- 1Department of Surgical Oncology and Endocrine Surgery, University Medical Center Utrecht, Utrecht, Netherlands
- 2Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
Purpose: Conventional thyroidectomy has been standard of care for surgical thyroid nodules. For cosmetic purposes different minimally invasive and remote-access surgical approaches have been developed. At present, the most used robotic and endoscopic thyroidectomy approaches are minimally invasive video assisted thyroidectomy (MIVAT), bilateral axillo-breast approach endoscopic thyroidectomy (BABA-ET), bilateral axillo-breast approach robotic thyroidectomy (BABA-RT), transoral endoscopic thyroidectomy via vestibular approach (TOETVA), retro-auricular endoscopic thyroidectomy (RA-ET), retro-auricular robotic thyroidectomy (RA-RT), gasless transaxillary endoscopic thyroidectomy (GTET) and robot assisted transaxillary surgery (RATS). The purpose of this systematic review was to evaluate whether minimally invasive techniques are not inferior to conventional thyroidectomy.
Methods: A systematic search was conducted in Medline, Embase and Web of Science to identify original articles investigating operating time, length of hospital stay and complication rates regarding recurrent laryngeal nerve injury and hypocalcemia, of the different minimally invasive techniques.
Results: Out of 569 identified manuscripts, 98 studies met the inclusion criteria. Most studies were retrospective in nature. The results of the systematic review varied. Thirty-one articles were included in the meta-analysis. Compared to the standard of care, the meta-analysis showed no significant difference in length of hospital stay, except a longer stay after BABA-ET. No significant difference in incidence of recurrent laryngeal nerve injury and hypocalcemia was seen. As expected, operating time was significantly longer for most minimally invasive techniques.
Conclusions: This is the first comprehensive systematic review and meta-analysis comparing the eight most commonly used minimally invasive thyroid surgeries individually with standard of care. It can be concluded that minimally invasive techniques do not lead to more complications or longer hospital stay and are, therefore, not inferior to conventional thyroidectomy.
Introduction
During the last century the number of detected thyroid nodules has increased significantly. At present, nearly 5% of the female population has a thyroid nodule (1). For thyroid nodules that require surgery, conventional thyroidectomy has been standard of care (2). The extent of surgery varies from lobectomy to total thyroidectomy. Due to new diagnostic techniques to detect small malignant lesions and better surveillance, the number of thyroidectomies performed has increased substantially (3). Conventional thyroidectomy provides excellent exposure of the thyroid but leaves the patient with a visible scar in the lower region of the neck. Since most patients with a thyroid nodule are young women, different techniques have emerged to avoid a potentially disfiguring scar (2).
The first innovative thyroid technique was the endoscopic thyroidectomy, first performed in 1997 by Huscher (4). Two years later Miccoli performed the first minimally invasive video assisted thyroidectomy (MIVAT) (5). In the following years different types of endoscopic remote access techniques were introduced. Of the many endoscopic remote access techniques, the gasless transaxillary endoscopic thyroidectomy (GTET), bilateral axillo-breast approach (BABA), retro-auricular (RA) facelift approach, and transoral endoscopic thyroidectomy via vestibular approach (TOETVA) are the most commonly used techniques today (6). To date TOETVA, as shown in Figure 1, is the only technique performed without cutaneous scars (9). In 2007, the Da Vinci robotic platform, was first used for robot-assisted transaxillary surgery (RATS) by Chung et al. (10). Since then, bilateral axillo-breast and RA approaches have also been developed for the Da Vinci system (10).
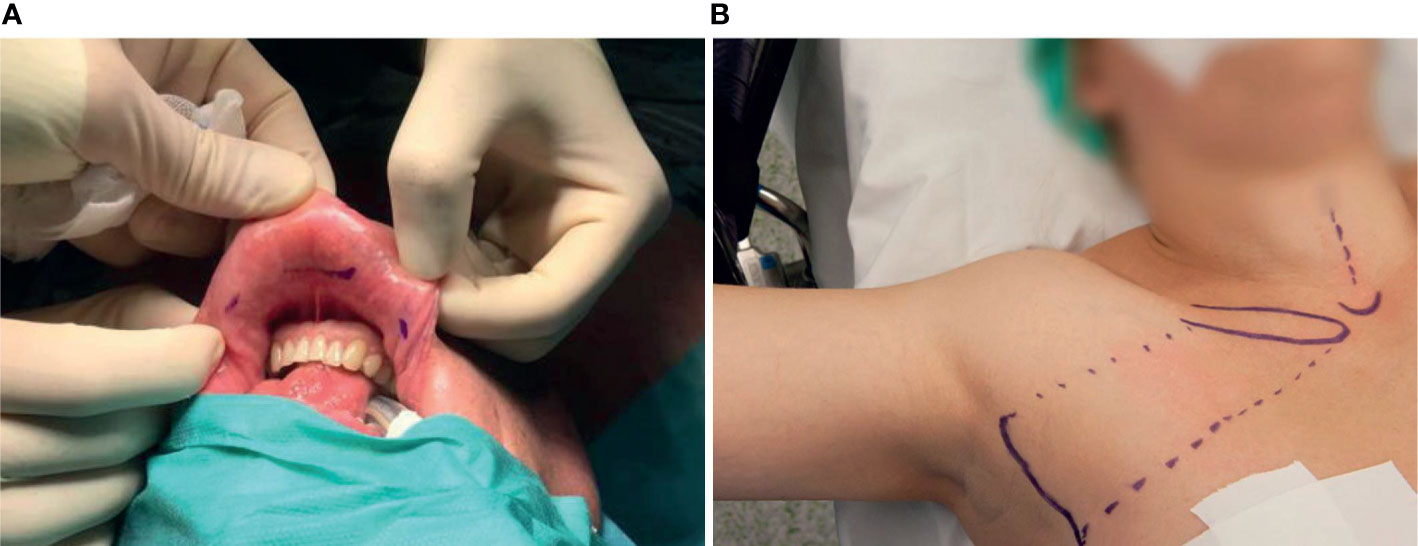
Figure 1 Preoperatively marked patients who will undergo (A) TOETVA (7). Three incisions will be made in the oral vestibule, one for the camera and two laterally for dissection and coagulation instruments; and (B) RATS (8). The incision site is marked laterally. The dotted lines mark the borders of the surgical working space.
In this systematic review, the MIVAT, TOETVA, transaxillary, bilateral axillo-breast and retro-auricular techniques are compared regarding operating time, hospital stay and complications.
Methods
Search Strategy
This systematic review was reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (PRISMA). Eligible studies were identified using Medline, Embase and Web of Science on 11 November 2020. There was no limitation to language or publication date during the search. Combinations of the following keywords and its synonyms were used in the search: “robotic thyroidectomy”, “endoscopic thyroidectomy”, “thyroid surgery”, “RATS”, “TOETVA”, “BABA”, “MIVAT”, “facelift” and “outcome”. In addition, reference lists of included studies were carefully analyzed for related studies. The full search can be found in the Supplementary Material.
Study Selection
Studies were included that reported total operating time, length of hospital stay, outcomes including transient/permanent recurrent laryngeal nerve (RLN) palsy and/or transient/permanent hypocalcemia; and were either a (non-)randomized controlled trial, controlled clinical trial or observational study. Studies with and without control groups were included. Only studies published as original articles and written in English were included. Exclusion criteria were preclinical studies, (systematic) reviews, guidelines, case reports, publications in abstract form only, editorials, letters or conference proceedings.
The titles and abstracts were reviewed by one author (DA) and discussed with another author (LHdV). This was followed by full-text review of potentially eligible studies. Disagreements were discussed and solved with help of a third reviewer (LL) when necessary.
Quality Analysis of the Studies
Non-randomized and observational studies were assessed using the MINORS checklist, while randomized controlled studies were assessed using the Cochrane risk of bias tool (11, 12).
Data Extraction
For each study included in the final analysis, the following data was extracted: title, study design, author, year of publication, geographic location, number of patients, patients’ age, gender, surgical approach, type of procedure, total operating time, hospital stay, transient RLN palsy (defined as hoarseness <6 months), permanent RLN palsy (hoarseness >6 months), transient hypocalcemia (defined as hypoparathyroidism <6 months) and permanent hypocalcemia (hypoparathyroidism >6 months). In most studies, hypoparathyroidism was defined as a reduction in serum iPTH and/or iCa concentration below the normal limit, with or without hypocalcemic symptoms. Due to heterogeneous reporting on cosmetic results, cosmetic satisfaction could not be analyzed in this study.
Both the mean and median were extracted from the articles, if available. Some articles reported results on partial, subtotal or total thyroidectomy; some studies reported results combining multiple extents of surgeries. Means were noted with SD and medians with ranges, if provided in the original article. To provide an impression of operating time and length of hospital stay, the median and interquartile range (IQR) was calculated per technique. This was done using the overall mean per article. The same was done for the incidence of RLN injury and hypocalcemia, using the percentage per article. Articles that described the mean operating time for both partial and total thyroidectomy were included to assess median overall operating time.
Statistical Analysis
Only studies comparing a minimal invasive technique to conventional thyroidectomy (standard of care) were included in the meta-analysis, studies without control arms were therefore not included. Data was analyzed using Review Manager software, version 5.0 (Cochrane Collaboration, Oxford, UK). Standardized mean difference (SMD) was calculated for continues variables and odds ratio (OR) for the dichotomous variables, including 95% confidence intervals (CI). The Mantel-Haenszel method for pooling was used in case of multiple odds ratios close to one and even sample sizes in both arms. In plots with zero events in one arm without one of these characteristics Peto’s method was used (13). I2 above 50% was considered substantial heterogeneity. A random effects model was used for all analyses. P <0.05 was considered to be statistically significant.
Results
Study Characteristics
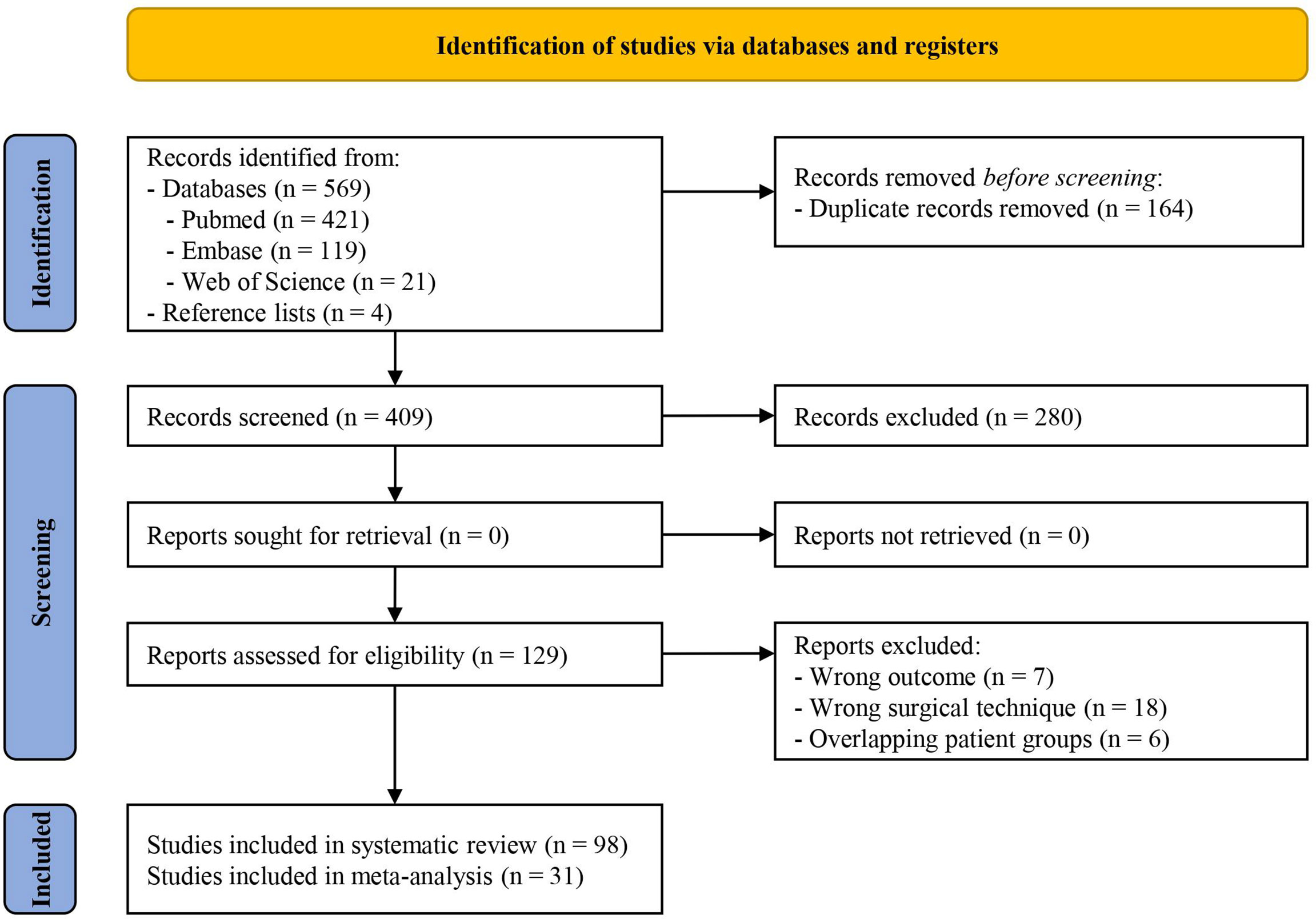
A flowchart of study selection is shown in Figure 2. A total of 569 articles were retrieved from the databases. Four additional references were found through the reference lists. After duplication removal 409 articles were left. All 409 articles were screened, and 280 articles were excluded based on the abstract, leaving 129 eligible articles. After reading the full text, 31 additional articles were excluded. Ninety-eight articles were included in the qualitative analysis (2, 14–110). Among the 98 articles, there were five randomized studies, one non-randomized study and 92 observational studies. Twenty-one studies were conducted in North America, three in South America, 11 in Europa, one in Africa and 62 in Asia. Study characteristics are shown in Supplementary Table 1.
