- 1Deggendorf Institute of Technology, Faculty of Applied Healthcare Sciences, Deggendorf, Germany
- 2Institute of Nursing Science and Practice, Paracelsus Medical University Salzburg, Salzburg, Austria
- 3Faculty of Health, School of Nursing Science, Witten/Herdecke University, Witten, Germany
Background: Acute patient care is becoming increasingly complex due to various factors (e.g., demographic changes, multimorbidity, organizational changes). Educating healthcare professionals as advanced practitioners at Master's level is one response to these challenges. Meanwhile, there are several empirical insights into advanced roles.
Aim: To provide an overview on the impact of advanced practitioners on acute care patients' outcomes and safety.
Methods: We conducted a mini-review. Therefore, a systematic literature search was carried out in the four databases Medline, CINAHL, Cochrane Library, and PEDro. After four researchers screened the results and extracted the data independently, the included studies were analyzed thematically and clustered along patients' outcomes. The results are presented narratively.
Results: 4,332 records were identified in the systematic search, and 67 articles were included in our review. Of these, the majority (n = 57) addressed the nursing profession. Advanced practitioners demonstrated an overall positive impact on acute care patients. They improved patients' vital signs, and reduced their mortality and adverse events (e.g., thrombosis, pneumonia, pressure injury). In addition, they shortened patients' length of stay and waiting times, and reduced admission rates. Patient satisfaction also increased after their implementation. When being compared to physicians, advanced practitioners in acute care demonstrated similar to equal patient outcomes and safety.
Conclusion: The identified studies highlight the benefits of advanced practitioners for acute care patients. While most studies were conducted in emergency departments or intensive care units, further research concerning other acute settings (e.g., psychiatry) or clinical conditions (e.g., cognitive impairment) is recommended.
1 Introduction
1.1 Background
Worldwide, healthcare professionals (HCP) are facing major changes in healthcare. Especially in acute care (AC), various factors lead to an increasingly complex area of action. On the one hand, demographic changes, multimorbidity, chronic diseases, polypharmacy (1), and more prescribers (2), among other factors, are reasons for the growing number of critically ill patients requiring complex treatment and intervention bundles (3, 4).
On the other hand, healthcare facilities have to deal with innovations, digitalization, and technological advances while considering hundreds of performance indicators, e.g., in the emergency department (ED) and intensive care unit (ICU) (5). The resulting complexity in acute care is defined as a “relational and dynamic phenomenon with multiple, interconnected processes characterized by its level of instability, uncertainty, and variability” (6).
To meet this growing complexity, facilities have to develop new organizational models and adopt these approaches in patient care (7). A key intervention is the renewed team composition (5), as HCPs are facing more complex treatment situations, and the demands and requirements on them are increasing (8–10). In order to ensure patient safety, a response to these increasing challenges is to educate nurses, physiotherapists and paramedics as advanced practitioners (AP), typically through specialized study programs and trainings.
Today, numerous international publications are available discussing the evaluation of APs (11–14). What is still missing, however, is an overview on the impact of APs on patients in AC.
1.2 Aim
The objective of our study is to derive and describe the impact of APs on AC patients' outcome and safety. In detail, we aim to provide an overview of different studies evaluating advanced practice nurses (APN), advanced practice physiotherapists (APPh), and advanced practice paramedics (APPa) in AC.
2 Methods
We designed a mini review. Therefore, two reviewers (LB, FS) independently carried out formative searches in the databases Medline (via PubMed) and Cumulative Index to Nursing and Allied Health Literature (CINAHL) to identify relevant keywords. Following this, we developed a systematic search in the entire research team.
Finally, we conducted the systematic search in the four databases Medline (via PubMed), CINAHL, Cochrane Library and PEDro (see Supplementary material S1) and documented this search according to the PRISMA methodology (15). The screening process was independently carried out by four reviewers who were or are still working as nurses (FS, LB), a physiotherapist (MF) or a paramedic (PD) in acute care.
In this review, we only included studies considering an AP as a person, who has a master's degree, and advanced knowledge and skills to ensure autonomous, situation-specific action. In their daily work, APs act in an evidence-based manner, and aim to ensure patient safety, improve outcomes, and reduce risks. They lead through complex, acute situations and have advanced decision-making skills. APs promote education in relation to health and illness, recognize training needs in practice, identify research gaps, develop questions from them, and use adequate methods to answer them sufficiently (16–19).
In addition to the reallocation of resources, studies had to define AC by the aspect of time. Most definitions consistently emphasize the unique characteristic of time pressure. Accordingly, AC encompasses all promotional, preventive, curative, rehabilitative, or palliative therapies whose effectiveness depends largely on time-sensitive and often rapid interventions (20, 21).
Furthermore, we only included English and German empirical studies or reviews that deal with APs in AC and evaluate their impact on patients. Publications were excluded if the description of their methodological approach was insufficient or missing, or if they only aimed to describe AP role development, but not AP evaluation.
After screening and data extraction, we initially subdivided the included studies along the investigated professions to derive better insights into advanced roles of each profession and their impact on patients. Studies were then thematically analyzed and outcomes were clustered using an inductive approach. Finally, the clusters were structured along the care process (diagnosis, treatment, results). As we did not critically appraise the included studies, results will only be presented in a narrative and descriptive form.
3 Results
In our systematic literature search, 4,332 records were identified. After removing 975 duplicates, we screened 3,357 titles and abstracts and 93 full texts. Finally, 67 studies were included in this review. The entire search and screening process is shown in Figure 1. Studies that were excluded during the full-text screening are integrated in Supplementary material S2.
