
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Disaster Emerg. Med. , 10 August 2023
Sec. Resuscitation and Cardiac Emergency Medicine
Volume 1 - 2023 | https://doi.org/10.3389/femer.2023.1231318
Objective: This study aimed to describe total pre-hospital delays (symptom onset to admission), patient delays (symptom onset to calling for help), and transport delays (calling for help to admission) experienced by patients with acute coronary syndrome (ACS) in Russia and identify factors associated with longer delays.
Methods: A prospective observational cohort study of ACS patients with myocardial infarction recruited in hospitals providing percutaneous coronary intervention (PCI) and those that do not (non-PCI) in 13 regions and at multiple levels of the health system in Russia. Data were collected on pre-hospital delays between symptom onset and admission to the hospital providing definitive treatment, divided into patient delay (time between symptom onset and calling for help) and transport delay (time between calling for help and admission).
Results: Of 902 patients, 701 (77.7%) had full data on pre-hospital delays. The median total pre-hospital delay in our study was 5.1 h, the median patient delay was 1.5 h, and the median transport delay was 2.1 h. Patient delays did not differ by age and sex, although having an ST-elevation myocardial infarction (STEMI) and certain symptom presentations, including severe pain, reduced delays. Transport delays were markedly reduced in those transported by emergency medical services (EMS) and taken directly to the hospital of definitive treatment (rather than to one closer but unable to offer PCI).
Although transport delays were reduced in those using EMS, just half of the patients using EMS had a transport delay of <2 h (first medical contact to admission). Among all patients taken directly to the hospital by EMS, 70% were STEMI patients. Of these STEMI patients, 78% had a transport delay of 2 h or more. Among these patients, only 16.0% received thrombolysis in the ambulance. As expected, regional differences were apparent with all types of delay, with the greatest variation found in transport delays.
Conclusion: Delays are currently longer than the European Society of Cardiology guidelines for STEMI patients and other severe cases. Reducing patient delays will reduce overall delays. Transport delays are inevitable in many regions of Russia, but better triage of patients, increased use of EMS, and early thrombolysis in EMS, particularly for STEMI patients facing excessive transport delays, will reduce delays and buy time before PCI.
Thrombolysis and percutaneous coronary intervention (PCI) have transformed the management of acute coronary syndrome (ACS), but to be effective, they must be undertaken rapidly after the onset of symptoms. The 2017 European Society of Cardiology (ESC) guidelines recommend primary PCI for those with ST-elevation myocardial infarction (STEMI) if it can be performed within 120 min of first medical contact; otherwise, thrombolysis is recommended (1). PCI is only recommended for very-high-risk non-STEMI patients but can be considered for others within 24 h of symptom onset (2).
The guidelines distinguish components of total ischaemic time, defined as the delay between symptom onset and procedure/reperfusion. Patient delay (PD) is defined as the delay between symptom onset and seeking help; system delay is divided into emergency medical services (EMS)/transport delays (TDs) and facility delays. PD is often the longest and most difficult to influence (3), more likely because of atypical symptoms or a failure to recognize the importance of the symptoms (4). TDs, between calling for help and admission to the hospital of definitive treatment, reflect the distance and performance of EMS. Facility delays reflect organizational factors, such as the availability of a 24-h service (1).
The Russian Federation has invested heavily in PCI services (5). However, its geography creates challenges (6), which is of concern given the high death rates from cardiovascular disease in Russia (7). This calls for an improved understanding of the delays involved and whom they affect. So far, there is little information about pre-hospital delays (PHDs) in Russia except for a few ACS registries; only one reports the median time from symptom onset until first contact as 3.4 h, and from first medical contact to hospitalization as 1.5 h (8). Published research internationally tends to focus on delays in hospitals rather than before arrival, with several studies from the first decade of the twentyfirst century reporting delays between symptom onset and arrival at a facility as 100 to 120 min, with a subsequent delay to fibrinolysis was ~30 min and to PCI ~90 min (9, 10).
We report data from hospitals across Russia in a study that included assessing the components of PHDs.
The study is set in the Russian Federation. The Russian health system is funded, primarily, by a system of compulsory health insurance, supplemented by government funding (11), and covers almost everyone (12). It faces particular geographical challenges arising from the low population density in many regions (6). Care is delivered in a mix of public and private facilities. The Russian government has made major investments in health infrastructure, the workforce, and quality improvement programmes (13). The treatment of myocardial infarctions (MIs) is generally managed according to the ESC guidelines (14).
The Acute Myocardial Infarction in Russia study enrolled patients admitted to 16 hospitals (rural, city, and federal) across 13 Russian regions, some providing primary PCI and others not, as was part of the International Project of Cardiovascular Disease in Russia. Further details, including hospital locations and the rationale for selection, are published elsewhere (15). The facilities were a convenience sample, reflecting the need to ensure a commitment by a local clinician. While this precluded a fully representative sample, we specifically included some small facilities and were able to ensure that the facilities included spanned the entire range when ranked by penetration of advanced technology. In brief, over 14 months (2015–2016), patients admitted to these facilities were selected based on the temporal proximity of admission to a set of randomly generated dates and times to avoid selection bias. Patients were eligible if between 18 and 75 years of age, hospitalized with ACS, and survived for 24 h following admission to enable informed consent. Each participant underwent a baseline interview, with follow-up interviews at 6 and 12 months. Treatment details were abstracted from medical records.
