- 1Department of South West Shewa Zonal Health, Oromia Health Bureau, Addis Ababa, Ethiopia
- 2Waliso Woreda Health Office, Oromia Health Bureau, Addis Ababa, Ethiopia
- 3Institute of Health Science, Wollega University, Nekemte, Ethiopia
- 4Department of Health Behaviour and Society, Faculty of Public Health, Jimma Institute of Health, Jimma Medical Center, Jimma, Ethiopia
- 5Department of Epidemiology, Faculty of Public Health, Jimma Institute of Health, Jimma University, Jimma, Ethiopia
Introduction: Road traffic injuries are a major global public health problem. They are fatal or non-fatal injuries resulting from a road traffic accident involving at least one moving vehicle on a path or road open to public traffic. Therefore, this study aimed to determine the trends in fatalities from road traffic injuries and the associated factors of patients admitted to the emergency department of St. Luke Hospital.
Methods: An institution-based cross-sectional study was conducted from July 10 to 30, 2019. The study on the trends in road traffic injuries was conducted monthly bases from January 1 to December 31, 2018. A total of 364 road traffic–injured victim records were included. A simple random sampling technique was used for the record selection. A structured data abstraction format was used to gather the required data. Binary logistic regression and multivariate logistic regression were used to determine the association between the outcome and explanatory variables. Adjusted odds ratios (AORs) at 95% confidence intervals were used to report independent variables.
Results and conclusions: The average annual fatalities from road traffic injuries was 8.34% deaths/month. The magnitude of road traffic injury fatalities was 8.79%. Of all victims who visited the hospital, 75.5% were male. The median age of the victims was 26 (51.6%), with a range from 6 to 70. The identified risk factors for road traffic injury fatalities were a lack of ambulance for transportation to the hospital after the accident (AOR = 7.093, 95% CI [1.950, 25.793], p = 0.003) and head injury (AOR = 2.515, 95% CI [1.075, 5.885], p = 0.034). Road traffic injury fatalities are an important public health problem that needs special attention. A shortage of ambulance service for transportation and injury sites related to head injury were associated factors. So it is important to establish and strengthen advanced prehospital care and an effective ambulance system for transporting victims with road traffic injuries.
Introduction
Road transportation provides great benefits to both nations and individuals by facilitating the movement of goods and people. However, road transportation has also placed a considerable burden on people's health in the form of road traffic injuries and the consequences of these injuries (1). Although the World Health Organization (WHO) reported the overall trend in the number of fatalities caused by road traffic collisions in low in middle-income countries, it has shown a rising trend since 2010 (2).
A road traffic injury (RTI) is defined as a fatal or non-fatal injury that occurs as a result of a road traffic crash that occurs on a way or street open to public traffic and involves at least one moving vehicle (3, 4). It is a major global public health problem that occurs due to collisions between vehicles, vehicles and pedestrians, vehicles and animals, or vehicles and geographical or architectural obstacles and has been a leading cause of mortality for many years that requires concerted efforts for effective and sustainable prevention (3, 5–8).
The factors for the increase in global road traffic injury fatalities are the growing number of motor vehicles, speeding, people not using seat belts and motorcyclists not using helmets, alcohol and other substance use, road type, weather conditions, and other human-related factors (9). However, there are no facilities for pedestrians and cyclists, and the increasing number of motor vehicles generally leads to reductions in walking and cycling (10).
For every 10 lives lost to traffic injuries, nine occur in low- and middle-income countries (11). RTIs are a growing public health issue that disproportionately affects vulnerable groups of road users, including the poor (2). Ninety percent of the world's fatalities on roads occur in low- and middle-income countries, even though these countries have approximately 54% of the world's vehicles (12).
Without immediate action being taken, the global number of deaths and injuries from road traffic accidents (RTAs) was predicted to be the third-leading cause of death by 2020 (13). Deaths from RTAs are also projected to increase from 1.2 million in 2004 to 2.4 million in 2030, primarily due to the increased motor vehicle ownership and use associated with economic growth in low- and middle-income countries (14).
The 2015 WHO report on road safety highlights that the situation is the worst in low-income countries and that there is a disproportionate number of deaths relative to the lower level of motorization. The African region continues to have the highest rates of road traffic deaths, while the lowest rates are in the European region (2). RTIs pose a high burden over the entire life course of people in sub-Saharan Africa, impacting not just young adults but also children and older adults. Nigeria, Ethiopia, South Africa, and Sudan together account for half of the RTI deaths in sub-Saharan Africa (15).
The Ethiopia Demographic Health Survey 2016, indicated that RTAs in Ethiopia accounted for the highest percentages of accidental injuries and deaths, accounting for 23% of all injuries (16). Therefore, this study aimed to identify the trends in fatalities from RTIs and the associated factors of patients admitted to the emergency department of St. Luke Catholic Hospital, South West Shewa Zone, Central Ethiopia, during 2019.
Materials and methods
Study area and period
This study was conducted in St. Luke Catholic Hospital and College of Nursing and Midwifery located in Woliso town of Oromia Regional State from July 10 to 30, 2019. The hospital has 200 beds and serves more than 400 outpatients per day. It is the only referral hospital in the South West Shewa Zone, serving a population of ~1.3 million people. The outpatient department is fully operational 5 days a week for routine outpatient consultations, and emergency room services are available 24 h every day, with 1 health officer on duty and 3 nurses, 1 surgeon, and 1 internist on call (17).
