- 1Department of Thyroid Surgery, The 1st Hospital of Jilin University, Changchun, China
- 2Department of Nephrology, The 1st Hospital of Jilin University, Changchun, China
Objective: Postoperative neck symptoms, including pain, swelling, uncomfortable feelings during swallowing, and incision adhesion formation, are common in patients after lobectomy through the traditional middle neck approach. A new unilateral supraclavicular approach is proposed to protect the anterior cervical region and reduce related complications. The aim of this study is to investigate the efficacy, safety, and advantages of the supraclavicular approach in lobectomy for unilateral papillary thyroid microcarcinoma (PTMC).
Methods: Two hundred sixty-three patients were recruited into either a conventional middle group (CM) or a new supraclavicular (NS) group. Clinicopathological features, surgically related variables, and postoperative symptoms were recorded. Quality of life (QOL) of all patients was assessed by the 12-item short-form health survey (SF-12) and thyroid cancer-specific QOL (THYCA-QoL) questionnaire in 3 and 12 months.
Results: There were no statistically significant differences in clinicopathological features (including sex, age, multifocality, extrathyroidal extension, histological variants, largest tumor diameter, Hashimoto’s thyroiditis, metastasized central lymph node, removed central lymph node, surgeon, BRAF mutation, and follow-up duration), hospitalization (including hospital cost, surgery time, and blood loss during surgery), and complications between the two groups. Patients who underwent lobectomy through the NS approach had significantly better SF-12 physical, mental, and THYCA-QoL than the CM group patients in both 3 and 12 months (all p < 0.001). Moreover, the NS group had a shorter hospitalization time.
Conclusion: In conclusion, the NS approach for lobectomy is a safe and effective method for reducing postoperative symptoms and increasing QOL in patients with unilateral PTMC in both 3 and 12 months’ follow-up.
Introduction
The incidence rate of thyroid cancer is increasing worldwide (1, 2). The rapid growth of papillary thyroid microcarcinoma (PTMC), which is defined as papillary thyroid carcinoma measuring ≤1 cm in the greatest dimension, is the main reason (3). The majority of PTMC patients have no clinical symptoms upon routine ultrasound (US) examination. In recent years, the development and popularization of high-frequency US and fine-needle aspiration (FNA) have further increased the diagnosis of PTMC (4). Most PTMC cases are low-risk. The recurrence rate is 1%–5%, and the 10-year mortality rate is as low as 0.3% (5). Therefore, active surveillance (AS) is recommended as an alternative treatment choice for low-risk PTMC cases (6). However, AS is not universally accepted because of the disparity in doctors’ knowledge and the concern of disease progression in the patient’s mind (7–9). Surgery is still the mainstay for the treatment of PTMC in many countries.
The good prognosis of PTMC led patients to pay more attention to postoperative quality of life (QOL), including postoperative functional recovery and cosmetic results (10). However, more than 50% of patients complain about a stretching, choking, or pressing feeling or discomfort or scarring in the middle neck postoperatively (11, 12). Some of them suffered these symptoms in the long term, which had a negative impact on QOL (13, 14). These neck discomforts might be caused by injury of the neck sensory nerve, adhesion of the larynx and strap muscles/subcutaneous tissues, and large tension of the middle neck, which is inevitable through the conventional middle (CM) neck approach (15, 16). Some studies have demonstrated better cosmetic results through the new supraclavicular (NS) approach (17, 18). But whether lobectomy through the NS approach could reduce neck discomforts and improve postoperative QOL is still unknown.
The aim of this study was to evaluate the potential benefits and risks of lobectomy through the NS approach. In this study, we will demonstrate several clinical concerns: 1) whether the NS approach reduces neck discomforts and improves neck postoperative QOL; and 2) whether the NS approach reduces postoperative complications. This study can demonstrate whether lobectomy through the NS approach is an effective and safe surgical method for unilateral PTMC.
Methods
Patient Selection
The Human Research Ethics Committee of the First Hospital of Jilin University approved this study (No. 2019-353). From November 2019 to July 2020, all unilateral PTMC patients who underwent lobectomy with unilateral central lymph node dissection (CLND) at the First Hospital of Jilin University were recommended for both CM and NS approaches at the same time. The surgeon will elaborate on both benefits and risks of these two surgical approaches, and patients can make a decision according to their preference. The exclusion criteria were as follows: patients’ age <18 years (1 case); those with surrounding neck structure invasion according to US and/or CT scan (6 cases); those with clinical lymph node metastasis (3 cases); those with persistent disease (0 cases); those with a history of neck radiotherapy (0 cases); and those with a history of previous thyroid surgery (3 cases). Finally, 263 unilateral PTMC patients were enrolled in our study.
