- 1Department of Psychiatry, Dalhousie University, Halifax, NS, Canada
- 2Department of Computer Science, Dalhousie University, Halifax, NS, Canada
- 3Department of Psychology, Dalhousie University, Halifax, NS, Canada
- 4Maritime SPOR Support Unit, Halifax, NS, Canada
- 5Centre for Research in Family Health, Halifax, NS, Canada
- 6Department of Psychology, Acadia University, Wolfville, NS, Canada
- 7Mental Health and Addictions, Nova Scotia Health, Halifax, NS, Canada
- 8Department of Psychology, York University, Toronto, ON, Canada
- 9Mental Health and Addictions, IWK Health, Halifax, NS, Canada
Background: Youth mental health service organizations continue to rapidly broaden their use of virtual care and digital mental health interventions as well as leverage artificial intelligence and other technologies to inform care decisions. However, many of these digital services have failed to alleviate persistent mental health disparities among equity-seeking populations and in some instances have exacerbated them. Transdisciplinary and intersectional knowledge exchange is greatly needed to address structural barriers to digital mental health engagement, develop and evaluate interventions with historically underserved communities, and ultimately promote more accessible, useful, and equitable care.
Methods: To that end, the Digital, Inclusive, Virtual, and Equitable Research Training in Mental Health Platform (DIVERT), the Maritime Strategy for Patient Oriented Research (SPOR) SUPPORT (Support for People and Patient-Oriented Research and Trials) Unit and IWK Mental Health Program invited researchers, policymakers, interprofessional mental health practitioners, trainees, computer scientists, health system administrators, community leaders and youth advocates to participate in a knowledge exchange workshop. The workshop aimed to (a) highlight local research and innovation in youth-focused digital mental health services; (b) learn more about current policy and practice issues in inclusive digital mental health for youth in Canada, (c) participate in generating action recommendations to address challenges to inclusive, diverse and equitable digital mental health services, and (d) to synthesize cross-sector feedback to inform future training curriculum, policy, strategic planning and to stimulate new lines of patient-oriented research.
Results: Eleven challenge themes emerged related to white-colonial normativity, lack of cultural humility, inaccessibility and affordability of participating in the digital world, lack of youth and community involvement, risks of too much digital time in youth's lives, and lack of scientific evidence derived from equity-deserving communities. Nine action recommendations focused on diversifying research and development funding, policy and standards, youth and community led promotion, long-term trust-building and collaboration, and needing to callout and advocate against unsafe digital services and processes.
Conclusion: Key policy, training and practice implications are discussed.
1 Introduction
There is mass proliferation of digital mental health services for youth involving remote sensing and wearables, chatbots, health and wellness behavior apps, bioinformatics tools, virtual reality, virtual visits, moderated online social therapy, text message services, patient portals, self-directed technologies for diagnosis, treatment, and decision support, and services informed by increasingly complex data analytics and artificial intelligence (AI) (1–6). Yet, innovations continue to be developed and tested with majority populations and their benefits continue to be unevenly distributed among equity-deserving populations (7, 8). There is a long history of technological advances either disproportionately benefiting already privileged groups (9) and even going so far as disadvantaging marginalized groups (10). As a newer field, youth-focused digital mental health draws together transdisciplinary expertise across computer science and health sectors and could play a key role in disrupting these historical patterns.
Although digital health services offer a critical opportunity to improve wellbeing and decrease the burden of mental illness for the global population, its content and methods must represent and reflect the conceptions of wellness and priorities of people in historically underrepresented populations alongside evidence-based models for care (11). Conceptions of mental health and treatment must be understood before digital health services are built and researched, as they play a significant role in shaping health-seeking behaviors, treatment decisions, perceptions of therapeutic experiences, and recovery. Transdisciplinary and intersectional knowledge exchange is greatly needed to understand how underserved and under-represented youth populations conceptualize mental wellness and digital treatment options, as well as what their expectations and motivations are for seeking support through digital modalities (11–13). If this deeper collaborative work is overlooked, then any deployment of technological innovation may fail to result in improved mental health and substance use outcomes for youth most in need (14), or worse, create further inequity or harm.
Health system decision-makers, computer scientists, mental health researchers, and educational leaders in this field need to develop deep understandings of anti-racist, anti-oppressive and intersectionality theories (15) and be willing to examine their own positionality and biases. One example of these gaps is evidenced in a review of mobile mental health app evaluation frameworks developed since 2015, in which only 58% of them considered at least one EDI criterion (16). Those involved in digital mental health services must commit to undertaking disruptive actions to redress entrenched colonial, systemic, and structural inequities in digital mental health service and research spaces that continue to afford unearned advantage to some and oppress others (17).
Foundational to fostering shared action towards more equitable and inclusive digital mental health is shared knowledge. Shared knowledge is enabled by trust, communication, the use of intermediaries and experiential opportunities (18). One venue to capture collective transdisciplinary wisdom in complex environments of rapidly changing knowledge, technical innovation, and practice like digital mental health are knowledge exchange workshops that focus on deliberate dialogue among diverse partners (19). Knowledge exchange events promote dynamic and non-linear communication and relationship-building that can accelerate impactful research and facilitate its application for the benefit of society (20).