Study design
An institution-based cross-sectional study was conducted.
Source population and study population
Source population
All RTI patients who attended the emergency department of St. Luke Hospital from January 1 to December 31, 2018, were considered.
Study population
All RTI patients who attended the emergency department of St. Luke Hospital who were admitted from January 1 to December 31, 2018, and fulfilled the inclusion criterion.
Eligibility criteria
Inclusion criteria:
➢ All road traffic–injured patients who attended the emergency department at St. Luke Hospital between January 1, 2018, and December 31, 2018.
Exclusion criteria:
➢ Those road traffic–injured patients who were transferred immediately to other hospitals and without outcome variables were excluded.
➢ The information indicating that patients died instantly at the scene was excluded.
Sample size and sampling technique/sampling procedures
Sample size determination
The sample size was determined based on the single population proportion formula. Based on the study conducted in Dilchora Hospital in 2016, the magnitude of RTI fatalities was 9.4% (18). The level of confidence (α) was taken as 95% (z α/2) = 1.96; to maximize the sample size, the margin of error was taken as 0.03, using the equation ,
where
p is the prevalence of RTI fatalities among injured patients,
zα/2 is the 95% confidence interval two-tailed test is equal to 1.96, and
d is the margin of error, which is taken as 3%, or 0.03.
Then, the calculated sample size is n = 364.
To determine the required sample size for the second specific objective of this study, different factors significantly associated with RTIs were considered with the following assumptions: 95% confidence level and a power of 80% using the Epi Info software program, version 7.2.2.2. The calculated sample size for selected variables and the maximum sample size are used for the final required sample size (Supplementary Table 1).
Finally, the required sample size for this study was determined by taking the maximum sample size from the first objective 364 with a magnitude of RTI fatalities.
Sampling technique and procedure
The study subjects were selected using a simple random sampling technique and were included in the study until the sample size was obtained. First, the card numbers of 866 victims from January 1 to December 31, 2018, were collected from the emergency room registration book to get the main files of the patients from the records room. Next, using the medical record numbers of patients, cards were collected from the card room. Road traffic–injured victims registered from January 1 to December 31, 2018, at the emergency department were listed based on the sequence of their card numbers for each month. To select the charts of victims, a sampling frame was developed from the victims' registration books, and each RTI patient card was accessed based on a simple random sampling technique. The injured patient charts were selected by a lottery method within the sampling frame (Figure 1).
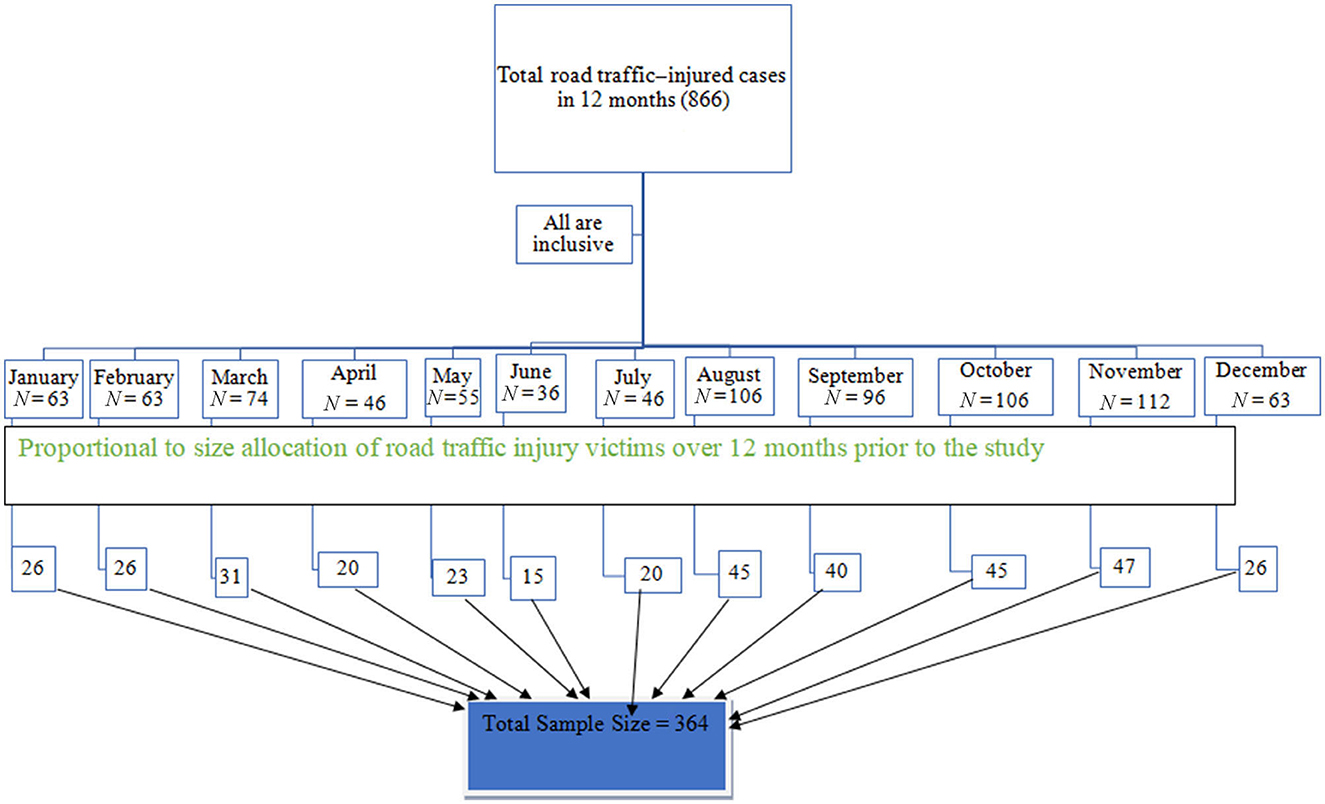
Figure 1. Schematic presentation of the sampling procedure from January 1 to December 30, 2018, of monthly road traffic–injured patients at St. Luke Hospital, South West Shewa Zone, Oromia.