Diagnosis and Treatment
The majority of PTMC patients were detected by US examination and diagnosed by FNA and BRAF mutation detection. If the largest diameter of thyroid nodule was larger than 0.5 cm and presented with one or more US malignant features, FNA for suspicious thyroid nodule was recommended for patients according to the Chinese guidelines of PTMC (19). For those with suspicious nodules with a diameter <0.5 cm, AS was recommended, unless patients persisted on surgery because of concern about malignancy. CT scans were only performed for PTMC patients with potential surrounding tissue invasion. Lobectomy through CM approach was performed as follows: along the natural skin crease about two fingers above the sternal notch, a circular incision measuring 4 to 5 cm was performed. A subplatysmal flap was produced until the deep cervical fascia was exposed. After the strap muscle was divided and retracted in the center, the thyroid was exposed, and lobectomy was performed. The NS approach was performed: the incision was designed between the anterior and posterior sternocleidomastoid and two fingers above the clavicle. The space between the sternal and clavicular heads was separated, and the omohyoid muscle was identified. The omohyoid muscle was freed, then the space between the strap muscle and thyroid was separated. Lobectomy was performed on the CM group (Supplementary 1 Video; website: https://pan.baidu.com/s/1j7AHTLy_ws6-SlycRwX4nw; password: eo0t).
CLND was performed as previously described (20).
Histopathological and Hospitalization Information
Histopathological characteristics, including multifocality, extrathyroidal extension (ETE), histological variants, largest tumor diameter (LTD), Hashimoto’s thyroiditis (HT), metastasized central lymph node (MCLN), removed central lymph node (RCLN), and BRAF mutation, were recorded. Hospitalization information and surgical complications like hospital stay, cost, surgical time, blood loss during surgery, hemorrhage, recurrent laryngeal nerve (RLN) injury, and parathyroid removal were also extracted from the patient’s database in the hospital. RLN injury was defined as loss of signal during neural monitoring and vocal cord paralysis during postoperative laparoscopy.
Follow-Up and Quality of Life Evaluation
All patients were followed up with physical examinations, thyroid function, US, and QOL assessment at 3-month intervals. To assess QOL in 3 and 12 months, all enrolled PTMC patients completed two questionnaires: the 12-item short-form health survey (SF-12) and thyroid cancer-specific QOL (THYCA-QoL) questionnaire. The SF-12, which consists of 12 questions, is a well-validated short-form of SF-36. Physical and Mental Component Summary scores were calculated after answers were combined and weighted (Supplementary 2 SF-12). Higher scores indicated a better health status. The THYCA-QoL contains 24 items that evaluate symptoms from thyroid cancer or its treatment, especially surgery. Each item was scored on a 4-point response scale ranging from 1, “not at all”, to 4, “very much”. Each score was converted into scores on seven multisymptom scales (neuromuscular, voice, concentration, sympathetic, throat/mouth, psychological, and sensory problems) and six single-symptom scales (problems with scarring, felt chilly, tingling hands/feet, gained weight, headache, and less interested in sex) (Supplementary 3 THYCA-QOL). Scores were linear-transformed to a 0–100 scale, and a higher score on this scale indicates more complaints.
Statistical Analysis
Continuous variables are presented as the means and standard deviations, while nominal variables are described as frequencies and proportions. The Mann–Whitney U test for continuous variables and Pearson’s chi-square tests were used for nominal variables, and p < 0.05 was considered statistically significant (2-sided). SPSS version 23 software (SPSS Inc., Chicago, IL) was used for all statistical analyses.
