- 1Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Qom University of Medical Sciences, Qom, Iran
- 2Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
- 3Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran
- 4Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Hamedan University of Medical Sciences, Hamedan, Iran
- 5Social Determinants of Health Research Center, Birjand University of Medical Sciences, Birjand, Iran
- 6Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
Aim: All over the world, many couples cannot conceive a child and have problems with pregnancy. Ovulation-inducing drugs are among the most important drugs used for the treatment of infertility. In recent years, there have been many debates about the relationship between fertility medication and cancer. Due to the lack of comprehensive study of this matter, and as understanding the relationship between the use of fertility drugs and cancer is of importance, the present study was conducted to investigate the relationship between infertility drugs and cancer in women.
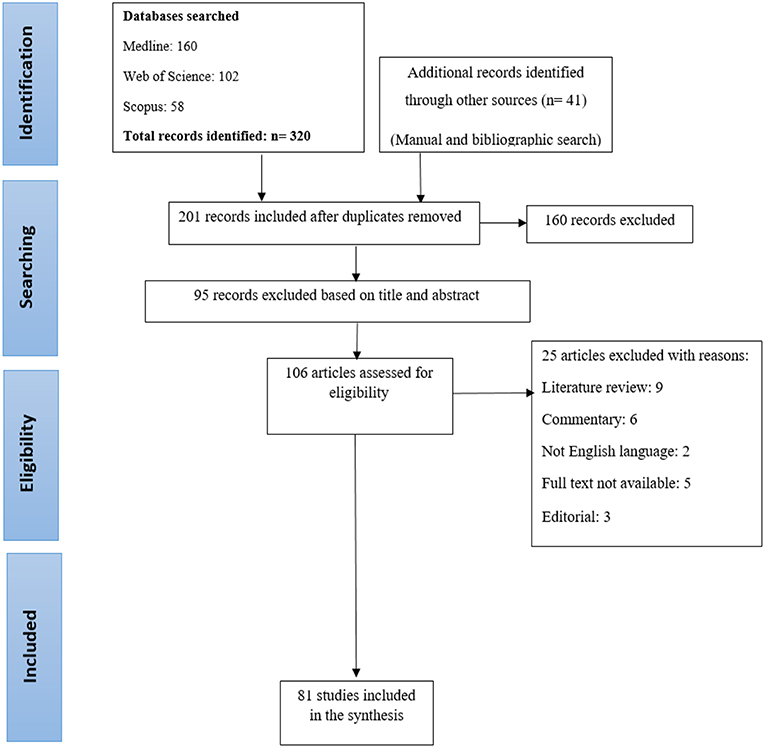
Materials and Methods: To determine the relationship between infertility treatment and cancer, a comprehensive search was carried out in databases such as; Medline, Web of Science Core Collection, and Scopus using keywords words; “infertility,” “ovulation induction,” “cancer,” “infertility treatment,” “ART,” “tumor,” “controlled ovarian stimulation,” “fertility agents,” and “neoplasms.” Full-text, English language, and original articles were included in this study.
Results: In total, 81 articles were entered into the study. The relationship between fertility medications and breast, ovary, endometrial, uterus, colon, thyroid, skin, cervical, and non-Hodgkin's lymphoma cancers were studied. Although the relationship between fertility medications and cancer is theoretically justifiable, most studies have shown that risk of cancer will not increase after fertility treatment.
Conclusion: The results of this study did not show that fertility medications increase the risk of cancer among users. In summary, the relationship between infertility treatment and cancer incidence remains an open question.
Introduction
All over the world, 48.5 million couples have problems with pregnancy, and many children are born with the help of fertility treatments, which primarily occurs in developing countries (1). After cancer and cardiovascular disease, infertility is the third most common disease (2). With increasing numbers of couples delaying parenting attempts, the prevalence of infertility is on the rise. Decreased fatality is one of the most important issues in Western countries, and is an essential part of reproductive health (1), which affects different aspects of life and imposes huge economic burdens on societies (2). Infertility is affected by various physiological, genetic, environmental, social, infectious, and nutritional factors (1, 3). Assisted reproductive technology (ART) is one of the most important strategies used today to increase the chance of fertility among infertile people (4). The ART uses many medications and techniques to increase the chance of fertility (5). Ovulation-inducing drugs are among the most important drugs used for the treatment of infertility, which affect the ovaries by increasing the levels of estrogen, progesterone, and gonadotropins. Complications of these drugs include ovarian hyper-stimulation syndrome, osteoporosis, and adverse pregnancy outcomes (6, 7).
In recent years, there have been many debates about the relationship between ovulation-inducing drugs, infertility treatment, and cancer (8–10). Changes in endogenous hormones that occur following the use of these drugs have raised many concerns about the safety of these treatments. Due to increasing infertility and the subsequent increase in the use of fertility drugs in recent years, investigating the long-term effects of these drugs are considerably important. It also raises the following question: Can the use of fertility drugs in the long-term cause cancer? Since understanding the relationship between the use of fertility drugs and cancer is important and due to the lack of comprehensive study in this regard, the present study was conducted to investigate the relationship between infertility drugs and cancer among women.
Materials and Methods
Search Strategy
To determine the relationship between infertility treatment and cancer, a comprehensive search for reliable articles was carried out in databases such as; Medline, Web of Science Core Collection (Indexes = SCI-EXPANDED, SSCI, A & HCI Timespan), and Scopus (all years), using keywords, including “infertility,” “ovulation induction,” “cancer,” “infertility treatment,” “ART,” “tumor,” “controlled ovarian stimulation,” “fertility agents,” and “neoplasms.” Combinations of these keywords were also used for the search. All keywords were checked with PubMed Medical Subject Heading (MeSH). Then, a manual search was conducted in valid journals for full-text articles and related systematic reviews. All retrieved articles were entered into the Endnote X7 software in one database. In order to reduce errors during the review phase, the PRISMA statement and Moher et al. (11) guidance were used.
Inclusion Criteria
Two researchers carefully reviewed the retrieved articles. The criteria for entering the study included; full-text articles, English language and original articles (case-control, retrospective and prospective cohort), the use of keywords in the title or abstract, articles with an abstract, and articles that have reviewed a type of malignancies associated with the use of fertility drugs. In vitro fertilization (IVF) and each of the clomiphene citrate regimens, the gonadotropins, human chorionic gonadotropin (hCG), human menopausal gonadotropin (hMG), gonadotropin-releasing hormone (GnRH) agonist, and antagonists were studied alone or in combination.
