
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
COMMUNITY CASE STUDY article
Front. Disaster Emerg. Med. , 12 June 2024
Sec. Disaster Medicine
Volume 2 - 2024 | https://doi.org/10.3389/femer.2024.1387704
This article is part of the Research Topic Disaster Medicine Education and Simulation View all 4 articles
 Shigehito Shiota1,2*
Shigehito Shiota1,2* Naoya Orita1,2
Naoya Orita1,2 Yuma Tsubakita1,3
Yuma Tsubakita1,3 Masaya Ichimoto1,2
Masaya Ichimoto1,2 Noboru Shimada1,2
Noboru Shimada1,2 Naoya Goto1,2
Naoya Goto1,2 Tomohiro Hirota1,2
Tomohiro Hirota1,2 Shunsuke Taito1,2
Shunsuke Taito1,2 Kazuhiko Hirata1,2
Kazuhiko Hirata1,2 Yukio Mikami1,3
Yukio Mikami1,3Early rehabilitation during disasters such as earthquakes is an important but often undervalued responsibility of medical teams. Both the development of simple tools for assessing the life functioning of evacuees and the standardization of intervention methods are urgent issues in disaster rehabilitation. The Japanese Rehabilitation Assistance Team (JRAT), an officially recognized organization consisting of 10 suborganisations, was established after gaining important experience with disaster rehabilitation in the aftermath of the Great East Japan Earthquake. We, the Hiroshima JRAT, were dispatched to the Monzen area of Wajima City to support disaster recovery after the 2024 Noto Peninsula Earthquake. Since disaster rehabilitation assistance was not well established in the Monzen area of Wajima City, the medical team consulted JRAT for guidance on triaging evacuees based on their life functioning. We developed a rehabilitation triage algorithm that classifies evacuees into four triage tags based on their ability to perform three simple movements: sitting up, standing up from the floor, and one-leg standing. In our triage algorithm, an inability to sit up is classified as a red tag (difficulty living in a shelter without assistance), an inability to stand up from the floor is classified as a yellow tag (individual intervention: introduction of beds and handrails), one-leg standing for <2 s is classified as a green tag (group intervention: installation of toilets and bath rails and use of walkers to prevent falls), and standing on one leg for more than 2 s is classified as a white tag (independent in ADLs). We worked with medical teams to triage 922 evacuees in 27 evacuation centers, resulting in the extraction of four red and eight yellow evacuees in 1 day. Our rehabilitation triage system has the potential to be a simple assessment tool for classifying the life functioning of disaster victims and linking them to appropriate supports.
On 1 January 2024, a 7.6-magnitude earthquake occurred on the Noto Peninsula in Ishikawa Prefecture, Japan. Wajima City and Shiga Town experienced the quake with an intensity of 7 (JMA), while Suzu City and surrounding regions felt a slightly lower intensity of 6+. In addition, Wajima City and Suzu City were severely damaged by a massive fire and a tsunami of up to 5 m. As of 29 January 2024, 236 people had been killed, 1,285 people were injured, 17,130 homes were damaged, and ~14,588 people were living in shelters (1). Immediately after the earthquake, life-saving medical teams from the Disaster Medical Assistance Team (DMAT), the Japanese Red Cross Society, and other organizations were dispatched to the area to provide emergency relief. However, as the situation transitioned from the acute phase to the subacute phase, the focus shifted away from emergency medical care toward the prevention of disaster-related deaths caused by the harsh living conditions of evacuation centers.
Earthquakes not only cause primary disabilities such as trauma and spinal cord injuries (2), but can also lead to psychological issues like anxiety and posttraumatic stress disorder from prolonged shelter living (3–5) and various physical health conditions, including deep vein thrombosis, heart failure, and respiratory infections (5–7). In recent years, early rehabilitation in the aftermath of disasters has been reported to improve outcomes for disaster survivors (8–10). Therefore, national measures designed to incorporate rehabilitation teams into the early stages of a disaster response are important (11). Unfortunately, the need for medical rehabilitation during disasters is not well recognized and is often not prioritized.