2 Method
2.1 Knowledge exchange workshop
As an extension to local cross-sector digital equity policy work (21) a scan of gaps in digital youth mental health services standards in Canada (1), implementation research within organizations that have youth digital mental health mandates (22, 23), focus groups with youth in the community and findings from local province-wide roll out of digital metal health services (24), this article reports on the findings of the “Inclusive Child & Youth Mental Health for the Digital Age” knowledge exchange workshop in Halifax/Kjipuktuk (Kjipuktuk is the Mi’kmaw name meaning “Great Harbour”), Canada in November, 2023. The knowledge exchange workshop was seen as a strategic platform to convene, share insights, foster collaboration and innovation among researchers, policymakers, practitioners, and those with lived experience.
The workshop aimed to (a) highlight local research and innovation in youth-focused digital mental health services; (b) learn more about current policy and practice issues in inclusive digital mental health for youth in Canada, (c) participate in generating recommendations and opportunities to address challenges to inclusive, diverse and equitable digital mental health services, and (d) to synthesize cross-sector feedback to inform training curriculum, policy, strategic planning and to stimulate new lines of patient-oriented research.
2.2 Co-host partners
The Digital, Inclusive, Virtual, and Equitable Research Training in Mental Health Platform (DIVERT) (https://divertmentalhealth.ca) is funded through the Canadian Institutes of Health Research (CIHR). DIVERT is a national transectoral (academic, patient and family, industry, health services) and transdisciplinary (psychology, social work, computer science, rehabilitation, medicine, and nursing) training program dedicated to gathering and promoting diverse approaches to how we understand, teach, research and provide mental health to children, youth, and their families. In addition, at its core it sets out to promote practical knowledge about technologies that can facilitate mental health care. DIVERT co-investigators and trainees working on the East Coast of Canada span multiple research institutions and labs working at the intersection of digital technologies and well-being (e.g., Persuasive Computing Lab, PROSIT, Corkum LABS, Centre for Research in Family Health).
The Maritime Strategy for Patient Oriented Research (SPOR) SUPPORT (Support for People and Patient-Oriented Research and Trials) Unit (collectively referred to as the MSSU) (https://mssu.ca/) works across the Maritime provinces (Nova Scotia, New Brunswick and Prince Edward Island) in Canada and is co-funded by the Canadian Institutes of Health Research (CIHR) initiative and individual provinces. The MSSU works as a connector between key sectoral groups by collaborating with patient/citizen partners, government, healthcare organizations, and the research community to ensure diverse perspectives in research (25).
The IWK Mental Health and Addictions Program is part of an academic women and children's teaching hospital in Halifax, NS. It has a complex pediatric mental health and substance use mandate. First, the program links to and from public health and community-based supports (e.g., non-governmental agencies) and primary care providers (e.g., family physicians and nurse practitioners). It also delivers secondary (e.g., community outpatient services) care for the surrounding metropolitan area, and tertiary (e.g., intensive or specialized) care for the whole province (e.g., only inpatient psychiatry unit). Last, is supports quaternary care for select mental health services (e.g., eating disorders, inpatient concurrent substance misuse/mental health disorders) for the broader region of Canadian east coast provinces. The mental health and addictions (MHA) team participates in a provincial governance group working with government and other health organizations to co-design a digital mental health strategy and service options for youth.
2.3 Structure
The workshop was organized into five main elements:
2.3.1 Indigenous knowledge sharing
As Indigenous knowledges have historically been silenced by dominant knowledge organization systems and practices, we sought to honour Indigenous knowledges at the event. A Mi’kmaw community member and invaluable shearer of cultural wisdom and multiple ways of knowing facilitated time for attendees to learn about the Mi’kmaw Medicine Wheel and sacred medicines through a hands-on sensory experience and storytelling. The community member also invited interested attendees to participate in a smudging ceremony and prayer of encouragement, inspiration and connection prior to the event.
2.3.2 Keynote
To situate the three main intersecting ideas of the event (youth mental health, digital innovation and equity, diversity, inclusivity, reconciliation, and accessibility an opening keynote address was given by the Nominated Principal Applicant for the DIVERT research team (Dr. Rebecca Pillai Riddell).
2.3.3 Pitch event
Five trainees (ranging from bachelor to post-doctoral stages of training) participated in a rapid one-minute pitch event to expose attendees to concrete examples of what a “digital mental health service” looks like, and how equity-diversity-inclusion (EDI) considerations show up in the design and research undertaken with these services (see Supplementary File 1). All other attendees were invited to act as panel judges and were given a scorecard to rate the pitches on two criteria (a) presentation structure and (b) engagement and clarity.
2.3.4 Discussion of challenges and action recommendations
The core element of the workshop was the formation of groups aimed at facilitating transsectoral/transdisciplinary discourse of key dimensions of digital strategies in child and youth mental health. Studies have consistently demonstrated the effectiveness of group formation methods in workshops, particularly those that prioritize diverse perspectives and intercultural, interdisciplinary collaboration (26). This approach ensures that attendees contribute varied insights, experiences, and expertise, thereby fostering a rich and dynamic environment conducive to meaningful knowledge exchange. Consequently, we incorporated intercultural and interdisciplinary factors into the group formation process, aligning with best practices identified in the literature. Attendees were organized into seven small groups (4–6 members each). Pre-event demographic data was used as a guide to shape maximum variation in group composition including professional disciplines (computer science, nursing, psychology), sectors (government, health systems, university), racially and ethnically minoritized group identity, gender, leadership levels (trainees, emerging, senior), and primary role of attendees (lived experience, advocate, clinician, administrator, researcher, policy-maker). Facilitators at each table were given a listen of four discussion-starter questions with prompts to guide attendees in conversation. For example the first question in the guide: Why aren't digital mental health services for youth and families as inclusive, equitable and diverse as they should be? Included two further prompts: (a) Are there assumptions or bias we make about digital mental health?; and (b) What worries you most about the current state of digital mental health for youth? Following a short break attendees returned to match those challenges with action recommendations. Each table then reported back during a large group discussion to validate and build on each other's ideas. Attendees were encouraged to jot down additional ideas on sticky notes and add to a dedicated wall space.
