- Department of Radiation Therapy and Radio-oncology, University of Leipzig, Leipzig, Germany
Radiation therapy is a cornerstone in the therapeutic management of craniopharyngioma. The close proximity to neighboring eloquent structures pose a particular challenge to radiation therapy. Modern treatment technologies including fractionated 3-D conformal radiotherapy, intensity modulated radiation therapy, and recently proton therapy are able to precisely cover the target while preserving surrounding tissue, Tumor controls between 80 and in access of 90% can be achieved. Alternative treatments consisting of radiosurgery, intracavitary application of isotopes, and brachytherapy also offer an acceptable tumor control and might be given in selected cases. More research is needed to establish the role of each treatment modality.
Introduction
Surgery and radiotherapy are the cornerstones in therapeutic management of craniopharyngioma. Radical excision is associated with a risk of mortality or morbidity particularly as hypothalamic damage, visual deterioration, and endocrine complication between 45 and 90% of cases. By contrast, recurrent disease after partial excision alone is observed between in 50 and 91% (Becker et al., 1999). Today less radical surgery in combination with radiation therapy are favored achieving a progression-free survival between 70 and 90% (Fahlbusch et al., 1999; Chiou et al., 2001; Tomita and Bowman, 2005).
New technologies are currently under investigation to achieve a better balance between tumor control and the risk for hazardous effects for surrounding eloquent structures such as the pituitary gland, hypothalamus, optic apparatus, and arteries at the base of the skull.
Role of Radiotherapy/Conventional Technologies
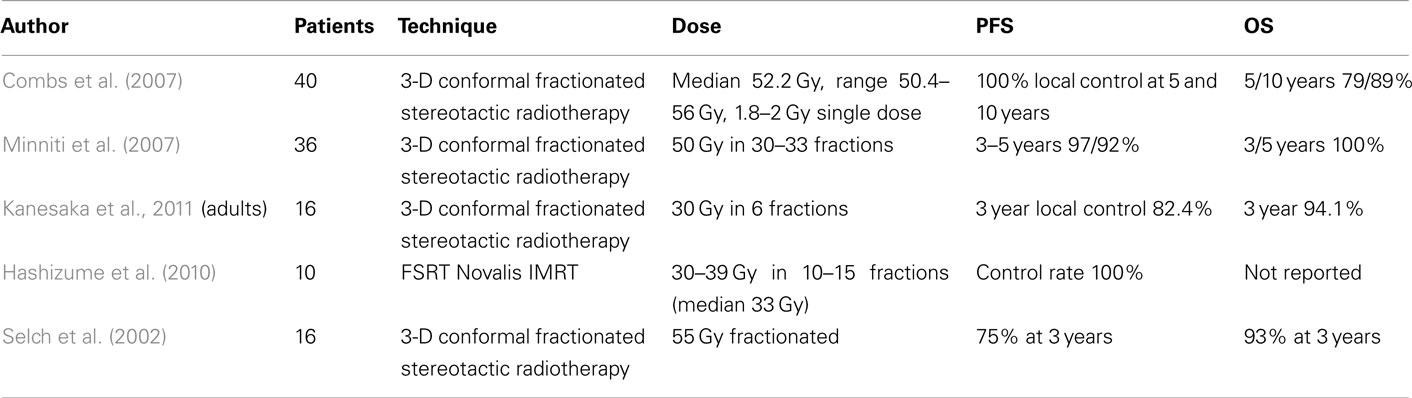
External fractionated radiotherapy is presently standard of care to achieve an optimal progression-free survival after non-radical excision (Wen et al., 1989; Hetelekidis et al., 1993; Merchant et al., 2002; Stripp et al., 2004; Karavitaki et al., 2005; Lin et al., 2008). An excellent long-term outcome of conventional radiotherapy was found in many retrospective series reporting 10 and 20 years progression-free survival up to 95 and 54% (Table 1).
