- 1Centre for Advanced Spatial Analysis (CASA), The Bartlett, University College London, London, United Kingdom
- 2Performance and Analytics Directorate, London Ambulance Service NHS Trust, London, United Kingdom
- 3Department of Arts and Sciences, University College London, London, United Kingdom
Exploring inequalities in ambulance and pre-hospital demand is important to improve service equity and reduce wider health inequalities. Maternity incidents amongst ambulance demand are a key area of focus because of the specialized care that is needed for patients, as well as the impact of wider determinants of health on pregnancy outcomes. Since there are spatial inequalities amongst pregnant patients who call for an ambulance, the aim of this study is to assess the underlying factors associated with pregnancy related ambulance complaints, to determine why maternity patients utilize the ambulance service. Local indicators of spatial autocorrelation were used to identify clusters of ambulance maternity demand within Greater London (UK). A negative binomial regression model was used to explore associations between socioeconomic, environmental, accessibility and demographic variables. Our results reveal that neighborhoods with low adult skills (i.e. qualifications/English language abilities) have a higher rate of demand. Moreover, our results imply that the demand for ambulance services may not be directly tied to health outcomes; rather, it might be more closely associated with patients' reasons for calling an ambulance, irrespective of the actual necessity. The benefits of identifying factors that drive demand in ambulance services are not just linked to improving equity, but also to reducing demand, ultimately relieving pressure on services if alternative options are identified or underlying causes addressed. Doing so can improve health inequalities by firstly, improving ambulance care equity by directly supporting a better allocation of resources within ambulance systems to target patterns in demand.
1 Introduction
Ambulance services in England are facing increasing organizational pressures and challenging performance. This can be partially attributable to growing demand, staffing issues, handover and waiting times, and post-pandemic difficulties (1–3). The reasons for this are complex and vary, including factors such as population growth and an aging population (4, 5). Since 2010, public services in England have also faced increased pressure from a freeze or significant cuts to funding, resulting in reduced services across the country, with variable impacts depending on individuals' location and access to services (6, 7). This is often described as a postcode lottery, meaning that residential locations determine the level of available public services and care (8, 47), with significant differences—or inequality—between services available to individuals (9–11, 48). With health services under pressure and severely lacking capacity, ambulance services have become increasingly viewed as the first, only, or last option available for many patients, and a reliable gateway into the healthcare system (12), which in turn increases pressure on ambulance services when other patient care options might be more appropriate (13, 46).
Maternity care services in England can often overlook ambulance services as a critical part of maternity care. Heys et al. (14) argued for increased training, research, and standardization for emergency pre-hospital maternity care provided. A common strand of ambulance and maternity services research focuses specifically on unplanned births or out of hospital births. Research on out of hospital births attended by ambulance services has found that socio-economic variables such as income, class, and ethnicity are associated with outsized demand of this type (15). Heys et al. (14) found that paramedics often have low clinical confidence when dealing with maternity patients if they have not received specialized maternity training or exposure to maternity incidents, as well as being unable to access expert maternity advice. Therefore, maternity care should be an important part of ambulance demand research but currently there is little literature focusing on the drivers of this demand type (15, 16). This study seeks to provide an overview of maternity ambulance incidents and identify inequalities and factors driving this type of demand.
While other metrics such as clinical quality indicators are published for ambulance trusts (17, 49), ambulance response times receive a significant amount of research focus, as the speed of pre-hospital response is often critical for patient outcomes (18). It is common for ambulance research to focus on increasing demand by optimizing ambulance resource systems with the goal to reduce response times. Incorporating equity measures into ambulance planning often focuses on equal resource distribution based on geography, rather than matching the needs of the population, whilst an approach that prioritizes an average level performance of service delivery can overlook the variations where inequities persist (19–21). This approach can categorize the understanding of equity as “horizontal,” rather than “vertical.” Horizontal equity refers to a focus on equal distribution everywhere, whilst vertical equity looks to balance and distribute resources accordingly to match existing health inequalities amongst different groups. Ambulance services and literature often have a high proportion of research and strategy focused on aging population, as this is a large and increasing share of emergency ambulance demand (4, 5, 17, 22). Complaint types with high acuity are commonly the focus of research on ambulance efficiency, as an improved response time can improve survival rates for these categories. These are often classed as category 1 incidents, where (in England) a response time of under 8 min is expected (17). However, for categories of incidents such as maternity cases that may be a small fraction of overall activity, and of lower acuity, there are still inequalities in the response to these incidents that warrant being addressed. This can be to the detriment of different incidents, where inequalities may persist, and where patient care can be improved. Within the London Ambulance Service (LAS) strategy, maternity incidents have been identified as an area where specialized care can be provided to improve patient care and outcomes (17, 61). This specialized pre-hospital care is important as it can often provide a better alternative pathway for patients, where conveyance to an emergency department may not be the most appropriate outcome. Allen et al. (55) noted that the National Health Service (NHS) legal cost for maternity care is one of the highest proportions of all clinical types, and so improved care, efficiency, and equity can look to reduce this financial aspect across all NHS services. Furthermore, maternity services have often been the focus of independent investigations into failings of care (14, 23) therefore there is increased interest nationally in improving care within this field.
This study aims to uncover spatial inequalities present in maternity incident demand and assess the underlying factors associated with geographical variations in ambulance demand rates. Determining utilization patterns of ambulances can promote equitable resource allocation and exploring wider determinants can explore how broader policy interventions may help alleviate demand in frontline medical services and reduce health inequalities. Examining underlying socio-economic and environmental factors that characterize hotspot areas can help determine how demand for ambulance resources can be reduced whilst at the same time patient care and equity improved.
2 Materials and methods
2.1 Setting
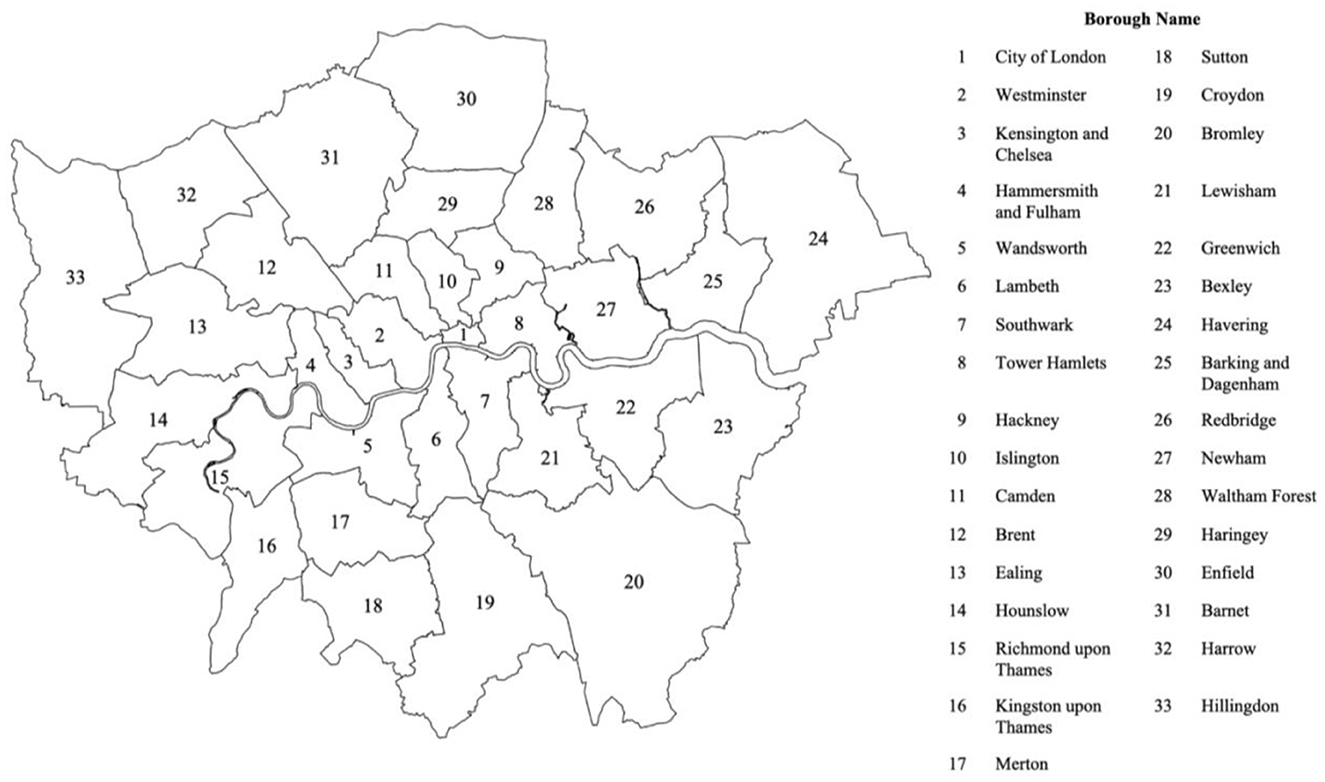
The London Ambulance Service (LAS) NHS Trust is the emergency medical care service that covers all Greater London. It is the busiest ambulance service in the UK, attending over 1 million incidents a year (17, 62). The LAS is the only ambulance trust in England to cover an entirely urban area, with a dense population of 8.8 million residents and is the only pan-London NHS trust. Greater London can be divided into five Integrated Care Systems, which centralize health and care operations for those areas. Analyses were conducted at Lower-level Super Output Areas (LSOA) geography level (defined by the UK census). This scale of administrative area was chosen as it allowed for the smallest scale of geographic area that data was available for, whilst also allowing for analysis on geographical inequalities by determining differences within boroughs. This scale also ensured patient anonymity by grouping to populations of ~1,500 individuals. The study area included 4,345 LSOAs excluding only one Greater London area containing Heathrow Airport due to the high volume of incidents within this one LSOA that did not occur in residential areas.
