- 1Stead Family Department of Pediatrics, Division of Pediatric Intensive Care, University of Iowa, Iowa City, IA, United States
- 2Department of Pediatrics, Division of Neonatal Intensive Care, University of Wisconsin, Madison, WI, United States
- 3Stead Family Department of Pediatrics, Division of Neonatal Intensive Care, University of Iowa, Iowa City, IA, United States
- 4Department of Biomedical Engineering, University of Iowa, Iowa City, IA, United States
- 5Stead Family Department of Pediatrics, Division of Pediatric Cardiology, University of Iowa, Iowa City, IA, United States
Background: The guideline recommended chest compression depth, rate, and recoil are essential factors for the return of spontaneous circulation (ROSC) in cardiopulmonary resuscitation (CPR). A pediatric resuscitation collaboration recently demonstrated that healthcare providers fail to meet the American Heart Association (AHA) guidelines, with the greatest difficulty being in achieving chest compression depth targets in infants. We hypothesized that the use of the heel of one hand [open palm technique (OPT)] will increase chest compression depth in infants compared to standard CPR techniques [two-finger technique (TFT), two thumb-encircling hand technique (TTT)].
Methods: A prospective, randomized, single-center study was completed using an infant manikin. Thirty pediatric critical care providers performed 2 min of CPR for each technique followed by 5 min of rest. Each participant completed a survey at the end that assessed the difficulty level in order to assess the feasibility of this new technique.
Results: The mean chest compression depth for the OPT was significantly deeper compared to TFT (2.61± 0.63 cm vs. 2.25 ± 0.54 cm, p = 0.0004) but not significantly deeper compared to TTT (2.43 ± 0.46 cm, p = 0.0820). OPT was graded as the easiest technique, followed by TTT (2.20 ± 0.76 vs. 3.17 ± 0.95, p < 0.0001) and then TFT (3.38 ± 0.83, p < 0.0001).
Conclusion: The use of OPT for infant CPR resulted in improved chest compression depth. OPT was considered the easiest technique compared to standard infant CPR techniques, thus making it feasible to perform. Importantly, all providers failed to meet the AHA infant chest compression depth goal of 4 cm, regardless of the technique. Future research is needed to optimize CPR technique and performance to achieve targeted chest compression depth in infants.
1. Introduction
Pediatric cardiac arrest requiring cardiopulmonary resuscitation (CPR) occurs in 2–6% of children admitted to pediatric intensive care units (PICU), resulting in high mortality (1–3). High-quality CPR is the primary component influencing survival and neurodevelopmental outcomes after cardiac arrest in infants (3). For infant resuscitation, the American Heart Association (AHA) recommends the delivery of high-quality chest compressions, which consist of a chest compression depth of at least one-third of the anterior–posterior diameter of the chest, or approximately 1.5 in (4 cm), a chest compression rate of 100–120 beats/min, and chest recoil for the establishment of return of spontaneous circulation (ROSC) (4, 5). An international pediatric resuscitation collaboration demonstrated that healthcare providers fail to meet the metrics of the AHA guidelines, with the greatest difficulty being in achieving chest compression depth targets in infants (6). Wolfe et al. demonstrated that deviations from the AHA guidelines during pediatric CPR are associated with decreased event survival (7). In the PICU, the rates of acute in-hospital cardiac arrest event survival (return of spontaneous circulation or return of circulation with extracorporeal support) are 78–90% and survival to discharge is 32–67%, with a favorable neurological outcome of 89–90% of survivors, as published in a recent multicenter observation study (8, 9). However, if quality CPR can be achieved, outcomes for pediatric IHCA could be improved.
Standard infant CPR techniques include the two-finger technique (TFT) for a single rescuer and the two thumb-encircling-hand thumb technique (TTT) for two rescuers (5). Chest compression techniques using fingers in infant CPR have been associated with inadequate compression depth and fatigue during CPR (5). Importantly, the reason for recommending compression with fingers in infant CPR is to reduce chest compression-related injuries, such as rib fractures or liver lacerations, in small infants (10–12). Since healthcare professionals provide inadequate chest compression depth and rate by standardized CPR techniques (13), there is a need for better techniques for effective infant CPR during pediatric cardiopulmonary arrest. We hypothesize that, by using the heel of the open palm [open palm technique (OPT)] rather than fingers for infant CPR, chest compression depth will increase.