We measured total PHDs between symptom onset and admission to the hospital providing definitive treatment (rather than one closer but unable to offer PCI), divided into PD (time between symptom onset and calling for help) and TD (time between calling for help and admission).
Total PHDs were divided into <2 h (shorter) and ≥2 h (longer); for PD and TD, the divisions of each were at <1 h (shorter) and ≥1 h (longer). These cut-offs reflect ESC recommendations for PHDs for STEMI patients, who require the most rapid treatment (1).
Data on patient characteristics, previous medical history, symptom presentation, pre-hospital behaviors, and admission characteristics are derived from the baseline patient questionnaire and hospital records at admission. Only one region, with a very sparse population (Khanty-Mansiysk), uses air ambulances systematically. Whilst we were unable to distinguish road and air ambulance transportation in the data, the overall use of air ambulances is low in all regions.
Delay indicators (PHD, PD, and TD) were described in hours, using the median and the interquartile range (IQR), and as shorter (PD, TD: <1 h; PHD: <2 h) or longer, using number (n) and proportion (%).
Continuous delays experienced by different groups were compared using the Mann–Whitney U test, as no delay data were normally distributed according to the Shapiro–Wilk test (p < 0.05). Categorical delay times were compared using the χ2 test, with Fisher's exact test as appropriate. Multivariable binary logistic regression models were used for all delay indicators, and independent variables were found to have a significant relationship in bivariate analyses. Age (≥ or <the median age of 60) and sex were included in base models, with distance added subsequently. Thrombolytic treatment (TLT), PCI timing, and the use and days in hospital were reported by categories of delay; TLT administration by EMS was also described.
All analyses were performed using complete cases. Data from three hospitals were excluded due to high proportions of missing data on delay indicators (Kazan and Saratov) and implausible delay times (Bryansk). All analyses were conducted using Stata 15 (16).
Among the 13 hospitals included in the analysis, 701 of 902 (77.7%) patients had complete data on PHDs. Of the 701, 4 died and 15 received no reperfusion treatment due to a prolonged PHD.
Table 1 reports the key characteristics of delays in hours. Of the patients in the sample, 93.3% were admitted to PCI hospitals, 76.7% were male, the median age was 60 years, 74.0% had STEMI, and 68.9% of patients arrived directly by ambulance, with 23.7% transferred from a non-PCI hospital and <5% coming by other routes.
Overall, most patients experienced PHDs longer than ESC recommendations, with 86.5% having a total PHD of <2 h (longer, n = 606); only 13.6 % (n = 95) of all patients arrived at the hospital within 2 h of symptom onset. The median PHD was 5.1 h (IQR 2.8–12.2) and <2 h in all hospitals regardless of whether the hospital was PCI-capable or not. There was considerable variation in median PHD across hospitals from 3.3 h (Arkhangelsk) to 11.6 h (Tver regional hospital; Table 2).
The median PD was 1.5 h (IQR 0.5–5.0). Overall, 38.0% of patients sought help within 1 h of symptom onset (n = 266). The PD median delay ranged from 0.5 h (Tver regional hospital) to 4.0 h (Tver non-PCI hospital), with admissions to four hospitals having a median PD of ≤ 1 h.
The median TD was 2.1 h (IQR 1.3–5.0), and 14.3% of patients had a transport time of <1 h after calling for help (n = 100). The median TD ranged from 1.2 h (Barnaul) to 8.5 h (Tver regional hospital) and was <1 h in all hospitals (Table 2).
Most patients eventually called EMS (87.0%, n = 610). Of those, 77.1% (470) were taken directly to the hospital by ambulance. Overall, 68.9% of patients were taken directly by ambulance to the hospital (n = 483), and 13 did not report calling EMS. Among patients being taken to the hospital directly by ambulance, the median TD was 1.7 h (IQR 1.1–2.5), and 18.9% had a PHD of <2 h. Among all other patients, the median TD was 7.1 h (IQR 3.7–15.8), of whom only 1.8% had an overall PHD of <2 h (p < 0.001). Most patients who did not call EMS and were not taken directly to the hospital were transferred from other medical facilities (including polyclinics and no-PCI hospitals); only nine people self-presented.
In the bivariate analyses, neither age nor socio-economic characteristics were associated with any type of delay. However, as expected, distance was a major determinant of overall delay. Few patients who traveled ≥40 km to the hospital were admitted within 2 h. Half of the patients were within 10 km of the hospital at the time of symptom onset. The further a patient was from the hospital at the time of symptom onset, the greater the proportion with a longer TD (Table 3). There were significant sex differences; women were more likely to have shorter TDs than men. However, men were more likely to be ≥40 km from the hospital at symptom onset; no sex difference exists when controlling for distance.