2.2. Ambulance demand data
Ambulance data comprising of “see and treat” incidents categorized with the primary complaint as “pregnancy, childbirth, miscarriage” from the London Ambulance Service (LAS) was used for this cross-sectional analysis. LAS demand data categorizes incidents into Chief Complaint groups. These are clinical groupings that help provide information to staff dealing with an incident. The largest chief complaint group is NHS 111 “Transfers,” whilst “Falls and Breathing Problems” are large categories; there is also a large group of incidents with an “unknown” chief complaint. This is worth acknowledging whilst using chief complaint categorization, as NHS 111 “Transfers” and “Unknown,” do not provide any clinical information for analysis, and there may be many maternity related incidents that were not categorized under the pregnancy chief complaint. Furthermore, incidents may not be accurately categorized by call handlers, and the true nature of an incident may change once patients are treated in person. Pregnancy incidents from 2010 to 2022 dispatch data were collated to LSOAs, and incident rates per 1,000 population were calculated for LSOAs across Greater London. Residential population levels from the 2021 Census were used to calculate incident rates, which includes all people registered at a household in an area.
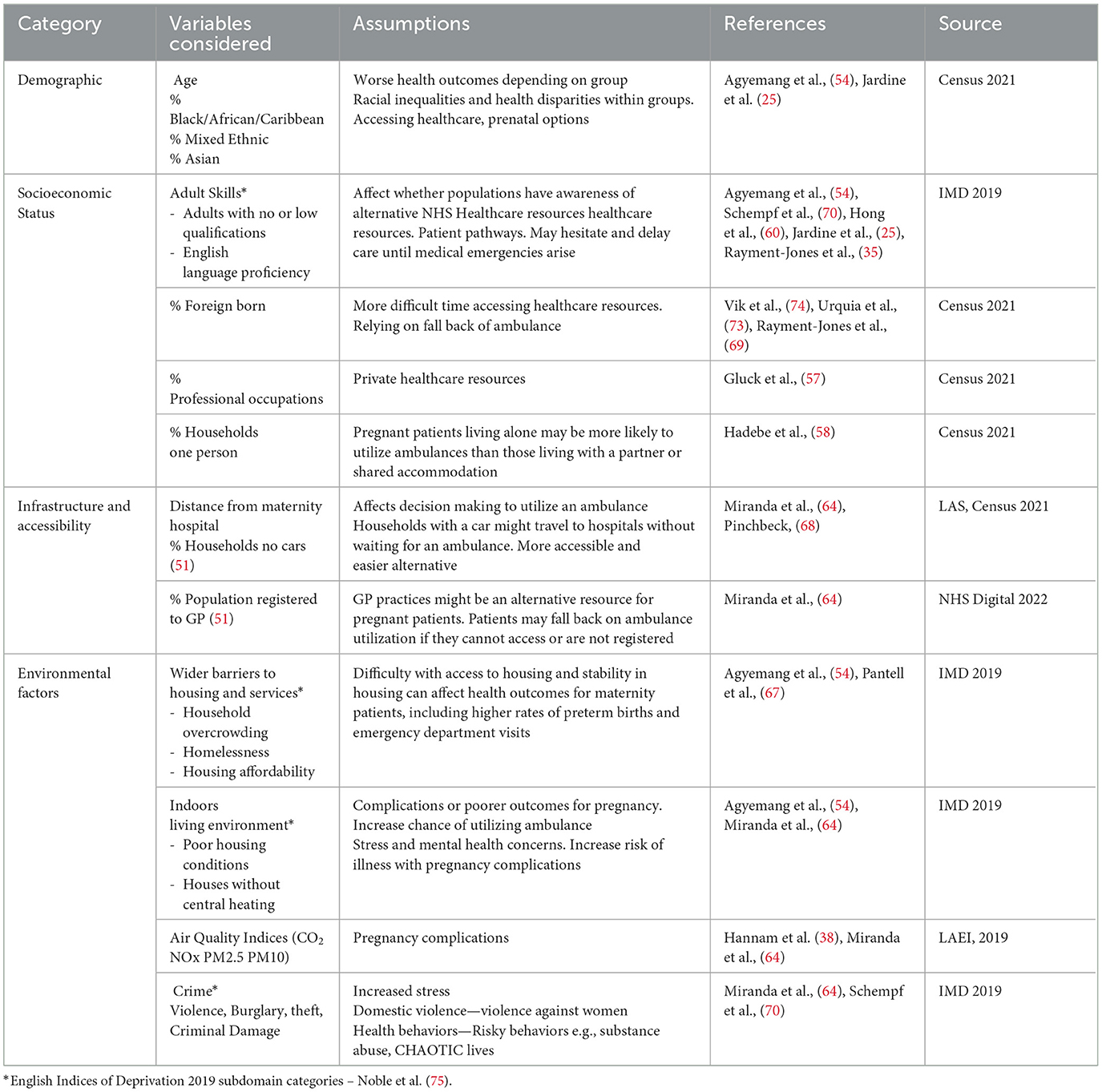
2.3. Independent variables
Independent variables used for analysis were of four categories: demographic, socioeconomic, infrastructure/accessibility, and environmental. The variables chosen for this study came from multiple sources. Data on locations of NHS hospitals with maternity facilities in Greater London was provided by LAS. The number of patients registered at General Practitioners (GP) practices was taken from NHS Digital with GP practices aggregated to LSOAs. This does not account for patients that may be registered at GP practices in one LSOA but live in another, as well as other accuracy issues such as ghost patients, list inflation, or over coverage (66). Variables categorized into socioeconomic, environmental, and accessibility were taken from the Index of Multiple Deprivation (IMD): indicators calculated and categorized into sub-domain scores of deprivation. Variables, including IMD sub-domains, were chosen based on a review of literature on ambulance demand studies and pregnancy related health outcomes (16) using sub-domains to allow effects beyond the overall deprivation score to be explored, whilst controlling for multicollinearity (the chosen variables are summarized in Table 1).
This study focused on three demographic variables derived from Census 2021 data. While age is generally associated with higher ambulance demand, it was not included in the modeling due to its low correlation with maternity ambulance incidents. The limited availability of data at this scale suggests that the relationship between older pregnant patients and ambulance incident rates is likely more discernible at the individual patient record level rather than through ecological analysis.
Ethnic disparities in healthcare access and maternity health outcomes, particularly among black women, have been emphasized in several studies (24–26, 52). To capture a comprehensive understanding of racial impacts amongst all ethnic census groups, our study incorporated the three main non-white census groups: (i) Black/African/Caribbean, (ii) Mixed Ethnic, (iii) Asian. Including these three categories also allows for accounting for the proportion of white to non-white demographics, allowing a more nuanced examination of the intersectional dynamics at play. Moreover, it acknowledges the heterogeneity within non-white populations, which is essential for developing targeted interventions and policies.
Sub-domains taken from the Index of Multiple Deprivation were reviewed and selected based on previous literature (50). For example, a score of Adult Skills (which combine both rates of education and English language proficiency) was considered, as there are several studies regarding adult education, language skills, and their effect on healthcare accessibility and health outcomes (24, 27, 65). This is applicable to maternity health outcomes too and relevant for emergency ambulance incidents as whether a patient needs an ambulance can be influenced by whether they sought alternative care, or if they delayed care until it became an emergency.
The number of households with lone parents was included as a measure to examine the effect of maternity patients living alone. Previous research indicates that lone mothers have a different experience of pregnancy as well as a lack of social network (28, 29), but their association with ambulance utilization is not as clear.
Low socioeconomic status has shown links to inequalities in adverse pregnancy outcomes. Factors such as professional occupations, were included because of association between professional work occupations, good health behaviors, and well-informed decisions. Furthermore, associations with physical stresses, risky behaviors, and poorer outcomes in pregnancy led us to include this factor (25, 30).
