
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Disaster Emerg. Med. , 17 July 2024
Sec. Disaster Medicine
Volume 2 - 2024 | https://doi.org/10.3389/femer.2024.1425788
 Toshiki Abe1*
Toshiki Abe1* Hiroaki Saito1,2
Hiroaki Saito1,2 Chika Yamamoto1
Chika Yamamoto1 Yuichiro Eguchi3,4
Yuichiro Eguchi3,4 Kei Sato3,4
Kei Sato3,4 Misato Matsumoto3,4
Misato Matsumoto3,4 Kengo Hitachi3,4
Kengo Hitachi3,4 Sakiko Inoue5
Sakiko Inoue5 Tianchen Zhao1
Tianchen Zhao1 Michioki Endo6
Michioki Endo6 Toyoaki Sawano1,7
Toyoaki Sawano1,7 Akihiko Ozaki8
Akihiko Ozaki8 Masaharu Tsubokura1
Masaharu Tsubokura1 Hiroyuki Beniya9
Hiroyuki Beniya9Natural disasters pose significant challenges to affected communities, particularly vulnerable populations such as older adults. The aftermath of the Great East Japan Earthquake highlighted the necessity of welfare shelters to provide essential care. However, little is known about the specific role of physical therapists in these shelters. The aim of this article is to share the experiences and contributions of physical therapists in a welfare shelter in Wajima, Ishikawa Prefecture, immediately after the 2024 Noto Peninsula earthquake. The earthquake, with a magnitude of 7.6, damaged 76,589 houses, injured over 1,100 people, resulting in 245 deaths. The authors comprised a multidisciplinary team, including physical therapists, that provided short-term medical support at a welfare shelter in Wajima. Through several examples, we describe the contribution of physical therapists to evacuees' health outcomes. Physical therapists played multifaceted roles in the welfare shelter, optimizing living environments, conducting physical screenings, and delivering continuous medical care, including respiratory care and exercise programs. The involvement of physical therapists in post-disaster evacuation shelters is crucial for enhancing emergency health care delivery and promoting community resilience.
Natural disasters, such as earthquakes, present substantial challenges to impacted communities. Rendering care to vulnerable populations, such as older people, who are particularly at risk during the acute phase of a disaster, is imperative (1–3). Vulnerable populations are susceptible to health issues not only due to the disaster itself but also because of evacuation (4–6). In the aftermath of the Great East Japan Earthquake, many residents experienced diverse secondary health effects attributable to evacuation (7–9). Providing urgent medical care to victims in the aftermath of such events emerges as a critical necessity (10). The Great East Japan Earthquake significantly impacted many older people and persons with disabilities, leading the Japanese government in 2013 to mandate the establishment of welfare shelter in each municipality (11). Designated by the city to prioritize individuals necessitating special attention, such as older people and persons with disabilities, welfare shelters serve as the primary nexus for afflicted residents requiring daily support.
Welfare shelters played an important role in the Noto Peninsula earthquake that struck on January 1, 2024. The earthquake affected Ishikawa Prefecture, including Wajima, a city with a large older adult population. As of 2021, 45% of the residents of Wajima were aged 65 years or older. This demographic requires effective disaster response strategies tailored to those in need of assistance, especially older adults. The seismic activity on the Noto Peninsula inflicted substantial damage to its infrastructure, disrupting vital services, such as roads, transportation, water supply, internet communications, and telephone network (12). Particularly, the northern segment of Ishikawa Prefecture encountered delays in rescue operations and aid distribution. Furthermore, this region is faced with a decreasing number of full-time physicians predating the earthquake, necessitating collaborative efforts with neighboring medical facilities to sustain the local health care infrastructure (13). Within the context of the fragile medical system in the region, welfare shelters assumed a pivotal role in providing temporary accommodation and essential resources to evacuees (11). Although this framework has been implemented across Japan and has received praise for its effectiveness in supporting vulnerable populations during disasters, few reports have explored the role and effectiveness of physical therapists in welfare shelters.
