluated using the general additive model.
Results: The proportion of obesity and abdominal obesity was 12.6% and 26.8%, respectively. Levels of long-term PM2.5 ranged from 13.2 to 72.1 μg/m3 with the mean of 46.6 μg/m3. Each 10 μg/m3 rise in PM2.5 was related to a higher obesity risk [OR 1.12 (95% CI 1.09-1.14)] and abdominal obesity [OR 1.10 (95% CI 1.07-1.13)]. The association between PM2.5 and obesity varied according to sunshine duration, with the highest ORs of 1.56 (95% CI 1.28-1.91) for obesity and 1.66 (95% CI 1.34-2.07) for abdominal obesity in the bottom quartile of sunlight exposure (3.21-5.34 hours/day).
Conclusion: Long-term PM2.5 effect on obesity risk among the general Chinese population are influenced by sunlight exposure. More attention might be paid to reduce the adverse impacts of exposure to air pollution under short sunshine duration conditions.
Introduction
Obesity represents a severe public health challenge globally. The prevalence of obesity came to a high level recently, exceeding 13% globally, and contributed to a decline in both quality of life and life expectancy (1–3). The Nutrition and Chronic Disease Status of Chinese Residents (2020) estimated that 16.4% of the Chinese adult residents were obese, and obesity prevalence was increasing (4). Obesity has been attributed to behavioral, genetic, socioeconomic, and environmental factors. Furthermore, air pollution has been considered as one of the main environmental causes affecting obesity (5).
Ambient fine particulate matter (PM2.5) has emerged as a major air pollution globally. A recent cross-sectional research of 2660 children suggested that PM2.5 was positively related to a high obesity risk (6). Meanwhile, meteorological factors, such as sunlight, are also regarded as novel potential environmental risk factors for obesity. Previous studies on sunlight exposure have shown that sunlight exposure decreased the risk of obesity (7). Recent in vitro and animal experiments have indicated that PM2.5 and limited sunlight exposure have several physiological effects in common, including systematic inflammation, insulin resistance, and stimulation of the differentiation of pre-adipocytes via reduction of serum vitamin D (8). These effects are all potentially linked with the pathogenesis of obesity. Therefore, it is far more likely that sunlight could modified the contribution of PM2.5 to obesity. Nevertheless, evidence for the potential impact of PM2.5 on obesity under different sunlight conditions is limited. Moreover, for countries with relatively high levels of PM2.5 like China, it is necessary to assess the sunlight effect on the relationship of PM2.5 with obesity.
Therefore, the research aimed to examine the relationship of PM2.5 and sunlight exposure with obesity risk among the general population in China using a national representative sample.
Material and Methods
Study Population
A sample of the general Chinese residents aged ≥18 years was obtained from September 2009 to September 2010, using a multistage, stratified, probability-proportional-to-size sampling method. We obtained participants from 13 provinces (Beijing, Sichuan, Inner Mongolia Autonomous Region, Jiangsu, Xinjiang Uyghur Autonomous Region, Ningxia Hui Autonomous Region, Zhejiang, Guangxi Zhuang Autonomous Region, Guangdong, Shanghai, Hubei, Hunan, and Shandong) in China. Information on participants’ sociodemographic status, lifestyle, and health history was obtained. Each questionnaire and on-site examination including anthropometric measurement was finished at community medical centers or hospitals by medical students, trained primary care physicians, and nurse practitioners. Detailed data collection and measuring methods have been mentioned previously (9). The study population for this survey included 47,204 participants with completed questionnaire and health examinations, and recruitment was conducted when participants’ addresses could be well-followed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Each subject provided informed written consent before data collection. The ethics committee at Peking University First Hospital approved the study (Approval number: [2007]056).
Outcomes
Anthropometric measurements (weight, height, waist and hip circumference) were performed by the staff members using standardized procedures. The body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2). BMI was categorized into non-obesity (BMI <28 kg/m2), and obesity (BMI ≥28 kg/m2). Waist circumference (WC) and waist-to-hip ratio (WHR) were categorized into non-abdominal obesity (WC<90 cm/WHR<0.9 for men; WC<80 cm/WHR<0.8 for women), and abdominal obesity (WC≥90 cm/WHR≥0.9 for men; WC≥80 cm/WHR≥0.8 for women) (10).
Exposure
Air pollution monitoring data were collected from satellite remote sensing (SRS) based on aerosol optical depth data obtained from multi-source satellite products (multi-angle imaging spectroradiometer, moderate resolution imaging spectroradiometer) and a geochemical transport model (11–13). PM2.5 levels were assessed from PM2.5 concentration map products obtained by SRS at a spatial resolution of 1 km.