Exclusion Criteria
Case reports, case series, systematic reviews, meta- analysis, and animal studies were excluded.
Extracting and Analyzing the Data
The articles were categorized according to their specific characteristics including the number of participants, type of study, and type of fertility regimen. The risk scale in this study included; Standardized Incidence Ratio (SIR), Incidence Rate Ratio (IRR), Hazard Ratio (HR), and Odds Ratio (OR).
Results
Characteristics of the Selected Studies
After a comprehensive search through the databases, 320 articles were entered into the study and the references of 41 articles were manually reviewed. Duplicate articles were removed using Endnote software (n = 160). During the initial evaluation, 201 articles were selected for the review. After reviewing the title and abstract, 95 articles that were not consistent with the purpose of this study or did not meet the inclusion criteria were removed. The full texts of other articles were carefully examined by two researchers, and 25 articles were removed for scientific reasons (literature review: 9, commentary: 6, not English language: 2, full text not available: 5, editorial: 3). At the end, 81 articles were selected for the review (Figure 1).
Relationship Between Steroid Hormones and Cancer
In general, cancer occurs as a result of the division of mutated cells. Therefore, the hormone and any factor that stimulates the growth of the cells can affect the occurrence of cancer (12). The relationship between steroid hormones and some types of cancers, such as breast and endometrium cancers, is well-documented (12–14). Estrogen, progesterone, and testosterone are steroid hormones that are produced following a series of biological responses and are derived from cholesterol. Estrogen, which is one of the most important female sex hormones, is produced in the ovaries, the adrenal cortex, and the placenta, and leads to the growth of the reproductive system and the development of sexual traits (15). Based on the results of studies, free estradiol and albumin-bounded estradiol are associated with an increased risk of breast cancer (16) and can enhance the progression of metastatic breast cancer (17). High levels of estradiol and estrogen hormones in women with breast cancer contribute to the progression of metastatic breast cancer (18). Estrogen can contribute to the onset of cancer by affecting the mitosis duplication of epithelial cells. Increasing mitotic activity can play a role in increased probability of mutation and DNA damage, and reduced apoptosis and growth of early tumors (13, 19).
The role of gonadotropins in the occurrence of cancer has also been discussed by researchers. High levels of LH and FSH cause exposure to uncontested estrogen in the menstrual cycle, which contributes to an increase in cancer. On the other hand, stimulating the synthesis of mitogenic growth factors by gonadotropins can contribute to the growth of breast cancer cells (20, 21). In addition, high levels of gonadotrophin, predict a weaker prognosis in people with breast cancer (21).
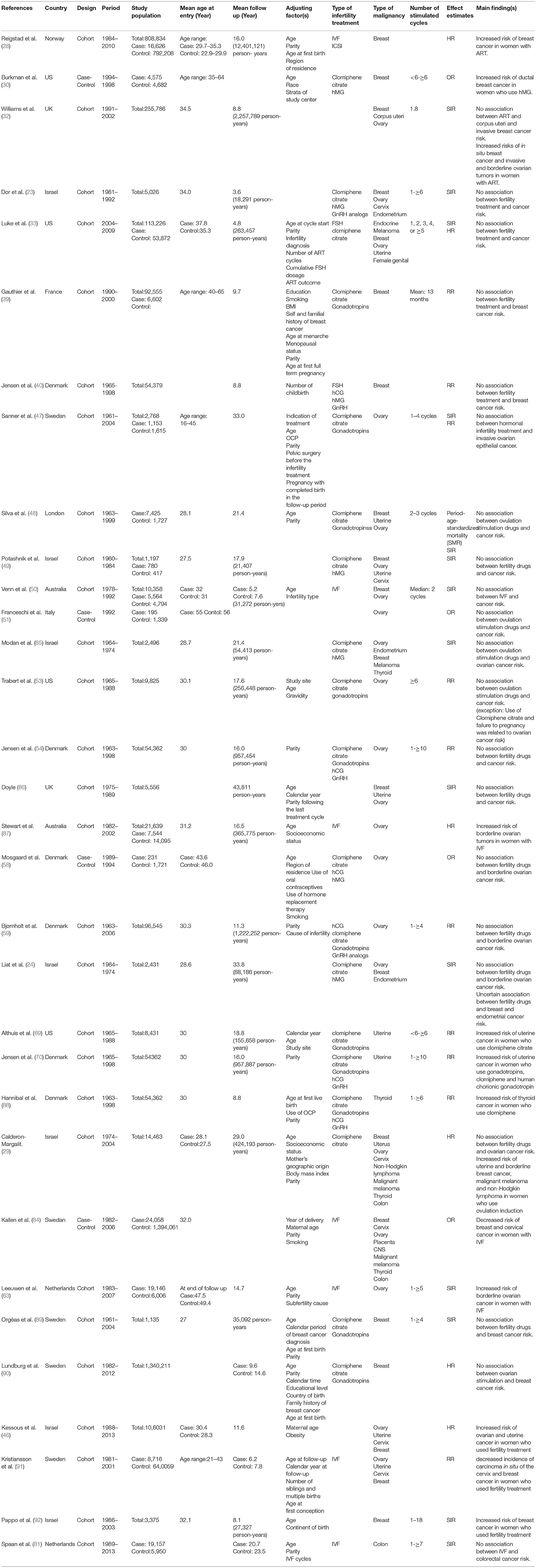
Analysis Based on the Type of Cancer (Table 1)
Breast Cancer
Breast cancer is a multifactorial disease and several risk factors are involved in its onset. The majority of breast cancers are hormone dependent (22). Several studies have pointed to the etiologic role of endogenous and exogenous hormones in increasing the risk of breast cancer. Therefore, the possible relationship between ovulation-inducing drugs and increased risk of breast cancer has been the subject of discussions by researchers (23–25). Compared with normal ovulation cycle, oestradiol concentration increase up to 10-fold in ovulation stimulation cycle (26). Treatment with fertility drugs is associated with an increased risk of breast cancer diagnosis in the first year after the treatment (27). The result of a cohort study of 808,834 women showed that the risk of breast cancer increased in individuals who gave birth following ART [adjusted hazard risk (HR) 1.20, 95% CI 1.01–1.42]. However, in this study confounding factors such as age of menarche, family history, history of breastfeeding, and obesity were not controlled (28). In a cohort study, the risk of breast cancer was increased among individuals who used ovulation-inducting drugs, although this risk was not statistically significant in primiparous women (29). The result of a case-control study of 35–64 years old women showed that, although the use of fertility drugs was not associated with an increased risk of breast cancer in general, the relative risk of breast cancer in people with a hMG use for more than 6 months or 6 cycles was about 2.7–3.8 (30). A case-control study found that IVF treatment after the age of 30 years was associated with an increased risk of breast cancer, however, the characteristics of breast tumors in subjects treated with IVF did not differ with the general population (31). Although the results of the above studies suggest a relationship between infertility treatment and the risk of breast cancer, a large, population based cohort study between 1991 and 2010 stated, regardless of infertility treatment, the risk of breast cancer in people who are incapable of conceiving or maintaining fetuses is increased by 2 times (32). Meanwhile, many researchers could not show a positive relationship between fertility treatment and breast cancer (32–38). The result of a cohort study of 98,997 women aged 40–65 years showed no relationship between the risk of breast cancer and infertility treatment, the type of treatment, the type of drug, the age of the person at the start of treatment, and the duration of treatment. The author of this study suggested that infertility treatments may be associated with an increased risk of breast cancer among women with a family history of breast cancer (39). In a cohort study of 54,362 women, Jensen showed no relationship between the duration of fertility drugs use, the time since the first use of drugs, and the risk of breast cancer (40). The results of a cohort study pointed to the potential association between family history and the use of ovulation-inducing drugs in the incidence of breast cancer (39). In general, according to the results of related studies, the relationship between fertility treatment and breast cancer has not been proven.