Previous studies have underscored the pivotal role of physical therapists in disaster response and recovery, showcasing the contribution of their skills and involvement within disaster teams in aiding evacuees and coordinating efforts during disasters (14, 15). Moreover, prior studies and systematic reviews concerning post-disaster rehabilitation advocate for early rehabilitation interventions for evacuees injured in natural disasters, which not only ameliorate disability but also enhance clinical outcomes (16, 17). Research on evacuees after the Great East Japan Earthquake has revealed a 1.6-fold increase in the risk of needing long-term care owing to evacuation (18), thus highlighting the importance of physical therapists at disaster sites. Despite the burgeoning acknowledgment of the significance of physical therapy during disasters, the precise involvement of physical therapists in welfare shelters immediately after earthquakes remains inadequately explored (19). Limited research has been conducted on the hurdles faced by physical therapists in delivering care in the post-disaster welfare shelter setting. Moreover, the paucity of data regarding the experiences and outcomes of physical therapy interventions in this context obstructs the refinement of disaster response strategies.
This report describes the role and experiences of physical therapists in a welfare shelter during the hyper-acute phase of the Noto Peninsula earthquake in Wajima City, Ishikawa Prefecture, Japan. By meticulously documenting the challenges, successes, and lessons derived from physical therapy interventions in this context, this case study is intended to provide insights and enable future disaster-response strategies to be enhanced.
From January 9 to 13, 2024, our seven-member team delivered short-term medical assistance in Wajima City. The team included a doctor, three nurses, two physical therapists, and a clerk. Operational activities, primarily focused on assisting evacuees, were conducted in a welfare shelter. The age range of the evacuees ranged from under 10 to over 100 years. On site, the two physical therapists assumed diverse responsibilities beyond their primary role as physical therapists.
On arrival at the site, the team facilitated the operation and organized supplies, preparing the environment to receive evacuees. We were in charge of a large bare room in which 10 evacuees were to sleep. New evacuees moved in after our arrival, and our first step was to gather information about them. Of the 22 evacuees assigned to the room, seven required wheelchair assistance, and 10 needed walking monitoring, reflecting the high level of assistance required by 77% of the evacuees. We arranged for the transportation of seven cardboard beds and six reclining beds from the Japan Self-Defense Forces to accommodate the evacuees. Our efforts also focused on optimizing the room's layout to ensure a seamless flow of evacuees and support personnel, emphasizing the efficient use of space and accessibility (Figure 1). To ensure adequate spacing, we set a minimum distance of 80 cm between the beds, considering the provision of care and transfer movements from wheelchairs.
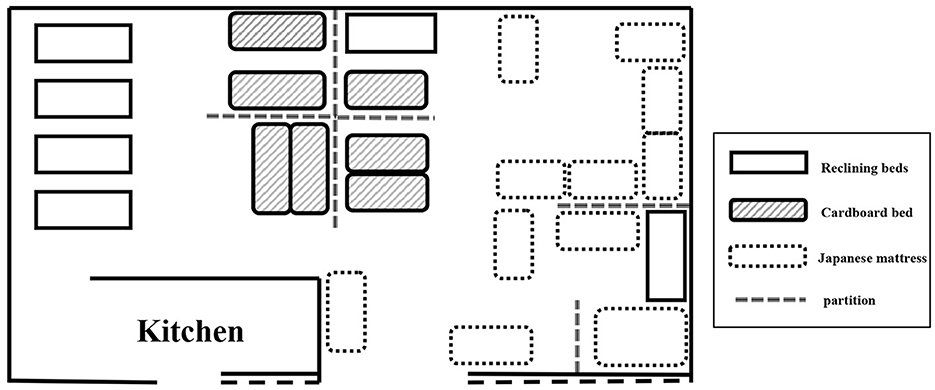
Figure 1. Layout of the welfare shelter room layout. Individual compartments in the shelter are secured using reclining beds, cardboard beds, and futons.
At the welfare shelter, we undertook the following steps: (1) collection and confirmation of information on the physical functioning of evacuees requiring wheelchairs and walking aids; (2) prioritization of evacuees to be placed on reclining and cardboard beds; and (3) review and arrangement of the layout of beds and evacuees. Decisions were made to assign evacuees with conditions such as hemiplegia or epilepsy, who needed assistance getting up, to reclining beds, whereas those who had difficulty rising from a lower position were placed on cardboard beds. Evacuees who were capable of walking, but were at risk of becoming frail owing to the evacuation, were positioned closer to the entrance for easier access. These environmental adjustments were carefully designed to enable evacuees to participate in daily activities and maintain their mobility. Additionally, we created a simple yet effective flow line from the beds to the hallway for wheelchair users, facilitated by strategically placing chairs along the path to ensure clear and accessible movement routes (Figure 2).