A total of 25,373 participants were included. Median age was 44 years. The vast majority of patients were female. Sample sizes ranged from five to 5,000 participants.
Thirteen articles described the bilateral axillo-breast approach endoscopic thyroidectomy (BABA-ET) in a total number of 1,567 patients, whilst the bilateral axillo-breast approach robotic thyroidectomy (BABA-RT) was described in 15 articles and included 1,498 patients. Eighteen articles described the results of the MIVAT in 4,180 patients. Fourteen articles described the TOETVA in 802 patients. There were five articles that conducted thyroidectomy through the retro-auricular endoscopic approach (RA-ET) in 89 patients. The retro-auricular robotic approach (RA-RT) included 55 patients in two articles. The GTET was described in ten papers and involved 2,017 patients. Thirty articles described the RATS and included the most patients, 15,165 in total.
Quality of Included Studies
All included studies were considered high quality. Full quality assessment can be found in Supplementary Tables 2, 3.
Operating Time
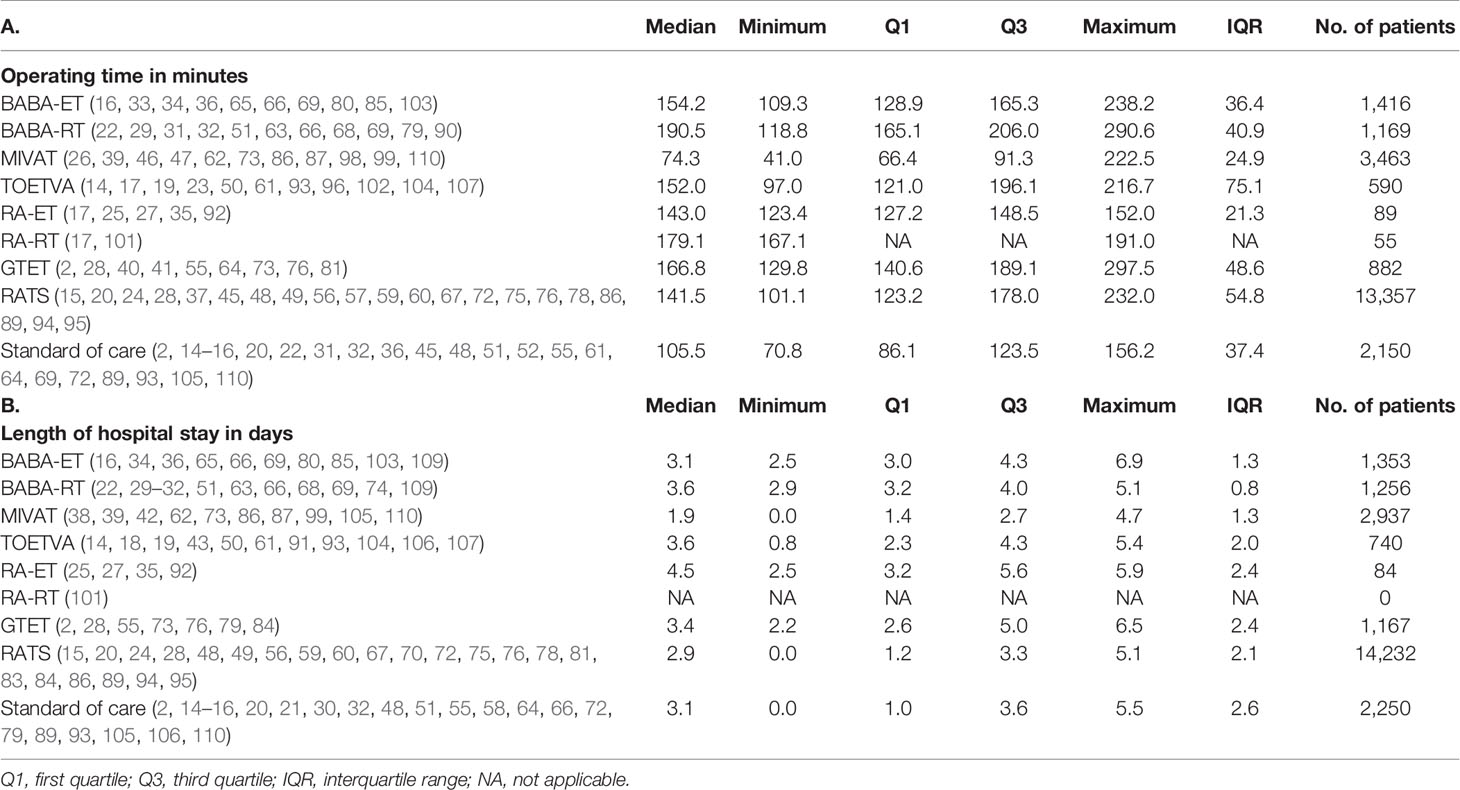
The mean or median operating times per study are shown in Supplementary Table 4. The median operating times including IQR per technique are shown in Table 1A. The median operating time of conventional thyroidectomy was 105.5 minutes. For all minimally invasive techniques, the median operating time was longer than the standard of care, with the exception of the MIVAT, which required 74.3 minutes.
The meta-analysis displayed in Figure 3 showed a significantly longer operating time for the BABA-ET, BABA-RT, MIVAT (lobectomy), TOETVA, RATS techniques in comparison to standard of care. Operating times for the MIVAT (total thyroidectomy) and GTET were not significantly different compared to standard of care.
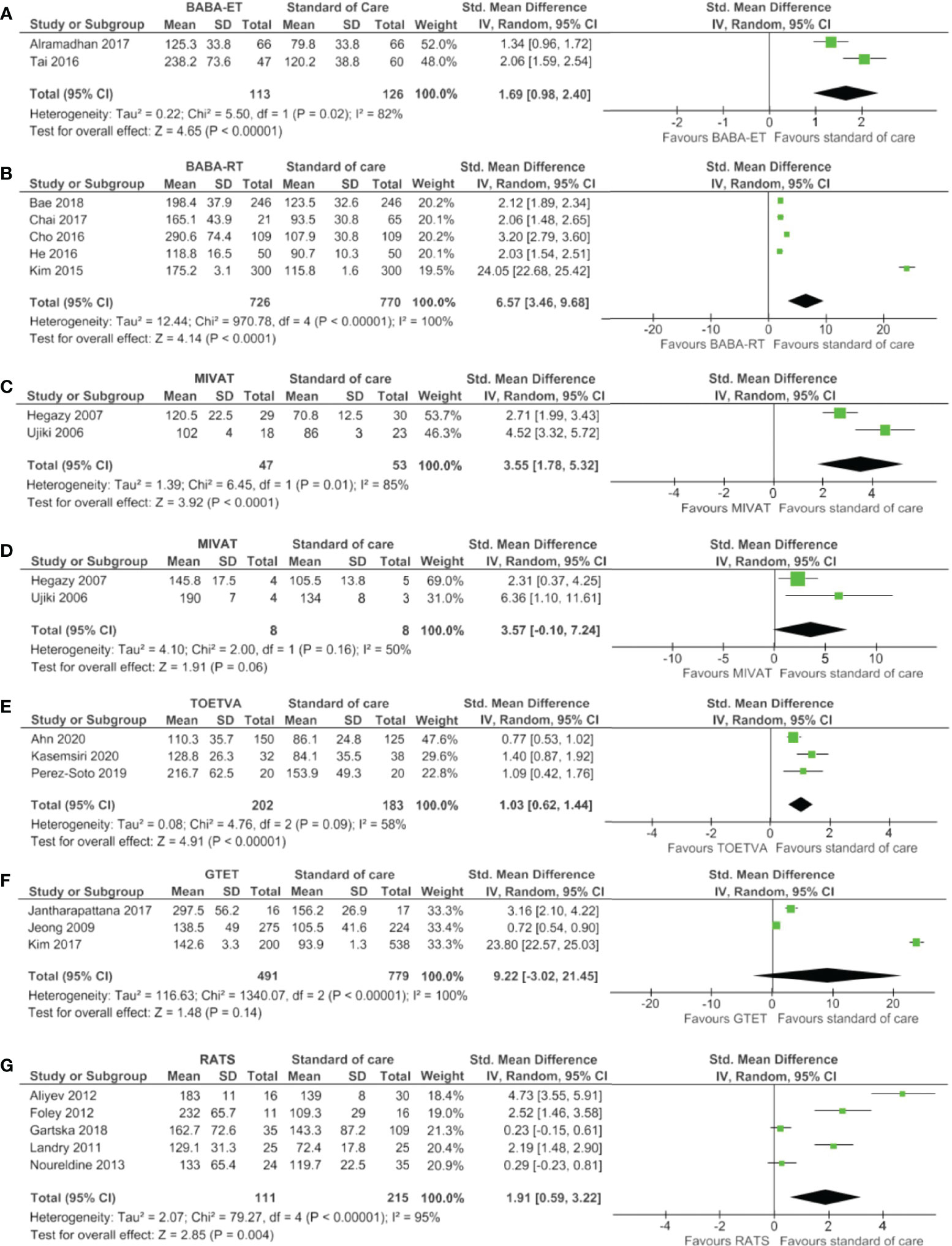
Figure 3 Forest plots of operating time for (A) BABA-ET, (B) BABA-RT, (C) MIVAT lobectomy, (D) MIVAT total thyroidectomy, (E) TOETVA, (F) GTET and (G) RATS.
Hospital Stay
Mean or median length of hospital stay per study is shown in Supplementary Table 4. The median length of hospital stay including IQR per technique is shown in Table 1B. A median hospital stay of approximately three days was reported for all techniques including the standard of care, except for the RA-ET and MIVAT which had a median hospital stay of 4.5 and 1.9 days, respectively. Length of hospital stay was not reported for the RA-RT.
The meta-analysis presented in Figure 4 showed a significantly longer length of hospital stay for the BABA-ET compared to the standard of care. For all other minimally invasive techniques, no significant difference was seen compared to standard of care.