Foreign born percentages in neighborhoods have been included due to previous literature associating foreign patients with poorer pregnancy outcomes, due to difficulty accessing healthcare services, or reluctance to connect due to fears of immigration status (14, 56, 74).
This study focuses on three accessibility factors as potential determinants of ambulance incident rates, considering their relevance to patients' decisions to call for an ambulance. These were: (i) distance to nearest maternity hospital, (ii) percentage of residents registered to a GP, and (iii) the percentage of households without access to a car. We theorize that the distance from the nearest maternity hospital could impact patients' choices to use ambulances for accessing care, drawing on insights from previous research discussing how distance influences accessibility to healthcare resources (31, 32).
The inclusion of the proportion of households with access to a car reflects its potential impact on patients' decisions regarding ambulance use. Individuals with access to a car might choose to directly seek care at an Emergency Department (ED). Furthermore, residents registered with General Practitioners (GPs) may play a role in influencing patient choices toward alternative care, potentially reducing reliance on ambulance services (5, 13). The accessibility of other primary care resources is also a crucial factor in shaping the utilization patterns of emergency medical services (33). An understanding of these diverse accessibility factors contributes to a more nuanced assessment of the dynamics influencing ambulance use across various scenarios.
Environmental factors are included primarily based on their influence on health outcomes amongst pregnancy related incidents. These factors include housing conditions, air quality, crime rates, housing access, and overcrowding. These factors therefore are considered for ambulance utilization.
Crime IMD deprivation scores are included as measure of societal risk, where women who are often living or experiencing higher social risk may be less likely to access preventative healthcare and therefore require emergency care more often. Highly deprived areas with high crime rates are an indicator representing areas of high stress, uncertainty, and chaotic lives, which can increase social risk (34, 35). Housing Insecurity, measuring by wider barriers to housing from the IMD, was included because of previous links between housing insecurity and maternity outcomes (36, 37). This is similar for air quality indicators, with previous literature indicating that poor air quality can be linked to poorer health outcomes amongst maternity patients (38, 39) and therefore more likely to utilize emergency pre-hospital care.
2.4. Statistical analysis
2.4.1. Spatial autocorrelation
Spatial autocorrelation is a branch of statistics that consists in an extension of autocorrelation methods through a second spatial dimension. Whilst autocorrelation measures the strength of relationship between values of residuals along a regression line, spatial autocorrelation involves the relationship between neighboring values. Neighboring values that are closely related would indicate a strong spatial autocorrelation and systematic variation. Values that would appear to be arranged randomly across space would show a weak spatial autocorrelation; complete spatial randomness is the complete random arrangement of values across an area. The I value is calculated alongside a p-value to ensure its statistical significance. Results where p < 0.05 would allow us to assume that spatial autocorrelation exists. A Moran's I value of zero would indicate complete spatial randomness. A positive Moran's I value indicates positive spatial autocorrelation and clustering while negative values would indicate neighboring values are not similar (40, 41).
