- 1Institute of Health and Nursing Sciences, Medical Faculty, University of Halle-Wittenberg, Halle, Germany
- 2SRH University of Health Study Program Medical Pedagogy, Gera, Germany
- 3German Red Cross (DRK) Rescue Service Göltzschtal gGmbH, Auerbach, Germany
Background: Every citizen in Germany is entitled to qualified emergency medical assistance. Due to annually increasing deployment figures and personnel shortages, it is no longer possible to guarantee 24/7 coverage of all emergency physician locations throughout Germany. Relief can be achieved through changes in the supply structures. Professional field analyses are the basis for the further development of training and care structures.
Methodology: All emergency physician deployments of a location in the rescue association Südwestsachsen that took place between 01.10.2022 and 31.01.2023 were retrospectively evaluated. For this purpose, the analogously created deployment protocols were examined with regard to demographic data as well as the invasive, non-invasive and pharmacological measures performed by emergency physicians.
Results: In N = 684 emergency missions, n = 471 (100%) invasive or non-invasive measures were performed by an emergency physician. At n = 383 (81.3%), the most frequently performed invasive measure was intravenous (i.v.) access. There were n = 710 (100%) pharmacological measures performed by an emergency physician. The most frequently performed pharmacologic measure was administration of a full electrolyte solution, with n = 223 (31.4%)
Discussion: Emergency physician interventions do not necessarily involve invasive, non-invasive, or pharmacologic measures. The emergency paramedic learns a variety of invasive, non-invasive, and pharmacologic measures in his or her training and could contribute to the reduction of emergency physician interventions. An adaptation of prehospital care structures based on evidence-based data and an update of the catalog of indications for emergency physician interventions would be elementary for this goal.
Introduction
In Germany, there are approximately 2,000 emergency physician bases, which are intended to guarantee comprehensive medical care for emergency patients. An increasing numbers of calls, caused by non-emergency patients using the emergency medical services, and a progressive shortage of specialists mean that not all locations can be continuously staffed. Nevertheless, in order to ensure medical care for every emergency patient in the future, the emergency physician resource must be deployed in a targeted manner according to the indications (1). The aim of this thesis is to counteract this problem and to contribute to the professional field analysis of the emergency medical service. Our work demonstrates, which measures are carried out by emergency physicians in the rescue service employment. A relief of the emergency physicians by emergency paramedics, as well as changes of the supply structures can be discussed on the basis of this and further investigations.
German emergency medical service
The term German emergency medical service refers to the use of the rescue service for critically injured or ill persons and for persons whose health is expected to be seriously damaged if they do not receive immediate medical care. The main goals of EMS service during missions are providing necessary medical care, the preparation of the transportability and the professional care during the transport to a suitable treatment facility for further care in a rescue vehicle equipped for this purpose (2).
The emergency physician
A statement of the Federal Court of Justice from 1992 states that every citizen in Germany is entitled to qualified emergency medical assistance in the rescue service, which corresponds to the respective state of medical knowledge and technology (1). A special qualification is required to work as an emergency physician in Germany. This is regulated at state level. The entry requirement is a completed medical degree. Furthermore, 24 months of further training must be completed in an area of direct patient care in the inpatient sector. Furthermore, 6 months of medical practice in intensive care medicine, anesthesiology or in the emergency department must be completed.
There are no uniform nationwide qualification requirements either in the rescue service laws or in the further training regulations of the federal states. For example, both the additional further training in emergency medicine and the specialist certificate in rescue services can qualify a doctor to work as an emergency physician in the rescue service. Further training generally consists of an 80-h course in general and specialized emergency treatment. After completing the course, 50 emergency medical missions in the public rescue service must be completed under the supervision of a responsible emergency doctor. Up to 25 of these missions can be completed in a special simulation training course.
Vocational field analysis
A vocational field analysis comprises several qualitative as well as quantitative instruments of vocational research. It provides scientific data and serves to determine and identify current conditions within an occupation. The aim of vocational field analyses is to identify vocational fields of action, which serve as a basis for the development of subject and vocational didactics as well as occupation-specific and realistic curricula (3). The prerequisite for the professionalization of an occupational profile is a training curriculum that is oriented to the actual factual circumstances of an occupation (4). Scientific data for vocational field analyses in emergency medical services still show large gaps according to the current status. Vocational scientific foundations that insist on evidence-based figures are not available at the current time (3).