Ovarian Cancer
Ovarian cancer is a rare and the most fatal gynecological disease worldwide (41). Regardless of infertility treatments, the risk of ovarian cancer may be altered with nulliparity (24), and infertility (42, 43). Therefore, the relationship between infertility treatment and ovarian cancer is difficult to prove. The “incessant ovulation theory” states that uninterrupted ovulation can contribute to the development of ovarian cancer by damaging ovary epithelium and, therefore, any factor that contributes to the reduction of ovulation can have a protective effect against ovarian cancer (44). Many studies have indicated that an increased risk of ovarian cancer is associated with the intake of clomiphene citrate and gonadotropin (25, 45). A cohort study conducted from 1988 to 2013 revealed that, the risk of ovarian cancer is increased in individuals treated with IVF (adjusted HR 3.9; 95% CI 1.2–12.6), (46). The results of a cohort study showed an increase in the incident of ovarian cancer after exposure to clomiphene citrate. The results also indicated that risk of cancer increases with increasing dosage of the drug among nulliparous women (25). Use of clomiphene citrate, due to ovulation disorders, increases the risk of ovarian cancer (SIR = 7.47; 95% CI 1.54–21.83), (47). Although a number of studies have suggested that using ovulation-inducing drugs is associated with ovarian cancer, many of them have not shown any significant increase in the risk of ovarian cancer by taking ovulation-inducing drugs (29, 33, 48–52). The result of a retrospective cohort study showed that women who use clomiphene citrate and remained nulligravid are more likely to develop ovarian cancer than those who use this drug and get pregnant (RR 3.63, 95% CI 1.36–9.72 vs. RR 0.88, 95% CI 0.47–1.63), (53). In a cohort study of 54,362 women, authors reported that the risk of ovarian cancer does not increase with the use of clomiphene citrate, gonadotropins, human chorionic gonadotropin, and gonadotropin-releasing hormone, and that there is no relationship between the duration of drug use, duration of follow-up, and pregnancy (54). An increased risk of ovarian cancer among those taking ovulation-inducing drugs should be an issue of interest to therapists and, therefore, more attention should be paid to the people's choices (45).
In several studies, researchers have investigated the relationship between borderline ovarian tumors and fertility treatments. The risk to develop borderline ovarian tumors increased in women undergoing IVF, while childbirth, hysterectomy and sterilization do not have protective effects (55). In a cohort study, the use of clomiphene citrate and gonadotropins increased the risk of borderline ovarian tumors by up to 3 times (SIR = 3.61; 95% CI 1.45–7.44), (47). A case-control study showed a relationship between borderline ovarian tumors and the use of ovulation-inducing drugs, especially hMG (56). The result of a study revealed that, although treatment with clomiphene citrate for <1 year is not associated with an increase in the risk of borderline tumors, its prolonged use increases this risk (57). In a case-control study, researchers concluded that, regardless of treatment, the risk of borderline ovarian tumors is two times higher in nulliparous women (58). Other researchers, however, could not show such a relationship (59, 60). A case-control study examined the correlation between five groups of fertility drugs including clomiphene citrate, human menopausal gonadotropins and follicle stimulating hormone, gonadotropin-releasing hormone analogs, human chorionic gonadotropins, progesterone and borderline ovarian tumors. The study found that use of progesterone was associated with an increased in borderline ovarian tumors, especially serous tumors, but no correlation was found between the borderline ovarian tumors and the use of other drugs (59). There is an ongoing debate about the relationship between fertility treatments and the risk of ovarian cancer and, so far, there has been no definitive evidence to confirm such relationship (24, 61, 62). The relationship between these drugs and the borderline ovarian tumors has only been reported in some studies (56, 63, 64).
Endometrial and Uterine Cancer
Endometrial cancer is one of the hormone-related cancers. Although the relationship between endometrial cancer and ovulation-inducting drugs is not clear, it appears that these drugs increase mitosis activity, DNA replication, mutation and malignancy by increasing serum level of estradiol during the follicular phase (65). However, by increasing oocyte cycles and pregnancy, the level of progesterone is significantly increased, and this plays a protective role against endometrial cancer. Results of several cohort studies showed an increase in endometrial cancer among women who used clomiphene citrate (24, 25). In a cohort study, researchers reported the highest increase in endometrial cancer among nulliparous women and those who have used more than 6 cycles of clomiphene (25). A cohort study which lasted for 30-years revealed that infertility is associated with an increased risk of endometrial cancer, and this risk does increase by ovulation induction (24). This is consistent with the finding of Brinton's study (66). The results of a case- control study supported previous research and stated duration of use of fertility drugs was positively associated with endometrial cancer risk (OR = 6.10; 95% CI, 0.96–38.6) (67). There have been a few studies that did not show any relationship between fertility treatment and endometrial cancer (68).