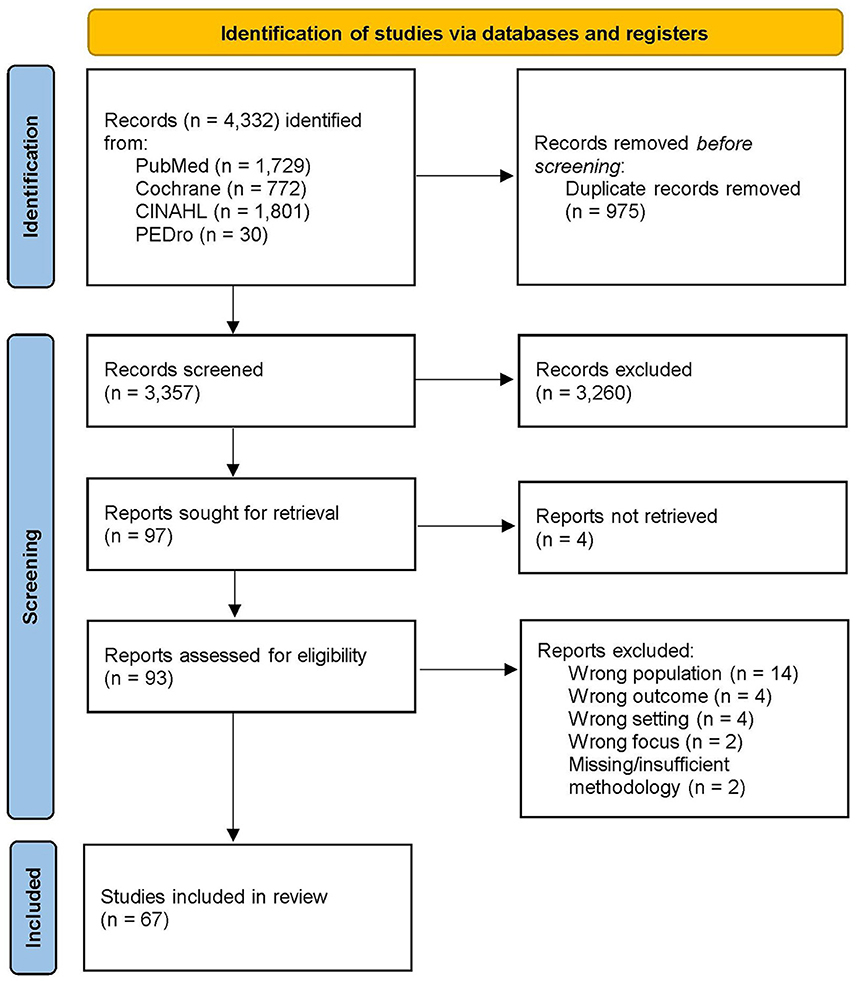
Figure 1. PRISMA-Flow diagram of the search and screening process (15).
In detail, we included 56 studies concerning advanced nursing roles (22–77), eight studies on advanced physiotherapy roles (78–85), two studies on advanced paramedics (86, 87), and one study concerning both advanced nurses and advanced physiotherapists (88).
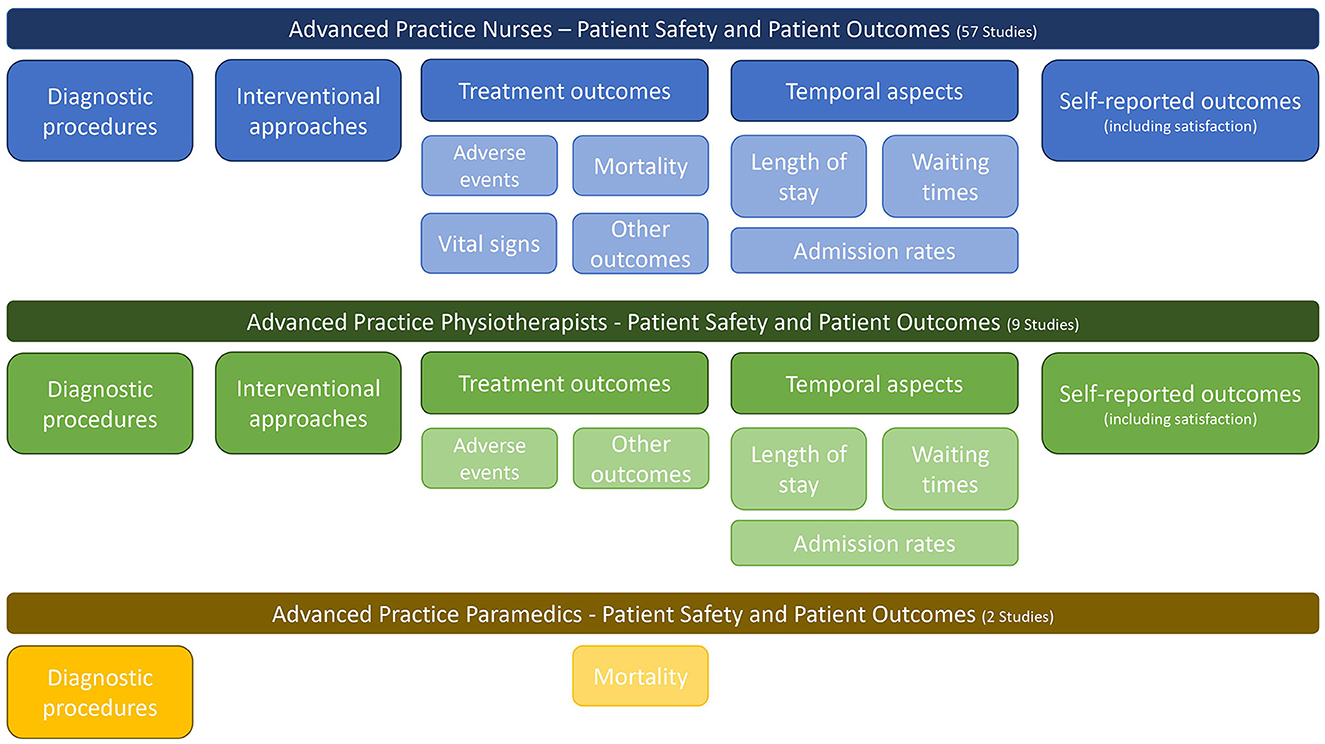
Figure 2 illustrates the major clusters of outcomes on which the identified studies and reviews can provide information. Along these clusters, the impact of APs on AC patients is reported below.
3.1 Impact of advanced practice nurses on patients' outcomes and safety
3.1.1 Diagnostic procedures
A total of 10 studies examined the diagnostic accuracy and competence of APNs. Compared to physicians, APNs ordered an equal number of diagnostic tests (25) and provided similar assessment and clinical examination results (77). APNs were also equally accurate or superior in the diagnosis and interpretation of X-rays in adults and children (28, 59, 69), fractures and other orthopedic injuries (51, 56, 60, 71), and electrocardiograms (61).