2. Materials and methods
2.1. Study participants
This study has been approved by the appropriate ethical committees related to the institution, and subjects gave informed consent to participate. This approval was provided by the Institutional Review Board of the University of Iowa (IRB ID # 202005129). An email was sent to providers in the PICU (physicians, fellows, advanced practice providers, nurses, and respiratory therapists) describing the study and asking for participation. Subjects that responded to the email gave verbal consent prior to starting the study. Each participant was asked to perform three infant CPR techniques followed by a survey at the end of the study.
2.2. Study design
A standardized infant full-body resuscitation skills training manikin (Laerdal Medical Product Number 220-25050) was used. The manikin was placed on a standard hospital crib with a CPR board underneath in a PICU hospital room at the University of Iowa Stead Family Children's Hospital. Participants were allowed to use a step stool to adjust their height. Participants were encouraged to use their dominant hand to perform the study. Before starting the procedure, participants received instructions on using the novel OPT from a single investigator (SP). Participants were allowed to practice the new technique and receive feedback before starting the timed compressions. The Research Randomizer software (www.randomizer.org) was used to randomize the order of the CPR techniques. Each participant performed three techniques: TFT, TTT, and novel OPT. Each technique was performed for 2 min followed by a break of 5 min, and the process was repeated. The infant manikin was attached to ZOLL R series monitor/defibrillator via ZOLL training pads to collect the data (ZOLL Medical, Chelmsford, MA). ZOLL R-series defibrillator monitors displaying the chest compression depth and the chest compression rate were covered with a piece of paper. No CPR performance feedback or CPR coaches were provided during the study. The defibrillator monitor device is not calibrated to give audio feedback on compression depth or rate when using the pediatric pads, indicated for use on patients <25 kg.
2.3. Study variables and outcome
The primary outcomes for the study were chest compression depth (cm), chest compression rate (beats per minute) and chest compression fraction (%) for all three techniques. These data were recorded by the ZOLL defibrillator, downloaded to a card, and reviewed by ZOLL Rescue Net Code Review software. Data were collected for first and second minute of CPR for each technique. A survey was provided at the end of study to assess feasibility, specifically relating to the difficulty level, of the new technique. A study survey (Supplementary Figure 1) was provided at the end of the study to record age, sex, and number of years working in PICU, and the difficulty level (5-point Likert scale) for each technique (TTT, TFT, OPT).
2.4. Statistical analysis
Categorial data from the surveys are presented as raw numbers and frequencies. Continuous data from CPR performance are presented as mean and standard deviation. The three techniques were compared using generalized linear modeling. Data were divided into two time intervals: the first minute and the second minute. The median values for each time interval for the three techniques were compared using the Wilcoxon signed rank test for each minute. As this was a pilot study with no prior use of this technique, there was no sample size or power analysis. Data were analyzed using SAS software (Cary, NC). Values of a p-value of < 0.05 were considered significant.
3. Results
A total of 30 pediatric critical care providers from the University of Iowa Stead Family Children's Hospital Pediatric Intensive Care Unit participated in the study. The University of Iowa Stead Family Children's Hospital PICU is a 28-bed unit with pediatric medical-surgical and cardiac patients. The PICU has approximately 1,500 admissions annually and provides advanced therapies including VADs, ECMO, CRRT, and solid organ transplants. The baseline characteristics of the participants are shown in Table 1.
The results of the three infant CPR techniques compared in the study are shown in Table 2. Mean chest compression depth during the entire 2-min trial was significantly deeper using OPT compared to TFT. However, chest compression depth was similar for OPT and TTT. TTT showed deeper chest compression depth than TFT, though this was not significant. Chest compression rate and chest compression fraction did not show significant differences in the three techniques (Table 2).
