- 1Independent Consultant, Sheffield, United Kingdom
- 2Safer Medicines Trust, Kingsbridge, United Kingdom
- 3Alliance for Human Relevant Science, London, United Kingdom
- 4Emulate Inc., Boston, MA, United States
- 5Department of Pharmacology and Therapeutics, Institute of Systems, Molecular and Integrative Biology, University of Liverpool, Liverpool, United Kingdom
- 6National Institute for Health Research (NIHR) Nottingham Biomedical Research Centre (BRC), Nottingham University Hospitals NHS Trust and the University of Nottingham, Nottingham, England, United Kingdom
- 7CN-BIO, Cambridge, United Kingdom
- 8Cyprotex, Kalamazoo, MI, United States
- 9School of Chemical, Materials and Biological Engineering (CMBE), University of Sheffield, Sheffield, United Kingdom
- 10Kirkstall Ltd, Sheffield, United Kingdom
- 11Animal Free Research UK, London, United Kingdom
- 12Independent Consultant, Macclesfield, United Kingdom
- 13The Physicians Committee, Washington, DC, United States
Predicting which drugs might have the potential to cause drug-induced liver injury (DILI) is highly complex and the current methods, 2D cell-based models and animal tests, are not sensitive enough to prevent some costly failures in clinical trials or to avoid all patient safety concerns for DILI post-market. Animal-based methods are hampered by important species differences in metabolism and adaptive immunity compared to humans and the standard 2D in vitro approaches have limited metabolic functionality and complexity. On 24 April 2023 the Alliance for Human Relevant Science (https://www.humanrelevantscience.org/) hosted a workshop at the Royal Society, London entitled Drug-Induced Liver Injury (DILI): Can Human-Focused Testing Improve Clinical Translation? The conclusion was that complex in vitro models (CIVMs) provide a significant step forward in the safety testing paradigm. This perspective article, written by the participants, builds on those discussions to provide a ‘state of play’ on liver CIVMs with recommendations for how to encourage their greater uptake by the pharmaceutical industry.
1 The importance of DILI
DILI is a multifactorial, potentially life-threatening adverse reaction to drugs and other chemicals (Fernandez-Checa et al., 2021). Patients typically present with non-specific symptoms such as weakness, poor appetite, nausea, abdominal pain, fever and may be hospitalised with jaundice and rash (Lu et al., 2016). The most severe and clinically concerning consequence of DILI is acute, life-threatening liver failure, which has a high fatality rate unless treated by liver transplantation. DILI is however associated with many hundreds of drugs that remain on the market, including well known painkillers, such as acetaminophen and diclofenac, antibiotics, such as amoxicillin-clavulanate and flucloxacillin, as well as many Chinese herbal medicines (Lu et al., 2016). DILI remains the most common cause of acute liver failure in Western countries (Torgersen et al., 2024), with acetaminophen overdose being responsible for 39% of all cases (Ostapowicz et al., 2002).
DILI is a leading reason for the failure of new drugs to obtain regulatory approval and for drug withdrawals post-market (Lee and Yoo, 2024). Redfern et al. (2010) found that DILI accounted for 13% of the safety reasons leading to failure in clinical trials. Since 2022 at least nine drugs were on clinical hold due to DILI risk (Jadalannagari and Ewart, 2024). In two separate large-scale reviews Onakpoya et al. (2016) and Siramshetty et al. (2016), found that hepatoxicity was the most common toxicity type responsible for the withdrawal of drugs from the market (18% and 21% of cases, respectively).
2 Challenges in predicting DILI
2.1 DILI mechanisms and clinical presentation
One of the major problems with predicting DILI in humans is that the underlying mechanisms are complex and are not fully understood (Weaver et al., 2020; Andrade et al., 2019). DILI has been classified traditionally into two types, direct (or intrinsic) and idiosyncratic (or iDILI). Intrinsic DILI is dose dependent and tends to have a rapid onset (typically within several days). Acetaminophen is the classic example of a drug that causes intrinsic DILI; it is safe when used at clinically approved doses but at excessive doses is metabolized within hepatocytes to a chemically reactive and cytotoxic intermediate. For the many hundreds of licensed drugs other than acetaminophen that cause DILI, the clinical presentation however is not overtly dose dependent, often has delayed onset (many weeks, or months) and is idiosyncratic (Andrade et al., 2019; Di Zeo-Sánchez et al., 2022). iDILI arises in patients given clinically approved drug doses and occurs very infrequently, due to a combination of chemical insults to liver cells plus susceptibility factors that arise only in some individuals. Chemical insults to liver cells may arise in multiple ways, which include chemically reactive metabolite formation, mitochondrial injury and/or bile salt accumulation within hepatocytes due to inhibition of the Bile Salt Export Pump (BSEP) (Kenna and Uetrecht, 2018). Numerous drug associations between iDILI risk and genetic polymorphisms in drug metabolizing enzymes and/or human leukocyte antigens (HLA) have been identified, as have adaptive immune responses and/or drug metabolites in susceptible patients (Daly, 2023; Aithal, 2019). In view of this, plus the low frequency and delayed onset of iDILI, it has been proposed that development of adaptive immune responses plays a key role in iDILI development (Kenna and Uetrecht, 2018; Andrade et al., 2019; Di Zeo-Sánchez et al., 2022) and the term immune-mediated or imDILI as a form of iDILI has begun to be used (Tasnim et al., 2021).