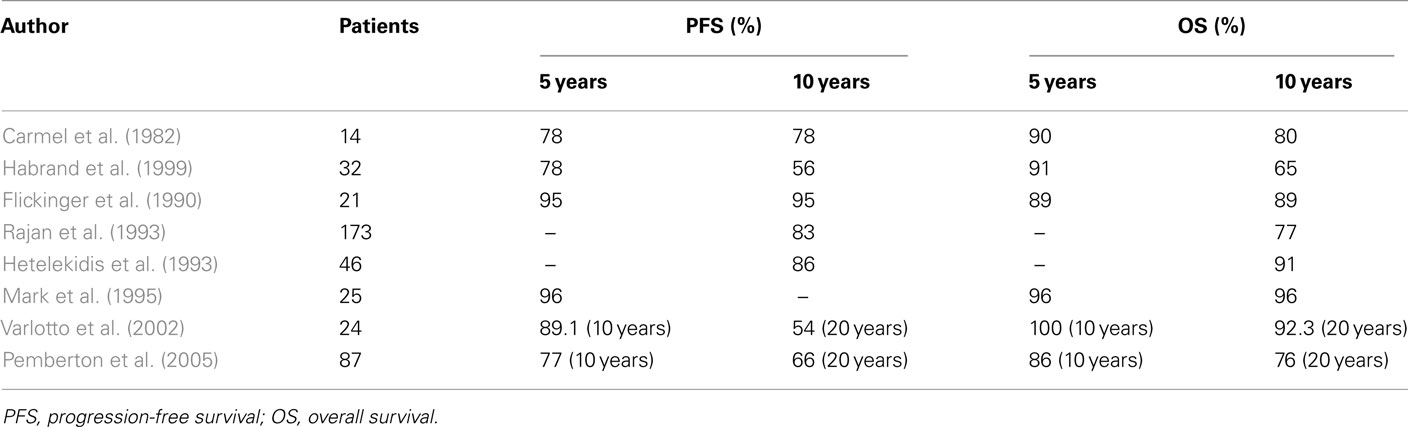
Table 1. Post-operative radiotherapy in craniopharyngioma/conventional techniques (tumor control and survival).
Modern Technologies in Radiation Therapy
Advances in radiation therapy technologies have opened up new approaches in the radio-oncological management of craniopharyngioma. The selection of the adequate treatment technology is of ongoing debate.
Fractionated Conformal Radiotherapy/Intensity Modulated Radiation Therapy
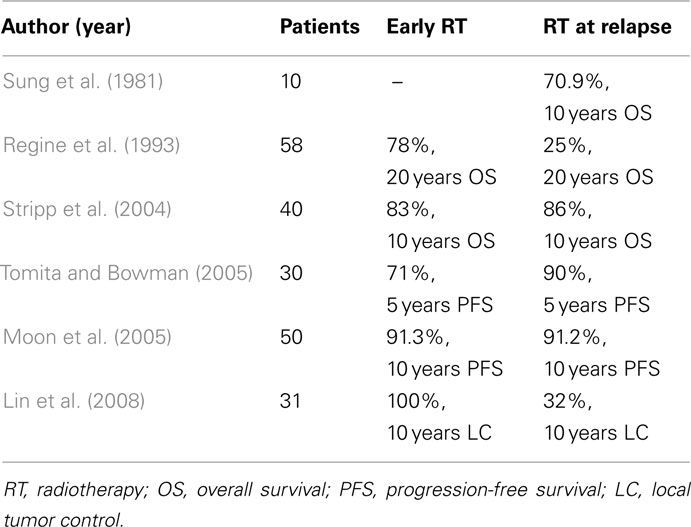
With the use of modern imaging technologies and treatment planning systems a precise coverage of the tumor area can be achieved by using stereotactic irradiation technologies. Stereotactic irradiation can be given in a single dose as stereotactic radiosurgery or in multiple doses as fractionated stereotactic radiotherapy. The modern systems permit an exact calculation of dose distribution within the tumor and provide a steeper dose gradient to surrounding normal tissue. If a cystic component is present, careful monitoring during radiotherapy is necessary (Winkfield et al., 2009). The results are shown in Table 2.