Results
Comparison of Baseline Characteristics
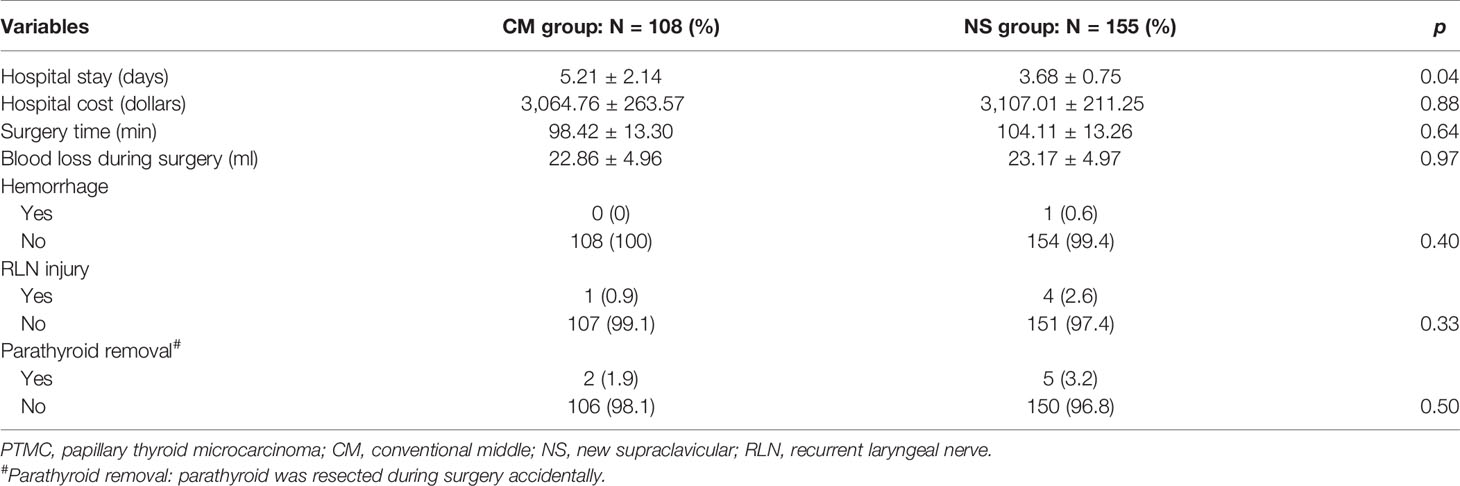
As shown in Table 1, baseline clinicopathological features, including sex, age, multifocality, ETE, histological variants, LTD, HT, MCLN, RCLN, surgeon, BRAF mutation, and follow-up duration, were compared between the CM and NS groups. These baseline characteristics, which may affect QOL, hospitalization, and surgical complications, were not different significantly between these two groups.
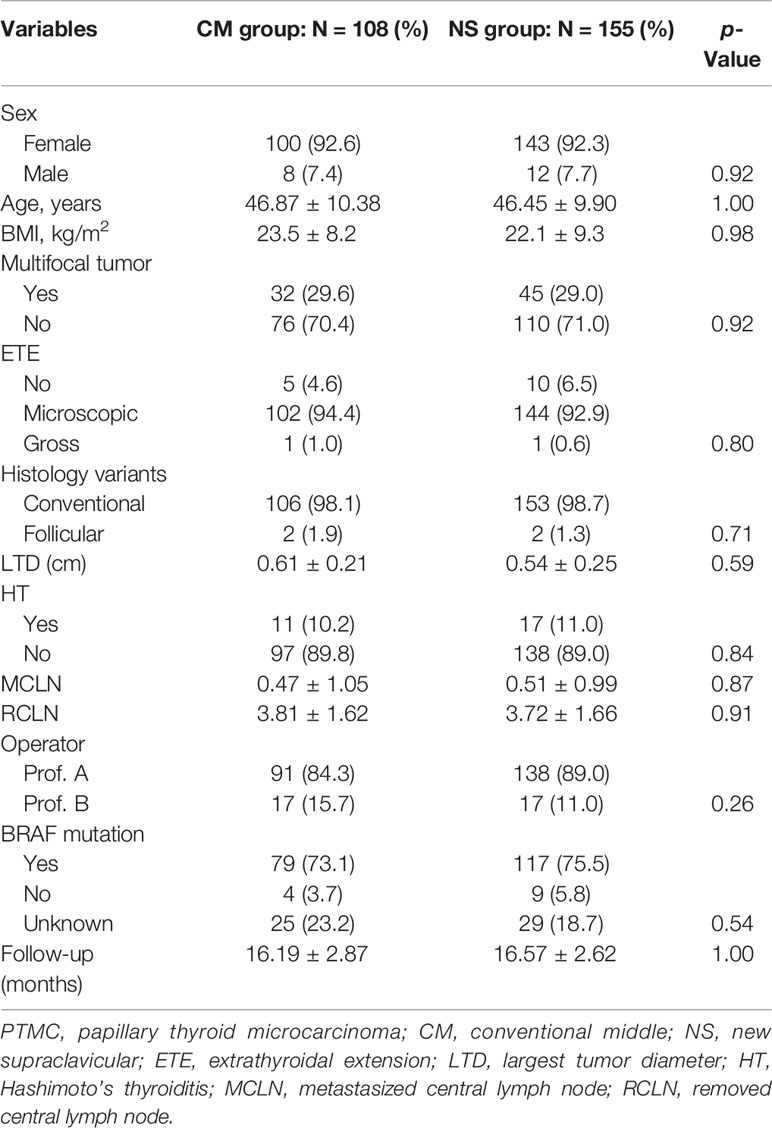
Table 1 Baseline clinicopathological feature comparison of PTMC patients between the CM and NS groups.
