- 1Department of Internal Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA, United States
- 2Department of Medicine, David Geffen School of Medicine at University of California, Los Angeles, CA, United States
- 3Vatche and Tamar Manoukian Division of Digestive Diseases, Department of Medicine, David Geffen School of Medicine at University of California, Los Angeles (UCLA), Los Angeles, CA, United States
- 4David Geffen School of Medicine at University of California, UCLA Microbiome Center, Los Angeles, CA, United States
- 5Division of Gastroenterology, Hepatology and Parenteral Nutrition, Veterans Administration Greater Los Angeles Healthcare System, Los Angeles, CA, United States
The study of the intestinal or gut microbiome is a newer field that is rapidly gaining attention. Bidirectional communication between gut microbes and the host can impact numerous biological systems regulating immunity and metabolism to either promote or negatively impact the host’s health. Habitual routines, dietary choices, socioeconomic status, education, host genetics, medical care and environmental factors can all contribute to the composition of an individual’s microbiome. A key environmental factor that may cause negative outcomes is the consumption of nicotine products. The effects of nicotine on the host can be exacerbated by poor dietary choices and together can impact the composition of the gut microbiota to promote the development of metabolic disease including non-alcoholic fatty liver disease. This review explores the contribution of nicotine, poor dietary choices and other unhealthy lifestyle factors to gut dysbiosis.
Introduction
There is considerable variation in microbiome composition and function across individuals. This interindividual variability and plasticity of the intestinal microbiota has hindered efforts to identify a “healthy” microbiota. Diversity and microbial stability are often used as key indicators of gut health because of their inverse association with chronic disease and metabolic dysfunction (1). Reduced microbial diversity has been shown to be associated with various disease states (1). Instability of the gut microbiome can be caused by many factors, including infection, diet, exercise, sleep pattern, exposure to antibiotics, and various co-morbidities. Gut dysbiosis is a broad term (2) that can be defined as the imbalance of gut microbiota associated with an unhealthy outcome. Dysbiosis involves the loss of beneficial microbial input or signal and an expansion of pathogenic microbes (pathobionts). Dysbiosis is thought to trigger pro-inflammatory effects and immune dysregulation associated with various disease states, including non-alcoholic steatohepatitis (NASH) (3).
In 2014, the International Scientific Association for Probiotics and Prebiotics (ISAPP) provided evidence-based recommendations of strain-specific probiotics for defined conditions (4). The microbiome has become a rising topic for the lay public and may hold the key to information capable of reducing co-morbidities and preventing disease (1). Of note, some companies market to the public the ability to analyze the microbiome of an individual to “provide precision nutrition for metabolic disease” (5). More research is needed, especially on the cross-communication between the microbiome and host in order to understand the impact of the microbiome on human disease (3).
Often, the terms “microbiome” and “microbiota” are used interchangeably. In an effort to define the terms more precisely (6) microbiota will be used to define the assemblage of microorganisms present in a defined environment, whereas (7), mostly the colon, but also the upper gastrointestinal tract (8), saliva (9), middle meatus (10), bronchial wash (11), sputum (12), subgingival (13), and throat (14). Microbiome will refer to the entire habitat of a host region with its surrounding environmental conditions, including all microorganisms, bacteria, archaea, lower and higher eukaryotes, viruses, and their genomes (6).
As will be discussed in the body of this review, fiber-depleted diets create a condition ripe for dysbiosis. Moreover, nicotine, the exposure to which may be increasing with the rise of electronic cigarettes (e-cigarettes), has been shown to accentuate the effect of diet and potentially disrupt the microbiome and promote disease.
Impact of Microbiota on Health
The gut is known to harbor a unique and dynamic microbiome as it is exposed to constant external stimuli, including diet, infectious agents, antibiotics and xenobiotics (15–17). Digestible and non-digestible carbohydrates, proteins, fats, polyphenols, prebiotics and probiotics can induce shifts in the microbiota and elicit effects on host immunologic and metabolic markers (18). There appears to be a close relationship between the gut microbiome, health, and diet, suggesting that improvements in health can be modulated via diet through the microbiota.
Microbiome, Immune Dysfunction, and Inflammation
The microbiome serves many important functions. In healthy individuals, it confers protection from pathogenic organisms that cause infection. For example, the microbiota produce short-chain fatty acids (SCFAs) via fermentation of complex plant carbohydrates, providing an energy source for colonocytes to maintain full differentiation and regeneration (19). Furthermore, the microbiota synthesizes essential vitamins and amino acids, regulate fat metabolism (20, 21), and produce various small molecules that interact with the host environment. The microbiome, in turn, regulates the development of the immune system (22). For example, a healthy microbiome has an anti-inflammatory function by inhibiting histone deacetylases in regulatory T cells (Tregs) through G-protein coupled receptors (GPCRs) (19).
The use of germ-free (GF) animals has provided evidence that specific microbiota influences the immune system differently. In 1885, Pasteur first proposed the generation of animals deprived of microorganisms to explore the relationship between microbes and their host (22). GF animals display significant defects in the development of primary (thymus and bone marrow) and secondary (lymph nodes and spleen) lymphoid organs and are associated with a decreased frequency of CD4+ and CD8+ intestinal T cell subsets. GF mice also have reduced numbers of intraepithelial lymphocytes that express the αβT cell receptor (TCR) (22, 23). Specific bacterial populations have been linked to specific T-cell effector subset development. For example, T helper 17 [Th17] cells, potent sources of interleukin-17 (IL-17), play a critical role in the clearance of pathogens and the maintenance of the mucosal barrier integrity (22). GF animals have an absence of Th17 (22) and thus, Th17 development is believed to be dependent on the intestinal microbiota (22). Additionally, recent studies have shown that the adhesion of certain microbes [e.g., segmented filamentous bacteria (SFB), Citrobacter rodentium, and Escherichia coli O157] is necessary to trigger a Th17 cell response in intestinal epithelial cells (24). This was shown by colonizing SFB in adult GF mice versus standard mouse microbiota (22, 24, 25). Colonization with SFB conferred enhanced protection compared with GF animals after infection with the bacterial pathogen citrobacter rodentium, a direct outcome of Th17-cell enrichment in these animal’s intestinal microbiomes (25). Interestingly, an exaggerated Th17 response is believed to promote autoimmune arthritis (25, 26), such that microbial signaling and host immune response requires a fine balance.
A unique bidirectional interaction between the mucosal immune system and the gut microbiota allows for the avoidance of an inappropriate immune response towards nonpathogenic microbes while suppressing pathogenic microbes (pathobionts) (27). For example, Bifidobacterium and lactic acid bacteria have been shown to secrete factors that hinder inflammation, presumably via the downregulation of interleukin-8 secretion, NF-kB dependent gene expression, and macrophage-attracting chemokine production (28). Furthermore, Bifidobacterium and lactic acid bacteria are associated with the upregulation of anti-inflammatory Treg cell gene expression (29). Some studies suggest that microbial-derived SCFAs may be contributing to the modulation of host immune responses directly via G-protein-coupled receptors and epigenetic mechanisms, such as methylation activity within the promoter regions of certain genes (30, 31).
Dysbiosis, as defined above, is believed to contribute to the development of various immune-mediated conditions, including inflammatory bowel disease (IBD) (21), rheumatoid arthritis (32), type 1 diabetes mellitus (33), multiple sclerosis (34), and systemic lupus erythematosus (SLE) (35), among many others. IBD, which comprises of Crohn’s disease and ulcerative colitis, is a chronic inflammatory disease that is increasing in prevalence worldwide (36) and has been proposed to arise from an inappropriate mucosal inflammatory response to dysbiosis; this response is believed to be a result of genetic susceptibility and environmental exposure (37). IBD patients have decreased microbial diversity compared with healthy controls, alongside alterations in both composition and function of the intestinal microbiome (38–43). Jacobs and colleagues investigated if unaffected siblings and parents of individuals with IBD carry a pre-disease microbial risk state due to shared genetic and environmental factors. By studying the microbiome and metabolome of pediatric IBD patients and their unaffected first-degree relatives (43), they were able to identify a high correlation between fecal microbial and metabolomics profiles and disease status. Their research proposed that in families at risk for IBD, healthy individuals possess an intestinal microbial/metabolomic state with increased susceptibility to IBD (43). This finding highlights the ability of microbes to increase susceptibility to inflammatory disease via the production of bioactive metabolites, which affect immune activity and epithelial function (43).
Microbiome and Obesity
Obesity, which confers an increased risk for numerous diseases, including hypercholesterolemia, hypertension, type 2 diabetes, cancer, non-alcoholic fatty liver disease (NAFLD), atherosclerosis, cardiovascular disease, and stroke (44, 45), is associated with gut dysbiosis (46). Intestinal microbiota influence the digestion, absorption, metabolism, and storage of ingested nutrients with profound effects on host physiology (46). Environmental and dietary factors can yield a microbiome that modulates host metabolism to promote obesity (46, 47). Advancements in studying the role of a high-fat diet (HFD) and Western diet (WD) on the microbiome has provided insights into the mechanisms of how gut dysbiosis leads to detrimental metabolic changes and why many individuals who consume a HFD or WD develop gut dysbiosis.
Studies of lean and genetically obese (ob/ob) mice (48, 49) and(fa/fa) rats (50) have revealed differences in their metabotypes [i.e., metabolic phenotypes (51)]. Lean and obese gut microbiomes are characterized by different representation of members of the Bacteroidetes, Firmicutes and Actinobacteria phyla of bacteria. One intriguing discovery that follows from these studies is the link between gut microbiomes and host energy harvest and homeostasis (52). Some individuals may harbor microbiota that are more efficient at energy harvest than others; for example, some types of bacteria may be better at processing carbohydrates than others. Other types of bacteria may be adept at manipulating host genes and metabolism in order to store energy, turn off satiety signals, or upregulate inflammatory pathways (52).
A higher baseline ratio of Firmicutes to Bacteroidetes ratio is seen in individuals with obesity, and for these subjects, a reduction in caloric intake resulted in a lower Firmicutes to Bacteroidetes ratio (53, 54). However, Magne et al. (55) reported that it was difficult to associate the Firmicutes/Bacteroidetes ratio with a determined health status or as a hallmark of obesity. Yet, low levels of Bifidobacterium, a key bacterial group, is notably linked to obesity, particularly in children (56). Furthermore, a gut microbiome that is largely dominated by Firmicutes showed altered methylation in gene promoters linked to obesity and cardiovascular disease (57). Some bacterial species, such as Lactobacillus spp., can be obesogenic or anti-obesogenic, depending on the specific strain; others have the potential to alleviate obesity-associated metabolic complications (58, 59). Part of the mechanism of action is via the interaction between the gut microbiota, host immunity, and gut barrier function (60, 61).
An abundance of Akkermansia muciniphila, has been linked to a healthy metabolic profile, with greater improvement in obesity-associated metabolic parameters (plasma triglycerides, body fat distribution, and insulin tolerance) for individuals with obesity following dietary intervention (62). These findings highlight the critical role of the gut microbiota in maintaining the metabolic integrity of the host, from energy harvest to metabolic activity. But energy intake is also balanced with energy expenditure, which segues to the topic of exercise and its impact on the microbiome.