Group exercises were conducted in the large room under the guidance of a physical therapist. The activities included movements targeting the spinal column and thorax, and exercises for the large joints of the shoulders and hips, suitable for seated individuals. These exercises were thoughtfully crafted to accommodate participants with respiratory conditions, ensuring their engagement without respiratory compromise.
As physical therapists, we played an important role in the physical screening of evacuees. When evacuees arrived at the welfare shelter, nurses briefly interviewed them regarding their medication and medical history. However, fully understanding the health status of evacuees was challenging at the time. Those conducting interviews also managed the shelter and assisted evacuees, which limited their time to gather detailed health information. Additionally, evacuees struggled to provide clear information owing to disaster-induced stress and anxiety.
Given the circumstances, we opted to conduct additional physical screening of evacuees with three active physical therapists. During this process, we screened 22 individuals, primarily by palpating the dorsal foot artery, checking for deep vein thrombosis, and enquiring about health complaints. We identified three individuals with health issues and promptly linked them to medical facilities. Specifically, an 80-year-old woman (Ms. A) complained of back pain, later diagnosed as a rib fracture. An 80-year-old man (Mr. B) cut his foot on glass resulting in suspected cellulitis, and a 60-year-old man (Mr. C) experienced worsening foot edema. The symptoms of Ms. A and Mr. B were reported to an on-site physician, and they were promptly transported to a medical facility for emergency treatment. A nurse provided appropriate foot care and guidance to Mr. C, resulting in a reduction of the edema.
On January 11, at approximately 20:00, a woman in her 60s presented with a fever of approximately 39°C and a reduction in oxygen saturation levels to approximately 80%. Initial physical assessment did not reveal signs of circulatory compromise, such as worsening peripheral coldness, edema, or arrhythmia. This information was relayed to the on-site physician, who diagnosed the woman with acute aspiration pneumonia. Formerly mobile with a wheelchair, the patient became bedridden post-evacuation, facing challenges in repositioning, mobilization, and transitioning to a seated posture unassisted. She required assistance with expectoration, sputum suctioning, and respiratory support. After administering antibiotics, the physician, nurse, and physical therapist provided respiratory care for approximately 1 h, including positional drainage, expectoration, suctioning of sputum, and adjustment of medications. This care temporarily increased the patient's oxygen saturation levels to 90%. However, the health care team was concerned that the patient's respiratory condition might worsen during the night; therefore, the team considered transferring the patient to a hospital. At the time, only one hospital in Wajima City was able to provide medical care, and we were concerned that the patient might not be provided with adequate treatment. In addition, the road conditions in the affected area were poor; getting around was expected to take more than twice as long as it did under normal circumstances. Therefore, the health care team decided that continued treatment at the welfare shelter was the best option. Nurses and physical therapists were assigned to provide care throughout the night. Nurses primarily monitored vital signs and made decisions regarding cooling and medication. Physical therapists performed positional drainage, expectorant suctioning, and frequent general and physical assessments based on vital information (Figure 3).

Figure 3. Care by medical personnel (doctors, nurses, and physical therapists). In the welfare shelter, some evacuees required medical care through the night. This photograph shows the squeezing and phlegm suctioning being performed.
The next day, the patient's temperature normalized to 37.5°C, and her oxygen saturation level increased to 92%. Her lung sounds improved, indicating an improvement in her respiratory status. In this case, continuous care at the welfare shelter was preferred over transferring the patient to a hospital and dealing with the challenges of nighttime travel. The presence of a physical therapist played a crucial role in delivering appropriate respiratory care during the emergency.
This report highlights the important role that physical therapists play in the disaster environment by assessing and improving the physical capabilities of evacuees. In a welfare shelter with limited resources, the organization of beds and movement flow facilitated operations. Physical therapists customized the shelter layout to individual needs, preserving physical wellbeing through group and individual exercises. Physical therapists also addressed conditions such as trauma and frailty, conducting screening to identify urgent medical needs. Even in non-medical settings, ongoing care by a physical therapist can improve patient outcomes without having to transfer the patient to hospital.