3.1.2 Interventional approaches
Another 12 articles reflected on treatments conducted by APNs in various situations. Comparing physicians and APNs, studies highlight equal interventional approaches in adults and children (24, 29, 57, 71, 77). Patients in APN groups received their surfactant sooner (24), were intubated more quickly (24), were offered analgesia more often (69), and reported an increase in nursing support, visits and provided information (35, 36, 54). The implementation of an APN led to an increased therapy involvement of patients and their families (55), and a decreased number of patients who left without treatment (64). Most minor injuries could also be treated independently by APNs (74).
3.1.3 Treatment outcomes
Six articles examined adverse events in patient treatment. Studies point to decreased complication rates after APN implementation (65). Advanced roles provided low complication rates when inserting central venous catheters (22), lower error rates in prescribing medication (27), reduced deep vein thrombosis rates (41), reduced pneumonia rates (41), and lower rates of hospital-acquired pressure injuries (44). While these five studies point to an equally low or decreased complication rate, one study did not examine any difference after the addition of an anesthesia APN (72).
Another five studies examined the impact of APNs on patients' vital signs. Neonates and babies were found to maintain or improve their vital signs (oxygen saturation, temperature, blood pressure, heart rate, blood gas) when being cared for by APNs (24, 53, 77). Also adult patients in APN groups experienced equal vital signs when compared to physician groups (52). In COPD patients, the implementation of APNs resulted in a higher oxygen saturation (23).
In addition, the overall mortality of AC patients decreased after the implementation of APNs in adults (62, 65, 75) and children (26). Compared to physicians, care provided by APNs resulted in an equal (42) or lower (50) ICU mortality and an equivalent hospital and 90-day mortality rate (50, 75).
Four studies examined other outcomes. APNs in an urgent care team could reduce the baseline dyspnea index in COPD patients (23). APNs also performed circumcisions on children, with equal results compared to physicians (39). Furthermore, body and limb functions as well as the ability to return to work were equal in APN and physician groups (88). Hemodialysis patients showed better blood parameters when being cared for by APNs additionally (67).
3.1.4 Temporal aspects
Twenty-one articles investigated patients' length of stay (LOS) as an outcome. The overall hospital LOS decreased in all studies reporting on the implementation of APNs (30, 32, 55, 63, 65, 70). When comparing APNs and physicians, studies highlight an either equal LOS (33, 46, 57, 75) or a decreased LOS in APN groups for adults (26, 37, 41, 50, 71, 75) and children (76). The ICU LOS decreased also after the implementation of APNs (38, 41, 62, 65). Compared to physicians, patients' ICU LOS was equal in adults (50) or reduced in children (35) when being cared for by APNs. The ED LOS was also reduced after the APN implementation (62) and when compared to physician-only groups (75). The hospital unit LOS was also decreased after the implementation of an APN (63). Only one study reported no difference in the ED LOS after APN implementation (68).
Another 14 articles examined the impact of APNs on patients' waiting times in different settings. Most studies report on overall shorter (28, 31, 45, 68, 70, 75) or equal (46, 68, 69, 71, 75) ED waiting times comparing APNs and physicians. Other studies demonstrate shorter times to first visits, diagnosis, and treatments (58, 62, 75) in the ED and the ICU, e.g., a faster application of analgesia (47) or stroke treatment (75) in APN groups. Concerning children, studies report a faster response to transfers after an APN implementation (53), but no difference in the preoperative preparation time (72).
In addition, a total of 14 studies examined the admission to and within a hospital. These highlight a lower hospital admission (49, 58) and readmission rate (66) after APN implementation. Compared to physicians, hospital admission and readmission rates were lower (26, 33, 43, 61) or equally low (36, 46, 70) in APN groups. Within the hospital, the implementation of APNs led to a reduced (40) or similar (62) ICU admission rate. Following a hospital stay, the time to transfer to rehabilitation could be reduced by implementing APNs (41). Another study found no difference in the transfer rate to follow-up clinics between APNs and physicians (31).
3.1.5 Self-reported outcomes
A further 23 studies investigated the impact of APNs on outcomes reported by patients themselves. While the implementation of APNs seemed to have no effect on patients' self-esteem and the maternal affect (26), it led to decreased psychological distress and increased perceived self-efficacy (73). Quality of life improved after implementation (67) and was equally high when compared to physician groups (88). Another 19 studies reflect on patients' satisfaction with the care provided by APNs. Overall, patients indicate a high (32, 34, 54, 59, 61, 63, 73, 75) or increased (67) level of satisfaction following APN implementation. Compared to physicians, patients in APN groups report an equal (28, 31, 52, 64, 70, 75) or higher (26, 48, 75) level of satisfaction with care. One study found that parental satisfaction did not change after the implementation of an anesthesia APN (72).
3.2 Impact of advanced practice physiotherapists on patients' outcomes and safety
3.2.1 Diagnostic procedures
A total of four studies examined the diagnostic skills of APPhs. As reported in three studies (80, 83, 84), there is a high level of agreement in terms of diagnosis between APPhs and surgeons. APPhs were able to diagnose an equal number of patients compared to physicians (82), and were twice more likely to correctly identify surgical patients in triage (80).
3.2.2 Interventional approaches
Another two studies reflected on the treatment provided by APPhs. One study highlights that APPhs made an autonomous decision regarding patient management in 77% of the included cases, and APPhs managed patients' treatment pathways without referral to a physician in four out of five cases (78). Comparing APPhs and physicians, one study (80) determines an almost equal treatment agreement in orthopedic patients with chronic hip and knee pain.
3.2.3 Treatment outcomes
Overall, two studies examined treatment outcomes. The first study found no difference in adverse events when patients were treated by either APPhs or physicians in the ED (79). In the second study, other outcomes were compared between APPh and physician groups, resulting in equal functional recovery of patients with tissue injuries and their ability to return to work in the same amount of time (88).