The meteorologic data such as sunshine duration was derived from surface meteorological observations in China’s meteorological stations obtained from the Surface Meteorological Observation Practice and the Nationwide Surface Climate Data Statistic Method (14–16). Sunshine duration was used to describe the period in a day when the intensity of the direct insolation reaches an average of 120 watts/meters2.
Annual individual PM2.5 exposure values and sunshine duration before the survey date were assigned to participants based on each participant’s residential address at the street level, which was geocoded into latitude and longitude. The five-year mean PM2.5 concentration and sunshine duration prior to the survey date were calculated as the primary exposure variables in our analysis. The details of the calculation of PM2.5 indicator and sunshine duration were presented previously (13, 17, 18).
Assessment of Other Covariates
Information on participants’ sociodemographic features (age, sex, household income, and educational background), life behaviors (current smoking, intakes of alcohol, exercise duration, fruit and vegetable diet, and daily protein intake), urban or rural residence, the annual exposure level of nitrogen dioxide was collected.
Statistical Analysis
Characteristics for people with obesity or abdominal obesity were reported as percentages or mean (standard deviation, SD). A comparison between those with and without obesity and abdominal obesity was conducted using t test or Wilcoxon rank-sum test (continuous variables), and Chi-squared test (categorical variables).
The general additive model (GAM) was applied to examine the obesity risk and abdominal obesity associated with an elevation of 10 μg/m3 in the level of long-term exposure to PM2.5. We included potential confounders that have been previously related to obesity. These covariates included age (continuous), sex (male/female), household income (low-income, middle-income, or high-income), educational background (≥high school versus <high school), rural (yes/no), current smoking (yes/no), and intakes of alcohol (never, five times per week to once per month, or almost once a day), the annual exposure level of nitrogen dioxide (continuous), and sunshine duration (continuous).