Physical therapists play a crucial role in assessing and addressing patients' physical capabilities in clinical settings. Moreover, their involvement in selecting appropriate aid equipment and optimizing living environments is pivotal. In the welfare shelter, where evacuees faced constraints in space and resources, physical therapists' organization of beds, and movement flow facilitated the smooth operation of the center amid frequent evacuee movement. Additionally, the tailoring of the shelter's layout according to each evacuee's physical abilities demonstrated the ability of physical therapists to assess and advance living environments based on individual needs. The living environment influences patients' level of independence and amount of physical activity. In a previous study focusing on the built environment and physical activity in German clinics, the distance between common spaces such as toilets and washrooms and living spaces was found to be closely related to independent mobility and physical activity (20). In addition, independent mobility of hospitalized patients is dependent on the availability of physical barriers, sufficient space for movement, and lines of flow (20–22). Physical therapists can help maintain the physical function of evacuees during disasters by making environmental improvements.
It is also important for evacuees to continue physical activity in evacuation sites during the acute post-disaster period. Physical therapists also have a useful role to play in helping evacuees to continue physical activity. Prolonged sedentary behavior and inadequate physical activity in evacuation centers can heighten the risk of frailty among evacuees (23). Our team of physical therapists aimed to preserve evacuees' physical wellbeing through both group and individual exercise interventions. The stressful environment of evacuation centers can also adversely affect evacuees' mental health (24). Engaging in low-impact exercises not only mitigates the physical strain and risks associated with evacuation, but also provides psychological relief, contributing to overall wellbeing (25–27).
Conducting a comprehensive health assessment in shelter settings after a disaster is challenging. In this case scenario, the physical therapists conducted additional physical screening, enabling a more detailed evaluation of evacuees' physical function and health status. Physical therapists are skilled in assessment and treatment based on initial physical findings and often support people with common trauma and frailty (28, 29). Within the welfare shelter in this study, the physical screenings by the physical therapists identified three evacuees needing medical attention, two of whom had traumatic conditions. This underscores the importance of early detection of physical ailments and urgent medical needs, reference to appropriate medical facilities, and emergency evacuation if necessary. It may be useful for physical therapists, together with doctors, nurses, and others, to participate in the initial screening of evacuees following a disaster.
In the case of the woman with pneumonia, mentioned previously, the intervention of a physical therapist improved the evacuee's respiratory condition without her being admitted to hospital. Physical therapists were able to contribute to both health improvement and the preservation of the physical fitness of the evacuees by providing continuous care in the welfare shelter without transferring them to a hospital. The mortality rate due to aspiration pneumonia increases in the post-disaster evacuation setting. After the Great East Japan Earthquake, the rates of pneumonia and disuse syndrome increased in the early stages of the disaster (30, 31), and that many people died without receiving adequate medical care due to the limited availability of human and material resources (32). Therefore, in the affected areas, measures are needed to manage respiratory diseases. As aspiration pneumonia is common among the older adults, it is essential to have staff available who can deal with patients with respiratory conditions in areas with large older adult populations.
Providing care to displaced people in shelters is particularly important in the immediate aftermath of a disaster, when health care resources are scarce. Older adults and those with fragile physical function have greater challenges with transport and evacuation than healthier, younger people. In the 2011 Great East Japan Earthquake, inadequate patient transport and prolonged travel time were among the factors leading to 3,802 earthquake-related deaths (30, 33–35). In addition, the risk of death associated with evacuation was 1.7 to 2.6 times higher among vulnerable populations (36), especially among older people who were hospitalized or in residential care. Therefore, it is necessary to raise awareness of evacuation risks and ensure an environment in which medical care can be provided with limited human resources in disaster-affected areas. The incidence of pneumonia is high after disasters because oral care and nursing care is interrupted. In individuals with pneumonia, the probability of survival can be increased by providing care in evacuation centers, not only with antibiotics and equipment, but also with physical interventions by nurses and physical therapists.