Exercise and the Intestinal Microbiome
Exercise has received much praise for its ability to regulate weight, insulin sensitivity, metabolic activity and contribute to overall improvement in health. There is growing evidence to support the role of exercise in regulating human intestinal microbiota (63–73). Emerging research shows that exercise training independently altered the composition and function of the gut microbiota (74–78). Matsumoto et al. originally found that 5 weeks of exercise training in animals resulted in an increased production of the short chain fatty acid butyrate, a product of the bacterial fermentation of dietary fiber by bacteria such as Bifidobacteria (79). Matsumoto et al. also found that exercise training in mice increased the relative abundance of butyrate-producing taxa (75, 80). Butyrate is the primary fuel for colonocytes and has been shown to increase colonic epithelial cell proliferation, regulate host immune system and gene expression, and promote the integrity of the gut barrier (74, 81, 82). Conflicting evidence still exists for exercise and the intestinal microbiome; for example, some rodent studies found that exercise reduced the ratio of Firmicutes to Bacteroidetes (77, 80, 83, 84), while others found that exercise increased the ratio (75, 76, 85). These discrepancies may be influenced by the kind and degree of exercise (e.g., in mice, voluntary wheel running or forced treadmill running), the contingencies of the diet, age of the animal, species/strain, and method of research.
In professional rugby players, Clarke et al. found that the intestinal microbiota showed an increase in alpha diversity (variance within the sample), with a higher relative abundance of 40 different bacterial taxa compared to lean sedentary controls (63); these athletes had a lower abundance of lactobacillus and bacteroides species than the lean sedentary group (63). Bressa et al. found that women who performed at least 3 hours of exercise per week had a greater abundance of Faecalibacterium prausnizii, Roseburia hominis , and A. muciniphilia compared to sedentary controls (64). A. muciniphila has been associated with lower body mass index (BMI) (62) and improved metabolic health in other studies, whereas F. prausnitzii and R. hominis are known to be butyrate producers (86). Overall, there is strong indication that exercise can benefit the intestinal microbiome by improving microbial diversity and increasing butyrate production.
Brain-Gut-Microbiome Interactions
Communication between the gut microbiota and the brain is an important area of research. A vital bidirectional signaling system between the gastrointestinal tract and the brain helps maintain metabolic homeostasis and is regulated via neural (central and enteric nervous systems, CNS and ENS, respectively), immunological, and hormonal systems (87). The perturbation of these systems through external factors, such as diet or antimicrobial use, leads to alterations within stress-response mechanisms, behavior, and neurologic health (88, 89).
A well-documented, clinical association of an aberrant gut-brain axis is the manifestation of stress-related symptoms, such as anxiety or depression, which can lead to constipation or diarrhea and is sometimes diagnosed as irritable bowel syndrome (IBS) (90). In animal models, Neufield and colleagues illustrated that colonization of GF mice with specific pathogen-free microbiota decreased anxiety-like behavior in a well-validated maze model of anxiolytic action (91). The study also showed changes in the murine neurochemistry, with upregulated expression of brain-derived neurotrophic factor (BDNF) mRNA in the hippocampal dentate gyrus (91). BDNF expression is believed to be critical for supporting synaptic plasticity and neuronal differentiation and survival. Stressful exposures can reduce the expression of BDNF, thereby theoretically affecting cognitive and emotional health (92). Bistoletti and colleagues demonstrated the effect of broad-spectrum antibiotics in transiently decreasing BDNF levels and increasing anxiety behaviors in juvenile mice (93). Together, these studies provide important evidence that the brain and behavior, specifically anxiety, can be influenced by the microbiota through the gut-brain axis.
IBS pathophysiology is not fully understood, but for many patients, an element of visceral hyperalgesia is implicated and alterations in the bidirectional communication of the gut-brain axis may cause an exaggerated pain response to an otherwise normal digestive process (94). Labus and colleagues identified a correlation between brain architecture and the gut microbiota in a distinct subgroup of IBS patients, suggesting that gut microbiota and their metabolites may influence specific brain structures. The authors concluded that a microbe-gut-brain axis plays an important role in the pathophysiology of disrupted sensory processing in IBS (95).
Emerging evidence also suggests that gut microbiota play an important role in several neurological conditions, such as Parkinson’s disease (PD), Alzheimer’s disease, and multiple sclerosis (96). Several studies have observed that PD patients may have gastrointestinal disorders before displaying motor symptoms, and suggested that gut dysbiosis may be implicated, but the specific link is not clearly understood (96). Studies in rats have demonstrated that alpha-synuclein (α-syn), a protein found in neural tissue and implicated in PD, misfolds and forms clumps in neural tissue in response to gut dysbiosis (97–99). One plausible hypothesis is that the innervation of the GI tract is easily damaged (96, 97) and that ENS injury is caused by an unknown PD pathogen that may present as α-syn pathology. Several clinical studies revealed that PD patients displayed α-syn aggregates in the enteroendocrine system (96, 97) and that these aggregates are related to damage of enteric neurons and associated with GI tract dysfunction. This type of protein aggregate accumulation affects both the myenteric and submucosal plexuses of the gut in PD patients and is gradually distributed from the most distal point of the esophagus to the rectum (96). Moreover, gut dysbiosis is believed to result in upregulated inflammatory pathways that may trigger the initiation of synucleinopathy (100–102). If a dysfunctional gut contributes to PD, then there lies a strong possibility that the gut affects the brain in a host of ways, including neurological and psychiatric disease.
Modulation of the Microbiota by Diet
The Composition of the Intestinal Microbiome Revolves Heavily Around Diet
Dietary factors are often potent modulators of microbiota composition and function. Transient, diet-induced alterations occur independently of body weight and adiposity and are detectable in humans within 24 to 48 hours after dietary intake (103). A micronutrient-dense, high-fiber diet with sufficient water intake and high-quality protein, along with avoidance of common Western dietary components, such as saturated and trans-fat, simple sugar, refined flour, high-fructose corn syrup, and other processed foods, is believed to have a protective effect regarding intestinal dysbiosis (104).
Particularly important for the health of the microbiome are carbohydrates (CHO) that are indigestible yet metabolically available to microbes within the intestines. Termed “microbiota-accessible carbohydrates” (MACs) (105), these include fermentable fibers and non-digestible polysaccharides found in resistant starch foods, such as those originating from plants (106). Intestinal microbes contain several hundred-fold more CHO-degrading enzymes than what is produced by human enterocytes; this enables the microbes to digest MACs for their primary source of energy (46).
The importance of MACs on microbiota composition and function is documented in multiple studies. In one illustrative mouse experiment, a diet low in MACs resulted in a decrease in numerous taxa and a loss of diversity across several generations of offspring that were not recovered after reintroduction of MACs (105, 107). In humans, a low-MAC diet results in poor production of intestinal microbiota-generated SCFA, which are known to reduce inflammation through a variety of mechanisms (104). Decreased SCFA production and increased mucus foraging by the microbiota demonstrate consequences to low MAC intake (46). However, the intake of excessive calories to obtain an increase in MAC cannot be recommended due to the consequence of a caloric surplus (108). Instead, balancing caloric intake based on basal metabolic rate and total daily energy expenditure, alongside consumption of micro-nutrient dense, high-fiber, well-balanced foods, may be a better approach for optimizing gut microbial and human health (109).
A high-protein diet (HPD) is another approach for potentially negating the harmful effects of a Western diet (WD). In a study done by Wang and colleagues, rats fed a WD for 12 weeks showed an increase in body weight and fat mass. When the rats were switched to a HPD for 6 weeks, the rats had reduced fat mass without significant weight loss, a retention of muscle mass, normalized blood glucose levels, and decreased feeding after intraperitoneal injection of cholecystokinin (CCK) compared to rats with diet-induced obesity treated with CCK (110). The authors concluded that a HPD may be useful in promoting fat loss, restoring glucose homeostasis, and improving CCK sensitivity, as well as maintaining muscle mass during periods of caloric restriction. Furthermore, since the HPD-fed rats showed an enrichment of 114 operational taxonomic units (OTUs) and depletion of 188 OTUs, it was concluded that the microbiome was involved with the measured metabolic alterations. An example of the significant microbial difference is the positive association between A. muciniphila and Phascolarctobacterium with decreased fat mass in the HPD-fed rats compared to WD-fed rats (110). A. muciniphila was identified to correlate with fat loss and may represent a secondary mechanism for the beneficial effects of HPD (110). Furthermore, the study showed that WD-fed rats had increased cytokine expression in the hypothalamus and dorsal medulla, which was unchanged after switching to HPD (110).
Kaptan and colleagues found consumption of a low-calorie diet by adolescent rats led to an increase in microbial diversity, adult neurogenesis, BDNF levels, and improved cognition (111). Conversely, mice fed a HFD exhibited gut dysbiosis, decreased synaptic plasticity, and increased anxiety-like behaviors (112–114).
Overall, diet has an important effect on the microbiome and its ability to communicate amongst different systems in the body. The studies noted above on MACs, WD, HPD, low-calorie diets, and HFD, and their effects on the microbiome, highlight the importance of maintaining a healthy gut microbiome through various dietary interventions.
Metabolic Health Impact of Various Diets on the Microbiome
Many diets emphasize the utility of a specific macronutrient (e.g., high-protein or low-fat) or the avoidance of a specific ingredient (e.g., dairy- or gluten-free). Several well-known diets have been studied for their ability to modulate intestinal microbiota, including WD (high animal fat/protein) (115–117), Mediterranean (MD) (high-fiber, high-monounsaturated fat, antioxidant-rich, and low in red meat) (118–120), vegetarian, vegan, and gluten-free (121–125).
The WD, which is high in animal protein and saturated fat and low in fiber, is usually low in MACs and has been shown to lead to a reduction in microbial diversity and altered functionality of the intestinal microbiota compared to control diets. Many studies document that a WD caused decreased diversity of Bifidobacterium and Eubacterium species, as well as increased Enterobacteria and Bacteroides (115–117). One mechanism by which gut microbes mediate the negative metabolic consequences of a HFD is through translocation of lipopolysaccharide (LPS), also known as endotoxin, a cell-wall component of Gram-negative bacteria. Increases in circulating LPS can occur after a high-fat meal, with exacerbated effects in individuals with obesity (126). Once in circulation, LPS elicits a potent inflammatory response via Toll-like receptor-4 (TLR-4) signaling, which has been implicated in the development of cardiovascular and metabolic disease (45, 127). Other functional differences include the association between the WD and an increase in the production of cancer-promoting nitrosamines (128, 129); this is likely related to the high quantity and poor quality of animal protein in the WD, especially processed meat.
The MD, largely acknowledged as a healthier diet than the WD, is characterized by intake of a beneficial fatty acid profile rich in mono- and polyunsaturated fatty acids, nondigestible fibrous plant sources and other low glycemic carbohydrates, and high levels of polyphenols, along with other antioxidants and micronutrients (119). Several studies have identified that a typical MD carries a lower risk of obesity, results in a better lipid profile, and lowers inflammation. From a microbial perspective, these characteristics were associated with increases in Prevotella, Lactobacillus, and Bifidobacterium, and decreases in Clostridium (130–135).
