- 1Department of Basic and Applied Medical Sciences, Ghent University Hospital, Ghent University, Ghent, Belgium
- 2Department of Emergency Medicine, Ghent University Hospital, Ghent, Belgium
- 3EMS Dispatch Centre 112 Flanders, Federal Department of Health, Ghent, Belgium
Aim: Bag-mask ventilation (BMV) is often applied during advanced cardiopulmonary resuscitation (CPR). Lay rescuers usually apply mouth-to-mouth ventilation, which is contraindicated in case of potential disease transmission (e.g., during the COVID-19 pandemic). This study evaluates the influence of rescuers' before BMV training in following the correct BMV procedures during adult and infant CPR.
Methods: Medical students (n = 112) were enrolled in a randomized cross-over manikin study: 60 first-year students (53.6%) (untrained, without any prior knowledge of CPR) and 52 fourth-year students (46.4%) (BLS-trained, with three consecutive years of basic CPR training), excluding Basic Life Support (BLS) certificate holders or lifeguards. Student-formed duos (i.e., two students from the same year working together) received a 15-min just-in-time onsite training in full CPR cycle using BMV and were tested during five cycles of 2-person CPR following the European Resuscitation Council (ERC) guidelines with the inclusion of BMV. Tidal volumes of 300–600 ml (adults) and 20–60 ml (infants) were considered as correct ventilations.
Results: From the initial 56 duos, 17 (30.4%) were excluded after applying incorrect numbers of ventilation or uninterpretable values. In adult CPR, comparing BLS-trained rescuers to untrained ones in correctly administrating ventilations using BMV after a 15-min just-in-time onsite training revealed no statistically significant difference [first years: 63.0% (n = 136 out of 216 ventilations); fourth years: 59.5% (n = 119 out of 200 ventilations); with a proportional difference of −3.5% (−12.8; 5.9)]. In infant CPR, a significant difference was observed in effective ventilations [first years: 55.5% (n = 120 out of 216 ventilations); fourth years: 72.3% (n = 133 out of 184 ventilations); with a proportional difference of 16.8 (7.25; 26.21)].
Conclusion: Two-person BMV is a complex skill to perform both in adults and children, requiring sufficient and regular training. Lay rescuers receiving a 15-min just-in-time onsite BMV training could perform decent BMV in an adult CPR setting. BMV during infant CPR requires more extensive prior training and should not be entrusted to lay rescuers, even after a 15-min just-in-time onsite training.
1. Introduction
In adults, the global average of out-of-hospital cardiac arrests (OHCA) was ~95.9/100,000/year in 2017. OHCA is the leading cause of death in developed industrial countries with the highest incidence happening at home (>66%), followed by the workplace and public places (±20%). A small increase in OHCA has been described in the European Resuscitation Council (ERC) 2020 guidelines. Cardiopulmonary resuscitation (CPR) should be provided to victims of cardiac arrest (CA), and usage of bag-mask ventilation (BMV) is strongly recommended in the first-line setting (1–5). In the pediatric population, OHCA is quite rare, with ~16,000 children worldwide going into OHCA, of which 40–50% occur in infants (6–9). With the leading cause of CA in children being a respiratory event, emphasis is put on the importance of ventilation and oxygenation support (10). From a technical point of view, BMV using the one-person technique produces a significantly smaller volume compared to the two-person BMV technique (11, 12) and increases the risk of a leak. Therefore, a two-person BMV technique is recommended by the ERC, especially in all cases where there is a risk of an inadequate seal or where the possibility of infectious disease transmission via aerosols may occur (7).
Investigation of BMV usage in untrained and BLS-trained rescuers formed the basis of this study. The evaluation focused on the difference in experience between the two groups and its influence on the number of effective ventilations. The main question explored was whether a layman is able to provide ventilations correctly during CPR using BMV both in adult and infant CPR. We define “layman” as persons with no to almost no knowledge of CPR. They may have witnessed CPR but have never carried out CPR themselves.