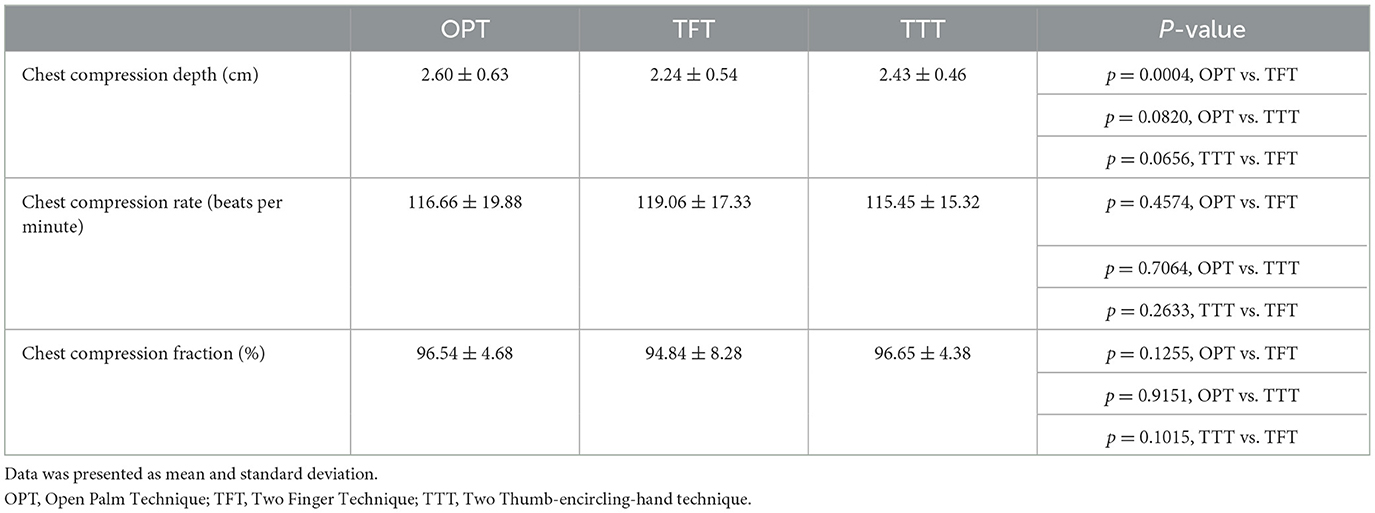
Table 2. Comparison of quality of 2-min mean chest compression depth, chest compression rate and chest compression fraction.
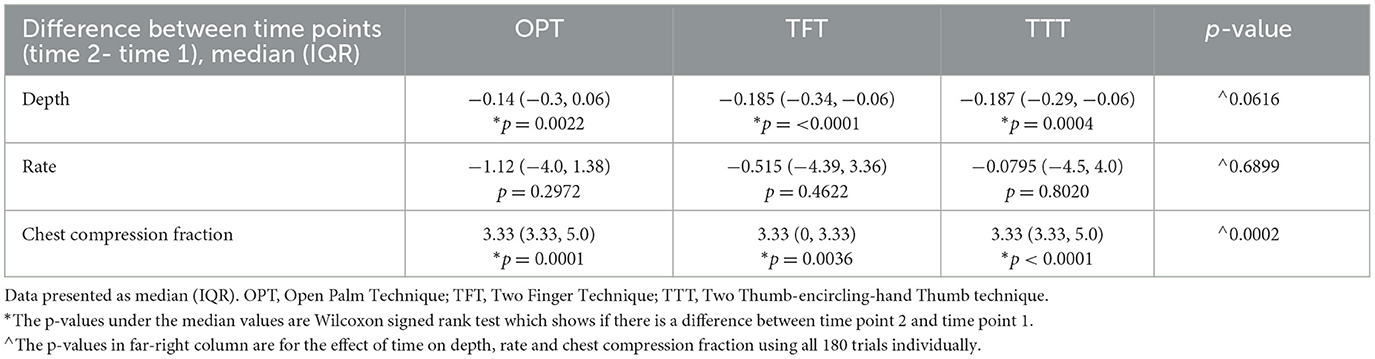
The chest compression depth was significantly better when OPT was used in the first minute (2.68 cm ± 0.65 cm) and the second minute (2.52 ± 0.61 cm). In comparison, TFT produced the lowest chest compression depth in the first minute (2.32 ± 0.51 cm) and second minute (2.17 ± 0.56 cm). Significant differences between time point 2 and time point 1 (2-min and 1-min, respectively) were observed for all three techniques individually (Table 3).