Comparison of Overall Quality of Life, Hospitalization, and Complications
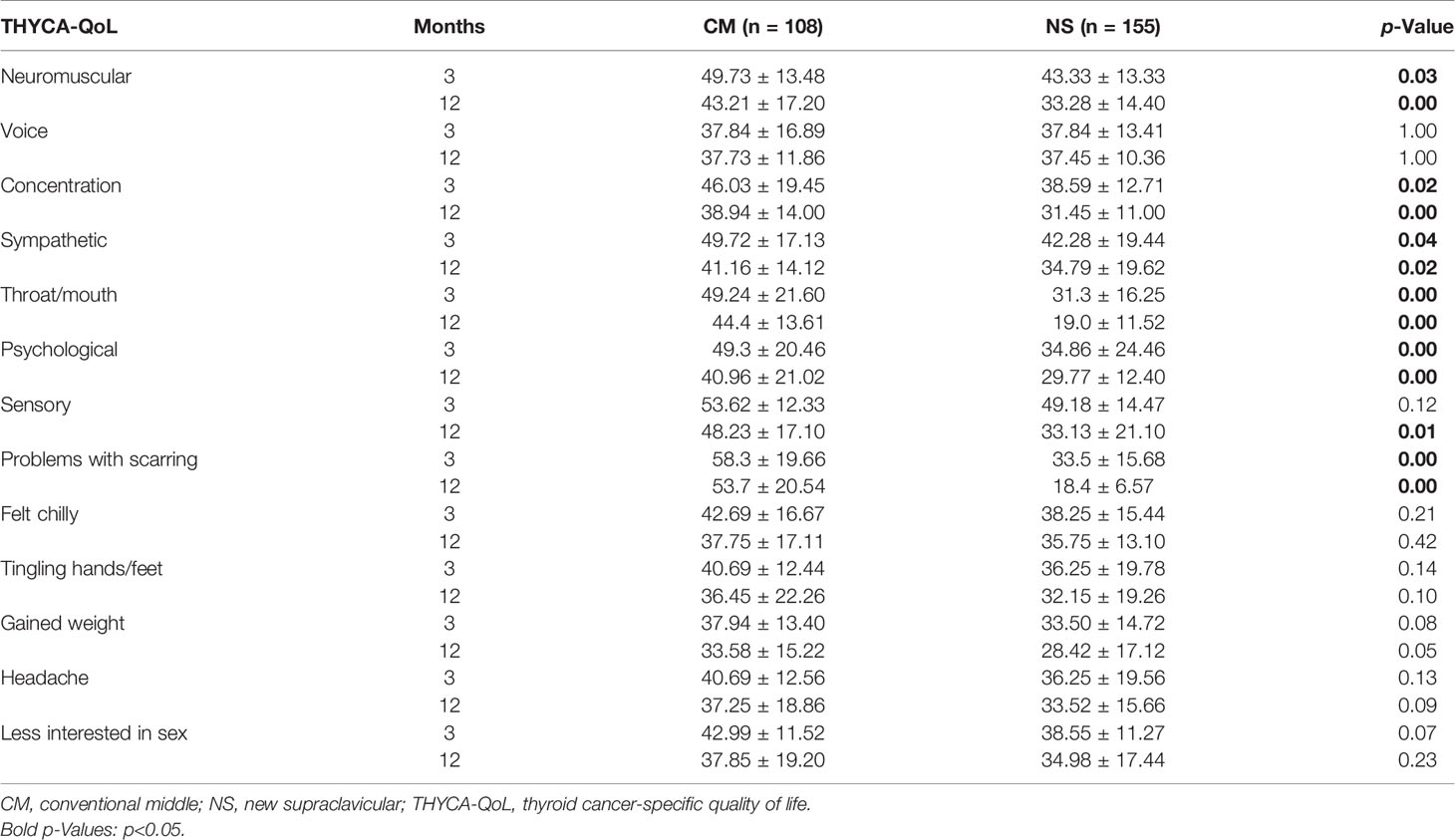
The comparison of general and thyroid cancer-specific QOL between CM and NS groups was performed and shown in Figure 1. Patients who underwent lobectomy through the NS approach had significantly better SF-12 physical, mental, and THYCA-QoL scores than the CM group patients in both 3 and 12 months (all p < 0.001). Moreover, hospitalization and surgical complications like hospital stay, cost, surgical time, blood loss during surgery, hemorrhage, RLN injury, and parathyroid removal were compared between these two groups. Hospital stay was significantly longer in the CM group (p = 0.04). Surgical complications related to the NS approach were low among both groups, and none of the complications were remarkably different between the groups, as shown in Table 2.