Diets enriched in fiber and fermentable, plant-based foods include vegan and vegetarian diets. These two diets were shown to promote significantly lower counts of Bacteroides and Bifidobacterium species (p < 0.001), compared to an unrestricted control diet (136). One study determined that differences in the intestinal microbiomes of subjects consuming an omnivorous diet versus subjects consuming a vegan or vegetarian diet showed significantly lower stool pH than controls (137). This is likely due to the formation of SCFA, like butyric acid, as well as lactic acid from Lactobacillus bacteria. A lower stool pH is believed to confer an element of colonization resistance against pathogens.
A fairly new diet that was initially recommended for those with celiac disease (CD) but has now gained popularity by the general population is the gluten-free diet (GFD). In patients with CD, GFD is intended to reduce the effects of an autoimmune response against deamidated gliadin (a component of gluten). However, in one study, Sanz et al. enrolled 10 healthy subjects to consume a GFD for 30 days and noted an associated decrease in beneficial populations of bacteria (Bifidobacterium and Lactobacillus), while potentially increasing unhealthy populations of bacteria; this was hypothesized to be caused by a reduced polysaccharide intake associated by GFD (121). In addition, the total number of Enterobacteriaceae and E. coli increased, theoretically increasing the risk for opportunistic pathogens (121). A different study on the effects of short-term GFD showed increases in Clostridiaceae and Victivallaceae, and reductions in Ruminococcus bromii, Veillonellaceae and Roseburia faecis (122). Veillonellaceae is considered to be a pro-inflammatory family of bacteria. The clinical consequence of GFD in non-celiac individuals is largely unknown and therefore GFD cannot be recommended for the general population based on the available data.
Intermittent fasting, another recently popular diet, led to changes in the microbiome as well as improvement in metabolic parameters (138). Eight weeks of intermittent fasting revealed that the community structure of the intestinal microbiota was not significantly changed overall, but there were changes in the abundance of Ruminococcaceae at the family level and Roseburia at the genus level. This was accompanied by an increased production of SCFA, decreased circulating levels of lipopolysaccharide (LPS) and inflammatory cytokines, ameliorated markers of oxidative stress, improved vasodilatory parameters, and reduced subject body fat mass (138). There is great need for further research on the health benefits of fasting and the role it plays in autophagy and cellular regeneration, especially in the liver.
Effect of Nicotine on Microbiome and Interactions With Diet
Smoking cigarettes has an impact on gut health, including changes in the microbiome that can affect overall health. Nicotine, the psychoactive component of tobacco, binds to nicotinic acetylcholine receptors (nAChR), such as the α4/β2 receptor, and low-affinity receptors, such as α7 in the CNS and peripheral tissues (139, 140). Nicotine, when given with a HFD, leads to hepatic and muscle steatosis that is thought to be due, at least in part, to increased abdominal fat lipolysis (141–143). In an animal study, we found that the α7nAChR agonist PNU-282987 protects against nicotine and HFD–induced hepatic steatosis in genetically obese mice (144). In this mouse model, smoke-exposed mice showed an alteration in colonic bacterial activity and community structure, with an increase of Lachnospiraceae sp (145).
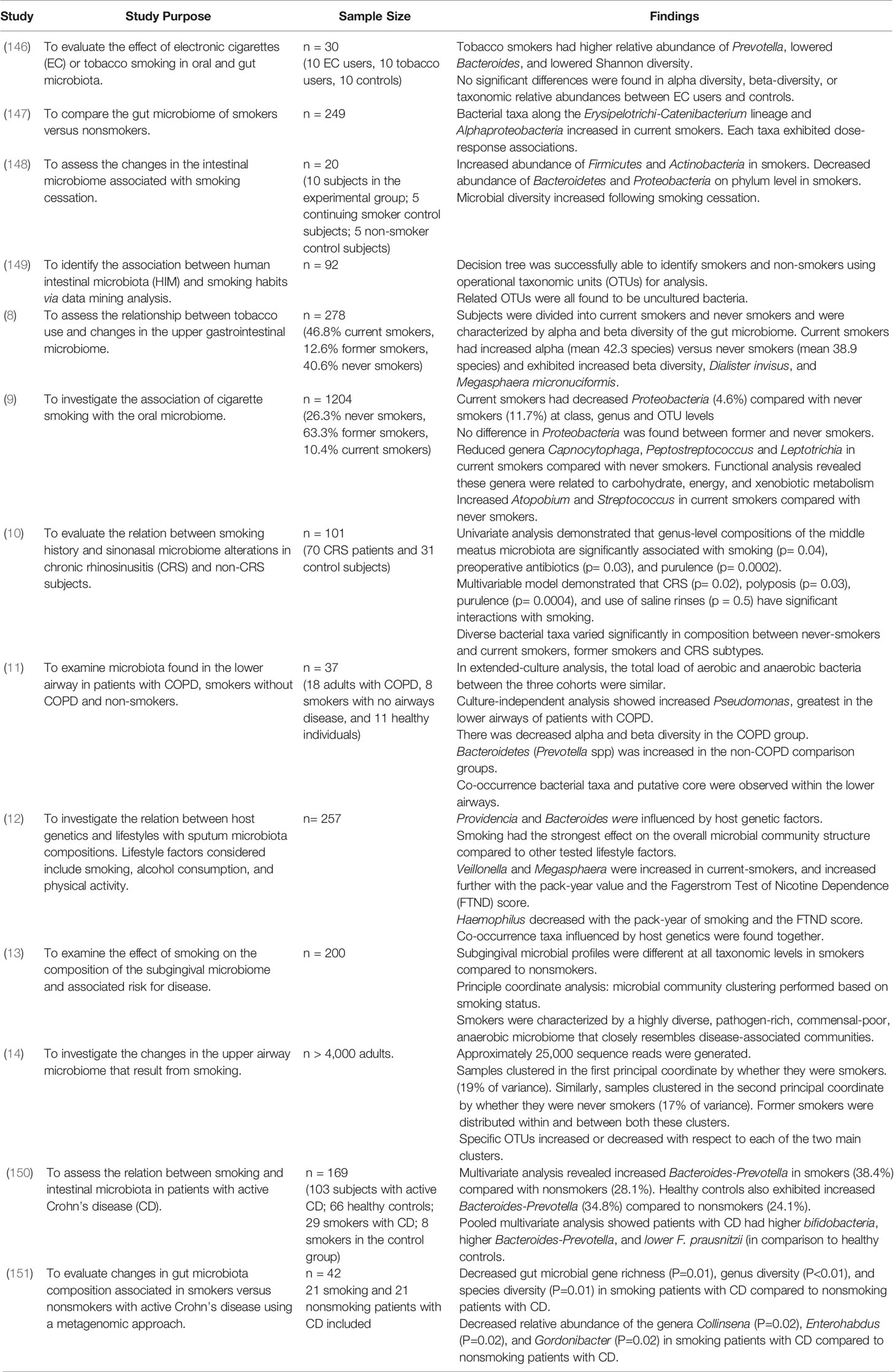
In human microbiome studies, tobacco smokers displayed a higher relative abundance of Prevotella, lower relative abundance of Bacteroides, and a lower Shannon diversity (a measurement of diversity) compared to controls (146). Biedermann and colleagues described a decrease of Bacteroides as well as alterations in the abundance of Alphaproteobacteria and Betaproteobacteria following the cessation of smoking (147). Indeed, smoking cessation induced profound changes in the gut microbiome, with an increase of Firmicutes and Actinobacteria and a decrease of Bacteroidetes and Proteobacteria at the phylum level; smoking cessation also induced an increase in microbial diversity (148). Importantly, the intestinal microbial composition of smokers and non-smokers were different when fed identical meals to avoid the influences of dietary factors (149). Other human studies have confirmed that smoking is associated with variances not only in the intestinal microbiome, but also the upper gastrointestinal tract (8), saliva (9), middle meatus (10), bronchial wash (11), sputum (12), subgingival (13), and throat (14).
Several studies investigated the intestinal microbiomes of smokers vs. non-smokers, but these involved mostly Crohn’s disease patients or had a small sample size (148, 150, 151). Nolan-Kenney and colleagues compared the composition of intestinal microbiomes in smokers vs. non-smokers by collecting stool samples in a cross-sectional study of 249 participants selected from the Health Effects of Arsenic Longitudinal Study (HEALS) in Bangladesh (147). They examined the associations between the status and the intensity of smoking with the relative abundance and presence of individual bacterial taxon, from phylum to genus (147). In current/active smokers, they found that the relative abundance of bacterial taxa among the Eryispelotrichi-to-Catenibacterium lineage was significantly higher compared to non-smokers (147). They calculated a 1.91 odds ratio (OR) (95% confidence interval [CI] = 1.36 to 2.69) for the genus Catenibacterium when comparing the mean relative abundance in current smokers with that in subjects who never smoked, and a 1.89 OR (95% CI = 1.39 to 2.56) for the family Erysipelotrichaceae, order Erysipelotrichale, and class Erysipelotrichi (false discovery rate-adjusted p-values=0.0008 to 0.01) (147). Moreover, for each of these bacterial taxa, a nicotine/smoking dose-response association was observed, with increasing mean relative abundance of specific taxa as packs per day of cigarettes increased. In addition, the presence of Alphaproteobacteria was significantly greater (OR = 4.85, false discovery rate-adjusted p-values = 0.04) in current smokers vs. non-smokers (147). The data are consistent with other studies that associate smoking and its intensity with a change in the intestinal microbial composition (Table 1), suggesting that cigarette smoking plays a significant role in gut dysbiosis, especially as the level of tobacco exposure increases.
Electronic Cigarettes (E-Cigarettes) and Public Health
E-cigarette use is a public health crisis that is sweeping the United States; this epidemic involves not only adults, but also teens. E-cigarettes came to the markets in the mid-2000s and were advertised as ‘safer’ alternatives to conventional cigarettes and an effective way to stop smoking (152). However, e-cigarettes are much less regulated than traditional cigarettes, leading to extremely variable nicotine levels, with some reaching levels above combustible cigarettes (153). Many studies have shown detrimental effects of e-cigarette use including on the liver, heart and lung (144, 145, 154–161). In a mouse model, we have found that e-cigarette use is linked to cardiovascular and hepatic diseases (144, 155, 159). Our laboratory is studying the effects of e-cigarettes on mouse microbiota and we will be reporting our results in the near future.
The study by Stewart and colleagues (146) also found that tobacco smoking had a significant effect on the bacterial profiles when compared to e-cigarette users. The most significant associations were an increased relative abundance of Prevotella (P=0.006) and decreased Bacteroides (P =0.036) in the stool of tobacco smokers versus e-cigarette users. In contrast, no significant difference was found in the alpha diversity, beta-diversity (variability in community composition) or taxonomic relative abundances between e-cigarette users and controls. Therefore, the authors concluded that the use of e-cigarette users may represent a safer alternative compared to tobacco smoking but caution that their study was only done in a small cohort of smokers and e-cigarette users. Stewart and colleagues proposed a larger, multi-location cohort study with e-cigarettes and conventional cigarette users to provide insight into their effects on the microbiome.