No significant differences were found among all three techniques for the mean chest compression rate and the chest compression fraction (Table 2). All rates were within the desired 100–120 bpm, and the chest compression fraction was >80%, as recommended by the AHA. The chest compression fraction was significantly higher in min 2 for all three techniques (Table 3).
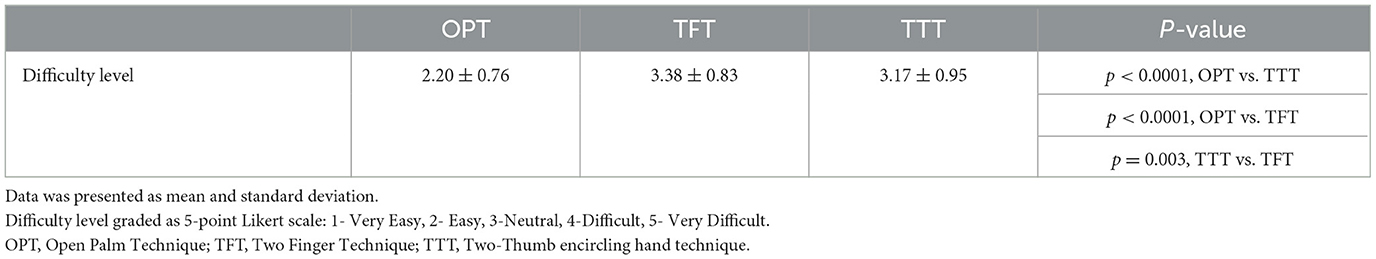
Participants completed a questionnaire at the end of the testing to assess the feasibility of this new technique by measuring the difficulty level compared to standard techniques. Figure 1 highlights the points on the Likert scale survey that were selected with the mean ± SD indicated by the bars. The OPT was graded as the easiest technique, followed by TTT (2.20 ± 0.76 vs. 3.17 ± 0.95, p < 0.0001) and then TFT (3.83 ± 0.83, p < 0.0001) (Table 4). Overall, the OPT was considered technically feasible as it was scored as the easiest technique in comparison to standard infant CPR techniques (TFT and TTT).

Figure 1. Survey results regarding difficulty level. The proportion of the shape highlights the frequency that number on the Likert scale was selected. The bar demonstrates the mean survey response and the standard deviation. OPT, open palm technique; TTT, two thumb-encircling hand technique; TFT, two-finger technique.
4. Discussion
To our knowledge, this is the first study demonstrating the use of one hand OPT for infant CPR. Our results showed a statistically significant increase in chest compression depth obtained with OPT compared to TFT. The OPT was rated as the easiest technique compared to standardized infant CPR techniques (TFT and TTT) by 30 experienced pediatric critical care providers, highlighting the feasibility of this new technique. All three techniques were able to achieve an optimal chest compression rate (100–120 beats/min) and a chest compression fraction (>80%) according to the AHA guidelines. No significant differences were found in chest compression fraction and chest compression rate.
High-quality CPR is the primary component influencing survival and neurodevelopmental outcomes after cardiac arrest in infants (3). The five components of high-quality CPR for infants are adequate chest compression rate (100–120 beats/min), adequate chest compression depth of at least one-third of the anterior–posterior diameter of the chest or approximately 1.5 in (4 cm), full chest recoil, minimized interruptions in chest compressions, and avoidance of excessive ventilation (14). The use of two standardized infant CPR techniques, TFT and TTT, has the limitations of inadequate chest compression depth, frequent interruptions, and rescuer fatigue due to the use of small hand muscles (5).
Studies comparing standardized infant CPR techniques indicate that TTT has a higher quality of chest compression and longer hand-off time compared to TFT but that the ratio of complete recoil is better with TFT than TTT (15–17). Another study involving 209 medical personnel and emergency workers who performed TFT and TTT on infant manikins could not achieve adequate chest compressions (18). In an international pediatric resuscitation collaboration, Niles et al. demonstrated that providers often do not meet the 2015 AHA guideline recommendations during the delivery of high-quality chest compressions. Compliance was poor for chest compression rate and depth in children, with the greatest difficulty in meeting chest compression targets in younger children (6). Similar observations have been noted during simulations. We were unable to achieve the targeted chest compression depth of 4 cm for infants, as recommended by the AHA guidelines with any of the three infant CPR techniques (OPT, TFT, or TTT).
