- 1Department of Emergency Medicine, Baylor College of Medicine, Houston, TX, United States
- 2Department of Emergency Medicine, Valley Regional Hospital, Claremont, NH, United States
- 3Department of Emergency Medicine, Thomas Jefferson University Hospital, Philadelphia, PA, United States
Introduction: The spread of COVID-19 has posed a significant challenge to educators in the disaster medicine community. While lectures can often be given remotely with little revision, simulations and other workshops can prove more challenging to adapt. Here, we describe our framework for conducting multi-site mass casualty simulations via video conference.
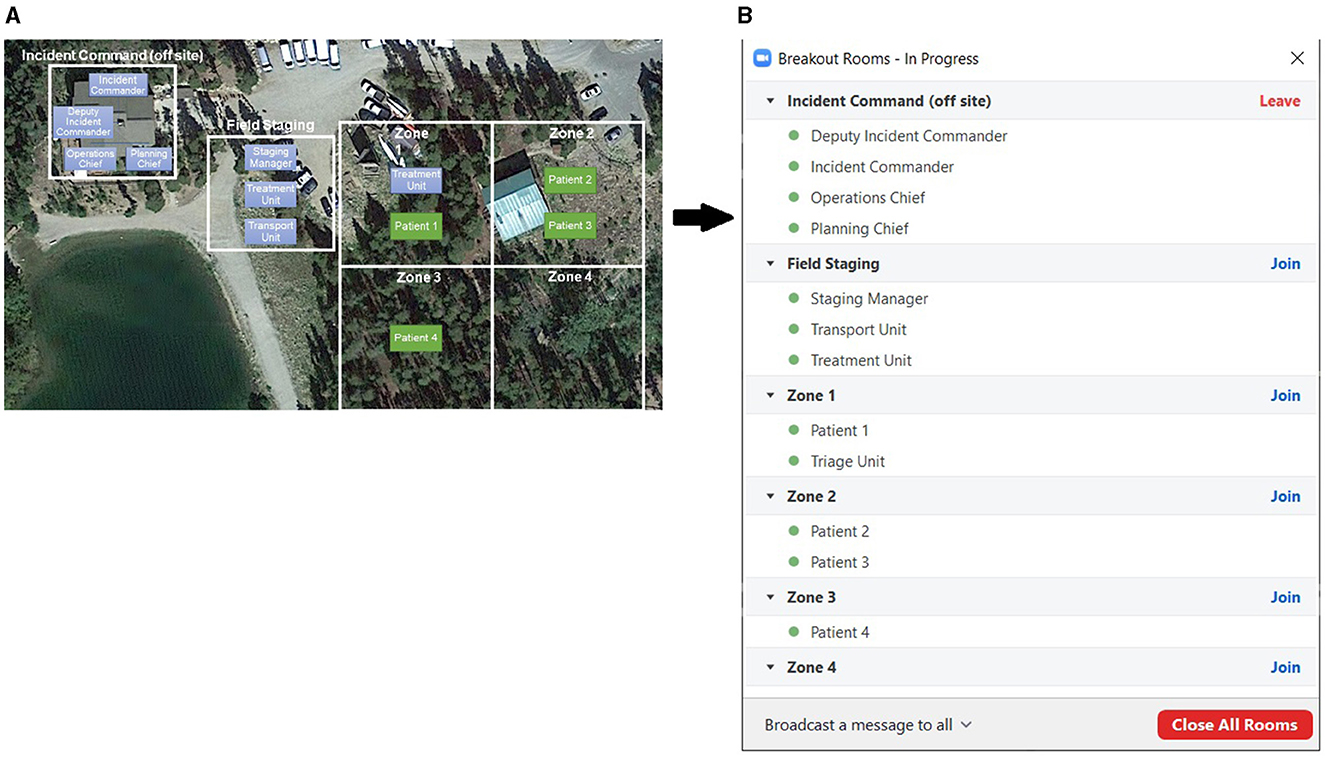
Methods: The authors of this paper adapted a mass casualty scenario from an in-person format to a virtual format delivered via the video conference software Zoom. Key physical locations of the simulated incident were mapped onto separate video conference breakout rooms. With this geographic framework established, rules were created to govern movement, communication, treatment, and transportation.