Of the 87.0% of patients who called EMS, 76.4% subsequently traveled by ambulance, although this varied considerably according to the hospital of admission, ranging from 28.6% to 100% (Table 1 in Supplementary Material 1).
EMS performance varied among levels of hospitals; most patients in city hospitals who called EMS subsequently traveled by ambulance (99%; Table 2 in Supplementary Material 1). Only 69.1 % of patients attending federal hospitals and 73.7% of patients attending regional hospitals did so. This reflects the many transfers from non-PCI hospitals (28.7% and 25.3%, respectively). Among patients who arrived at the treating hospital directly by ambulance, TD did not differ by level of hospital (Table 2 in Supplementary Material 1).
MI type was associated with differences in PD. Among all patients, 74.0% had STEMIs (n = 519). The median PD time was significantly shorter for STEMI patients, being less than half that of other patients (1.1 h vs. 2.4 hrs, p < 0.001). A greater proportion of STEMI patients had a shorter PD (<1 h) than other ACS patients (p = 0.002). The median TD did not differ by MI type.
Overall, 37.9% of patients had a shorter PD (<1 h). PD was not associated with chest pain but was associated with weakness and self-described severe pain. Of patients reporting severe pain, 43.8% had a short PD, compared to 31.5% of patients who did not have severe pain (p = 0.001). Of those reporting weakness, 42.9% had a short PD compared to 34.7% of people who did not experience weakness (p = 0.029). We found no other significant differences in short PD by specific symptoms.
Prior MI, angina, or co-morbidity were not associated with PD or TD. Patients who had diabetes (15.1%, n = 106) were less likely to have a shorter PD, although not significantly so (30.2% vs. 39.3%, p.074).
There was some evidence that the effect of diabetes on delays varied by MI type. Only 20.6% of non-STEMI patients with diabetes had a short PD, compared to 34.7% of STEMI patients with diabetes, 30.4% of non-STEMI patients with no diabetes, and 42.3% of STEMI patients with no diabetes (p = 0.008, Table 3 in Supplementary Material 1).
Detailed information on presenting symptoms by patient characteristics is available in Supplementary Material 2. Male patients were more likely to report chest pain, severe pain, and breathlessness and less likely to report indigestion and nausea than women. Few significant differences in symptom presentation by age and MI type exist; STEMI patients reported weakness more than other ACS patients, and older patients reported palpitations more than younger patients. STEMI patients reported higher rates of nausea, palpitations, sweating, severe pain, and radiating chest pain than other ACS patients, although these differences were not significant. Diabetic patients presented with different symptoms and were less likely to report pain (severe pain, jaw pain, radiating chest pain). Diabetic patients reporting no pain prolonged calling for help compared to those that did experience pain (p = 0.004).
Presenting symptoms were not significantly associated with PD, save for some exceptions. Severe pain increased the likelihood of a shorter PD. Patients reporting chest pain were more likely to call EMS. This difference was not significant; however, nearly all patients reported chest pain (92.9%; Table 4). Of patients with chest pain, 37.5% had a PD ≥1 h compared to 44.0% of patients not reporting chest pain. The majority of patients reporting radiating chest pain (83.3%, n = 240) called EMS, although they were less likely to call EMS than other patients (Adj. OR 0.62, 95% CI [0.39, 0.97], Table 4). Among patients not reporting chest pain (n = 50), a bivariate analysis showed that weakness was associated with a significantly shorter PD; 59.1% of those experiencing weakness had a short PD compared to 40.9% of those without (p = 0.015). No other symptoms were associated with shorter PD among this subgroup, although a greater proportion of those with severe pain and breathlessness called for help earlier. Of all patients, 56.8% reported excessive sweating, which increased the odds of calling EMS (Adj. OR 1.86, 95% CI [1.19, 2.92]). These results were consistent in both the unadjusted and adjusted models (Table 4). There were no significant differences in PD by the time of symptom onset, and there were fewer early callers when symptoms started during the night (Table 5). No significant differences in TD due to time of day existed, overall or among patients traveling by ambulance. However, EMS callers seemed to face slightly longer transportation times during the day, possibly due to ambulance availability and traffic. We found no seasonal difference.