According to a cohort of 29,700 IVF women, the incidence of uterine sarcoma increases in women who have history of infertility (8). In a large cohort study, authors reported that the risk of uterine cancer in people taking ovulation-stimulating drugs is increased by 3 times, and this risk will increase by 8 times after taking clomiphene citrate for 12 months (29). Based on the results of a retrospective cohort study, the risk of uterine cancer increases with the increase in the dose of clomiphene citrate, its cycle of use, and the time since its first use, The risk is also increased in nulligravid and obese individuals (69). A cohort study concluded that consumption of more than 2,250 mg of clomiphene is associated with a 2.6-fold increase in the risk of uterus cancers (48). In 2009, researchers in a population based cohort study pointed to the relationship between the high dosages of gonadotropins and hCG and uterine cancer among the gonadotropins and hCG users (70). Infertility drugs may increase estrogen level during the follicular phase of ovulation stimulation cycles, and use of hCG and clomiphene for more than 6 months may increase the risk of uterine cancer (54). In general, uterine and endometrial cancers do not have high prevalence among different age groups, especially young people who are the target group in most studies, and therefore it is challenging to determine the relationship between endometrial cancer and the use of ovulation-inducing drugs.
Thyroid Cancer
The effect of exogenous hormonal agents on estrogen dependent malignancies has been discussed by many researchers. Stimulation of ovulation is associated with increased level of TSH hormone in the circulation, which causes cell proliferation in the gland (25). Some medications, such as clomiphene citrate, may have a greater effect on the thyroid gland due to longer half-life (71). The results of various studies suggest a link between thyroid cancer and ART (25, 71). A cohort study concluded that, the use of clomiphene citrate is associated with a 2-fold increase in the risk of thyroid cancer, and this risk is not statistically significant among the users of gonadotropins, hCG, and GnRH (71). The risk of thyroid cancer is higher among nulligravid women who take clomiphene citrate (72, 73). However, in a cohort study, the risk of thyroid cancer was higher among parous individuals who were taking clomiphene citrate (71). The use of clomiphene (RR = 2.28; 95% CI: 1.08–4.82) and progesterone (RR = 10.14; 95% CI: 1.93–53.33) is associated with an increased risk of thyroid cancer (71). Other studies have not shown any relationship between fertility drugs and thyroid cancer. Authors in a cohort study stated that there is no evidence of any relationship between gonadotropins and thyroid cancer (73). In a study, aggressive pattern of papillary thyroid carcinoma was seen among thyroid cancer patients who had received IVF treatment in the past and this may cause a delay in the thyroid cancer diagnosis. In this study, thyroid cancer was diagnosed after 4 years from the last IVF treatment (74). The present study did not find any relationship between fertility treatment and thyroid cancer.
Skin Cancer
Skin cancer endangers many people's lives due to death or disability. Age, gender, diet, and genetics affect incidence of this cancer (75). Potential effect of oral contraceptive pills on melanoma (76, 77), has been a source of concern for researchers about the role of fertility drugs on this cancer. In a cohort study, the incident of skin cancer (except melanoma) was higher in those who were using IVF treatment (78). Researchers stated that, although in general infertility treatment is not associated with the risk of malignant melanoma, the use of clomiphene citrate is associated with an increased risk of malignant melanoma, and this risk is more pronounced among those who have been waiting for pregnancy for more than a year (29). In a cohort study, authors concluded that although infertility is not associated with an increased risk of malignant melanoma, exposure to fertility drugs in women with infertile partners increases the risk of melanoma, and this risk is also reduced in women who receive a low dose of fertility drugs (79). According to a retrospective cohort study, infertile women with progesterone deficiencies had higher melanoma risk (80). In a retrospective cohort study among 8,422 women in 1965–1988, the researchers confirmed this result and concluded that, the use of fertility treatment does not significantly alter the risk of melanoma. In this study, clomiphene citrate had a stronger effect on the risk of melanoma (RR = 2; 95% CI:0.9–4.6) (73). Overall, the results of studies have shown no relationship between the risk of melanoma and fertility drugs.
Colon Cancer
Although lifestyle is one of the most important risk factors for colon cancer, sex hormones may also affect the etiology of colon cancer. The results of a cohort study showed that infertility treatment does not increase the risk of colon cancer (73). The result of a 21-year follow-up in a cohort study showed that ovarian stimulation for IVF does not increase the risk of breast cancer in comparison with the general population (81). Furthermore, after a 30 year follow-up of 9,892 women treated with pre- IVF fertility drugs, researchers found that these drugs have no effect on colorectal cancer. The increase in IVF cycles and a greater amount of gonadotropin ampoules did not alter this risk (72). Other studies showed that ovulation stimulation for IVF does not increase the risk of colon cancer in comparison with the general population (48, 81). Estrogen is considered to be protective against colorectal cancer (82), and so this cancer is expected to decrease in women who use fertility drugs. In addition, lower level of insulin- like growth factor I in women who use exogenous hormones, may play a role in reducing colorectal cancer in these group (81). Generally, the results of present study suggest that fertility treatment is not a risk factor for colon cancer.
Cervical Cancer
Cervical cancer is the fourth most common cancer among women (83). Twenty years follow up of 8,422 women during 1965–1988 showed that infertility treatment does not change the risk of cervical cancer (73). According to a cohort study, ovulation induction reduces the risk of cervical cancer (48). Other cohort studies reported a lower risk of cervical cancer in people undergoing IVF treatment (23, 78, 84). Ultimately, researchers have reported that, due to regular screening and periodic examinations of infertile people, the risk of cervical cancer is lower among these people (25). In addition, parity and full- term pregnancy increase the risk of cervical cancer, therefore, it seems that this cancer is less prevalent among infertile women (83).
Non-Hodgkin's Lymphoma
Ovulation induction is associated with an increased risk of non-Hodgkin's lymphoma, and this risk is more pronounced in primiparous women as well as the first 5 years after childbirth (HR 2.63, 95% CI: 1.02, 6.82) (29).
Conclusion
The purpose of this study was to determine the relationship between the use of fertility drugs and cancer. Due to the correlation between hormonal and reproductive factors and women's cancers, much more attention has been paid to the relationship between the use of fertility drugs and cancer in recent years. Although this relationship is theoretically justifiable, the complex and multiple factors that are involved in the onset of cancer make it difficult to determine the definite relationship between the use of these drugs and cancer. In spite of the relationship that exists between the ovulation-inducing drugs and cancer in some cohort studies, the results of our study showed no significant increase in the incidence of cancer by infertility treatment. According to the results of this study, there is no definitive relationship between the use of fertility drugs and cancer, and only some observational studies have pointed to this relationship. So, the following question still cannot be answered: Are fertility drugs safe?