Proton Therapy
The major advantage of proton therapy is the high degree of dose conformity to the target. Beltran et al. (2011) retrospectively evaluated proton treatment plans with IMRT plan. He concluded that compared with photon IMRT proton therapy has the potential to significantly reduce whole brain and body irradiation. Fitzek et al. treated 15 patients with craniopharyngioma with a mix of photon and protons. The tumor control rates at 5 and 10 years were 93 and 85%, respectively (Fitzek et al., 2006). Luu et al. (2006) treated 16 patients. Local control could be achieved in 14 of 15 patients (Luu et al., 2006).
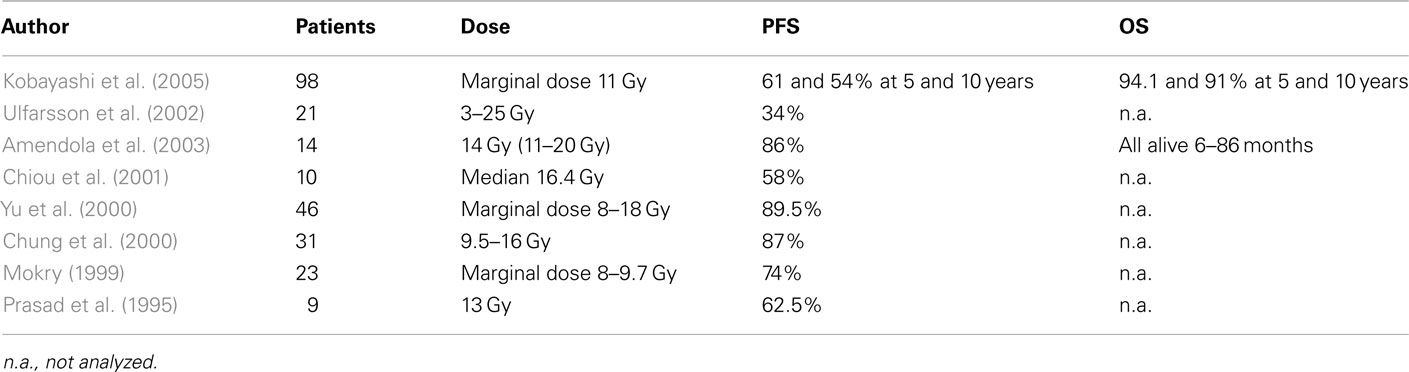
Timing of Radiation Therapy
Often immediate post-operative radiation therapy is favored in order to obviate early tumor progression leading to a functional deterioration caused by tumor growth or the necessity for repeat surgery. Others favor a watch-and-wait strategy fearing the long-term adverse effects of radiation therapy. The recent series of Stripp et al. (2004), Tomita and Bowman (2005), and Moon et al. (2005) showed no differences between progression-free and overall survival between the different approaches (Table 3). However, in the recent series of Lin et al. (2008) early radiation therapy yielded a 100% local control rate at 10 years as compared with 32% when radiation therapy was performed at relapse.
Other Technologies
Radiosurgery
Stereotactic radiosurgery is an alternative to fractionated treatments in patients with craniopharyngioma harboring smaller lesions. The reported results of radiosurgery, however, suggest that tumor control is inferior to fractionated treatments and might carry the risk for optic neuropathies unless only smaller lesions are treated away from the optic apparatus (Tishler et al., 1993). Minniti et al. (2009) reviewed eight published series and found an average tumor control rate of 90% for solid tumors, 88% for cystic tumors, and 60% for mixed tumors (Table 4).
CyberKnife
CyberKnife includes a compact linear accelerator mounted on a robotic arm combined with the pair of diagnostic X-ray sources permitting an online reproducibility of the incident beams and a subsequent adjustment of the beam with a precision below 1 mm. Lee et al. reported results obtained in 16 patients treated for residual recurrent craniopharyngioma Tumor shrinkage was achieved in 7 of these 11 patients and tumor control in another 3 patients. The overall tumor control was achieved in 91% of patients without complications (Lee et al., 2008).
Interstitial Brachytherapy
There is one report from Barlas et al. (2000) in two patients in whom iodine125-seeds were implanted delivering a dose of 67 and 60 Gy to tumor periphery. Response was partially observed in one and tumor completely resolved in the other patient 24 months after treatment. Radiation induced toxicity or recurrence has not been reported 6 years after treatment.