Current state of procedures during EMS missions in Thuringia
In a study in the German rescue service area of Thuringia, N = 1,760 emergency physician interventions were evaluated. Thereby, 1,373 (100%) invasive and non-invasive single measures were performed. The most frequently performed measure was intravenous access with n = 1,051 (76.5%). In addition, 2,163 (100%) pharmacological single measures were performed by emergency physicians. The most frequently used medication was whole electrolyte solution, which was applied in n = 457 (21.1%). In more than 50% of the missions, no measures were performed for which an emergency physician would have been necessary (5).
Aim and research question
The aim of the study is to determine which measures are taken by the emergency physicians in the Rescue association Südwestsachsen. For this purpose, demographic data, invasive and non-invasive as well as pharmacological measures are analyzed.
The work is to contribute to the completion of the professional field analysis of the emergency physician and to provide first current data from the Saxon area. Since other analyses are already taking place in this field, a possible comparison of these is conceivable.
Methodology
A retrospective data evaluation was chosen as the research design. The data were taken as a cross-sectional study from the rescue protocols of the emergency medical services from a rescue station of the Rescue association Südwestsachsen.
For the investigation, a rescue station with an emergency physician location from the Rescue association Südwestsachsen was selected in consultation with the medical director of emergency medical services. The ambulance station selected for the study has two ambulances and one emergency ambulance, which are on duty around the clock. Since the emergency ambulance has to cover a larger area, it also encounters vehicles from other rescue stations as standard.
Approval
Permission to conduct the study was obtained through the two medical directors of ambulance services and the managing director of the rescue association. For this purpose, the background and intentions were explained both verbally with the Medical Director of Rescue Services and in writing for the other two parties.
Implementation of the study
Every emergency operation carried out by an ambulance or emergency medical service vehicle must be documented. This is required by §9 par. 2 of the SächLRettDPVO. For the study, a rescue station with an emergency physician location from the rescue association Südwestsachsen was selected in consultation with the Medical Director of Rescue Services. The rescue station selected for the investigation has two ambulances and one emergency doctor vehicle, which are on duty around the clock.
If an emergency physician is involved in the care, he or she must take over the documentation. Demographic data, as well as diagnostic, invasive, non-invasive and pharmacological measures are written down on the protocols. Likewise, a diagnosis or suspected diagnosis is determined. The rescue protocols are collected in the rescue stations and forwarded at regular intervals to the medical directors of rescue services for checking and archiving. The documentation of the missions in the rescue association Südwestsachsen is done analogously.
This study looks at the missions that took place between 01.10.2022 and 31.01.2023.
Extraction of data
An analysis of the data was performed using Microsoft Excel. After completion of the data collection, 10% of the data sets were randomly checked for errors. Since no errors were identified during this process, a complete check of the data set was not performed. The data were analyzed via the program and made comparable. During the period studied, a total of N = 684 (100%) emergency medical vehicle calls could be evaluated.
Ethics
The study protocol was submitted to the Ethics Committee of the Medical Faculty, University of Halle-Wittenberg and positively reviewed (Edit. No. 2022-102).
Results
Demographics
Of N = 684 emergency cases, n = 357 (52.19%) patients were male and n = 327 (47.81%) were female. The mean age of the patients was 64.52 years. The minimum age was 0 years and the maximum age was 101 years.
Specialties and suspected diagnoses
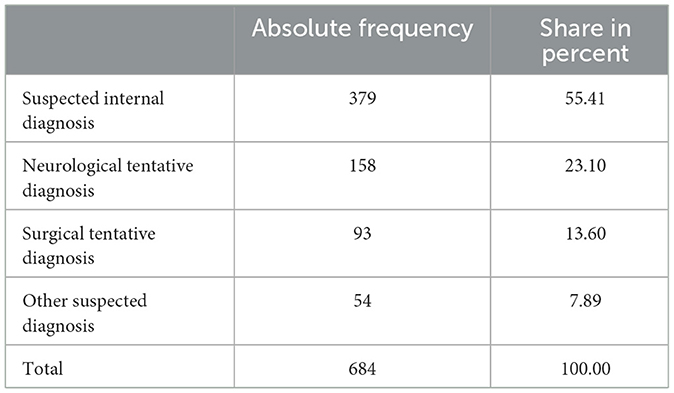
A breakdown of the N = 684 emergency calls showed that, at n = 379 (55.41%), the most frequent emergency calls could be assigned to the internal medicine specialty (Table 1).