Genome-wide association studies have identified several gene variants associated with iDILI (Nicoletti et al., 2017) so screening patients for these gene variants post-market could reduce iDILI cases (Aithal and Grove, 2015). For example, Koido et al. (2020) developed a polygenic risk score (PRS) to predict the susceptibility to DILI in patients treated with various antibiotics. This was replicated in vitro using primary hepatocytes and stem cell-derived organoids from multiple donors with in silico screening then used to identify compounds that elicited transcriptomic signatures present in the hepatocytes from individuals with an elevated PRS. This is paving the way for a “polygenicity-in-a-dish” or a “village-in-a-dish” strategy that could be used prior to clinical trials to stratify patients into different risk categories (Neavin et al., 2023). However, because the incidence of iDILI is low for most drugs, currently pre-prescription genotyping is not considered cost-effective (Krantz et al., 2024).
2.2 Limitations of animal safety studies for DILI assessment
Whilst tests conducted in animals prior to clinical trials are reportedly good at correctly identifying drugs with low DILI risk, they are notoriously bad at identifying liver-toxic drugs as such. Indeed Ballet (2015), noted that “most compounds associated with iDILI give negative results in animal toxicology studies”. In other words, animal tests for DILI have high specificity and low sensitivity.
A large retrospective review by the pharmaceutical industry found that the positive concordance between liver toxicity in animal tests and human DILI in clinical trials was 55% (Olson et al., 2000). However, a more recent study by the industry found the positive concordance with human liver toxicities was only 33% (rats), 27% (dogs), and 50% (monkeys) (Monticello et al., 2017). The diabetic drug, troglitazone (Rezulin®) is an example of the consequences of the poor sensitivity of animal safety tests for the assessment of human iDILI risk. Troglitazone was withdrawn from the US market in 2000 after causing at least 89 patient cases of acute liver failure, of whom 78 died or needed a liver transplant (Graham et al., 2003). Animal safety tests prior to clinical trials of the drug presumably did not detect evidence of concerning liver adverse effects and subsequently published human and animal trials have also given inconsistent results, highlighting the difficulty in predicting iDILI even in humans and the need for a more mechanistic approach (Dirven et al., 2021).
One important reason for the poor human DILI predictivity of animal safety tests is likely to be the substantial differences in drug metabolism and disposition between animals and humans (Martignoni et al., 2006; O’Brien et al., 2004). These arise in part due to species-specific differences in expression of cytochromes P450 (CYPs) and other important drug metabolising enzymes, plus genetic variabilities in the human population (Bailey et al., 2014; Martignoni et al., 2006). Whilst ADME data can be used to select the most appropriate species for tests, this may not always be possible, for example Turpeinen et al. (2008), found significant variation in the profile of CYP activity between species, with rats being the most divergent from humans. Since the production of chemically reactive drug metabolites is an important DILI mechanism that may cause both intrinsic DILI (Weaver et al., 2020) and iDILI (Kenna and Uetrecht, 2018), animal-based safety tests may have limited value specifically for assessment of human DILI risk.
Species-specific differences in sensitivity to adverse effects of drug metabolites may also arise. Russomanno et al. (2023) used a systems approach to demonstrate that, despite being given the same burden of the acetaminophen metabolite, rats were far less sensitive than mice to liver injury caused by acetaminophen due to their more robust basal and adaptive stress response capacity. Species differences in drug transporters in the liver also have been identified, which can result in marked species differences in drug exposure within liver cells. Notably, deaths of clinical trial patients due to intrinsic DILI caused by the test anti-viral drug fialuridine were later linked to species differences in the equilibrative nucleoside transporter, which resulted in markedly higher mitochondrial drug exposure within hepatocytes in humans than in mice or rats (Lee et al., 2006).
Species variability in drug disposition may result in drug exposures in animal safety studies that are insufficient to enable reliable assessment of both intrinsic and iDILI (Di Zeo-Sánchez et al., 2022; Dirven et al., 2021; Ballet, 2015; Weaver et al., 2020). In addition, the restricted timescale of the animal repeat dose tests conducted prior to initial clinical trials (several weeks at most) is insufficient to explore risk of iDILI that may arise in susceptible humans only after many weeks or months (Olson et al., 2000; Ng et al., 2012). Species variability also has been observed in the sensitivity of the biomarkers that are used to assess DILI. Plasma levels of aminotransferase enzymes that are released from damaged cells are used routinely to detect injury to the hepatobiliary system in humans. However Olson et al. (2000), reported that these enzymes are relatively insensitive markers of DILI in animals.
The animals used in tests are genetically very similar (Le Bras, 2024) and so, even if there were not the species differences, there is not enough genetic variation in the animals to explore genetic variability as a DILI susceptibility factor (Ballet, 2015). Turpeinen et al. (2008) observed that the widest interindividual variability in liver microsomes was found in humans and monkeys. This lack of genetic variability is exacerbated by the necessarily small numbers of animals used in tests, which could therefore not be expected to explore risk of iDILI that may occur very infrequently in human patients (i.e. 1 in 10,000 patients for flucloxacillin) (Williams et al., 2013; Ballet, 2015).