Data collection tools and procedures
The data for the study were extracted from routinely registered client medical records and the emergency department registration book. The data were collected using a pretested format from the sample population according to the inclusion criterion. The data collection tool was adapted from the injury surveillance guideline document developed by the WHO in 2004 (19). The data were collected and supervised by two diploma holders and one degree-holding nurse, respectively.
Study variables
Dependent variable
RTI fatality.
Independent variables
Demographic and socioeconomic factors included age, sex, residence, and type of injured person (pedestrian, passenger, driver, motorbike driver). The environmental factor was the mode of transportation to the hospital after the injury occurred. The characteristics of RTI victims during admission included the site of injury, whether first aid was received before arriving at the hospital, the source of referral, and the time between the RTA and admission.
Data quality management
To ensure the quality of data, the format was pretested using 5% of the sample size, which is 18 records, before the actual data collection. Necessary modifications were made based on the pretest findings. To maintain data quality, 1 day of training was given to data collectors and a supervisor. The completeness and consistency of the data were checked daily by both the supervisor and the principal investigator. Correctly completed formats were collected from data collectors and entered into the Epi-Data Manager software, version 4.4.2.
Data processing and analysis procedures
Data processing procedure
The collected data were entered into Epi-data Manager 4.4.2 and then exported to SPSS, version 23.0, for statistical analysis. The data were checked for completeness and inconsistencies, cleaned, and coded. The data were then entered into the Epi-Data Manager software, version 4.4.2, and were cleaned and edited. The frequency distribution of the variables was examined for data entry errors.
Data analysis procedures
A descriptive analysis was done by computing proportions and summary statistics. Simple frequencies, summary measures, tables, and figures were used to present the data. A binary logistic regression was used to describe the association between each independent variable with the dependent variable. Variables with a p < 0.25 were used for the multivariate logistic regression model to control for the effects of other confounders, and finally, the variables that have an association with road traffic injury fatality were identified based on adjusted odds ratios (AORs), with 95% confidence values and p < 0.05. The variables were entered in the multivariable model using the backward stepwise regression method. Model fitness was checked by using the Hosmer–Lemeshow goodness-of-fit test. Finally, AORs and 95% confidence intervals were used to report the independent variables associated with RTI fatalities.
Ethical consideration
Ethical clearance was secured from the institutional review board (IRB) of the Institute of Health of Jimma University on February 27, 2019, reference number IHRPGD/181/2019. The IRB of the institute waived the informed consent as the study does not directly work with study participants. No informed consent was obtained from subjects and/or their legal guardian(s) as the study used secondary data. A support letter was written from the South West Shewa Zonal Health Office to St. Luke Hospital. Then a letter of permission was obtained from St. Luke Hospital. All methods were carried out according to relevant guidelines and regulations. To ensure confidentiality, names and other identifiers of patients, physicians, and other health care workers' recommendations were not recorded in the data abstraction format.
Results
A total of 364 RTI victims were included in the study, making the response rate of 100%. Of all victims who visited the hospital, 275 (75.5%) were male. The median age of victims was 26, with a range from 6 to 70. The highest number of victims was 188 (51.6%) in the 15–29-year-old age group, followed by those in the 30–44-year-old age group (92, 25.3%). RTA victims presenting to the hospital more commonly occurred as victims coming from outside Woliso (242, 66.5%) than from Woliso (122, 33.5%).
Of the total victims of RTA participants in the study, 177 (48.6%) were pedestrians, followed by passengers and motorbike drivers, which accounted for 130 (35.7%) and 49 (13.5%), respectively.
The highest number of RTIs occurred on weekdays (136, 37.36%).
From a total of 364 cases of RTIs, only 16 (4.3%) were transported by ambulance to the hospital, whereas 11 (3%) and 337 (92.6%) were transported to the hospital by police car and another method, respectively (Table 1).