2.3.5 Panel to showcase future intersections of research, policy, and practice
The workshop closed out with an interactive, audience-guided panel discussion. The 4-member panel was intentionally selected to maximize diversity across disciplines (computer science, psychology, psychiatry), gender, role (policy, clinicians, intervention developer), career stage (trainees, established researchers) and racially and ethnically minoritized group identity.
2.4 Steering group and attendees
The Steering Committee members were identified via requests to DIVERT Co-Investigators and IWK MHA leaders seeking trainees or students, in particular from equity-deserving groups. Among the 11-member volunteer group were individuals with lived experience with mental health or substance use challenges, members of racially and ethnically minoritized groups, newcomers to Canada, gender diverse, trainees at various stages of study across multiple professional disciplines (computer science, psychology/neuroscience), representatives from both clinical and policy roles at both provincial health authorities, as well as representation from all three host organizations. A list of potential attendees was generated that bridged local health system leadership, government, youth and caregiver advocacy, EDI advocacy, researchers, innovation leaders, trainees and faculty working on digital mental health projects at the local and national level. A limit of 40 event attendees was determined at outset due to budget and planning constraints.
2.5 Pre-event preparation
Facilitators and note-takers for small-group table discussions were recruited and a pre-event meeting was held to provide tips and strategies for facilitating dialogue, prompts to encourage deeper reflection, and to answer any questions. A note-taking sheet and guide were developed and made available to facilitators. Trainees participating in the Pitch Event were given two months’ notice to develop their pitch slides (one to two slides) and were provided criteria on how the pitches would be scored along with tips for preparing a great pitch. At the request of panelists, a series of mock questions were provided two-weeks in advance to help prepare them for the discussion.
2.6 Workshop logistics
The 3-hour event was held from 9:00a.m. to 12:00 p.m., November 6th, 2023 on the Dalhousie University campus. We promoted networking interactions (breakfast event prior to meeting, short breaks, dedicated meet-and-greet time for trainees afterwards). A brief pre-workshop survey was used to collect attendee demographic data. Attendees were informed prior to registration and during the event that a de-identified summary of event learnings would be made publicly available. Attendees who were trainees or community members with lived experience received $100 honorariums. As the workshop involved evaluation for program planning rather than research, no ethical approval was necessary based on Article 2.5 of the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans (27).
2.7 Data gathering, analysis and validation
Nine sets of field notes from table facilitators and trainees along with sticky notes from poster boards in the room were digitized. Rapid analysis approaches have the potential to deliver valid, timely findings while taking less time to complete (28) so a rapid analysis of attendee input captured in facilitator notes was undertaken and informed by the Framework Method (29). As an initial step, familiarization with all nine sets of facilitators’ notes required multiple line-by-line close readings after which a paraphrase or label (a “code”) was applied that described what was interpreted to be most important in each line. Keywords, descriptors or technical terms were also underlined as a way to capture emphasis, tone, and urgency. After coding four sets of notes, one author (LW) compared the labels that had been applied and developed a set of initial codes. This preliminary coding framework was then applied to the remaining sets of notes but with flexibility to add a “new” code if something emerged that did not fit any of the existing coding labels. Charting of key themes was aimed at striking a balance between reducing the data on the one hand and retaining the original meanings and “feel” of the facilitator's words on the other. Gradually, characteristics of and differences between the codes were identified and wording of key themes refined iteratively. The process was undertaken separately for key themes related to “challenges” and “actions”. The positionality of the primary coder (e.g., white, cis-gender academic) necessitated further discussion and meaning-making with a broader group of voices. To review the credibility of the interpretation and improve trustworthiness, an initial draft of themes was shared and discussed with eleven members of the authorship group, a number of whom were facilitators at the event and the rest attendees themselves. Their direct experience at the event was vital to the interpretive process of coding. The broader coding review group was racially, ethnically, age and gender diverse with expertise across disciplines, organizational affiliations and career stage. Members had opportunities to provide and reflect on each other's written comments on the preliminary coding as well as engage in large-group or individual discussions about the codes. For example, a virtual data-analysis meeting with the authorship team was held to review early synthesis efforts, explore rival interpretations, refine theme structures and work towards consensus around key implications. Through this process codes were in some instances modified, regrouped, or renamed into the final version. This member-checking and validation process helped ensure accuracy and resonance with attendees’ experiences (30).
An online post-event evaluation survey was co-developed to align with other DIVERT and MSSU regional meeting evaluation processes. The critical evaluation allowed attendees to provide insights on the event's structure, content, and overall experience. The four-question survey was emailed to all attendees the morning following the event. Descriptive statistics were used to summarize results.