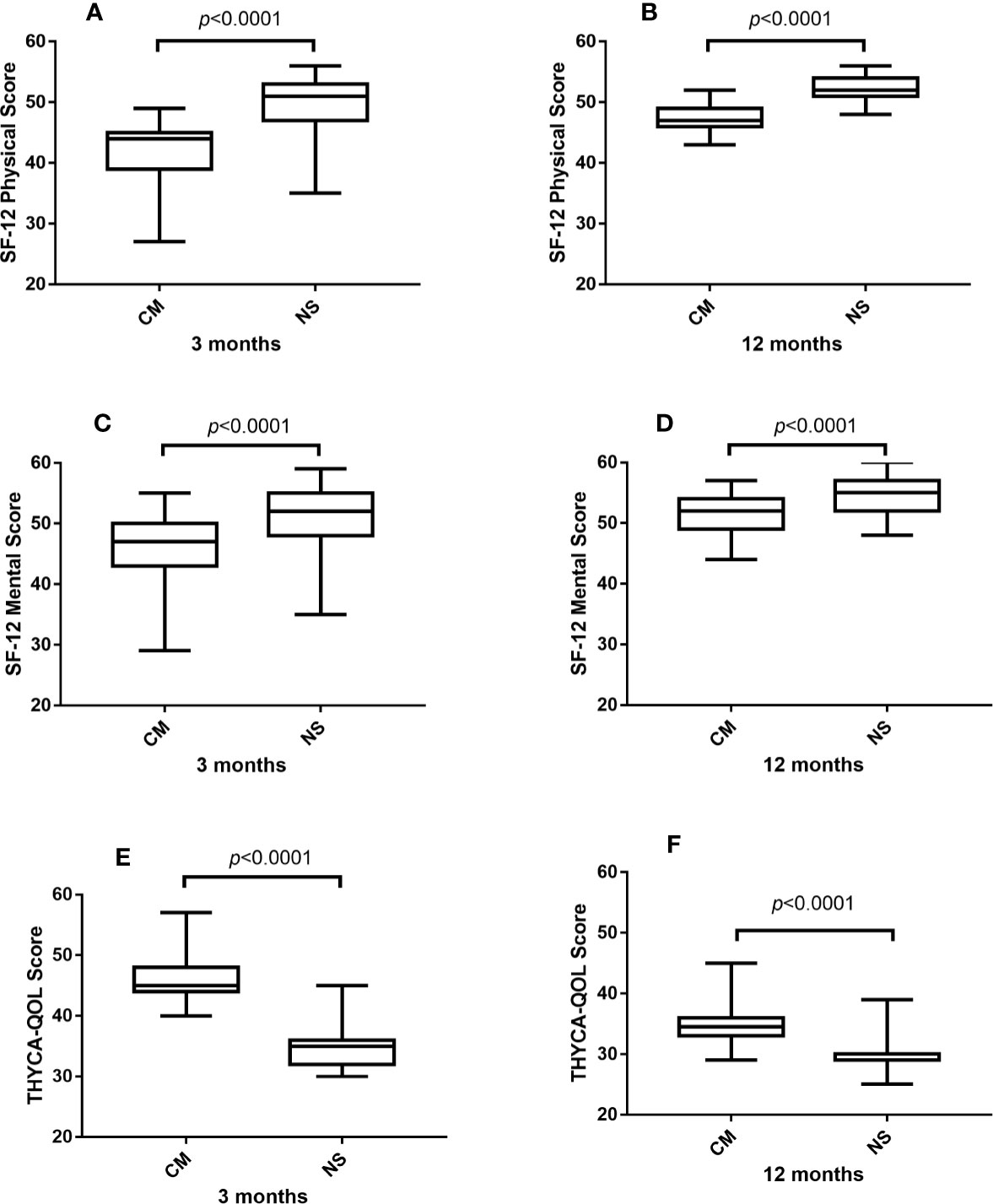
Figure 1 Comparison of SF-12 physical (A, B), mental score (C, D), and THYCA-QoL score (E, F) between CM and NS group in 3 and 12 months. SF-12, 12-item short-form health survey; THYCA-QoL, thyroid cancer-specific quality of life.