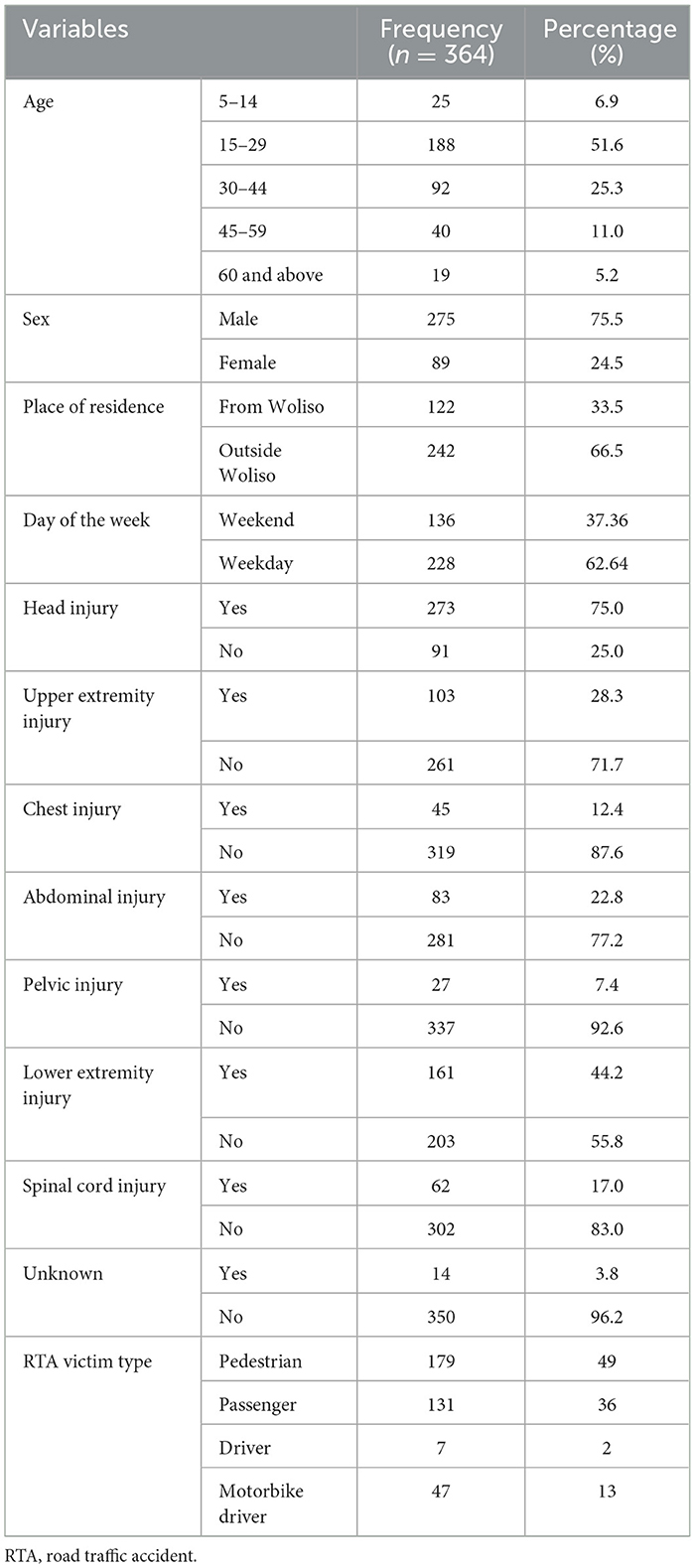
Table 1. General characteristics of the study population from January 1 to December 30, 2018, in St. Luke Hospital, South West Shewa Zone, Oromia Region.
Characteristics of RTI victims during admission
Of the total RTA victims included in this study, 199 (54.7%) were admitted to the emergency department of the hospital within less than 1 h, and 165 (45.3%) were admitted 1–12 h after the accident. Of those admitted to the hospital, 27 (7.7%), 128 (35.2%), and 208 (57.1%) were referred from the hospital, a health center, or did not have a referral, respectively. Of the admitted RTA victims, 191 (52.5%) received first aid before they were sent to the hospital.
According to the injury site of the victim, head injuries accounted for the highest (196, 53.8%), followed by lower extremity injuries (162, 44.5%).
Trends in RTI fatalities
The trends in RTI fatalities vary from month to month; the highest number of road traffic injuries was recorded in November, followed by August and October 2018. From January to December 2018, 866 RTIs occurred. The trends in RTI fatalities also varied seasonally (Figure 2).