The interaction between PM2.5 and sunshine duration for the risk of obesity and abdominal obesity was tested. This was accomplished by including their multiplicative interaction term in the GAM, given the a priori hypothesized relationship between these two factors. Then the stratified analyses were performed if the significant interaction was identified. The relationship between PM2.5 and obesity or abdominal obesity risk across different sunshine duration strata (as quartiles) was assessed.
We performed sensitivity analyses to assess whether the outcomes were robust. We used one-year average PM2.5 instead of five-year PM2.5 and adjusted for varied covariates in the analysis, including exercise duration, fruit and vegetable diet, and daily protein intake as potential confounders. Logistics models were applied to assess the association instead of GAM. We also performed stratified analyses by south/north and longitude (UTC+7, UTC+8) to control the influence of PM2.5 composition on obesity.
The P<0.05 (two-sided) was statistically significant. All analyses were conducted by SAS 9.4.
Results
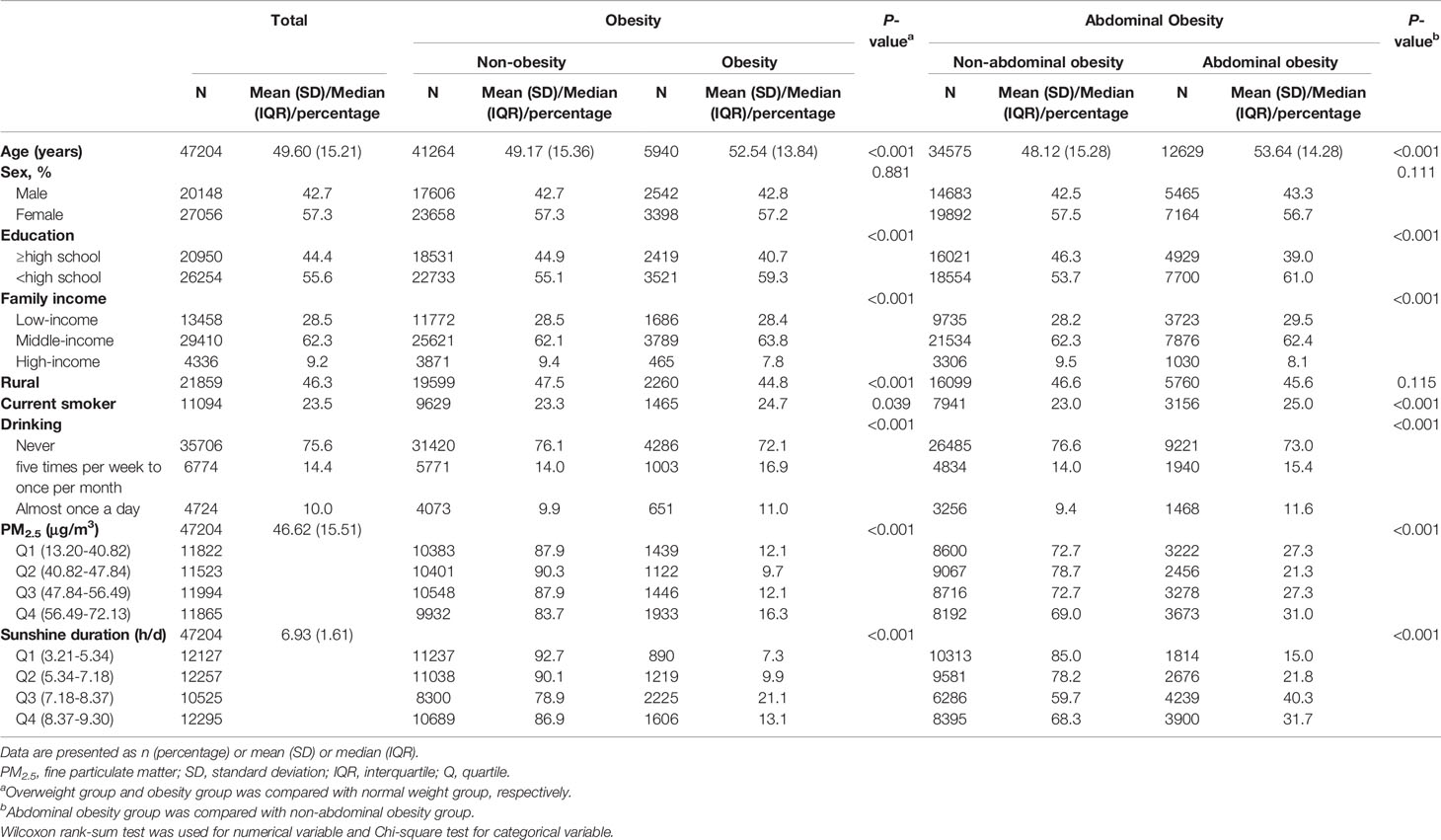
Participants Characteristics are presented in Table 1. Among 47,204 participants, 5,940 (12.6%) and 12,629 (26.8%) were obese and abdominal obese, respectively. Over half of the subjects were women (55.0%), and the mean age was 49.6 ± 15.2 years. Compared with non-obesity participants, those with obesity were more likely to be older, have less education, smoke, drink alcohol frequently.
Estimated PM2.5 levels ranged from 13.20 μg/m3 to 72.13 μg/m3 for five-year exposure, and the overall mean ambient PM2.5 concentration in the study population reached 46.62 μg/m3 (SD of 15.51 μg/m3). The overall mean five-year sunshine duration was 6.93 hours (SD of 1.61 hours) per day. The PM2.5 and sunshine duration levels by each province were diverse (Table S1).
The relationship of PM2.5 exposure with obesity risk and abdominal obesity risk was significant after adjusting for potential confounding factors (Table 2). A five-year average PM2.5 level increase of 10 μg/m3 was positively related to obesity risk [OR 1.12 (95% CI, 1.09-1.14)]. A positively significant association was also observed for abdominal obesity [OR 1.10 (95% CI, 1.07-1.13)].
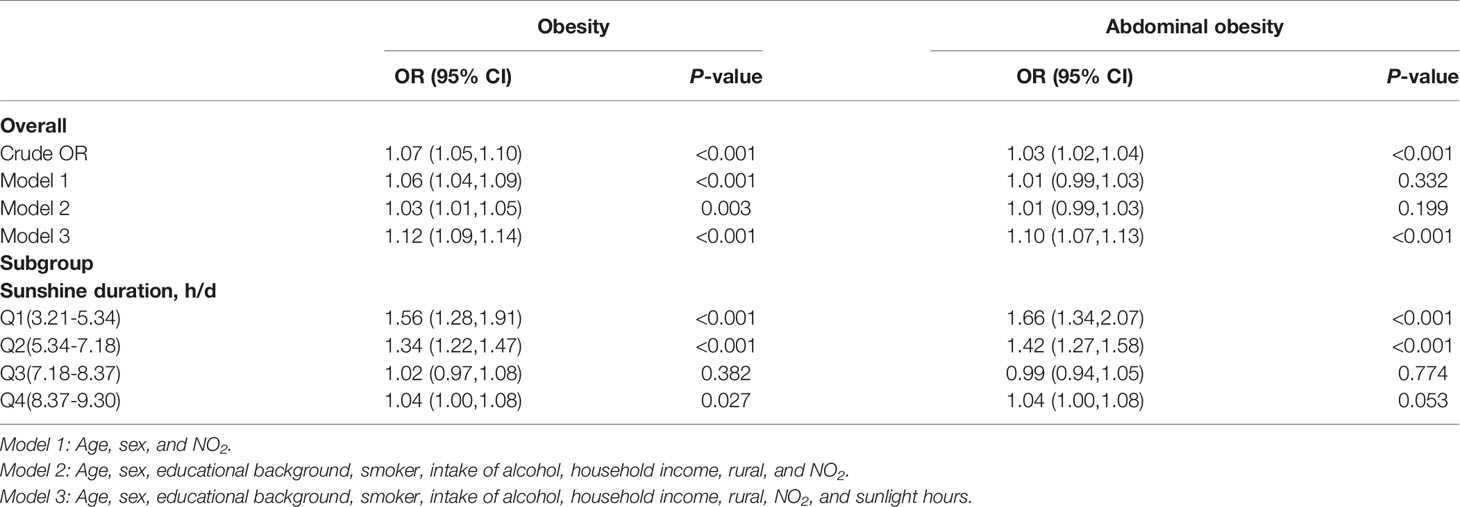
Table 2 Estimated effects of 5-year mean PM2.5 (10μg/m3) on the risk of obesity and abdominal obesity in China.