Comparison of Postoperative Symptoms According to Thyroid Cancer-Specific Quality of Life
Postoperative symptoms, including neuromuscular, voice, concentration, sympathetic, throat/mouth, psychological, and sensory problems, problems with scarring, felt chilly, tingling hands/feet, gained weight, headache, and less interested in sex, were evaluated and recorded during follow-up (exclusion of possible concomitant pathologies like gastroesophageal reflux). As shown in Table 3, more patients of the CM group suffered severe postoperative negative symptoms such as neuromuscular, concentration, sympathetic, throat/mouth, psychological, and problems with scarring in both 3 and 12 months (all p < 0.05). On the other hand, patients of the NS group presented with fewer sensory problems only in 12 months (p < 0.05).
Discussion
Still, until now, the potential benefits and risks of lobectomy through the NS approach for unilateral PTMC patients remain unknown. Our study demonstrated that patients who underwent lobectomy by the NS approach showed better physical, mental, and thyroid-cancer specific QOL than patients who underwent the CM approach after adjustment for all potential confounders for QOL. Moreover, patients in the NS group spent less time in the hospital, and they did not suffer significantly from more surgical complications. Furthermore, more patients of the CM group suffered severe postoperative negative symptoms such as neuromuscular, concentration, sympathetic, throat/mouth, and psychological problems with scarring in both 3 and 12 months.
The anterior neck area refers to the triangular area between the inner edges of the sternocleidomastoid muscles on both sides. The lower boundary is the sternal notch, while the upper boundary is the lower edge of the mandible. Moreover, the hyoid bone has divided this area into the upper and lower parts. And the lower part of the anterior neck area, which is also known as the anterior functional area of the neck, is the most vulnerable area affected by thyroid surgery (21–23).
The anterior area of the neck shares three main functions (24–27). 1) Sensory function: Lobectomy through the CM approach will injure the end branches of the transverse cervical nerve inevitably, which leads to skin numbness, pressing, or stitching feeling during wound healing. The NS approach will divide the space between the sternal and clavicular heads of the sternocleidomastoid muscle, which will not injure the transverse cervical nerve. 2) Movement function: Middle neck discomfort symptoms including difficulty in swallowing and pulling sensations during neck extension might be caused by adhesion of the larynx and strap muscles or subcutaneous tissues. Dysphagia was always reported after thyroid surgery through the CM approach because the adhesion restricts the upward movement of the larynx during swallowing. The NS approach will not divide the subplatysmal flap and strap muscle. And the adhesion between the larynx and other neck structures will not happen. 3) Cosmetic function: the tension of the middle neck is larger than that of the lateral neck. An incisional scar is more likely to form because of higher tension in the skin. The incision of the NS approach is located in the lateral neck and is more likely to get better cosmetic results. According to our study, the NS approach shared fewer postoperative neck negative symptoms (including neck discomforts, difficulty in swallowing, throat lump, and concerns about neck scarring) in both 3 and 12 months. The gasless transaxillary laparoscopic thyroid surgery also resects the thyroid between the sternal and clavicular heads of the sternocleidomastoid muscle. In agreement with our study, patients who underwent transaxillary laparoscopic thyroid surgery also presented with better postoperative neck symptoms (28–30).
However, lobectomy by the NS approach has some limitations: 1) removal of the contralateral gland, although feasible, is much more difficult through the NS approach. Excessive traction of the incision or separation of the strap muscle will increase the formation of postoperative incision scars. 2) Before surgery, evaluation of the location of the tumor and the lymph node metastasis in the central department is needed. If the tumor is more likely to invade the RLN, trachea, or esophagus, or the central lymph node metastasis is serious, it will be difficult to remove the contralateral gland. 3) If the tumor recurs in the contralateral gland, it is difficult to remove the contralateral gland again from the original incision.
Furthermore, several limitations in the study must be noted. First, the relatively small number of patients may generate some bias in our study. Also, the small number of patients limits the probability of propensity score matching to eliminate potential cofounders when the QOL between the CM group and NS group is compared. Some unknown and unmeasured confounders may influence the strength of the result, although many factors have been considered for baseline comparison, as shown in Table 1. Secondly, these clinical care strategies, like hospitalization time and cost for PTMC patients, were different from those in other countries. The potential discrepancy may limit the generalizability of these findings to other hospitals. Finally, different surgeons may have differences in incision protection, subcutaneous dissociation, and suture techniques. Ideally, it is best to compare patients of the same surgeon.