Several other manikin studies have investigated alternate strategies for infant CPR including a new two-thumb technique with thumbs angles at 90°, a knocking finger technique, a flexed two-finger chest compression technique, and utilization of compression devices like plate-assisted pinch device or palm pressor (19–23). A significant benefit to the utilization of one hand OPT is the avoidance of small hand muscles (fingers and thumb) and the lack of need to carry or find a compression device. Multiple experienced pediatric critical care participants in our study commented on the ease of performing OPT (Figure 1). In a randomized study performed on manikins, a 1-min shift cycle group achieved better chest compression depth, chest compression rate, and chest recoil in comparison to a 2-min shift cycle group that experienced higher rescuer fatigue (24). In our study, the data was collected for the first minute and the second minute of CPR for each technique. Each technique had higher chest compression depth and chest compression rate for the first minute in comparison to the second minute as shown in Table 3. A randomized crossover adult study evaluating the quality of 2-min chest compression indicated optimal chest compression in the first 30 s of CPR in comparison to the last 30 s of 2-min chest compression (25). However, the use of a feedback device to sustain optimal chest compressions from the initial 30 s to the last 30 s of a 2-min chest compression was encouraged (25). No CPR feedback or verbal feedback was given during our study.
Standard infant CPR techniques, including TFT and TTT, are used for resuscitation in neonates with small chest diameter (5). However, TFT and TTT are also for infants with greater weights and wider chest diameter, posing several challenges. Both standard techniques rely on the use of small muscles, making the techniques prone to finger and provider fatigue (26). TFT uses fingers with different lengths, requiring more vertical force to achieve adequate chest compression leading to finger and rescuer fatigue (14). Lack of support of the elbow while performing TFT and TTT contributes to unsteadiness during CPR (18). The OPT was developed by considering the challenges faced by rescuers with fatigue, especially considering the size differences between neonates and larger infants. The OPT allows providers to apply pressure with the entire arm, constant contact, and better chest recoil, which is lacking in TFT and TTT, respectively (18). The OPT was considered the easiest of the three techniques. However, due to the limited one-time application of this technique, we were not able to assess the fatigue that would occur during multiple rounds of CPR.
Our study had several limitations. First, the use of a manikin model in a simulated study may not directly translate results to real infants. We recognized that chest compliance of humans may differ based on age, underlying diseases, and anatomic abnormalities, which is not the case for manikins. Second, the use of fingers for infant CPR was suggested to reduce chest compression–related injuries such as rib fractures or liver lacerations. However, our study could not assess the risk of chest compression injury with the use of OPT. It is also unknown how OPT might work in children with instrumentation such as a tracheostomy or pacemaker in place. Third, it is difficult to estimate whether the experience of pediatric critical care providers created a bias in achieving better chest compression depth, chest compression rate, and chest compression fraction or if bias was created during the pre-simulation practice session where providers learned this new technique. Finally, the study was performed as in-hospital CPR as participants performed continuous 2-min CPR without ventilation and no other interruptions or distractions. It is unknown how OPT may compare to standard techniques in a true code environment and when ventilation is utilized.
5. Conclusion
Our study evaluated the performance of a novel single-hand OPT for infant CPR. The rationale for this new technique was based on the inability of healthcare providers to achieve metrics set by the AHA guidelines through standardized infant CPR techniques. We found that providers using the OPT achieved deeper chest compression depth in comparison to TFT. Critical care providers found the technique easiest compared to the two standard techniques, thus indicating that this would be feasible as a new technique for infant CPR. However, we were unable to achieve the 4-cm chest compression depth goal set by the AHA guidelines with any of the three CPR techniques. Further research is needed to optimize CPR performance to achieve the targeted chest compression depth in infants.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study involving human participants was approved by the University of Iowa Institutional Review Board (IRB ID # 202005129). The participants provided verbal consent to participate in this study.