Intracavitary Application of Isotopes
Approximately 90% of craniopharyngioma display a cystic component often leading to a space occupying clinically relevant effect. There are different series reporting on the intracavitary application of different isotopes such as Rhenium186, Yttrium90, or Phosporus32. The nuclides emit β-rays with a therapeutic range within only a few millimeters. Response rates and cyst controls can be achieved in more than 80% of case. Tumors with a solid component, however, are insufficiently controlled (Voges et al., 1997; Hasegawa et al., 2004). Deterioration of visual function due to ionizing irradiation of the nuclides can occur (Table 5).
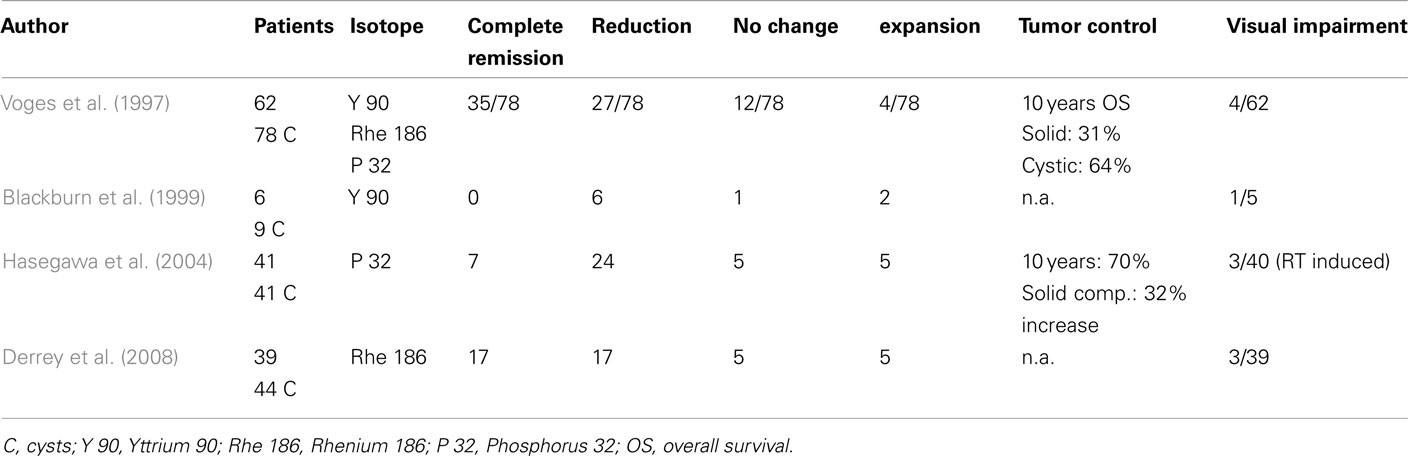
Table 5. Intracavitary instillation of radionuclides/impact on tumor control and visual function (modified according to Derrey et al., 2008).
Conclusion
Standard treatments today consist of fractionated external irradiation therapy. The recent developments in modern treatment technologies permit an exact delineation of target and non-target surrounding normal tissue (Merchant et al., 2006). Tumor control and overall survival might be improved as compared with the excellent results obtained with conventional treatments at shorter follow-up periods. Longer follow-up periods, however, are warranted. Today the 5-year progression-free survival after modern fractionated irradiation is in the range between 80 and 100%. Good results are achieved with a combined approach (surgery + radiation therapy) using standard fractionation. The recently introduced proton therapy opens up the possibility for a better sparing of normal surrounding tissue. Presently data are, however, limited and the expected improvement of functional outcome remains yet to be proven.
Post-operative radiation therapy is superior to surveillance after non-radical resection in terms of progression-free survival. The impact of different timing on functional outcome is still unknown. The current prospective German study Craniopharyngioma 2007 is addressing this issue in a randomized prospective study.