Nicotine Interaction with Diet in NAFLD and Obesity
NAFLD poses a significant health risk, affecting 20 to 40% of adults in the general American population and over 70% of individuals with obesity (44). Alongside obesity, nicotine is acknowledged as a risk factor for NAFLD (162, 163). There are at least three mechanisms by which smoking and/or nicotine appear to have adverse effects on the liver: toxic, immunologic, and oncogenic (164). The toxic effects include oxidative stress, which results in the activation of stellate cells, leading to fibrosis; an increase in proinflammatory cytokines (e.g., IL-1, IL-6, IL-8, TNF alpha) is a direct contributor to liver cell injury. The immunologic effects of smoking are both cell-mediated (e.g., apoptosis of lymphocytes, impaired natural killer cell activity) and humoral (i.e., suppression of antibody formation). The oncogenic effects of smoking include carcinogens found in cigarettes, such as hydrocarbons, nitrosamines, tar, and vinyl chloride that can lead to NAFLD. Tobacco consumption has also been implicated in the reduction of p53, a tumor-suppressing gene, which may be a common pathway of oncogenesis for many neoplasms (164).
In addition to the three mechanisms noted above, nicotine also appears to exacerbate obesity-induced hepatic steatosis (44) via gut dysbiosis and its influence on the pathogenesis of NAFLD (44, 165–167). When nicotine is combined with a HFD in mice, there is a significant increase in the levels of serum and hepatic triglyceride, as well as circulating free fatty acids (141, 143, 161). In mice, nicotine exacerbates hepatic steatosis through increased hepatocellular apoptosis and oxidative stress, as well as decreased phosphorylation (i.e., inactivation) of adenosine-5-monophosphate-activated protein kinase. This, in turn, results in the up-regulation of sterol response element-binding protein 1-c, fatty acid synthase, and activation of acetyl-coenzyme A-carboxylase, which yields further hepatic lipogenesis (44). Nicotine also increases endoplasmic reticulum (ER) stress (44) that modulates many factors, including nuclear factor 2 erythroid-related factor 2 (Nrf2), c-Jun N-terminal kinase (JNK), nuclear factor κB (NF-κB), and c/EBP homologous protein. These all contribute to the inflammatory process associated with smoking and are part of the cellular defense against oxidative stress, often resulting in cell death (44). For instance, Nrf2 serves as a master regulator of a cellular defense system against oxidative stress (168, 169) and JNK is activated in several animal models of obesity and also in patients with NASH. The activation of JNK has been demonstrated in HFD-induced hepatic steatosis in apoplipoprotein-E knockout mice (170) and nicotine plus HFD-induced hepatic steatosis in obese mice (141); the genetic deletion of JNK in animal models resulted in attenuation of fatty liver (171). NF-κB is an important transcription factor and primary regulator of inflammatory pathways. Consistent activation of NF-κB signaling has been documented in animal models of NAFLD as well as in patients with NASH (172). Thus, the data suggest that the use of nicotine-based products results in increased oxidative stress, upregulated inflammation, perturbed hepatic lipid homeostasis, apoptosis, and autophagy, which contribute to hepatic steatosis and progression to NASH (173).
Lastly, nicotine may contribute to increased gut permeability and has been implicated in poor outcomes in IBD patients (174). Miele and colleagues showed that patients with biopsy-proven NAFLD also experienced significantly greater gut permeability due to the disruption of intercellular tight junctions in the intestine compared to healthy volunteers (175). Both increased gut permeability and the prevalence of small intestinal bacterial overgrowth (SIBO), which is correlated with the severity of steatosis in NAFLD patients (175). Since smoking appears to induce profound changes in the intestinal microbiota (148, 176), we hypothesize that nicotine with HFD could compound and lead to increased intestinal permeability, LPS activation of TLRs and the inflammasome (167), induce changes in SCFAs metabolism (167), decreased choline availability, and increased trimethylamine production (167), all of which could contribute to a nicotine-derived pathway and result in the pathogenesis of NAFLD.
Conclusion and Perspective
A healthy intestinal microbiome is dependent on a delicate balance of various microorganisms that is susceptible to external lifestyle factors, including unhealthy diet, lack of exercise, smoking and nicotine-exposure. Lifestyle modification can alter the variable portion of the microbiome. Exercise may hold numerous potential benefits for the health of the intestinal microbiome, not only through improved insulin sensitivity, weight loss, and improved cardiovascular health, but also through its impacts on the intestinal microbiota composition. Use of nicotine-based products (e-cigarettes and traditional cigarettes) leads to known health consequences, but also may be a major contributor to gut dysbiosis and increased gut permeability. More research is needed to confirm the importance of avoiding nicotine-based products to optimize gut health and lessen the risk of gut dysbiosis. Additionally, the effects of nicotine use on the gut immune system should be more closely evaluated. Moving forward, the ability of the microbiome to recover from external factors, such as nicotine and unhealthy diets, should also be evaluated. With the number of young adults and teens consuming nicotine via e-cigarettes on the rise, the long-term effect of nicotine has become more relevant. Effects of nicotine, either alone or in combination with the WD, on the intestinal microbiome remain to be elucidated.
Author Contributions
JM and SG performed the literature review. JM wrote the first draft of the paper. All other authors contributed to the writing and editing of the paper. All authors contributed to the article and approved the submitted version.
Funding
Funded by NIH grants MD012579-01, R25 DA050723, U54 MD007598, DOD CDMRP grant PR190942, VA CDA2 IK2CX001717, and California Tobacco-Related Disease Research Program (TRDRP) Community Practice-Based Research Implementation Award 28CP-0040.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Editorial review was provided by the NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
References
1. Cotillard A, Kennedy SP, Kong LC, Prifti E, Pons N, Le Chatelier E, et al. Dietary Intervention Impact on Gut Microbial Gene Richness. Nature (2013) 500:585–8. doi: 10.1038/nature12480
3. Toor D, Wsson MK, Kumar P, Karthikeyan G, Kaushik NK, Goel C, et al. Dysbiosis Disrupts Gut Immune Homeostasis and Promotes Gastric Diseases. Int J Mol Sci (2019) 20:2432. doi: 10.3390/ijms20102432
4. Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert Consensus Document. The International Scientific Association for Probiotics and Prebiotics Consensus Statement on the Scope and Appropriate Use of the Term Probiotic. Nat Rev Gastroenterol Hepatol (2014) 11:506–14. doi: 10.1038/nrgastro.2014.66
5. (2020). Available at: https://www.daytwo.com (Accessed December 24).
6. Marchesi JR, Ravel J. The Vocabulary of Microbiome Research: A Proposal. Microbiome (2015) 3:31. doi: 10.1186/s40168-015-0094-5
7. Clemente JC, Manasson J, Scher JU. The Role of the Gut Microbiome in Systemic Inflammatory Disease. BMJ (2018) 360:j5145. doi: 10.1136/bmj.j5145
8. Vogtmann E, Flores R, Yu G, Freedman ND, Shi J, Gail MH, et al. Association Between Tobacco Use and the Upper Gastrointestinal Microbiome Among Chinese Men. Cancer Causes Control (2015) 26:581–8. doi: 10.1007/s10552-015-0535-2
9. Wu J, Peters BA, Dominianni C, Zhang Y, Pei Z, Yang L, et al. Cigarette Smoking and the Oral Microbiome in a Large Study of American Adults. Isme J (2016) 10:2435–46. doi: 10.1038/ismej.2016.37
10. Ramakrishnan VR, Frank DN. Impact of Cigarette Smoking on the Middle Meatus Microbiome in Health and Chronic Rhinosinusitis. Int Forum Allergy Rhinol (2015) 5:981–9. doi: 10.1002/alr.21626
11. Einarsson GG, Comer DM, McIlreavey L, Parkhill J, Ennis M, Tunney MM, et al. Community Dynamics and the Lower Airway Microbiota in Stable Chronic Obstructive Pulmonary Disease, Smokers and Healthy non-Smokers. Thorax (2016) 71:795–803. doi: 10.1136/thoraxjnl-2015-207235
12. Lim MY, Yoon HS, Rho M, Sung J, Song YM, Lee K, et al. Analysis of the Association Between Host Genetics, Smoking, and Sputum Microbiota in Healthy Humans. Sci Rep (2016) 6:23745. doi: 10.1038/srep23745
13. Mason MR, Preshaw PM, Nagaraja HN, Dabdoub SM, Rahman A, Kumar PS. The Subgingival Microbiome of Clinically Healthy Current and Never Smokers. Isme J (2015) 9:268–72. doi: 10.1038/ismej.2014.114
14. Cox MJ, Hunter M, Musk AW, Cookson WO, James A, Moffatt MF. The Upper Airway Microbiome of Smokers, Ex-Smokers And Never-Smokers In Busselton, Western Australia, A52. Smoking Lung Dis (2011) pp:A6358–8. doi: 10.1164/ajrccm-conference.2011.183.1_MeetingAbstracts.A6358
15. Koh A, De Vadder F, Kovatcheva-Datchary P, Backhed F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell (2016) 165:1332–45. doi: 10.1016/j.cell.2016.05.041
16. Laukens D, Brinkman BM, Raes J, De Vos M, Vandenabeele P. Heterogeneity of the Gut Microbiome in Mice: Guidelines for Optimizing Experimental Design. FEMS Microbiol Rev (2016) 40:117–32. doi: 10.1093/femsre/fuv036
17. Thaiss CA, Levy M, Korem T, Dohnalova L, Shapiro H, Jaitin DA, et al. Microbiota Diurnal Rhythmicity Programs Host Transcriptome Oscillations. Cell (2016) 167:1495–510. doi: 10.1016/j.cell.2016.11.003
18. Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of Diet on the Gut Microbiome and Implications for Human Health. J Transl Med (2017) 15:73. doi: 10.1186/s12967-017-1175-y
19. Berer K, Krishnamoorthy G. Microbial View of Central Nervous System Autoimmunity. FEBS Lett (2014) 588:4207–13. doi: 10.1016/j.febslet.2014.04.007
20. Frick JS, Autenrieth IB. The Gut Microflora and its Variety of Roles in Health and Disease. Curr Top Microbiol Immunol (2013) 358:273–89. doi: 10.1007/82_2012_217
21. Ahmed I, Roy BC, Khan SA, Septer S, Umar S. Microbiome, Metabolome and Inflammatory Bowel Disease. Microorganisms (2016) 4. doi: 10.3390/microorganisms4020020
22. Gensollen T, Iyer SS, Kasper DL, Blumberg RS. How Colonization by Microbiota in Early Life Shapes the Immune System. Science (2016) 352:539–44. doi: 10.1126/science.aad9378
23. Umesaki Y, Setoyama H, Matsumoto S, Okada Y. Expansion of Alpha Beta T-cell Receptor-Bearing Intestinal Intraepithelial Lymphocytes After Microbial Colonization in Germ-Free Mice and its Independence From Thymus. Immunology (1993) 79:32–7.