We observed an inverse J-shaped relationship of PM2.5 level with risk of obesity/abdominal obesity as the sunshine duration increased (Table 2; P value for interaction <0.001), with the lowest risk at 7.18-8.37 h/d. The highest effect estimates of PM2.5 for obesity (OR 1.56; 95%CI, 1.28-1.91) and abdominal obesity (OR 1.66; 95% CI, 1.34-2.07) were observed in the bottom quartile of sunlight exposure (3.21-5.34 h/d).
Sensitivity analyzes also revealed a positively significant relationship of categorized PM2.5 exposure with obesity risk (P value for trend <0.001), and the OR increased gradually across the categories, except for abdominal obesity in the highest exposure group (Supplemental Figure 1). The findings were stable after adding other potential confounders to the multivariable models (Table S2). The association of the one-year mean PM2.5 with the risk of obesity and abdominal obesity showed no substantial change of the risk estimates as to the five-year mean PM2.5 (Table S3). The association assessed by logistics models was also similar to the association assessed by GAMs (Table S4). The subgroup analyses suggested that the obesity risk attributed to PM2.5 attenuated as the sunshine duration increased, especially in south areas (Table S5).
Discussion
We presented the first study to investigate the effect modification of sunlight on the impact of PM2.5 on obesity risk. An inverse J-shaped relationship of PM2.5 with obesity and abdominal obesity risk was observed as the sunshine duration increased, with the lowest risk at the middle sunshine duration group (7.18-8.37 h/d) and the highest risk at the bottom quartile (3.21-5.34 h/d).
Most previous studies revealed a positively significant relationship of PM2.5 level with obesity (6, 19–24). However, several cross-sectional surveys revealed no association between PM2.5 and obesity (25–27), which could be explained by the relatively low level of PM2.5 exposure. For instance, in the Framingham Heart Study (27), the annual mean PM2.5 level reached 10.6 μg/m3, which closely came to the standard from World Health Organization (yearly mean PM2.5: 10μg/m3). Additionally, several studies reporting no association between PM2.5 and obesity mainly focused on subjects living in the area with an abundant sun exposure (25, 26). Our study extended previous observation between PM2.5 and obesity to regions with relatively high level of PM2.5 exposure. Besides, previous evidence revealed that the risk of abdominal obesity was higher with a high PM2.5 concentration in rural areas (19), and short-term exposure has been linked to abdominal obesity (23). Our study further identified a positively significant relationship of long-term effect of PM2.5 with abdominal obesity risk.
We observed that the relationship of PM2.5 with obesity was influenced by the sunshine duration. Previous studies suggested that sunlight exposure might promote the synthesis of vitamin D and nitric oxide, which in turn could lead to a reduced risk of adiposity accumulation (8, 28). In addition, sunlight exposure may stimulate browning recruitment in white adipose tissue via over-expression of cyclooxygenase-2 (COX-2) (29) and facilitated systemic energy expenditure through a myogenic factor 5 (myf-5) independent pathway (30). A cross-sectional study found that the elevated January sunshine duration was associated with an decreased risk of obesity (7). Furthermore, recent studies using latitude (31) and altitude as substitutes for sunlight exposure indicated that decreased latitude (32) or increased altitude (33) (substituting for elevated sunlight exposure) was related to a reduced risk of obesity. However, excess exposure to ultraviolet radiation could overwhelm the cutaneous antioxidant capacity, leading to inflammation and oxidative stress (8, 34). Therefore, sunshine duration exceeding the appropriate range may associate with an elevated risk of obesity, which is consistent with our results.