The Japanese Disaster Rehabilitation Assistance Team (JRAT) was organized to provide rehabilitation services during disasters. Formed in the aftermath of the Great East Japan Earthquake, JRAT has since been activated in response to earthquakes, torrential rain disasters, and typhoon disasters across Japan. The primary aim of JRAT's rehabilitation efforts is to prevent a decline in activity levels and disaster-related deaths among victims and to help them rebuild independent lives as quickly as possible (12). JRAT rehabilitation support involves a comprehensive assessment of the person and environment based on the International Classification of Functioning, Disability, and Health (ICF) (Figure 1) (13). In addition, JRAT provides programs to modify shelter environments and facilitates activities for evacuees based on ICF assessments (e.g., conducting group exercise programs, installing handrails in toilets and bathrooms, introducing beds, and using walking aids).
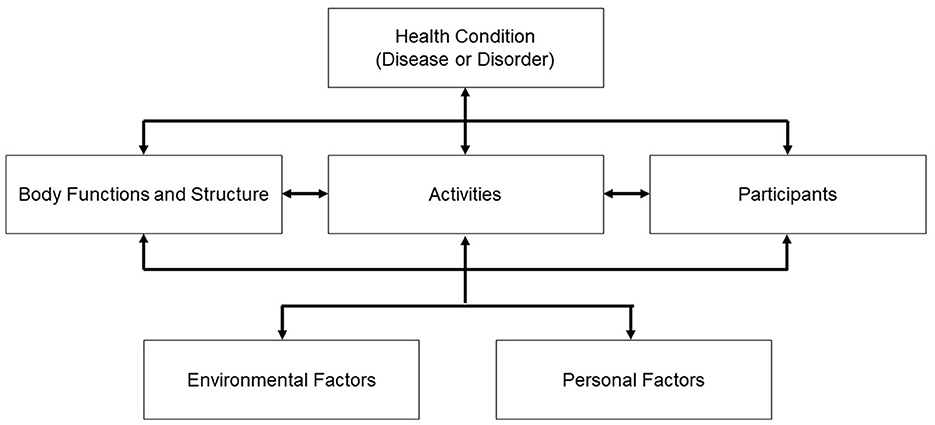
Figure 1. International classification of functioning, disability, and health (13). The changes in environmental factors, including living in shelters after an earthquake, inhibit an evacuee's participation in work and community interactions, resulting in a deterioration in physical and mental functioning due to low activity levels, which can then lead to worsening health conditions, such as frailty, and fractures due to falls.
This community case study describes the methodology of rehabilitation triage that JRAT developed in Wajima City to assess daily life functioning in a simple manner. In addition, we present the details of our rehabilitation algorithm as it corresponds to each triage tag.
Wajima City is located at the tip of the Noto Peninsula, where tourism, fishing, and traditional crafts, such as Wajima-nuri, thrive. With a population of 24,500, Wajima City faces challenges associated with rapid aging, with ~50% of its population being over 65 years old. Medical resources are scarce, with only one midsized hospital providing inpatient care and medical personnel is limited. In addition, the regions faces potential accessibility issues during a major disaster due to the discontinuation of the railroad, and the presence of are few major roads.
During the Noto Peninsula earthquake, 101 people died (three disaster-related deaths) in Wajima City, and 3,289 people were forced to live in evacuation centers because one-third of the buildings had been damaged (Figure 2). In the Monzen area, 922 evacuees spent their time in seven welfare shelters and 27 evacuation centers. During the acute phase of the earthquake, two DMATs, four Japan Medical Association Teams (JMAT), and one Disaster Health Emergency Assistance Team (DHEAT) were dispatched to provide treatment and care based on health status, using the Simple Triage and Rapid Treatment Triage (START) method. Dialysis and ventilator patients were transported to hospitals that were less affected, and the health of evacuees with medical conditions was being monitored by medical teams.