24. Atarashi K, Tanoue T, Ando M, Kamada N, Nagano Y, Narushima S, et al. Th17 Cell Induction by Adhesion of Microbes to Intestinal Epithelial Cells. Cell (2015) 163:367–80. doi: 10.1016/j.cell.2015.08.058
25. Ivanov II, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, et al. Induction of Intestinal Th17 Cells by Segmented Filamentous Bacteria. Cell (2009) 139:485–98. doi: 10.1016/j.cell.2009.09.033
26. Schicho R, Marsche G, Storr M. Cardiovascular Complications in Inflammatory Bowel Disease. Curr Drug Targets (2015) 16:181–8. doi: 10.2174/1389450116666150202161500
27. Jacobs JP, Braun J. Immune and Genetic Gardening of the Intestinal Microbiome. FEBS Lett (2014) 588:4102–11. doi: 10.1016/j.febslet.2014.02.052
28. Delcenserie V, Martel D, Lamoureux M, Amiot J, Boutin Y, Roy D. Immunomodulatory Effects of Probiotics in the Intestinal Tract. Curr Issues Mol Biol (2008) 10:37–54.
29. Kwon HK, Lee CG, So JS, Chae CS, Hwang JS, Sahoo A, et al. Generation of Regulatory Dendritic Cells and CD4+Foxp3+ T Cells by Probiotics Administration Suppresses Immune Disorders. Proc Natl Acad Sci USA (2010) 107:2159–64. doi: 10.1073/pnas.0904055107
30. Andrade ME, Araújo RS, de Barros PA, Soares AD, Abrantes FA, Generoso Sde V, et al. The Role of Immunomodulators on Intestinal Barrier Homeostasis in Experimental Models. Clin Nutr (2015) 34:1080–7. doi: 10.1016/j.clnu.2015.01.012
31. Tilg H, Moschen AR. Food, Immunity, and the Microbiome. Gastroenterology (2015) 148:1107–19. doi: 10.1053/j.gastro.2014.12.036
32. Bergot AS, Giri R, Thomas R. The Microbiome and Rheumatoid Arthritis. Best Pract Res Clin Rheumatol (2020) 101497. doi: 10.1016/j.berh.2020.101497
33. Han H, Li Y, Fang J, Liu G, Yin J, Li T, et al. Gut Microbiota and Type 1 Diabetes. Int J Mol Sci (2018) 19. doi: 10.3390/ijms19040995
34. Mirza A, Mao-Draayer Y. The Gut Microbiome and Microbial Translocation in Multiple Sclerosis. Clin Immunol (2017) 183:213–24. doi: 10.1016/j.clim.2017.03.001
35. Katz-Agranov N, Zandman-Goddard G. The Microbiome and Systemic Lupus Erythematosus. Immunol Res (2017) 65:432–7. doi: 10.1007/s12026-017-8906-2
36. Ng SC, Bernstein CN, Vatn MH, Lakatos PL, Loftus EV Jr., Tysk C, et al. Geographical Variability and Environmental Risk Factors in Inflammatory Bowel Disease. Gut (2013) 62:630–49. doi: 10.1136/gutjnl-2012-303661
37. McGovern DP, Kugathasan S, Cho JH. Genetics of Inflammatory Bowel Diseases. Gastroenterology (2015) 149:1163–76. doi: 10.1053/j.gastro.2015.08.001
38. Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-Phylogenetic Characterization of Microbial Community Imbalances in Human Inflammatory Bowel Diseases. Proc Natl Acad Sci USA (2007) 104:13780–5. doi: 10.1073/pnas.0706625104
39. Willing BP, Dicksved J, Halfvarson J, Andersson AF, Lucio M, Zheng Z, et al. A Pyrosequencing Study in Twins Shows That Gastrointestinal Microbial Profiles Vary With Inflammatory Bowel Disease Phenotypes. Gastroenterology (2010) 139:1844–54. doi: 10.1053/j.gastro.2010.08.049
40. Morgan XC, Tickle TL, Sokol H, Gevers D, Devaney KL, Ward DV, et al. Dysfunction of the Intestinal Microbiome in Inflammatory Bowel Disease and Treatment. Genome Biol (2012) 13:R79. doi: 10.1186/gb-2012-13-9-r79
41. Gevers D, Kugathasan S, Denson LA, Vazquez-Baeza Y, Van Treuren W, Ren B, et al. The Treatment-Naive Microbiome in New-Onset Crohn’s Disease. Cell Host Microbe (2014) 15:382–92. doi: 10.1016/j.chom.2014.02.005
42. Lewis JD, Chen EZ, Baldassano RN, Otley AR, Griffiths AM, Lee D, et al. Inflammation, Antibiotics, and Diet as Environmental Stressors of the Gut Microbiome in Pediatric Crohn’s Disease. Cell Host Microbe (2015) 18:489–500. doi: 10.1016/j.chom.2015.09.008
43. Jacobs JP, Goudarzi M, Singh N, Tong M, McHardy IH, Ruegger P, et al. A Disease-Associated Microbial and Metabolomics State in Relatives of Pediatric Inflammatory Bowel Disease Patients. Cell Mol Gastroenterol Hepatol (2016) 2:750–66. doi: 10.1016/j.jcmgh.2016.06.004
44. Sinha-Hikim AP, Sinha-Hikim I, Friedman TC. Connection of Nicotine to Diet-Induced Obesity and Non-Alcoholic Fatty Liver Disease: Cellular and Mechanistic Insights. Front Endocrinol (Lausanne) (2017) 8:23. doi: 10.3389/fendo.2017.00023
45. Apovian CM. Obesity: Definition, Comorbidities, Causes, and Burden. Am J Manag Care (2016) 22:s176–85.
46. Gentile CL, Weir TL. The Gut Microbiota at the Intersection of Diet and Human Health. Science (2018) 362:776–80. doi: 10.1126/science.aau5812
47. Gerard P. Gut Microbiome and Obesity. How to Prove Causality? Ann Am Thorac Soc (2017) 14:S354–s356. doi: 10.1513/AnnalsATS.201702-117AW
48. Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity Alters Gut Microbial Ecology. Proc Natl Acad Sci USA (2005) 102:11070–5. doi: 10.1073/pnas.0504978102
49. Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An Obesity-Associated Gut Microbiome With Increased Capacity for Energy Harvest. Nature (2006) 444:1027–31. doi: 10.1038/nature05414
50. Waldram A, Holmes E, Wang Y, Rantalainen M, Wilson ID, Tuohy KM, et al. Top-Down Systems Biology Modeling of Host Metabotype-Microbiome Associations in Obese Rodents. J Proteome Res (2009) 8:2361–75. doi: 10.1021/pr8009885
51. Palmnas M, Brunius C, Shi L, Rostgaard-Hansen A, Torres NE, Gonzalez-Dominguez R, et al. Perspective: Metabotyping-A Potential Personalized Nutrition Strategy for Precision Prevention of Cardiometabolic Disease. Adv Nutr (2019) 11:524–32. doi: 10.1093/advances/nmz121
52. Turnbaugh PJ, Gordon JI. The Core Gut Microbiome, Energy Balance and Obesity. J Physiol (2009) 587:4153–8. doi: 10.1113/jphysiol.2009.174136
53. Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial Ecology: Human Gut Microbes Associated With Obesity. Nature (2006) 444:1022–3. doi: 10.1038/4441022a
54. Karlsson F, Tremaroli V, Nielsen J, Bäckhed F. Assessing the Human Gut Microbiota in Metabolic Diseases. Diabetes (2013) 62:3341–9. doi: 10.2337/db13-0844
55. Magne F, Gotteland M, Gauthier L, Zazueta A, Pesoa S, Navarrete P, et al. The Firmicutes/Bacteroidetes Ratio: A Relevant Marker of Gut Dysbiosis in Obese Patients? Nutrients (2020) 12. doi: 10.3390/nu12051474
56. Abenavoli L, Scarpellini E, Colica C, Boccuto L, Salehi B, Sharifi-Rad J, et al. Gut Microbiota and Obesity: A Role for Probiotics. Nutrients (2019) 11. doi: 10.3390/nu11112690
57. Kumar H, Lund R, Laiho A, Lundelin K, Ley RE, Isolauri E, et al. Gut Microbiota as an Epigenetic Regulator: Pilot Study Based on Whole-Genome Methylation Analysis. mBio (2014) 5. doi: 10.1128/mBio.02113-14
58. Aller R, De Luis DA, Izaola O, Conde R, Gonzalez Sagrado M, Primo D, et al. Effect of a Probiotic on Liver Aminotransferases in Nonalcoholic Fatty Liver Disease Patients: A Double Blind Randomized Clinical Trial. Eur Rev Med Pharmacol Sci (2011) 15:1090–5.