3 Results
3.1 Attendees
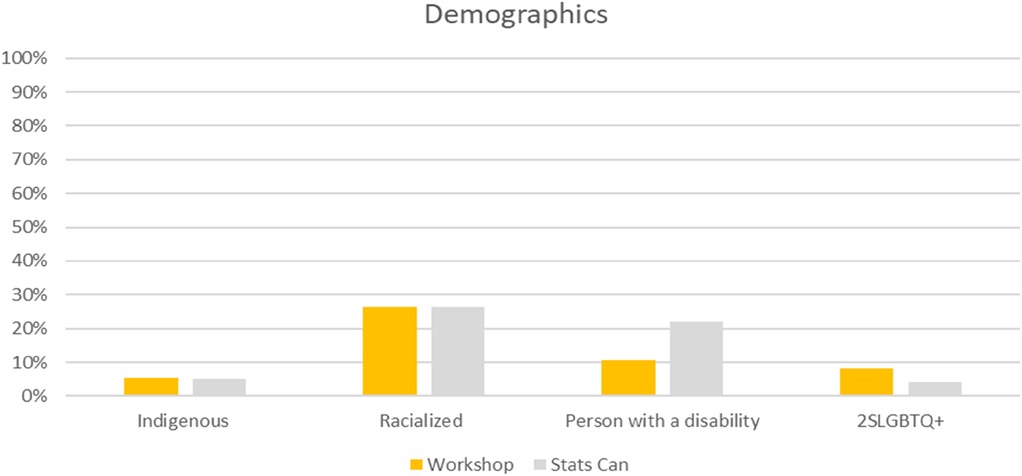
Thirty-eight people attended the event. As a basic check on the representativeness of event attendees in relation to the diversity of the general Canadian population, we compared attendee demographics characteristics to Statistics Canada data (see Figure 1). The percentage of attendees who self-identified as Indigenous, racially and ethnically minoritized, or members of the 2SLGBTQI+ (Two-Spirit, Lesbian, Gay, Bisexual, Transgender, Queer and/or Questioning, Intersex, and many other ways people self-identify) community met or exceeded Stats Canada population figures, even when not including the five percent of attendees who indicated “preferred not to say” to each of those questions of identity. The workshop had an over-representation of women (66%) compared to the general population, though not inconsistent with healthcare gender disparities, where women make up 75% of the workforce (31). There were 11% of attendees who did not report or preferred not to provide information on their gender. Attendees who identified as a person with a disability (11%) were significantly underrepresented when compared to the general population (22%), though 13% of attendees did not provide a response to that question.
The group of attendees reflected diversity across disciplines and expertise (see Figure 2), including nursing (8%), social work (8%), computer science/information technologies (26%), policy/health system administration (34%) and psychology/psychiatry (42%). Reflective of the