Results: Three separate virtual MCI drills were conducted. Both students and instructors were able to grasp the new format quickly. Students reported the drills to be informative and engaging, and instructors felt the drills mimicked the real-world experience well. This format had the added benefit of allowing multiple rounds of simulation to occur in rapid succession.
Discussion: Using breakout rooms to simulate physical locations can be a simple and intuitive framework for adapting disaster scenarios for remote delivery. We believe other instructors can utilize this framework to increase the availability of their educational content.
Introduction
Both man-made and environmental disasters have increased in frequency over the past few decades (1–3). Despite this, medical students, residents, and other health professionals often fail to receive significant training in disaster medicine and disaster response (4, 5). This holds true not only in the US but also in other countries globally (6, 7). Multiple curricula are being developed to address this deficit and to formalize disaster medical education (8, 9). Recent research has shown that drills and simulations may be particularly effective training tools (10).
Disaster simulations can improve student knowledge, skill transfer, confidence, and enthusiasm (11, 12). Participation in disaster simulations can also improve interpersonal skills such as leadership, communication, teamwork, and adaptability, which may be under-emphasized in more traditional medical education (13, 14). Unfortunately, disaster simulations often require large in-person gatherings. These may be limited by high cost and logistical requirements. The need for travel restrictions and physical distancing during COVID-19 further limited these types of gatherings, forcing many educators to rethink how disaster simulations could be conducted (15).
BreckWild is a month-long medical student elective for 3rd- and 4th-year medical students. It is sponsored by the Wilderness Medical Society and is held in Breckenridge, Colorado. It includes a significant focus on disaster medicine, search and rescue, and mass casualty response. About 15–20 students attend this course annually. Prior to 2019, BreckWild had only been conducted in person. This manuscript shares our experience in redesigning a virtually simulated mass casualty drill and the subsequent student response. While prior efforts at disaster education have made use of board games, video games, or augmented or virtual reality (16), our simulation was performed using commercially available video conferencing software.
Methods
Curriculum design
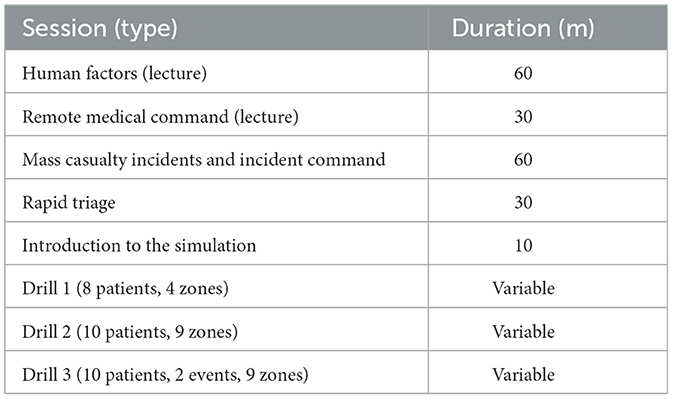
We used the Zoom video conference software (17) to host the virtual form of the elective. As with the original elective, we dedicated a full day to mass casualty incidents and response. Lecture topics included mass casualty incidents, the incident command system, field triage, and a small 10-min instructional lecture explaining the simulation interface and game rules. We then held three mass casualty simulations of increasing complexity. A summary of the day's schedule can be seen in Table 1.
Simulation scenarios were designed as a tabletop exercise for incident commanders and a rules-based simulation for field responders. Facilitation of this setup required a video conference platform able to perform the tasks below:
• Host the full class (between 30–40 total students, instructors, and guests) simultaneously.
• Allow the conference host to subdivide the conference into multiple breakout rooms.
• Allow participants to move themselves between the breakout rooms in real-time.
• Limit audio/visual communication to participants within the same breakout room only.