59. Nardone G, Compare D, Liguori E, Di Mauro V, Rocco A, Barone M, et al. Protective Effects of Lactobacillus Paracasei F19 in a Rat Model of Oxidative and Metabolic Hepatic Injury. Am J Physiol Gastrointest Liver Physiol (2010) 299:G669–76. doi: 10.1152/ajpgi.00188.2010
60. Safari Z, Gerard P. The Links Between the Gut Microbiome and non-Alcoholic Fatty Liver Disease (NAFLD). Cell Mol Life Sci (2019) 76:1541–58. doi: 10.1007/s00018-019-03011-w
61. Compare D, Coccoli P, Rocco A, Nardone OM, De Maria S, Cartenì M, et al. Gut–Liver Axis: The Impact of Gut Microbiota on non Alcoholic Fatty Liver Disease. Nutr Metab Cardiovasc Dis (2012) 22:471–6. doi: 10.1016/j.numecd.2012.02.007
62. Dao MC, Everard A, Aron-Wisnewsky J, Sokolovska N, Prifti E, Verger EO, et al. Akkermansia Muciniphila and Improved Metabolic Health During a Dietary Intervention in Obesity: Relationship With Gut Microbiome Richness and Ecology. Gut (2016) 65:426–36. doi: 10.1136/gutjnl-2014-308778
63. Clarke SF, Murphy EF, O’Sullivan O, Lucey AJ, Humphreys M, Hogan A, et al. Exercise and Associated Dietary Extremes Impact on Gut Microbial Diversity. Gut (2014) 63:1913–20. doi: 10.1136/gutjnl-2013-306541
64. Bressa C, Bailén-Andrino M, Pérez-Santiago J, González-Soltero R, Pérez M, Montalvo-Lominchar MG, et al. Differences in Gut Microbiota Profile Between Women With Active Lifestyle and Sedentary Women. PloS One (2017) 12:e0171352. doi: 10.1371/journal.pone.0171352
65. Durk RP, Castillo E, Márquez-Magaña L, Grosicki GJ, Bolter ND, Lee CM, et al. Gut Microbiota Composition Is Related to Cardiorespiratory Fitness in Healthy Young Adults. Int J Sport Nutr Exerc Metab (2019) 29:249–53. doi: 10.1123/ijsnem.2018-0024
66. Estaki M, Pither J, Baumeister P, Little JP, Gill SK, Ghosh S, et al. Cardiorespiratory Fitness as a Predictor of Intestinal Microbial Diversity and Distinct Metagenomic Functions. Microbiome (2016) 4:42. doi: 10.1186/s40168-016-0189-7
67. Barton W, Penney NC, Cronin O, Garcia-Perez I, Molloy MG, Holmes E, et al. The Microbiome of Professional Athletes Differs From That of More Sedentary Subjects in Composition and Particularly at the Functional Metabolic Level. Gut (2018) 67:625–33. doi: 10.1136/gutjnl-2016-313627
68. Allen JM, Mailing LJ, Niemiro GM, Moore R, Cook MD, White BA, et al. Exercise Alters Gut Microbiota Composition and Function in Lean and Obese Humans. Med Sci Sports Exerc (2018) 50:747–57. doi: 10.1249/mss.0000000000001495
69. Cronin O, Barton W, Skuse P, Penney NC, Garcia-Perez I, Murphy EF, et al. A Prospective Metagenomic and Metabolomic Analysis of the Impact of Exercise and/or Whey Protein Supplementation on the Gut Microbiome of Sedentary Adults. mSystems (2018) 3. doi: 10.1128/mSystems.00044-18
70. Munukka E, Ahtiainen JP, Puigbó P, Jalkanen S, Pahkala K, Keskitalo A, et al. Six-Week Endurance Exercise Alters Gut Metagenome That Is Not Reflected in Systemic Metabolism in Over-weight Women. Front Microbiol (2018) 9:2323. doi: 10.3389/fmicb.2018.02323
71. Stewart CJ, Nelson A, Campbell MD, Walker M, Stevenson EJ, Shaw JA, et al. Gut Microbiota of Type 1 Diabetes Patients With Good Glycaemic Control and High Physical Fitness is Similar to People Without Diabetes: An Observational Study. Diabetes Med (2017) 34:127–34. doi: 10.1111/dme.13140
72. Yang Y, Shi Y, Wiklund P, Tan X, Wu N, Zhang X, et al. The Association Between Cardiorespiratory Fitness and Gut Microbiota Composition in Premenopausal Women. Nutrients (2017) 9. doi: 10.3390/nu9080792
73. Paulsen JA, Ptacek TS, Carter SJ, Liu N, Kumar R, Hyndman L, et al. Gut Microbiota Composition Associated With Alterations in Cardiorespiratory Fitness and Psychosocial Outcomes Among Breast Cancer Survivors. Support Care Cancer (2017) 25:1563–70. doi: 10.1007/s00520-016-3568-5
74. Mailing LJ, Allen JM, Buford TW, Fields CJ, Woods JA. Exercise and the Gut Microbiome: A Review of the Evidence, Potential Mechanisms, and Implications for Human Health. Exerc Sport Sci Rev (2019) 47:75–85. doi: 10.1249/jes.0000000000000183
75. Kang SS, Jeraldo PR, Kurti A, Miller ME, Cook MD, Whitlock K, et al. Diet and Exercise Orthogonally Alter the Gut Microbiome and Reveal Independent Associations With Anxiety and Cognition. Mol Neurodegener (2014) 9:36. doi: 10.1186/1750-1326-9-36
76. Petriz BA, Castro AP, Almeida JA, Gomes CP, Fernandes GR, Kruger RH, et al. Exercise Induction of Gut Microbiota Modifications in Obese, non-Obese and Hypertensive Rats. BMC Genomics (2014) 15:511. doi: 10.1186/1471-2164-15-511
77. Denou E, Marcinko K, Surette MG, Steinberg GR, Schertzer JD. High-Intensity Exercise Training Increases the Diversity and Metabolic Capacity of the Mouse Distal Gut Microbiota During Diet-Induced Obesity. Am J Physiol Endocrinol Metab (2016) 310:E982–93. doi: 10.1152/ajpendo.00537.2015
78. Campbell SC, Wisniewski PJ, Noji M, McGuinness LR, Häggblom MM, Lightfoot SA, et al. The Effect of Diet and Exercise on Intestinal Integrity and Microbial Diversity in Mice. PloS One (2016) 11:e0150502. doi: 10.1371/journal.pone.0150502
79. Matsumoto M, Inoue R, Tsukahara T, Ushida K, Chiji H, Matsubara N, et al. Voluntary Running Exercise Alters Microbiota Composition and Increases N-Butyrate Concentration in the Rat Cecum. Biosci Biotechnol Biochem (2008) 72:572–6. doi: 10.1271/bbb.70474
80. Evans CC, LePard KJ, Kwak JW, Stancukas MC, Laskowski S, Dougherty J, et al. Exercise Prevents Weight Gain and Alters the Gut Microbiota in a Mouse Model of High Fat Diet-Induced Obesity. PloS One (2014) 9:e92193. doi: 10.1371/journal.pone.0092193
81. Säemann MD, Böhmig GA, Osterreicher CH, Burtscher H, Parolini O, Diakos C, et al. Anti-Inflammatory Effects of Sodium Butyrate on Human Monocytes: Potent Inhibition of IL-12 and Up-Regulation of IL-10 Production. FASEB J (2000) 14:2380–2. doi: 10.1096/fj.00-0359fje
82. Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate Enhances the Intestinal Barrier by Facilitating Tight Junction Assembly Via activation AMP-activated Protein Kinase Caco-2 Cell Monolayers. J Nutr (2009) 139:1619–25. doi: 10.3945/jn.109.104638
83. Queipo-Ortuño MI, Seoane LM, Murri M, Pardo M, Gomez-Zumaquero JM, Cardona F, et al. Gut Microbiota Composition in Male Rat Models Under Different Nutritional Status and Physical Activity and its Association With Serum Leptin and Ghrelin Levels. PloS One (2013) 8:e65465. doi: 10.1371/journal.pone.0065465
84. Mika A, Van Treuren W, González A, Herrera JJ, Knight R, Fleshner M. Exercise is More Effective at Altering Gut Microbial Composition and Producing Stable Changes in Lean Mass in Juvenile Versus Adult Male F344 Rats. PloS One (2015) 10:e0125889. doi: 10.1371/journal.pone.0125889
85. Lambert JE, Myslicki JP, Bomhof MR, Belke DD, Shearer J, Reimer RA. Exercise Training Modifies Gut Microbiota in Normal and Diabetic Mice. Appl Physiol Nutr Metab (2015) 40:749–52. doi: 10.1139/apnm-2014-0452
86. Louis P, Flint HJ. Diversity, Metabolism and Microbial Ecology of Butyrate-Producing Bacteria From the Human Large Intestine. FEMS Microbiol Lett (2009) 294:1–8. doi: 10.1111/j.1574-6968.2009.01514.x
87. Ma Q, Xing C, Long W, Wang HY, Liu Q, Wang RF. Impact of Microbiota on Central Nervous System and Neurological Diseases: The Gut-Brain Axis. J Neuroinflamm (2019) 16:53. doi: 10.1186/s12974-019-1434-3
88. Rhee SH, Pothoulakis C, Mayer EA. Principles and Clinical Implications of the Brain-Gut-Enteric Microbiota Axis. Nat Rev Gastroenterol Hepatol (2009) 6:306–14. doi: 10.1038/nrgastro.2009.35
89. Rogers GB, Keating DJ, Young RL, Wong ML, Licinio J, Wesselingh S. From Gut Dysbiosis to Altered Brain Function and Mental Illness: Mechanisms and Pathways. Mol Psychiatry (2016) 21:738–48. doi: 10.1038/mp.2016.50
90. Moser G, Fournier C, Peter J. Intestinal Microbiome-Gut-Brain Axis and Irritable Bowel Syndrome. Wiener Medizinische Wochenschrift (1946) (2018) 168:62–6. doi: 10.1007/s10354-017-0592-0
91. Neufeld KM, Kang N, Bienenstock J, Foster JA. Reduced Anxiety-Like Behavior and Central Neurochemical Change in Germ-Free Mice. Neurogastroenterol Motil (2011) 23:255–64. doi: 10.1111/j.1365-2982.2010.01620.x
92. Duman RS, Deyama S, Fogaça MV. Role of BDNF in the Pathophysiology and Treatment of Depression: Activity-dependent Effects Distinguish Rapid-Acting Antidepressants. Eur J Neurosci (2019) 53:126–39. doi: 10.1111/ejn.14630
93. Bistoletti M, Caputi V, Baranzini N, Marchesi N, Filpa V, Marsilio I, et al. Antibiotic Treatment-Induced Dysbiosis Differently Affects BDNF and TrkB Expression in the Brain and in the Gut of Juvenile Mice. PloS One (2019) 14:e0212856. doi: 10.1371/journal.pone.0212856
94. Mayer EA, Labus JS, Tillisch K, Cole SW, Baldi P. Towards a Systems View of IBS. Nat Rev Gastroenterol Hepatol (2015) 12:592–605. doi: 10.1038/nrgastro.2015.121
95. Labus JS, Hollister EB, Jacobs J, Kirbach K, Oezguen N, Gupta A, et al. Differences in Gut Microbial Composition Correlate With Regional Brain Volumes in Irritable Bowel Syndrome. Microbiome (2017) 5:49. doi: 10.1186/s40168-017-0260-z
96. Yang D, Zhao D, Ali Shah SZ, Wu W, Lai M, Zhang X, et al. The Role of the Gut Microbiota in the Pathogenesis of Parkinson’s Disease. Front Neurol (2019) 10:1155. doi: 10.3389/fneur.2019.01155