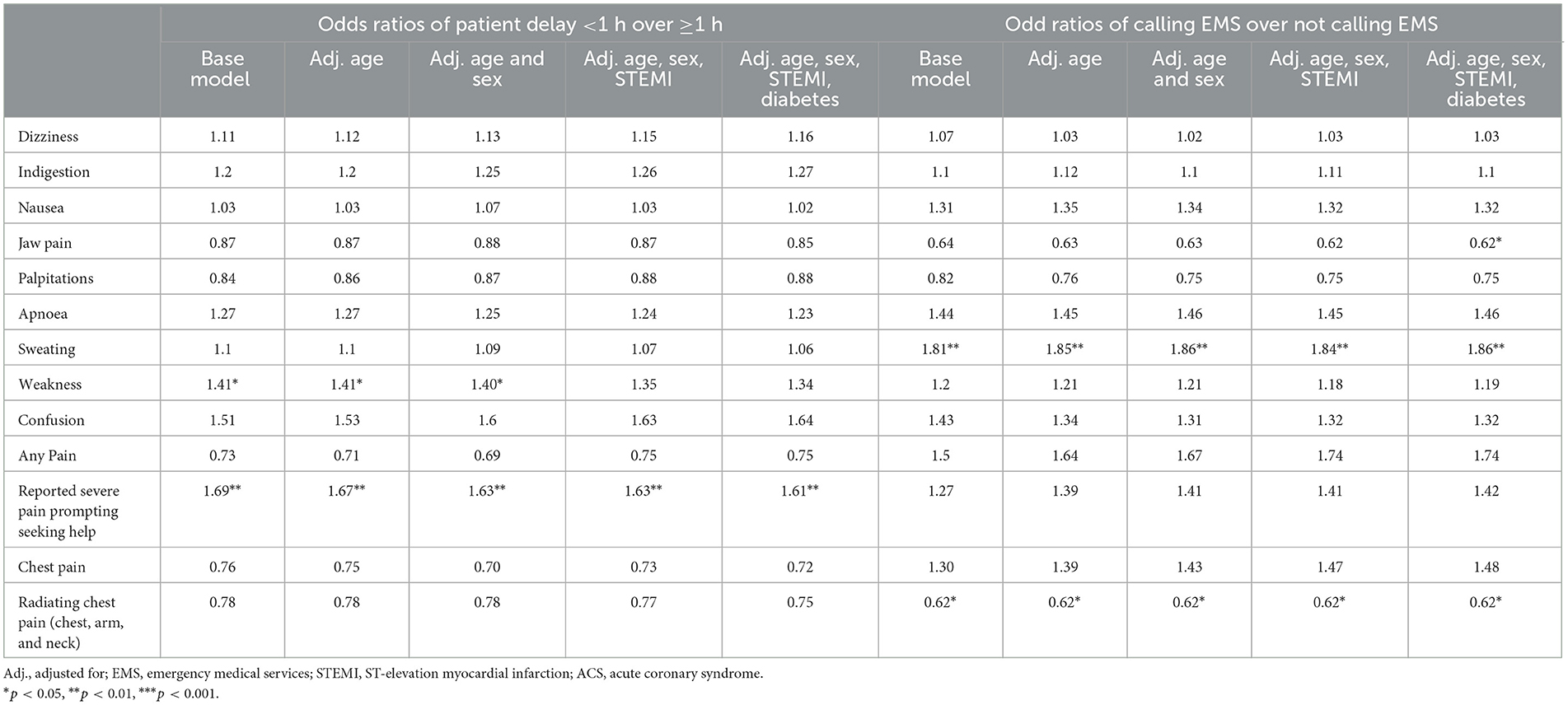
Table 4. Unadjusted and adjusted odds ratios for patient delay of <1 h and calling EMS by individual symptom.
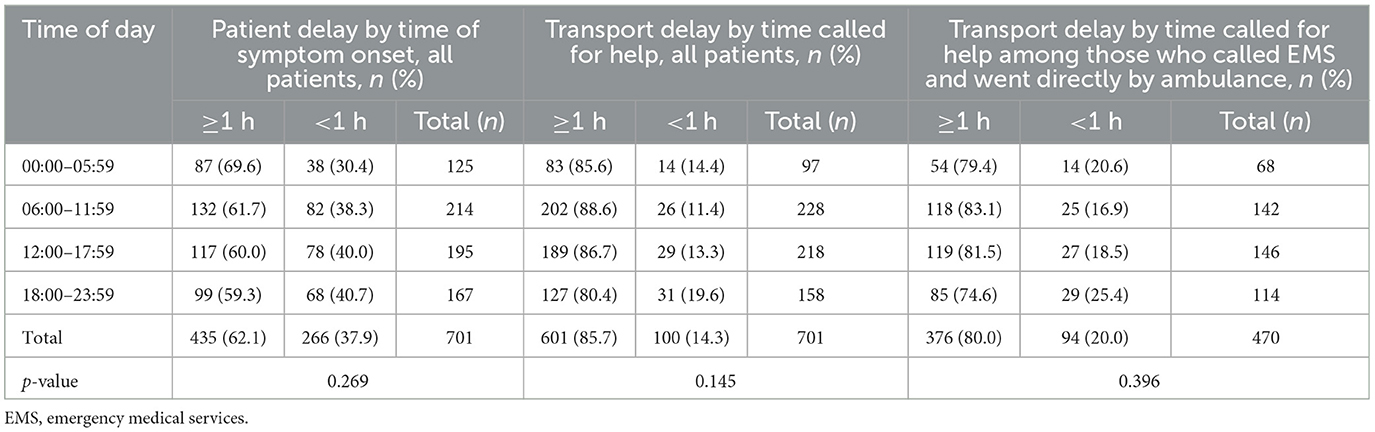
Table 5. Patient delay by time of day of symptom onset; transport delay by time of day called for help.