2. Methods
Recruitment of medical students from the Faculty of Medicine and Health Sciences, Ghent University, Belgium, started after receiving approval from the medical ethics committee of Ghent University Hospital. Students were invited to participate via a message posted on the official communication forum of the University (Ufora). The inclusion criteria were as follows: (1) being a medical student and (2) being able to perform five cycles of CPR. The exclusion criteria involved lifeguards and officially certified Basic Life Support (BLS) providers. The enrolled students had limited to no experience with BMV. First-year medical students were enrolled in the study before following the compulsory CPR training in their curriculum. As such, they had no experience in CPR and received a 15-min just-in-time onsite training. They were considered to be untrained rescuers. Fourth-year medical students had already received three consecutive training sessions in CPR spread over 3 years as per their curriculum. They were considered BLS-trained rescuers in both adult and infant CPR. A priori data were not available and, taking into account recruitment difficulties within the available time period (COVID-19 pandemic), a convenience sample of 112 participants was gathered.
Students formed duos within their year (n = 56 with each duo consisting of two students working together) and followed a 15-min just-in-time onsite training about the full CPR cycle, including the use of bag-mask ventilation (BMV). For first-year students, this was their first CPR training during their medical curriculum, whereas fourth years received their fourth CPR training during their medical training. This 15-min just-in-time onsite training was not part of the actual testing. Actual testing consisted of providing five cycles of CPR with BMV on the manikin (adult and infant). Details are explained in the study by Geerts et al. (13). BMV was administered using the Ambu® SPUR® II–Disposable Resuscitator (Ambu, Copenhagen, Denmark) in adults, with a resuscitator volume of 1,475 ml and a stroke volume of 600 ml for one hand and a stroke volume of 1,000 ml for two hands. The AMBU was coupled to an AERObag®-BM06-3V, PVC resuscitation mask with a valve, and the mask used was size 3. In infant manikins, a BAG II child resuscitator and a size 1 disposable mask were applied (Laerdal®, Stavenger, Norway).