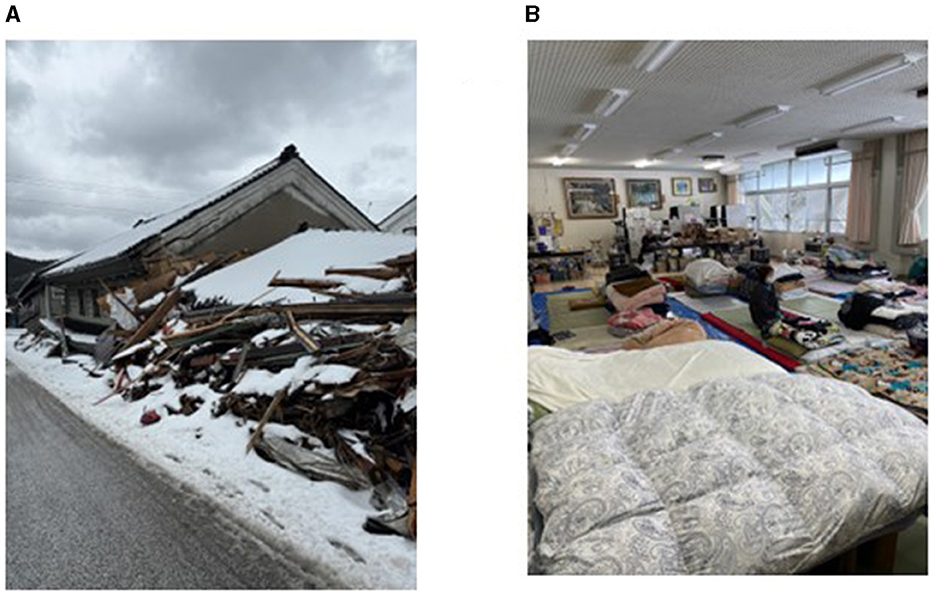
Figure 2. (A) Damage to houses; (B) Evacuation shelter (people sleeping on futons on the floor, with few beds).
Hiroshima JRAT was first dispatched as an advance team to Monzen area in Wajima City between 25 to 27 January 2024, during the sub-acute phase of the disaster. On the first day of our deployment, we gave a presentation to the medical team explaining the need for rehabilitation support and the activities of the JRAT. Several medical teams were aware of the need for disaster rehabilitation but did not know the specific activities involved. We visited several shelters to assess the environment and the life functioning of evacuees. Notably, evacuees often had not informed the medical team of any fractures, bruises, or other pain from falls. We also identified problems with daily functioning by assessing evacuees and reporting this information to the DMAT and JMAT. In addition, we made environmental adjustments, such as introducing mats for the older adults who were having difficulty standing up and canes for those with an unsteady gait. As a result of these efforts, JMAT consulted us for guidance on ways to triage the life functioning of evacuees. One of the reasons why this type of triage was required was that most of the evacuees were old, and some were unable to continue living in evacuation centers because of advanced disuse syndrome. Therefore, there was an urgent need to identify the care and rehabilitation needs of all evacuees through a simple assessment of their daily functioning. Accordingly, we developed a triage algorithm that enabled an easy assessment of daily life functioning without requiring any knowledge of rehabilitation medicine.
The rehabilitation triage algorithm that we developed is based on the ICF, which enables a simple and efficient assessment of life functioning (Figure 3). It demonstrates whether evacuees can continue to live independently based on their individual life functioning. General triage, as represented by the START method, is classified into five tags (red: highest-priority treatment group; yellow: non-urgent treatment group; green: light treatment group; white: uninjured; and black: death or non-treatment group) (14). Our triage algorithm categorized patients into four triage tags based on their ability to perform three basic activities of daily living (ADLs), including sitting up, standing up from the floor, and one-leg standing. Using our algorithm, an inability to sit up is classified as a red tag and indicates difficulty living in a shelter without assistance. An inability to stand up from the floor is classified as a yellow tag and indicates the need to introduce a bed and handrails on an individual level. One-leg standing for < 2 s is classified as a green tag, signaling the need for group interventions like installing toilets and bath rails and utilizing walkers to mitigate fall risks. Finally, standing on one leg for more than 2 s is classified as a white tag, independent in ADLs. This method of triaging is expected to help standardize rehabilitation support based on life functioning.