Local Indicators of Spatial Autocorrelation were used to identify clusters of similar rates within the study area. The local Moran's I value for a local spatial object is calculated using the formula:
Where m2 is a constant for locations, wij is the spatial weight of observation i and j, is the attribute mean. n is the number of observations. Using local spatial scores can allow a nuanced understanding of where high or low clusters are within the region and to also identify spatial outliers, such as high areas amongst low values and low areas amongst high. Areas that were significant hotspots (p-value < 0.05), alongside borough variation, are used to examine differences in regression models compared to global results.
2.4.2. Negative binomial regression
A negative binomial regression model was used, as it allows for overdispersion by adding an extra parameter to the model that estimates the extra variation in the count data beyond what is explained by the mean. Negative binomial regression equation is commonly represented as:
Where the expected value for the outcome variable yi is represented as λi, βk is the regression coefficient for the corresponding variable xk. The error term σεi is included for negative binomial regressions and accounts for the overdispersion, differing from regular Poisson regression types (53). The full model used for this study can be represented as:
Results are presented as Incident Rate Ratios (IRR). Two levels of regression models were implemented: one for the overall Greater London area, and another was applied to each of the 33 London boroughs to unveil the spatial differences.
3 Results
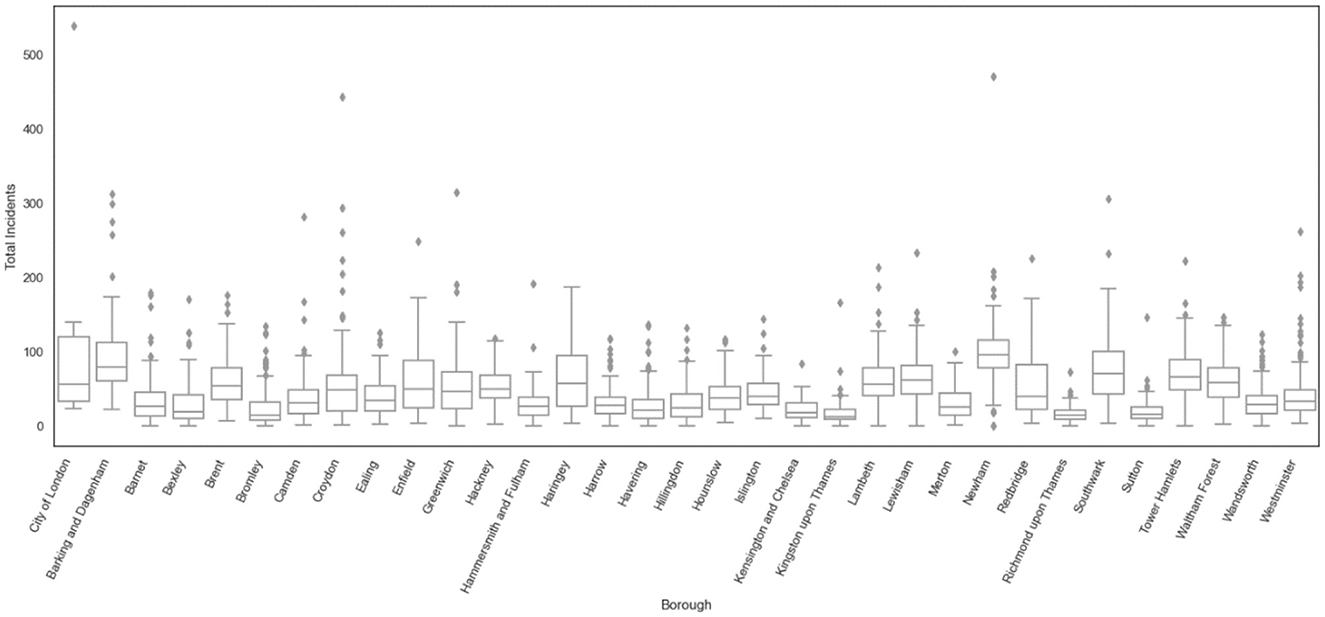
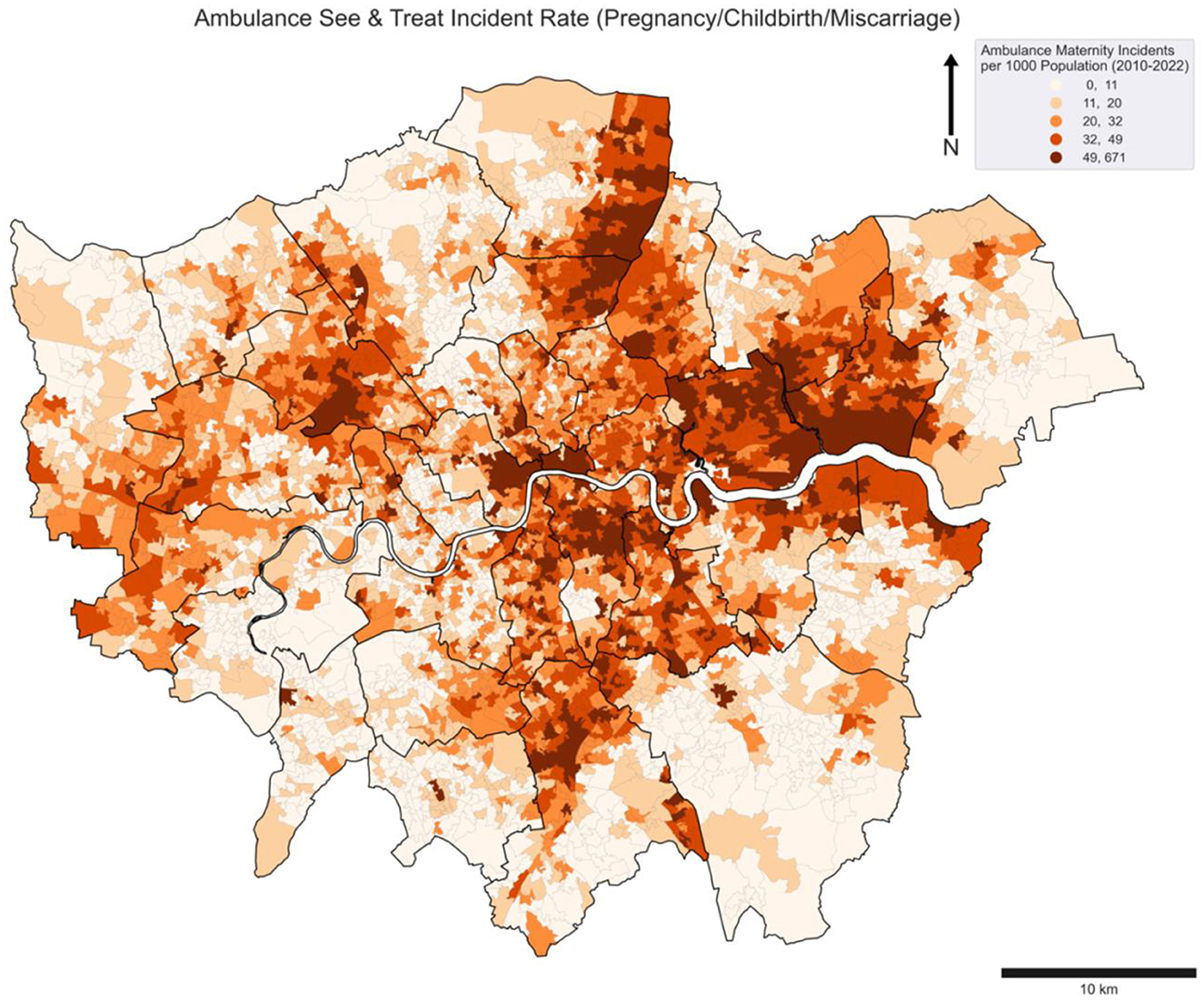
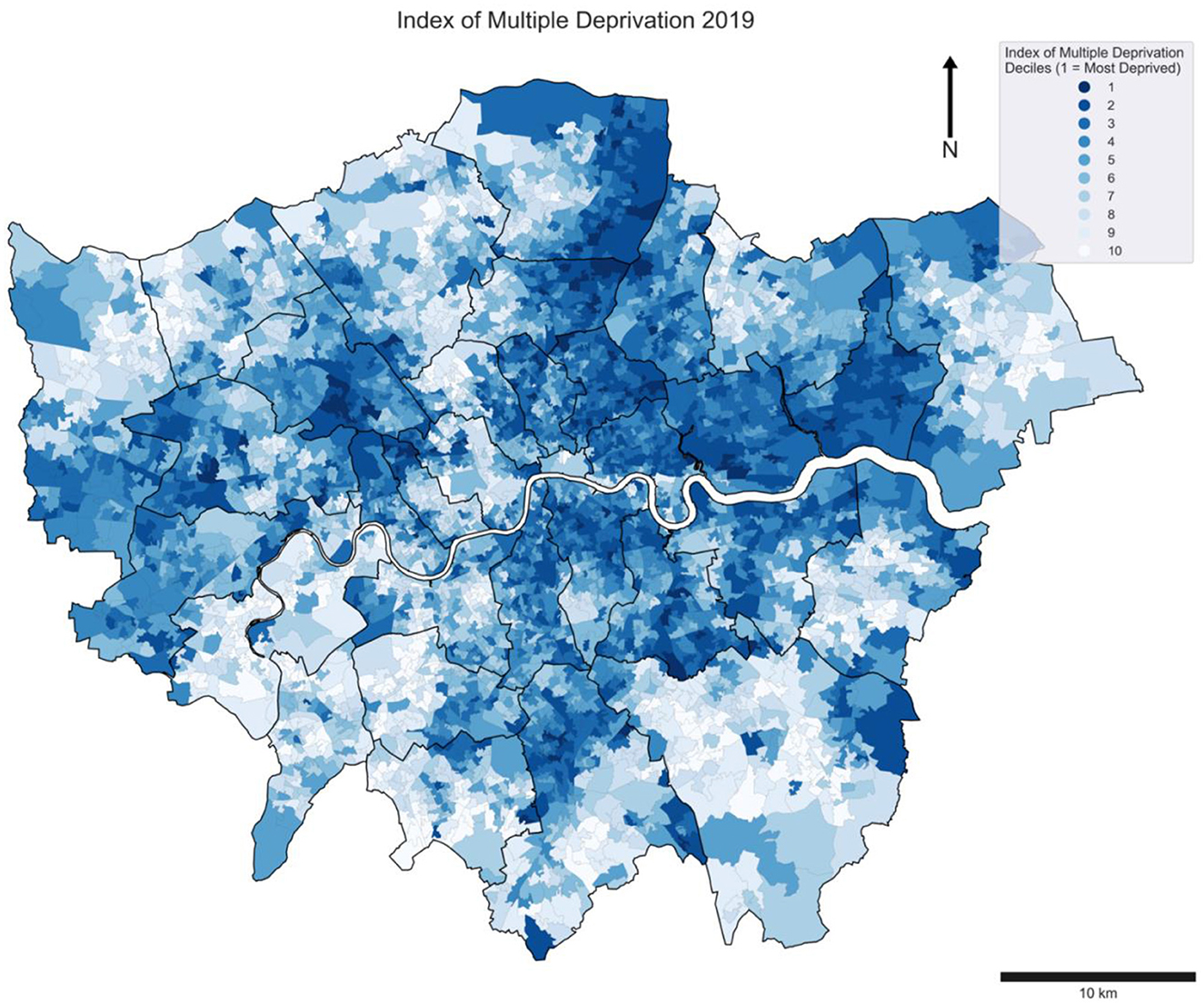
Between 2010–2022 there were 231,118 emergency ambulance incidents categorized as “Pregnancy, Childbirth, Miscarriage,” with the minimum per LSOA reported as 0 and the maximum 1,659 incidents. There were 22 LSOAs out of a total of 4,835 that had zero reported incidents. The median number of incidents per LSOA is 38 (Figure 1). Incidents per 1,000 people (Figure 2) show the distribution of incident rates across Greater London. This indicates that rates are not consistent with population levels. Across Greater London the incident rate pattern shows boroughs that have higher rates, such as London Borough of Newham, which has the highest median of incident rates per LSOA, excluding the City of London (Figure 3). Some boroughs have significant LSOA outliers such as Croydon, Greenwich, Southwark, and Westminster with areas of relatively high incident rates, relative to their surrounding neighborhoods. This reflects areas of traditionally high deprivation amongst boroughs where there is a large range of deprivation. Figure 4 shows the deprivation rates from the IMD 2019 for comparison with ambulance incident rates.
Spearman rank correlation coefficient results suggest a high range of correlation deprivation scores (between −0.30 and 0.79), indicating that deprivation sub-domains may better reflect the relationship with demand rates. Other chosen variables ranged from 0.77 (% Black/African/Caribbean) to 0.20 (air quality pm 2.5). These results were used to inform the feature selection for regression analysis.