Radiosurgery as an option for circumscribed small lesions away from the optic apparatus is an attractive option because normal surrounding tissue is excellently spared. Single dose radiotherapy is, however, associated with an inferior tumor control according to retrospective data. CyberKnife as a new technological development utilizing image guided high precision stereotactic radiotherapy is able to use the radiobiologically advantageous fractionation concept. Interstitial treatments like the intracystic application of radioactive colloids might be used in selected cases in which only cystic tumors are present. It is, however, more a historical experience and should not be favored in the area of modern treatment technologies. Brachytherapy is of limited importance and the experiences so far obtained are very scarce. Minimizing the dose to non-target tissue will be the future step to reduce the risk for late effects. Reproducible data in prospective settings including neurocognitive function, quality of life, visual, and endocrinological function are still missing and require further research and evaluation. Table 6 gives an overview of the current technologies.
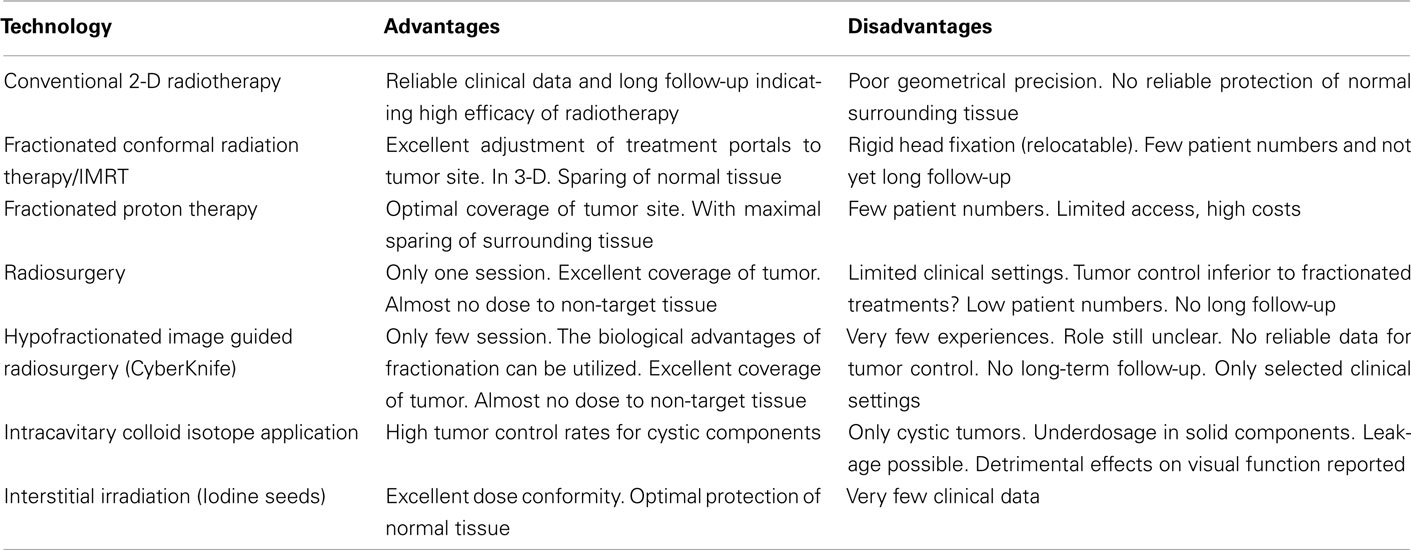
Table 6. Advantages and disadvantages of modern treatment technologies in radiotherapy of craniopharyngioma.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Amendola, B. E., Wolf, A., Coy, S. R., and Amendola, M. A. (2003). Role of radiosurgery in craniopharyngiomas: a preliminary report. Med. Pediatr. Oncol. 41, 123–127.
Barlas, O., Bayindir, C., and Can, M. (2000). Interstitial irradiation for craniopharyngioma. Acta Neurochir. (Wien) 142, 389–395.
Becker, G., Kortmann, R. D., Skalej, M., and Bamberg, M. (1999). The role of radiotherapy in the treatment of craniopharyngioma – indications, results, side effects. Front. Radiat. Ther. Oncol. 33, 100–113.