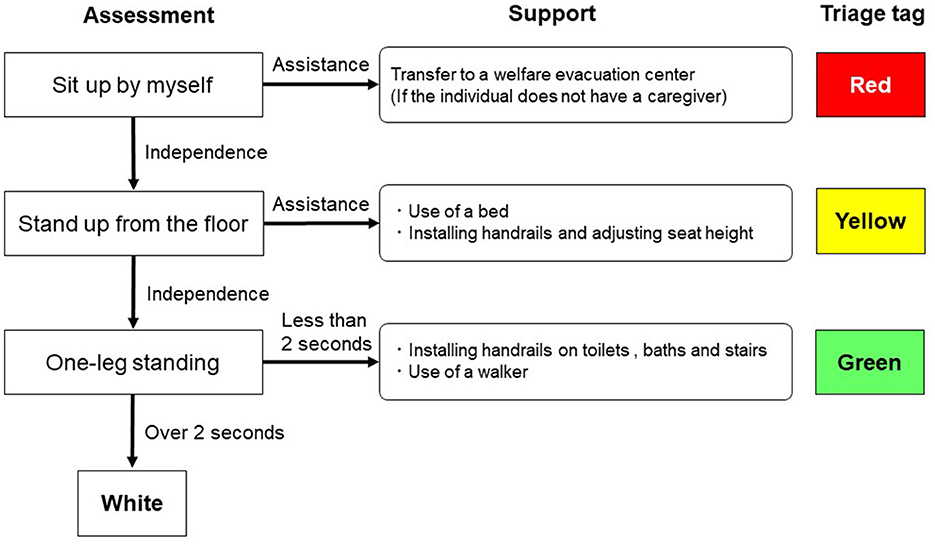
Figure 3. Monzen rehabilitation triage algorithm. The triage algorithm has three stages: assessments of ”sitting up,“ ”standing up from the floor,“ and ”one-leg standing.“ A triage tag is determined, and support is provided by JRAT accordingly. If a patient has difficulty ”standing up from the floor,“ but can stand up from a bed, the evacuee is considered to have a ”modified green“ triage tag.
Rehabilitation triage requires a simple measurement of ADLs. In medical rehabilitation, the Functional Independence Measure (FIM) is commonly used for assessing ADLs; however, this tool cannot be used in disaster situations because it takes time to measure and requires specialized learning (15). Thus, we were faced with the need to develop a simplified assessment measure that could be performed by teams that do not specialize in rehabilitation, such as DMAT and JMAT. Therefore, we created a system to identify the ability to perform three basic movements: sitting up, standing up from the floor, and standing on one leg (Figure 4).
The ability to sit up is the first movement in all ADLs and has been reported to be associated with ADL independence (16, 17). If an evacuee is unable to get up independently, it will be difficult for him or her to use the toilet without a caregiver. Evacuees who are unable to manage toileting independently are encouraged to seek refuge in welfare shelters, ensuring considerations of dignity and hygiene are upheld.
Standing up from the floor is a simple method of assessing physical function and is a predictor of ADL independence (18, 19). Evacuees who have difficulty standing up from the floor are also unable to use the toilet alone and require a caregiver to maintain hygiene. However, even if a patient has difficulty getting up from the floor, the introduction of a bed often enables him or her to stand up and move independently (18). In our rehabilitation triage method, evacuees who have been introduced to a bed and can then stand up are considered to have a “modified green” triage tag.