97. Braak H, de Vos RA, Bohl J, Del Tredici K. Gastric Alpha-Synuclein Immunoreactive Inclusions in Meissner’s and Auerbach’s Plexuses in Cases Staged for Parkinson’s Disease-Related Brain Pathology. Neurosci Lett (2006) 396:67–72. doi: 10.1016/j.neulet.2005.11.012
98. Savica R, Carlin JM, Grossardt BR, Bower JH, Ahlskog JE, Maraganore DM, et al. Medical Records Documentation of Constipation Preceding Parkinson Disease: A Case-Control Study. Neurology (2009) 73:1752–8. doi: 10.1212/WNL.0b013e3181c34af5
99. Shannon KM, Keshavarzian A, Dodiya HB, Jakate S, Kordower JH. Is Alpha-Synuclein in the Colon a Biomarker for Premotor Parkinson’s Disease? Evidence From 3 Cases. Mov Disord (2012) 27:716–9. doi: 10.1002/mds.25020
100. Stojkovska I, Wagner BM, Morrison BE. Parkinson’s Disease and Enhanced Inflammatory Response. Exp Biol Med (Maywood) (2015) 240:1387–95. doi: 10.1177/1535370215576313
101. Powell N, Walker MM, Talley NJ. The Mucosal Immune System: Master Regulator of Bidirectional Gut-Brain Communications. Nat Rev Gastroenterol Hepatol (2017) 14:143–59. doi: 10.1038/nrgastro.2016.191
102. Proctor C, Thiennimitr P, Chattipakorn N, Chattipakorn SC. Diet, Gut Microbiota and Cognition. Metab Brain Dis (2017) 32:1–17. doi: 10.1007/s11011-016-9917-8
103. David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet Rapidly and Reproducibly Alters the Human Gut Microbiome. Nature (2014) 505:559–63. doi: 10.1038/nature12820
104. Sonnenburg ED, Sonnenburg JL. Starving Our Microbial Self: The Deleterious Consequences of a Diet Deficient in Microbiota-Accessible Carbohydrates. Cell Metab (2014) 20:779–86. doi: 10.1016/j.cmet.2014.07.003
105. Sonnenburg ED, Smits SA, Tikhonov M, Higginbottom SK, Wingreen NS, Sonnenburg JL. Diet-Induced Extinctions in the Gut Microbiota Compound Over Generations. Nature (2016) 529:212–5. doi: 10.1038/nature16504
106. Daien CI, Pinget GV, Tan JK, Macia L. Detrimental Impact of Microbiota-Accessible Carbohydrate-Deprived Diet on Gut and Immune Homeostasis: An Overview. Front Immunol (2017) 8:548. doi: 10.3389/fimmu.2017.00548
107. Smits SA, Leach J, Sonnenburg ED, Gonzalez CG, Lichtman JS, Reid G, et al. Seasonal Cycling in the Gut Microbiome of the Hadza Hunter-Gatherers of Tanzania. Science (2017) 357:802–6. doi: 10.1126/science.aan4834
108. den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. The Role of Short-Chain Fatty Acids in the Interplay Between Diet, Gut Microbiota, and Host Energy Metabolism. J Lipid Res (2013) 54:2325–40. doi: 10.1194/jlr.R036012
109. Jampolis MB, Rothkopf MM, Li Z, Diamond SJ, Allen K, Abdelhadi RA, et al. Principles of Healthful Eating. Curr Nutr Rep (2016) 5:180–90. doi: 10.1007/s13668-016-0168-4
110. Wang L, Jacobs JP, Lagishetty V, Yuan PQ, Wu SV, Million M, et al. High-Protein Diet Improves Sensitivity to Cholecystokinin and Shifts the Cecal Microbiome Without Altering Brain Inflammation in Diet-Induced Obesity in Rats. Am J Physiol Regul Integr Comp Physiol (2017) 313:R473–r486. doi: 10.1152/ajpregu.00105.2017
111. Kaptan Z, Akgun-Dar K, Kapucu A, Dedeakayogullari H, Batu S, Uzum G. Long Term Consequences on Spatial Learning-Memory of Low-Calorie Diet During Adolescence in Female Rats; Hippocampal and Prefrontal Cortex BDNF Level, Expression of NeuN and Cell Proliferation in Dentate Gyrus. Brain Res (2015) 1618:194–204. doi: 10.1016/j.brainres.2015.05.041
112. Liu Z, Patil IY, Jiang T, Sancheti H, Walsh JP, Stiles BL, et al. High-Fat Diet Induces Hepatic Insulin Resistance and Impairment of Synaptic Plasticity. PloS One (2015) 10:e0128274. doi: 10.1371/journal.pone.0128274
113. Daniel H, Gholami AM, Berry D, Desmarchelier C, Hahne H, Loh G, et al. High-Fat Diet Alters Gut Microbiota Physiology in Mice. ISME J (2014) 8:295–308. doi: 10.1038/ismej.2013.155
114. Sharma S, Fernandes MF, Fulton S. Adaptations in Brain Reward Circuitry Underlie Palatable Food Cravings and Anxiety Induced by High-Fat Diet Withdrawal. Int J Obes (Lond) (2013) 37:1183–91. doi: 10.1038/ijo.2012.197
115. Wu GD, Chen J, Hoffmann C, Bittinger K, Chen YY, Keilbaugh SA, et al. Linking Long-Term Dietary Patterns With Gut Microbial Enterotypes. Science (2011) 334:105–8. doi: 10.1126/science.1208344
116. Reddy BS, Weisburger JH, Wynder EL. Effects of High Risk and Low Risk Diets for Colon Carcinogenesis on Fecal Microflora and Steroids in Man. J Nutr (1975) 105:878–84. doi: 10.1093/jn/105.7.878
117. Drasar BS, Crowther JS, Goddard P, Hawksworth G, Hill MJ, Peach S, et al. The Relation Between Diet and the Gut Microflora in Man. Proc Nutr Soc (1973) 32:49–52. doi: 10.1079/pns19730014
118. De Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, et al. High-Level Adherence to a Mediterranean Diet Beneficially Impacts the Gut Microbiota and Associated Metabolome. Gut (2016) 65:1812–21. doi: 10.1136/gutjnl-2015-309957
119. Lopez-Legarrea P, Fuller NR, Zulet MA, Martinez JA, Caterson ID. The Influence of Mediterranean, Carbohydrate and High Protein Diets on Gut Microbiota Composition in the Treatment of Obesity and Associated Inflammatory State. Asia Pac J Clin Nutr (2014) 23:360–8. doi: 10.6133/apjcn.2014.23.3.16
120. Del Chierico F, Vernocchi P, Dallapiccola B, Putignani L. Mediterranean Diet and Health: Food Effects on Gut Microbiota and Disease Control. Int J Mol Sci (2014) 15:11678–99. doi: 10.3390/ijms150711678
121. Sanz Y. Effects of a Gluten-Free Diet on Gut Microbiota and Immune Function in Healthy Adult Humans. Gut Microbes (2010) 1:135–7. doi: 10.4161/gmic.1.3.11868
122. Bonder MJ, Tigchelaar EF, Cai X, Trynka G, Cenit MC, Hrdlickova B, et al. The Influence of a Short-Term Gluten-Free Diet on the Human Gut Microbiome. Genome Med (2016) 8:45. doi: 10.1186/s13073-016-0295-y
123. De Palma G, Nadal I, Collado MC, Sanz Y. Effects of a Gluten-Free Diet on Gut Microbiota and Immune Function in Healthy Adult Human Subjects. Br J Nutr (2009) 102:1154–60. doi: 10.1017/s0007114509371767
124. Lorenzo Pisarello MJ, Vintiñi EO, González SN, Pagani F, Medina MS. Decrease in Lactobacilli in the Intestinal Microbiota of Celiac Children With a Gluten-Free Diet, and Selection of Potentially Probiotic Strains. Can J Microbiol (2015) 61:32–7. doi: 10.1139/cjm-2014-0472
125. Wacklin P, Laurikka P, Lindfors K, Collin P, Salmi T, Lähdeaho ML, et al. Altered Duodenal Microbiota Composition in Celiac Disease Patients Suffering From Persistent Symptoms on a Long-Term Gluten-Free Diet. Am J Gastroenterol (2014) 109:1933–41. doi: 10.1038/ajg.2014.355
126. Vors C, Pineau G, Drai J, Meugnier E, Pesenti S, Laville M, et al. Postprandial Endotoxemia Linked With Chylomicrons and Lipopolysaccharides Handling in Obese Versus Lean Men: A Lipid Dose-Effect Trial. J Clin Endocrinol Metab (2015) 100:3427–35. doi: 10.1210/jc.2015-2518
127. Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes (2007) 56:1761–72. doi: 10.2337/db06-1491
128. Mitsuoka T. [the Effect of Nutrition on Intestinal Flora]. Nahrung (1984) 28:619–25. doi: 10.1002/food.19840280616
129. Park JE, Seo JE, Lee JY, Kwon H. Distribution of Seven N-Nitrosamines in Food. Toxicol Res (2015) 31:279–88. doi: 10.5487/tr.2015.31.3.279
130. Fava F, Gitau R, Griffin BA, Gibson GR, Tuohy KM, Lovegrove JA. The Type and Quantity of Dietary Fat and Carbohydrate Alter Faecal Microbiome and Short-Chain Fatty Acid Excretion in a Metabolic Syndrome ‘At-Risk’ Population. Int J Obes (Lond) (2013) 37:216–23. doi: 10.1038/ijo.2012.33
131. Queipo-Ortuño MI, Boto-Ordóñez M, Murri M, Gomez-Zumaquero JM, Clemente-Postigo M, Estruch R, et al. Influence of Red Wine Polyphenols and Ethanol on the Gut Microbiota Ecology and Biochemical Biomarkers. Am J Clin Nutr (2012) 95:1323–34. doi: 10.3945/ajcn.111.027847
132. Bialonska D, Ramnani P, Kasimsetty SG, Muntha KR, Gibson GR, Ferreira D. The Influence of Pomegranate by-Product and Punicalagins on Selected Groups of Human Intestinal Microbiota. Int J Food Microbiol (2010) 140:175–82. doi: 10.1016/j.ijfoodmicro.2010.03.038
133. Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, et al. Differential Adaptation of Human Gut Microbiota to Bariatric Surgery-Induced Weight Loss: Links With Metabolic and Low-Grade Inflammation Markers. Diabetes (2010) 59:3049–57. doi: 10.2337/db10-0253
134. Clemente-Postigo M, Queipo-Ortuño MI, Murri M, Boto-Ordoñez M, Perez-Martinez P, Andres-Lacueva C, et al. Endotoxin Increase After Fat Overload is Related to Postprandial Hypertriglyceridemia in Morbidly Obese Patients. J Lipid Res (2012) 53:973–8. doi: 10.1194/jlr.P020909
135. Koloverou E, Panagiotakos DB, Pitsavos C, Chrysohoou C, Georgousopoulou EN, Grekas A, et al. Adherence to Mediterranean Diet and 10-Year Incidence (2002-2012) of Diabetes: Correlations With Inflammatory and Oxidative Stress Biomarkers in the ATTICA Cohort Study. Diabetes Metab Res Rev (2016) 32:73–81. doi: 10.1002/dmrr.2672
136. Wu GD, Compher C, Chen EZ, Smith SA, Shah RD, Bittinger K, et al. Comparative Metabolomics in Vegans and Omnivores Reveal Constraints on Diet-Dependent Gut Microbiota Metabolite Production. Gut (2016) 65:63–72. doi: 10.1136/gutjnl-2014-308209
137. Zimmer J, Lange B, Frick JS, Sauer H, Zimmermann K, Schwiertz A, et al. A Vegan or Vegetarian Diet Substantially Alters the Human Colonic Faecal Microbiota. Eur J Clin Nutr (2012) 66:53–60. doi: 10.1038/ejcn.2011.141