TLT is indicated for patients unlikely to receive timely PCI intervention. More than 90% (n = 439) of all patients traveling directly via EMS had a pre-hospital electrocardiogram (ECG). Among these patients, 315 were STEMI patients—of which 51 (16.2%) received TLT in the ambulance. Overall, 66.4% of patients receiving a STEMI diagnosis pre-hospital arrival had a TD of <2 h, and one-fifth had a TD of <1 h. A greater proportion of those receiving TLT in the ambulance arrived ≥2 h (n = 25/51, 49.2%) compared to those who did not (n = 81/264, 30.7%, p = 0.011). Five patients with no pre-hospital ECG reported receiving TLT from EMS.
Over a fifth of patients calling EMS were not taken directly to their hospital of definitive treatment (21.2%, n = 140). Most went to non-PCI hospitals with a later transfer to a PCI hospital (129/144, 92.1%). TLT administration was known for 123 patients (90.2% were STEMI patients), none had TLT prior to the non-PCI hospital, and 68 had TLT prior to admission to the subsequent PCI hospital.
The majority of patients admitted to PCI hospitals received a PCI (84.7%), and there was no significant difference in the odds of having a PCI by a shorter PHD, controlling for STEMI status (OR 0.90, 95% [CI 0.49, 1.64]) or by PD or TD. Among the 430 STEMI patients admitted to PCI hospitals, the time to PCI was available for 400. There was no significant difference between those arriving earlier (median 0.8 h) and those arriving later (median 1.0 h).
Regardless of PHD being <2 h or not, the median days in hospital were the same (11 days). The Killip class was available for 667 patients, 14% (n = 96) of whom had a Killip class of II or above. The median days in hospital did not differ significantly between Killip class I or II and above (11 vs. 12 days, p = 0.320). The duration of stay in hospitals at different levels of the health system varied significantly (p < 0.001); the longest median stay was in facilities not providing PCI (14 days, range 2–18), with federal hospitals having a median of 11 days (range 6–23); regional hospitals, 11 days (range 2–32); and city hospitals, 12 days (range 6–51).
To our knowledge, this is the largest and most detailed study of PHDs experienced by patients with ACS in Russia. It is purposefully descriptive in design to capture the continuity of ACS care in diverse regions of Russia and at multiple levels of the health system, thereby moving beyond large, unrepresentative centers of population in this vast country.
The EMS system in Russia is based on a general principle of reaching a patient within 20 min of a call to EMS. There are general EMS teams served both by paramedics and physicians and specialist teams that include cardiology. If an MI is suspected during the call, the cardiology EMS will be sent, or if a specialized cardiology EMS is not available, a physician-lead EMS will be sent. It is challenging to compare what we have found in this study of 13 diverse Russian hospitals with the findings in other countries as the Russian context is not typical of many industrialized countries. Issues that arise in densely populated urban settings are very different from those in sparsely populated rural ones, while advances in care make comparisons with earlier periods problematic. Furthermore, most studies have focused on delays in hospitals rather than on delays prior to arrival. However, one international study, including hospitals across four continents in the early 2000s, offers some insights, although it does not report countries separately. The delay between symptom onset and arrival was ~100 to 120 min, and the subsequent delay to fibrinolysis was ~30 min and to PCI ~90 min (9). A larger study of 21 European countries (including Russia), undertaken at the end of the 2000s, obtained similar results, although, again, the data were not broken down by country (10).
PHDs in Russia are comparable to a 2016 retrospective study in Sweden (also 5.1 h), which excluded patients who died, although this study was limited to those presenting with a first MI only (17). It found a PD of 3.1 h, twice that of Russia (1.5 h), whilst the median TD in Sweden was nearly half that of Russia (1.2 h compared to 2.1 h) (17).
Data from registries in Russia suggest that PHDs in Russia are declining. Our study included a purposively sampled selection of hospitals at different levels of the health system, so it cannot be regarded as providing a representative sample of Russian facilities. The PDs we found were shorter than the few reports from registry-based studies in Russia (18), but the total PHDs were longer (19).
In most countries, PDs constitute the largest proportion of PHDs and are considered to be the hardest element to influence. Whilst more than 56% of our patients have longer TDs than PDs, this could be due to our study design, which sought to capture the diverse characteristics of PCI and non-PCI hospitals across Russia. However, over two-thirds of our sample waited more than 60 min to seek help after symptom onset, with no systematic differences by age or sex. Evidence on the role of sex from other studies is conflicting (19–23). Education, wealth, or health insurance status were not found to make a difference; however, the type of MI and the presenting symptoms were associated with delays.
STEMI patients were more likely to seek help earlier, consistent with other studies (24–26). This may reflect differences in pathogenesis and associated symptoms (24). Whilst we found no clear difference in symptom presentation between STEMI patients and other ACS patients except “weakness,” STEMI patients were less likely to have co-morbidities or a history of previous symptoms. This could suggest that it is “unusual” symptoms that are associated with shorter delays, although we are unable to explore this further with our data and we lack data on symptom severity. Additionally, in line with some other studies (27, 28), diabetic patients experienced extended PDs. Those with diabetes are at higher risk of MI (29). Differences in pain perception and attribution of symptoms to their disease could play a role (30). Of diabetic patients not reporting pain, 80% waited over an hour to call for help. Finally, patients who reported thinking that their symptoms were heart-related reported significantly shorter PDs, but this could reflect hindsight bias.