3.2.4 Temporal aspects
Length of stay as an outcome for patients in the ED with musculoskeletal complaints was investigated in two studies. In one study, the implementation of APPhs as primary contact clinicians for patients shortened the time between admission and discharge (79). In another study, a decrease in the LOS of patients treated by APPhs compared to those treated by APNs or physicians was determined (85).
The influence of APPhs on waiting times for ED patients was examined in three studies. An overall shorter waiting time, a shorter time to treatment (85) and a shorter time from triage to assessment (79) were reported. Patients with musculoskeletal complaints also received analgesia sooner after the implementation of an APPh (81).
Focusing on admission rates, there was a reduced 30-day re-attendance in urgent care centers for patients treated by APPhs (82). Compared to treatment by APNs or physicians, fewer APPh patients were admitted to hospital (85).
3.2.5 Self-reported outcomes
The results of two studies highlighted patients' self-reported experiences. One study indicated an equal quality of life 2–8 weeks after a tissue injury when the patients were treated by either APPhs or physicians (88). Patients also reported that they were highly satisfied with the treatment provided by APPhs (84).
3.3 Impact of advanced practice paramedics on patients' outcomes and safety
Overall, two studies reported outcomes after an APPa implementation. One study showed a high concordance between APPa diagnosis and in-hospital diagnosis (86). Another study reported an increase in patients' long-term survival rate when an APPa was involved in the treatment of their out of hospital cardiac arrest (87).
4 Discussion
4.1 Summary of evidence
This mini review aimed to provide an overview on the impact of APs in AC. The results of this study emphasize that APs have an overall positive impact on acute patients' outcomes and safety. Included studies point to an improved quality of care after the implementation of APs and similar or equal patient outcomes when comparing APs and physicians. APs could also provide a high quality of care for complex cohorts (e.g., preterm babies), resulting in reduced mortality rates, shorter LOS, or an overall increased patient satisfaction.
These findings are in line with the results of research in other settings. A systematic review on cancer patients indicates that patient satisfaction and symptom management were considerably improved by APs (89). Another study on geriatric outpatients highlights reduced waiting times and faster access to care (90), as also described by our review. An additional review on patients with chronic kidney disease reports improved laboratory parameters and vital signs after the implementation of APs (91).
While most of our included studies were conducted in the ED and the ICU and focused on the implementation of APs into a specific setting, studies on APs that deal with specific conditions (e.g., ECMO, respiration, cognitive impairments) are still lacking. In addition, studies on prehospital or rehabilitative acute care are missing. Moreover, we could only identify one study from the area of psychiatry (73).
The transition between acute and long-term care is fluid and not sharp in many places. While our review was rigorous in its approach and only included studies when highlighting the factor “time”, we also identified studies reflecting on APs in subacute and long-term patient care (92–95).
Most of the studies in our review deal with APNs. While 57 studies are available for this group in AC and numerous findings on patient outcomes can be identified, there is a lack of further evidence for APPhs (n = 9) and APPas (n = 2). This is certainly due to the much later development of advanced roles in the field of physiotherapy and paramedicine.
The methodological approach of these studies was quite similar. On the one hand, observational designs were used to evaluate the implementation of APs using a pre/post comparison. On the other hand, patients were grouped, treated by APs or physicians, and then compared with each other. Whether it is always appropriate to compare APs with physicians is open to debate. The results of the studies are convincing and indicate that some activities can be taken over by APs. This can also reduce the workload of physicians and free up their resources. It must be the clear objective to work together in order to ensure high-quality care for patients and not to be irritated by these comparisons against each other.
4.2 Limitations
The quality of included studies varies widely. However, due to the mini review design, we did not conduct a critical appraisal of the retrieved results. Therefore, our findings have to be interpreted with caution. In addition, we only included German and English articles. Relevant studies published in other languages may have been excluded. Publication bias can also not be ruled out.
Furthermore, we chose a one-sided perspective on the subject. While we were only concerned with the role of the APs, it remains unclear what other HCPs were doing in the care of the patients. In addition, we only extracted the outcomes relevant to the patient. We did not consider any further aspects such as cost effectiveness, which may also be relevant to the process.
5 Conclusion
The results of this review demonstrate the overall and differentiated benefits of APs. In the vast majority of included studies, their implementation in AC led to improved patient outcomes and safety or to equivalent results when compared to physicians. Thus, the assumption that APs are a key response to the increasing complexity in AC can be confirmed.
Therefore, we highly recommend the development and implementation of AP roles in acute settings. Nevertheless, an appropriate implementation process for APs is crucial to effectively provide high-quality care to patients. The integration of new roles is therefore an overall task for the entire healthcare facilities and their respective AC teams.
While APNs appear to be widely investigated, research on APPhs and APPas is still lacking. Future studies should therefore focus on the evaluation of advanced roles in physiotherapy and paramedicine. Furthermore, specific acute settings (e.g., psychiatry) and conditions (e.g., cognitive impairment) need to be addressed.