Experimental studies suggest possible mechanisms for the effect modification of sunlight on the PM2.5 in the pathogenesis of obesity. In vitro and in vivo experiments revealed that both of PM2.5 and sunlight exposure induced the reactive oxygen species (ROS) generation and the expression of COX-2 gene (29, 35, 36), while with various pathways. PM2.5 could induce generation of the highly reactive hydroxyl radical through catalyzing Fenton’s reaction (37, 38), and could activate COX-2 expression through ROS-nuclear factor kappa B (NF-κB) pathway (39). Meanwhile, sunlight exposure could stimulate ROS production by activating the catalase and promoting nitric oxide synthase synthesis (35), and could activate the expression of COX-2 via protein-tyrosine phosphorylation (40). Both excessive ROS production and COX-2 activation led to the progress of systematic inflammation, insulin resistance, and increased oxidative stress (41–43), contributing to an elevated risk of obesity (44, 45).
The study has strengths that deserve mention. The major strength is that the participants were enrolled from multiple centers with relatively high PM2.5 levels and the striking latitude gradient. This study has limitations as well. First, our study population was derived from pre-existing cross-sectional study. Causal inferences on effect of PM2.5 and sunlight on the risk of obesity or abdominal obesity could not be made because this study did not capture the obesity status prior to exposure. Second, we didn’t assess the effects of gaseous pollutants except for NO2. However, NO2 was one of the major predictors of health effects and was highly correlated with other gaseous pollutants (46). Third, our assessment of PM2.5 and sunlight exposure were ascertained based on the nominal levels but not measured levels, which is common in big data surveys. Fourth, we did not collect the information on the workplace, which leads to the effect evaluation of environmental exposure only based on home address. Fifth, we did not take the effect of potential discrepancy in PM2.5 components as a variable into consideration. Furthermore, the possibility of residual confounding could not be excluded.
In conclusion, the present research reveals that the relationship between PM2.5 and obesity or abdominal obesity risk varies by sunshine duration, and stronger relationship were observed in short-sunshine-time regions compared to medium- and long-sunshine-time regions. An improved understanding of this interaction effect may offer important insights for lowering obesity risk attributed to environmental factors.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available. Requests to access these datasets should be directed to zhanglx@bjmu.edu.cn.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committee at Peking University First Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
RC and LZ contributed to the conception and design of the study. RC and CY contributed to the literature review. RC, CY, PL, JW, and LZ contributed to the data collection and data quality control. ZL, WW, YueW, and CL provided the air pollution exposure data. YanW collected the meteorological data. RC, CY, JW, and LZ cleaned, analysed, and visualized the data. RC, CY, JW, and LZ supervised the analysis and generation of results, and directly accessed and verified the data. RC wrote the manuscript. LZ and CY reviewed and edited the manuscript. All authors contributed to data interpretation, and reviewed and approved the final version manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding
This study was supported by grants from the National Natural Science Foundation of China (91846101, 82003529, 81771938, 81900665, 82090021), Beijing Nova Programme Interdisciplinary Cooperation Project (Z191100001119008), National Key R&D Program of the Ministry of Science and Technology of China (2019YFC2005000), Chinese Scientific and Technical Innovation Project 2030 (2018AAA0102100), the University of Michigan Health System-Peking University Health Science Center Joint Institute for Translational and Clinical Research (BMU2018JI012, BMU2019JI005, 71017Y2027), CAMS Innovation Fund for Medical Sciences (2019-I2M-5-046), and PKU-Baidu Fund (2019BD017, 2020BD032).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.790294/full#supplementary-material
Abbreviations
PM2.5, fine particulate matter; WC, waist circumference; WHR, waist-to-hip ratio; OR, odds ratio; CI, confidence interval; BMI, body mass index; SRS, satellite remote sensing; NO2, nitrogen dioxide; GAM, general additive model; COX-2, cyclooxygenase-2; myf-5, myogenic factor 5; ROS, reactive oxygen species; NF-κB, nuclear factor kappa B.
References
1. World Health Organization. Obesity and Overweight (2020). Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed September 23, 2021).
2. Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, et al. Secular Trends in the Prevalence of General and Abdominal Obesity Among Chinese Adults, 1993-2009. Obes Rev (2012) 13(3):287–96. doi: 10.1111/j.1467-789X.2011.00944.x
3. Bluher M. Obesity: Global Epidemiology and Pathogenesis. Nat Rev Endocrinol (2019) 15(5):288–98. doi: 10.1038/s41574-019-0176-8
4. Chinese National Health and Family Planning Commission. Report on the Nutrition and Chronic Disease Status of Chinese Residents. Beijing: People’s Medical Publishing House (2020).