Author contributions
SP co-developed concept, performed simulations, collected data, and wrote initial draft and approved final version. SB, TE, and MR assisted with study design and methods, reviewed data, reviewed initial draft, and assisted with revisions and approved final version. EN reviewed data, reviewed initial draft, and assisted with revisions and approved final version. TC assisted with study design, reviewed data and performed analysis, reviewed initial draft, and assisted with revisions and approved final version. DA and SH co-developed concept, assisted with study design and methods, reviewed data, reviewed initial draft, and assisted with revisions and approved final version. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge ZOLL for their Investigator-Initiated Research Grant (Haskell 2020–03) and the providers in the University of Iowa Stead Family Children's Hospital Pediatric Intensive Care Unit for their participation.
Conflict of interest
DA and SH have participated in the writing groups for the AHA Pediatric Basic Life Support and Pediatric Advanced Life Support. DA also serves as the Chair of the Emergency Cardiovascular Care for the AHA.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/femer.2023.1235092/full#supplementary-material
References
1. Slonim AD, Patel KM, Ruttimann UE, Pollack MM. Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. (1997) 25:1951–5. doi: 10.1097/00003246-199712000-00008
2. Suominen P, Olkkola KT, Voipio V, Korpela R, Palo R, Räsänen J. Utstein style reporting of in-hospital paediatric cardiopulmonary resuscitation. Resuscitation. (2000) 45:17–25. doi: 10.1016/S0300-9572(00)00167-2
3. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the resuscitation outcomes consortium Epistry-Cardiac arrest. Circulation. (2009) 119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678
4. Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2015) 132:S414–435. doi: 10.1161/CIR.0000000000000259
5. Atkins DL, Berger S, Duff JP, Gonzales JC, Hunt EA, Joyner BL, et al. Part 11: pediatric basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2015) 132:S519–525. doi: 10.1161/CIR.0000000000000265
6. Niles DE, Duval-Arnould J, Skellett S, Knight L, Su F, Raymond TT, et al. Characterization of pediatric in-hospital cardiopulmonary resuscitation quality metrics across an international resuscitation collaborative. Pediatr Crit Care Med. (2018) 19:421–32. doi: 10.1097/PCC.0000000000001520
7. Wolfe HA, Morgan RW, Zhang B, Topjian AA, Fink EL, Berg RA, et al. Deviations from AHA guidelines during pediatric cardiopulmonary resuscitation are associated with decreased event survival. Resuscitation. (2020) 149:89–99. doi: 10.1016/j.resuscitation.2020.01.035
8. Berg RA, Nadkarni VM, Clark AE, Moler F, Meert K, Harrison RE, et al. Incidence and outcomes of cardiopulmonary resuscitation in PICUs. Crit Care Med. (2016) 44:798–808. doi: 10.1097/CCM.0000000000001484
9. Holmberg MJ, Wiberg S, Ross CE, Kleinman M, Hoeyer-Nielsen AK, Donnino MW, et al. Trends in survival after pediatric in-hospital cardiac arrest in the United States. Circulation. (2019) 140:1398–408. doi: 10.1161/CIRCULATIONAHA.119.041667
10. Bush CM, Jones JS, Cohle SD, Johnson H. Pediatric injuries from cardiopulmonary resuscitation. Ann Emerg Med. (1996) 28:40–4. doi: 10.1016/S0196-0644(96)70137-3
11. Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. (2004) 63:327–38. doi: 10.1016/j.resuscitation.2004.05.019
12. Thaler MM, Krause VW. Serious trauma in children after external cardiac massage. N Engl J Med. (1962) 267:500–1. doi: 10.1056/NEJM196209062671009
13. Martin PS, Kemp AM, Theobald PS, Maguire SA, Jones MD. Do chest compressions during simulated infant CPR comply with international recommendations? Arch Dis Child. (2013) 98:576–81. doi: 10.1136/archdischild-2012-302583