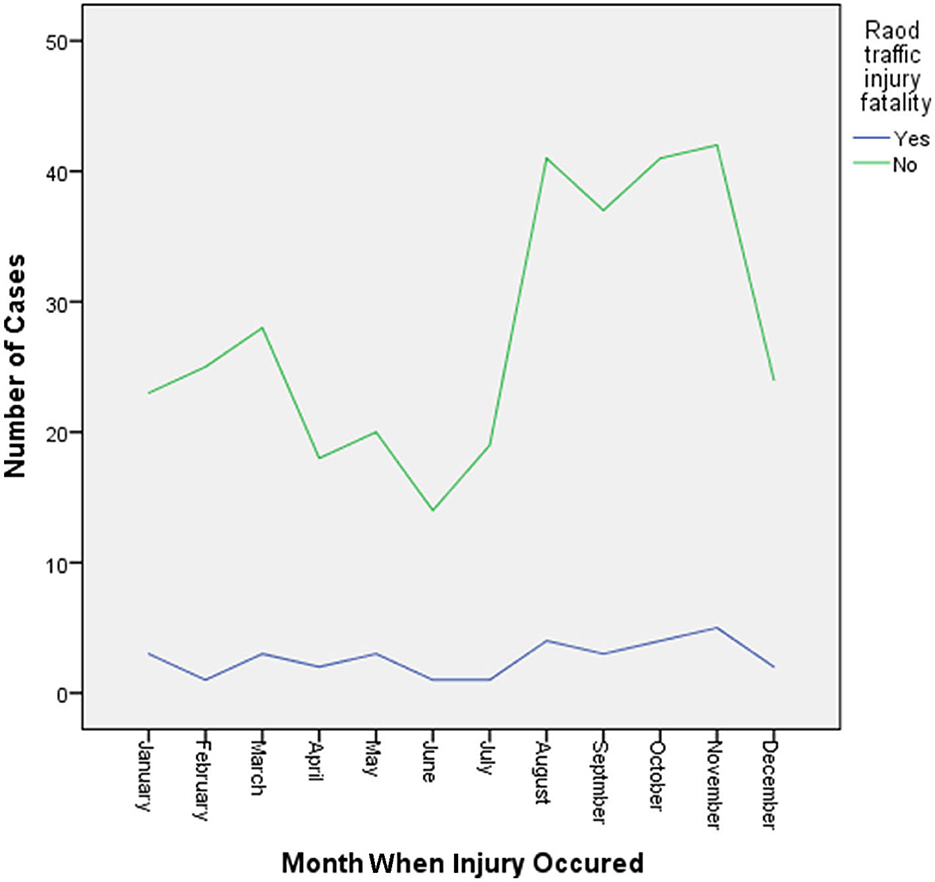
Figure 2. Trends in road traffic injuries from January 1 to December 30, 2018, in St. Luke Hospital, South West Shewa Zone, Oromia Region.
Road traffic fatality cross-tabulation
Many cases of fatality recorded in the current study occurred outside of the study area (Woliso, 10.2%), males (9.5%) were most often RTI fatality victims, and those in the 15–29-year-old age range experienced the most deaths (10.5%). The most frequent RTI fatality victims were motor vehicle drivers (22.4%), there was no significant variation of fatality among the seasons in Ethiopia in the study area, and among all fatalities, most victims (12.1%) arrived at the hospital within 1–12 h of the accident occurring (Table 2).
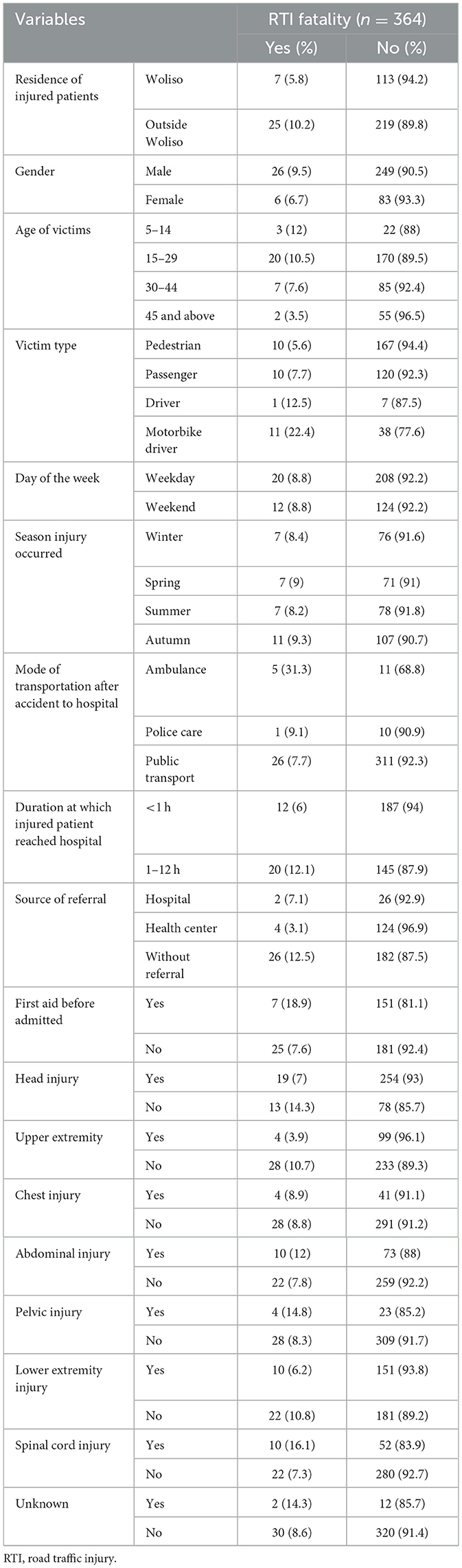
Table 2. Cross-tabulation of RTI fatalities from January 1 to December 30, 2018, in St. Luke Hospital, South West Shewa Zone, Oromia Region.
Factors associated with RTI fatalities
A binary logistic regression analysis was undertaken to screen candidate variables for the final model using a p < 0.25. In the binary logistic regression analysis, RTI fatality was significantly associated with variables like victim type, the day the injury occurred, the duration between the occurrence of the injury and the patient reaching the hospital, and the location of injury (head, upper extremity, chest, abdomen, pelvis, lower extremity, and/or spinal cord injury) at a p < 0.05 (Table 3).

Table 3. Binary logistic regression of factors associated with RTI fatalities from January 1 to December 30, 2018, in St. Luke Hospital, South West Shewa Zone, Oromia Region.