One-legged standing is widely used as a simple method for assessing balance capacity and is strongly associated with fall risk (20–23). The cut-off time for standing on one leg has varied from 3 to 30 s in previous studies (20, 21), and we struggled to identify an appropriate cut-off value for our assessment. Eventually, we decided to set a strict cut-off value of 2 s because our goal was to broadly identify those at risk of falls and provide them with rehabilitation assistance. Evacuation centers often lack barrier-free environments, and some evacuees have fallen and sustained injuries like broken bones on steps or between toilets and bathrooms. Installing handrails on steps and introducing walking aids such as wheelchairs and canes can enable safe mobility and prevent low activity by maintaining opportunities for self-care.
For evacuees who triage as red or yellow, individualized rehabilitation programs are needed to improve disuse syndrome and ADLs. For evacuees who triage as white or green, group exercise is recommended to prevent disuse syndrome and deep vein thromboses. In addition, role-playing in shelters, such as cooking, washing clothes, cleaning, and carrying goods, can improve activity levels and maintain opportunities for interpersonal interactions, which can prevent secondary disabilities such as isolation and depression.
Our proposed rehabilitation triage algorithm was accepted by the medical teams in the Monzen area, and we lectured them on how to triage the evacuees. All medical teams then split up and triaged all evacuees in the district. Seven medical teams were able to complete the triaging of all evacuees at 27 evacuation centers in 1 day using this triage system. As a result, we identified four red and eight yellow evacuees (Figure 5). Based on the experience in the Monzen area, the Ishikawa JRAT responsible for disaster rehabilitation in the Noto Peninsula earthquake adopted the Rehabilitation Triage Algorithm. The Ishikawa JRAT is recommended utilizing our triage algorithm for JRATs dispatched to take charge of disaster rehabilitation after the Noto Peninsula earthquake.
In our experience in the Monzen area, upon our arrival, the evacuation list had already been prepared and the health status of evacuees had already been assessed, as the disaster had progressed to the subacute phase. If it had been in the acute phase, however, life triage would have taken precedence, and rehabilitation triage would have been a lower priority. In addition, rehabilitation triaging of all evacuees requires a temporary investment of many human resources. If multiple medical teams had not been dispatched, as in this case, it would have been difficult to perform rehabilitation triage within a short period of time. This case report also has some limitations as it is an observation of a new triage algorithm. It has not been compared to other triage systems, it has not been externally validated, and there is no clear follow-up to assess its effectiveness in long-term outcomes.
In the sub-acute phase of a major earthquake, rehabilitation support based on triage of not only life but also function was an urgent issue. The rehabilitation triage algorithm we have developed is characterized by the fact that it does not require special tools and can be used by non-rehabilitation professionals to easily classify function. The START method, which is commonly used for primary triage, aims to determine treatment priorities quickly by means of a simple physical assessment. The Physiological and Anatomical Triage (PAT) method, used as a secondary triage, confirms physiological and anatomical lethality. Our rehabilitation triage differs from the START and PAT methods in the purpose and target of triage. The present case study showed that even non-rehabilitation professionals can immediately identify red and yellow evacuees by assessing their actual behavior. In addition, the number of people with triage tags in each evacuation center can be ascertained to clarify the number of cots, handrails, and portable toilets needed, leading to the establishment of an efficient support system. Our experience with disaster rehabilitation in the Noto Peninsula earthquake highlighted the importance of raising awareness of disaster rehabilitation and standardizing assessments and interventions in order to maintain the ADLs of disaster victims and prevent disaster-related deaths.