All data were registered using Laerdal's Resusci Anne QCPR and the Resusci Baby QCPR manikin (Laerdal®). The following outcomes were measured: tidal volume [TV] (in ml) and frequency of ventilations, compression depth (in mm), recoil, and hands-off time (in seconds). The primary outcome consisted of the number of correctly administered ventilations, the frequency, and the TV. Secondary outcomes focused on the mean ventilation volume, compression depth, recoil, and hands-off time, all registered using the Resusci Adult QCPR and Resusci Baby QCPR manikin (Laerdal®). Student duos failing in the adult or pediatric BLS algorithms or delivering volumes above 60 ml (maximum volume reported by infant QCPR system) were not retained in the analysis (Figure 1). The standard normal for TV with the infant QCPR system is 20–40 ml. However, 40–60 ml was considered an alternative acceptable normal. Indeed, an estimated normal TV according to ERC guidelines would oscillate between 6 and 8 ml/kg ideal body weight. A ventilation interval of 400–600 ml in adults was chosen, which usually applies to an adult weighing 70 kg.
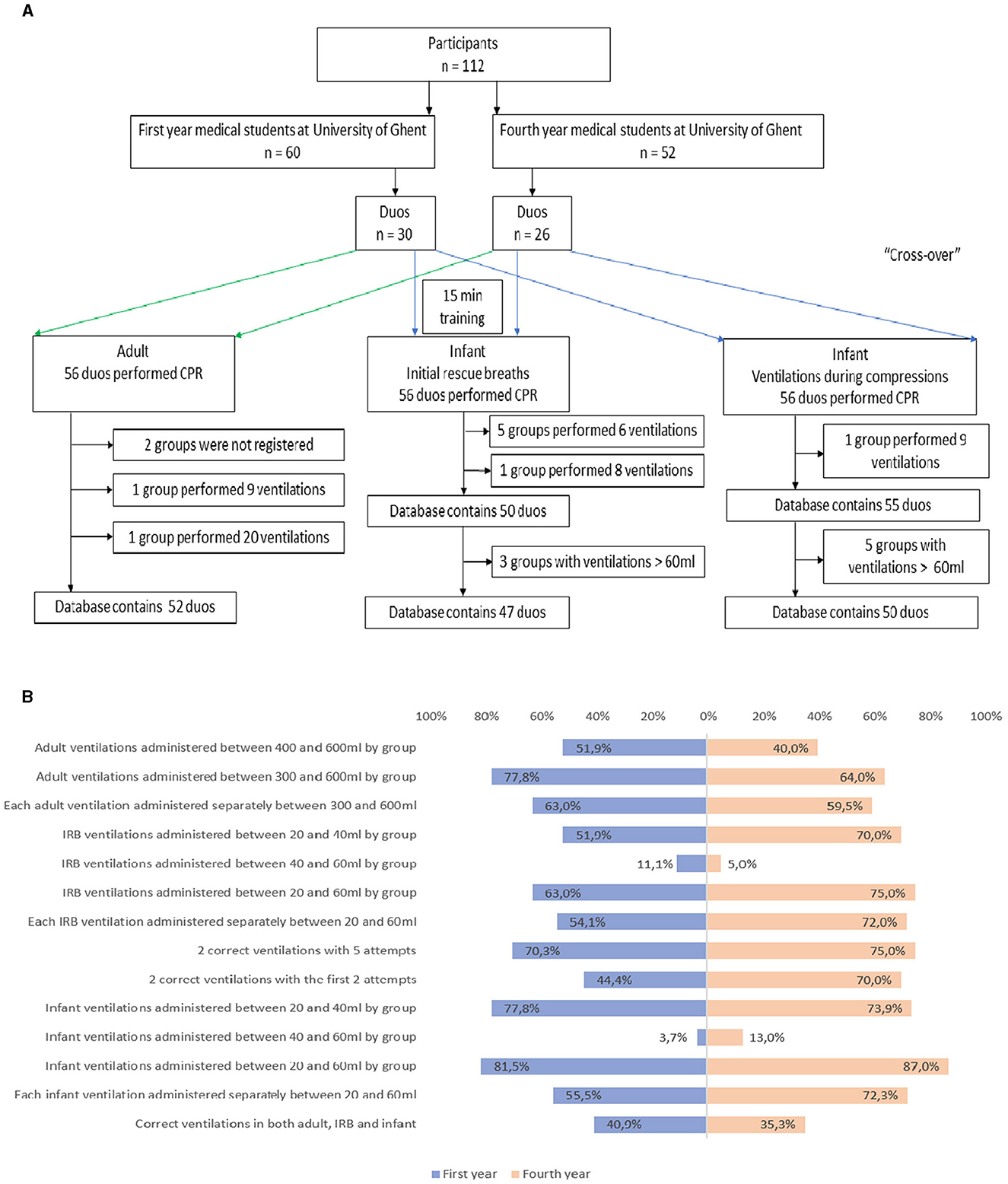
Figure 1. (A) Participants' flow during the study and data cleaning. In both adult and infant CPR, duos not able to perform five cycles of CPR following the ERC guidelines 2020 or delivering ventilation volumes higher than 60 ml in infant CPR were not included in the statistical analysis. (B) Graph showing the differences in results between first-year (untrained) and fourth-year (BLS-trained) medical students. Percentages per year (blue: first years; orange: fourth years) are displayed per category. Lines 1-3 display results in adult ventilation. Lines 4-7 unveil results about IRB. Lines 8 and 9 show results about correct ventilations and the number of attempts provided. Lines 10-13 provide infant ventilation percentages, and the last line shows the correct ventilation percentages across all three categories (adult, IRB, and infant).
Overall, 39 duos (69.6%) from the initial 56 were able to perform the adult, initial rescue breaths (IRB), and infant protocols in a way that conformed to the ERC guidelines 2020 and were, therefore, further included for statistical analysis (Figure 1). In the adult manikin, the excluded duos (n = 2) achieved overinsufflation. This exclusion resulted in a bias of 3.7%. From the excluded duos during infant CPR, one duo performed an incorrect number of ventilations and five duos overinsufflated the infant. Their exclusion yielded a bias in results of 10%.
Statistical analysis involved using the chi-squared test for categorical and ordinal variables. The Shapiro-Wilk test assessed normality in continuous variables by screening the QQ plots. This was followed by either the Mann-Whitney-U test, the unpaired Student's t-test, or the Wilcoxon Signed-Rank test accordingly (IBM SPSS Statistics 27). The significance level was set at 0.05. Differences between proportions were analyzed using the Miettinen-Nurminen method (Statsdirect® 3.3.5).