Author contributions
LB: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing, Validation. MF: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing, Validation. PD: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing, Validation. CR: Conceptualization, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing, Supervision. FS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/femer.2024.1399779/full#supplementary-material
References
1. Naik H, Murray TM, Khan M, Daly-Grafstein D, Liu G, Kassen BO, et al. Population-based trends in complexity of hospital inpatients. JAMA Intern Med. (2024) 184:183–92. doi: 10.1001/jamainternmed.2023.7410
2. Maciejewski ML, Powers BJ, Sanders LL, Farley JF, Hansen RA, Sleath B, et al. The intersection of patient complexity, prescriber continuity and acute care utilization. J Gen Intern Med. (2014) 29:594–601. doi: 10.1007/s11606-013-2746-0
3. Vincent J-L. Critical care - where have we been and where are we going? Crit care. (2013) 17:S2. doi: 10.1186/cc11500
4. Arabi YM, Azoulay E, Al-Dorzi HM, Phua J, Salluh J, Binnie A, et al. How the COVID-19 pandemic will change the future of critical care. Intens Care Med. (2021) 47:282–91. doi: 10.1007/s00134-021-06352-y
5. Austin EE, Blakely B, Tufanaru C, Selwood A, Braithwaite J, Clay-Williams R. Strategies to measure and improve emergency department performance: a scoping review. Scand J Trauma Resusc Emerg Med. (2020) 28:55. doi: 10.1186/s13049-020-00749-2
6. Huber E, Kleinknecht-Dolf M, Kugler C, Spirig R. Patient-related complexity of nursing care in acute care hospitals - an updated concept. Scand J Caring Sci. (2021) 35:178–95. doi: 10.1111/scs.12833
7. Pietrantonio F, Orlandini F, Moriconi L, La Regina M. Acute complex care model: an organizational approach for the medical care of hospitalized acute complex patients. Eur J Intern Med. (2015) 26:759–65. doi: 10.1016/j.ejim.2015.08.011
8. Egerod I, Kaldan G, Nordentoft S, Larsen A, Herling SF, Thomsen T, et al. Skills, competencies, and policies for advanced practice critical care nursing in Europe: a scoping review. Nurse Educ Pract. (2021) 54:103142. doi: 10.1016/j.nepr.2021.103142
9. Bhutta ZA, Chen L, Cohen J, Crisp N, Evans T, Fineberg H, et al. Education of health professionals for the 21st century: a global independent Commission. Lancet. (2010) 375:1137–8. doi: 10.1016/S0140-6736(10)60450-3
10. Codreanu A. A VUCA action framework for a VUCA environment. Leadership challenges and solutions. J Defense Resour Manage. (2016) 7:31–8. Available online at: https://doaj.org/article/de3b2db947d7499fac1f7c3a6e75ec84
11. Kleinpell RM, Grabenkort WR, Kapu AN, Constantine R, Sicoutris C. Nurse practitioners and physician assistants in acute and critical care: a concise review of the literature and data 2008-2018. Crit Care Med. (2019) 47:1442–9. doi: 10.1097/CCM.0000000000003925
12. Denton G, Davies V, Whyman E, Arora N. A narrative review of the training structure, role, and safety profile of advanced critical care practitioners in adult intensive services in the United Kingdom. Aust Crit Care. (2023) 36:145–50. doi: 10.1016/j.aucc.2022.12.005
13. Scanlon A, Murphy M, Smolowitz J, Lewis V. Advanced nursing practice and advanced practice nursing roles within low and lower-middle-income countries. J Nurs Scholarsh. (2023) 55:484–93. doi: 10.1111/jnu.12838
14. Bryant-Lukosius D, Dicenso A. A framework for the introduction and evaluation of advanced practice nursing roles. J Adv Nurs. (2004) 48:530–40. doi: 10.1111/j.1365-2648.2004.03235.x
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
16. Chartered Society of Physiotherapy (CSP). Advanced Practice in Physiotherapy: Understanding the Contribution of Advanced Practice in Physiotherapy to Transforming Lives, Maximising Independence and Empowering Populations. (2017). Available online at: https://ss-usa.s3.amazonaws.com/c/308473270/media/58755da45096b287d86254784974192/CSP_Advanced_Practice_Physiotherapy%20%282016%29.pdf (accessed February 5, 2024).
17. Health Education England (HEE) National Health Service England (NHS). Multi-professional Framework for Advanced Clinical Practice in England. (2017). https://healtheducationengland.sharepoint.com/sites/APWC/_layouts/15/download.aspx?SourceUrl=%2Fsites%2FAPWC%2FShared%20Documents%2FHome%2FMulti%2Dprofessional%20framework%20for%20advanced%20clinical%20practice%20in%20England%2Fmulti%2Dprofessionalframeworkforadvancedclinicalpracticeinengland%20%281%29%2Epdf (accessed February 5, 2024).
18. International Council of Nurses (ICN). Guidelines on Advanced Practice Nursing. (2020). Available online at: https://www.icn.ch/system/files/documents/2020-04/ICN_APN%20Report_EN_WEB.pdf (accessed October 30, 2023).
19. World Physiotherapy. Advanced Physical Therapy Practice: Policy Statement. (2019). Available online at: https://world.physio/sites/default/files/2020-04/PS-2019-APTP_0.pdf (accessed February 5, 2024).
20. Canadian Institute for Health Information (CIHI). Acute Care. (2023). Available online at: https://www.cihi.ca/en/topics/acute-care (accessed October 30, 2023).
21. Hirshon JM, Risko N, Calvello E, Stewart de Ramirez S, Narayan M, Theodosis C, et al. Health systems and services: the role of acute care. Bull World Health Org. (2013) 91:386–8. doi: 10.2471/BLT.12.112664
22. Alexandrou E, Spencer TR, Frost SA, Mifflin N, Davidson PM, Hillman KM. Central venous catheter placement by advanced practice nurses demonstrates low procedural complication and infection rates - a report from 13 years of service. Crit Care Med. (2014) 42:536–43. doi: 10.1097/CCM.0b013e3182a667f0
23. Ansari K, Shamssain M, Farrow M, Keaney NP. Hospital-at-home care for exacerbations of chronic obstructive pulmonary disease: an observational cohort study of patients managed in hospital or by nurse practitioners in the community. Chron Respir Dis. (2009) 6:69–74. doi: 10.1177/1479972309102728
24. Aubrey WR, Yoxall CW. Evaluation of the role of the neonatal nurse practitioner in resuscitation of preterm infants at birth. Arch Dis Child Fetal Neonatal Ed. (2001) 85:F96–9. doi: 10.1136/fn.85.2.F96