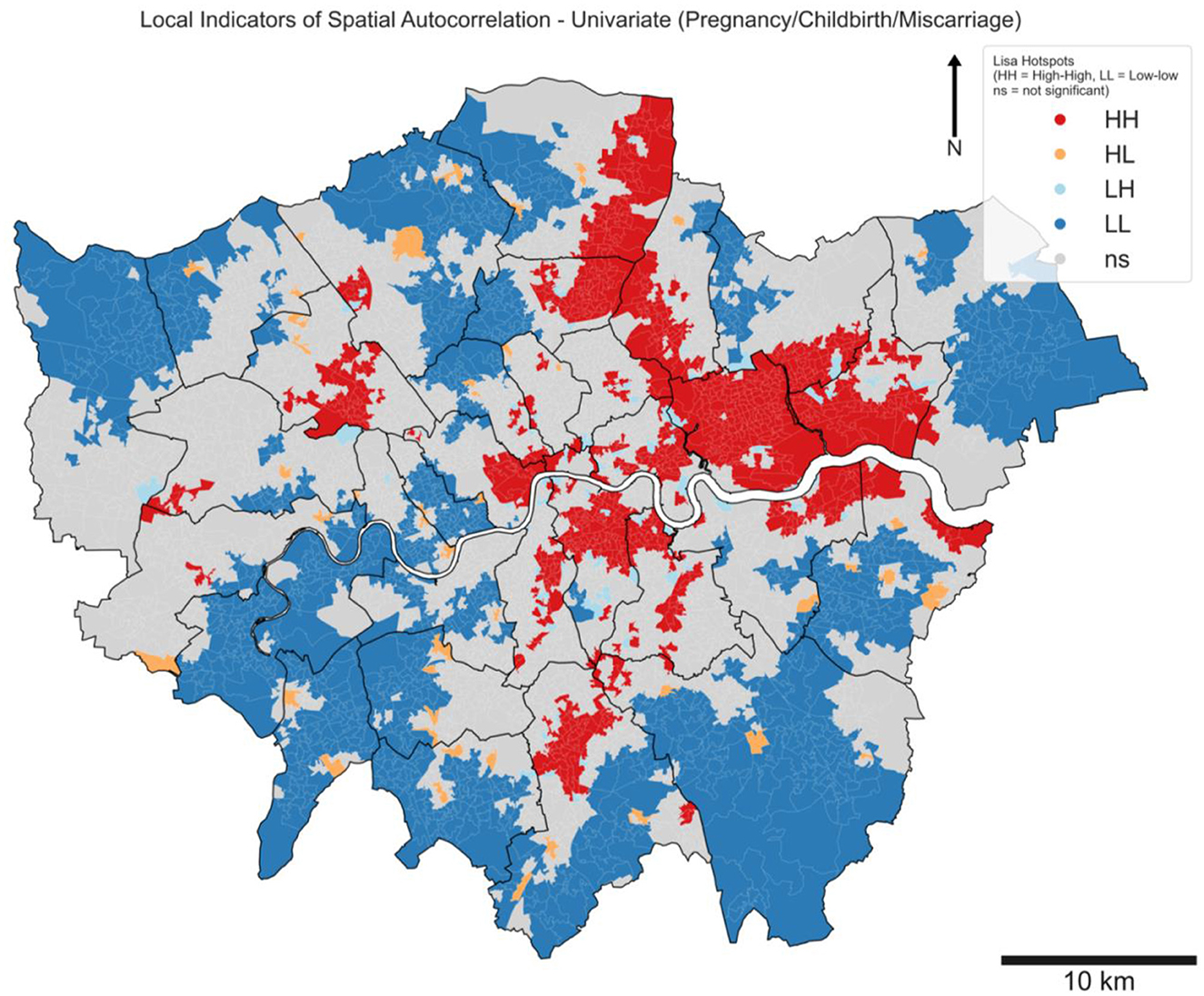
LISA hotspots (Figure 5) show significant variation between east and west, as well as north and south. This suggests that rates of pregnancy complaints are clustered in specific areas within London neighborhoods (i.e. Newham and Barking and Dagenham have the highest number of hotspots per borough: the largest proportion of hotspots falls within North East London Integrated Care System). This ranges considerably between boroughs from Newham containing 140 LSOA hotspots to 3 boroughs containing only 1. This suggests a substantial level of demand inequality within this clinical complaint type.
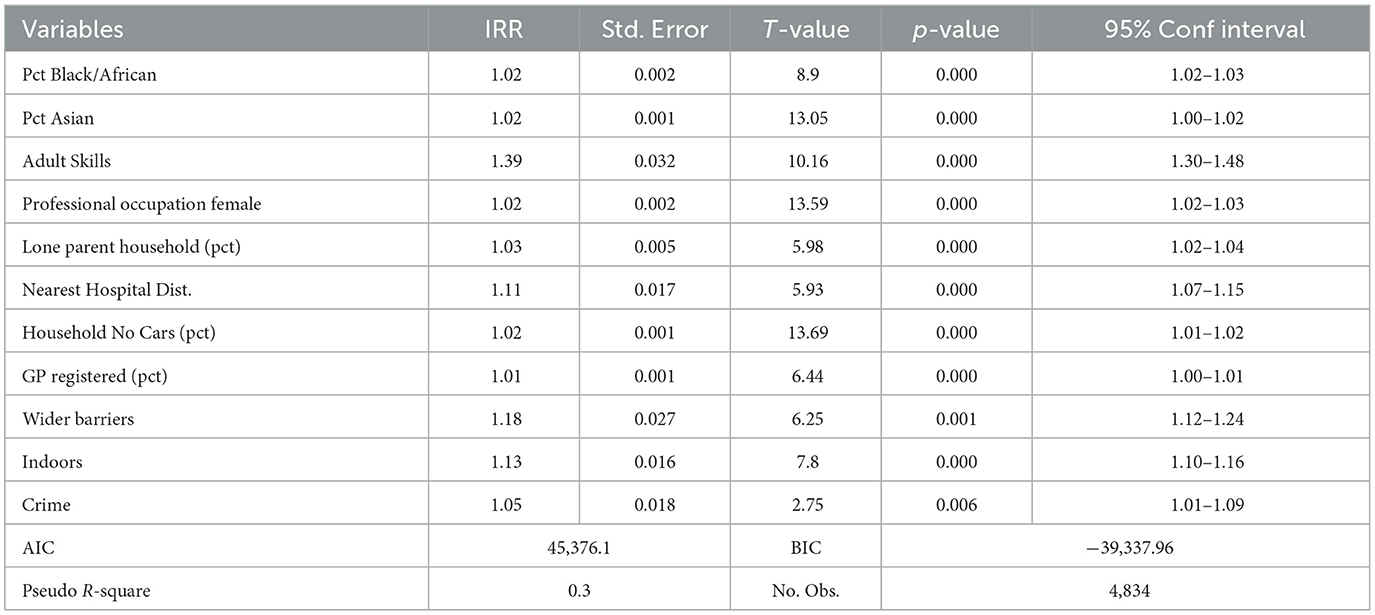
Our regression results (Table 2) show that neighborhoods with low rates amongst the Adult Skills IMD subdomain have an IRR of 1.39 (1.30–1.48), indicating a 39% higher rate of demand in neighborhoods with low adult skills. Low adult skills can contribute to a lack of understanding of alternative care pathways, early issue recognition and patient self-efficacy, the ability for a patient to seek appropriate healthcare services earlier. Other deprivation scores of wider barriers to housing and indoor housing conditions have scores of 1.18 (1.12–1.24) and 1.13 (1.1–1.16) respectively. This indicates that neighborhoods with a poorer housing quality have a 13% higher rate of pregnancy ambulance incidents.
Other meaningful associations are rates of households with no cars and distance of neighborhoods to a maternity hospital. These factors indicate that accessibility for patients to alternative local services may have an influence on a patient's decision to use ambulance services or seek alternative care before their circumstances become an emergency. Alternative/easier routes to a hospital rather than through ambulance use could also explain this strong relationship as patients may not wish to wait for an ambulance to arrive.
For the local regression results, some factors, including the percentage of residents with black ethnicity, have a consistent effect (IRR) across London boroughs. Other factors, such as Adult Skills, have a large distribution from borough to borough, with a difference in adult skills IRR values of 0.86 in Camden and 1.58 in Barking and Dagenham (Figure 6). This suggests that the effect of low adult skills varies across boroughs where healthcare services are delivered through different systems.
4 Discussion
Ambulance services are a small part of the NHS maternity care pathway. Many pregnant people will never need to use this service during their pregnancy; however, for those who do, it can be an important and crucial step in this pathway. One assumption made in this research is that high ambulance demand can be an indicator that maternity patients have poor health outcomes, as previous literature suggests this is the case for births that require emergency ambulance assistance (15, 63, 71, 72). Alternatively, another assumption that can explain factors associated with this demand is that patients have utilized ambulance services when an alternative option was more appropriate. Factors associated with high demand in this study can fall into one of these two categories.
Adult Skills, which include language abilities and qualification levels, have the strongest association of all the factors considered in this study. We argue that adult skills are a strong driver because this factor can fall into both categories of demand usage, poor health outcomes, and poor decision making. Poor health outcomes in many clinical fields have already been associated with lower rates of qualifications amongst populations. This can influence maternity demand as pregnant patients delayed seeking health services earlier in their care. This delay could turn an issue that may be treated elsewhere, or prevented, into a potential emergency that requires an ambulance. Areas where populations have higher qualifications may seek treatment either through GP appointments, or through a maternity hospital or midwife service provided, therefore avoiding ambulance service use. Adult Skill levels can also suggest how well patients can navigate the NHS care system. Poor language skills have been linked with poor pregnancy outcomes, as well as difficulty for patients to access healthcare services (59). Often it can be due to lack of understanding that patients can disengage with care or struggle to attend the consistent care and appointments that maternity patients require. Poor language skills are linked with maternity services being contacted later into pregnancies (27, 72). Our findings suggest that these associations will persist further into patients care and resolve with patients with these poorer language skills relying more heavily on emergency care during their pregnancy.
The strong associations between poor Adult Skills and higher ambulance demand can partially be explained through the lack of understanding of care pathways for pregnant patients and the utilization of ambulance services when this may not be the most appropriate outcome. Many NHS trusts' maternity units provide 24-h services for pregnant patients to call with concerns. Nevertheless, patients who utilize ambulances as an option may not have exhausted other alternative care pathways (13). A possible explanation of this association could be through poor adult skill levels in neighborhoods where ambulance calls are frequent but perhaps not necessary. Further exploration of this could be researched through individual ambulance patient records, or through data where the outcomes for patients, if they are treated at home or conveyed to an emergency department or other facility, indicate whether the call was necessary.