The results of the multivariable analysis showed that the mode of transportation to the hospital after the injury occurred and a head injury were independently associated with RTI fatalities. Accordingly, fatalities were seven times more likely for those transported by a public transportation facility compared with those transported by ambulance (AOR 7.093, 95% CI [1.950, 25.793]). RTI victims who had a head injury were 2.5-fold more likely to die compared to those who did not have a head injury (AOR 2.515, 95% CI [1.075, 5.885]; Table 4).
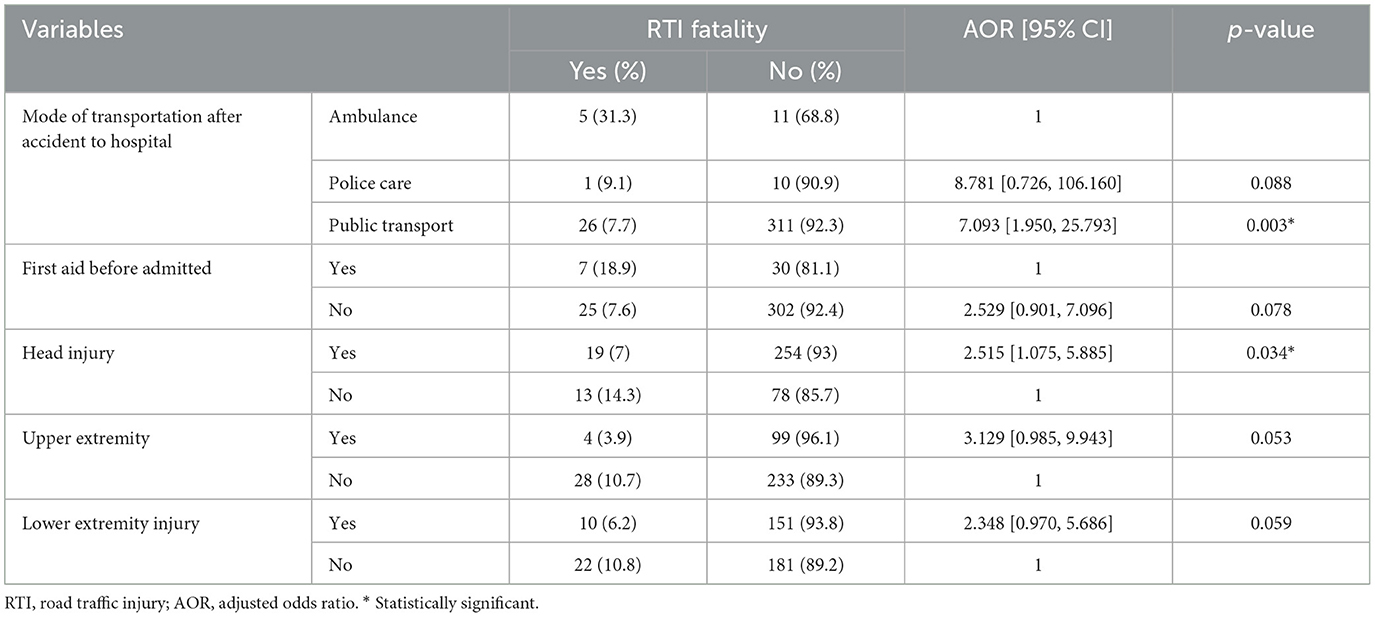
Table 4. Multivariate logistic regression of factors associated with RTI fatality from January 1 to December 30, 2018, in St. Luke Hospital, South West Shewa Zone, Oromia Region.
Discussion
The trend of RTI fatalities in this study shows that between January and December 2018, there were 32 deaths, or ~3 deaths per month on average. The highest RTI rate was observed during November, which accounted for 13% of total injuries compared to an average of 8.3% per month during the study period. A similar study conducted in the emergency department of Zewditu Memorial Hospital showed that between September 2014 and August 2015, ~779 RTI cases were admitted to the emergency department, which was about 8.34% cases per month on average (20). The main reasons for the increase in RTIs may be the increase in the number of vehicle owners, the risky driving behaviors of drivers, poor enforcement of traffic safety rules, and poor road-use behavior of pedestrians.
This study revealed that there were 32 (8.79%) RTI fatalities out of the 364 study participants admitted to the emergency department of the hospital because of an RTI. A higher death rate was observed in this study compared to a study conducted in Tikur Anbesa Specialized Hospital on injury characteristics and outcomes that revealed that in all RTI victims reaching the hospital, 7.4% died (21). Other studies conducted at Wolayita Sodo Hospital and Zewditu Memorial Hospital indicated that 6% and 1%, respectively, died (20, 22). Fatalities in this study were lower than those reported in the same study conducted in Dilchora referral hospital, Dire Dawa (9.4%) (18), and at the tertiary care center in Lucknow, India (13.1%) (23). Because the hospital where the study was conducted was used as a referral center and many victims were linked to another health facility, life-threatening cases may have led to higher death rates.