3. Results
In adult CPR, BMV aims to achieve a TV of 5/6–8 ml/kg. A ventilation volume (VV) of 300–400 ml was therefore considered acceptable in the adult manikin. Untrained students reached an average VV of 422.95 ml (SD 163.07), whereas trained students achieved 435.73 ml (SD 137.58), with no significance between the two groups [t(50) = −0.304; (95% CI: −97.16; 71.62)]. These average VVs exceed the upper limit. Only 51.9% of the untrained group (n = 14 out of 27 duos) and 40.0% of the trained group (n = 10 out of 25 duos) reached the target volume of 400–600 ml, with a Pearson chi-square coefficient of 0.734 (p = 0.392; Figure 2). This exceeds the proposed significance level, allowing rejection of the null hypothesis stating that untrained and trained groups perform differently during BMV in adult CPR. When the interval was expanded to 300–600 ml, the percentage of untrained and trained duos achieving the target volume increased to 77.8% (n = 21 out of 27 duos) and 64.0% (n = 16 out of 25 duos), respectively (Figure 1B), with a Pearson chi-square coefficient of 1.201 and the difference not reaching significance (p = 0.273). Lay rescuers appear to perform equally in BMV compared to BLS-trained rescuers during adult CPR after a 15-min just-in-time training. Prior training of medical students (3 years of medical curriculum and the CPR training sessions included in that curriculum) did not appear to be mandatory in delivering decent BMV in adult CPR. For each volume administered separately, 63.0% (n = 136 out of 216 ventilations) untrained and 59.5% (n = 119 out of 200 ventilations) trained duos reached a volume within the 300–600 ml interval, but without significance (p = 0.632; Figure 2).
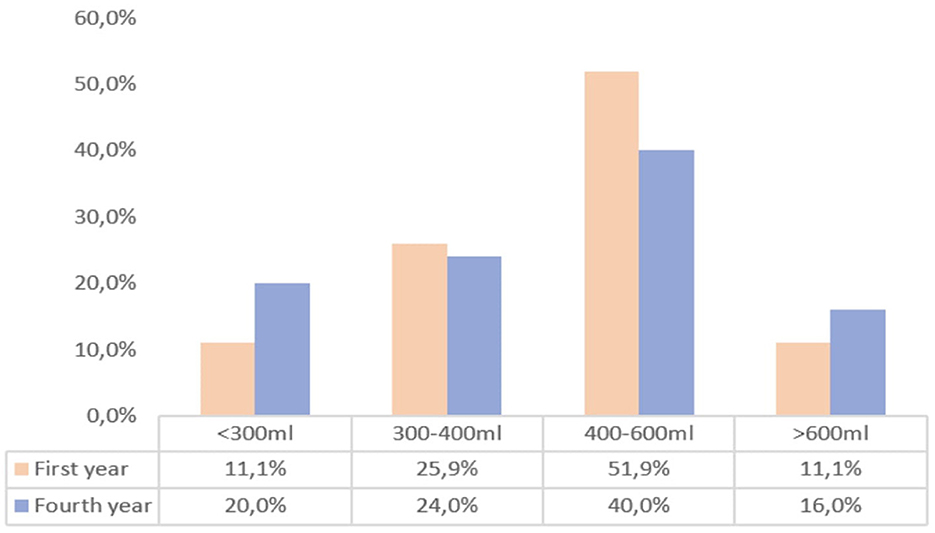
Figure 2. Bar graph representing the percentage of duos that administer a certain volume divided by year in adult CPR. The orange bars represent the percentages of first-year (untrained) duos that deliver a certain ventilation volume in adult manikins (<300, 300–400, 400–600, and >600 ml). The blue bars represent the percentages of fourth-year (BLS-trained) duos that deliver a certain ventilation volume in adult manikins (<300, 300–400, 400–600, and >600 ml).