138. Guo Y, Luo S, Ye Y, Yin S, Fan J, Xia M. Intermittent Fasting Improves Cardiometabolic Risk Factors and Alters Gut Microbiota in Metabolic Syndrome Patients. J Clin Endocrinol Metab (2021) 106:64–79. doi: 10.1210/clinem/dgaa644
139. McFadden KL, Cornier MA, Tregellas JR. The Role of Alpha-7 Nicotinic Receptors in Food Intake Behaviors. Front Psychol (2014) 5:553. doi: 10.3389/fpsyg.2014.00553
140. Dani JA, De Biasi M. Cellular Mechanisms of Nicotine Addiction. Pharmacol Biochem Behav (2001) 70:439–46. doi: 10.1016/s0091-3057(01)00652-9
141. Friedman TC, Sinha-Hikim I, Parveen M, Najjar SM, Liu Y, Mangubat M, et al. Additive Effects of Nicotine and High-Fat Diet on Hepatic Steatosis in Male Mice. Endocrinology (2012) 153:5809–20. doi: 10.1210/en.2012-1750
142. Ivey R, Desai M, Green K, Sinha-Hikim I, Friedman TC, Sinha-Hikim AP. Additive Effects of Nicotine and High-Fat Diet on Hepatocellular Apoptosis in Mice: Involvement of Caspase 2 and Inducible Nitric Oxide Synthase-Mediated Intrinsic Pathway Signaling. Horm Metab Res (2014) 46:568–73. doi: 10.1055/s-0034-1375610
143. Sinha-Hikim I, Friedman TC, Shin CS, Lee D, Ivey R, Sinha-Hikim AP. Nicotine in Combination With a High-Fat Diet Causes Intramyocellular Mitochondrial Abnormalities in Male Mice. Endocrinology (2014) 155:865–72. doi: 10.1210/en.2013-1795
144. Hasan MK, Friedman TC, Sims C, Lee DL, Espinoza-Derout J, Ume A, et al. Alpha7-Nicotinic Acetylcholine Receptor Agonist Ameliorates Nicotine Plus High-Fat Diet-Induced Hepatic Steatosis in Male Mice by Inhibiting Oxidative Stress and Stimulating Ampk Signaling. Endocrinology (2018) 159:931–44. doi: 10.1210/en.2017-00594
145. Allais L, Kerckhof FM, Verschuere S, Bracke KR, De Smet R, Laukens D, et al. Chronic Cigarette Smoke Exposure Induces Microbial and Inflammatory Shifts and Mucin Changes in the Murine Gut. Environ Microbiol (2016) 18:1352–63. doi: 10.1111/1462-2920.12934
146. Stewart CJ, Auchtung TA, Ajami NJ, Velasquez K, Smith DP, De La Garza R, et al. 2ndEffects of Tobacco Smoke and Electronic Cigarette Vapor Exposure on the Oral and Gut Microbiota in Humans: A Pilot Study. PeerJ (2018) 6:e4693. doi: 10.7717/peerj.4693
147. Nolan-Kenney R, Wu F, Hu J, Yang L, Kelly D, Li H, et al. The Association Between Smoking and Gut Microbiome in Bangladesh. Nicotine Tob Res (2019) 22:1339–46. doi: 10.1093/ntr/ntz220
148. Biedermann L, Zeitz J, Mwinyi J, Sutter-Minder E, Rehman A, Ott SJ, et al. Smoking Cessation Induces Profound Changes in the Composition of the Intestinal Microbiota in Humans. PloS One (2013) 8:e59260. doi: 10.1371/journal.pone.0059260
149. Kobayashi T, Fujiwara K. Identification of Heavy Smokers Through Their Intestinal Microbiota by Data Mining Analysis. Biosci Microbiota Food Health (2013) 32:77–80. doi: 10.12938/bmfh.32.77
150. Benjamin JL, Hedin CR, Koutsoumpas A, Ng SC, McCarthy NE, Prescott NJ, et al. Smokers With Active Crohn’s Disease Have a Clinically Relevant Dysbiosis of the Gastrointestinal Microbiota. Inflammation Bowel Dis (2012) 18:1092–100. doi: 10.1002/ibd.21864
151. Opstelten JL, Plassais J, van Mil SW, Achouri E, Pichaud M, Siersema PD, et al. Gut Microbial Diversity Is Reduced in Smokers With Crohn’s Disease. Inflammation Bowel Dis (2016) 22:2070–7. doi: 10.1097/mib.0000000000000875
152. Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A Randomized Trial of E-Cigarettes Versus Nicotine-Replacement Therapy. N Engl J Med (2019) 380:629–37. doi: 10.1056/NEJMoa1808779
153. Barrington-Trimis JL, Leventhal AM. Adolescents’ Use of “Pod Mod” E-Cigarettes - Urgent Concerns. N Engl J Med (2018) 379:1099–102. doi: 10.1056/NEJMp1805758
154. DeVito EE, Krishnan-Sarin S. E-Cigarettes: Impact of E-Liquid Components and Device Characteristics on Nicotine Exposure. Curr Neuropharmacol (2018) 16:438–59. doi: 10.2174/1570159x15666171016164430
155. Espinoza-Derout J, Hasan KM, Shao XM, Jordan MC, Sims C, Lee DL, et al. Chronic Intermittent Electronic Cigarette Exposure Induces Cardiac Dysfunction and Atherosclerosis in Apolipoprotein-E Knockout Mice. Am J Physiol Heart Circ Physiol (2019) 317. doi: 10.1152/ajpheart.00738.2018
156. Lanza ST, Russell MA, Braymiller JL. Emergence of Electronic Cigarette Use in US Adolescents and the Link to Traditional Cigarette Use. Addict Behav (2017) 67:38–43. doi: 10.1016/j.addbeh.2016.12.003
157. Noel A, Hansen S, Zaman A, Perveen Z, Pinkston R, Hossain E, et al. In Utero Exposures to Electronic-Cigarette Aerosols Impair the Wnt Signaling During Mouse Lung Development. Am J Physiol Lung Cell Mol Physiol (2020) 318:L705–22. doi: 10.1152/ajplung.00408.2019
158. Benowitz NL, Burbank AD. Cardiovascular Toxicity of Nicotine: Implications for Electronic Cigarette Use. Trends Cardiovasc Med (2016) 26:515–23. doi: 10.1016/j.tcm.2016.03.001
159. Sinha-Hikim I, Friedman TC, Falz M, Chalfant V, Hasan MK, Espinoza-Derout J, et al. Nicotine Plus a High-Fat Diet Triggers Cardiomyocyte Apoptosis. Cell Tissue Res (2017) 368:159–70. doi: 10.1007/s00441-016-2536-1
160. Wang Z, Wang D, Wang Y. Cigarette Smoking and Adipose Tissue: The Emerging Role in Progression of Atherosclerosis. Mediators Inflammation (2017) 2017:3102737. doi: 10.1155/2017/3102737
161. Wu Y, Song P, Zhang W, Liu J, Dai X, Liu Z, et al. Activation of Ampkα2 in Adipocytes is Essential for Nicotine-Induced Insulin Resistance. vivo Nat Med (2015) 21:373–82. doi: 10.1038/nm.3826
162. Hamabe A, Uto H, Imamura Y, Kusano K, Mawatari S, Kumagai K, et al. Impact of Cigarette Smoking on Onset of Nonalcoholic Fatty Liver Disease Over a 10-Year Period. J Gastroenterol (2011) 46:769–78. doi: 10.1007/s00535-011-0376-z
163. Zein CO, Unalp A, Colvin R, Liu YC, McCullough AJ. Smoking and Severity of Hepatic Fibrosis in Nonalcoholic Fatty Liver Disease. J Hepatol (2011) 54:753–9. doi: 10.1016/j.jhep.2010.07.040
165. Spencer MD, Hamp TJ, Reid RW, Fischer LM, Zeisel SH, Fodor AA. Association Between Composition of the Human Gastrointestinal Microbiome and Development of Fatty Liver With Choline Deficiency. Gastroenterology (2011) 140:976–86. doi: 10.1053/j.gastro.2010.11.049
166. Tremaroli V, Backhed F. Functional Interactions Between the Gut Microbiota and Host Metabolism. Nature (2012) 489:242–9. doi: 10.1038/nature11552
167. Leung C, Rivera L, Furness JB, Angus PW. The Role of the Gut Microbiota in NAFLD. Nat Rev Gastroenterol Hepatol (2016) 13:412–25. doi: 10.1038/nrgastro.2016.85
168. Motohashi H, Yamamoto M. Nrf2-Keap1 Defines a Physiologically Important Stress Response Mechanism. Trends Mol Med (2004) 10:549–57. doi: 10.1016/j.molmed.2004.09.003
169. Nguyen T, Nioi P, Pickett CB. The Nrf2-antioxidant Response Element Signaling Pathway and its Activation by Oxidative Stress. J Biol Chem (2009) 284:13291–5. doi: 10.1074/jbc.R900010200
170. Sinha-Hikim I, Sinha-Hikim AP, Shen R, Kim HJ, French SW, Vaziri ND, et al. A Novel Cystine Based Antioxidant Attenuates Oxidative Stress and Hepatic Steatosis in Diet-Induced Obese Mice. Exp Mol Pathol (2011) 91:419–28. doi: 10.1016/j.yexmp.2011.04.009
171. Trauner M, Arrese M, Wagner M. Fatty Liver and Lipotoxicity. Biochim Biophys Acta (2010) 1801:299–310. doi: 10.1016/j.bbalip.2009.10.007
172. Buzzetti E, Pinzani M, Tsochatzis EA. The Multiple-Hit Pathogenesis of non-Alcoholic Fatty Liver Disease (NAFLD). Metabolism (2016) 65:1038–48. doi: 10.1016/j.metabol.2015.12.012
173. Bozaykut P, Sahin A, Karademir B, Ozer NK. Endoplasmic Reticulum Stress Related Molecular Mechanisms in Nonalcoholic Steatohepatitis. Mech Ageing Dev (2016) 157:17–29. doi: 10.1016/j.mad.2016.07.001
174. Malickova K, Francova I, Lukas M, Kolar M, Kralikova E, Bortlik M, et al. Fecal Zonulin is Elevated in Crohn’s Disease and in Cigarette Smokers. Pract Lab Med (2017) 9:39–44. doi: 10.1016/j.plabm.2017.09.001
175. Miele L, Valenza V, La Torre G, Montalto M, Cammarota G, Ricci R, et al. Increased Intestinal Permeability and Tight Junction Alterations in Nonalcoholic Fatty Liver Disease. Hepatology (2009) 49:1877–87. doi: 10.1002/hep.22848
Keywords: gut microbiome, gut microbiota, gut dysbiosis, nicotine, obesity, high-fat diet, nonalcoholic fatty liver disease, e-cigarette
Citation: Martinez JE, Kahana DD, Ghuman S, Wilson HP, Wilson J, Kim SCJ, Lagishetty V, Jacobs JP, Sinha-Hikim AP and Friedman TC (2021) Unhealthy Lifestyle and Gut Dysbiosis: A Better Understanding of the Effects of Poor Diet and Nicotine on the Intestinal Microbiome. Front. Endocrinol. 12:667066. doi: 10.3389/fendo.2021.667066
Received: 11 February 2021; Accepted: 17 May 2021;
Published: 08 June 2021.
Edited by:
Petia Kovatcheva-Datchary, University of Würzburg, GermanyReviewed by:
Raylene A. Reimer, University of Calgary, CanadaMarie-Christine Simon, University of Bonn, Germany
Copyright © 2021 Martinez, Kahana, Ghuman, Wilson, Wilson, Kim, Lagishetty, Jacobs, Sinha-Hikim and Friedman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Theodore C. Friedman, dGhlb2RvcmVmcmllZG1hbkBjZHJld3UuZWR1
†Present address:Jason E. MartinezLewis Katz School of Medicine, Temple University, Philadelphia, PA, United States
 Jason E. Martinez1
Jason E. Martinez1 Haley P. Wilson
Haley P. Wilson Venu Lagishetty
Venu Lagishetty Jonathan P. Jacobs
Jonathan P. Jacobs Amiya P. Sinha-Hikim
Amiya P. Sinha-Hikim Theodore C. Friedman
Theodore C. Friedman