Beltran, C., Roca, M., and Merchant, T. E. (2011). On the benefits and risks of proton therapy in pediatric craniopharyngioma. Int. J. Radiat. Oncol. Biol. Phys. [Epub ahead of print].
Blackburn, T. P., Doughty, D., and Plowman, P. N. (1999). Stereotactic intracavitary therapy of recurrent cystic craniopharyngioma by instillation of 90yttrium. Br. J. Neurosurg. 13, 359–365.
Carmel, P. W., Antunes, J. L., and Chang, C. H. (1982). Craniopharyngiomas in children. Neurosurgery 11, 382–389.
Chiou, S. M., Lunsford, L. D., Niranjan, A., Kondziolka, D., and Flickinger, J. C. (2001). Stereotactic radiosurgery of residual or recurrent craniopharyngioma, after surgery, with or without radiation therapy. Neuro-oncology 3, 159–166.
Chung, W. Y., Pan, D. H., Shiau, C. Y., Guo, W. Y., and Wang, L. W. (2000). Gamma knife radiosurgery for craniopharyngiomas. J. Neurosurg. 93(Suppl. 3), 47–56.
Combs, S. E., Thilmann, C., Huber, P. E., Hoess, A., Debus, J., and Schulz-Ertner, D. (2007). Achievement of long-term local control in patients with craniopharyngiomas using high precision stereotactic radiotherapy. Cancer 109, 2308–2314.
Derrey, S., Blond, S., Reyns, N., Touzet, G., Carpentier, P., Gauthier, H., and Dhellemmes, P. (2008). Management of cystic craniopharyngiomas with stereotactic endocavitary irradiation using colloidal 186Re: a retrospective study of 48 consecutive patients. Neurosurgery 63, 1045–1052; discussion 1052–1053.
Fahlbusch, R., Honegger, J., Paulus, W., Huk, W., and Buchfelder, M. (1999). Surgical treatment of craniopharyngiomas: experience with 168 patients. J. Neurosurg. 90, 237–250.
Fitzek, M. M., Linggood, R. M., Adams, J., and Munzenrider, J. E. (2006). Combined proton and photon irradiation for craniopharyngioma: long-term results of the early cohort of patients treated at Harvard Cyclotron Laboratory and Massachusetts General Hospital. Int. J. Radiat. Oncol. Biol. Phys. 64, 1348–1354.
Flickinger, J. C., Lunsford, L. D., Singer, J., Cano, E. R., and Deutsch, M. (1990). Megavoltage external beam irradiation of craniopharyngiomas: analysis of tumor control and morbidity. Int. J. Radiat. Oncol. Biol. Phys. 19, 117–122.
Habrand, J. L., Ganry, O., Couanet, D., Rouxel, V., Levy-Piedbois, C., Pierre-Kahn, A., and Kalifa, C. (1999). The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int. J. Radiat. Oncol. Biol. Phys. 44, 255–263.
Hasegawa, T., Kondziolka, D., Hadjipanayis, C. G., and Lunsford, L. D. (2004). Management of cystic craniopharyngiomas with phosphorus-32 intracavitary irradiation. Neurosurgery 54, 813–822.
Hashizume, C., Mori, Y., Kobayashi, T., Shibamoto, Y., Nagai, A., and Hayashi, N. (2010). Stereotactic radiotherapy using Novalis for craniopharyngioma adjacent to optic pathways. J. Neurooncol. 98, 239–247.
Hetelekidis, S., Barnes, P. D., Tao, M. L., Fischer, E. G., Schneider, L., Scott, R. M., and Tarbell, N. J. (1993). 20-Year experience in childhood craniopharyngioma. Int. J. Radiat. Oncol. Biol. Phys. 27, 189–195.
Kanesaka, N., Mikami, R., Nakayama, H., Nogi, S., Tajima, Y., Nakajima, N., Wada, J., Miki, T., Haraoka, J., Okubo, M., Sugahara, S., and Tokuuye, K. (2011). Preliminary results of fractionated stereotactic radiotherapy after cyst drainage for craniopharyngioma in adults. Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2011.05.014. [Epub ahead of print].