Performance of invasive and non-invasive measures by an emergency physician
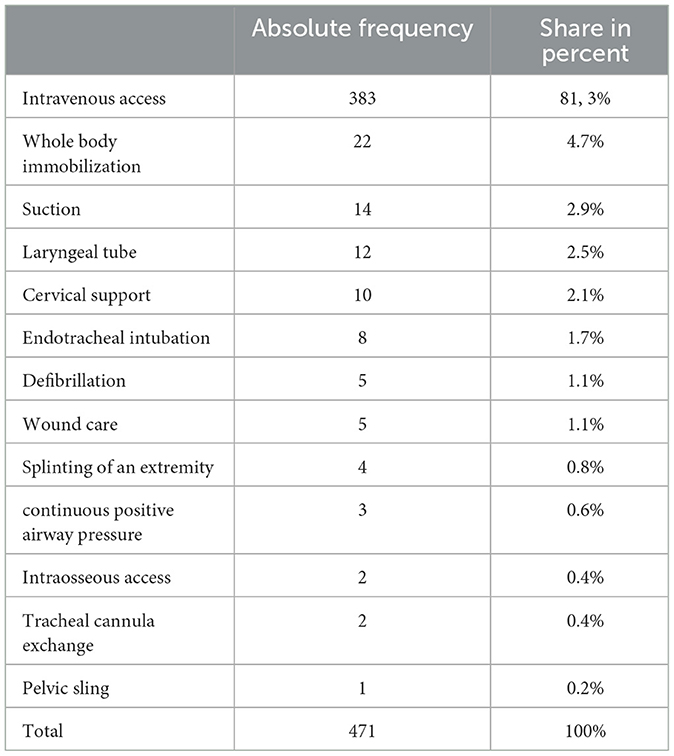
Of N = 684 emergency interventions, invasive or non-invasive measures were performed by an emergency physician in n = 471 (100%). At n = 383 (81.3%), the most frequently performed measure was intravenous (i.v.) access (Table 2).
Performance of pharmacological measures by an emergency physician
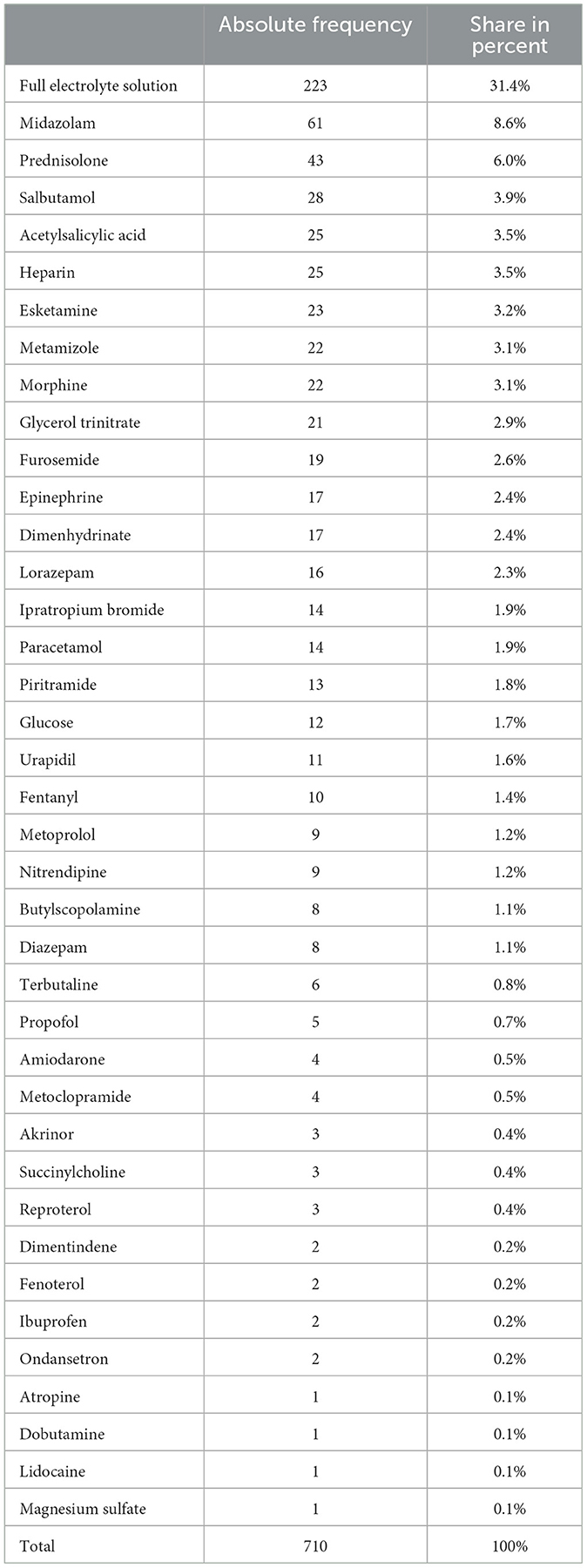
Of N = 684 emergency interventions, n = 710 (100%) pharmacological measures were performed by an emergency physician. The most frequently performed pharmacological measure was the administration of a full electrolyte solution, with n = 223 (31.4%) (Table 3).