In the infant manikin, a VV of 20–40 ml was set as the target. Untrained pairs reached an average VV of 25.78 ml (SD 10.04), and trained students reached 31.15 ml (SD 9.11), with both groups not reaching significance between them. The percentage of duos that managed to ventilate the infant during the compressions with a volume of 20–40 ml was 77.8% (n = 21 out of 27 duos) for untrained and 73.9% (n = 17 out of 23 duos) for trained students (Figure 3), with no relationship between these differences. When the interval was extended to 20–60 ml, 81.5% untrained and 86.9% trained participants ventilated in a correct manner (Figure 1B). When looking at each volume administered separately, 55.5% (n = 120 out of 216 ventilations) first years and 72.3% (n = 133 out of 184 ventilations) fourth years reached a VV within the interval of 20–60 ml (Figure 1B). This difference is statistically significant with a Pearson chi-square coefficient of 11.960 (p < 0.001). The value of the Pearson chi-square indicates this significant difference is not due to coincidence. BMV in infant CPR appears to benefit from prior training. Lay rescuers seem to be less capable of decent BMV in infant CPR, even after a 15-min just-in-time training.
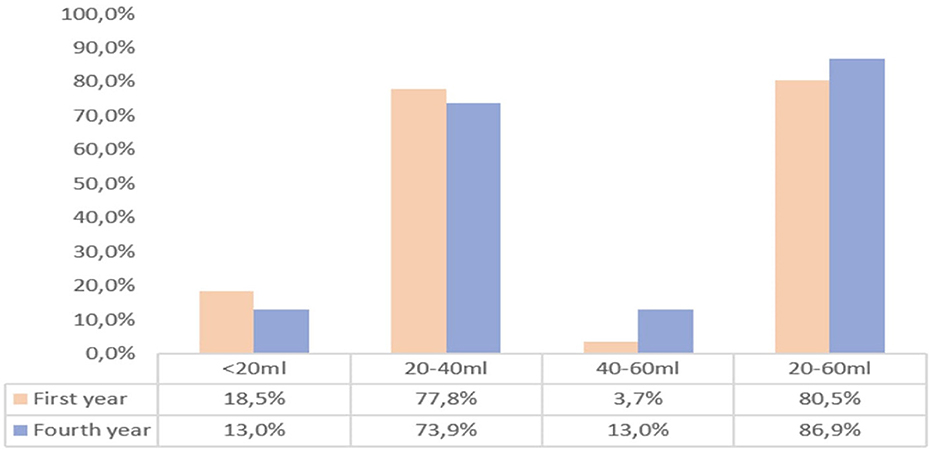
Figure 3. Bar graph representing the percentage of duos that administer a certain volume divided by year in infant CPR. The orange bars represent the percentages of first-year (untrained) duos that deliver a certain ventilation volume in adult manikins (<20, 20–40, 40–60, and >60 ml). The blue bars represent the percentages of fourth-year (BLS-trained) duos that deliver a certain ventilation volume in adult manikins (<20, 20–40, 40–60, and >60 ml).
4. Discussion
This study suggests that lay rescuers could deliver decent BMV in adult CPR after a 15-min just-in-time training, whereas BMV during infant CPR should not be entrusted to them.
Strengths and weaknesses of this study have been described in detail elsewhere (13). Of note is that the abovementioned results may be subject to some limitations. Indeed, measuring averages can yield a correct VV when it is calculated as the mean of a very weak ventilation and a very strong one. This might explain the absence of statistical difference observed in adult BMV between untrained and BLS-trained medical students. Therefore, each ventilation was investigated separately and independently of the group, revealing a new trend. For the 300–600 ml interval, a slight increase in the number of duos performing correct ventilations was noticed in BLS-trained students. The expanded interval of 300–600 ml unveiled a small increase in untrained students, probably forming a more accurate reflection of reality. Another limitation may be found in the just-in-time training, as the propensity to administer correct ventilation with BMV is low in untrained students, thereby achieving similar results as the BLS-trained students. The experience the fourth-year students acquired during their medical curriculum is restrained and could be explained by the lack of sufficient practice opportunities. Of note is that first-year students may have witnessed CPR on a prior occasion, thereby inducing a bias. However, lay rescuers might also have witnessed CPR in their lives.