25. Begaz T, Elashoff D, Grogan TR, Talan D, Taira BR. Differences in test ordering between nurse practitioners and attending emergency physicians when acting as Provider in Triage. Am J Emerg Med. (2017) 35:1426–9. doi: 10.1016/j.ajem.2017.04.027
26. Brooten D, Naylor MD, York R, Brown LP, Munro BH, Hollingsworth AO, et al. Lessons learned from testing the quality cost model of Advanced Practice Nursing (APN) transitional care. J Nurs Scholarsh. (2002) 34:369–75. doi: 10.1111/j.1547-5069.2002.00369.x
27. Carberry M, Connelly S, Murphy J, A. prospective audit of a nurse independent prescribing within critical care. Nurs Crit Care. (2013) 18:135–41. doi: 10.1111/j.1478-5153.2012.00534.x
28. Carter AJE, Chochinov AH, A. systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. CJEM. (2007) 9:286–95. doi: 10.1017/S1481803500015189
29. Choudhry N, Charlton C, Bodansky D, Ul Islam S, Doherty J, Liversedge G, et al. Performance of advanced nurse practitioners in minor trauma patients. J. Nurse Pract. (2021) 17:723–6. doi: 10.1016/j.nurpra.2021.01.005
30. Collins N, Miller R, Kapu A, Martin R, Morton M, Forrester M, et al. Outcomes of adding acute care nurse practitioners to a Level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction. J Trauma Acute Care Surg. (2014) 76:353–7. doi: 10.1097/TA.0000000000000097
31. Cooper MA, Lindsay GM, Kinn S, Swann IJ. Evaluating Emergency Nurse Practitioner services: a randomized controlled trial. J Adv Nurs. (2002) 40:721–30. doi: 10.1046/j.1365-2648.2002.02431.x
32. Dach C, von Lendner I, Cecini R. Implementierung einer “Nurse Practitioner”-Rolle in der stationären. Chirurgie Pflege. (2023) 36:179–85. doi: 10.1024/1012-5302/a000924
33. David D, Britting L, Dalton J. Cardiac acute care nurse practitioner and 30-day readmission. J Cardiovasc Nurs. (2015) 30:248–55. doi: 10.1097/JCN.0000000000000147
34. Desrochers F, Donivan E, Mehta A, Laizner AM. A psychosocial oncology program: perceptions of the telephone-triage assessment. Support Care Cancer. (2016) 24:2937–44. doi: 10.1007/s00520-016-3091-8
35. Fanta K, Cook B, Falcone RA, Rickets C, Schweer L, Brown RL, et al. Pediatric trauma nurse practitioners provide excellent care with superior patient satisfaction for injured children. J Pediatr Surg. (2006) 41:277–81. doi: 10.1016/j.jpedsurg.2005.10.049
36. Fedel PR, Pennington G. Clinical nurse specialist collaboration with a community-based palliative care program: an evidence-based practice project. Clin Nurse Spec. (2021) 35:88–95. doi: 10.1097/NUR.0000000000000581
37. Fry M, Fong J, Asha S, Arendts G. A 12-month evaluation of the impact of transitional emergency nurse practitioners in one metropolitan Emergency Department. Aust Emerg Nurs J. (2011) 14:4–8. doi: 10.1016/j.aenj.2010.10.001
38. Fukuda T, Sakurai H, Kashiwagi M. Efforts to reduce the length of stay in a low-intensity ICU: Changes in the ICU brought about by collaboration between Certified Nurse Specialists as head nurses and intensivists. PLoS ONE. (2020) 15:e0234879. doi: 10.1371/journal.pone.0234879
39. Giramonti KM, Kogan BA. Pediatric penile surgery by a nurse practitioner in the operating room. J Pediatr Urol. (2018) 14:573–6. doi: 10.1016/j.jpurol.2018.07.027
40. Green A, Edmonds L. Bridging the gap between the intensive care unit and general wards-the ICU Liaison Nurse. Intens Crit Care Nurs. (2004) 20:133–43. doi: 10.1016/S0964-3397(04)00024-2
41. Holliday A, Samanta D, Budinger J, Hardway J, Bethea A. An outcome analysis of nurse practitioners in acute care trauma services. J Trauma Nurs. (2017) 24:365–70. doi: 10.1097/JTN.0000000000000327
42. Huang M-H, Hsieh H-Y, van de Mortel T. The impact of the addition of nurse practitioners to surgical intensive care units: a retrospective cohort study. Aust Crit Care. (2019) 32:244–8. doi: 10.1016/j.aucc.2018.05.004
43. Huws DW, Cashmore D, Newcombe RG, Roberts C, Vincent J, Elwyn G. Impact of case management by advanced practice nurses in primary care on unplanned hospital admissions: a controlled intervention study. BMC Health Serv Res. (2008) 8:115. doi: 10.1186/1472-6963-8-115
44. Irvin C, Sedlak E, Walton C, Collier S, Bernhofer EI. Hospital-acquired pressure injuries: the significance of the advanced practice registered nurse's role in a community hospital. J Am Assoc Nurse Pract. (2017) 29:203–8. doi: 10.1002/2327-6924.12440
45. Jennings N, Clifford S, Fox AR, O'Connell J, Gardner G. The impact of nurse practitioner services on cost, quality of care, satisfaction and waiting times in the emergency department: a systematic review. Int J Nurs Stud. (2015) 52:421–35. doi: 10.1016/j.ijnurstu.2014.07.006
46. Jennings N, Gardner G, O'Reilly G, Mitra B. Emergency NP model of care in an Australian Emergency Department. J Nurse Practit. (2015) 11:774–81. doi: 10.1016/j.nurpra.2015.05.008
47. Jennings N, Gardner G, O'Reilly G, Mitra B. Evaluating emergency nurse practitioner service effectiveness on achieving timely analgesia: a pragmatic randomized controlled trial. Acad Emerg Med. (2015) 22:676–84. doi: 10.1111/acem.12687
48. Jennings N, Lee G, Chao K, Keating S. A survey of patient satisfaction in a metropolitan Emergency Department: comparing nurse practitioners and emergency physicians. Int J Nurs Pract. (2009) 15:213–8. doi: 10.1111/j.1440-172X.2009.01746.x
49. Kemp AE. Mass-gathering events: the role of advanced nurse practitioners in reducing referrals to local health care agencies. Prehosp Disaster Med. (2016) 31:58–63. doi: 10.1017/S1049023X15005543
50. Landsperger JS, Semler MW, Wang L, Byrne DW, Wheeler AP. Outcomes of nurse practitioner-delivered critical care: a prospective cohort study. Chest. (2016) 149:1146–54. doi: 10.1016/j.chest.2015.12.015
51. Lau LH, Kerr D, Law I, Ritchie P. Nurse practitioners treating ankle and foot injuries using the Ottawa Ankle Rules: a comparative study in the emergency department. Australas Emerg Nurs J. (2013) 16:110–5. doi: 10.1016/j.aenj.2013.05.007
52. Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary care outcomes in patients treated by nurse practitioners or physicians: two-year follow-up. Med Care Res Rev. (2004) 61:332–51. doi: 10.1177/1077558704266821