Execution of a transport
Of the total N = 684 emergency calls, n = 512 (74.85%) emergency calls involved transporting the patient to a hospital.
Discussion
In the study by Koch and Sauerbier (5), the most frequently identified suspected diagnosis was psychiatric emergency. This occurred in 11.9% of all call-outs (5). In the study presented here, psychiatric emergency also has a high proportion with 8.33%. Deployments with psychosocial problems are considered to be a partial reason for the steadily increasing number of deployments of emergency medical services (6).
Of N = 684 emergency calls, invasive or non-invasive action was performed by an emergency physician in n = 471 (100%). At n = 383 (81.3%), the most frequently performed invasive measure was intravenous (i.v.) access. There were n = 710 (100%) pharmacological measures performed by an emergency physician. The most frequently performed pharmacological measure was the administration of a full electrolyte solution, with n = 223 (31.4%).
The study by Koch and Sauerbier (5) came to the same results. Here, at least one invasive or non-invasive measure was performed in 61.5% of emergency interventions. Again, intravenous access was performed most frequently (5). The frequency of intravenous access could be explained by the fact that it serves as a basis for performing further invasive measures and medication applications. It is often established early in patient care (7). A pharmacological measure was taken in 55.12% of the missions. The most frequently applied drug in this case was the full electrolyte solution. Also in this point, similar results can be found in the study of Koch and Sauerbier (5). Here, a medication was administered in 59.7% of the deployments. Full electrolyte solution was also found to be the most common medication (5).
Fields of activity of emergency physicians and paramedics
The study shows that emergency physician missions are not necessarily accompanied by invasive, non-invasive or pharmacological measures. In only 55–60% of the missions at least one of these measures was performed. This raises the question at this point whether the resource emergency physician was necessary in the remaining missions without measures having taken place or whether the care of the patient by exclusively emergency paramedics would have been just as conceivable. Especially in the case of psychiatric incidents, the primary emergency physician alerting could be dispensed with. Here, the numbers of invasive, non-invasive, and pharmacological measures performed were significantly lower than for missions with different suspected diagnoses.
In their training, emergency paramedics learn a variety of invasive curative as well as pharmacological measures in order to be able to adequately treat the multitude of different emergency images. Since the Training Act—Emergency Paramedic Act (NotSanG) is valid nationwide, every emergency paramedic has the same competencies after completing their training. They are limited in their later work only by the various instructions of the medical directors of rescue services of the rescue associations.
At this point, it can be mentioned that emergency paramedics would not only be able to independently take over primary emergency physician missions without invasive, non-invasive, or pharmacological measures having taken place, but also those missions in which no measure has been carried out that must necessarily be performed by a physician. Over 80% of the invasive, non-invasive or pharmacological measures analyzed in this study, which were carried out by emergency physicians, could also have been carried out by emergency paramedics, as they had learned these during their training.
Uniform nationwide regulation of out-of-hospital care structures would not be possible at the present time, as legislation is based at the state level. Thus, each federal state independently determines the indications that are necessary for the deployment of an emergency physician. Emergency paramedics are also restricted in their learned competencies by the instructions and recommendations for action of the medical directors of rescue services (§4 par. 2c NotSanG). Through a nationwide uniform regulation of the rescue service, the same care and support could be guaranteed for every citizen of the Federal Republic.