3 From 2D to 3D: moving towards a more physiologically-relevant DILI model
3.1 Types of CIVM
Over the last 10 years, there has been a dramatic uptake in the use of in vitro methods in biomedical research and testing (Taylor et al., 2024). Technological developments have created more complex in vitro models (CIVMs), including spheroids, organoids, 3D tissues, organ-on-a-chip and microphysiological systems (MPS) (Ekert et al., 2020). The US Food and Drug Administration (FDA) IQ MPS Affiliate, under the umbrella of the Innovation and Quality (IQ) consortium of pharmaceutical and biotechnology companies, have defined CIVMs as “systems having a multi-cellular environment within a biopolymer or tissue-derived matrix, a 3D structure potentially including two or more of the following: mechanical factors such as stretch or perfusion (e.g., breathing, gut peristalsis, flow), incorporating primary or stem cell-derived cells, and/or including immune system components” (Baran et al., 2022).
The design of liver-focussed CIVMs can vary massively—from plate format and high-throughput to media circulation (single-pass, circulated) and cell source (e.g., cell line, primary, iPSC) (see review by Jadalannagari and Ewart (2024). For example, Emulate’s Liver-Chip microfluidic model includes primary human hepatocytes (PHHs) “sandwiched” with primary liver sinusoidal endothelial, stellate and Kupffer cells in an adjacent channel, separated by a porous membrane, with media flow (Ewart et al., 2022). CN-Bio’s PhysioMimixⓇ MPS platform includes PHH and Kupffer cells seeded into scaffolds to induce the formation of a liver sinusoid type structure, also with media flow (Novac et al., 2022). Cyprotex utilises ultra-low attachment plates for the formation of primary human liver microtissues (hLiMTs) consisting of primary human hepatocytes and non-parenchymal cell fractions in a static model (Walker et al., 2020).
3.2 Advantages of CIVMs beyond 2D cell-based models
CIVMs involve more complex designs, mimicking actual liver structure including 3D cultures with the aid of supportive environments such as scaffolds, fibroblasts and perfusion of media (Tasnim et al., 2021), making them more physiologically relevant than 2D models (Weaver et al., 2020; Bell et al., 2018). There is evidence that this leads to better predictive power; Proctor et al. (2017) reported higher sensitivity (52% compared to 33%) using the 3D In Sphero InSight™ Human Liver Microtissue system compared to a 2D PHH system. One reason for this might be that 3D cultures are more metabolically active and stable than 2D. This applies to cell lines such as HepaRG and HepG2 (Sison-Young et al., 2015) and PHHs (Donato et al., 2022; Proctor et al., 2017; Bell et al., 2018), which both lose their phenotype and metabolic functionality, for example, CYP450 activity, within days. The EU-funded ToxRisk project demonstrated that HepG2 cell lines shared only 7 out of 20 human liver specific pathways compared to 19 using 3D liver hLiMTs (Gupta et al., 2021). The National Toxicology Program (NTP) of National Institutes of Health (NIH) showed that HepaRG spheroids exhibit physiologically relevant levels of CYP activity and maintained a stable phenotype for at least 28 days in culture (Ramaiahgari et al., 2017). And CN-Bio’s PhysioMimixⓇ MPS platform of PHHs has been demonstrated to be capable of expressing CYP enzymes over 28 days (Novac et al., 2022). With functional lifespans of up to 4 weeks, CIVM systems are closer to mimicking clinical trial timescales (Walker et al., 2020) but do not yet provide an advantage in that respect over animal based non-clinical trial timescales. Furthermore, they produce key biomarkers of liver functionality, such as albumin, alanine transaminase (ALT) and urea, at levels greater than 2D models and comparable to those seen clinically (Baudy et al., 2020; Novac et al., 2022; Ewart et al., 2022).
Although the most abundant cell type in the liver is the hepatocytes, non-parenchymal cells (NPCs), which include Kupffer cells, hepatic stellate cells, and liver endothelial cells, account for 20% of the liver mass. Co-cultures of hepatocytes with these NPCs not only provide a more physiologically relevant system, but also stabilise the isolated heptaocyte phenotype, prolonging its longevity (Tasnim et al., 2021). Medium flow and oxygen transport generated by pumps (Wilkinson, 2023) also enhance the formation of liver organoid-like structures, increasing their lifespan (Ramachandren et al., 2015). This may arise by flow influencing the levels of extracellular matrix (ECM)-associated proteins which encourage the further development and differentiation of the organoid structure (Michielin, et al., 2020). Further development of CIVMs can bring the systems even closer to functional human livers. For example Tomlinson et al. (2019), replicated the three main zones along a liver sinusoid by elevating the cells to different heights within three chambers of the Quasi-VivoⓇ system effectively altering their exposure to oxygen levels corresponding to those found in vivo. They reported better functionality of the liver cells in the system as a result. The, inclusion of immune cells may also offer greater predictive power in view of the role of immune responses in iDILI but this is only just beginning to be explored by CIVM developers (Di Zeo-Sánchez et al., 2022). Any potential benefit by the inclusion of cholangiocytes (liver epithelial cells) in CIVMs has also not been yet fully explored. Furthermore, whilst there is, as with 2D models, the option to include PHHs or hLiMTs from many donors to address the genetic variability of iDILI, this is also not yet commonplace (Di Zeo- Sánchez et al., 2022).