Although, the small sample size, short-term follow-up, and lack of control over confounding variables are some of the most important limitations of such studies, more studies are needed to achieve a better result. Since, the large proportion of people who use ovulation-inducing drugs are young, long-term follow-up can better detect the onset of cancer among them. At the end, the relationship between infertility treatment and cancer incidence remains an open question.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. (2012) 9:e1001356. doi: 10.1371/journal.pmed.1001356
2. Cong J, Li P, Zheng L, Tan J. Prevalence and risk factors of infertility at a rural site of Northern China. PLoS One. (2016) 11:e0155563. doi: 10.1371/journal.pone.0155563
3. Brugo-Olmedo S, Chillik C, Kopelman S. Definition and causes of infertility. Reprod Biomed Online. (2001) 2:173–85. doi: 10.1016/S1472-6483(10)62193-1
4. Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted reproductive technology surveillance—United States, 2014. MMWR Surveil Summ. (2017) 66:1. doi: 10.15585/mmwr.ss6606a1
5. Al-Shawaf T, Zosmer A, Dirnfeld M, Grudzinskas G. Safety of drugs used in assisted reproduction techniques. Drug Safety. (2005) 28:513–28. doi: 10.2165/00002018-200528060-00004
6. Klemetti R, Sevón T, Gissler M, Hemminki E. Complications of IVF and ovulation induction. Hum Reprod. (2005) 20:3293–300. doi: 10.1093/humrep/dei253
7. Shelley J, Venn A, Lumley J. Long-term effects on women of assisted reproduction. Int J Technol Assess Health Care. (1999) 15:36–51. doi: 10.1017/S0266462399015159
8. Venn A, Jones P, Quinn M, Healy D. Characteristics of ovarian and uterine cancers in a cohort of in vitro fertilization patients. Gynecol Oncol. (2001) 82:64–8. doi: 10.1006/gyno.2001.6209
9. Brinton LA, Scoccia B, Moghissi KS, Westhoff CL, Niwa S, Ruggieri D, et al. Long-term relationship of ovulation-stimulating drugs to breast cancer risk. Cancer Epidemiol Prevent Biomark. (2014) 23:584–93. doi: 10.1158/1055-9965.EPI-13-0996
10. Brinton L. Long-term effects of ovulation-stimulating drugs on cancer risk. Reprod Biomed Online. (2007) 15:38–44. doi: 10.1016/S1472-6483(10)60689-X
11. Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. (2010) 8:336–41. doi: 10.1016/j.ijsu.2010.02.007
12. Group ECW. Hormones and breast cancer. Hum Reprod Update. (2004) 10:281–93. doi: 10.1093/humupd/dmh025
13. Brown SB, Hankinson SE. Endogenous estrogens and the risk of breast, endometrial, and ovarian cancers. Steroids. (2015) 99:8–10. doi: 10.1016/j.steroids.2014.12.013
14. Brinton LA, Trabert B, Anderson GL, Falk RT, Felix AS, Fuhrman BJ, et al. Serum estrogens and estrogen metabolites and endometrial cancer risk among postmenopausal women. Cancer Epidemiol Prevent Biomark. (2016) 25:1081–9. doi: 10.1158/1055-9965.EPI-16-0225
15. Bohra A, Bhateja S. Carcinogenesis and sex hormones: a review. Endocrinol Metab Synd. (2015) 4:2161. doi: 10.4172/2161-1017.1000156
16. Toniolo PG, Levitz M, Zeleniuch-Jacquotte A, Banerjee S, Koenig KL, Shore RE, et al. A prospective study of endogenous estrogens and breast cancer in postmenopausal women. J Natl Cancer Inst. (1995) 87:190–7. doi: 10.1093/jnci/87.3.190
17. Yang X, Belosay A, Du M, Fan TM, Turner RT, Iwaniec UT, et al. Estradiol increases ER-negative breast cancer metastasis in an experimental model. Clin Exp Metast. (2013) 30:711–21. doi: 10.1007/s10585-012-9559-0
18. Key T, Appleby P, Barnes I, Reeves G. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst. (2002) 94:606–16. doi: 10.1093/jnci/94.8.606
19. Yue W, Wang JP, Li Y, Fan P, Liu G, Zhang N, et al. Effects of estrogen on breast cancer development: role of estrogen receptor independent mechanisms. Int J Cancer. (2010) 127:1748–57. doi: 10.1002/ijc.25207
20. Schneider J, Martín-Gutiérrez S, Tresguerres JA, García-Velasco JA. Circulating estradiol defines the tumor phenotype in menopausal breast cancer patients. Maturitas. (2009) 64:43–5. doi: 10.1016/j.maturitas.2009.07.001
21. Pujol P, Daures JP, Brouillet JP, Chang S, Rouanet P, Bringer J, et al. A prospective prognostic study of the hormonal milieu at the time of surgery in premenopausal breast carcinoma. Cancer. (2001) 91:1854–61. doi: 10.1002/1097-0142(20010515)91:10<1854::AID-CNCR1206>3.0.CO;2-Y
22. Sönmezer M, Cil AP, Oktem O, Oktay K. Breast cancer diagnosis following ovarian stimulation: are the tumours different? Reprod Biomed Online. (2010) 21:266–71. doi: 10.1016/j.rbmo.2010.05.006
23. Dor J, Lerner-Geva L, Rabinovici J, Chetrit A, Levran D, Lunenfeld B, et al. Cancer incidence in a cohort of infertile women who underwent in vitro fertilization. Fertil Steril. (2002) 77:324–7. doi: 10.1016/S0015-0282(01)02986-7
24. Liat L-G, Jaron R, Liraz O, Shlomo M, Bruno L. Are infertility treatments a potential risk factor for cancer development? Perspective of 30 years of follow-up. Gynecol Endocrinol. (2012) 28:809–14. doi: 10.3109/09513590.2012.671391
25. Reigstad MM, Storeng R, Myklebust TÅ, Oldereid NB, Omland AK, Robsahm TE, et al. Cancer risk in women treated with fertility drugs according to parity status—a registry-based cohort study. Cancer Epidemiol Prevent Biomark. (2017) 26:953–62. doi: 10.1158/1055-9965.EPI-16-0809