Critique
The present work exclusively discloses the measures carried out by emergency physicians from one location of the rescue association Südwestsachsen over a short period of investigation. No generally valid statements for the rescue association Südwestsachsen or the Free State of Saxony can be drawn from the resulting scope. For this, further investigations would have to follow.
Another limitation is the analogous documentation of operations. The quality of the documentation depends on the emergency physicians. Both errors due to poor legibility of the protocols and incomplete documentation can be assumed. It can be assumed that more invasive, non-invasive and pharmacological measures were performed, but these were not documented on the rescue protocols.
Conclusion and outlook
The study presented here provides for the first time data on the measures performed by emergency physicians from the rescue association Südwestsachsen. Thus, it contributes to a small part of the professional field research of the rescue service.
In this study it could be shown that the emergency physician is sent to a large number of operations for which there is no emergency physician indication on site. The emergency paramedic could independently take over missions that are within the scope of his competences and thus contribute to a reduction of emergency physician missions. Over 80% of the invasive, non-invasive and pharmacological measures evaluated by emergency physicians in this study could already be carried out independently by emergency paramedics today. If emergency paramedics were to take over non-indicated emergency medical interventions, this could relieve the burden on the emergency medical system and guarantee medical care for patients in vital danger. The prerequisite for this would be changes and adjustments in prehospital care structures based on evidence-based data from professional field analyses. In order to achieve a general professionalization of the rescue service, comprehensive studies of the actual work of rescue personnel throughout Germany would be elementary. This is the only way to compensate for rising deployment figures and staff shortages.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SK: Writing—original draft. MS: Writing—original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
MS was employed by German Red Cross (DRK) Rescue Service Göltzschtal gGmbH.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sefrin P, Dörges V. Problems in emergency medical care. Notarzt. (2022) 38:310–313. doi: 10.1055/a-1921-6664
2. Koch S, Steinkrauß M. Development and structure of emergency medical services in Germany. In: Emergency Medical Services - Rescue, Stuttgart, Georg Thieme Verlag KG. (2023). p. 18–35.
3. Frieß C, Koch S. On the need for an occupational field analysis in emergency medical services - A current presentation and project-based overview. Teach Learn Health Care. (2022) 5–14. doi: 10.52205/llig/16
4. Becker M, Spöttl G. Vocational science research its empirical relevance for curriculum development. Vocational Business Education. (2006). Available online at: http://www.bwpat.de/ausgabe11/becker_spoettl_bwpat11.pdf (accessed November 30, 2023).
5. Koch S, Sauerbier T. Occupational field analysis of invasive and non - invasive as well as pharmacological measures by emergency physicians in the German emergency medical service - a retrospective cross-sectional study of the interventions carried out in the German emergency. EC Emer Med Crit Care. (2023) 1–9. doi: 10.3389/femer.2023.1302612
6. Lauer D, Bandlow S, Rathje M, Seidl A, Karutz H. Changes and developments in pre-hospital emergency care: key challenges for ambulance service management. Federal Health Gazette. (2022) 65:987–995. doi: 10.1007/s00103-022-03588-x
Keywords: emergency physician, emergency paramedic, emergency medical service, invasive and non-invasive measures, pharmacological measures, vocational field analysis
Citation: Koch S and Suffeda M (2023) Performance of invasive, non-invasive, and pharmacological measures by emergency physicians in the German emergency medical services. A retrospective cross-sectional study from the rescue association Südwestsachsen. Front. Disaster Emerg. Med. 1:1302612. doi: 10.3389/femer.2023.1302612
Received: 26 September 2023; Accepted: 21 November 2023;
Published: 15 December 2023.
Edited by:
Benedikt Treml, Innsbruck Medical University, AustriaReviewed by:
Ozgur Karcioglu, University of Health Sciences, TürkiyeTamorish Kole, University of South Wales, United Kingdom
Copyright © 2023 Koch and Suffeda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sebastian Koch, c2ViYXN0aWFuLmtvY2hAc3JoLmRl
 Sebastian Koch
Sebastian Koch Michelle Suffeda3
Michelle Suffeda3