Assessment tools and intervention methods for disaster rehabilitation are not yet well established. Based on our experience, a rehabilitation triage algorithm is imperative to establish a method for rehabilitation support based on simplified assessments. In addition, personnel must be trained to appropriately practice rehabilitation triage and support. The ability of JRAT to act immediately in the event of a disaster has been determined by an agreement with each individual prefecture. However, we believe that positioning JRAT activities at the national level within disaster medicine is a shortcut to protecting people's health and rebuilding disaster victims' lives. In the future, we plan to develop a system that can triage using video motion capture on smartphones, enabling rehabilitation triage to be performed without a medical team. It is also necessary to establish a system to easily tabulate triage results at each local shelter. Such a system would make it possible to efficiently determine the number of people entering welfare shelters, the number of beds needed in each shelter, and the amount of welfare equipment required, such as portable toilets and handrails.
During the Noto Peninsula earthquake, Hiroshima JRAT developed and implemented a rehabilitation triage algorithm in the Monzen area of Wajima City. We worked with medical teams to effectively triage evacuees at all evacuation centers in 1 day. Further studies are needed to identify relevant rehabilitation triage items, cut-off values, and a system for sharing results.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
SS: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. NO: Data curation, Investigation, Writing – review & editing. YT: Data curation, Investigation, Writing – review & editing. MI: Data curation, Investigation, Writing – review & editing. NS: Data curation, Investigation, Writing – review & editing. NG: Project administration, Resources, Writing – review & editing. TH: Project administration, Resources, Writing – review & editing. ST: Project administration, Resources, Writing – review & editing. KH: Project administration, Resources, Writing – review & editing. YM: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors are grateful to JRAT and Ishikawa JRAT for their generous support of rehabilitation assistance activities in the region. We would like to thank Editage (http://www.editage.jp) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cabinet Office: Damage from the Noto Peninsula Earthquake of 2024. (2024) Available online at: https://www.bousai.go.jp/updates/r60101notojishin/r60101notojishin/pdf/r60101notojishin_24.pdf (accessed January 30, 2024).
2. Amatya B, Galea M, Li J, Khan F. Medical rehabilitation in disaster relief: towards a new perspective. J Rehabil Med. (2017) 49:620–28. doi: 10.2340/16501977-2250
3. Fan F, Zhang Y, Yang Y, Mo L, Liu X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. J Trauma Stress. (2011) 24:44–53. doi: 10.1002/jts.20599
4. Yun K, Lurie N, Hyde PS. Moving mental health into the disaster-preparedness spotlight. N Engl J Med. (2010) 363:1193–5. doi: 10.1056/NEJMp1008304
5. Chan EY, Griffiths S. Comparison of health needs of older people between affected rural and urban areas after the 2005 Kashmir, Pakistan earthquake. Prehosp Disaster Med. (2009) 24:365–71. doi: 10.1017/S1049023X00007159
6. Mori K, Ugai K, Nonami Y, Kirimura T, Kondo C, Nakamura T, et al. Health needs of patients with chronic diseases who lived through the great Hanshin earthquake. Disaster Manag Response. (2007) 5:8–13. doi: 10.1016/j.dmr.2006.11.002
7. Chan EY, Sondorp E. Medical interventions following natural disasters: missing out on chronic medical needs. Asia Pac J Public Health. (2007) 19:45–51. doi: 10.1177/101053950701901S08
8. Burns AS, O'Connell C, Rathore F. Meeting the challenges of spinal cord injury care following sudden onset disaster: lessons learned. J Rehabil Med. (2012) 44:414–20. doi: 10.2340/16501977-0974
9. Hu X, Zhang X, Gosney JE, Reinhardt JD, Chen S, Jin H, et al. Analysis of functional status, quality of life and community integration in earthquake survivors with spinal cord injury at hospital discharge and one-year follow-up in the community. J Rehabil Med. (2012) 44:200–5. doi: 10.2340/16501977-0944
10. Mills JA, Durham J, Packirisamy V. Rehabilitation services in disaster response. Bull World Health Organ. (2017) 95:162–4. doi: 10.2471/BLT.15.157024
11. Amatya B, Khan F. Disaster response and management: the integral role of rehabilitation. Ann Rehabil Med. (2023) 47:237–60. doi: 10.5535/arm.23071
12. Japan Disaster Rehabilitation Assistance Team: Organization Overview. (2024) Available online at: https://www.jrat.jp/aisatsu_kurihara.html (accessed February 10, 2024).