intersectional perspectives of each attendee, there were a mix of individuals with lived experience with mental health or substance use conditions (16%), trainees and students (26%), academic faculty (29%), and those in health service roles (e.g., clinicians, policymakers, administrators; 42%). A significant portion of the group (18%) identified “other” perspectives they brought to the discussion, including research staff, youth and caregiver advocates, Indigenous and EDI consultants, non-governmental organization/non-profit sector and digital service providers.
3.2 Challenges and action recommendations
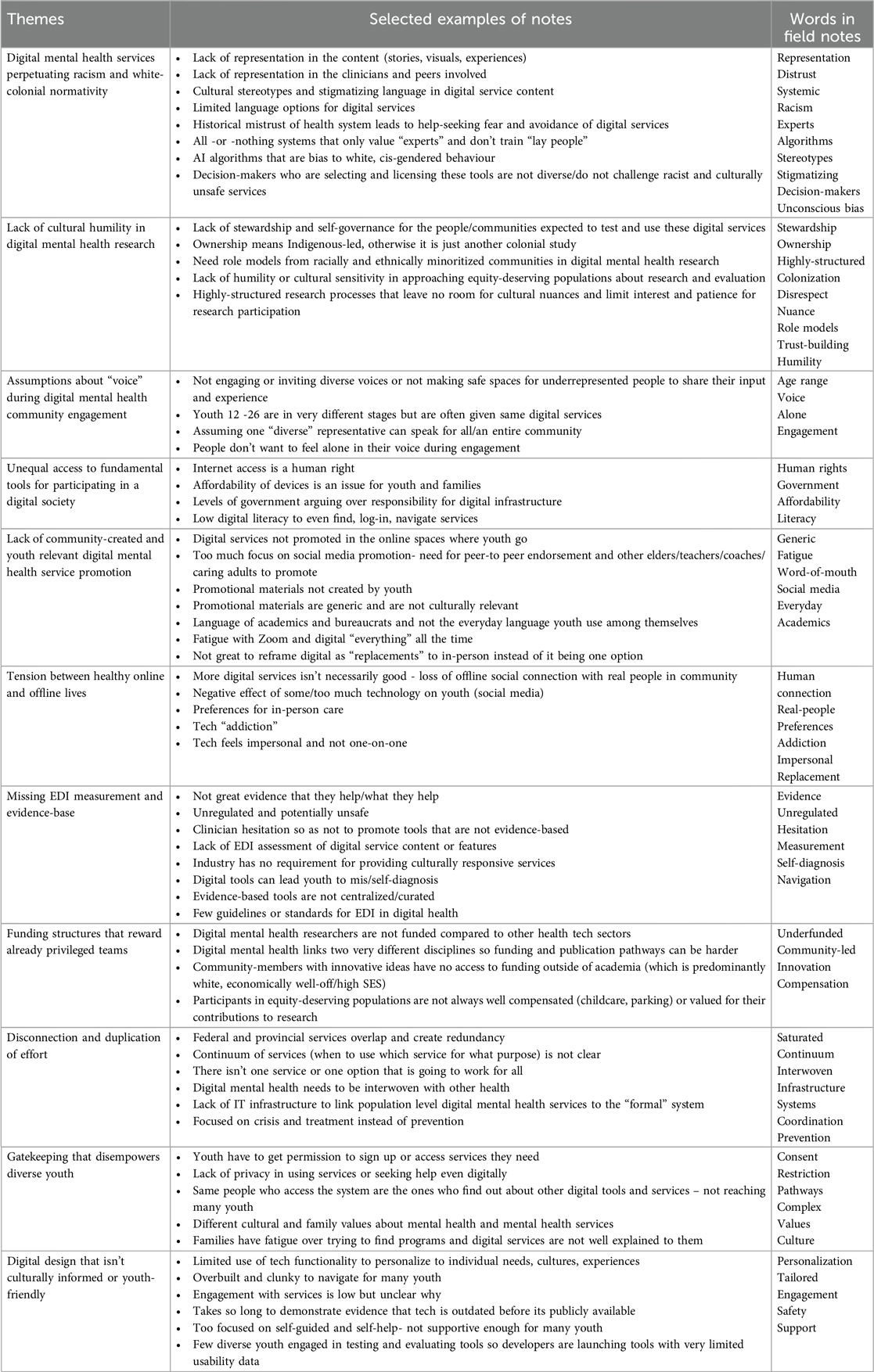
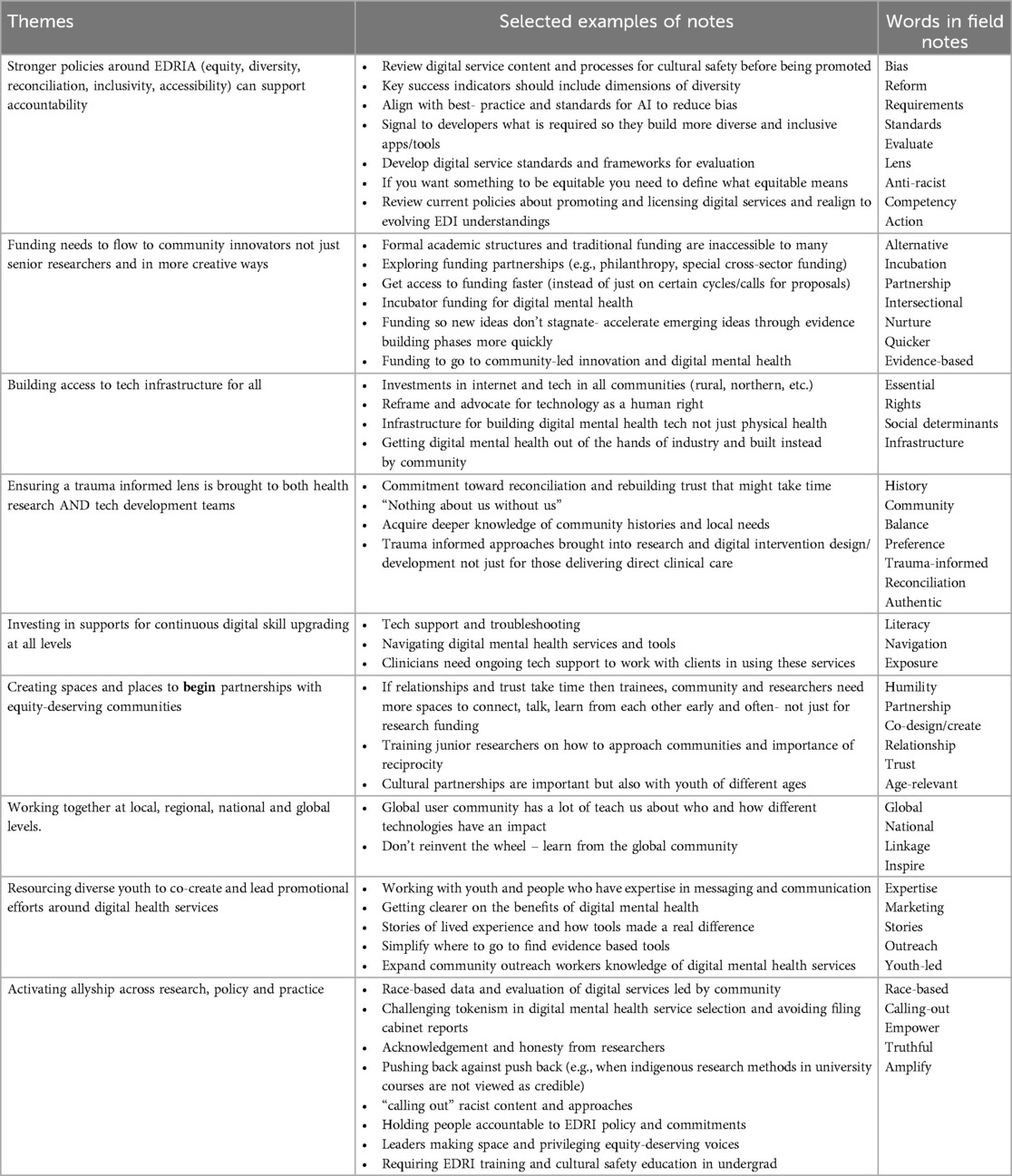
The insights gathered from discussions groups brought to the forefront 11 key themes in relation to the challenges faced (see Table 1) and nine action recommendations to fortify the efficacy and inclusivity of digital health tools for youth in the future (see Table 2). Generally, racism, discrimination, and oppression were viewed as chronic and embedded in digital mental health innovation processes, including in the hierarchy and ownership of data, mental health knowledges, and promotional strategies involved in launching digital health services. The rapid rate of technology development means computer science and mental health-sector graduates must be prepared to address not only the challenges with current technologies, but also think critically about how their personal, academic, and professional environments will be shaped by digital health services in the future.