Although results are encouraging in applying correct ventilations in adult CPR, the need for regular and thorough training is crucial in BMV to attain proficiency, as stated by the American Heart Association and other authors (14–17). Of note is that the used manikin is not a perfect reflection of reality and results should be interpreted with caution. Indeed, a body mass index >26 kg/m2, the presence of a beard, lack of teeth, and a history of snoring have been shown to be associated with difficult BMV (18, 19). All these real-life aspects are not present in the adult manikins. A recent statement paper from the National Association of EMS Physicians (NAEMSP) proposes that teaching the E-O grip over the E-C grip to novices is favorable. In the E-O grip, the operator encircles the mask neck with the first two digits of the hand and the other digits maintain the chin lift, providing a better seal of the mask to the face (20). Using a BMV expert-reviewed checklist during BMV skills teaching to medical students could be of valuable help (21).
In infant manikin ventilation, no significant differences could be observed regarding the mean volume between first-year and fourth-year students. A separate analysis of each individual ventilation revealed a significant difference between fourth-year students achieving the interval of 20–60 ml as compared to first-year students. This could partly be explained by better knowledge of neutral head positioning of the infant by the more experienced students. Sufficient ventilation was only reached by a smaller proportion of duos. A possible explanation may reside in the manikins used in the just-in-time training, which produced a whistle every time a volume was administered in the interval of 20–40 ml. Avoiding hyperventilation in the infant may have been of influence during BMV. A checklist based on the International Network for Simulation-based Pediatric Innovation, Research, and Education (INSPIRE) network checklist for neonatal BMV was created for the pediatric population. Training in pediatric medicine shifts toward entrustment-based assessment as competence during unsupervised practice forms the end point of medical training (22). Incorporating such a checklist in basic medical training might be worth considering.
From the results of this study, two different messages can be conveyed. In infant CPR, the question can be asked whether this limited success rate in untrained rescuers is worth spending time on, as the majority of the ventilations turned out to be insufficient to have an effect. In contrast, 15-min just-in-time adult BMV training can leave laypersons with a decent capacity to apply correct BMV in adult CPR. In a study from 1983, half of the emergency medical technicians failed to ventilate sufficiently with one-person adult BMV. The present study applied the two-person technique, which could explain the encouraging results. If possible, the two-person technique should be favored over the one-person technique, both in adult and infant BMV, especially considering the great variability in oxygen delivery in BMV and the necessity to avoid gastric inflation (23–25). In medical students, the need to teach the two-person technique in BMV is therefore of great importance (20, 26–32).
5. Conclusion
To conclude, this study evaluated the ability of laypersons to perform BMV. By providing a short training beforehand, encouraging results can be achieved in BMV in adult CPR as opposed to BMV during infant CPR, where prior skills are deemed necessary. During BMV in infant CPR, laypeople scored a significantly lower volume than the minimally trained rescuers. Rescuers are encouraged by the ERC to apply the two-person BMV technique both in adult and infant CPR, and this recommendation was further strengthened by these results.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of the Ghent University Hospital.
Author contributions
GB: Data curation, Investigation, Methodology, Software, Visualization, Writing—original draft. AG: Data curation, Investigation, Methodology, Software, Visualization, Writing—original draft. MC: Software, Validation, Writing—original draft. EC-L: Data curation, Investigation, Software, Validation, Writing—original draft. SH: Data curation, Funding acquisition, Investigation, Methodology, Software, Validation, Visualization, Writing—original draft. PV: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing—review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by a BeSEDiM R-Aiders grant 2022-2023.