Karavitaki, N., Brufani, C., Warner, J. T., Adams, C. B., Richards, P., Ansorge, O., Shine, B., Turner, H. E., and Wass, J. A. (2005). Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin. Endocrinol. (Oxf.) 62, 397–409.
Kobayashi, T., Kida, Y., Mori, Y., and Hasegawa, T. (2005). Long-term results of gamma knife surgery for the treatment of craniopharyngioma in 98 consecutive cases. J. Neurosurg. 103(Suppl.), 482–488.
Lee, M., Kalani, M. Y., Cheshier, S., Gibbs, I. C., Adler, J. R., and Chang, S. D. (2008). Radiation therapy and CyberKnife radiosurgery in the management of craniopharyngiomas. Neurosurg. Focus 24, E4.
Lin, L. L., El Naqa, I., Leonard, J. R., Park, T. S., Hollander, A. S., Michalski, J. M., and Mansur, D. B. (2008). Long-term outcome in children treated for craniopharyngioma with and without radiotherapy. J. Neurosurg. Pediatr. 1, 126–130.
Luu, Q. T., Loredo, L. N., Archambeau, J. O., Yonemoto, L. T., Slater, J. M., and Slater, J. D. (2006). Fractionated proton radiation treatment for pediatric craniopharyngioma: preliminary report. Cancer J. 12, 155–159.
Mark, R. J., Lutge, W. R., Shimizu, K. T., Tran, L. M., Selch, M. T., and Parker, R. G. (1995). Craniopharyngioma: treatment in the CT and MR imaging era. Radiology 197, 195–198.
Merchant, T. E., Kiehna, E. N., Kun, L. E., Mulhern, R. K., Li, C., Xiong, X., Boop, F. A., and Sanford, R. A. (2006). Phase II trial of conformal radiation therapy for pediatric patients with craniopharyngioma and correlation of surgical factors and radiation dosimetry with change in cognitive function. J. Neurosurg. 104, 94–102.
Merchant, T. E., Kiehna, E. N., Sanford, R. A., Mulhern, R. K., Thompson, S. J., and Wilson, M. W. (2002). Craniopharyngioma: the St. Jude Children’s Research Hospital experience 1984–2001. Int. J. Radiat. Oncol. Biol. Phys. 53, 533–542.
Minniti, G., Esposito, V., Amichetti, M., and Enrici, R. M. (2009). The role of fractionated radiotherapy and radiosurgery in the management of patients with craniopharyngioma. Neurosurg. Rev. 32, 125–132.
Minniti, G., Saran, F., Traish, D., Soomal, R., Sardell, S., Gonsalves, A., Ashley, S., Warrington, J., Burke, K., Mosleh-Shirazi, A., and Brada, M. (2007). Fractionated stereotactic conformal radiotherapy following conservative surgery in the control of craniopharyngiomas. Radiother. Oncol. 82, 90–95.
Mokry, M. (1999). Craniopharyngiomas: a six year experience with Gamma Knife radiosurgery. Stereotact. Funct. Neurosurg. 72(Suppl. 1), 140–149.
Moon, S. H., Kim, I. H., Park, S. W., Kim, I., Hong, S., Park, C. I., Wang, K. C., and Cho, B. K. (2005). Early adjuvant radiotherapy toward long-term survival and better quality of life for craniopharyngiomas – a study in single institute. Childs Nerv. Syst. 21, 799–807.
Pemberton, L. S., Dougal, M., Magee, B., and Gattamaneni, H. R. (2005). Experience of external beam radiotherapy given adjuvantly or at relapse following surgery for craniopharyngioma. Radiother. Oncol. 77, 99–104.
Prasad, D., Steiner, M., and Steiner, L. (1995). Gamma knife surgery for craniopharyngioma. Acta Neurochir. (Wien) 134, 167–176.
Rajan, B., Ashley, S., Gorman, C., Jose, C. C., Horwich, A., Bloom, H. J., Marsh, H., and Brada, M. (1993). Craniopharyngioma – a long-term results following limited surgery and radiotherapy. Radiother. Oncol. 26, 1–10.
Regine, W. F., Mohiuddin, M., and Kramer, S. (1993). Long-term results of pediatric and adult craniopharyngiomas treated with combined surgery and radiation. Radiat. Oncol. 27, 13–21.