While we specifically used Zoom, we suspect other video conference software with these features would function similarly. Given these features, we were able to reconfigure our MCI drill as a virtual exercise. Our primary framework involved mapping geographic locations onto conference breakout rooms. This geographic adaptation can be seen in Figure 1. Once this framework existed, we adopted the following game rules for our simulation:
• Breakout rooms serve as geographic locations.
• Participants can assign themselves to different breakout rooms in real time to simulate movement.
• Within a breakout room (same location), participants are able to see and hear each other directly through the interface.
• Between different breakout rooms (different locations), participants cannot see or hear each other directly through the interface. Alternative means of communication (cell phones, texting, virtual “runners”) are necessary.
• Actions such as treatment and transport can be verbalized. These actions require 1–2 min, during which providers are unavailable to assist their team in any other way.
• Participants should change their usernames or captions to match their designated roles.
• Participants should not use the administrative aspects of the Zoom interface to acquire any information they could not access in real life.
Once we established our rules, we conducted our existing scenarios over the video conference software. A sample scenario flow is listed below.
• The video conference is divided into multiple rooms to simulate the physical geography of the drill.
• Instructor removes 8–10 students from the main group into a “patient pool” room and privately assigns them patient roles. While in the patient pool, instructors answer any questions from the simulated patients on their roles. The patients then move themselves to appropriate breakout rooms where they can be “discovered.”
• The remaining students are designated as responders and are placed into the breakout room representing incident command.
• The responders are informed that a mass casualty incident has occurred. They are asked to form an incident command system, move between the various sites of the incident, triage the patients in the field using the Simple Triage and Rapid Treatment (START) triage algorithm, verbalize any intended treatments, and verbalize intent to transport patients away from the scene.
• In the incident command tent, this follows the format of a tabletop exercise. The incident commander and officers receive information from other responders in the field but generally stay within the tent and take no physical action.
• In the field, this follows the format of a rules-based simulation. Responders move themselves through the various locations to mimic search-and-rescue. Responders also directly speak with the patients through the interface to acquire history.
• The drill is considered complete when all patients have been discovered, triaged, treated, and transported.
• Instructors observe response during the drill.
Data collection
Instructors kept quantitative measurements of student performance during the drill, including time to establish incident command, time to first patient contact, and time to drill completion.
After the drill, instructors conducted a 5–10 min informal debrief with both patients and responders in attendance.
As part of normal course quality improvement efforts, students were also asked to complete a survey regarding their course experience using a 5-point Likert scale.
Results
Interface
Students appeared to adjust to the video conference interface and game rules rapidly. Following the instructional lecture, all students were able to grasp the mechanics governing movement, communication, treatment, and transportation. Minor technical difficulties were occasionally noted, but these could be addressed in real-time. No student was forced to sit out any simulation.
Instructor impressions
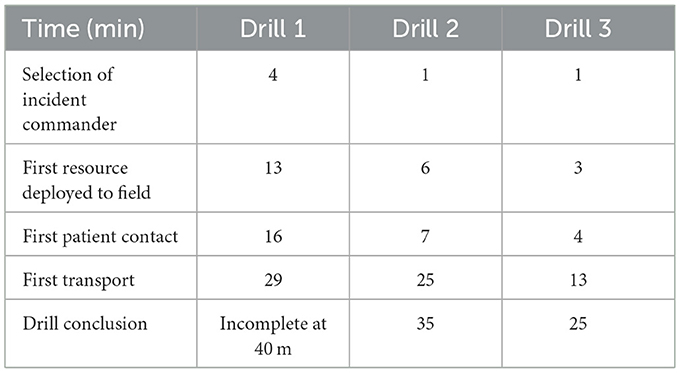
Both the course instructors and guest observers noted the simulation strongly mimicked real-life drills. Times to critical actions improved between successive iterations of the drill, as can be seen in Table 2. Students initially struggled with the designation of authority, subsequently with communication, and ultimately with tracking and loss of granular data. The use of a virtual medium did not appear to meaningfully change student behavior or the progression of learning.
Student response
Student response was generally positive. Students reported increased confidence in topics related to mass casualty incidents as seen in Table 3. They also appreciated the simulation of geography, logistics/communication, and triage. Students overwhelmingly stated the simulation held value beyond the lecture content alone.