Housing quality deprivation, measured through both indoor living environments and wider barriers to housing, shows a strong association with ambulance maternity rates. Areas with high deprivation scores in wider barriers to housing (Table 1) were 18% more likely to have emergency incidents, while poorer indoor living environments had 11% higher rates. These associations can be linked to poor health outcomes in pregnancy, rather than whether patients utilize ambulances inappropriately. Previous links between health conditions and poor housing conditions indicate that this relationship is known (42), and these results show that this can manifest itself with higher demand on emergency ambulance care. Wider barriers to housing can again be linked through poorer maternity health outcomes, with stable access to housing having specific links to better pregnancy outcomes (36, 37). This study suggests that patients may resort to ambulance services as a response to these challenges.
The findings regarding ethnicity and its association with ambulance demand seemingly run contrary to previous literature regarding health outcomes, which consistently highlights a strong connection with pregnancy outcomes, particularly amongst the black ethnic category (24, 25). This implies that while ethnicity can indeed influence pregnancy results, this influence doesn't necessarily translate into heightened emergency ambulance utilization. It suggests a scenario where some patients might forego ambulance services even when essential, potentially leading to an underestimation of actual healthcare needs. Moreover, the study implies that the demand for ambulance services may not be directly tied to health outcomes; rather, it might be more closely associated with patients' reasons for calling an ambulance, irrespective of the actual necessity.
Another factor which supports that demand is linked to patient decision making is the distance of neighborhoods to a maternity hospital. Our findings suggest that the further an LSOA is from a maternity hospital the more likely it is that a patient may call an ambulance. An explanation for this could be that those who may live closer to maternity hospitals may forgo an ambulance to just travel directly to maternity facilities, which may be possible for many within a reasonable distance from a facility. This may be exasperated in more recent years as public perception of ambulance waiting times may lead to patients finding alternative ways to receive prompt appropriate healthcare.
Borough regression results indicate that for some factors the effects vary, while others have more consistent effects. The 'Black/Black British/Caribbean category shows a consistent effect across areas whilst for Adult Skills the effect is more varied. The links between borough differences can be linked to wider impacts on ambulance utilization and can be tied back to the reasons why patients will or will not call for an ambulance.
It is important to acknowledge the potential of improving equity within demand through better service resources' allocations and strategy designs (43). In London, the LAS is the only pan London NHS trust that operates in all 33 boroughs. This places it in the unique position to provide an equitable service across very distinct neighborhoods and help provide a continuity of care that other local NHS trusts may struggle to provide.
NHS England published a 3-year delivery plan for maternity and neonatal services, which sets out how trusts, Integrated Care Systems (ICS), and Integrated Care Board (ICB) can manage and improve maternity services and care in England. However, the strategy does not mention how joined pre-hospital services can be included as part of this care improvement. Ambulance trusts aren't mentioned at all within this plan (44). London Ambulance Trust describe providing specialized midwives as part of their strategy to provide specialized maternity care (17). These resources can be deployed to improve the outcomes for patients through a unique position of a continuity often across geographical areas that can span NHS trusts, as is the case within Greater London. This could improve care pathways where calls that do not require an emergency ambulance response are addressed with ambulance maternity resources and handed over to more appropriate maternity care locally, rather than conveyance to an emergency department (68). However, to understand the disparities between areas and target resources to reduce these inequalities, it is important to consider how other forms of healthcare at local levels are provided and their interaction and influence on ambulance utilization.
More widely, it is clear that ambulance demand can be influenced by healthcare services outside of emergency medical services. NHS local care framework is arranged through Integrated Care Systems (ICS) In London; this consists of five ICS, with boroughs divided into the five based on geography. The way that these care boards provide services have similarities, but also differences in funding priorities, staff levels, approaches to communications and outreach, resource distribution approaches, and can influence how patients may utilize healthcare services (45). Care provided by local NHS trusts and ICS can impact the outcomes of patients utilizing ambulance services either because of poor health outcomes or inappropriate usage. For example, the influence of poor Adult Skills on ambulance demand for maternity incidents could necessitate involving local NHS trusts to intervene and target communication to pregnant patients for healthcare access to reduce demand downstream. Clearer communication of local midwifery teams to emphasize that patients should call early and not wait for issues to become emergencies has the potential to reduce delays and patients requiring an ambulance.
Targeting the root causes of demand can also aim to decrease disparities in health. In regions like London, where social factors impact health and create vulnerable communities, addressing these issues can lead to improved population health outcomes, which in turn can alleviate pressure on health services such as ambulance services. For example, wider socio-economic policies that influence housing deprivation levels, if appropriately targeted for improvement, could also influence to reduce demand levels of ambulance services.
The benefits of identifying factors that drive demand in ambulance services are not just linked to improving equity, as specialized resources can be more effectively allocated, or overall demand reduced, this has the potential to benefit the overall ambulance resource allocation efficiency, as resources can be used alternatively on other incident types. This is particularly beneficial for maternity incident reduction as this clinical incident type often results in lengthy response times.
5 Conclusion
This research has identified significant inequalities within ambulance demand, which are predominantly explained by a range of socio-economic, environmental, and accessibility factors. Addressing these inequalities requires both short and long-term strategies. In the short term, ambulance services can adapt resource allocation to better target local disparities. For instance, specialized resources and training, such as a dedicated midwife team, can be deployed to improve patient care in areas with high maternity incident rates.
In the long term, broader societal interventions are essential. These could include enhancing access to healthcare, improving socio-economic conditions, and addressing environmental factors that contribute to health disparities. Such interventions not only reduce the demand for emergency healthcare services but also mitigate the underlying health inequalities. For policymakers and healthcare providers, this research underscores the need for targeted and tailored approaches to resource allocation and service delivery. It also highlights the potential benefits of integrated care models and community-based health initiatives.
Future research should continue to explore inequalities across different clinical groupings within ambulance demand. Additionally, examining demand through other lenses, such as acuity categories (e.g., categories 1–4) and conveyance rates, could provide further insights into how best to allocate resources and reduce disparities. Expanding the scope of research to include these dimensions will enhance our understanding of ambulance demand patterns and support the development of more effective intervention strategies.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions. London Ambulance Data needs to be approved by the NHS Trust Research Team if it is required to be shared. Requests to access these datasets should be directed to c2FtLm11cnBoeS4yMEB1Y2wuYWMudWs=.
Author contributions
SM: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. CZ: Conceptualization, Supervision, Writing – review & editing. FL: Conceptualization, Writing – review & editing. LR: Data curation, Writing – review & editing. YG: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project has received funding from the European Research Council (ERC) under the European Union's Horizon 2020 research and innovation programme (grant agreement no. 949670) and from Economic and Social Research Council, UK (grant no. ES/Y010558/1).