3.3 Reproducibility and predictivity of CIVMs
There is growing evidence of the enhanced predictive capability of CIVMs (see Walker et al., 2020), including greater sensitivity, predicting DILI across many drugs that were considered safe in animal tests. Comparing the models fairly, however, is fraught with difficulty due to differences in their construction and liver cell components, including the number of donors, duration of exposures and endpoints. The IQ MPS Affiliate has helped by providing guidance on the best approaches to benchmark complex liver models, including key performance metrics and a list of 20 reference compounds (Baudy et al., 2020).
Although there are papers reporting aspects of model reproducibility (Rubiano et al., 2021; Lim et al., 2023; Eckstrum et al., 2022; Bell et al., 2018), it is still early days in terms of published evidence for the intra and inter laboratory reproducibility and predictivity of CIVMs using an agreed reference compound set (Di Zeo-Sánchez et al., 2022). To date only Emulate (Ewart et al., 2022) have published the sensitivity and specificity of their Liver-Chip using the IQ MPS Affiliate compounds plus an additional sub-set of drugs with a high DILI score that had not been detected in spheroids or animal tests. Emulate report a sensitivity of 87% and specificity of 100%, including the detection of troglitazone toxicity.
Several research groups are now proposing strategies to integrate CIVMs into the drug development pipeline alongside existing assays to improve prediction and reduce attrition, including the FDA (Ribeiro et al., 2019), the EU funded Innovative Medicines Initiative Mechanism-Based Integrated Systems for the Prediction of Drug-Induced Liver Injury (IMI MIP-DILI) (Weaver et al., 2020) and CIVM developers (Levner and Ewart, 2023; Walker et al., 2020).
4 The outlook for CIVMs
The evidence for the greater sensitivity of various CIVMs for the prediction of DILI compared to the current methods warrants their greater adoption. It has been estimated that the greater precision of models such as Emulate’s Liver-Chip would generate a $3 billion productivity gain for the pharmaceutical industry by identifying failing drug candidates earlier on in the pre-clinical process (Ewart et al., 2022). Their use would also be consistent with efforts in the US and Europe towards the full replacement of animal testing (see EC, 2023 and US Congress, 2022). Accelerating this need is the ever-increasing number of biological drugs being developed; over the last 10 years, the percentage of biologics approved by the FDA has increased from 16% in 2012 to 40% in 2022 (FDA, 2022). These new drug modalities, which include antibody, cell, and gene therapies, are generally highly specific for human genetic and protein sequences, necessitating the need for ever more human-relevant technologies for safety prediction.
However, a decade after their introduction, routine use of CIVMs by the pharmaceutical industry is still disappointingly limited (Jadalannagari and Ewart, 2024). We suggest three major reasons for this.
1. The fact that animals are used for other aspects of toxicity such that CIVMs used for DILI could only be a partial replacement for the required regulatory tests (scientific barrier).
2. Their relatively high cost, particularly upon set-up (economic barrier).
3. No clear way forward in terms of regulatory qualification (regulatory barrier).
We suggest some solutions to these economic, regulatory and scientific barriers in Table 1.
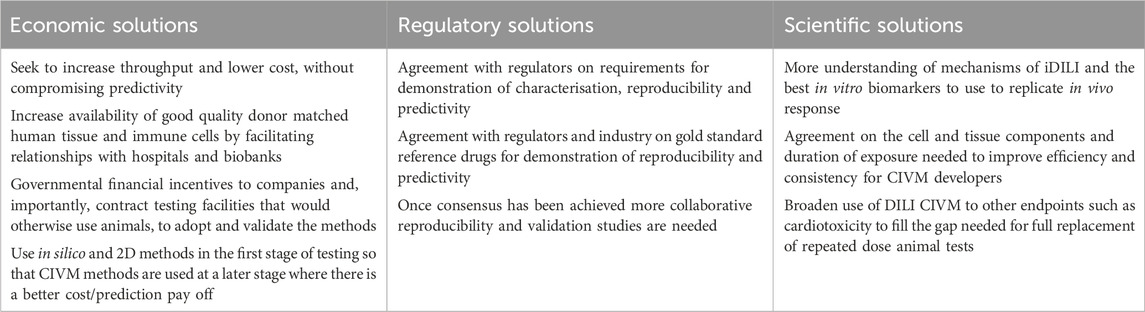
Table 1. Suggestions to address the economic, regulatory and scientific barriers limiting greater uptake of CIVMs.
Without characterisation and evidence of performance for a defined regulatory need, new methods will struggle to be approved by regulators and adopted by drug developers. A potential solution is continued cooperation between regulatory agencies and the pharmaceutical industry, academia, and developers to produce guidelines on the qualification of these methods (Ekert et al., 2020). There has been a workshop with the FDA and the IQ MPS Affiliate (Baran et al., 2022) and Emulate’s Liver-Chip has become the first organ-on-a-chip to be accepted into the Innovative Science and Technology Approaches for New Drugs (ISTAND) Pilot Program, receiving FDA support in the journey towards becoming a qualified Drug Development Tool (DDT) (FDA US Food and Drug Administration, 2024). This is a start but more collaboration and outputs—such as guidelines and agreed reference compound lists—are needed (Di Zeo-Sánchez et al., 2022).