The lack of systematic differences in PD with different risk factors (age, sex, and co-morbidity), and, in particular, prior MI, unlike in other studies (4), suggests a concerning lack of information about MI among those at greatest risk. However, survivor bias may be influencing results. In addition, whilst nearly all patients in our sample reported chest pain, men were more likely to report chest pain than women, even when controlling for age (women in our sample were older) and MI type; this is in line with studies that find that the typical symptom presentation is different in women and men (31, 32).
Timely access to reperfusion treatment for STEMI patients is vital to maximize success. We have previously shown that most STEMI patients in Russia are treated early in their infarction (14), but the median TDs in our study were 2.2 h, with 85.2% of STEMI patients (n = 442/519) having a TD of ≥1 h and 52.8% (370/701) having a TD of ≥2 h, outside the ESC recommendations. ESC guidelines recommend PCI within 2 h following first contact with the health system for STEMI patients, where no TLT is administered. In our sample, 49.1% of STEMI patients who called EMS arrived within 2 h. Among the 231 who did not arrive within 2 h, 49.8% were taken directly by ambulance (n = 115); of these, only 21.7% received TLT (n = 25).
Most patients called EMS and traveled directly to the hospital; doing so markedly increased the probability of arriving within 2 h, even allowing for distance. Extended delays among a quarter of all MI patients transferred from non-PCI hospitals suggest prolonged door-in to door-out times, although we could not assess the reasons why. This calls for further investigation, including exploring the potential for earlier fibrinolysis and reinforcing earlier calls for agreed-on guidelines on transfers (33). This has become even more important in the light of a recent French study showing worse outcomes among those arriving indirectly at facilities offering PCIs (34).
The geography of Russia means that, in many regions with dispersed populations, road transport will never be able to meet ESC guidance. Consequently, we recommend measures that will increase access to thrombolysis during EMS transport. This seems the most realistic strategy for MI patients, given that it is opposed to focusing on improving largely intractable TDs in Russia, as it buys time before PCIs. It will be facilitated by the recent expansion of air ambulance services in Russia, following pilot projects in eight regions in 2013–2015, something that is the only option in regions with very sparse populations scattered over large distances and with few roads. Interventions to increase awareness of seeking care for certain symptoms as a means of reducing delay have been disappointing (35), but looking ahead, there may be potential for innovative app-based approaches (36).
Our study has some limitations. Patients who survived <24 h after admission were excluded as the primary purpose was to understand the management of MI and subsequent secondary prevention. As we only include patients who made contact with the health system following ACS symptoms, there may be survivor bias, in particular where patients with particularly severe MIs died before engaging with the health system or did not survive for 24 h after admission. Additionally, the quality of information provided by patients when interviewed may be associated with the severity of their clinical condition at baseline interview, potentially introducing recall bias regarding information other than the objective clinical information recorded in medical records.
Despite recent investments in PCI capacity in Russian hospitals, many patients, including STEMI patients, continue to experience delays longer than the ESC guidelines. Whilst the geography of Russia precludes meeting the ESC guidelines in some regions, for those regions that can, there remains some way to go.
Whilst most patients called EMS, if more did so immediately after symptom onset, regardless of the time of day, delays could be reduced. Too many patients reach PCI hospitals indirectly, via polyclinics or non-PCI hospitals, another problem that could be addressed with improved triage. Finally, our study provides further support for early thrombolysis when STEMI patients face excessive TDs.
The datasets presented in this article are not readily available because applications for data from this study will be considered by the IPCDR steering group. Requests to access the datasets should be directed to DL, ZGF2aWQubGVvbkBsc2h0bS5hYy51aw==.
This main study and the pilot study was approved by the Ethics Committees at the National Research Institute for Preventive Medicine, Moscow, Russia (approval number 01-04/15 dated 03.02.2015) and at the London School of Hygiene & Tropical Medicine, London, UK (approval number 9993 dated 1 June 2015). All study participants signed informed consent to participate in the study, to grant the access to medical history and other medical documentation and to be contacted at 6 and 12 months after hospitalization. The patients/participants provided their written informed consent to participate in this study.
MM, HS, AK, DL, and KB conceptualised the research article. AK and NB oversaw the data collection. KB cleaned, managed, and analysed the data. KB, MM, HS, DL, and AK interpreted the results. KB prepared the first draft. MM, HS, DL, and AK provided the critical revisions of the article. All the authors approved the final version of the article to be published.
This study was conducted as part of the International Project on Cardiovascular Disease in Russia (IPCDR). IPCDR is supported by the Wellcome Trust [100217/Z/12], the Norwegian Ministry of Health, the Norwegian Institute of Public Health, and UiT, the Arctic University of Norway. DL's contribution was partially supported by the Basic Research Program of the National Research University Higher School of Economics. KB has been supported by a FWF Austrian Science Fund Lise Meitner Award [M-3069-B].