3.3 Panel discussion
In responding to audience-questions, panelists highlighted challenges, successes, and lessons learned about diversity in digital mental health services. Specifically, (a) how transdisciplinary knowledge is vital to the future of digital health design and implementation but requires the time to build new shared language across disciplines, (b) how important it is for leaders to be curious and not avoid learning about emerging or unfamiliar technologies and ways they might address inequities; (c) how too often adult assumptions about what youth want guide digital health policy (e.g., believing all youth want to engage with digital mental health services); and (d) how culturally-safe care a low bar aimed at limiting harm but culturally-centered care prioritizes the intersection of mental health and culture and actively seeks to integrate cultural knowledge, awareness, and understanding into digital health service design.
3.4 Event evaluations
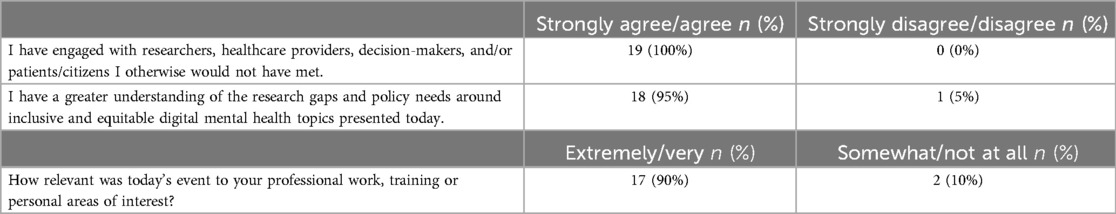
Fifty percent of attendees (19/38) completed post-event evaluations (see Table 3). Overall, attendees saw value in making intersectional and interdisciplinary connections with 100% of those who responded (n = 19) strongly agreeing or agreeing the event allowed them to engage others they otherwise would not have met. As one attendee commented:
“I owe the knowledge I’ve gained to attending the event. The table grouping was like magic, providing me with insights into existing digital tools from various angles. This experience allowed me to uncover numerous research avenues that have the potential to enhance our understanding and advance digital tools for mental health to a new level.” – Attendee
4 Recommendations
The knowledge exchange workshop is one of the first of its kind in Canada to bring transdisciplinary and cross-sector groups together to jointly share experience and discuss current and future tensions within the system of digital mental health services for youth populations specifically. The workshop built off of prior local focus groups and workshops with youth themselves and was only one component of a larger series of local and national youth engagement sessions designed to ensure youth perspectives are heard alongside other key partners on the issue. Results of those other engagements will be published elsewhere. While a number of attendees were youth (aged 26 and under) there is value in thinking about how future events could combine audiences in these kinds of workshops so that youth have direct contact with policy and health system leadership.
4.1 Policy
Most challenges and necessary actions raised by attendees were situated at the organizational and community levels. This should be a signal that while action to address digital health service inequities can be undertaken by individuals, explicit and deliberate action is required by governments, health care and academic institutions to facilitate larger impacts on structural factors. This finding aligns with recent American Psychological Association guidelines promoting population health approaches that leverage technology to promote community health not just promoting online tools to individuals (32). Further, findings from the workshop suggest broadening our understanding of the role of digital tools in prevention and early intervention to maintain wellbeing not just as interventional treatment for youth with significant symptoms or functional impairment. Funding sources and appropriate timelines are required from funding agencies to allow researchers and communities to build true and genuine relationships to build digital health tools for and with community Our findings support recommendations for increasing digital mental health reach and uptake through youth and community engagement (33). This will become increasingly important in Canada as the recently launched Mental Health Commission of Canada eMental Health Strategy for Canada has explicitly identified the need to address EDI gaps and to engage those with lived experience in co-identifying policy and service priorities (34). Once digital health tools have been developed, their release into the live environment of the healthcare system offers critical moments for evaluating and addressing any impacts on health inequity and health systems leaders should prioritize that evaluation. Policies should not only enhance access to digital infrastructure but prioritize digital mental health initiatives that genuinely reflect local cultural dynamics and youth needs. For example, educational messaging and promotion around digital mental health service benefits and relevance is best created by youth, for youth in their own communities (35). These policies should seamlessly blend technology innovation aims while prioritizing trust-building with diverse communities.