Our experience indicates that the presence of physical therapists in welfare shelters is indispensable to the delivery of appropriate medical services during disasters and is a key element in safeguarding the health and safety of communities during disasters. We have reported our experience of an earthquake disaster based on a single-center case study of short duration. More cases and analysis of the post-disaster activities of physical therapists are needed to provide more comprehensive documentation of the usefulness of physical therapy activities in post-disaster evacuation settings.
Our experience of providing medical support at a welfare shelter immediately after the Noto Peninsula earthquake illustrates the potential contribution that physical therapists can make in the acute phase of a disaster. Physical therapists can contribute to the environmental arrangements of evacuation facilities, screening of patients, and treatment in collaboration with doctors and nurses. In times of disaster, multidisciplinary teams of healthcare professionals should work together from the early stages to provide comprehensive care. Additional studies of the role of physical therapists in providing support in the acute post-disaster period are needed.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article because this material consists mainly of images from disaster sites where lifesaving is a top priority. Therefore, it was difficult to obtain written signatures in the field regarding the individuals included in the images. However, individuals included in the images who could be identified were contacted individually at a later date to obtain their consent to use the image data.
TA: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. HS: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. CY: Data curation, Writing – original draft, Writing – review & editing. YE: Conceptualization, Writing – original draft, Writing – review & editing. KS: Conceptualization, Writing – original draft, Writing – review & editing. MM: Conceptualization, Writing – original draft, Writing – review & editing. KH: Conceptualization, Writing – original draft, Writing – review & editing. SI: Conceptualization, Writing – original draft, Writing – review & editing. TZ: Conceptualization, Writing – original draft, Writing – review & editing. ME: Writing – original draft, Writing – review & editing. TS: Writing – original draft, Writing – review & editing. AO: Writing – original draft, Writing – review & editing. MT: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. HB: Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Japan Science and Technology Agency (JST), Grant Number JPMJPF2301.
We express our deepest respect for the staff members who have supported the disaster site since the beginning of the disaster, and to the people who are providing support to the affected areas and wish for the earliest possible recovery of the people affected by the disaster. We thank the Institute of Medical Care and Societal Health, a non-profit organization for their support. In addition, we are grateful to Editage (www.editage.com) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rivera JD. The impact of evacuating on short-term disaster recovery: a study of individuals affected by Hurricane Harvey living in Texas counties. Int J Disaster Risk Reduct. (2020) 44:101424. doi: 10.1016/j.ijdrr.2019.101424
2. Bell SA, Horowitz J, Iwashyna TJ. Health outcomes after disaster for older adults with chronic disease: a systematic review. Gerontologist. (2020) 60:e535–e47. doi: 10.1093/geront/gnz123
3. Ngo EB. When disasters and age collide: reviewing vulnerability of the elderly. Natural Hazards Review. (2001) 2:80–9. doi: 10.1061/(ASCE)1527-6988(2001)2:2(80)
4. Marshall J, Wiltshire J, Delva J, Bello T, Masys A. Natural and manmade disasters: vulnerable populations. In: Global health security: Recognizing vulnerabilities, creating opportunities. (2020). p. 143–61. doi: 10.1007/978-3-030-23491-1_7
5. Kako M, Steenkamp M, Ryan B, Arbon P, Takada Y. Best practice for evacuation centres accommodating vulnerable populations: a literature review. Int J Disast Risk Reduct. (2020) 46:101497. doi: 10.1016/j.ijdrr.2020.101497
6. Bayraktar N, Yilmaz Ü. Vulnerability of elderly people in disasters: A systematic review. Turk Geriatri Dergisi. (2018) 21:467–82.
7. Tsubokura M. Secondary health issues associated with the Fukushima Daiichi nuclear accident, based on the experiences of Soma and Minamisoma Cities. J Nat Inst Public Health. (2018) 67:71–83.
8. Hashimoto S, Nagai M, Fukuma S, Ohira T, Hosoya M, Yasumura S, et al. Influence of post-disaster evacuation on incidence of metabolic syndrome. J Atheroscler Thromb. (2017) 24:327–37. doi: 10.5551/jat.35824
9. Yasumura S, Goto A, Yamazaki S, Reich MR. Excess mortality among relocated institutionalized elderly after the Fukushima nuclear disaster. Public Health. (2013) 127:186–8. doi: 10.1016/j.puhe.2012.10.019
10. Timalsina R, Songwathana P. Factors enhancing resilience among older adults experiencing disaster: a systematic review. Australas Emerg Care. (2020) 23:11–22. doi: 10.1016/j.auec.2019.12.007
11. Disaster Management COiJ. White Paper on Disaster Management 2022. (2022) Available from: https://www.bousai.go.jp/en/documentation/white_paper/pdf/2022/R4_hakusho_english.pdf (accessed December 02, 2022).