The authors would like to acknowledge the participants and personnel of the Acute Myocardial Infarction in Russia study for their contributions in terms of time and effort.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/femer.2023.1231318/full#supplementary-material
1. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2017) 39:119–77. doi: 10.1093/eurheartj/ehx393
2. Collet J-P, Thiele H, Barbato E. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2020) 20:92. doi: 10.1093/eurheartj/ehaa909
3. Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted H-H, Trautner S, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. Jama. (2010) 304:763–71. doi: 10.1001/jama.2010.1139
4. Nielsen CG, Laut KG, Jensen LO, Ravkilde J, Terkelsen CJ, Kristensen SD. Patient delay in patients with ST-elevation myocardial infarction: time patterns and predictors for a prolonged delay. Euro Heart J Acute Cardiovascul Care. (2017) 6:583–91. doi: 10.1177/2048872616676570
5. Kontsevaya A, Sabgaida T, Ivanova A, Leon DA, McKee M. How has the management of acute coronary syndrome changed in the Russian Federation during the last 10 years? Health Policy. (2017) 121:1274–9. doi: 10.1016/j.healthpol.2017.09.018
6. Timonin S, Kontsevaya A, McKee M, Leon DA. Reducing geographic inequalities in access times for acute treatment of myocardial infarction in a large country: the example of Russia. Int J Epidemiol. (2018) 47:1594–602. doi: 10.1093/ije/dyy146
7. World Health Organization. Global Health Observatory data respository—Total NCD Mortality Data by country (2018).
8. Erlikh A, Gratsiansky N. Registry of Acute Coronary Syndromes ≪RECORD-3≫. characteristics of patients and treatment during initial hospitalization. Kardiologiia. (2016) 4:16–24. doi: 10.18565/cardio.2016.4.16-24
9. Spencer FA, Montalescot G, Fox KAA, Goodman SG, Granger CB, Goldberg RJ, et al. Delay to reperfusion in patients with acute myocardial infarction presenting to acute care hospitals: an international perspective. Eur Heart J. (2010) 31:1328–36. doi: 10.1093/eurheartj/ehq057
10. Schiele F, Hochadel M, Tubaro M, Meneveau N, Wojakowski W, Gierlotka M, et al. Reperfusion strategy in Europe: temporal trends in performance measures for reperfusion therapy in ST-elevation myocardial infarction. Eur Heart J. (2010) 31:2614–24. doi: 10.1093/eurheartj/ehq305
11. Popovich L, Potapchik E, Shishkin S, Richardson E, Vacroux A, Mathivet B. Russian federation: health system review. Health Syst Transit. (2011) 13:1–190.
12. Perlman F, Balabanova D, McKee M. An analysis of trends and determinants of health insurance and healthcare utilisation in the Russian population between 2000 and 2004: the 'inverse care law' in action. BMC Health Serv Res. (2009) 9:68. doi: 10.1186/1472-6963-9-68
13. Vlassov VV, Bates K, McKee M. Quality improvement in hospitals in the Russian Federation, 2000-2016: a systematic review. Health Econ Policy Law. (2020) 15:403–13. doi: 10.1017/S1744133119000252
14. Kontsevaya AV, Bates K, Schirmer H, Bobrova N, Leon D, McKee M. Management of patients with acute ST-segment elevation myocardial infarction in Russian hospitals adheres to international guidelines. Open Heart. (2020) 7:e001134. doi: 10.1136/openhrt-2019-001134
15. Kontsevaya A, Bobrova N, Barbarash O, Duplyakov D, Efanov A, Galyavich A, et al. The management of acute myocardial infarction in the Russian Federation: protocol for a study of patient pathways. Wellcome Open Res. (2017) 2:89. doi: 10.12688/wellcomeopenres.12478.1
17. Nilsson G, Mooe T, Söderström L, Samuelsson E. Pre-hospital delay in patients with first time myocardial infarction: an observational study in a northern Swedish population. BMC Cardiovascul Disord. (2016) 16:93. doi: 10.1186/s12872-016-0271-x
18. Sagaydak OV, OschepkovaEV PY, Kiselev AR, Konosova ID, Gridnev VI. Approaches to optimization of ACS patients care timing characteristics in Federal ACS Registry system and Russian ministry of health monitoring system. Kardiologicheskii vestnik. (2017) 12:82–7.
19. Kontsevaya AV, Kononets EN, Goryachkin EA. Delayed help-seeking for emergency medical care of patients with acute coronary syndrome/myocardial infarction: review of studies. Russian J Cardiol. (2019) 8:132–9. doi: 10.15829/1560-4071-2019-8-132-139
20. Ladwig K-H, Fang X, Wolf K, Hoschar S, Albarqouni L, Ronel J, et al. Comparison of delay times between symptom onset of an acute st-elevation myocardial infarction and hospital arrival in men and women <65 years versus ≥65 years of age.: findings from the multicenter munich examination of delay in patients experiencing acute myocardial infarction (MEDEA) study. Am J Cardiol. (2017) 120:2128–34. doi: 10.1016/j.amjcard.2017.09.005
21. Poorhosseini H, Saadat M, Salarifar M, Mortazavi SH, Geraiely B. Pre-hospital delay and its contributing factors in patients with st-elevation myocardial infarction; a cross sectional study. Arch Acad Emerg Med. (2019) 7:e29.