26. Sonmezer M, Oktay K. Fertility preservation in female patients. Hum Reprod Update. (2004) 10:251–66. doi: 10.1093/humupd/dmh021
27. Venn A, Watson L, Bruinsma F, Giles G, Healy D. Risk of cancer after use of fertility drugs with in-vitro fertilisation. Lancet. (1999) 354:1586–90. doi: 10.1016/S0140-6736(99)05203-4
28. Reigstad MM, Larsen IK, Myklebust TÅ, Robsahm TE, Oldereid NB, Omland AK, et al. Risk of breast cancer following fertility treatment—a registry based cohort study of parous women in Norway. Int J Cancer. (2015) 136:1140–8. doi: 10.1002/ijc.29069
29. Calderon-Margalit R, Friedlander Y, Yanetz R, Kleinhaus K, Perrin M, Manor O, et al. Cancer risk after exposure to treatments for ovulation induction. Am J Epidemiol. (2008) 169:365–75. doi: 10.1093/aje/kwn318
30. Burkman RT, Tang M-TC, Malone KE, Marchbanks PA, McDonald JA, Folger SG. Infertility drugs and the risk of breast cancer: findings from the National Institute of child health and human development women's contraceptive and reproductive experiences study. Fertil Steril. (2003) 79:844–51. doi: 10.1016/S0015-0282(02)04950-6
31. Katz D, Paltiel O, Peretz T, Revel A, Sharon N, Maly B, et al. Beginning IVF treatments after age 30 increases the risk of breast cancer: results of a case-control study. Breast J. (2008) 14:517–22. doi: 10.1111/j.1524-4741.2008.00641.x
32. Williams CL, Jones ME, Swerdlow AJ, Botting BJ, Davies MC, Jacobs I, et al. Risks of ovarian, breast, and corpus uteri cancer in women treated with assisted reproductive technology in Great Britain, 1991-2010: data linkage study including 2.2 million person years of observation. BMJ. (2018) 362:k2644. doi: 10.1136/bmj.k2644
33. Luke B, Brown MB, Spector LG, Missmer SA, Leach RE, Williams M, et al. Cancer in women after assisted reproductive technology. Fertil Steril. (2015) 104:1218–26. doi: 10.1016/j.fertnstert.2015.07.1135
34. Terry KL, Willett WC, Rich-Edwards JW, Michels KB. A prospective study of infertility due to ovulatory disorders, ovulation induction, and incidence of breast cancer. Arch Intern Med. (2006) 166:2484–9. doi: 10.1001/archinte.166.22.2484
35. Kotsopoulos J, Librach CL, Lubinski J, Gronwald J, Kim-Sing C, Ghadirian P, et al. Infertility, treatment of infertility, and the risk of breast cancer among women with BRCA1 and BRCA2 mutations: a case–control study. Cancer Causes Control. (2008) 19:1111–9. doi: 10.1007/s10552-008-9175-0
36. Ricci E, Parazzini F, Negri E, Marsico S, La Vecchia C. Fertility drugs and the risk of breast cancer. Human Reprod. (1999) 14:1653–5. doi: 10.1093/humrep/14.6.1653
37. Braga C, Negri E, La Vecchia C, Parazzini F, Dal Maso L, Franceschi S. Fertility treatment and risk of breast cancer. Hum Reprod. (1996) 11:300–3. doi: 10.1093/HUMREP/11.2.300
38. Bernstein L, Hanisch R, Sullivan-Halley J, Ross RK. Treatment with human chorionic gonadotropin and risk of breast cancer. Cancer Epidemiol Biomark Prevent. (1995) 4:437–40.
39. Gauthier E, Paoletti X, Clavel-Chapelon F. Breast cancer risk associated with being treated for infertility: results from the French E3N cohort study. Hum Reprod. (2004) 19:2216–21. doi: 10.1093/humrep/deh422
40. Jensen A, Sharif H, Svare EI, Frederiksen K, Kjaer SK. Risk of breast cancer after exposure to fertility drugs: results from a large Danish cohort study. Cancer Epidemiol Biomark Prevent. (2007) 16:1400–7. doi: 10.1158/1055-9965.EPI-07-0075
41. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. (2015) 65:87–108. doi: 10.3322/caac.21262
42. Rasmussen ELK, Hannibal CG, Dehlendorff C, Baandrup L, Junge J, Vang R, et al. Parity, infertility, oral contraceptives, and hormone replacement therapy and the risk of ovarian serous borderline tumors: a nationwide case-control study. Gynecol Oncol. (2017) 144:571–6. doi: 10.1016/j.ygyno.2017.01.002
43. Rodriguez C, Tatham LM, Calle EE, Thun MJ, Jacobs EJ, Heath CW Jr. Infertility and risk of fatal ovarian cancer in a prospective cohort of US women. Cancer Causes Control. (1998) 9:645–51. doi: 10.1023/A:1008845106869
44. Fathalla MF. Incessant ovulation–a factor in ovarian neoplasia? Lancet. (1971) 2:163. doi: 10.1016/S0140-6736(71)92335-X
45. Brinton LA, Lamb EJ, Moghissi KS, Scoccia B, Althuis MD, Mabie JE, et al. Ovarian cancer risk after the use of ovulation-stimulating drugs. Obstetr Gynecol. (2004) 103:1194–203. doi: 10.1097/01.AOG.0000128139.92313.74
46. Kessous R, Davidson E, Meirovitz M, Sergienko R, Sheiner E. The risk of female malignancies after fertility treatments: a cohort study with 25-year follow-up. J Cancer Res Clin Oncol. (2016) 142:287–93. doi: 10.1007/s00432-015-2035-x
47. Sanner K, Conner P, Bergfeldt K, Dickman P, Sundfeldt K, Bergh T, et al. Ovarian epithelial neoplasia after hormonal infertility treatment: long-term follow-up of a historical cohort in Sweden. Ferti Steril. (2009) 91:1152–8. doi: 10.1016/j.fertnstert.2008.01.073