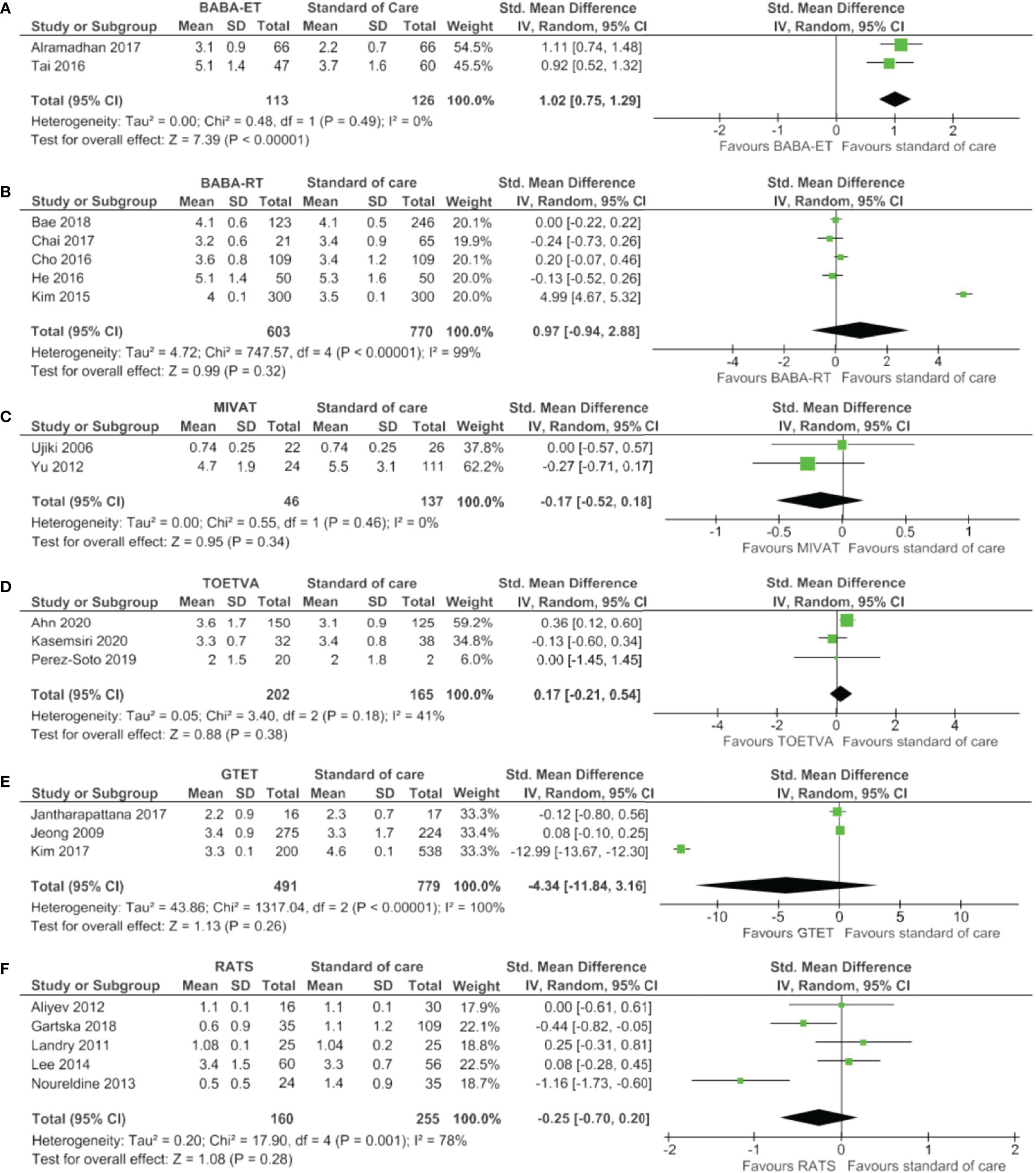
Figure 4 Forests plots of hospital stay for (A) BABA-ET, (B) BABA-RT, (C) MIVAT, (D) TOETVA, (E) GTET and (F) RATS.
Transient RLN Injury
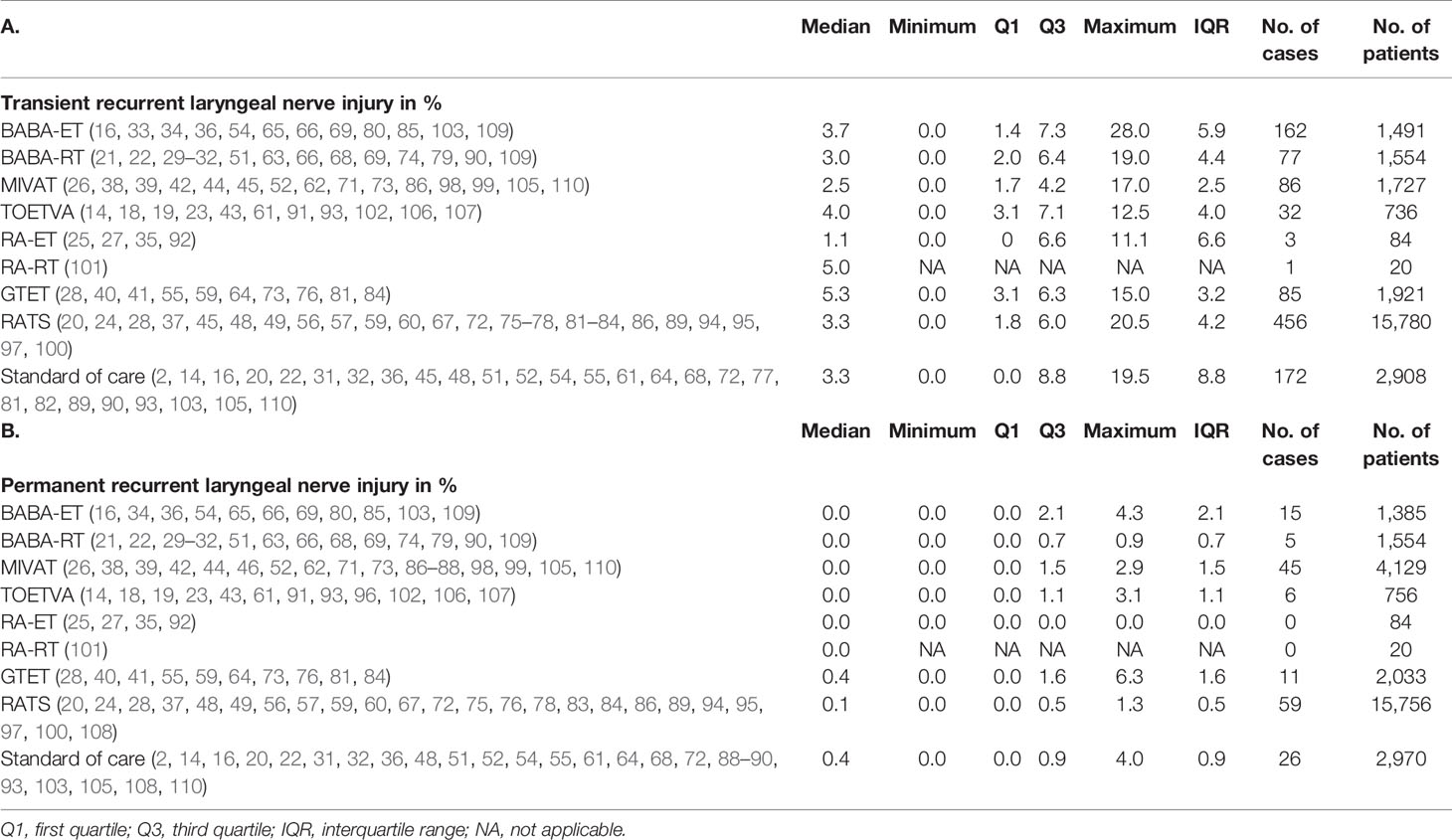
Results on transient RLN injury can be found in Supplementary Table 4 per study and in Table 2A per technique. The median incidence of transient RLN injury after BABA-ET (3.7% of 1,491 patients), BABA-RT (3.0% of 1,554 patients), MIVAT (2.5% of 1,727 patients), TOETVA (4.0% of 736 patients) and RATS (3.3% of 15,780) was comparable to the standard of care, which was 3.3% of 2,908 patients. The median incidence of RLN injury was higher in RA-RT and GTET patients (5.0% of 20 patients and 5.3% of 1,921 patients, respectively) and lower after RA-ET (1.1% of 84 patients).
As shown in Figure 5, the meta-analysis showed no significant difference between the minimally invasive techniques and the standard of care considering transient RLN injury.
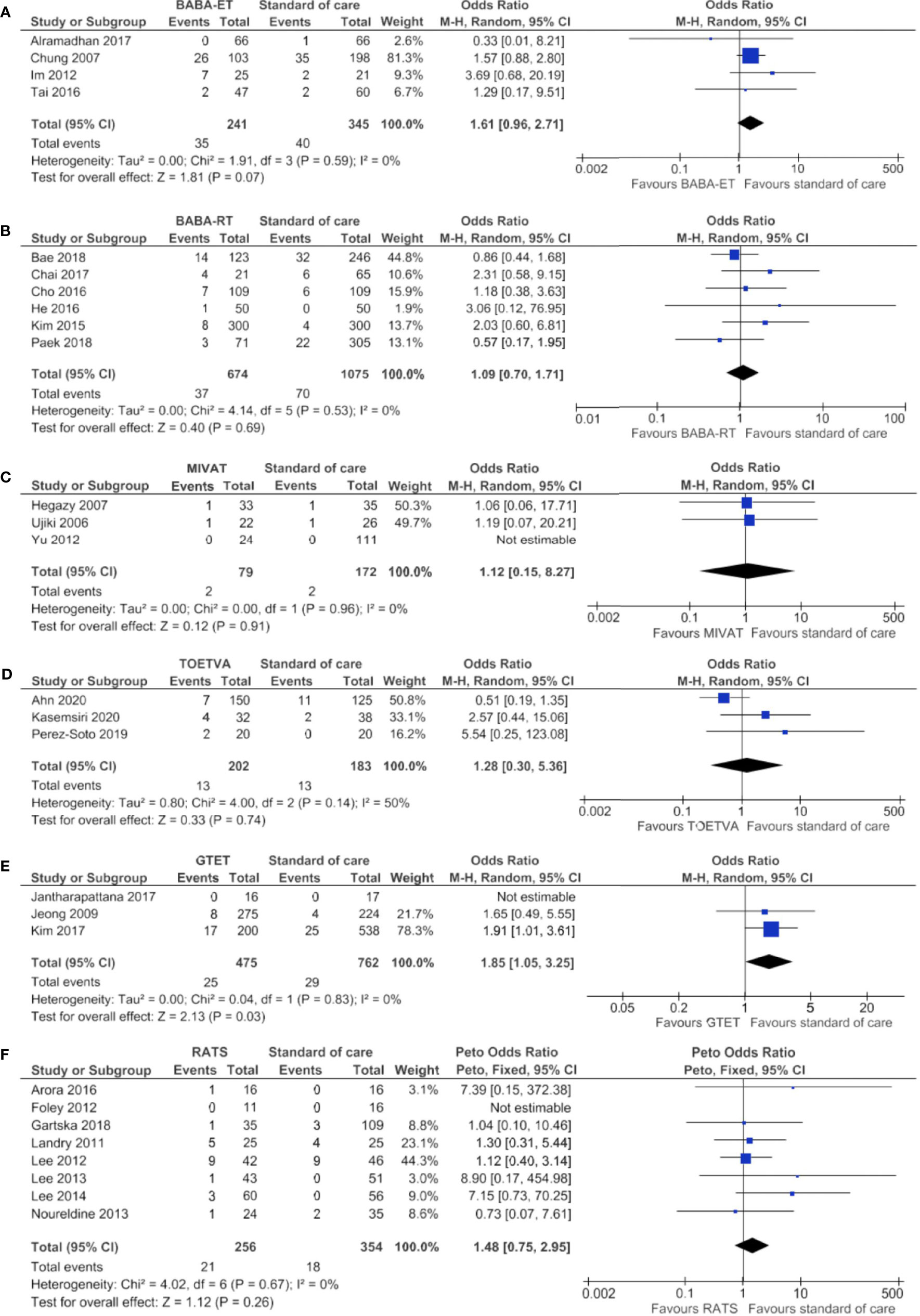
Figure 5 Forests plots of transient recurrent laryngeal nerve injury for (A) BABA-ET, (B) BABA-RT, (C) MIVAT, (D) TOETVA, (E) GTET and (F) RATS.