Limitations
Several limitations to this work must be highlighted. First, we note that our virtual drill was not intended to replace in-person training entirely. Students noted the drill to be relatively weak in simulating direct patient care. The simulation also failed to mimic physical stressors, such as weather and fatigue, and the psychosocial stressors of being in a disaster environment.
Additionally, this course revision was not designed for educational research. Our sample size is small, and our available metrics to assess participant learning are limited to the data presented. Beyond this, in the absence of similar data from prior years' in-person drills and given differences in those drills' timings and goals, we cannot directly compare in-person and virtual course formats.
Further, all of our participants had access to computers or other devices for this virtual form of the elective. Our simulations could not function without each participant having a functioning personal computer, tablet, or phone with audio/visual capabilities and internet access.
Additionally, despite the small introductory lecture to the interface and each participant having their own device, we did encounter occasional technical difficulties. Rarely, students would drop from their rooms and require re-invitation or lose the ability to move themselves between rooms. Ensuring a quality simulation required a dedicated instructor to address these types of issues. Students also mentioned that having multiple responders and patients within a single breakout room led to significant background noise. Additional “dummy” rooms could be created to alleviate this in future iterations.
Finally, we note this course required the meeting host to purchase a paid format of the Zoom software. Requisite features were unavailable in the unpaid version.
Discussion
Here, we present our experience converting a mass casualty simulation for use with commercially available video conference software. Students seemed to grasp this new interface quickly and easily, and we were able to conduct our simulations with a broadly positive response. Adapting this exercise helped preserve one of the most popular and impactful simulations from a previously in-person elective.
This virtual MCI simulation was also high-yield. In the original elective, executing this simulation required physical travel, patient packaging, and transport. A single iteration often required 4 h to complete. By contrast, virtually, we completed three different MCI scenarios in under 3 h. While the virtual form could not convey physical skills such as patient packaging and transport, it had the advantage of allowing more practice of flow and communication—our primary objective for this specific learning exercise.
As disaster medicine continues to grow as a specialty, the demand for education will increase correspondingly. In-person education, while preferable, may not always be a viable option. Virtual simulation is one way to expand disaster medicine education while harnessing some of the creativity and innovation inherent to the field. Virtual simulations have low cost and logistical requirements. Using this type of framework to create virtual simulations could allow educators to increase the availability of their educational content moving forward.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Thomas Jefferson University Office of Human Resources, Institution Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because minimal risk to subjects- no identifiable data or protected information was collected from subjects. This was done as part of routine course feedback/QI. The study was deemed exempt.
Author contributions
AP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. JR: Conceptualization, Methodology, Project administration, Writing – review & editing. LP: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge the Wilderness Medical Society and the Sidney Kimmel Medical College for the opportunity to host this course in a virtual format. We additionally acknowledge the Breckenridge Outdoor Education Center for its historical support as the host of the in-person elective.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Coleman L. Frequency of man-made disasters in the 20th century. J Conting Crisis Manag. (2006) 14:3–11. doi: 10.1111/j.1468-5973.2006.00476.x
2. Smith A. 2010–2019: A landmark decade of US. billion-dollar weather and climate disasters. In: National Oceanic and Atmospheric Administration. (2020).