53. Leslie A, Stephenson T. Neonatal transfers by advanced neonatal nurse practitioners and paediatric registrars. Arch Dis Child Fetal Neonatal Ed. (2003) 88:F509–12. doi: 10.1136/fn.88.6.F509
54. McDevitt J, Melby V. An evaluation of the quality of Emergency Nurse Practitioner services for patients presenting with minor injuries to one rural urgent care centre in the UK: a descriptive study. J Clin Nurs. (2015) 24:523–35. doi: 10.1111/jocn.12639
55. Miller SK. Impact of a gerontological nurse practitioner on the nursing home elderly in the acute care setting. AACN Clin Issues. (1997) 8:609–15. doi: 10.1097/00044067-199711000-00012
56. Miniard JL, Ballman K. Nurse practitioner triage of the neurosurgical patient: a patient-centered care delivery model. J Neurosci Nurs. (2018) 50:244–6. doi: 10.1097/JNN.0000000000000374
57. Morris DS, Reilly P, Rohrbach J, Telford G, Kim P, Sims CA. The influence of unit-based nurse practitioners on hospital outcomes and readmission rates for patients with trauma. J Trauma Acute Care Surg. (2012) 73:474–8. doi: 10.1097/TA.0b013e31825882bb
58. Moxham L, McMahon-Parkes K. An evaluation of the impact of advanced nurse practitioner triage and clinical intervention for medically expected patients referred to an acute National Health Service hospital. J Clin Nurs. (2020) 29:3679–86. doi: 10.1111/jocn.15392
59. Organ K, Chinnick P, Stanhope B. Evaluating the introduction of a paediatric emergency nurse practitioner service. Emerg Nurse. (2005) 13:8–11. doi: 10.7748/en.13.7.8.s14
60. Resler J, Hackworth J, Mayo E, Rouse TM. Detection of missed injuries in a pediatric trauma center with the addition of acute care pediatric nurse practitioners. J Trauma Nurs. (2014) 21:272–5; quiz 276-7. doi: 10.1097/JTN.0000000000000080
61. Roche TE, Gardner G, Jack L. The effectiveness of emergency nurse practitioner service in the management of patients presenting to rural hospitals with chest pain: a multisite prospective longitudinal nested cohort study. BMC Health Serv Res. (2017) 17:445. doi: 10.1186/s12913-017-2395-9
62. Sa W, Shuihong C, Jingfen J, Mao Z, Zhiting G, Danping Y, et al. The effect of trauma advanced practice nurse programme at a Level I regional trauma centre in mainland China. Nurs Open. (2023) 10:6559–65. doi: 10.1002/nop2.1911
63. Sarkissian S, Wennberg R. Effects of the acute care nurse practitioner role on epilepsy monitoring outcomes. Outcomes Manag Nurs Pract. (1999) 3:161–6.
64. Shand W, Klemmer D, Grubb S, Chesney S, Olsen B, So L. Research to action: nurse practitioners in the emergency department, emergency department transition clinic and intravenous therapy clinic at Strathcona Community Hospital. CJEN. (2020) 43:23–7. doi: 10.29173/cjen44
65. Sise CB, Sise MJ, Kelley DM, Walker SB, Calvo RY, Shackford SR, et al. Resource commitment to improve outcomes and increase value at a level I trauma center. J Trauma. (2011) 70:560–8. doi: 10.1097/TA.0b013e31820c7b79
66. Smith J, Pan D, Novelli M. A nurse practitioner–led intervention to reduce hospital readmissions. J Nurse Practit. (2016) 12:311–6. doi: 10.1016/j.nurpra.2015.11.020
67. Stanley M, Worrall-Carter L, Rahman MA, McEvedy S, Langham R. Assessment of an established dialysis nurse practitioner model of care using mixed methods research. Contemp Nurse. (2015) 51:148–62. doi: 10.1080/10376178.2016.1157029
68. Steiner IP, Nichols DN, Blitz S, Tapper L, Stagg AP, Sharma L, et al. Impact of a nurse practitioner on patient care in a Canadian emergency department. CJEM. (2009) 11:207–14. doi: 10.1017/S1481803500011222
69. Thompson W, Meskell P. Evaluation of an advanced nurse practitioner (emergency care)—An Irish perspective. J Nurse Practit. (2012) 8:200–5. doi: 10.1016/j.nurpra.2011.09.002
70. Tucker A, Bernard M. Making the case for nurse practitioners in the emergency department: a clinical case study. Adv Emerg Nurs J. (2015) 37:308–12. doi: 10.1097/TME.0000000000000081
71. van der Linden C, Reijnen R, de Vos R. Diagnostic accuracy of emergency nurse practitioners versus physicians related to minor illnesses and injuries. J Emerg Nurs. (2010) 36:311–6. doi: 10.1016/j.jen.2009.08.012
72. Varughese AM, Byczkowski TL, Wittkugel EP, Kotagal U, Dean Kurth C. Impact of a nurse practitioner-assisted preoperative assessment program on quality. Paediatr Anaesth. (2006) 16:723–33. doi: 10.1111/j.1460-9592.2006.01856.x
73. Wand T, White K, Patching J, Dixon J, Green T. Outcomes from the evaluation of an emergency department-based mental health nurse practitioner outpatient service in Australia. J Am Acad Nurse Pract. (2012) 24:149–59. doi: 10.1111/j.1745-7599.2011.00709.x
74. Wilson A, Shifaza F. An evaluation of the effectiveness and acceptability of nurse practitioners in an adult emergency department. Int J Nurs Pract. (2008) 14:149–56. doi: 10.1111/j.1440-172X.2008.00678.x
75. Woo BFY, Lee JXY, Tam WWS. The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: a systematic review. Hum Resour Health. (2017) 15:63. doi: 10.1186/s12960-017-0237-9
76. Wood C, Hurley C, Wettlaufer J, Penque M, Shaha SH, Lillis K. Retrospective comparison of emergency department length of stay for procedural sedation and analgesia by nurse practitioners and physicians. Pediatr Emerg Care. (2007) 23:709–12. doi: 10.1097/PEC.0b013e318155ade4
77. Woods L. Evaluating the clinical effectiveness of neonatal nurse practitioners: an exploratory study. J Clin Nurs. (2006) 15:35–44. doi: 10.1111/j.1365-2702.2005.01246.x
78. Fennelly O, Blake C, FitzGerald O, Breen R, Ashton J, Brennan A, et al. Advanced practice physiotherapy-led triage in Irish orthopaedic and rheumatology services: national data audit. BMC Musculoskelet Disord. (2018) 19:181. doi: 10.1186/s12891-018-2106-7
79. Howland D, Cunniffe G, Morris S, Staunton P. An evaluation of the effectiveness of an advanced practice physiotherapist in the emergency department setting in Ireland. Ir J Med Sci. (2023). doi: 10.1007/s11845-023-03567-4 [Epub ahead of print].