5. An R, Ji M, Yan H, Guan C. Impact of Ambient Air Pollution on Obesity: A Systematic Review. Int J Obes (Lond) (2018) 42(6):1112–26. doi: 10.1038/s41366-018-0089-y
6. de Bont J, Casas M, Barrera-Gomez J, Cirach M, Rivas I, Valvi D, et al. Ambient Air Pollution and Overweight and Obesity in School-Aged Children in Barcelona, Spain. Environ Int (2019) 125:58–64. doi: 10.1016/j.envint.2019.01.048
7. von Hippel P, Benson R. Obesity and the Natural Environment Across US Counties. Am J Public Health (2014) 104(7):1287–93. doi: 10.2105/AJPH.2013.301838
8. Barrea L, Savastano S, Di Somma C, Savanelli MC, Nappi F, Albanese L, et al. Low Serum Vitamin D-Status, Air Pollution and Obesity: A Dangerous Liaison. Rev Endocr Metab Disord (2017) 18(2):207–14. doi: 10.1007/s11154-016-9388-6
9. Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of Chronic Kidney Disease in China: A Cross-Sectional Survey. Lancet (2012) 379(9818):815–22. doi: 10.1016/S0140-6736(12)60033-6
10. Du P, Wang HJ, Zhang B, Qi SF, Mi YJ, Liu DW, et al. Prevalence of Abdominal Obesity Among Chinese Adults in 2011. J Epidemiol (2017) 27(6):282–6. doi: 10.1016/j.je.2017.03.001
11. Lee HJ, Liu Y, Coull BA, Schwartz J, Koutrakis P. A Novel Calibration Approach of MODIS AOD Data to Predict PM2.5 Concentrations. Atmos Chem Phys (2011) 11(15):7991–8002. doi: 10.5194/acp-11-7991-2011
12. Guo J, Xia F, Zhang Y, Liu H, Li J, Lou M, et al. Impact of Diurnal Variability and Meteorological Factors on the PM2.5 - AOD Relationship: Implications for PM2.5 Remote Sensing. Environ Pollut (2017) 221:94–104. doi: 10.1016/j.envpol.2016.11.043
13. Lv B, Hu Y, Chang HH, Russell AG, Cai J, Xu B, et al. Daily Estimation of Ground-Level PM2.5 Concentrations at 4km Resolution Over Beijing-Tianjin-Hebei by Fusing MODIS AOD and Ground Observations. Sci Total Environ (2017) 580:235–44. doi: 10.1016/j.scitotenv.2016.12.049
14. Wang G, Wu Z, Xu F, Zang H, Deng L, Sun C, et al. CMA (China Meteorological Administration). Core Metadata Content of Meteorological Dataset (QX/T 39-2005). Beijing, China (in Chinese: China Meteorological Press (2005).
15. CMA (China Meteorological Administration). Standard of the Surface Observation About Meteorology. Beijing, China (in Chinese: China Meteorological Press (1954).
16. Chen T, Zhang N, Jin J, Li S, Guan Y, Shen X, et al. CMA (China Meteorological Administration). Standard of the Surface Observation About Meteorology. Beijing, China (in Chinese: China Meteorological Press (2003).