Permanent RLN Injury
Permanent RLN injury results are shown in Supplementary Table 4 per study and in Table 2B per technique. The median incidence of permanent RLN injury was 0.4% in 2,970 standard of care patients and was comparable for all minimally invasive techniques, ranging from 0.0% to 0.4%.
Figure 6 shows the meta-analysis, which confirmed no significant difference for the BABA-ET, BABA-RT, MIVAT, TOETVA, GTET and RATS compared to the standard of care.
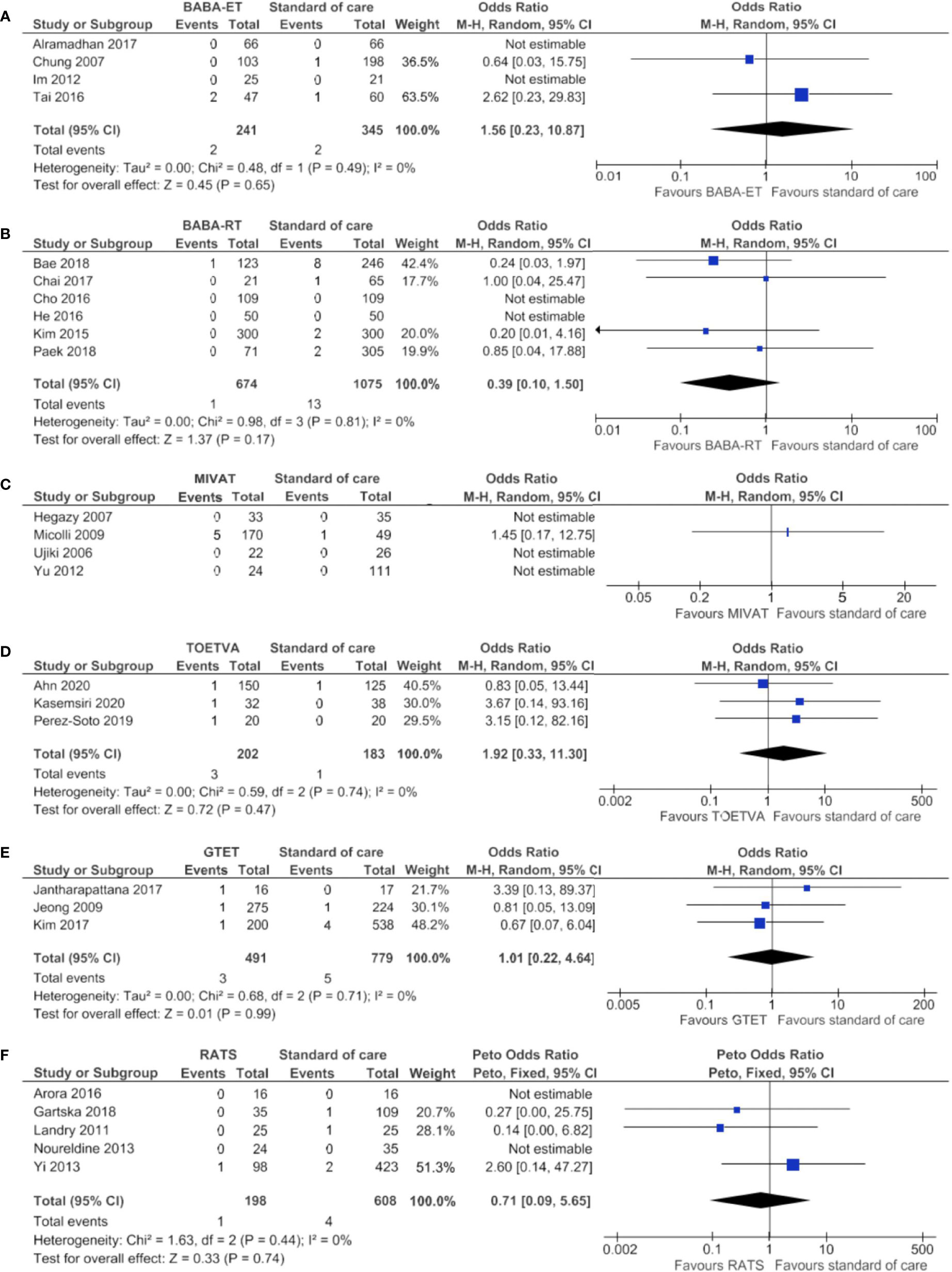
Figure 6 Forests plots of permanent recurrent laryngeal nerve injury for (A) BABA-ET, (B) BABA-RT, (C) MIVAT, (D) TOETVA, (E) GTET and (F) RATS.
Transient Hypocalcemia
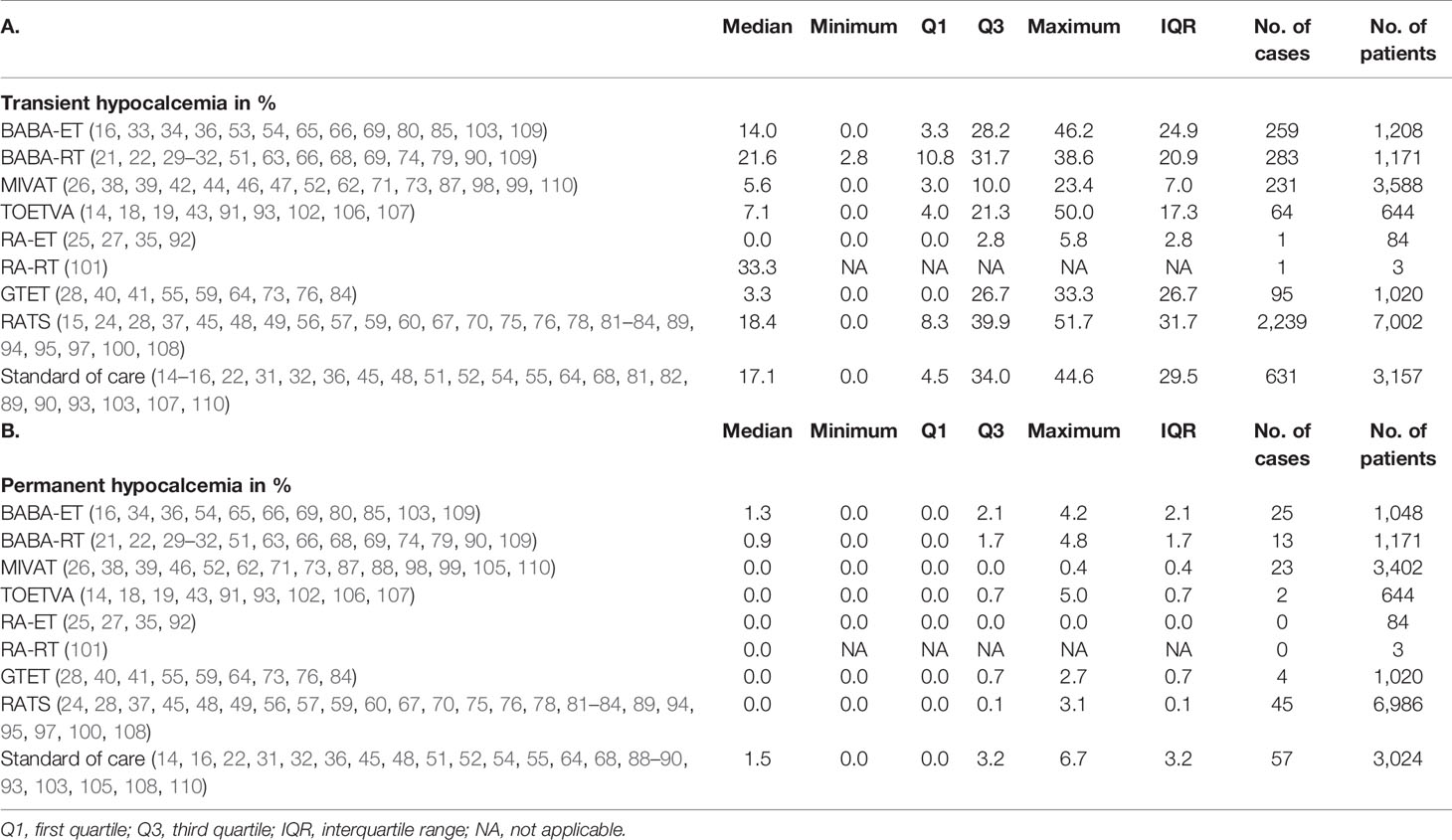
Results on the incidence of transient hypocalcemia can be found in Supplementary Table 4 per study and in Table 3A per technique. The median incidence of transient hypocalcemia seemed to vary between techniques. Transient hypocalcemia occurred in 17.1% of 3,157 patients after standard of care, which was similar to the incidence after RATS (18.4% of 7,002 patients). The median incidence was lower after BABA-ET, MIVAT, TOETVA, RA-ET and GTET (14.0% of 1,208 patients, 5.6% of 3,588 patients, 7.1% of 644 patients, 0.0% of 84 patients and 3.3% of 1,020 patients, respectively) and higher after BABA-RT and RA-RT (21.6% of 1,171 patients and one of three patients, respectively).
The meta-analysis is displayed in Figure 7 and showed no significant difference between the minimally invasive techniques and standard of care.
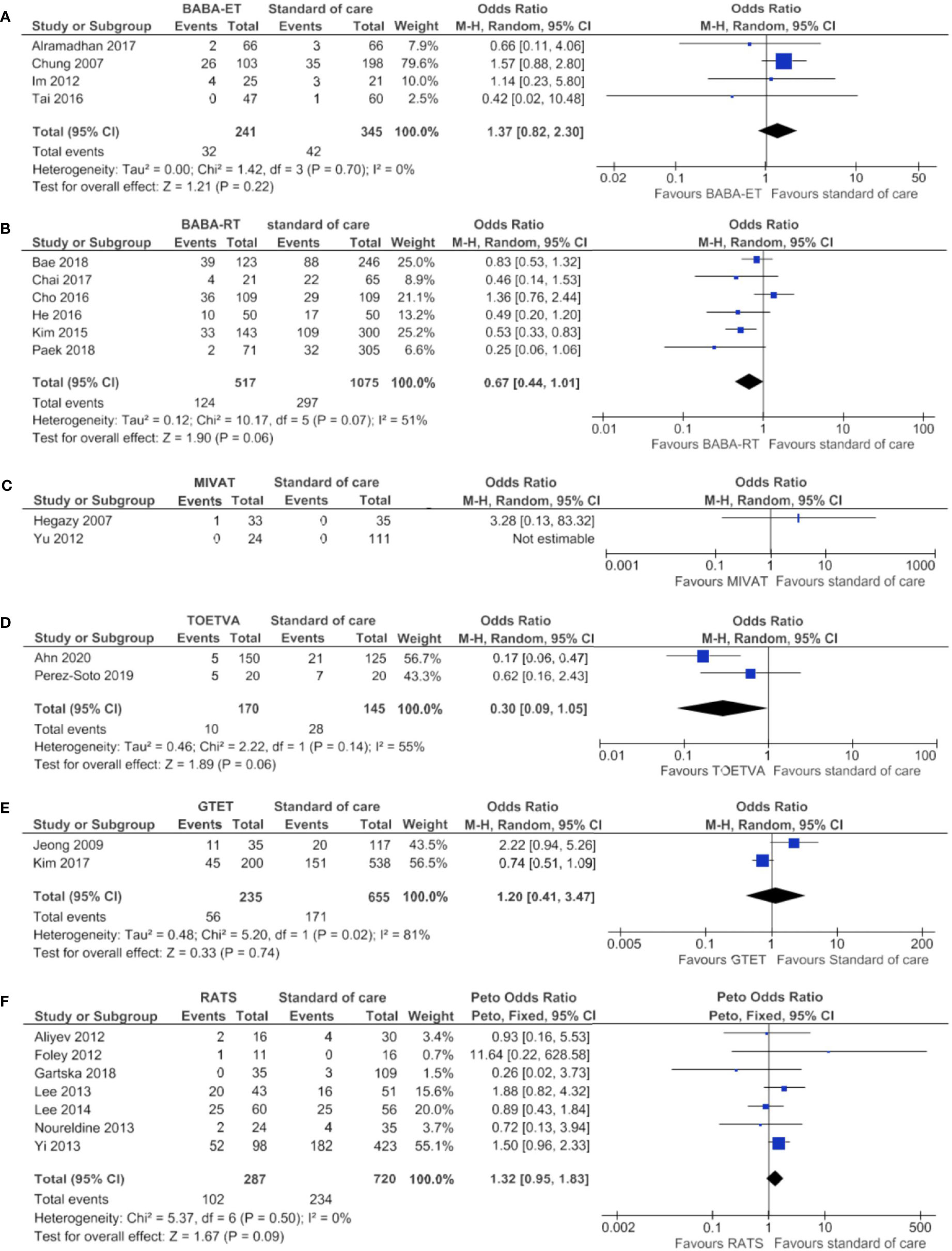
Figure 7 Forests plots of transient hypocalcemia for (A) BABA-ET, (B) BABA-RT, (C) MIVAT, (D) TOETVA, (E) GTET and (F) RATS.