14. Chang CY, Lin PC, Chien YJ, Chen CS, Wu MY. Analysis of chest-compression depth and full recoil in two infant chest-compression techniques performed by a single rescuer: systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17:4018. doi: 10.3390/ijerph17114018
15. Udassi S, Udassi JP, Lamb MA, Theriaque DW, Shuster JJ, Zaritsky AL, et al. Two-thumb technique is superior to two-finger technique during lone rescuer infant manikin CPR. Resuscitation. (2010) 81:712–7. doi: 10.1016/j.resuscitation.2009.12.029
16. Lee SY, Hong JY, Oh JH, Son S-H. The superiority of the two-thumb over the two-finger technique for single-rescuer infant cardiopulmonary resuscitation. Eur J Emerg Med. (2018) 25:372–6. doi: 10.1097/MEJ.0000000000000461
17. Jo CH, Jung HS, Cho GC, Oh YJ. Over-the-head two-thumb encircling technique as an alternative to the two-finger technique in the in-hospital infant cardiac arrest setting: a randomised crossover simulation study. Emerg Med J. (2015) 32:703–7. doi: 10.1136/emermed-2014-203873
18. Whitelaw CC, Slywka B, Goldsmith LJ. Comparison of a two-finger versus two-thumb method for chest compressions by healthcare providers in an infant mechanical model. Resuscitation. (2000) 43:213–6. doi: 10.1016/S0300-9572(99)00145-8
19. Rodriguez-Ruiz E, Martínez-Puga A, Carballo-Fazanes A, Abelairas-Gómez C, Rodríguez-Nuñez A. Two new chest compression methods might challenge the standard in a simulated infant model. Eur J Pediatr. (2019) 178:1529–35. doi: 10.1007/s00431-019-03452-2
20. Jung WJ, Hwang SO, Kim HI, Cha YS, Kim OH, Kim H, et al. 'Knocking-fingers' chest compression technique in infant cardiac arrest: single-rescuer manikin study. Eur J Emerg Med. (2019) 26:261–5. doi: 10.1097/MEJ.0000000000000539
21. Yang D, Kim KH, Oh JH, Son S, Cho J, Seo KM. Development and evaluation of a New chest compression technique for cardiopulmonary resuscitation in infants. Pediatr Cardiol. (2019) 40:1217–23. doi: 10.1007/s00246-019-02135-x
22. Paek SH, Kim DK, Lee JH, Kwak YH. Comparison of standard and alternative methods for chest compressions in a single rescuer infant CPR: a prospective simulation study. PLoS ONE. (2019) 14:e0226632. doi: 10.1371/journal.pone.0226632
23. Park JW, Jung JY, Kim J, Kwak YH, Kim DK, Lee JC, et al. A novel infant chest compression assist device using a palm rather than fingers: a randomized crossover trial. Prehosp Emerg Care. (2019) 23:74–82. doi: 10.1080/10903127.2018.1471559
24. Heydari F, Eghdami K, Zamani M, Golshani K, Masoumi B. Evaluation of the effect of shift cycle time on chest compression quality during cardiopulmonary resuscitation. Tzu Chi Med J. (2021) 33:270–4. doi: 10.4103/tcmj.tcmj_228_20
25. Wu C, You J, Liu S, Ying L, Gao Y, Li Y, et al. Effect of a feedback system on the quality of 2-minute chest compression-only cardiopulmonary resuscitation: a randomized crossover simulation study. J Int Med Res. (2020) 48:300060519894440. doi: 10.1177/0300060519894440
Keywords: cardiopulmonary resuscitation (CPR), chest compression depth, infants, manikin, CPR technique
Citation: Patel S, Balikai S, Elgin TG, Newell EA, Colaizy TT, Raghavan ML, Atkins DL and Haskell SE (2023) One hand open palm technique for infant CPR. Front. Disaster Emerg. Med. 1:1235092. doi: 10.3389/femer.2023.1235092
Received: 05 June 2023; Accepted: 21 July 2023;
Published: 31 August 2023.
Edited by:
Ioannis Pantazopoulos, University of Thessaly, GreeceReviewed by:
Csaba Dioszeghy, Surrey and Sussex Healthcare NHS Trust, United KingdomAnthony Lagina, Wayne State University, United States
Copyright © 2023 Patel, Balikai, Elgin, Newell, Colaizy, Raghavan, Atkins and Haskell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah E. Haskell, c2FyYWgtaGFza2VsbEB1aW93YS5lZHU=
 Shruti Patel1
Shruti Patel1 Timothy G. Elgin
Timothy G. Elgin Tarah T. Colaizy
Tarah T. Colaizy Sarah E. Haskell
Sarah E. Haskell