We believe that economics will eventually be the driver of change in the pharmaceutical industry, especially as throughput increases and set-up costs decrease, but only after some of the scientific and regulatory barriers have been overcome. Unfortunately, since animal tests potentially address—albeit inadequately—toxicities in all organs, replacement of an animal test for DILI will not result in automatic replacement of the standard animal tests conducted to address drug safety, reducing the economic attractiveness of these alternative methods to drug companies. However, given the compelling evidence of their advanced physiological relevance to human livers and the growing evidence of their predictive power, there is never a better time to seriously consider their implementation in the standard drug testing paradigm.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
KT: Conceptualization, Investigation, Writing–original draft, Writing–review and editing. RR: Funding acquisition, Project administration, Writing–original draft, Writing–review and editing. LE: Writing–original draft, Writing–review and editing. CG: Writing–original draft, Writing–review and editing. GR: Writing–original draft, Writing–review and editing. GA: Writing–original draft, Writing–review and editing. TK: Writing–original draft, Writing–review and editing. CB: Writing–original draft, Writing–review and editing. JW: Writing–original draft, Writing–review and editing. SM: Writing–original draft, Writing–review and editing. JK: Conceptualization, Project administration, Writing–original draft, Writing–review and editing. JB: Conceptualization, Funding acquisition, Project administration, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The workshop was organised and funded by the Alliance for Human Relevant Science, London, UK. KT was funded by Alliance members: Replacing Animal Research (formerly FRAME), (Animal Free Research UK), Certara, The Humane Research Trust and CN-Bio to produce the initial draft of the paper. Certara was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Acknowledgments
Thanks to the remaining workshop presenters not named as authors; Bhumika Singh (Kirkstall Ltd.) and Mihael Polymeropoulos (Vanda Pharmaceuticals). Additional thanks to Ross Dobie (Animal Free Research UK) for comments on the draft. KT was funded by Alliance members: Replacing Animal Research (formerly FRAME), Animal Free Research United Kingdom, Certara, The Humane Research Trust and CN-Bio to produce the initial draft of the paper.
Conflict of interest
Author LE was employed by Emulate Inc. Author TK was employed by CN-BIO. Author CB was employed by Cyprotex. Author JW was employed by Kirkstall Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aithal, G. P. (2019). Of potions, poisons, polygonum and pre-emptive polymorphism. Hepatol. 70, 8–10. doi:10.1002/hep.30798
Aithal, G. P., and Grove, J. I. (2015). Genome-wide association studies in drug-induced liver injury: step change in understanding the pathogenesis. Semin. Liver Dis. 35, 421–431. doi:10.1055/s-0035-1567829
Andrade, R., Aithal, G., Björnsson, E., Kaplowitz, N., Kullak-Ublick, G., Larrey, D., et al. (2019). EASL clinical practice guidelines: drug-induced liver injury. J. Hepatol. 70, 1222–1261. doi:10.1016/j.jhep.2019.02.014
Bailey, J., Thew, M., and Balls, M. (2014). An analysis of the use of animal models in predicting human toxicology and drug safety. Altern. Laboratory Animals 42 (3), 181–199. doi:10.1177/026119291404200306
Ballet, F. (2015). Preventing drug-induced liver injury: how useful are animal models? Dig. Dis. 33, 477–485. doi:10.1159/000374093
Baran, S. W., Brown, P. C., Baudy, A. R., Fitzpatrick, S. C., Frantz, C., Fullerton, A., et al. (2022). Perspectives on the evaluation and adoption of complex in vitro models in drug development: workshop with the FDA and the pharmaceutical industry (IQ MPS Affiliate). ALTEX 39, 297–314. doi:10.14573/altex.2112203
Baudy, A. R., Otieno, M. A., Hewitt, P., Gan, J., Roth, A., Keller, D., et al. (2020). Liver microphysiological systems development guidelines for safety risk assessment in the pharmaceutical industry. Lab. Chip 20, 215–225. doi:10.1039/c9lc00768g
Bell, C. C., Dankers, A. C. A., Lauschke, V. M., Sison-Young, R., Jenkins, R., Rowe, C., et al. (2018). Comparison of hepatic 2D sandwich cultures and 3D spheroids for long-term toxicity applications: a multicenter study. Tox. Sci. 162, 655–666. doi:10.1093/toxsci/kfx289
Daly, A. K. (2023). Genetics of drug-induced liver injury: current knowledge and future prospects. Clin. Trans. Sci. 16, 37–42. doi:10.1111/cts.13424
Dirven, H., Vist, G. E., Bandhakavi, S., Mehta, J., Fitch, S. E., Pound, P., et al. (2021). Performance of preclinical models in predicting drug-induced liver injury in humans: a systematic review. Sci. Rep. 11, 6403. doi:10.1038/s41598-021-85708-2
Di Zeo-Sánchez, D. E., Segovia-Zafra, A., Matilla-Cabello, G., Pinazo-Bandera, J. M., Andrade, R. J., Lucena, M. I., et al. (2022). Modeling drug-induced liver injury: current status and future prospects. Expert Opin. Drug Metab. Toxicol. 18, 555–573. doi:10.1080/17425255.2022.2122810
Donato, M. T., Gallego-Ferrer, G., and Tolosa, L. (2022). In vitro models for studying chronic drug-induced liver injury. Int. J. Mol. Sci. 23, 11428. doi:10.3390/ijms231911428
EC. (2023). Communication from the commission on the European citizens’ initiative (ECI) save cruelty-free cosmetics – commit to a Europe without animal testing Brussels, 25.7.2023. C(2023) 5041 final.