13. WHO: International Classification of Functioning Disability and Health (ICF). (2024) Available online at: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health (accessed February 10, 2024).
14. Franc JM, Kirkland SW, Wisnesky UD, Campbell S, Rowe BH. METASTART a systematic review and meta-analysis of the diagnostic accuracy of the Simple Triage and Rapid Treatment (START) algorithm for disaster triage. Prehosp Disaster Med. (2022) 37:106–16. doi: 10.1017/S1049023X2100131X
15. Reinhardt JD Li J, Gosney J, Rathore FA, Haig AJ, Marx M, et al. Disability and health-related rehabilitation in international disaster relief. Glob Health Action. (2011) 4:7191. doi: 10.3402/gha.v4i0.7191
16. Hashimoto K, Higuchi K, Nakayama Y, Abo M. Ability for basic movement as an early predictor of functioning related to activities of daily living in stroke patients. Neurorehabil Neural Repair. (2007) 21:353–7. doi: 10.1177/1545968306297870
17. Chen WC, Hsiao MY, Wang TG. Prognostic factors of functional outcome in post-acute stroke in the rehabilitation unit. J Formos Med Assoc. (2022) 121:670–8. doi: 10.1016/j.jfma.2021.07.009
18. Alexander NB, Galecki AT, Nyquist LV, Hofmeyer MR, Grunawalt JC, Grenier ML, et al. Chair and bed rise performance in ADL-impaired congregate housing residents. J Am Geriatr Soc. (2000) 48:526–33. doi: 10.1111/j.1532-5415.2000.tb04999.x
19. Ardali G, States RA, Brody LT, Godwin EM. The relationship between performance of sit-to-stand from a chair and getting down and up from the floor in community-dwelling older adults. Physiother Theory Pract. (2022) 38:818–29. doi: 10.1080/09593985.2020.1802796
20. Hurvitz EA, Richardson JK, Werner RA, Ruhl AM, Dixon MR. Unipedal stance testing as an indicator of fall risk among older outpatients. Arch Phys Med Rehabil. (2000) 81:587–91. doi: 10.1053/mr.2000.6293
21. Demircioglu A, Kezban Sahin Ü, Acaröz S. Discriminative ability of the four balance measures for previous fall experience in Turkish community-dwelling older adults. J Aging Phys Act. (2022) 30:980–6. doi: 10.1123/japa.2021-0415
22. Moreira MN, Bilton TL, Dias RC, Ferriolli E, Perracini MR. What are the main physical functioning factors associated with falls among older people with different perceived fall risk? Physiother Res Int. (2017) 22:1664. doi: 10.1002/pri.1664
Keywords: ICF, rehabilitation triage, disaster, JRAT, Noto peninsula earthquake
Citation: Shiota S, Orita N, Tsubakita Y, Ichimoto M, Shimada N, Goto N, Hirota T, Taito S, Hirata K and Mikami Y (2024) Development and implementation of a rehabilitation triage algorithm for disasters in the subacute phase: an experience from the 2024 Noto peninsula earthquake. Front. Disaster Emerg. Med. 2:1387704. doi: 10.3389/femer.2024.1387704
Received: 18 February 2024; Accepted: 28 May 2024;
Published: 12 June 2024.
Edited by:
Fadi Issa, Beth Israel Deaconess Medical Center and Harvard Medical School, United StatesReviewed by:
Ryan Hata, Indiana University, United StatesCopyright © 2024 Shiota, Orita, Tsubakita, Ichimoto, Shimada, Goto, Hirota, Taito, Hirata and Mikami. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shigehito Shiota, sshiota@hiroshima-u.ac.jp
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.