4.2 Training
To better prepare trainees to advocate for and create more inclusive and equitable mental health technologies they must be encouraged to interrogate both the systems and structures around them and the products and therapeutic innovations they create. Both computer science and mental health clinicians connected to digital mental health design (especially those from dominant identities based on race, ethnicity, gender, sexuality, ability, and socioeconomic class) should deepen their cultural competence. Training that validates, facilitates, liberates, and empowers those who are historically underrepresented to cultivate their identities and direct digital health innovation should be prioritized (36). Attendees affirmed that building more equitable digital services can only happen through collaborative work. That 100% (n = 19) of attendees who evaluated the workshop indicated they made connections at the event with people they otherwise never would have underlies the necessity of organizational leadership in being intentional in organizing ongoing opportunities for knowledge exchange. Steps to increase cross-talk between disparate disciplines, perspectives and cultures can decrease feelings of isolation, and promote cultural humility and reciprocity. Within the Canadian landscape the DIVERT mental health training platform has a significant role to play in promoting a national community of transdisciplinary mental health researchers and clinicians that will champion an inclusive and accessible mental health care system for youth. Findings of the workshop highlight how post-secondary training needs to not only focus on digital and clinical competency development but building capacity in allyship, anti-oppressive practice and community partnership (37).
4.3 Research
Researchers and those who fund innovation opportunities should (a) center equity in their teams and theoretical approaches, (b) prioritize examination of the intersectionality of various factors such as race, gender, socioeconomic status, and sexual orientation in the context of youth digital mental health use and outcomes (38), (c) focus on issues of digital literacy and engagement, (d) use “out to the box” funding approaches to accelerate availability of culturally relevant, community-led services, (e) explore methods that amplify perspectives, world views and needs of underserved populations, (f) ensure ethical approaches for collecting, stewarding and using digital health data are used, (g) advance co-design methods (39) and research processes that amplify youth perspectives and preferences and influence the development of programs and policies that affect their lives (6), and (h) think about ways to make the tools they develop more easily adapted to different communities or marginalized groups. Generally, our findings align with and extend evidence from reviews of existing evidence (40, 41) adding to a rich and evolving global literature in digital mental health.
5 Limitations
People living with a disability (i.e., physical, sensory, and cognitive) were statistically underrepresented in the attendee group when compared to the general population. There was some health sector diversity representation but no attendees from occupational recreational therapy. We explored themes based on facilitator notes not on the first-voice of attendees in the discussion which may have introduced bias. While the authorship team engaged in the broader data analysis represented diverse intersectional perspectives, and there were opportunities for member-checking we recognize that the positionality of the primary coder may have introduced unintended bias. The post-workshop survey was not completed by all attendees and could reflect bias toward positive responses.
6 Conclusions
Active and continuous collaboration among these disciplines and roles is vital to ensure cultural, structural, financial, geographic, and material differences that shape a young person's ability to encounter and engage with digital mental health are considered. We urge digital health developers and mental health leaders to consider all aspects of digital equity, and to come together routinely to revisit the lessons learned here so that we achieve a more equitable, fair, and just mental healthcare system that leads to better outcomes for all youth.
Author contributions
MA: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. BB: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. MD: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. AI: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. EL: Conceptualization, Data curation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. PM: Validation, Writing – original draft, Writing – review & editing. SM: Conceptualization, Writing – original draft, Writing – review & editing. KM: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. GO-D: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. RO: Validation, Writing – original draft, Writing – review & editing. RP: Conceptualization, Funding acquisition, Project administration, Resources, Writing – original draft, Writing – review & editing. LW: Conceptualization, Data curation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. VY: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Efforts for this event were supported by CIHR grants #42488 and #180215, the IWK Mental Health and Addictions Program and the MSSU. The MSSU is funded by Canadian Institutes of Health Research with a 1:1 match with provincial funding partners. The Maritime funding partners include New Brunswick Department of Health, Nova Scotia Department of Health and Wellness, Prince Edward Island Department of Health and Wellness, the University of Prince Edward Island and ResearchNB. The opinions, results and conclusions reported in this paper are those of the authors and do not necessarily represent the official views of any of the funding organizations.