3. Vahdati A, Gholipour C, Talebian M, Vahdati S, Mahmoudieh T. Disaster in South-East of Iran: saravan earthquake with minimum mortality. Eurasian J Emer Med. (2014) 13:216. doi: 10.5152/jaem.2014.02418
4. Barrimah I, Ishag A, Al-Mohaimeed A. Disaster medicine education for medical students: Is it a real need? Med Teach. (2016) 38:S60–5. doi: 10.3109/0142159X.2016.1142515
5. Sarin R, Cattamanchi S, Alqahtani A, Aljohani M, Kleim M, Ciottone G, et al. Disaster education: a survey study to analyze disaster medicine training in emergency medicine residency programs in the United States. Prehosp Disaster Med. (2017) 32:368–73. doi: 10.1017/S1049023X17000267
6. Su T, Han X, Chen F, Du Y, Zhang H, Yin J, et al. Knowledge levels and training needs of disaster medicine among health professionals, medical students, and local residents in Shanghai, China. PLoS ONE. (2013) 8:e67041. doi: 10.1371/journal.pone.0067041
7. Rezaee R, Peyravi M, Marzaleh MA, Khorram-Manesh A. Needs assessment for standardized educational program for Iranian Medical Students in crisis and disaster management. J Adv Med Educ Profess. (2019) 7:95. doi: 10.30476/JAMP.2019.44713
8. Pfenninger E, Domres BD, Stahl W, Bauer A, Houser CM, Himmelseher S. Medical student disaster medicine education: the development of an educational resource. Int J Emerg Med. (2010) 3:9–20. doi: 10.1007/s12245-009-0140-9
9. Ngo J, Schertzer K, Harter P, Smith-Coggins R. Disaster medicine: a multi-modality curriculum designed and implemented for emergency medicine residents. Disaster Med Public Health Prep. (2016) 10:611–4. doi: 10.1017/dmp.2016.8
10. Ingrassia P, Ragazzoni L, Tengattini M, Carenzo L, Della Corte F. Nationwide program of education for undergraduates in the field of disaster medicine: development of a core curriculum centered on blended learning and simulation tools. Prehosp Disaster Med. (2014) 29:508–15. doi: 10.1017/S1049023X14000831
11. Cook D, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. Jama. (2011) 306:978–88. doi: 10.1001/jama.2011.1234
12. McCoy L, Pettit RK, Lewis JH, Allgood JA, Bay C, Schwartz F. Evaluating medical student engagement during virtual patient simulations: a sequential, mixed methods study. BMC Med Educ. (2016) 16:1–15. doi: 10.1186/s12909-016-0530-7
13. Reade M, Maar M, Cardinal N, Boesch L, Lacarte S, Rollins T, et al. The impact of hidden curriculum in wilderness-based educational events on Interprofessional competencies: a mixed-method study. J Res Interprof Pract Educ. (2017) 6:1–16. doi: 10.22230/jripe.2017v6n2a235
14. Smith H, Reade M, Maar M, Jeeves N. Developing a grounded theory for interprofessional collaboration acquisition using facilitator and actor perspectives in simulated wilderness medical emergencies. Rural Remote Health. (2017) 17:3880. doi: 10.22605/RRH3880
15. Kivlehan SM, Tenney K, Plasmati S, Bollettino V, Farineau K, Nilles EJ, et al. Humanitarian training with virtual simulation during a pandemic. Disaster Med Public Health Prepar. (2022) 16:2103–2107. doi: 10.1017/dmp.2021.152
16. Solinska-Nowak A, Magnuszewski P, Curl M, French A, Keating A, Mochizuki J, et al. An overview of serious games for disaster risk management–Prospects and limitations for informing actions to arrest increasing risk. Int J Disast Risk Reduc. (2018) 31:1013–29. doi: 10.1016/j.ijdrr.2018.09.001
17. Zoom Video Communications. [Computer software]. San Jose, CA (2024). Available at: https://zoom.us (accessed February 21, 2020).
Keywords: disaster medicine, medical education, mass casualty incident, video conference, simulation
Citation: Padaki AS, Rudner JR and Phillips LL (2024) Virtual simulation of mass casualty drills: using breakout rooms to simulate physical locations. Front. Disaster Emerg. Med. 2:1389656. doi: 10.3389/femer.2024.1389656
Received: 21 February 2024; Accepted: 28 August 2024;
Published: 12 September 2024.
Edited by:
Fadi Issa, Beth Israel Deaconess Medical Center and Harvard Medical School, United StatesReviewed by:
Samad Shams Vahdati, Tabriz University of Medical Sciences, IranRyan Hata, Indiana University, United States
Copyright © 2024 Padaki, Rudner and Phillips. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amit S. Padaki, YW1pdC5wYWRha2lAYmNtLmVkdQ==
 Amit S. Padaki
Amit S. Padaki Joshua R. Rudner2
Joshua R. Rudner2