48. dos Santos Silva I, Wark P, McCormack V, Mayer D, Overton C, Little V, et al. Ovulation-stimulation drugs and cancer risks: a long-term follow-up of a British cohort. Br J Cancer. (2009) 100:1824. doi: 10.1038/sj.bjc.6605086
49. Potashnik G, Lerner-Geva L, Genkin L, Chetrit A, Lunenfeld E, Porath A. Fertility drugs and the risk of breast and ovarian cancers: results of a long-term follow-up study. Fertil Steril. (1999) 71:853–9. doi: 10.1016/S0015-0282(99)00085-0
50. Venn A, Watson L, Lumley J, Gilles G, King C, Healy D. Breast and ovarian cancer incidence after infertility and in vitro fertilisation. Lancet. (1995) 346:995–1000. doi: 10.1016/S0140-6736(95)91687-3
51. Franceschi S, Vecchia CL, Negri E, Guarneri S, Montella M, Conti E, et al. Infertility: Fertility drugs and risk of epithelial ovarian cancer in Italy. Hum Reprod. (1994) 9:1673–5. doi: 10.1093/oxfordjournals.humrep.a138771
52. Parazzini F, Pelucchi C, Negri E, Franceschi S, Talamini R, Montella M, et al. Use of fertility drugs and risk of ovarian cancer. Hum Reprod. (2001) 16:1372–5. doi: 10.1093/humrep/16.1.196-a
53. Trabert B, Lamb EJ, Scoccia B, Moghissi KS, Westhoff CL, Niwa S, et al. Ovulation-inducing drugs and ovarian cancer risk: results from an extended follow-up of a large United States infertility cohort. Fertil Steril. (2013) 100:1660–6. doi: 10.1016/j.fertnstert.2013.08.008
54. Jensen A, Sharif H, Frederiksen K, Kjær SK. Use of fertility drugs and risk of ovarian cancer: danish population based cohort study. BMJ. (2009) 338:b249. doi: 10.1136/bmj.b249
55. Stewart LM, Holman CDAJ, Finn JC, Preen DB, Hart R. in vitro fertilization is associated with an increased risk of borderline ovarian tumours. Gynecol Oncol. (2013) 129:372–6. doi: 10.1016/j.ygyno.2013.01.027
56. Shushan A, Paltiel O, Iscovich J, Elchalal U, Peretz T, Schenker JG. Human menopausal gonadotropin and the risk of epithelial ovarian cancer. Fertil Steril. (1996) 65:13–8. doi: 10.1016/S0015-0282(16)58020-0
57. Rossing MA, Daling JR, Weiss NS, Moore DE, Self SG. Ovarian tumors in a cohort of infertile women. N Engl J Med. (1994) 331:771–6. doi: 10.1056/NEJM199409223311204
58. Mosgaard BJ, Lidegaard O, Kjaer SK, Schou G, Andersen AN. Ovarian stimulation and borderline ovarian tumors: a case-control study. Fertil Steril. (1998) 70:1049–55. doi: 10.1016/S0015-0282(98)00337-9
59. Bjørnholt SM, Kjaer SK, Nielsen TSS, Jensen A. Risk for borderline ovarian tumours after exposure to fertility drugs: results of a population-based cohort study. Hum Reprod. (2014) 30:222–31. doi: 10.1093/humrep/deu297
60. Cusidó M, Fábregas R, Barris S P, Escayola C, Barri PN. Ovulation induction treatment and risk of borderline ovarian tumors. Gynecol Endocrinol. (2007) 23:373–6. doi: 10.1080/09513590701350341
61. Gronwald J, Glass K, Rosen B, Karlan B, Tung N, Neuhausen SL, et al. Treatment of infertility does not increase the risk of ovarian cancer among women with a BRCA1 or BRCA2 mutation. Fertil Steril. (2016) 105:781–5. doi: 10.1016/j.fertnstert.2015.11.034
62. Lerner-Geva L, Geva E, Lessing J, Chetrit A, Modan B, Amit A. The possible association between in vitro fertilization treatments and cancer development. Int J Gynecol Cancer. (2003) 13:23–7. doi: 10.1136/ijgc-00009577-200301000-00004
63. van Leeuwen FE, Klip H, Mooij TM, van de Swaluw AM, Lambalk CB, Kortman M, et al. Risk of borderline and invasive ovarian tumours after ovarian stimulation for in vitro fertilization in a large Dutch cohort. Hum Reprod. (2011) 26:3456–65. doi: 10.1093/humrep/der322
64. Ness RB, Cramer DW, Goodman MT, Kjaer SK, Mallin K, Mosgaard BJ, et al. Infertility, fertility drugs, and ovarian cancer: a pooled analysis of case-control studies. Am J Epidemiol. (2002) 155:217–24. doi: 10.1093/aje/155.3.217
65. Louis LS, Saso S, Ghaem-Maghami S, Abdalla H, Smith JR. The relationship between infertility treatment and cancer including gynaecological cancers. Obstetr Gynaecol. (2013) 15:177–83. doi: 10.1111/tog.12040
66. Brinton LA, Westhoff CL, Scoccia B, Lamb EJ, Althuis MD, Mabie JE, et al. Causes of infertility as predictors of subsequent cancer risk. Epidemiology. (2005) 16:500–7. doi: 10.1097/01.ede.0000164812.02181.d5
67. Parazzini F, Pelucchi C, Talamini R, Montella M, La Vecchia C. Use of fertility drugs and risk of endometrial cancer in an Italian case–control study. Eur J Cancer Prevent. (2010) 19:428–30. doi: 10.1097/CEJ.0b013e32833d9388
68. Benshushan A, Paltiel O, Brzezinski A, Tanos V, Barchana M, Shoshani O, et al. Ovulation induction and risk of endometrial cancer: a pilot study. Eur J Obstet Gynecol Reprod Biol. (2001) 98:53–7. doi: 10.1016/S0301-2115(01)00344-X
69. Althuis MD, Moghissi KS, Westhoff CL, Scoccia B, Lamb EJ, Lubin JH, et al. Uterine cancer after use of clomiphene citrate to induce ovulation. Am J Epidemiol. (2005) 161:607–15. doi: 10.1093/aje/kwi084
70. Jensen A, Sharif H, Kjaer SK. Use of fertility drugs and risk of uterine cancer: results from a large Danish population-based cohort study. Am J Epidemiol. (2009) 170:1408–14. doi: 10.1093/aje/kwp290
71. Hannibal CG, Jensen A, Sharif H, Kjaer SK. Risk of thyroid cancer after exposure to fertility drugs: results from a large Danish cohort study. Hum Reprod. (2007) 23:451–6. doi: 10.1093/humrep/dem381