Permanent Hypocalcemia
Results on permanent hypocalcemia can be found in in Supplementary Table 4 per study and in Table 3B per technique. The median incidence of permanent hypocalcemia after standard of care was 1.5% of 3,024 patients. The median incidence was lower for all other minimally invasive techniques and varied between 0.0% and 1.3%.
The meta-analysis in Figure 8, showed no significant difference in incidence of transient hypocalcemia after BABA-ET, BABA-RT, MIVAT, TOETVA, GTET and RATS compared to the standard of care.
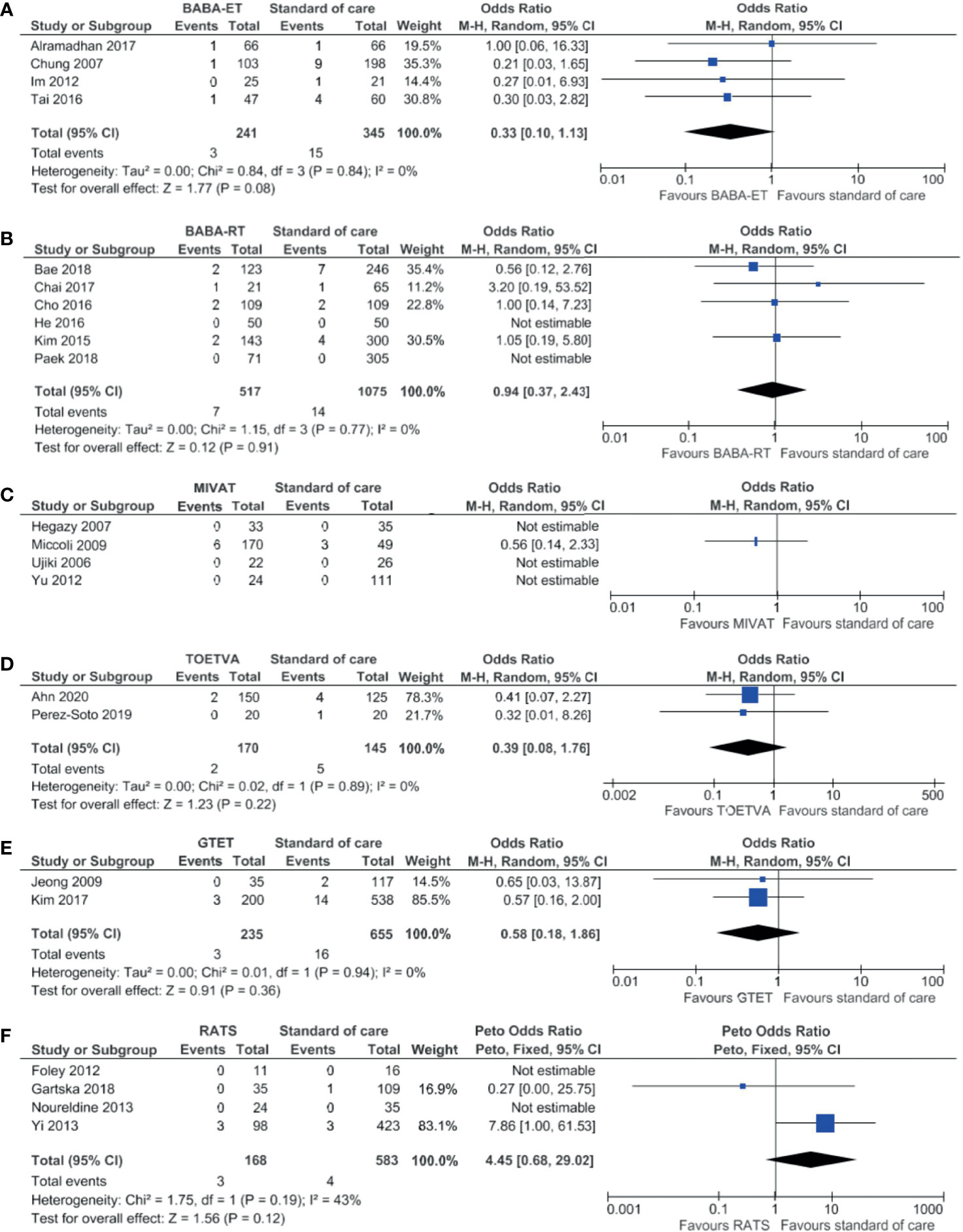
Figure 8 Forests plots of permanent hypocalcemia for (A) BABA-ET, (B) BABA-RT, (C) MIVAT, (D) TOETVA, (E) GTET and (F) RATS.
Discussion
This systematic review and meta-analysis shows that minimally invasive techniques are not inferior to cervical thyroidectomy with regards to length of hospital stay, transient RLN injury, permanent RLN injury, transient hypocalcemia and permanent hypocalcemia. Prior to this study, multiple systematic reviews have been published regarding either the robotic thyroidectomy techniques or endoscopic thyroidectomy techniques (111–119). However, these systematic reviews combine the different types of techniques. In this systematic review and meta-analysis all minimally invasive techniques were analyzed independently. To the best of our knowledge, this is the largest and most comprehensive systematic review and meta-analysis comparing the eight widely used robotic and endoscopic thyroidectomy techniques.
While the results of our systematic review suggest that the MIVAT is the only minimally invasive technique with a shorter operating time than standard of care, the meta-analysis showed that all techniques, except the GTET have a longer operating time than standard of care. This is to be expected since the docking of the robot platform is time consuming, and in some techniques a subcutaneous route to the thyroid needs to be developed. This longer operating time for the endoscopic and robotic surgical techniques is in concordance with the findings of two other meta-analyses (117, 119).
To provide an overview of the operating time and length of hospital stay, the median overall operating time and hospital stay were calculated. Many studies did not provide the percentage of total thyroidectomies or lobectomies. This makes interpretation of median operating time and length of hospital stay not reliable. The meta-analysis revealed that there was no significant difference regarding the length of hospital stay, between the minimally invasive techniques compared to standard of care, with the exception of shorter hospital stay after BABA-ET. In other studies, also no significant difference was found between the minimally invasive techniques and the conventional approach (112, 114, 116, 117, 119). However, length of hospital stay is not a good metric to assess the best thyroidectomy approach, since it is mostly determined by local prevailing hospital protocols rather than outcome of surgery.
The systematic review showed that the RA-RT and GTET patients had more transient RLN injury compared to the standard of care, while the incidence was lower or comparable after the other techniques. The meta-analysis showed that for the BABA-ET, BABA-RT, RATS, MIVAT and TOETVA no significant difference was found in transient RLN injury when compared to the cervical thyroidectomy. Results from the systematic review regarding the permanent RLN injury showed that the BABA-ET and MIVAT were the only two techniques with more permanent RLN injuries than the standard of care. The meta-analysis, however, showed that none of the minimally invasive technique had a statistically significant difference with the standard of care. Other meta-analyses also found no significant difference in RLN injury (112, 114, 119).
Risk of hypocalcemia is largely influenced by the surgical extent. However, in most articles it was not clearly stated whether hypocalcemia was reported for all surgical extents or solely for total thyroidectomy. Results from this systematic review regarding transient hypocalcemia differed between the techniques. It seemed that the BABA-ET, MIVAT, TOETVA, RA-ET and GTET led to fewer transient hypocalcemia cases than the standard of care. The meta-analysis showed no statistically significant difference between standard of care and minimally invasive techniques. The systematic review showed that all minimally invasive techniques had less cases of permanent hypocalcemia than the standard of care. The meta-analysis showed no significant difference between the minimally invasive techniques and standard of care considering permanent hypocalcemia. Other meta-analyses also found no statistical difference in hypocalcemia between minimally invasive techniques and conventional thyroidectomy (112, 117, 119). Only Jiang et al. reported a lower incidence of hypocalcemia after the endoscopic technique (116). The RA-ET and RA-RT could not be included in the meta-analysis, because of lacking control arms. Therefore the results of RA-ET and RA-RT are solely based on the systematic review.
Minimally invasive techniques can also be used to perform completion thyroidectomies in patients who have undergone minimally invasive thyroid surgery before. Of the studies included in this article, completion thyroidectomy was described by eight studies, using all mentioned techniques except the RA-ET and RA-RT (31, 34, 41, 43, 46, 57, 65, 89). Moreover, several other studies described the safety and feasibility of minimally invasive techniques for the completion thyroidectomy, showing the vast range of application of these techniques (65, 120–122). It is advised to either perform re-operation within two weeks after initial surgery or after two to three months to minimize complications due to adhesions (57, 65, 120).
This systematic review has few limitations. First, there were only a few randomized studies included. The majority of the articles are retrospective in nature, which may have led to selection and reporting bias. Furthermore, only the studies with control groups, a minority of the articles, could be included in the meta-analysis. Lastly, the incidence of permanent RLN injury and permanent hypocalcemia was low in all groups, which made it difficult to show differences between standard of care and minimally invasive techniques.
Previous meta-analyses included mainly studies from Asia (112, 115, 116). Strength of our paper is the inclusion of studies from North America and European countries, in addition to the previously reported Asian articles. Therefore, our results are also applicable to Western populations.
Conclusion
This study provides a comprehensive review on the most used minimally invasive thyroid surgical techniques. From the systematic review and meta-analysis, it can be concluded that for selected patients, these modern techniques are not inferior to standard of care and are a safe alternative, with the advantage of avoiding a potentially disfiguring scar in the neck.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.719397/full#supplementary-material
References
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel DJ, Nikiforov YE. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer. The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid (2016) 26:1–133. doi: 10.1089/thy.2015.0020
2. Jantharapattana K. Transaxillary Gasless Endoscopic Thyroidectomy Versus Conventional Open Thyroidectomy: A Randomized Study. Eur Arch Otorhinolaryngol (2017) 274:495–500. doi: 10.1007/s00405-016-4242-8
3. Vaccarella S, Franceschi S, Bray F, Wild CP, Plummer M, Dal Maso L. Worldwide Thyroid Cancer Epidemic? The Increasing Impact of Overdiagnosis. N Engl J Med (2016) 375:614–7. doi: 10.1056/NEJMp1604412
4. Huscher CS, Chiodini S, Napolitano C, Recher A. Endoscopic Right Thyroid Lobectomy. Surg Endosc (1997) 11:877. doi: 10.1007/s004649900476
5. Miccoli P, Berti P, Conte M, Bendinelli C, Marcocci C. Minimally Invasive Surgery for Thyroid Small Nodules: Preliminary Report. J Endocrinol Invest (1999) 22:849–51. doi: 10.1007/BF03343657
6. Tae K, Ji YB, Song CM, Ryu J. Robotic and Endoscopic Thyroid Surgery: Evolution and Advances. Clin Exp Otorhinolaryngol (2019) 12:1–11. doi: 10.21053/ceo.2018.00766
7. Vriens MR, Borel Rinkes IHM. TOETVA: Schildklierchirurgie Zonder Blijvend Litteken [TOETVA: Thyroid Surgery Without Permanent Scar]. Ned Tijdschr Geneeskd (2019) 163:D3397. doi: 10.21037/gs.2018.02.01
8. Vriens MR, Kist JW, Lodewijk L, van Hillegersberg R, Borel Rinkes IHM. Robotgeassisteerde Transaxillaire Schildklieroperatie [Robot-Assisted Transaxillary Thyroid Surgery]. Ned Tijdschr Geneeskd (2013) 157(28):A5841.