Eckstrum, K., Striz, A., Ferguson, M., Zhao, Y., and Sprando, R. (2022). Evaluation of the utility of the beta human liver emulation system (BHLES) for CFSAN's regulatory toxicology program. Food Chem. Toxicol. 161, 112828. doi:10.1016/j.fct.2022.112828
Ekert, J. E., Deakyne, J., Pribul-Allen, P., Terry, R., Schofield, C., Jeong, C. G., et al. (2020). Recommended guidelines for developing, qualifying, and implementing complex in vitro models (CIVMs) for drug discovery. SLAS Discov. 25, 1174–1190. doi:10.1177/2472555220923332
Ewart, L., Apostolou, A., Briggs, S. A., Carman, C. V., Chaff, J. T., Heng, A. R., et al. (2022). Performance assessment and economic analysis of a human Liver-Chip for predictive toxicology. Commun. Med. 2, 154. doi:10.1038/s43856-022-00209-1
FDA (2022). New drug therapy approvals 2022. FDA statement 10 jan 2023. Available at: https://www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/new-drug-therapy-approvals-2022.
FDA, US Food and Drug Administration (2024). FDA's ISTAND Pilot Program accepts a submission of first organ-on-a-chip technology designed to predict human drug-induced liver injury (DILI). Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fdas-istand-pilot-program-accepts-submission-first-organ-chip-technology-designed-predict-human-drug.
Fernandez-Checa, F. C., Bagnaninchi, P., Ye, H., Sancho-Bru, P., Falcon-Perez, J. M., Royo, F., et al. (2021). Advanced preclinical models for evaluation of drug-induced liver injury – consensus statement by the European Drug-Induced Liver Injury Network [PRO-EURO-DILI-NET]. J. Hepatol. 75, 935–959. doi:10.1016/j.jhep.2021.06.021
Graham, D. J., Green, L., Senior, J. R., and Nourjah, P. (2003). Troglitazone-induced liver failure: a case study. Am. J. Med. 114, 299–306. doi:10.1016/s0002-9343(02)01529-2
Gupta, R., Schrooders, Y., Hauser, D., van Herwijnen, M., Albrecht, W., Ter Braak, B., et al. (2021). Comparing in vitro human liver models to in vivo human liver using RNA-Seq. Arch. Toxicol. 95, 573–589. doi:10.1007/s00204-020-02937-6
Jadalannagari, S., and Ewart, L. (2024). Beyond the hype and toward application: liver complex in vitro models in preclinical drug safety. Expert Opin. Drug Metab. Toxicol. 20, 607–619. doi:10.1080/17425255.2024.2328794
Kenna, J. G., and Uetrecht, J. (2018). Do in vitro assays predict drug candidate idiosyncratic drug-induced liver injury risk? Drug Metab. Dispos. 46, 1658–1669. doi:10.1124/dmd.118.082719
Koido, M., Kawakami, E., Fukumura, J., Noguchi, Y., Ohori, M., Nio, Y., et al. (2020). Polygenic architecture informs potential vulnerability to drug-induced liver injury. Nat. Med. 26, 1541–1548. doi:10.1038/s41591-020-1023-0
Krantz, M. S., Marks, M. E., and Phillips, E. J. (2024). The clinical application of genetic testing in DILI, are we there yet? Clin. Liver Dis. Hob. 23, e0218. doi:10.1097/CLD.0000000000000218
Lee, E. W., Lai, Y., Zhang, H., and Unadkatet, J. D. (2006). Identification of the mitochondrial targeting signal of the human equilibrative nucleoside transporter 1 (hENT1): implications for interspecies differences in mitochondrial toxicity of fialuridine. J. Biol. Chem. 281, 16700–16706. doi:10.1074/jbc.M513825200
Lee, S., and Yoo, S. (2024). InterDILI: interpretable prediction of drug-induced liver injury through permutation feature importance and attention mechanism. J. Cheminformat. 16, 1. doi:10.1186/s13321-023-00796-8
Levner, D., and Ewart, L. (2023). Integrating Liver-Chip data into pharmaceutical decision-making processes. Expert Opin. Drug Discov. 18, 1313–1320. doi:10.1080/17460441.2023.2255127
Lim, A. Y., Kato, Y., Sakolish, C., Valdiviezo, A., Han, G., Bajaj, P., et al. (2023). Reproducibility and robustness of a liver microphysiological system PhysioMimix LC12 under varying culture conditions and cell type combinations. Bioeng. (Basel). 10, 1195. doi:10.3390/bioengineering10101195