This study revealed that RTA victims referred to the hospital who had not gotten an ambulance as a mode of transportation after the occurrence of injury were more than seven times more likely to die from an RTI compared to those who did get an ambulance (AOR = 7.093, 95% CI [1.950, 25.793]). According to a 2013 WHO road safety report on the African region, five countries have no ambulance services. In 22 countries (50%), experts estimate that < 10% of seriously injured patients benefited from ambulance evacuation. In only nine of the 44 countries (22%) are a reasonable proportion (50% and above) of injured patients taken to hospital by ambulance (24). This may be because those who got an ambulance received first aid before they reached the hospital, minimizing the chance of death.
Injuries to the head are the main cause of death from RTIs. This study showed that RTA victims who had head injuries were more than two times more likely to die compared to those who did not have a head injury (AOR = 2.515, 95% CI [1.075, 5.885]). This finding is lower than the study conducted in Taiwan in 2016 that showed that those who had head injuries were >14 times more likely to die compared to those who did not have a head injury (AOR = 14.6, 95% CI [7.7, 27.8]) (25). A study done in Tanzania also reported that head injuries are the most common type of injury sustained, which predisposed victims to prolonged hospitalization and mortality (26). This may be due to the seriousness of a head injury, which has the potential to cause death in injured victims.
The study results showed that there is no significant association between the victims' residence area, gender, age, source of referral, or injury characteristics like chest injuries, abdominal injuries, or upper and lower extremity injuries with emergency department treatment fatalities of RTA victims.
In this study, both males and females were exposed to RTI fatalities. The study's results showed that males were highly affected by RTI fatalities, accounting for 26 (81.25%) among RTI victims. It is in line with a similar study conducted in Iran in 2016 that showed males accounted for almost 78.7% of RTIs (27). Similarly, a study conducted in Tanzania in 2012 also showed that the male-to-female ratio of RTI fatalities was 2.1:1 (26). A cross-sectional study conducted at Tikur Anbesa Specialized Hospital composed of 71.7% male and 28.3% female RTA victims resulted in a male-to-female fatality ratio of 2.6:1 (21). That more males than females die from RTIs may be explained by the movement of males to support their families and their exposure to high-risk activities.
According to this study, RTI fatalities were higher among those aged 15–29 (20, 10.5%), followed by those aged 30–44 (7, 7.6%). A similar study done in India in 2013 also showed that the highest number of victims of RTI fatalities (51.8%) were 16–30 years of age, followed by those aged 31–45 years (25.1%) (28). The study conducted in Burrayu town in 2016 also showed that those aged 18–30 accounted for 59% of the total fatalities, followed by those aged 31–50, who accounted for 20% (29). The higher vulnerability of those aged 15–29 may be because productive age groups, in the effort to earn income for their family and themselves, expose themselves to traffic injuries. In contrast to this study, a study in India in 2016 showed that the 30–44-year-old age group is the most vulnerable to road accident fatalities (35%), followed by the 15–29-year-old age group, which accounted for 29.9% (30).
Limitations
Because secondary data were used, the current study was unable to identify crash characteristics, and drivers' behaviors like using substances (alcohol, khat, and others) were not studied. And the records also lack some important data, such as driver's level, the quality of roads, and the utilization of seat belts, helmets, and mobile phones. Also, we did not consider any variables with clinical significance unless it was statistically significant. Therefore, generalizing these results should be done with caution.
Conclusion and recommendations
RTI fatalities are an important public health problem. The trends of RTIs varied from month to month, and the highest number of deaths occurred from August to November 2018. A lack of ambulance services for transporting RTI victims to the hospital after the accident and head injuries were the main causes of death from an RTI.
Appropriate preventive measures targeting reducing the occurrence of RTIs are necessary to reduce deaths from RTIs and reduce the number of families exposed to social crises due to the death of their family member due to an accident or RTI.
The Oromia Regional Health Bureau and the Ministry of Health should organize the availability and accessibility of prehospital care services for RTI victims.
Moreover, the Transport Authority and traffic police should work with other stakeholders and take appropriate measures to reduce the problems caused by RTIs in the region. They should work on the provision of important messages to all members of the community regarding knowledge and practices of road safety measures, such as the appropriate use of the road by pedestrians and avoiding risky driving behaviors. Besides this, the traffic police and Transport Authority should make the use of motorcycle helmets compulsory for motorbike users to decrease RTAs.
Further research should be conducted to explore the risk factors that hinder and/or aggravate the frequency of RTAs in the community.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical clearance was secured from the Institutional Review Board of the Institute of Health of Jimma University on February 27, 2019, reference number, IHRPGD/181/2019.
Author contributions
TB: Conceptualization, Formal analysis, Investigation, Methodology, Software, Supervision, Visualization, Writing—original draft, Writing—review & editing, Data curation, Funding acquisition, Project administration, Resources, Validation. SS: Data curation, Formal analysis, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing. GF: Formal analysis, Supervision, Visualization, Writing—original draft, Writing—review & editing, Conceptualization, Investigation, Methodology, Software. KW: Conceptualization, Investigation, Methodology, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge St. Luke Catholic Hospital and College of Nursing and Midwifery staff for their facilitation role during the data collection process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/femer.2023.1328817/full#supplementary-material
References
3. Ghaffar A, Hyder AA, Masud TI. The burden of road traffic injuries in developing countries : the 1st national injury survey of Pakistan. Public Health. (2004) 118:211–7. doi: 10.1016/j.puhe.2003.05.003
6. Bener A, Burgut HR, Sidahmed H, Albuz R, Sanya R. Khan WA. Road traffic injuries and risk factors. California J Health Prom. (2009) 7:92–101. doi: 10.32398/cjhp.v7i2.2017
7. Chisholm D, Naci H. Road Traffic Injury Prevention : An Assessment of Risk Exposure and Intervention Cost-Effectiveness in Different World Regions. Geneva: World Health Organization (2008). p. 1–59.