9. Luna-Ortiz K, Gómez-Pedraza A, Anuwong A. Lessons Learned From the Transoral Endoscopic Thyroidectomy With Vestibular Approach (TOETVA) for the Treatment of Thyroid Carcinoma. Ann Surg Oncol (2020) 27:1356–60. doi: 10.1245/s10434-019-07899-3
10. Chang E, Kim HY, Koh YW, Chung WY. Overview of Robotic Thyroidectomy. Gland Surg (2017) 6:218–28. doi: 10.21037/gs.2017.03.18
11. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (Minors): Development and Validation of a New Instrument. ANZ J Surg (2003) 73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x
12. Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing Risk of Bias in a Randomized Trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 6.2 (Updated February 2021). Chichester (UK): Cochrane (2021). Available at: www.training.cochrane.org/handbook.
13. Deeks JJ, Higgins JPT, Altman DG. Chapter 10: Analysing Data and Undertaking Meta-Analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 6.2 (Updated February 2021). Chichester (UK): Cochrane (2021). Available at: www.training.cochrane.org/handbook.
14. Ahn JH, Yi JW. Transoral Endoscopic Thyroidectomy for Thyroid Carcinoma: Outcomes and Surgical Completeness in 150 Single-Surgeon Cases. Surg Endosc (2020) 34:861–7. doi: 10.1007/s00464-019-06841-8
15. Aliyev S, Taskin HE, Agcaoglu O, Aksoy E, Milas M, Siperstein A, et al. Robotic Transaxillary Total Thyroidectomy Through a Single Axillary Incision. Surgery (2013) 153:705–10. doi: 10.1016/j.surg.2012.10.013
16. Alramadhan M, Choe JH, Lee JH, Kim JH, Kim JS. Propensity Score-Matched Analysis of the Endoscopic Bilateral Axillo-Breast Approach (BABA) Versus Conventional Open Thyroidectomy in Patients With Benign or Intermediate Fine-Needle Aspiration Cytology Results, a Retrospective Study. Int J Surg (2017) 48:9–15. doi: 10.1016/j.ijsu.2017.09.077
17. Alshehri M, Mohamed HE, Moulthrop T, Kandil E. Robotic Thyroidectomy and Parathyroidectomy: An Initial Experience With Retroauricular Approach. Head Neck (2017) 39:1568–72. doi: 10.1002/hed.24794
18. Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg (2016) 40:491–7. doi: 10.1007/s00268-015-3320-1
19. Anuwong A, Sasanakietkul T, Jitpratoom P, Ketwong K, Kim HY, Dionigi G, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA): Indications, Techniques and Results. Surg Endosc (2018) 32:456–65. doi: 10.1007/s00464-017-5705-8
20. Arora A, Garas G, Sharma S, Muthuswamy K, Budge J, Palazzo F, et al. Comparing Transaxillary Robotic Thyroidectomy With Conventional Surgery in a UK Population: A Case Control Study. Int J Surg (2016) 27:110–7. doi: 10.1016/j.ijsu.2016.01.071
21. Bae DS, Suh BJ, Park JK, Koo do H. Technical, Oncological, and Functional Safety of Bilateral Axillo-Breast Approach (BABA) Robotic Total Thyroidectomy. Surg Laparosc Endosc Percutan Tech (2016) 26:253–8. doi: 10.1097/SLE.0000000000000262
22. Bae DS, Koo do H. A Propensity Score-Matched Comparison Study of Surgical Outcomes in Patients With Differentiated Thyroid Cancer After Robotic Versus Open Total Thyroidectomy. World J Surg (2019) 43:540–51. doi: 10.1007/s00268-018-4802-8
23. Bakkar S, Al Hyari M, Naghawi M, Corsini C, Miccoli P. Transoral Thyroidectomy: A Viable Surgical Option With Unprecedented Complications-A Case Series. J Endocrin (2018) 41(7):809–13. doi: 10.1007/s40618-017-0808-6
24. Ban EJ, Yoo JY, Kim WW, Son HY, Park S, Lee SH, et al. Surgical Complications After Robotic Thyroidectomy for Thyroid Carcinoma: A Single Center Experience With 3,000 Patients. Surg Endosc (2014) 28:2555–63. doi: 10.1007/s00464-014-3502-1
25. Ban MH, Chang JW, Kim WS, Byeon HK, Koh YQ, Park JH. Minimal Endoscope-Assisted Thyroidectomy Through a Retroauricular Approach: An Evolving Solo Surgery Technique. Surg Laparosc Endosc Percutan Tech (2016) 26:e109–12. doi: 10.1097/SLE.0000000000000353
26. Bellotti C, Capponi MG, Cinquepalmi M, Castagnola G, Marchetta S, Mallozzi F, et al. MIVAT: The Last 2 Years Experience, Tips and Techniques After More Than 10 Years. Surg Endosc (2018) 32:2340–4. doi: 10.1007/s00464-017-5929-7
27. Byeon HK, Holsinger FC, Tufano RP, Park JH, Sim NS, Kim WS, et al. Endoscopic Retroauricular Thyroidectomy: Preliminary Results. Surg Endosc (2016) 30:355–65. doi: 10.1007/s00464-015-4202-1
28. Cabot JC, Lee CR, Brunaud L, Kleiman DA, Chung WY, Fahey TJ, et al. Robotic and Endoscopic Transaxillary Thyroidectomies may be Cost Prohibitive When Compared to Standard Cervical Thyroidectomy: A Cost Analysis. Surgery (2012) 152:1016–24. doi: 10.1016/j.surg.2012.08.029
29. Chae S, Min SY, Park WS. Comparison Study of Robotic Thyroidectomies Through a Bilateral Axillo-Breast Approach and a Transoral Approach. J Laparoendosc Adv Surg Tech A (2020) 30:175–82. doi: 10.1089/lap.2019.0585
30. Chai YJ, Kim HY, Kim HK, Jun SH, Dionigi G, Anuwong A, et al. Comparative Analysis of 2 Robotic Thyroidectomy Procedures: Transoral Versus Bilateral Axillo-Breast Approach. Head Neck (2018) 40:886–92. doi: 10.1002/hed.25034
31. Chai YJ, Suh H, Woo JW, Yu HW, Song RY, Kwon H, et al. Surgical Safety and Oncological Completeness of Robotic Thyroidectomy for Thyroid Carcinoma Larger Than 2 Cm. Surg Endosc (2017) 31:1235–40. doi: 10.1007/s00464-016-5097-1
32. Cho JN, Park WS, Min SY, Han SA, Song JW. Surgical Outcomes of Robotic Thyroidectomy vs. Conventional Open Thyroidectomy for Papillary Thyroid Carcinoma. World J Surg Oncol (2016) 14:181. doi: 10.1186/s12957-016-0929-y
33. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic Thyroidectomy Using a New Bilateral Axillo-Breast Approach. World J Surg (2007) 31:601–6. doi: 10.1007/s00268-006-0481-y
34. Choi Y, Lee KE, Chung KW, Kim SW, Choe JH, Koo do H, et al. Endoscopic Thyroidectomy via Bilateral Axillo-Breast Approach (BABA): Review of 512 Cases in a Single Institute. Surg Endosc (2012) 26:948–55. doi: 10.1007/s00464-011-1973-x
35. Chung EJ, Park MW, Cho JG, Baek SK, Kwon SY, Woo JS, et al. A Prospective 1-Year Comparative Study of Endoscopic Thyroidectomy via a Retroauricular Approach Versus Conventional Open Thyroidectomy at a Single Institution. Ann Surg Oncol (2015) 22:3014–21. doi: 10.1245/s10434-014-4361-7
36. Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, et al. Endoscopic Thyroidectomy for Thyroid Malignancies: Comparison With Conventional Open Thyroidectomy. World J Surg (2007) 31:2302–8. doi: 10.1007/s00268-007-9117-0
37. Ciabatti PG, Burali G, D’Ascanio L. Single-Incision Robot-Assisted Transaxillary Surgery for Early-Stage Papillary Thyroid Cancer. Ann Otol Rhinol Laryngol (2012) 121:811–5. doi: 10.1177/000348941212101207
38. Dedivitis RA, Guimarães AV. Preliminary Results From Minimally Invasive Video-Assisted Thyroidectomy. Sao Paulo Med J (2005) 123:298–9. doi: 10.1590/S1516-31802005000600011
39. Dobrinja C, Trevisan G, Makovac P, Liguori G. Minimally Invasive Video-Assisted Thyroidectomy Compared With Conventional Thyroidectomy in a General Surgery Department. Surg Endosc (2009) 23:2263–7. doi: 10.1007/s00464-008-0303-4
40. Duncan TD, Rashid Q, Speights F, Ejeh I. Endoscopic Transaxillary Approach to the Thyroid Gland: Our Early Experience. Surg Endosc (2007) 21:2166–71. doi: 10.1007/s00464-007-9325-6
41. Duncan TD, Rashid Q, Speights F, Ejeh I. Transaxillary Endoscopic Thyroidectomy: An Alternative to Traditional Open Thyroidectomy. J Natl Med Assoc (2009) 101:783–7. doi: 10.1016/S0027-9684(15)31006-3
42. Fan Y, Guo B, Guo S, Kang J, Wu B, Zhang P, et al. Minimally Invasive Video-Assisted Thyroidectomy: Experience of 300 Cases. Surg Endosc (2010) 24:2393–400. doi: 10.1007/s00464-010-0960-y
43. Fernandez Ranvier G, Meknat A, Guevara DE, Llorente PM, Vidal Fortuny J, Sneider M, et al. International Multi-Institutional Experience With the Transoral Endoscopic Thyroidectomy Vestibular Approach. J Laparoendosc Adv Surg Tech A (2020) 30:278–83. doi: 10.1089/lap.2019.0645
44. Fík Z, Astl J, Zábrodský M, Lukeš P, Merunka I, Betka J, et al. Minimally Invasive Video-Assisted Versus Minimally Invasive Nonendoscopic Thyroidectomy. BioMed Res Int (2014) 2014:45017. doi: 10.1155/2014/450170
45. Foley CS, Agcaoglu O, Siperstein AE, Berber E. Robotic Transaxillary Endocrine Surgery: A Comparison With Conventional Open Technique. Surg Endosc (2012) 26:2259–66. doi: 10.1007/s00464-012-2169-8
46. Frank E, Park J, Simantal A Jr, Vuong C, Liu Y, Kwon D, et al. Minimally Invasive Video-Assisted Thyroidectomy: Almost a Decade of Experience at an Academic Center. Am Surg (2016) 82:949–52. doi: 10.1177/000313481608201019
47. Gagner M, Inabnet WB. Endoscopic Thyroidectomy for Solitary Thyroid Nodules. Thyroid (2001) 11:161–3. doi: 10.1089/105072501300042848
48. Garstka M, Mohsin K, Ali DB, Shalaby H, Ibraheem K, Farag M, et al. Well-Differentiated Thyroid Cancer and Robotic Transaxillary Surgery at a North American Institution. J Surg Res (2018) 228:170–8. doi: 10.1016/j.jss.2018.03.030
49. Giulianotti PC, Addeo P, Buchs NC, Ayloo SM, Bianco FM. Robotic Thyroidectomy: An Initial Experience With the Gasless Transaxillary Approach. J Laparoendosc Adv Surg Tech A (2012) 22:387–91. doi: 10.1089/lap.2010.0380
50. Guo F, Wang W, Zhu X, Xiang C, Wang P, Wang Y. Comparative Study Between Endoscopic Thyroid Surgery via the Oral Vestibular Approach and the Areola Approach. J Laparoendosc Adv Surg Tech A (2020) 30:170–4. doi: 10.1089/lap.2019.0562