80. Jovic D, Mulford J, Ogden K, Zalucki N. Diagnosis and management of chronic hip and knee pain in a Tasmanian orthopaedic clinic: a study assessing the diagnostic and treatment planning decisions of an advanced scope physiotherapist. Aust J Prim Health. (2019) 25:60–5. doi: 10.1071/PY18076
81. Jovic D, Tuckerman K, Bergenroth C, Tran V. Time to analgesia for musculoskeletal presentations in Tasmanian emergency departments: a case-controlled comparative observational study investigating the impact of advanced practice physiotherapists. Aust Health Rev. (2023) 47:268–73. doi: 10.1071/AH23032
82. McDonough A, Lennox A, Angus M, Coumbarides A. An analysis of the utility, effectiveness and scope of advanced physiotherapy practitioners in an urgent treatment centre pilot. Physiotherapy. (2022) 115:61–5. doi: 10.1016/j.physio.2021.12.005
83. Ó Mír M, O'Sullivan C, Lennon O, Blake C. An evaluation of diagnostic agreement rates between advanced practice physiotherapists and paediatric orthopaedic consultants for children with musculoskeletal complaints. Musculoskelet Care. (2018) 16:433–9. doi: 10.1002/msc.1357
84. Robarts S, Stratford P, Kennedy D, Malcolm B, Finkelstein J. Evaluation of an advanced-practice physiotherapist in triaging patients with lumbar spine pain: surgeon-physiotherapist level of agreement and patient satisfaction. Can J Surg. (2017) 60:266–72. doi: 10.1503/cjs.013416
85. Sayer JM, Kinsella RM, Cary BA, Burge AT, Kimmel LA, Harding P. Advanced musculoskeletal physiotherapists are effective and safe in managing patients with acute low back pain presenting to emergency departments. Aust Health Rev. (2018) 42:321–6. doi: 10.1071/AH16211
86. Cummins NM, Dixon M, Garavan C, Landymore E, Mulligan N, O'Donnell C. Can advanced paramedics in the field diagnose patients and predict hospital admission? Emerg Med J. (2013) 30:1043–7. doi: 10.1136/emermed-2012-201899
87. Pemberton K, Franklin RC, Bosley E, Watt K. Pre-hospital predictors of long-term survival from out-of-hospital cardiac arrest. Australas Emerg Care. (2023) 26:184–92. doi: 10.1016/j.auec.2022.10.006
88. McClellan CM, Cramp F, Powell J, Benger JR. A randomised trial comparing the clinical effectiveness of different emergency department healthcare professionals in soft tissue injury management. BMJ Open. (2012) 2:e001092. doi: 10.1136/bmjopen-2012-001092
89. Alotaibi T, Al Anizi CA. The impact of advanced nurse practitioner (ANP) role on adult patients with cancer: a quantitative systematic review. Appl Nurs Res. (2020) 56:151370. doi: 10.1016/j.apnr.2020.151370
90. Saxon RL, Gray MA, Oprescu FI. Reducing geriatric outpatient waiting times: Impact of an advanced health practitioner. Australas J Ageing. (2018) 37:48–53. doi: 10.1111/ajag.12459
91. McCrory G, Patton D, Moore Z, O'Connor T, Nugent L. The impact of advanced nurse practitioners on patient outcomes in chronic kidney disease: a systematic review. J Ren Care. (2018) 44:197–209. doi: 10.1111/jorc.12245
92. Garg R, Metzger C, Rein R, Lortie M, Underwood P, Hurwitz S, et al. Nurse practitioner-mediated intervention for preoperative control of diabetes in elective surgery patients. J Am Assoc Nurse Pract. (2016) 28:528–33. doi: 10.1002/2327-6924.12365
93. Harbman P. The development and testing of a nurse practitioner secondary prevention intervention for patients after acute myocardial infarction: a prospective cohort study. Int J Nurs Stud. (2014) 51:1542–56. doi: 10.1016/j.ijnurstu.2014.04.004
94. Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. (1999) 281:613–20. doi: 10.1001/jama.281.7.613
Keywords: acute care, advanced practitioner, advanced nurse, advanced physiotherapist, advanced paramedic, patient safety, patient outcome
Citation: Bauernfeind L, Fels M, Dahlmann P, Rester C and Sterr F (2024) The impact of advanced practitioners on patients in acute care—A mini review. Front. Disaster Emerg. Med. 2:1399779. doi: 10.3389/femer.2024.1399779
Received: 12 March 2024; Accepted: 08 May 2024;
Published: 21 May 2024.
Edited by:
Theodore Chan, University of California, San Diego, United StatesReviewed by:
Jan-Cedric Hansen, Centre d'Hébergement et d'Accompagnement Gérontologique (CHAG), FranceCopyright © 2024 Bauernfeind, Fels, Dahlmann, Rester and Sterr. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fritz Sterr, ZnJpdHouc3RlcnJAdGgtZGVnLmRl
†These authors have contributed equally to this work
 Lydia Bauernfeind
Lydia Bauernfeind Milena Fels
Milena Fels Philipp Dahlmann
Philipp Dahlmann Christian Rester1
Christian Rester1 Fritz Sterr
Fritz Sterr