22. Rivero F, Bastante T, Cuesta J, Benedicto A, Salamanca J, Restrepo J-A, et al. Factors associated with delays in seeking medical attention in patients with st-segment elevation acute coronary syndrome. Rev Esp Cardiol (Engl Ed). (2016) 69:279–85. doi: 10.1016/j.rec.2015.07.029
23. Sederholm Lawesson S, Isaksson R-M, Ericsson M, Ängerud K, Thylén I. Gender disparities in first medical contact and delay in ST-elevation myocardial infarction: a prospective multicentre Swedish survey study. BMJ Open. (2018) 8:e020211. doi: 10.1136/bmjopen-2017-020211
24. McKee G, Mooney M, O'Donnell S, O'Brien F, Biddle MJ, Moser DK. Multivariate analysis of predictors of pre-hospital delay in acute coronary syndrome. Int J Cardiol. (2013) 168:2706–13. doi: 10.1016/j.ijcard.2013.03.022
25. Investigators TA. Management of acute coronary syndromes in developing countries: acute coronary events—a multinational survey of current management strategies. Am Heart J. (2011) 162:852–9. doi: 10.1016/j.ahj.2011.07.029
26. Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A. Pre-hospital delay in patients with acute coronary syndrome: factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs. (2009) 8:26–33. doi: 10.1016/j.ejcnurse.2008.05.001
27. Ahmed S, Khan A, Ali SI, Saad M, Jawaid H, Islam M, et al. Differences in symptoms and presentation delay times in myocardial infarction patients with and without diabetes: A cross-sectional study in Pakistan. Indian Heart J. (2018) 70:241–5. doi: 10.1016/j.ihj.2017.07.013
28. Ängerud KH, Thylén I, Lawesson SS, Eliasson M, Näslund U, Brulin C, et al. Symptoms and delay times during myocardial infarction in 694 patients with and without diabetes; an explorative cross-sectional study. BMC Cardiovascul Disord. (2016) 16:108. doi: 10.1186/s12872-016-0282-7
29. Fox CS, Coady S, Sorlie PD, Sr RBD, Pencina MJ, Vasan RS, et al. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. (2007) 115:1544–50. doi: 10.1161/CIRCULATIONAHA.106.658948
30. Berman N, Jones MM, De Coster DA. ‘Just like a normal pain', what do people with diabetes mellitus experience when having a myocardial infarction: a qualitative study recruited from UK hospitals. BMJ Open. (2017) 7:e015736. doi: 10.1136/bmjopen-2016-015736
31. Liakos M, Parikh PB. Gender disparities in presentation, management, and outcomes of acute myocardial infarction. Curr Cardiol Rep. (2018) 20:64. doi: 10.1007/s11886-018-1006-7
32. Ferry AV, Anand A, Strachan FE, Mooney L, Stewart SD, Marshall L, et al. Presenting symptoms in men and women diagnosed with myocardial infarction using sex-specific criteria. J Am Heart Assoc. (2019) 8:e012307. doi: 10.1161/JAHA.119.012307
33. Miedema MD, Newell MC, Duval S, Garberich RF, Handran CB, Larson DM, et al. Causes of delay and associated mortality in patients transferred with st-segment– elevation myocardial infarction. Circulation. (2011) 124:1636–44. doi: 10.1161/CIRCULATIONAHA.111.033118
34. Beygui F, Roule V, Ivanes F, Dechery T, Bizeau O, Roussel L, et al. Indirect transfer to catheterization laboratory for st elevation myocardial infarction is associated with mortality independent of system delays: insights from the france-pci registry. Front Cardiovasc Med. (2022) 9:793067. doi: 10.3389/fcvm.2022.793067
35. Hedges JR, Feldman HA, Bittner V, Goldberg RJ, Zapka J, Osganian SK, et al. Impact of community intervention to reduce patient delay time on use of reperfusion therapy for acute myocardial infarction: rapid early action for coronary treatment (REACT) trial REACT Study Group. Acad Emerg Med. (2000) 7:862–72. doi: 10.1111/j.1553-2712.2000.tb02063.x
Keywords: Russia, access, cardiovascular disease, delay, EMS
Citation: Bates K, Schirmer H, Kontsevaya A, Bobrova N, Leon DA and McKee M (2023) Pre-hospital delays among patients with acute coronary syndrome in the Russian Federation: a multicentre prospective observational cohort study (the AMIR Study). Front. Disaster Emerg. Med. 1:1231318. doi: 10.3389/femer.2023.1231318
Received: 30 May 2023; Accepted: 20 July 2023;
Published: 10 August 2023.
Edited by:
Ioannis Pantazopoulos, University of Thessaly, GreeceReviewed by:
Ismet Çelebi, Gazi University, TürkiyeCopyright © 2023 Bates, Schirmer, Kontsevaya, Bobrova, Leon and McKee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin McKee, bWFydGluLm1ja2VlQGxzaHRtLmFjLnVr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.