51. He QQ, Zhu J, Zhuang DY, Fan ZY, Zheng LM, Zhou P, et al. Comparative Study Between Robotic Total Thyroidectomy With Central Lymph Node Dissection via Bilateral Axillo-Breast Approach and Conventional Open Procedure for Papillary Thyroid Microcarcinoma. Chin Med J (2016) 129:2160–6. doi: 10.4103/0366-6999.189911
52. Hegazy MA, Khater AA, Setit AE, Amin MA, Kotb SZ, El shafei MA, et al. Minimally Invasive Video-Assisted Thyroidectomy for Small Follicular Thyroid Nodules. World J Surg (2007) 31:1743–50. doi: 10.1007/s00268-007-9147-7
53. Hur SM, Kim SH, Lee SK, Kim WW, Choe JH, Lee JE, et al. New Endoscopic Thyroidectomy With the Bilateral Areolar Approach: A Comparison With the Bilateral Axillo-Breast Approach. Surg Laparosc Endosc Percutan Tech (2011) 21:219–24. doi: 10.1097/SLE.0b013e3182239989
54. Im HJ, Koo do H, Paeng JC, Lee KE, Chung YS, Lim I, et al. Evaluation of Surgical Completeness in Endoscopic Thyroidectomy Compared With Open Thyroidectomy With Regard to Remnant Ablation. Clin Nucl Med (2012) 37:148–51. doi: 10.1097/RLU.0b013e3182335fdc
55. Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, et al. Comparative Study of Endoscopic Thyroidectomy Versus Conventional Open Thyroidectomy in Papillary Thyroid Microcarcinoma (PTMC) Patients. J Surg Oncol (2009) 100:477–80. doi: 10.1002/jso.21367
56. Kandil E, Winters R, Aslam R, Friedlander P, Bellows C. Transaxillary Gasless Robotic Thyroid Surgery With Nerve Monitoring: Initial Two Experince in a North American Center. Minim Invasive Ther Allied Technol (2012) 21:90–5. doi: 10.3109/13645706.2011.561862
57. Kandil EH, Noureldine SI, Yao L, Slakey DP. Robotic Transaxillary Thyroidectomy: An Examination of the First One Hundred Cases. J Am Coll Surg (2012) 214:558–64. doi: 10.1016/j.jamcollsurg.2012.01.002
58. Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, et al. Gasless Endoscopic Thyroidectomy Using Trans-Axillary Approach; Surgical Outcome of 581 Patients. Endocr J (2009) 56:361–9. doi: 10.1507/endocrj.K08E-306
59. Kang SW, Lee SC, Lee SH, Lee KY, Jeong JJ, Lee YS, et al. Robotic Thyroid Surgery Using a Gasless, Transaxillary Approach and the Da Vinci S System: The Operative Outcomes of 338 Consecutive Patients. Surgery (2009) 146:1048–55. doi: 10.1016/j.surg.2009.09.007
60. Kang SW, Park JH, Jeong JS, Lee CR, Park S, Lee SH, et al. Prospects of Robotic Thyroidectomy Using a Gasless, Transaxillary Approach for the Management of Thyroid Carcinoma. Surg Laparosc Endosc Percutan Tech (2011) 21:223–9. doi: 10.1097/SLE.0b013e3182266f31
61. Kasemsiri P, Trakulkajornsak S, Bamroong P, Mahawerawat K, Piromchai P, Ratanaanekchai T. Comparison of Quality of Life Between Patients Undergoing Trans-Oral Endoscopic Thyroid Surgery and Conventional Open Surgery. BMC Surg (2020) 20:18. doi: 10.1186/s12893-020-0685-3
62. Kim AJ, Liu JC, Ganly I, Kraus DH. Minimally Invasive Video-Assisted Thyroidectomy 2.0: Expanded Indications in a Tertiary Care Cancer Center. Head Neck (2011) 33:1557–60. doi: 10.1002/hed.21633
63. Kim EB, Cho JW, Lee YM, Sung TY, Yoon JH, Chung KW, et al. Postsurgical Outcomes and Surgical Completeness of Robotic Thyroid Surgery: A Single Surgeon’s Experience on 700 Cases. J Laparoendosc Adv Surg Tech A (2018) 28:540–5. doi: 10.1089/lap.2017.0597
64. Kim EY, Lee KH, Park YL, Park CH, Lee CR, Jeong JJ, et al. Single-Incision, Gasless, Endoscopic Trans-Axillary Total Thyroidectomy: A Feasible and Oncologic Safe Surgery in Patients With Papillary Thyroid Carcinoma. J Laparoendosc Adv Surg Tech A (2017) 27:1158–64. doi: 10.1089/lap.2016.0669
65. Kim SJ, Lee KE, Choe JH, Lee J, Koo do H, Oh SK, et al. Endoscopic Completion Thyroidectomy by the Bilateral Axillo-Breast Approach. Surg Laparosc Endosc Percutan Tech (2010) 20:312–6. doi: 10.1097/SLE.0b013e3181f195fc
66. Kim SK, Woo JW, Park I, Lee JH, Choe JH, Kim JH, et al. Propensity Score-Matched Analysis of Robotic Versus Endoscopic Bilateral Axillo-Breast Approach (BABA) Thyroidectomy in Papillary Thyroid Carcinoma. Langenbeck’s Arch Surg (2017) 402:243–50. doi: 10.1007/s00423-016-1528-7
67. Kim W, Kim K, Kim M, Choi J, Lee C, Lee J, et al. Yonsei Experience of 5,000 Transaxillary Robotic Thyroidectomies. World J Surg (2018) 42:393–401. doi: 10.1007/s00268-017-4209-y
68. Kim WW, Jung JH, Park HY. A Single Surgeon’s Experience and Surgical Outcomes of 300 Robotic Thyroid Surgeries Using a Bilateral Axillo-Breast Approach. J Surg Oncol (2015) 111:135–40. doi: 10.1002/jso.23793
69. Kim WW, Kim JS, Hur SM, Kim SH, Lee SK, Choi JH, et al. Is Robotic Surgery Superior to Endoscopic and Open Surgeries in Thyroid Cancer? World J Surg (2011) 35:779–84. doi: 10.1007/s00268-011-0960-7
70. Kuppersmith RB, Holsinger FC. Robotic Thyroid Surgery: An Initial Experience With North American Patients. Laryngoscope (2011) 121:521–6. doi: 10.1002/lary.21347
71. Lai SY, Walvekar RR, Ferris RL. Minimally Invasive Video-Assisted Thyroidectomy: Expanded Indications and Oncologic Completeness. Head Neck (2008) 30:1403–7. doi: 10.1002/hed.20883
72. Landry CS, Grubbs EG, Warneke CL, Ormond M, Chua C, Lee JE, et al. Robot-Assisted Transaxillary Thyroid Surgery in the United States: Is it Comparable to Open Thyroid Lobectomy? Ann Surg Oncol (2012) 19:1269–74. doi: 10.1245/s10434-011-2075-7
73. Lang BH, Wong KP. A Comparison of Surgical Morbidity and Scar Appearance Between Gasless, Transaxillary Endoscopic Thyroidectomy (GTET) and Minimally Invasive Video-Assisted Thyroidectomy (VAT). Ann Surg Oncol (2013) 20:646–52. doi: 10.1245/s10434-012-2613-y
74. Lee HY, Yang IS, Hwang SB, Lee JB, Bae JW, Kim HY. Robotic Thyroid Surgery for Papillary Thyroid Carcinoma: Lessons Learned From 100 Consecutive Surgeries. Surg Laparosc Endosc Percutan Tech A (2015) 25:27–32. doi: 10.1097/SLE.0b013e3182a2b0ae
75. Lee J, Kang SW, Jung JJ, Choi UJ, Yun JH, Nam KH, et al. Multicenter Study of Robotic Thyroidectomy: Short-Term Postoperative Outcomes and Surgeon Ergonomic Considerations. Ann Surg Oncol (2011) 18:2538–47. doi: 10.1245/s10434-011-1628-0
76. Lee J, Lee JH, Nah KY, Soh EY, Chung WY. Comparison of Endoscopic and Robotic Thyroidectomy. Ann Surg Oncol (2011) 18:1439–46. doi: 10.1245/s10434-010-1486-1
77. Lee J, Na KY, Kim RM, Oh Y, Lee JH, Lee J, et al. Postoperative Functional Voice Changes After Conventional Open or Robotic Thyroidectomy: A Prospective Trial. Ann Surg Oncol (2012) 19:2963–70. doi: 10.1245/s10434-012-2253-2
78. Lee J, Yun JH, Nam KH, Choi UJ, Chung WY, Soh EY. Perioperative Clinical Outcomes After Robotic Thyroidectomy for Thyroid Carcinoma: A Multicenter Study. Surg Endosc (2011) 25:906–12. doi: 10.1007/s00464-010-1296-3
79. Lee KE, Koo do H, Kim SJ, Lee J, Park KS, Oh SK, et al. Outcomes of 109 Patients With Papillary Thyroid Carcinoma Who Underwent Robotic Total Thyroidectomy With Central Node Dissection via the Bilateral Axillo-Breast Approach. Surgery (2010) 148:1207–13. doi: 10.1016/j.surg.2010.09.018
80. Lee MC, Park H, Choi IJ, Lee BC, Lee GH. Comparative Study of a Gasless Transaxillary Approach Versus a Bilateral Axillo-Breast Approach for Endoscopic Thyroidectomy in a Single Institute. Head Neck (2014) 36:702–8. doi: 10.1002/hed.23349
81. Lee S, Kim HY, Lee CR, Park S, Son H, Kang SW, et al. A Prospective Comparison of Patient Body Image After Robotic Thyroidectomy and Conventional Open Thyroidectomy in Patients With Papillary Thyroid Carcinoma. Surgery (2014) 156:117–25. doi: 10.1016/j.surg.2014.02.007
82. Lee S, Lee CR, Lee SC, Park S, Kim HY, Son H, et al. Surgical Completeness of Robotic Thyroidectomy: A Prospective Comparison With Conventional Open Thyroidectomy in Papillary Thyroid Carcinoma Patients. Surg Endosc (2014) 28:1068–75. doi: 10.1007/s00464-013-3303-y
83. Lee S, Rye HR, Park JH, Kim KH, Kang SW, Jeong JJ, et al. Excellence in Robotic Thyroid Surgery: A Comparative Study of Robot-Assisted Versus Conventional Endoscopic Thyroidectomy in Papillary Thyroid Microcarcinoma Patients. Ann Surg (2011) 253:1060–6. doi: 10.1097/SLA.0b013e3182138b54
84. Lee YM, Yi O, Sung TY, Chung KW, Yoon JH, Hong SJ. Surgical Outcomes of Robotic Thyroid Surgery Using a Double Incision Gasless Transaxillary Approach: Analysis of 400 Cases Treated by the Same Surgeon. Head Neck (2014) 36:1413–9. doi: 10.1002/hed.23472
85. Liu SYW, Wong SKH, Chiu PWY, Ng EKW, Liu SY-W, Wong SK-H, et al. Endoscopic Thyroid Lobectomy Using Bilateral Axillo-Breast Approach: Surgical Techniques and Outcomes. Surg Pract (2015) 19:128–32. doi: 10.1111/1744-1633.12124
86. Materazzi G, Fregoli L, Manzini G, Baggiani A, Miccoli M, Miccoli P. Cosmetic Result and Overall Satisfaction After Minimally Invasive Video-Assisted Thyroidectomy (MIVAT) Versus Robot-Assisted Transaxillary Thyroidectomy (RATT): A Prospective Randomized Study. World J Surg (2014) 38:1282–8. doi: 10.1007/s00268-014-2483-5
87. Miccoli P, Biricotti M, Matteucci V, Ambrosini CE, Wu J, Materazzi G. Minimally Invasive Video-Assisted Thyroidectomy: Reflections After More Than 2400 Cases Performed. Surg Endosc (2016) 30:2489–95. doi: 10.1007/s00464-015-4503-4