Acknowledgments
The authors would like to acknowledge the support of UBEL Doctoral Training Program. The authors than London Ambulance Service, particularly the Performance and Analytics Team for providing the dataset, offering advice and support throughout this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Alarilla A, Stafford M, Coughlan E, Keith J, Tallack C. Why have Ambulance waiting Times Been Getting Worse? Worcester, MA: The Health Foundation. (2022)
2. Mahase E. Ambulance trusts declare critical incidents amid “unprecedented” and “sustained” pressure. BMJ. (2022) 379:o3048. doi: 10.1136/bmj.o3048
3. Mahase E. Covid-19: hospital and ambulance services struggle with huge demand and staff illness. BMJ. (2022) 377:o950. doi: 10.1136/bmj.o950
4. Lowthian JA, Cameron PA, Stoelwinder JU, Curtis A, Currell A, Cooke MW, et al. Increasing utilisation of emergency ambulances. Aust Health Rev. (2011) 35:63. doi: 10.1071/AH09866
5. Lowthian JA, Jolley DJ, Curtis AJ, Currell A, Cameron PA, Stoelwinder JU, et al. The challenges of population ageing: accelerating demand for emergency ambulance services by older patients, 1995-2015. Med J Aust. (2011) 194:574–8. doi: 10.5694/j.1326-5377.2011.tb03107.x
6. Pearce JR, Richardson EA, Mitchell RJ, Shortt NK. Environmental justice and health: the implications of the socio-spatial distribution of multiple environmental deprivation for health inequalities in the United Kingdom: environmental justice and health. Trans Inst Br Geogr. (2010) 35:522–39. doi: 10.1111/j.1475-5661.2010.00399.x
7. Patel JA, Nielsen FBH, Badiani AA, Assi S, Unadkat VA, Patel B, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. (2020) 183:110–1. doi: 10.1016/j.puhe.2020.05.006
8. Russell J, Greenhalgh T, Lewis H, MacKenzie I, Maskrey N, Montgomery J, et al. Addressing the “postcode lottery” in local resource allocation decisions: a framework for clinical commissioning groups. J R Soc Med. (2013) 106:120–3. doi: 10.1177/0141076813479192
9. Regmi K, Mudyarabikwa O. A systematic review of the factors - barriers and enablers - affecting the implementation of clinical commissioning policy to reduce health inequalities in the National Health Service (NHS), UK. Public Health. (2020) 186:271–82. doi: 10.1016/j.puhe.2020.07.027
10. Hassler J, Ceccato V. Socio-spatial disparities in access to emergency health care—a scandinavian case study. PLOS ONE. (2021) 16:e0261319. doi: 10.1371/journal.pone.0261319
11. Thomson LJ, Gordon-Nesbitt R, Elsden E, Chatterjee HJ. The role of cultural, community and natural assets in addressing societal and structural health inequalities in the UK: future research priorities. Int J Equity Health. (2021) 20:249. doi: 10.1186/s12939-021-01590-4
12. Evans BA, Khanom A, Edwards A, Edwards B, Farr A, Foster T, et al. Experiences and views of people who frequently call emergency ambulance services: a qualitative study of UK service users. Health Expect. (2024) 27:e13856. doi: 10.1111/hex.13856
13. Booker MJ, Purdy S, Barnes R, Shaw ARG. Ambulance use for “primary care” problems: an ethnographic study of seeking and providing help in a UK ambulance service. BMJ Open. (2019) 9:e033037. doi: 10.1136/bmjopen-2019-033037
14. Heys S, Main C, Humphreys A, Torrance R. Displaced risk. Keeping mothers and babies safe: a UK ambulance service lens. Br Paramed J. (2023) 8:52–6. doi: 10.29045/14784726.2023.9.8.2.52
15. McLelland G, McKenna L, Morgans A, Smith K. Epidemiology of unplanned out-of-hospital births attended by paramedics. BMC Pregnancy Childbirth. (2018) 18:15. doi: 10.1186/s12884-017-1638-4
16. Andrew E, Nehme Z, Cameron P, Smith K. Drivers of increasing emergency ambulance demand. Prehosp Emerg Care. (2020) 24:385. doi: 10.1080/10903127.2019.1635670
17. LAS. Clinical quality indicators, London Ambulance Service NHS Trust. (2023). Available at: https://www.londonambulance.nhs.uk/about-us/how-we-aredoing/clinical-quality-indicators/ (accessed February 21, 2024).
18. Holmén J, Herlitz J, Ricksten SE, Strömsöe A, Hagberg E, Axelsson C, et al. Shortening ambulance response time increases survival in out-of-hospital cardiac arrest. J Am Heart Assoc. (2020) 9:e017048. doi: 10.1161/JAHA.120.017048
19. Price L. Treating the clock and not the patient: ambulance response times and risk. Qual Saf Health Care. (2006) 15:127–30. doi: 10.1136/qshc.2005.015651
20. Aringhieri R, Bruni ME, Khodaparasti S, van Essen JT. Emergency medical services and beyond: addressing new challenges through a wide literature review. Comput Oper Res. (2017) 78:349–68. doi: 10.1016/j.cor.2016.09.016
21. Grot M, Nagel L, Becker T, Mareike Fiebrandt P, Werners B. Fairness or efficiency-Managing this conflict in emergency medical services location planning. Comput Ind Eng. (2022) 173:108664. doi: 10.1016/j.cie.2022.108664
22. Cantwell K, Burgess S, Morgans A, Smith K, Livingston M, Dietze P, et al. Temporal trends in falls cases seen by EMS in melbourne. Injury. (2015) 47:266–71. doi: 10.1016/j.injury.2015.10.073
23. Dixon-Woods M. Learning from maternity service failures at East Kent Hospitals. BMJ. (2022) 379:o2755. doi: 10.1136/bmj.o2755
24. Kingdon C, Roberts D, Turner MA, Storey C, Crossland N, Finlayson KW, et al. Inequalities and stillbirth in the UK: a meta-narrative review. BMJ Open. (2019) 9:e029672. doi: 10.1136/bmjopen-2019-029672
25. Jardine J, Walker K, Gurol-Urganci I, Webster K, Muller P, Hawdon J, et al. Adverse pregnancy outcomes attributable to socioeconomic and ethnic inequalities in England: a national cohort study. Lancet. (2021) 398:1905–12. doi: 10.1016/S0140-6736(21)01595-6
26. Fernandez Turienzo C, Newburn M, Agyepong A, Buabeng R, Dignam A, Abe C, et al. Addressing inequities in maternal health among women living in communities of social disadvantage and ethnic diversity. BMC Public Health. (2021) 21:176. doi: 10.1186/s12889-021-10182-4
27. Heetkamp KM, Peters IA, Bertens LCM, Knapen MFCM. An unwanted pregnancy and language proficiency level are associated with first antenatal visit after the first trimester: Results from a prospective cohort study. Midwifery. (2020) 89:102784. doi: 10.1016/j.midw.2020.102784
28. Kramer MS, Séguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol. (2000) 14:194–210. doi: 10.1046/j.1365-3016.2000.00266.x
29. Tomanovic S. Experience of unplanned maternity: case studies of two young single mothers in Belgrade. Sociologija. (2020) 62:153–70. doi: 10.2298/SOC2002153T
30. Snelgrove JW, Murphy KE. Preterm birth and social inequality: assessing the effects of material and psychosocial disadvantage in a UK birth cohort. Acta Obstet Gynecol Scand. (2015) 94:766–75. doi: 10.1111/aogs.12648
31. Hanchate AD, Paasche-Orlow MK, Dyer KS, Baker WE, Feng C, Feldman J, et al. Geographic variation in use of ambulance transport to the emergency department. Ann Emerg Med. (2017) 70:533–43.e7. doi: 10.1016/j.annemergmed.2017.03.029
32. Varner CE, Park AL, Little D, Ray JG. Emergency department use by pregnant women in Ontario: a retrospective population-based cohort study. CMAJ Open. (2020) 8:E304–12. doi: 10.9778/cmajo.20190154
33. Jasani G, Liang Y, McNeilly B, Stryckman B, Marcozzi D, Gingold D, et al. Association between primary care availability and emergency medical services utilization. J Emerg Med. (2023) 64:448–54. doi: 10.1016/j.jemermed.2023.01.002
34. Clemens T, Dibben C. Living in stressful neighbourhoods during pregnancy: an observational study of crime rates and birth outcomes. Eur J Public Health. (2016) 27:197–202. doi: 10.1093/eurpub/ckw131
35. Rayment-Jones H, Dalrymple K, Harris JM, Harden A, Parslow E, Georgi T, et al. Project20: maternity care mechanisms that improve access and engagement for women with social risk factors in the UK – a mixed-methods, realist evaluation. BMJ Open. (2023) 13:e064291. doi: 10.1136/bmjopen-2022-064291
36. Leifheit KM, Schwartz GL, Pollack CE, Edin KJ, Black MM, Jennings JM, et al. Severe housing insecurity during pregnancy: association with adverse birth and infant outcomes. Int J Environ Res Public Health. (2020) 17:8659. doi: 10.3390/ijerph17228659
37. Robinson K, Sherman ADF, Ogunwole S, Meggett J, Sharps P. Social determinant of housing instability and adverse pregnancy outcomes: a scoping review. J Perinat Neonatal Nurs. (2022) 36:118–30. doi: 10.1097/JPN.0000000000000648
38. Hannam K, McNamee R, Baker P, Sibley C, Agius R. Air pollution exposure and adverse pregnancy outcomes in a large UK birth cohort: use of a novel spatio-temporal modelling technique. Scand J Work Environ Health. (2014) 40:518–30. doi: 10.5271/sjweh.3423
39. Shang L, Huang L, Yang L, Leng L, Qi C, Xie G, et al. Impact of air pollution exposure during various periods of pregnancy on term birth weight: a large-sample, retrospective population-based cohort study. Environ Sci Pollut Res. (2021) 28:3296–306. doi: 10.1007/s11356-020-10705-3
40. Anselin L. Local indicators of spatial association—LISA. Geogr Anal. (1995) 27:93–115. doi: 10.1111/j.1538-4632.1995.tb00338.x
41. Sauer J, Oshan T, Rey S, Wilf LJ. The importance of null hypotheses: understanding differences in local Moran's under heteroskedasticity. Geogr Anal. (2022) 54:752–68. doi: 10.1111/gean.12304
42. Nowak AL, Giurgescu C. The built environment and birth outcomes: a systematic review. MCN Am J Matern Child Nurs. (2017) 42:14–20. doi: 10.1097/NMC.0000000000000299
43. NHS England. Equity and equality: Guidance for local maternity systems. (2021). Available at: https://www.england.nhs.uk/~publication/equity-and-equality-guidance-for-localmaternity-systems/ (accessed February 21, 2024).