12. Cabinet Office GoJ. The 2024 Noto Peninsula Earthquake Damage Report. (2024). Available online at: https://www.bousai.go.jp/updates/r60101notojishin/r60101notojishin/index.html (accessed March 26, 2024).
13. Prefecture I. Ishikawa Prefecture Medical Plan (2023). Available online at: https://www.pref.ishikawa.lg.jp/iryou/support/iryoukeikaku/iryoukeikaku.html (accessed March 26, 2024).
14. Trivedi N. Physiotherapy in disaster management: physiotherapist view. Natl J Integr Res Med. (2018) 8:32–4.
15. Amatya B, Galea M, Li J, Khan F. Medical rehabilitation in disaster relief: Towards a new perspective. J Rehabil Med. (2017) 49:620–8. doi: 10.2340/16501977-2250
16. Reinhardt JD, Li J, Gosney J, Rathore FA, Haig AJ, Marx M, et al. Disability and health-related rehabilitation in international disaster relief. Glob Health Action. (2011) 4:7191. doi: 10.3402/gha.v4i0.7191
17. Khan F, Amatya B, Gosney J, Rathore FA, Burkle FM. Medical rehabilitation in natural disasters: a review. Arch Phys Med Rehabil. (2015) 96:1709–27. doi: 10.1016/j.apmr.2015.02.007
18. Moriyama N, Morita T, Nishikawa Y, Kobashi Y, Murakami M, Ozaki A, et al. Association of living in evacuation areas with long-term care need after the fukushima accident. J Am Med Dir Assoc. (2022) 23:111–6.e1. doi: 10.1016/j.jamda.2021.05.030
19. Harrison RM. Preliminary investigation into the role of physiotherapists in disaster response. Prehosp Disaster Med. (2007) 22:462–5. doi: 10.1017/S1049023X00005227
20. Kevdzija M, Marquardt G. Stroke patients' nonscheduled activity during inpatient rehabilitation and its relationship with the architectural layout: a multicenter shadowing study. Top Stroke Rehabil. (2022) 29:9–15. doi: 10.1080/10749357.2020.1871281
21. Kevdzija M, Marquardt G. Physical barriers to mobility of stroke patients in rehabilitation clinics. In: Breaking Down barriers: Usability, accessibility and inclusive design, Springer International Publishing. (2018). p. 147–57. doi: 10.1007/978-3-319-75028-6_13
22. Eng XW, Brauer SG, Kuys SS, Lord M, Hayward KS. Factors Affecting the ability of the stroke survivor to drive their own recovery outside of therapy during inpatient stroke rehabilitation. Stroke Res Treat. (2014) 2014:626538. doi: 10.1155/2014/626538
23. Okazaki K, Ohira T, Sakai A, Shimabukuro M, Kazama JJ, Takahashi A, et al. Lifestyle factors associated with undernutrition in older people after the great east japan earthquake: a prospective study in the fukushima health management survey. Int J Environ Res Public Health. (2022) 19:3399. doi: 10.3390/ijerph19063399
24. Hori A, Hoshino H, Miura I, Hisamura M, Wada A, Itagaki S, et al. Psychiatric outpatients after the 3.11 complex disaster in Fukushima, Japan. Ann Glob Health. (2016) 82:798–805. doi: 10.1016/j.aogh.2016.09.010
25. Gordon BR, McDowell CP, Hallgren M, Meyer JD, Lyons M, Herring MP. Association of efficacy of resistance exercise training with depressive symptoms: meta-analysis and meta-regression analysis of randomized clinical trials. JAMA Psychiatry. (2018) 75:566–76. doi: 10.1001/jamapsychiatry.2018.0572
26. Smith PJ, Merwin RM. The role of exercise in management of mental health disorders: an integrative review. Annu Rev Med. (2021) 72:45–62. doi: 10.1146/annurev-med-060619-022943
27. Morres ID, Hatzigeorgiadis A, Stathi A, Comoutos N, Arpin-Cribbie C, Krommidas C, et al. Aerobic exercise for adult patients with major depressive disorder in mental health services: a systematic review and meta-analysis. Depress Anxiety. (2019) 36:39–53. doi: 10.1002/da.22842