9. Hyder PAA, Puvanachandra DP, Allen KA. Road Traffic Injury Trauma Care: Innovations For Policy (Road Trip) Road Traffic Injury. (2013). Available online at: https://2020.wish.org.qa/app/uploads/2021/01/27425_WISH_Road_Injuries_Report_web.pdf
12. WHO. Road-Traffic-Injuries @. (2018). Available online at: www.who.int (accessed December 21, 2018).
13. UN. General Assembly on Transforming our World: the 2030 Agenda for Sustainable Development. (2015). p. 1–35.
15. Bhalla K, Harrison J, Abraham J, Bartels D, Naghavi M, Lozano R, et al. Burden of Road Injuries in Sub-Saharan Africa. (2014). p. 1–112.
17. St.Luke. Index. (2019). Available online at: www.stlukecatholichospital.org. (accessed September 10, 2019).
18. Negesa L, Egziabher G, Mohammed J. Assessment of Magnitude and Treatment Outcome of Road Traffic Accident from January 2013-January 2015 in Dilchora Referral Hospital, Diredawa Eastern Ethiopia. (2017).
19. WHO. Guidelines for Conducting Community Surveys on Injuries and Violence. Geneva: WHO. (2004). p. 1–151.
20. Getachew S, Ali E, Silkondez W, Abebe D, Deressa W, Enquessilase F, et al. The burden of road traffic injuries in an emergency department in Addis Ababa, Ethiopia. (2016) 6:66–71. doi: 10.5588/pha.15.0082
21. Seid M, Azazh A, Enquselassie F, Yisma E. Injury characteristics and outcome of road traffic accident among victims at Adult Emergency Department of Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia : a prospective hospital based study. BMC Emerg Med. (2015) 15:1–9. doi: 10.1186/s12873-015-0035-4
22. Hailemichael F, Suleiman M, Wondimagegn P. Magnitude and outcomes of road traffic accidents at Hospitals in Wolaita Zone, SNNPR, Ethiopia. BMC Res Notes. (2015) 8:1–5. doi: 10.1186/s13104-015-1094-z
23. Chauhan A, Ahmed N, Singh JV, Singh VK, Singh A. Kumar S. Disability and mortality following road traffic injury: a follow-up study from a tertiary care centre of India. Int J Communt Med Public Health. (2017) 4:4712–7. doi: 10.18203/2394-6040.ijcmph20175356
25. Huang C, Rau C, Chuang J, Kuo P. Characteristics and outcomes of patients injured in road traffic crashes and transported by emergency medical services. Int J Environ Res Public Health. (2016) 13:236. doi: 10.3390/ijerph13020236
26. Chalya PL, Mabula JB, Dass RM, Mbelenge N. Ngayomela IH. Injury characteristics and outcome of road traffic crash victims at Bugando Medical Centre in Northwestern Tanzania. J Trauma Manag Outcomes. (2012) 6:1. doi: 10.1186/1752-2897-6-1
27. Hamzeh B, Naja F, Karamimatin B, Ahmadijouybari T. Salari A. Epidemiology of traffic crash mortality in west of Iran in a 9 year period. Chin J Traumatol. (2016) 19:70–4. doi: 10.1016/j.cjtee.2015.12.007
28. Rao BB, Sudharani G. Prevalence of Road Traffic Injury and Associated Factors Among Patients Visiting the Emergency Department of Osmania General Hospital, Hyderabad, Telangana, India Abstract: Introduction. (2015). p. 146–9.
29. Bewket TT, Dachew AB, Bifftu BB. Incidence of road traffic injury and associated factors among patients visiting the emergency department of Tikur Anbessa specialized teaching hospital, Addis Ababa, Ethiopia. Emerg. Med. Int. (2014) 2014:0–5. doi: 10.1155/2014/439818
Keywords: road traffic injury, road traffic injury fatality, factors, South West Shewa, Ethiopia
Citation: Beyera TM, Serbessa SD, Fetensa G and Woldemichael K (2024) Trends in fatalities from road traffic injuries and associated factors of patients admitted to the emergency department of St. Luke Hospital, South West Shewa Zone, Ethiopia. Front. Disaster Emerg. Med. 1:1328817. doi: 10.3389/femer.2023.1328817
Received: 27 October 2023; Accepted: 27 December 2023;
Published: 12 January 2024.
Edited by:
Hao Wang, JPS Health Network, United StatesReviewed by:
Nobuhiro Sato, Niigata City General Hospital, JapanIsmet Çelebi, Gazi University, Türkiye
Copyright © 2024 Beyera, Serbessa, Fetensa and Woldemichael. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getahun Fetensa, ZmV0ZW5zYWdldGFodW5AZ21haWwuY29t
 Teshale Merga Beyera1
Teshale Merga Beyera1 Getahun Fetensa
Getahun Fetensa