Acknowledgments
The authors wish to acknowledge all students who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Porzer M, Mrazkova E, Homza M, Janout V. Out-of-hospital cardiac arrest. Biomed Pap Med Fac Univ Palacky Olomouc Czechoslov. (2017) 161:348–53. doi: 10.5507/bp.2017.054
2. Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, et al. European resuscitation council guidelines for resuscitation 2015: section 2. Adult basic life support and automated external defibrillation. Resuscitation. (2015) 95:81–99. doi: 10.1016/j.resuscitation.2015.07.015
3. Olasveengen TM, Semeraro F, Ristagno G, Castren M, Handley A, Kuzovlev A, et al. European resuscitation council guidelines 2021: basic life support. Resuscitation. (2021) 161:98–114. doi: 10.1016/j.resuscitation.2021.02.009
4. Rea T, Kudenchuk PJ, Sayre MR, Doll A, Eisenberg M. Out of hospital cardiac arrest: past, present, and future. Resuscitation. (2021) 165:101–9. doi: 10.1016/j.resuscitation.2021.06.010
5. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA. (2019) 321:1200–10. doi: 10.1001/jama.2019.1696
6. Gräsner JT, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I, et al. Survival after out-of-hospital cardiac arrest in Europe - results of the EuReCa TWO study. Resuscitation. (2020) 148:218–26. doi: 10.1016/j.resuscitation.2019.12.042
7. de Van de Voorde PV, Turner NM, Djakow J, de Lucas N, Martinez-Mejias A, Biarent D, et al. European resuscitation council guidelines 2021: paediatric life support. Resuscitation. (2021) 161:327–87. doi: 10.1016/j.resuscitation.2021.02.015
8. Knudson JD, Neish SR, Cabrera AG, Lowry AW, Shamszad P, Morales DLS, et al. Prevalence and outcomes of pediatric in-hospital cardiopulmonary resuscitation in the United States: an analysis of the kids' inpatient database*. Crit Care Med. (2012) 40:2940–4. doi: 10.1097/CCM.0b013e31825feb3f
9. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the resuscitation outcomes consortium epistry–cardiac arrest. Circulation. (2009) 119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678
10. Mick NW, Williams RJ. Pediatric cardiac arrest resuscitation. Emerg Med Clin North Am. (2020) 38:819–39. doi: 10.1016/j.emc.2020.06.007
11. Kitagawa KH, Nakamura NM, Yamamoto L. Retention of pediatric bag-mask ventilation efficacy skill by inexperienced medical student resuscitators using standard bag-mask ventilation masks, pocket masks, and blob masks. Am J Emerg Med. (2006) 24:223–6. doi: 10.1016/j.ajem.2005.10.009
12. Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, et al. European resuscitation council guidelines 2021: adult advanced life support. Resuscitation. (2021) 161:115–51. doi: 10.1016/j.resuscitation.2021.02.010
13. Geerts A, Herbelet S, Borremans G, Coppens M, Christiaens-Leysen E, Van de Voorde P, et al. Five vs. two initial rescue breaths during infant basic life support: a manikin study using bag-mask-ventilation. Front Pediatr. (2022) 10:1067971. doi: 10.3389/fped.2022.1067971
14. Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2015) 132:S414–35. doi: 10.1161/CIR.0000000000000259
15. Augustine JA, Seidel DR, McCabe JB. Ventilation performance using a self-inflating anesthesia bag: effect of operator characteristics. Am J Emerg Med. (1987) 5:267–70. doi: 10.1016/0735-6757(87)90348-2
16. Bauman EB, Joffe AM, Lenz L, DeVries SA, Hetzel S, Seider SP. An evaluation of bag-valve-mask ventilation using an ergonomically designed facemask among novice users: a simulation-based pilot study. Resuscitation. (2010) 81:1161–5. doi: 10.1016/j.resuscitation.2010.05.005
17. Strzelecki C, Shelton CL, Cunningham J, Dean C, Naz-Thomas S, Stocking K, et al. randomised controlled trial of bag-valve-mask teaching techniques. Clin Teach. (2020) 17:41–6. doi: 10.1111/tct.13008
18. Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. (2000) 92:1229–36. doi: 10.1097/00000542-200005000-00009
19. Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O'Reilly M, et al. Incidence and predictors of difficultand impossible mask ventilation. Anesthesiology. (2006) 105:885–91. doi: 10.1097/00000542-200611000-00007
20. Lyng JW, Guyette FX, Levy M, Bosson N. Prehospital manual ventilation: an NAEMSP position statement and resource document. Prehosp Emerg Care. (2022) 26:23–31. doi: 10.1080/10903127.2021.1981506
21. Pandey A, McHugh M, Michael M. Teaching and assessing bag valve mask ventilation to 4th year medical students via checklist. West J Emerg Med. (2022) 23.