Conclusion
In conclusion, lobectomy by the NS approach is a safe and effective method for reducing postoperative neck discomforts and increasing QOL in patients with unilateral PTMC in both 3 and 12 months’ follow-up.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of the First Hospital of Jilin University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.766444/full#supplementary-material
References
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin (2017) 67:7–30. doi: 10.3322/caac.21387
2. Kitahara CM, Sosa JA. The Changing Incidence of Thyroid Cancer. Nat Rev Endocrinol (2016) 12:646–53. doi: 10.1038/nrendo.2016.110
3. Soares P, Celestino R, Gaspar da Rocha A, Sobrinho-Simões M. Papillary Thyroid Microcarcinoma:How to Diagnose and Manage This Epidemic? Int J Surg Pathol (2014) 22:113–9. doi: 10.1177/1066896913517394
4. Xu S, Han Y. The Overdiagnosis of Thyroid Micropapillary Carcinoma: The Rising Incidence, Inert Biological Behavior, and Countermeasures. J Oncol (2021) 2021:5544232. doi: 10.1155/2021/5544232
5. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. JAMA (2017) 317:1338–48. doi: 10.1001/jama.2017.2719
6. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid (2016) 26:1–133. doi: 10.1089/thy.2015.0020
7. Nickel B, Brito JP, Barratt A, Jordan S, Moynihan R, McCaffery K. Clinicians' Views on Management and Terminology for Papillary Thyroid Microcarcinoma: A Qualitative Study. Thyroid (2017) 27:661–71. doi: 10.1089/thy.2016.0483
8. Jensen CB, Saucke MC, Pitt SC. Active Surveillance for Thyroid Cancer: A Qualitative Study of Barriers and Facilitators to Implementation. BMC Cancer (2021) 21:471. doi: 10.1186/s12885-021-08230-8
9. Roman BR, Brito JP, Saucke MC, Lohia S, Jensen CB, Zaborek N, et al. National Survey of Endocrinologists and Surgeons Regarding Active Surveillance for Low-Risk Papillary Thyroid Cancer. Endocr Pract (2021) 27:1–7. doi: 10.1016/j.eprac.2020.11.003
10. Barbus E, Pestean C, Larg MI, Piciu D. Quality of Life in Thyroid Cancer Patients: A Literature Review. Clujul Med (2017) 90:147–53. doi: 10.15386/cjmed-703
11. Lee JS, Kim JP, Ryu JS, Woo SH. Effect of Wound Massage on Neck Discomfort and Voice Changes After Thyroidectomy. Surgery (2018) 164:965–71. doi: 10.1016/j.surg.2018.05.029
12. Scerrino G, Tudisca C, Bonventre S, Raspanti C, Picone D, Porrello C, et al. Swallowing Disorders After Thyroidectomy: What We Know and Where We Are. A Systematic Review. Int J Surg (2017) 41 Suppl 1:S94–S102. doi: 10.1016/j.ijsu.2017.03.078
13. Rodriguez-Torres J, Lopez-Lopez L, Cabrera-Martos I, Torres-Sanchez I, Ortiz-Rubio A, Valenza MC. Musculoskeletal Neck Disorders in Thyroid Cancer Patients After Thyroidectomy. Eur J Cancer Care (Engl) (2019) 28:e13053. doi: 10.1111/ecc.13053
14. Park YM, Oh KH, Cho JG, Baek SK, Kwon SY, Jung KY, et al. Changes in Voice- and Swallowing-Related Symptoms After Thyroidectomy: One-Year Follow-Up Study. Ann Otol Rhinol Laryngol (2018) 127:171–7. doi: 10.1177/0003489417751472
15. Ha TK, Kim DW, Park HK, Shin GW, Heo YJ, Baek JW, et al. Comparison of Postoperative Neck Pain and Discomfort, Swallowing Difficulty, and Voice Change After Conventional Open, Endoscopic, and Robotic Thyroidectomy: A Single-Center Cohort Study. Front Endocrinol (Lausanne) (2018) 9:416. doi: 10.3389/fendo.2018.00416