Lu, R. J., Zhang, Y., Tang, F. L., Zheng, Z. W., Fan, Z. D., Zhu, S. M., et al. (2016). Clinical characteristics of drug-induced liver injury and related risk factors. Exp. Ther. Med. 12, 2606–2616. doi:10.3892/etm.2016.3627
Martignoni, M., Groothuis, G. M. M., and de Kanter, R. (2006). Species differences between mouse, rat, dog, monkey and human CYP-mediated drug metabolism, inhibition and induction. Expert Opin. Drug Metab. Toxicol. 2, 875–894. doi:10.1517/17425255.2.6.875
Michielin, F., Giobbe, G. G., Luni, C., Hu, Q., Maroni, I., Orford, M. R., et al. (2020). The microfluidic environment reveals a hidden role of self-organizing extracellular matrix in hepatic commitment and organoid formation of hiPSCs. Cell Rep. 33, 108453. doi:10.1016/j.celrep.2020.108453
Monticello, T. M., Jones, T. W., Dambach, D. M., Potter, D. M., Bolt, M. W., Liu, M., et al. (2017). Current nonclinical testing paradigm enables safe entry to First-In-Human clinical trials: the IQ consortium nonclinical to clinical translational database. Toxicol. Appl. Pharmacol. 334, 100–109. doi:10.1016/j.taap.2017.09.006
Neavin, D. R., Steinmann, A. M., Farbehi, N., Chiu, H. S., Daniszewski, M. S., Arora, H., et al. (2023). A village in a dish model system for population-scale hiPSC studies. Nat. Commun. 14, 3240. doi:10.1038/s41467-023-38704-1
Ng, W., Lobach, A. R., Zhu, X., Chen, X., Liu, F., Metushi, I. G., et al. (2012). Animal models of idiosyncratic drug reactions. Adv. Pharmacol. 63, 81–135. doi:10.1016/B978-0-12-398339-8.00003-3
Nicoletti, P., Aithal, G. P., Bjornsson, E. S., Andrade, R. J., Sawle, A., Arrese, M., et al. (2017). Association of liver injury from specific drugs, or groups of drugs, with polymorphisms in HLA and other genes in a genome-wide association study. Gastroenterol. 152, 1078–1089. doi:10.1053/j.gastro.2016.12.016
Novac, O., Silva, R., Young, L. M., Lachani, K., Hughes, D., and Kostrzewski, T. (2022). Human liver microphysiological system for assessing drug-induced liver toxicity in vitro. J. Vis. Exp. 179. doi:10.3791/63389
O’Brien, P. J., Chan, K., and Silber, P. M. (2004). Human and animal hepatocytes in vitro with extrapolation in vivo. Chem. Biol. Interact. 150, 97–114. doi:10.1016/j.cbi.2004.09.003
Olson, H., Betton, G., Robinson, D., Thomas, K., Monro, A., Kolaja, G., et al. (2000). Concordance of the toxicity of pharmaceuticals in humans and in animals. Regul. Toxicol. Pharmacol. 32, 56–67. doi:10.1006/rtph.2000.1399
Onakpoya, I. J., Heneghan, C. J., and Aronson, J. K. (2016). Post-marketing withdrawal of 462 medicinal products because of adverse drug reactions: a systematic review of the world literature. BMC Med. 14, 10. doi:10.1186/s12916-016-0553-2
Ostapowicz, G., Fontana, R. J., Schiødt, F. V., Larson, A., Davern, T. J., Han, S. H., et al. (2002). Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann. Intern Med. 137, 947–954. doi:10.7326/0003-4819-137-12-200212170-00007
Proctor, W. R., Foster, A. J., Vogt, J., Summers, C., Middleton, B., Pilling, M. A., et al. (2017). Utility of spherical human liver microtissues for prediction of clinical drug-induced liver injury. Arch. Toxicol. 91, 2849–2863. doi:10.1007/s00204-017-2002-1
Ramachandran, S. D., Schirmer, K., Münst, B., Heinz, S., Ghafoory, S., Wölfl, S., et al. (2015). In vitro generation of functional liver organoid-like structures using adult human cells. PLoS One 10, e0139345. doi:10.1371/journal.pone.0139345
Ramaiahgari, S. C., Waidyanatha, S., Dixon, D., DeVito, M. J., Paules, R. S., and Ferguson, S. S. (2017). Three-dimensional (3D) HepaRG spheroid model with physiologically relevant xenobiotic metabolism competence and hepatocyte functionality for liver toxicity screening. Toxicol. Sci. 60, 189–190. doi:10.1093/toxsci/kfx122
Redfern, W. S., Ewart, L., Hammond, T. G., Bialecki, R., Kinter, L., Lindgren, S., et al. (2010). Impact and frequency of different toxicities throughout the pharmaceutical life cycle (abstract 1081). Toxicologist 114, 231.