44. NHS England. Three year delivery plan for maternity and neonatal services. (2023). Available at: https://www.england.nhs.uk/wpcontent/uploads/2023/03/B1915-three-year-delivery-planfor-maternity-and-neonatal-services-march-2023.pdf (accessed February 21, 2024).
45. Charles A, Naylor C, Murray R. Integrated care systems in London: Challenges and opportunities ahead. (2021). Available at: https://assets.kingsfund.org.uk/f/256914/x/084d2c5253/integrated_care_systems_london_2021.pdf (accessed February 21, 2024).
46. Campagna S, Conti A, Dimonte V, Dalmasso M, Starnini M, Gianino MM, et al. Trends and characteristics of emergency medical services in Italy: a 5-years population-based registry analysis. Healthcare. (2020) 8:551. doi: 10.3390/healthcare8040551
48. Marmot M. Social determinants of health inequalities. Lancet. (2005) 365:1099–104. doi: 10.1016/S0140-6736(05)71146-6
49. Murphy A, Wakai A, Walsh C, Cummins F, O'Sullivan R. Development of key performance indicators for prehospital emergency care. Emerg Med J. (2016) 33:286–92. doi: 10.1136/emermed-2015-204793
50. Newton JN, Briggs AD, Murray CJ, Dicker D, Foreman KJ, Wang H, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2015) 386:2257–74.
51. Proctor A, Baxter H, Booker MJ. What factors are associated with ambulance use for non-emergency problems in children? A systematic mapping review and qualitative synthesis. BMJ Open. (2021) 11:e049443. doi: 10.1136/bmjopen-2021-049443
52. Puthussery S, Twamley K, Macfarlane A, Harding S, Baron M. “You need that loving tender care”: maternity care experiences and expectations of ethnic minority women born in the United Kingdom. J Health Serv Res Policy. (2010) 15:156–62. doi: 10.1258/jhsrp.2009.009067
53. Whittle RS, Diaz-Artiles A. An ecological study of socioeconomic predictors in detection of COVID-19 cases across neighborhoods in New York City. BMC Med. (2020) 18:271. doi: 10.1186/s12916-020-01731-6
54. Agyemang C, Vrijkotte TGM, Droomers M, Van Der Wal MF, Bonsel GJ, Stronks K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. J Epidemiol Commun Health. (2009) 63:755–60. doi: 10.1136/jech.2008.080408
55. Allen T, Walshe K, Proudlove N, Sutton M. The measurement and improvement of maternity service performance through inspection and rating: an observational study of maternity services in acute hospitals in England. Health Policy. (2020) 124:1233–8. doi: 10.1016/j.healthpol.2020.08.007
56. Farrant O., Eisen S, Van Tulleken C, Ward A, Longley N. Why asylum seekers deserve better healthcare, and how we can give it to them. BMJ. (2022) 376:n3069. doi: 10.1136/bmj.n3069
57. Gluck O, Pinchas-Cohen T, Hiaev Z, Rubinstein H, Bar J, Kovo M. The impact of childbirth education classes on delivery outcome. Int J Gynecol Obstet. (2020) 148:300–4. doi: 10.1002/ijgo.13016
58. Hadebe R, Seed PT, Essien D, Headen K, Mahmud S, Owasil S, et al. Can birth outcome inequality be reduced using targeted caseload midwifery in a deprived diverse inner city population? A retrospective cohort study, London, UK. BMJ Open. (2021) 11:e049991. doi: 10.1136/bmjopen-2021-049991
59. Henry J, Beruf C, Fischer T. Access to health care for pregnant Arabic-speaking refugee women and mothers in Germany. Qual Health Res. (2020) 30:437–47. doi: 10.1177/1049732319873620
60. Hong K, Hwang H, Han H, Chae J, Choi J, Jeong Y, et al. Perspectives on antenatal education associated with pregnancy outcomes: systematic review and meta-analysis. Women Birth. (2021) 34:219–30. doi: 10.1016/j.wombi.2020.04.002
61. LAS. Our Strategic Intent 2018/19—2022/23. London Ambulance Service NHS Trust (2017). Available at: https://www.londonambulance.nhs.uk/wp-content/uploads/2018/02/Our-strategic-intent-2.1.pdf
62. LAS. Annual Report & Accounts 2018/19. London Ambulance Service NHS Trust (2018). Available at: https://www.londonambulance.nhs.uk/wp-content/uploads/2019/08/London-Ambulance-Service-Annual-Report-Accounts-2018-19.pdf
63. Loughney A, Collis R, Dastgir S. Birth before arrival at delivery suite: associations and consequences. Br J Midwifery. (2006) 14:204–8. doi: 10.12968/bjom.2006.14.4.20786
64. Miranda ML, Maxson P, Edwards S. Environmental contributions to disparities in pregnancy outcomes. Epidemiol Rev. (2009) 31:67–83. doi: 10.1093/epirev/mxp011
65. Murugesu L, Damman OC, Timmermans DRM, De Wit S, Nieuwenhuijze M, Smets EMA, et al. Health literate-sensitive shared decision-making in maternity care: needs for support among maternity care professionals in the Netherlands. BMC Pregnancy Childbirth. (2023) 23:594. doi: 10.1186/s12884-023-05915-9
66. NHS Digital. Patients Registered at a GP Practice, January 2023 (2023). Available at: https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice/january-2023
67. Pantell MS, Baer RJ, Torres JM, Felder JN, Gomez AM, Chambers BD, et al. Associations between unstable housing, obstetric outcomes, and perinatal health care utilization. Am J Obstet Gynecol MFM. (2019) 1:100053. doi: 10.1016/j.ajogmf.2019.100053
68. Pinchbeck EW. Convenient primary care and emergency hospital utilisation. J Health Econ. (2019) 68:102242. doi: 10.1016/j.jhealeco.2019.102242
69. Rayment-Jones H, Harris J, Harden A, Khan Z, Sandall J. How do women with social risk factors experience United Kingdom maternity care? A realist synthesis. Birth. (2019) 46:461–74. doi: 10.1111/birt.12446
70. Schempf A, Strobino D, O'Campo P. Neighborhood effects on birthweight: an exploration of psychosocial and behavioral pathways in Baltimore, 1995–1996. Soc Sci Med. (2009) 68:100–10. doi: 10.1016/j.socscimed.2008.10.006
71. Thornton CE, Dahlen HG. Born before arrival in NSW, Australia (2000-2011): a linked population data study of incidence, location, associated factors and maternal and neonatal outcomes. BMJ Open. (2018) 8:e019328. doi: 10.1136/bmjopen-2017-019328
72. Unterscheider J, Ma'ayeh M, Geary MP. Born before arrival births: impact of a changing obstetric population. J Obstet Gynaecol. (2011) 31:721–3. doi: 10.3109/01443615.2011.605484
73. Urquia ML, Berger H, Ray JG. Risk of adverse outcomes among infants of immigrant women according to birth-weight curves tailored to maternal world region of origin. Can Med Assoc J. (2015) 187:E32–40. doi: 10.1503/cmaj.140748
74. Vik ES, Aasheim V, Nilsen RM, Small R, Moster D, Schytt E. Paternal country of origin and adverse neonatal outcomes in births to foreign-born women in Norway: a population-based cohort study. PLoS Med. (2020) 17:e1003395. doi: 10.1371/journal.pmed.1003395
Keywords: ambulance, inequality, maternity, pregnancy, pre-hospital, demand, equity, efficiency
Citation: Murphy S, Zhong C, Lopane FD, Rogerson L and Gong Y (2024) Socio-economic factors affecting spatial inequalities in pregnancy-related ambulance attendances in Greater London. Front. Disaster Emerg. Med. 2:1402957. doi: 10.3389/femer.2024.1402957
Received: 18 March 2024; Accepted: 07 October 2024;
Published: 28 October 2024.
Edited by:
Melanie Reuter-Oppermann, University of Twente, NetherlandsReviewed by:
Philipp Dahlmann, Deggendorf Institute of Technology, GermanyTheodoros Aslanidis, Agios Pavlos General Hospital, Greece
Copyright © 2024 Murphy, Zhong, Lopane, Rogerson and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sam Murphy, c2FtLm11cnBoeS4yMEB1Y2wuYWMudWs=; Chen Zhong, Yy56aG9uZ0B1Y2wuYWMudWs=
 Sam Murphy
Sam Murphy Chen Zhong
Chen Zhong Fulvio D. Lopane
Fulvio D. Lopane Luke Rogerson2
Luke Rogerson2 Yi Gong
Yi Gong