Selch, M. T., DeSalles, A. A., Wade, M., Lee, S. P., Solberg, T. D., Wallace, R. E., Ford, J. M., Rubino, G., Cabatan-Awang, C., and Withers, H. R. (2002). Initial clinical results of stereotactic radiotherapy for the treatment of craniopharyngiomas. Technol. Cancer Res. Treat. 1, 51–60.
Stripp, D. C., Maity, A., Janss, A. J., Belasco, J. B., Tochner, Z. A., Goldwein, J. W., Moshang, T., Rorke, L. B., Phillips, P. C., Sutton, L. N., and Shu, H. K. (2004). Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int. J. Radiat. Oncol. Biol. Phys. 58, 714–720.
Sung, D. I., Chang, C. H., and Harisiadis, L. (1981). Treatment results of craniopharyngiomas. Cancer 47, 847–852.
Tishler, R. B., Loeffler, J. S., Lunsford, L. D., Duma, C., Alexander, E. III, Kooy, H. M., and Flickinger, J. C. (1993). Tolerance of cranial nerves of the cavernous sinus to radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 27, 215–221.
Tomita, T., and Bowman, R. M. (2005). Craniopharyngiomas in children: surgical experience at Children’s Memorial Hospital. Childs Nerv. Syst. 21, 729–746.
Ulfarsson, E., Lindquist, C., Roberts, M., Rahn, T., Lindquist, M., Thoren, M., and Lippitz, B. (2002). Gamma knife radiosurgery for craniopharyngiomas: long-term results in the first Swedish patients. J. Neurosurg. 97(Suppl.), 613–622.
Varlotto, J. M., Flickinger, J. C., Kondziolka, D., Lunsford, L. D., and Deutsch, M. (2002). External beam irradiation of craniopharyngiomas: long-term analysis of tumor control and morbidity. Int. J. Radiat. Oncol. Biol. Phys. 54, 492–499.
Voges, J., Sturm, V., Lehrke, R., Treuer, H., Gauss, C., and Berthold, F. (1997). Cystic craniopharyngioma: long-term results after intracavitary irradiation with stereotactically applied colloidal beta-emitting radioactive sources. Neurosurgery 40, 263–270.
Wen, B. C., Hussey, D. H., Staples, J., Hitchon, P. W., Jani, S. K., Vigliotti, A. P., and Doornbos, J. F. (1989). A comparison of the roles of surgery and radiation therapy in the management of craniopharyngiomas. Int. J. Radiat. Oncol. Biol. Phys. 16, 17–24.
Winkfield, K. M., Linsenmeier, C., Yock, T. I., Grant, P. E., Yeap, B. Y., Butler, W. E., and Tarbell, N. J. (2009). Surveillance of craniopharyngioma cyst growth in children treated with proton radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 73, 716–721.
Keywords: craniopharyngioma, radiotherapy, post-operative
Citation: Kortmann R-D (2011) Different approaches in radiation therapy of craniopharyngioma. Front. Endocrin. 2:100. doi: 10.3389/fendo.2011.00100
Received: 29 July 2011;
Paper pending published: 07 September 2011;
Accepted: 28 November 2011;
Published online: 20 December 2011.
Edited by:
Hermann Lothar Mueller, Klinikum Oldenburg gGmbH, GermanyReviewed by:
Ya-Xiong Tao, Auburn University, USAFrederic Castinetti, Assistance Publique Hopitaux de Marseille, France
Alapetite Claire, Institut Curie, France
Copyright: © 2011 Kortmann. This is an open-access article distributed under the terms of the Creative Commons Attribution Non Commercial License, which permits non-commercial use, distribution, and reproduction in other forums, provided the original authors and source are credited.
*Correspondence: Rolf-Dieter Kortmann, Department of Radiation Therapy and Radio-oncology, University of Leipzig, Stephanstr. 9a, 04103 Leipzig, Germany. e-mail:cm9sZi1kaWV0ZXIua29ydG1hbm5AbWVkaXppbi51bmktbGVpcHppZy5kZQ==