16. Krekeler BN, Wendt E, Macdonald C, Orne J, Francis DO, Sippel R, et al. Patient-Reported Dysphagia After Thyroidectomy: A Qualitative Study. JAMA Otolaryngol Head Neck Surg (2018) 144:342–8. doi: 10.1001/jamaoto.2017.3378
17. Ren YX, Yang J, Sun WZ, Chen Y, Wu XF, Huang N, et al. Application of Lateral Supraclavicular Incision in Unilateral Thyroid Papillary Carcinoma Surgery. Braz J Otorhinolaryngol (2021). doi: 10.1016/j.bjorl.2021.03.010
18. Chen ZQ, Wang L, Li T, Hu SY, Zhi XT. Supraclavicular Lateral Collar Incision Versus Conventional Approach for Thyroidectomy: Supplement for Minimally Invasive Techniques With Extended Indications. J Laparoendosc Adv Surg Tech A (2011) 21:45–50. doi: 10.1089/lap.2010.0236
19. Gao M, Ge M, Ji Q, Cheng R, Lu H, Guan H, et al. 2016 Chinese Expert Consensus and Guidelines for the Diagnosis and Treatment of Papillary Thyroid Microcarcinoma. Cancer Biol Med (2017) 14:203–11. doi: 10.20892/j.issn.2095-3941.2017.0051
20. Zhang X, Zhang L, Xue S, Wang P, Chen G. Predictive Factors of Lateral Lymph Node Metastasis in Solitary Papillary Thyroid Microcarcinoma Without Gross Extrathyroidal Extension. Asian J Surg (2019) 42:563–70. doi: 10.1016/j.asjsur.2018.07.003
21. Brodie AG. Anatomy and Physiology of Head and Neck Musculature. Am J Orthod (1950) 36:831–44. doi: 10.1016/0002-9416(50)90038-8
22. Kohan EJ, Wirth GA. Anatomy of the Neck. Clinics Plast Surg (2014) 41:1–6. doi: 10.1016/j.cps.2013.09.016
23. Carlson GW. Surgical Anatomy of the Neck. Surg Clin North Am (1993) 73:837–52. doi: 10.1016/s0039-6109(16)46087-1
24. Stone JA, Figueroa RE. Embryology and Anatomy of the Neck. Neuroimaging Clin N Am (2000) 10:55–+.
25. Giorgio SMD, Mansi L. Atlas of Anatomy: Head, Neck, and Neuroanatomy. Eur J Nucl Med Mol Imaging (2017) 44:735–. doi: 10.1007/s00259-017-3623-6
26. Huettner F, Vasconez LO, de la Torre JI. Neck Rejuvenation-Anatomy and Clinical Correlation. Facial Plast Surg (2012) 28:40–51. doi: 10.1055/s-0032-1305789
27. Bogduk N. The Anatomy and Pathophysiology of Neck Pain. Phys Med Rehabil Clin N Am (2003) 14:455–72. doi: 10.1016/S1047-9651(03)00041-X
28. Kang JB, Kim EY, Park YL, Park CH, Yun J-S. A Comparison of Postoperative Pain After Conventional Open Thyroidectomy and Single-Incision, Gasless, Endoscopic Transaxillary Thyroidectomy: A Single Institute Prospective Study. Ann Surg Treat Res (2017) 92:9–14. doi: 10.4174/astr.2017.92.1.9
29. Jantharapattana K, Maethasith J. Transaxillary Gasless Endoscopic Thyroidectomy Versus Conventional Open Thyroidectomy: A Randomized Study. Eur Arch Otorhinolaryngol (2017) 274:495–500. doi: 10.1007/s00405-016-4242-8
Keywords: supraclavicular approach, lobectomy, papillary thyroid microcarcinoma, postoperative symptom, prospective
Citation: Xue S, Wang Q, Chen G, Wang P and Zhang L (2022) Supraclavicular Approach of Lobectomy Improves Quality of Life for Patients With Unilateral Papillary Thyroid Microcarcinoma: A Prospective Cohort Study. Front. Endocrinol. 12:766444. doi: 10.3389/fendo.2021.766444
Received: 29 August 2021; Accepted: 29 November 2021;
Published: 04 January 2022.
Edited by:
Eleonora Molinaro, University of Pisa, ItalyReviewed by:
Yu Lan, Nankai University, ChinaGabriele Materazzi, University of Pisa, Italy
Maria Cristina Campopiano, University of Pisa, Italy
Copyright © 2022 Xue, Wang, Chen, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Zhang, emhhbmdsaTEyM0BqbHUuZWR1LmNu; Guang Chen, Y2d1YW5nQGpsdS5lZHUuY24=
 Shuai Xue
Shuai Xue Qiuli Wang1
Qiuli Wang1