Ribeiro, A. J. S., Yang, X., Patel, V., Madabushi, R., and Strauss, D. G. (2019). Liver microphysiological systems for predicting and evaluating drug effects. Clin. Pharmacol. Ther. 106, 139–147. doi:10.1002/cpt.1458
Rubiano, A., Indapurkar, A., Yokosawa, R., Miedzik, A., Rosenzweig, B., Arefin, A., et al. (2021). Characterizing the reproducibility in using a liver microphysiological system for assaying drug toxicity, metabolism, and accumulation. Clin. Transl. Sci. 14, 1049–1061. doi:10.1111/cts.12969
Russomanno, G., Sison-Young, R., Livoti, L. A., Coghlan, H., Jenkins, R. E., Kunnen, S. J., et al. (2023). A systems approach reveals species differences in hepatic stress response capacity. Toxicol. Sci. 196, 112–125. doi:10.1093/toxsci/kfad085
Siramshetty, V. B., Nickel, J., Omieczynski, C., Gohlke, B. O., Drwal, M. N., and Preissner, R. (2016). WITHDRAWN--a resource for withdrawn and discontinued drugs. Nucleic Acids Res. 44, D1080–D1086. doi:10.1093/nar/gkv1192
Sison-Young, R. L. C., Mitsa, D., Jenkins, R. E., Mottram, D., Alexandre, E., Richert, L., et al. (2015). Comparative proteomic characterization of 4 human liver-derived single cell culture models reveals significant variation in the capacity for drug disposition, bioactivation, and detoxication. Toxicol. Sci. 147, 412–424. doi:10.1093/toxsci/kfv136
Tasnim, F., Huang, X., Lee, C. Z. W., Ginhoux, F., and Yu, H. (2021). Recent advances in models of immune-mediated drug-induced liver injury. Front. Toxicol. 3, 605392. doi:10.3389/ftox.2021.605392
Taylor, K., Modi, S., and Bailey, J. (2024). An analysis of trends in the use of animal and non-animal methods in biomedical research and toxicology publications. Front. Lab. Chip Technol. 3. doi:10.3389/frlct.2024.1426895
Tomlinson, L., Hyndman, L., Firman, J. W., Bentley, R., Kyffin, J. A., Webb, S. D., et al. (2019). In vitro liver zonation of primary rat hepatocytes. Front. Bioeng. Biotechnol. Sec. Tissue Eng. Regen. Med. 7, 17. doi:10.3389/fbioe.2019.00017
Torgersen, J., Mezochow, A. K., Newcomb, C. W., Carbonari, D. M., Hennessy, S., Rentsch, C. T., et al. (2024). Severe acute liver injury after hepatotoxic medication initiation in real-world data. J. Am. Med. Assoc. Intern. Med. 184, 943–952. doi:10.1001/jamainternmed.2024.1836
Turpeinen, M., Ghiciuc, C., Opritoui, M., Tursas, L., Pelkonen, O., and Pasanen, M. (2008). Predictive value of animal models for human cytochrome P450 (CYP)-mediated metabolism: a comparative study in vitro. Xenobiotica 37, 1367–1377. doi:10.1080/00498250701658312
US Congress (2022). S.5002 - 117th congress (2021-2022): FDA modernization act 2.0. Available at: http://www.congress.gov/bill/117th-congress/senate-bill/5002/text.
Walker, P. A., Ryder, S., Lavado, A., Dilworth, C., and Riley, R. J. (2020). The evolution of strategies to minimise the risk of human drug-induced liver injury (DILI) in drug discovery and development. Arch. Toxicol. 94, 2559–2585. doi:10.1007/s00204-020-02763-w
Weaver, R. J., Blomme, E. A., Chadwick, A. E., Copple, I. M., Gerets, H. H. J., Goldring, C. E., et al. (2020). Managing the challenge of drug-induced liver injury: a roadmap for the development and deployment of preclinical predictive models. Nat. Rev. Drug Discov. 19, 131–148. doi:10.1038/s41573-019-0048-x
Wilkinson, J. M. (2023). A review of complex in vitro cell culture stressing the importance of fluid flow and illustrated by organ on a chip liver models. Front. Toxicol. 5, 1170193. doi:10.3389/ftox.2023.1170193
Keywords: DILI, liver injury, in vitro methods, animal testing, replacement, spheroids, microphysiological systems, safety testing
Citation: Taylor K, Ram R, Ewart L, Goldring C, Russomanno G, Aithal GP, Kostrzewski T, Bauch C, Wilkinson JM, Modi S, Kenna JG and Bailey J (2025) Perspective: How complex in vitro models are addressing the challenges of predicting drug-induced liver injury. Front. Drug Discov. 5:1536756. doi: 10.3389/fddsv.2025.1536756
Received: 29 November 2024; Accepted: 24 January 2025;
Published: 19 February 2025.
Edited by:
Kuldeep K. Roy, University of Petroleum and Energy Studies, IndiaCopyright © 2025 Taylor, Ram, Ewart, Goldring, Russomanno, Aithal, Kostrzewski, Bauch, Wilkinson, Modi, Kenna and Bailey. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: R. Ram, cmViZWNjYUBzYWZlcm1lZGljaW5lcy5vcmc=
 K. Taylor
K. Taylor R. Ram
R. Ram L. Ewart
L. Ewart C. Goldring5
C. Goldring5 G. Russomanno
G. Russomanno G. P. Aithal
G. P. Aithal C. Bauch
C. Bauch J. M. Wilkinson
J. M. Wilkinson S. Modi
S. Modi J. G. Kenna
J. G. Kenna J. Bailey
J. Bailey