17. Liang Z, Wei F, Wang Y, Huang J, Jiang H, Sun F, et al. The Context-Dependent Effect of Urban Form on Air Pollution: A Panel Data Analysis. Remote Sens (2020) 12(11):1793. doi: 10.3390/rs12111793
18. Han R, Wang S, Shen W, Wang J, Wu K, Ren Z, et al. Spatial and Temporal Variation of Haze in China From 1961 to 2012. J Environ Sci (China) (2016) 46:134–46. doi: 10.1016/j.jes.2015.12.033
19. Liu X, Tu R, Qiao D, Niu M, Li R, Mao Z, et al. Association Between Long-Term Exposure to Ambient Air Pollution and Obesity in a Chinese Rural Population: The Henan Rural Cohort Study. Environ Pollut (2020) 260:114077. doi: 10.1016/j.envpol.2020.114077
20. Yang Z, Song Q, Li J, Zhang Y. Air Pollution as a Cause of Obesity: Micro-Level Evidence From Chinese Cities. Int J Environ Res Public Health (2019) 16(21):4296. doi: 10.3390/ijerph16214296
21. Zhang N, Wang L, Zhang M, Nazroo J. Air Quality and Obesity at Older Ages in China: The Role of Duration, Severity and Pollutants. PloS One (2019) 14(12):e0226279. doi: 10.1371/journal.pone.0226279
22. Guo Q, Xue T, Jia C, Wang B, Cao S, Zhao X, et al. Association Between Exposure to Fine Particulate Matter and Obesity in Children: A National Representative Cross-Sectional Study in China. Environ Int (2020) 143:105950. doi: 10.1016/j.envint.2020.105950
23. Furlong MA, Klimentidis YC. Associations of Air Pollution With Obesity and Body Fat Percentage, and Modification by Polygenic Risk Score for BMI in the UK Biobank. Environ Res (2020) 185:109364. doi: 10.1016/j.envres.2020.109364
24. Deschenes O, Wang H, Wang S, Zhang P. The Effect of Air Pollution on Body Weight and Obesity: Evidence From China. J Dev Econ (2020) 145:102461. doi: 10.1016/j.jdeveco.2020.102461
25. Kim JS, Chen Z, Alderete TL, Toledo-Corral C, Lurmann F, Berhane K, et al. Associations of Air Pollution, Obesity and Cardiometabolic Health in Young Adults: The Meta-AIR Study. Environ Int (2019) 133(Pt A):105180. doi: 10.1016/j.envint.2019.105180
26. Fioravanti S, Cesaroni G, Badaloni C, Michelozzi P, Forastiere F, Porta D. Traffic-Related Air Pollution and Childhood Obesity in an Italian Birth Cohort. Environ Res (2018) 160:479–86. doi: 10.1016/j.envres.2017.10.003
27. Li W, Dorans KS, Wilker EH, Rice MB, Schwartz J, Coull BA, et al. Residential Proximity to Major Roadways, Fine Particulate Matter, and Adiposity: The Framingham Heart Study. Obes (Silver Spring) (2016) 24(12):2593–9. doi: 10.1002/oby.21630
28. Dhamrait GK, Panchal K, Fleury NJ, Abel TN, Ancliffe MK, Crew RC, et al. Characterising Nitric Oxide-Mediated Metabolic Benefits of Low-Dose Ultraviolet Radiation in the Mouse: A Focus on Brown Adipose Tissue. Diabetologia (2020) 63(1):179–93. doi: 10.1007/s00125-019-05022-5
29. Vegiopoulos A, Muller-Decker K, Strzoda D, Schmitt I, Chichelnitskiy E, Ostertag A, et al. Cyclooxygenase-2 Controls Energy Homeostasis in Mice by De Novo Recruitment of Brown Adipocytes. Science (2010) 328(5982):1158–61. doi: 10.1126/science.1186034
30. Madsen L, Pedersen LM, Lillefosse HH, Fjaere E, Bronstad I, Hao Q, et al. UCP1 Induction During Recruitment of Brown Adipocytes in White Adipose Tissue Is Dependent on Cyclooxygenase Activity. PloS One (2010) 5(6):e11391. doi: 10.1371/journal.pone.0011391
31. Jelinek GA, Marck CH, Weiland TJ, Pereira N, van der Meer DM, Hadgkiss EJ. Latitude, Sun Exposure and Vitamin D Supplementation: Associations With Quality of Life and Disease Outcomes in a Large International Cohort of People With Multiple Sclerosis. BMC Neurol (2015) 15:132. doi: 10.1186/s12883-015-0394-1
32. Muldowney S, Lucey AJ, Paschos G, Martinez JA, Bandarra N, Thorsdottir I, et al. Relationships Between Vitamin D Status and Cardio-Metabolic Risk Factors in Young European Adults. Ann Nutr Metab (2011) 58(2):85–93. doi: 10.1159/000324600