88. Miccoli P, Pinchera A, Materazzi G, Biagini A, Berti P, Faviana P, et al. Surgical Treatment of Low- and Intermediate-Risk Papillary Thyroid Cancer With Minimally Invasive Video-Assisted Thyroidectomy. J Clin Endocrinol Metab (2009) 94:1618–22. doi: 10.1210/jc.2008-1418
89. Noureldine SI, Jackson NR, Tufano RP, Kandil E. A Comparative North American Experience of Robotic Thyroidectomy in a Thyroid Cancer Population. Langenbecks Arch Surg (2013) 398:1069–74. doi: 10.1007/s00423-013-1123-0
90. Paek SH, Kang KH, Park SJ. A Comparison of Robotic Versus Open Thyroidectomy for Papillary Thyroid Cancer. Surg Laparosc Endosc Percutan Tech (2018) 28:170–3. doi: 10.1097/SLE.0000000000000529
91. Park JO, Anuwong A, Kim MR, Sun DI, Kim MS. Transoral Endoscopic Thyroid Surgery in a Korean Population. Surg Endosc (2019) 33:2104–13. doi: 10.1007/s00464-018-6481-9
92. Park JO, Kim SY, Chun BJ, Joo YH, Cho JH, Park YH, et al. Endoscope-Assisted Facelift Thyroid Surgery: An Initial Experience Using a New Endoscopic Technique. Surg Endosc (2015) 29:1469–75. doi: 10.1007/s00464-014-3826-x
93. Pérez-Soto SH, Ponce de León-Ballesteros G, Montalvo-Hernández J, Sierra-Salazar M, Pantoja Millán JP, Herrera-Hernández MF, et al. Transoral Endoscopic Thyroidectomy by Vestibular Approach-Initial Experience and Comparative Analysis in the First Reported Mexican Cohort. J Laparoendosc Adv Surg Tech A (2019) 29:1526–31. doi: 10.1089/lap.2019.0537
94. Piccoli M, Mullineris B, Gozzo D, Colli G, Pecchini F, Nigro C, et al. Evolution Strategies in Transaxillary Robotic Thyroidectomy: Considerations on the First 449 Cases Performed. J Laparoendosc Adv Surg Tech A (2019) 29:433–40. doi: 10.1089/lap.2019.0021
95. Prete FP, Marzaioli R, Lattarulo S, Paradies D, Barile G, D’Addetta MV, et al. Transaxillary Robotic-Assisted Thyroid Surgery: Technique and Results of a Preliminary Experience on the Da Vinci Xi Platform. BMC Surg (2019) 18:19. doi: 10.1186/s12893-019-0473-0
96. Razavi CR, Khadem MGA, Fondong A, Clark JH, Richmon JD, Tufano RP, et al. Early Outcomes in Transoral Vestibular Thyroidectomy: Robotic Versus Endoscopic Techniques. Head Neck (2018) 40:2246–53. doi: 10.1002/hed.25323
97. Ryu HR, Kang SW, Lee SH, Rhee KY, Jeong JJ, Nam KH, et al. Feasibility and Safety of a New Robotic Thyroidectomy Through a Gasless, Transaxillary Single-Incision Approach. J Am Coll Surg (2010) 211:e13–9. doi: 10.1016/j.jamcollsurg.2010.05.021
98. Schabram J, Vorländer C, Wahl RA. Differentiated Operative Strategy in Minimally Invasive, Video-Assisted Thyroid Surgery Results in 196 Patients. World J Surg (2004) 28:1282–6. doi: 10.1007/s00268-004-7681-0
99. Shan YZ, Zhou LM, Yu ZF, Wang SG, Gao GL, Shen Y, et al. Comparison Between Transareola Singlesite Endoscopic Thyroidectomy and Minimally Invasive Video-Assisted Thyroidectomy. J Int Med Res (2012) 40:2213–9. doi: 10.1177/030006051204000619
100. Stang MT, Yip L, Wharry L, Bartlett DL, McCoy KL, Carty SE. Gasless Transaxillary Endoscopic Thyroidectomy With Robotic Assistance: A High-Volume Experience in North America. Thyroid (2018) 28:1655–61. doi: 10.1089/thy.2018.0404
101. Sung ES, Ji YB, Song CM, Yun BR, Chung WS, Tae K. Robotic Thyroidectomy: Comparison of a Postauricular Facelift Approach With a Gasless Unilateral Axillary Approach. Otolaryngol Head Neck Surg (2016) 154:997–1004. doi: 10.1177/0194599816636366
102. Tae K, Lee DW, Song CM, Ji YB, Park JH, Kim DS, et al. Early Experience of Transoral Thyroidectomy: Comparison of Robotic and Endoscopic Procedures. Head Neck (2019) 41:730–8. doi: 10.1002/hed.25426
103. Tai DKC, Chick W-K, Chan PCM, Lau C-H, Tang DLC. Experience of Endoscopic Thyroidectomy in a Single-Centre Institution. Surg Pr (2016) 20:161–5. doi: 10.1111/1744-1633.12216
104. Tesseroli MAS, Spagnol M, Sanabria Á. Transoral Endoscopic Thyroidectomy by Vestibular Approach (TOETVA): Initial Experience in Brazil. Rev Col Bras Cir (2018) 45:e1951. doi: 10.1590/0100-6991e-20181951
105. Ujiki MB, Sturgeon C, Denham D, Yip L, Angelos P. Minimally Invasive Video-Assisted Thyroidectomy for Follicular Neoplasm: Is There an Advantage Over Conventional Thyroidectomy? Ann Surg Oncol (2006) 13:182–6. doi: 10.1245/ASO.2006.03.057
106. Wang Y, Zhang Z, Zhao Q, Xie Q, Yan H, Yu X, et al. Transoral Endoscopic Thyroid Surgery via the Tri-Vestibular Approach With a Hybrid Space-Maintaining Method: A Preliminary Report. Head Neck (2018) 40:1774–9. doi: 10.1002/hed.25157
107. Yi JW, Yoon SG, Kim HS, Yu HW, Kim SJ, Chai YJ, et al. Transoral Endoscopic Surgery for Papillary Thyroid Carcinoma: Initial Experiences of a Single Surgeon in South Korea. Ann Surg Treat Res (2018) 95:73–9. doi: 10.4174/astr.2018.95.2.73
108. Yi O, Yoon JH, Lee YM, Sung TY, Chung KW, Kim TY, et al. Technical and Oncologic Safety of Robotic Thyroid Surgery. Ann Surg Oncol (2013) 20:1927–33. doi: 10.1245/s10434-012-2850-0
109. Yoo H, Chae BJ, Park HS, Kim KH, Kim SH, Song BJ, et al. Comparison of Surgical Outcomes Between Endoscopic and Robotic Thyroidectomy. J Surg Oncol (2012) 105:705–8. doi: 10.1002/jso.22106
110. Yu JJ, Bao SL, Yu SL, Zhang DQ, Loo WT, Chow LW, et al. Minimally Invasive Video-Assisted Thyroidectomy for the Early-Stage Differential Thyroid Carcinoma. J Transl Med (2012) 10:S13. doi: 10.1186/1479-5876-10-S1-S13
111. Liu J, Song T, Xu M. Minimally Invasive Video-Assisted Versus Conventional Open Thyroidectomy: A Systematic Review of Available Data. Surg Today (2012) 42:848–56. doi: 10.1007/s00595-012-0130-z
112. Pan J, Zhou H, Zhao X, Ding H, Wei L, Qin L, et al. Robotic Thyroidectomy Versus Conventional Open Thyroidectomy for Thyroid Cancer: A Systematic Review and Meta-Analysis. Surg Endosc (2017) 31:3985–4001. doi: 10.1007/s00464-017-5433-0
113. Jackson N, Yao L, Tufano R, Kandil E. Safety of Robotic Thyroidectomy Approaches: Meta-Analysis and Systematic Review. Head Neck (2013) 36:137–43. doi: 10.1002/hed.23223
114. Sun G, Peress L, Pynnonen M. Systematic Review and Meta-Analysis of Robotic vs Conventional Thyroidectomy Approaches for Thyroid Disease. Otolaryngol Head Neck Surg (2014) 150:520–32. doi: 10.1177/0194599814521779
115. Kandil E, Hammad A, Walvekar R, Hu T, Masoodi H, Mohamed S, et al. Robotic Thyroidectomy Versus Nonrobotic Approaches. Surg Innov (2015) 23:317–25. doi: 10.1177/1553350615613451
116. Jiang WJ, Yan PJ, Zhao CL, Si MB, Tian W, Zhang YI, et al. Comparison of Total Endoscopic Thyroidectomy With Conventional Open Thyroidectomy for Treatment of Papillary Thyroid Cancer: A Systematic Review and Meta-Analysis. Surg Endosc (2020) 34:1891–903. doi: 10.1007/s00464-019-07283-y
117. Chen C, Huang S, Huang A, Jia Y, Wang J, Mao M, et al. Total Endoscopic Thyroidectomy Versus Conventional Open Thyroidectomy in Thyroid Cancer: A Systematic Review and Meta-Analysis. Ther Clin Risk Manag (2018) 14:2349–61. doi: 10.2147/TCRM.S183612
118. Lang B, Wong C, Tsang J, Wong K. A Systematic Review and Meta-Analysis Comparing Outcomes Between Robotic-Assisted Thyroidectomy and Non-Robotic Endoscopic Thyroidectomy. J Surg Res (2014) 191:389–98. doi: 10.1016/j.jss.2014.04.023
119. Xing Z, Qiu Y, Abuduwaili M, Xia B, Fei Y, Zhu J, et al. Surgical Outcomes of Different Approaches in Robotic Assisted Thyroidectomy for Thyroid Cancer: A Systematic Review and Bayesian Network Meta-Analysis. Int J Surg (2021) 89:105941. doi: 10.1016/j.ijsu.2021.105941
120. Wu YJ, Chi SY, Chan YC, Chou FF, Wee SY, Wu KT. Scarless Completion Thyroidectomy After Initial Transoral Approach for Differentiated Thyroid Cancer: How and When to Start? Surg Laparosc Endosc Percutan Tech (2021). doi: 10.1097/SLE.0000000000000933
121. Kwak J, Kim SJ, Xu Z, Lee K, Ahn JH, Yu HW, et al. Robotic Completion Thyroidectomy via the Bilateral Axillo-Breast Approach. J Clin Med (2021) 10:1707. doi: 10.3390/jcm10081707
Keywords: minimally invasive video assisted thyroidectomy (MIVAT), bilateral axillo-breast approach endoscopic thyroidectomy (BABA-ET), bilateral axillo-breast approach robotic thyroidectomy (BABA-RT), transoral endoscopic thyroidectomy via vestibular approach (TOETVA), retro-auricular endoscopic thyroidectomy (RA-ET), retro-auricular robotic thyroidectomy (RA-RT), gasless transaxillary endoscopic thyroidectomy (GTET), robot assisted transaxillary surgery (RATS)
Citation: de Vries LH, Aykan D, Lodewijk L, Damen JAA, Borel Rinkes IHM and Vriens MR (2021) Outcomes of Minimally Invasive Thyroid Surgery – A Systematic Review and Meta-Analysis. Front. Endocrinol. 12:719397. doi: 10.3389/fendo.2021.719397
Received: 02 June 2021; Accepted: 26 July 2021;
Published: 12 August 2021.
Edited by:
Schelto Kruijff, University Medical Center Groningen, NetherlandsReviewed by:
Pier Francesco Alesina, Fondazione Ricerca e Cura Giovanni Paolo II, ItalyCarlotta Giani, University of Pisa, Italy
Copyright © 2021 de Vries, Aykan, Lodewijk, Damen, Borel Rinkes and Vriens. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Menno R. Vriens, TXZyaWVuc0B1bWN1dHJlY2h0Lm5s
†These authors have contributed equally to this work and share first authorship
 Lisa H. de Vries
Lisa H. de Vries Dilay Aykan
Dilay Aykan Lutske Lodewijk
Lutske Lodewijk Johanna A. A. Damen2
Johanna A. A. Damen2 Inne H. M. Borel Rinkes
Inne H. M. Borel Rinkes Menno R. Vriens
Menno R. Vriens