22. Whalen AM, Merves MH, Kharayat P, Barry JS, Glass KM, Berg RA, et al. Validity evidence for a novel, comprehensive bag-mask ventilation assessment tool. J Pediatr. (2022) 245:165–71. doi: 10.1016/j.jpeds.2022.02.017
23. Elling R, Politis J. An evaluation of emergency medical technicians' ability to use manual ventilation devices. Ann Emerg Med. (1983) 12:765–8. doi: 10.1016/S0196-0644(83)80254-6
24. Dodds JM, Appelqvist DI, Paleologos MS, Downey RG. Variability in oxygen delivery with bag-valve-mask devices: an observational laboratory simulation study. Anaesth Intensive Care. (2023) 51:130–40. doi: 10.1177/0310057X221119824
25. Kim TY, Kim S, Han S II, Oh Hwang S, Jung WJ, Roh Y II, et al. Gastric inflation in prehospital cardiopulmonary resuscitation: aspiration pneumonia and resuscitation outcomes. Rev Cardiovasc Med. (2023) 24:198. doi: 10.31083/j.rcm2407198
26. Gerber L, Botha M, Laher AE. Modified two-rescuer CPR with a two-handed mask-face seal technique is superior to conventional two-rescuer CPR with a one-handed mask-face seal technique. J Emerg Med. (2021) 61:252–8. doi: 10.1016/j.jemermed.2021.03.005
27. Hess D, Baran C. Ventilatory volumes using mouth-to-mouth, mouth-to-mask, and bag-valve-mask techniques. Am J Emerg Med. (1985) 3:292–6. doi: 10.1016/0735-6757(85)90049-X
28. Joffe AM, Hetzel S, Liew ECA. two-handed jaw-thrust technique is superior to the one-handed “EC-clamp” technique for mask ventilation in the apneic unconscious person. Anesthesiology. (2010) 113:873–9. doi: 10.1097/ALN.0b013e3181ec6414
29. Otten D, Liao MM, Wolken R, Douglas IS, Mishra R, Kao A, et al. Comparison of bag-valve-mask hand-sealing techniques in a simulated model. Ann Emerg Med. (2014) 63:6–12. doi: 10.1016/j.annemergmed.2013.07.014
30. Jesudian MC, Harrison RR, Keenan RL, Maull KI. Bag-valve-mask ventilation; two rescuers are better than one: preliminary report. Crit Care Med. (1985) 13:122–3. doi: 10.1097/00003246-198502000-00015
31. Davidovic L, LaCovey D, Pitetti RD. Comparison of 1- versus 2-person bag-valve-mask techniques for manikin ventilation of infants and children. Ann Emerg Med. (2005) 46:37–42. doi: 10.1016/j.annemergmed.2005.02.005
Keywords: cardiopulmonary resuscitation (CPR), manikin study, bag-mask ventilation, adult, pediatric, Basic Life Support (BLS)
Citation: Borremans G, Geerts A, Coppens M, Christiaens-Leysen E, Herbelet S and Van de Voorde P (2023) Bag-mask ventilation by low- or untrained rescuers during adult and pediatric resuscitation: a randomized cross-over manikin study. Front. Disaster Emerg. Med. 1:1274501. doi: 10.3389/femer.2023.1274501
Received: 08 August 2023; Accepted: 12 October 2023;
Published: 14 November 2023.
Edited by:
Ioannis Pantazopoulos, University of Thessaly, GreeceReviewed by:
Ozgur Karcioglu, University of Health Sciences, TürkiyeCsaba Dioszeghy, Surrey and Sussex Healthcare NHS Trust, United Kingdom
Copyright © 2023 Borremans, Geerts, Coppens, Christiaens-Leysen, Herbelet and Van de Voorde. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patrick Van de Voorde, cGF0cmljay52YW5kZXZvb3JkZUB1Z2VudC5iZQ==
†These authors have contributed equally to this work and share last authorship
 Gautier Borremans1
Gautier Borremans1 Anke Geerts
Anke Geerts Erik Christiaens-Leysen
Erik Christiaens-Leysen Sandrine Herbelet
Sandrine Herbelet