33. Woolcott OO, Castillo OA, Gutierrez C, Elashoff RM, Stefanovski D, Bergman RN. Inverse Association Between Diabetes and Altitude: A Cross-Sectional Study in the Adult Population of the United States. Obesity (2014) 22(9):2080–90. doi: 10.1002/oby.20800
34. Nichols JA, Katiyar SK. Skin Photoprotection by Natural Polyphenols: Anti-Inflammatory, Antioxidant and DNA Repair Mechanisms. Arch Dermatol Res (2010) 302(2):71–83. doi: 10.1007/s00403-009-1001-3
35. de Jager TL, Cockrell AE, Du Plessis SS. Ultraviolet Light Induced Generation of Reactive Oxygen Species. Adv Exp Med Biol (2017) 996:15–23. doi: 10.1007/978-3-319-56017-5_2
36. Lakey PSJ, Berkemeier T, Tong HJ, Arangio AM, Lucas K, Poschl U, et al. Chemical Exposure-Response Relationship Between Air Pollutants and Reactive Oxygen Species in the Human Respiratory Tract. Sci Rep-Uk (2016) 6:32916. doi: 10.1038/srep32916
37. Andersson H, Piras E, Demma J, Hellman B, Brittebo E. Low Levels of the Air Pollutant 1-Nitropyrene Induce DNA Damage, Increased Levels of Reactive Oxygen Species and Endoplasmic Reticulum Stress in Human Endothelial Cells. Toxicology (2009) 262(1):57–64. doi: 10.1016/j.tox.2009.05.008
38. Park JH, Troxel AB, Harvey RG, Penning TM. Polycyclic Aromatic Hydrocarbon (PAH) O-Quinones Produced by the Aldo-Keto-Reductases (Akrs) Generate Abasic Sites, Oxidized Pyrimidines, and 8-Oxo-Dguo via Reactive Oxygen Species. Chem Res Toxicol (2006) 19(5):719–28. doi: 10.1021/tx0600245
39. Li B, Guo L, Ku T, Chen M, Li G, Sang N. PM2.5 Exposure Stimulates COX-2-Mediated Excitatory Synaptic Transmission via ROS-NF-KappaB Pathway. Chemosphere (2018) 190:124–34. doi: 10.1016/j.chemosphere.2017.09.098
40. Isoherranen K, Punnonen K, Jansen C, Uotila P. Ultraviolet Irradiation Induces Cyclooxygenase-2 Expression in Keratinocytes. Br J Dermatol (1999) 140(6):1017–22. doi: 10.1046/j.1365-2133.1999.02897.x
41. Hsieh PS, Jin JS, Chiang CF, Chan PC, Chen CH, Shih KC. COX-2-Mediated Inflammation in Fat Is Crucial for Obesity-Linked Insulin Resistance and Fatty Liver. Obesity (2009) 17(6):1150–7. doi: 10.1038/oby.2008.674
42. Hu X, Cifarelli V, Sun S, Kuda O, Abumrad NA, Su X. Major Role of Adipocyte Prostaglandin E2 in Lipolysis-Induced Macrophage Recruitment. J Lipid Res (2016) 57(4):663–73. doi: 10.1194/jlr.M066530
43. Tian YF, Hsia TL, Hsieh CH, Huang DW, Chen CH, Hsieh PS. The Importance of Cyclooxygenase 2-Mediated Oxidative Stress in Obesity-Induced Muscular Insulin Resistance in High-Fat-Fed Rats. Life Sci (2011) 89(3-4):107–14. doi: 10.1016/j.lfs.2011.05.006
44. Leloup C, Tourrel-Cuzin C, Magnan C, Karaca M, Castel J, Carneiro L, et al. Mitochondrial Reactive Oxygen Species Are Obligatory Signals for Glucose-Induced Insulin Secretion. Diabetes (2009) 58(3):673–81. doi: 10.2337/db07-1056
45. Loh K, Deng H, Fukushima A, Cai X, Boivin B, Galic S, et al. Reactive Oxygen Species Enhance Insulin Sensitivity. Cell Metab (2009) 10(4):260–72. doi: 10.1016/j.cmet.2009.08.009
Keywords: obesity, abdominal obesity, PM2.5 concentration, sunlight, air pollution
Citation: Chen R, Yang C, Li P, Wang J, Liang Z, Wang W, Wang Y, Liang C, Meng R, Wang H-y, Peng S, Sun X, Su Z, Kong G, Wang Y and Zhang L (2022) Long-Term Exposure to Ambient PM2.5, Sunlight, and Obesity: A Nationwide Study in China. Front. Endocrinol. 12:790294. doi: 10.3389/fendo.2021.790294
Received: 06 October 2021; Accepted: 30 November 2021;
Published: 07 January 2022.
Edited by:
Andrea P. Rossi, Ca’ Foncello Hospital, ItalyReviewed by:
Guozhu Ye, Institute of Urban Environment (CAS), ChinaYan-Bo Zhang, Huazhong University of Science and Technology, China
Copyright © 2022 Chen, Yang, Li, Wang, Liang, Wang, Wang, Liang, Meng, Wang, Peng, Sun, Su, Kong, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luxia Zhang, emhhbmdseEBiam11LmVkdS5jbg==
 Rui Chen
Rui Chen Chao Yang
Chao Yang Pengfei Li3
Pengfei Li3 Jinwei Wang
Jinwei Wang Wanzhou Wang
Wanzhou Wang Ruogu Meng
Ruogu Meng Huai-yu Wang
Huai-yu Wang Guilan Kong
Guilan Kong Luxia Zhang
Luxia Zhang