28. Leahy A, McNamara R, Reddin C, Corey G, Carroll I, O'Neill A, et al. The impact of frailty Screening of Older adults with muLtidisciplinary assessment of those At Risk during emergency hospital attendance on the quality, safety and cost-effectiveness of care (SOLAR): a randomised controlled trial. Trials. (2021) 22:581. doi: 10.1186/s13063-021-05525-w
29. Goodman D, Harvey D, Cavanagh T, Nieman R. Implementation of an expanded-scope-of-practice physiotherapist role in a regional hospital emergency department. Rural Remote Health. (2018) 18:4212. doi: 10.22605/RRH4212
30. Maeda K, Shamoto H, Furuya S. Feeding support team for frail, disabled, or elderly people during the early phase of a disaster. Tohoku J Exp Med. (2017) 242:259–61. doi: 10.1620/tjem.242.259
31. Kawashima M, Sawano T, Murakami M, Moriyama N, Kitazawa K, Uchi Y, et al. Association between the deaths indirectly caused by the Fukushima Daiichi nuclear power plant accident (disaster-related deaths) and pre-disaster long-term care certificate level: a retrospective observational analysis. Int J Disast Risk Reduct. (2023) 96:103989. doi: 10.1016/j.ijdrr.2023.103989
32. Sawano T, Senoo Y, Yoshida I, Ozaki A, Nishikawa Y, Hori A, et al. Emergency Hospital evacuation from a hospital within 5 km radius of fukushima daiichi nuclear power plant: a retrospective analysis of disaster preparedness for hospitalized patients. Disaster Med Public Health Prep. (2022) 16:2190–3. doi: 10.1017/dmp.2021.265
33. Sawano T, Senoo Y, Nonaka S, Ozaki A, Nishikawa Y, Hori A, et al. Mortality risk associated with nuclear disasters depends on the time during and following evacuation of hospitals near nuclear power plants: an observational and qualitative study. Int J Disast Risk Reduct. (2023) 85:103514. doi: 10.1016/j.ijdrr.2022.103514
34. Reconstruction Agency JG. Number of disaster-related deaths of East Japan Earthquake. (2024). Available online at: https://www.reconstruction.go.jp/topics/main-cat2/sub-cat2-6/20240301_kanrenshi.pdf (accessed December 31, 2023).
35. Sawano T, Nishikawa Y, Ozaki A, Leppold C, Takiguchi M, Saito H, et al. Premature death associated with long-term evacuation among a vulnerable population after the Fukushima nuclear disaster: a case report. Medicine (Baltimore). (2019) 98:e16162. doi: 10.1097/MD.0000000000016162
Keywords: disasters, disease prevention, shelters, physiotherapy, environmental adjustments, post-disaster acute phase, vulnerable population, population resilience
Citation: Abe T, Saito H, Yamamoto C, Eguchi Y, Sato K, Matsumoto M, Hitachi K, Inoue S, Zhao T, Endo M, Sawano T, Ozaki A, Tsubokura M and Beniya H (2024) Role of physical therapists in providing care to older adults in welfare shelters during the hyper-acute phase of a disaster: lessons learned in Wajima City, Japan, after the 2024 Noto Peninsula earthquake. Front. Disaster Emerg. Med. 2:1425788. doi: 10.3389/femer.2024.1425788
Received: 30 April 2024; Accepted: 28 June 2024;
Published: 17 July 2024.
Edited by:
Benoit Viault, Centre Hospitalier Universitaire de Toulouse, FranceReviewed by:
Jan-Cedric Hansen, Centre d'Hébergement et d'Accompagnement Gérontologique (CHAG), FranceCopyright © 2024 Abe, Saito, Yamamoto, Eguchi, Sato, Matsumoto, Hitachi, Inoue, Zhao, Endo, Sawano, Ozaki, Tsubokura and Beniya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Toshiki Abe, YS10b3NoaUBmbXUuYWMuanA=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.