72. Brinton LA, Moghissi KS, Scoccia B, Lamb EJ, Trabert B, Niwa S, et al. Effects of fertility drugs on cancers other than breast and gynecologic malignancies. Fertil Steril. (2015) 104:980–8. doi: 10.1016/j.fertnstert.2015.06.045
73. Althuis MD, Scoccia B, Lamb EJ, Moghissi KS, Westhoff CL, Mabie JE, et al. Melanoma, thyroid, cervical, and colon cancer risk after use of fertility drugs. Am J Obstet Gynecol. (2005) 193:668–74. doi: 10.1016/j.ajog.2005.01.091
74. Pazaitou-Panayiotou K, Toulis K, Mandanas S, Tarlatzis B. Thyroid cancer after in vitro fertilization: a retrospective, non-consecutive case-series analysis. Gynecol Endocrinol. (2014) 30:569–72. doi: 10.3109/09513590.2014.907258
75. Pakzad R, Ghoncheh M, Pournamdar Z, Pakzad I, Momenimovahed Z, Salehiniya H, et al. Spatial analysis of skin cancer incidence in Iran. Asian Pacific J Cancer Prevent. (2016) 17:33–7. doi: 10.7314/APJCP.2016.17.S3.33
76. Feskanich D, Hunter D, Willett W, Spiegelman D, Stampfer M, Speizer F, et al. Oral contraceptive use and risk of melanoma in premenopausal women. Br J Cancer. (1999) 81:918. doi: 10.1038/sj.bjc.6690787
77. Beral V, Evans S, Shaw H, Milton G. Oral contraceptive use and malignant melanoma in Australia. Br J Cancer. (1984) 50:681. doi: 10.1038/bjc.1984.236
78. Yli-Kuha A-N, Gissler M, Klemetti R, Luoto R, Hemminki E. Cancer morbidity in a cohort of 9175 Finnish women treated for infertility. Hum Reprod. (2012) 27:1149–55. doi: 10.1093/humrep/des031
79. Young P, Purdie D, Jackman L, Molloy D, Green A. A study of infertility treatment and melanoma. Melanoma Res. (2001) 11:535–41. doi: 10.1097/00008390-200110000-00015
80. Brinton LA, Melton LJ III, Malkasian GD Jr, Bond A, Hoover R. Cancer risk after evaluation for infertility. Am J Epidemiol. (1989) 129:712–22. doi: 10.1093/oxfordjournals.aje.a115186
81. Spaan M, Van Den Belt-dusebout AW, Burger CW, van Leeuwen FE, Schats R, Lambalk C, et al. Risk of colorectal cancer after ovarian stimulation for in vitro fertilization. Clin Gastroenterol Hepatol. (2016) 14:729–37. e5. doi: 10.1016/j.cgh.2015.12.018
82. Campbell PT, Newcomb P, Gallinger S, Cotterchio M, McLaughlin JR. Exogenous hormones and colorectal cancer risk in Canada: associations stratified by clinically defined familial risk of cancer. Cancer Causes Control. (2007) 18:723–33. doi: 10.1007/s10552-007-9015-7
83. Momenimovahed Z, Salehiniya H. Incidence, mortality and risk factors of cervical cancer in the world. Biomed Res Ther. (2017) 4:1795–811. doi: 10.15419/bmrat.v4i12.386
84. Kallen B, Finnstrom O, Lindam A, Nilsson E, Nygren KG, Olausson PO. Malignancies among women who gave birth after in vitro fertilization. Hum Reprod. (2011) 26:253–8. doi: 10.1093/humrep/deq307
85. Modan B, Ron E, Lerner-Geva L, Blumstein T, Menczer J, Rabinovici J, et al. Cancer incidence in a cohort of infertile women. Am J Epidemiol. (1998) 147:1038–42. doi: 10.1093/oxfordjournals.aje.a009397
86. Doyle P, Maconochie N, Beral V, Swerdlow AJ, Tan SL. Cancer incidence following treatment for infertility at a clinic in the UK. Hum Reprod. (2002) 17:2209–13. doi: 10.1093/humrep/17.8.2209
87. Stewart LM, Holman CAJ, Aboagye-Sarfo P, Finn JC, Preen DB, Hart R. in vitro fertilization, endometriosis, nulliparity and ovarian cancer risk. Gynecol Oncol. (2013) 128:260–4. doi: 10.1016/j.ygyno.2012.10.023
88. Moleti M, Sturniolo G, Di Mauro M, Russo M, Vermiglio F. Female reproductive factors and differentiated thyroid cancer. Front Endocrinol. (2017) 8:111. doi: 10.3389/fendo.2017.00111
89. Orgeas CC, Sanner K, Hall P, Conner P, Holte J, Nilsson SJ, et al. Breast cancer incidence after hormonal infertility treatment in Sweden: a cohort study. Am J Obstet Gynecol. (2009) 200:72.e1–7. doi: 10.1016/j.ajog.2008.08.066
90. Lundberg FE, Iliadou AN, Rodriguez-Wallberg K, Bergh C, Gemzell-Danielsson K, Johansson AL. Ovarian stimulation and risk of breast cancer in Swedish women. Fertil Steril. (2017) 108:137–44. doi: 10.1016/j.fertnstert.2017.05.010
91. Kristiansson P, Björ O, Wramsby H. Tumour incidence in Swedish women who gave birth following Ivf treatment. Hum Reprod. (2007) 22:421–6. doi: 10.1093/humrep/del411
Keywords: infertility, ovulation induction, cancer, infertility treatment, controlled ovarian stimulation, fertility agents, neoplasms
Citation: Momenimovahed Z, Taheri S, Tiznobaik A and Salehiniya H (2019) Do the Fertility Drugs Increase the Risk of Cancer? A Review Study. Front. Endocrinol. 10:313. doi: 10.3389/fendo.2019.00313
Received: 08 December 2018; Accepted: 30 April 2019;
Published: 24 May 2019.
Edited by:
Leif Johan Bungum, IVI Middle East Fertility Clinic LLC, United Arab EmiratesReviewed by:
Livio Casarini, University of Modena and Reggio Emilia, ItalyHakan Yarali, Anatolia IVF Center, Turkey
Copyright © 2019 Momenimovahed, Taheri, Tiznobaik and Salehiniya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hamid Salehiniya, YWxlc2FsZWg3MEB5YWhvby5jb20=
 Zohre Momenimovahed
Zohre Momenimovahed Safoura Taheri3
Safoura Taheri3 Hamid Salehiniya
Hamid Salehiniya