Acknowledgments
Yolanda Pennell, Courtney Pennell, Negar Vakili, Jeremy Smith, Claire Keenan, Alandra Wood, Natalie Jarvis, Chloe Eward, Sahil Chawla, Dr. Jill Chorney, Ryan Wilson, Dr. Sandra Meier, Dr. Penny Corkum, Maureen Brennan, Dr. Alexa Bagnell, Dr. Vincent Agyapong, Digital Advisory at IWK, HealthyMindsNS, NSH MHA, OAMH. We would like to thank all attendees, youth and caregiver advocates, community members, trainees, health system leaders, affiliated scientists and partners who made time to attend or were involved in helping to organize the event.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2024.1449129/full#supplementary-material
References
1. Kemp J, Chorney J, Kassam I, MacDonald J, MacDonald T, Wozney L, et al. Learning about the current state of digital mental health interventions for Canadian youth to inform future decision-making: mixed methods study. J Med Internet Res. (2021) 23(10):e30491. doi: 10.2196/30491
2. Jerrott S, Clark S, Chorney J, Coulombe A, Wozney L. Feasibility of text messages for enhancing therapeutic engagement among youth and caregivers initiating outpatient mental health treatment: mixed methods study. JMIR Form Res. (2022) 6(8):e35685. doi: 10.2196/35685
3. Suruliraj B, Bessenyei K, Bagnell A, McGrath P, Wozney L, Orji R, et al. Mobile sensing apps and self-management of mental health during the COVID-19 pandemic: web-based survey. JMIR Form Res. (2021) 5(4):e24180. doi: 10.2196/24180
4. Alvarez-Jimenez M, Koval P, Schmaal L, Bendall S, O’Sullivan S, Cagliarini D, et al. The horyzons project: a randomized controlled trial of a novel online social therapy to maintain treatment effects from specialist first-episode psychosis services. World Psychiatry. (2021) 20(2):233–43. doi: 10.1002/wps.20858
5. MacDougall S, Jerrott S, Clark S, Campbell LA, Murphy A, Wozney L. Text message interventions in adolescent mental health and addiction services: scoping review. JMIR Ment Health. (2021) 8(1):e16508. doi: 10.2196/16508
6. Negar V, Curran J, Walls R, Phillips D, Miller A, Cassidy C, et al. Preferences for text-messaged supports during youth transition to adult mental health services: a theory-informed modified e-Delphi study. JMIR Form Res. (2024) 8:e51690. doi: 10.2196/51690
7. Friis-Healy EA, Nagy GA, Kollins SH. It is time to REACT: opportunities for digital mental health apps to reduce mental health disparities in racially and ethnically minoritized groups. JMIR Ment Health. (2021) 8(1):e25456. doi: 10.2196/25456
8. Bear HA, Ayala Nunes L, Ramos G, Manchanda T, Fernandes B, Chabursky S, et al. The acceptability, engagement, and feasibility of mental health apps for marginalized and underserved young people: systematic review and qualitative study. J Med Internet Res. (2024) 26:e48964. doi: 10.2196/48964
9. Iyamu I, Gómez-Ramírez O, Xu AX, Chang HJ, Watt S, Mckee G, et al. Challenges in the development of digital public health interventions and mapped solutions: findings from a scoping review. Digit Health. (2022) 8:0552076221102255. doi: 10.1177/20552076221102255
10. Straw I, Callison-Burch C. Artificial intelligence in mental health and the biases of language based models. PLoS One. (2020) 15(12):e0240376. doi: 10.1371/journal.pone.0240376
11. Kozelka EE, Jenkins JH, Carpenter-Song E. Advancing health equity in digital mental health: lessons from medical anthropology for global mental health. JMIR Ment Health. (2021) 8(8):e28555. doi: 10.2196/28555
12. Brewer LC, Fortuna KL, Jones C, Walker R, Hayes SN, Patten CA, et al. Back to the future: achieving health equity through health informatics and digital health. JMIR Mhealth Uhealth. (2020) 8(1):e14512. doi: 10.2196/14512
13. Holly L, Smith RD, Ndili N, Franz C, Stevens EAG. A review of digital health strategies in 10 countries with young populations: do they serve the health and wellbeing of children and youth in a digital age? Front Digit Health. (2022) 4. doi: 10.3389/fdgth.2022.817810
14. Huh J, Koola J, Contreras A, Castillo AK, Ruiz M, Tedone KG, et al. Consumer health informatics adoption among underserved populations: thinking beyond the digital divide. Yearb Med Inform. (2018) 27(1):146–55. doi: 10.1055/s-0038-1641217
15. Figueroa CA, Luo T, Aguilera A, Lyles CR. The need for feminist intersectionality in digital health. Lancet Digit Health. (2021) 3(8):e526–33. doi: 10.1016/S2589-7500(21)00118-7
16. Ramos G, Ponting C, Labao JP, Sobowale K. Considerations of diversity, equity, and inclusion in mental health apps: a scoping review of evaluation frameworks. Behav Res Ther. (2021) 147:103990. doi: 10.1016/j.brat.2021.103990
17. Veinot TC, Mitchell H, Ancker JS. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc. (2018) 25(8):1080–8. doi: 10.1093/jamia/ocy052
18. de Wit-de Vries E, Dolfsma WA, van der Windt HJ, et al. Knowledge transfer in university–industry research partnerships: a review. J Technol Transf. (2019) 44:1236–55. doi: 10.1007/s10961-018-9660-x
19. Boyko JA, Lavis JN, Abelson J, Dobbins M, Carter N. Deliberative dialogues as a mechanism for knowledge translation and exchange in health systems decision-making. Soc Sci Med. (2012) 75(11):1938–45. doi: 10.1016/j.socscimed.2012.06.016
20. Ward V, Smith S, House A, Hamer S. Exploring knowledge exchange: a useful framework for practice and policy. Soc Sci Med. (2012) 74(3):297–304. doi: 10.1016/j.socscimed.2011.09.021
21. National Collaborating Centre for Determinants of Health and Nova Scotia Health. Digital Equity in Health Services: Practice Brief. Antigonish, Halifax, NS: NCCDH, St. Francis Xavier University, NSH, Mental Health and Addictions Program (2022). Available online at: https://nccdh.ca/resources/entry/digital-equity-in-health-services
22. Gehring ND, McGrath P, Wozney L, Soleimani A, Bennett K, Hartling L, et al. Pediatric eMental healthcare technologies: a systematic review of implementation foci in research studies, and government and organizational documents. Implement Sci. (2017) 12(1):76. doi: 10.1186/s13012-017-0608-6
23. Wozney L, Newton AS, Gehring ND, Bennett K, Huguet A, Hartling L, et al. Implementation of eMental health care: viewpoints from key informants from organizations and agencies with eHealth mandates. BMC Med Inform Decis Mak. (2017) 17(1):78. doi: 10.1186/s12911-017-0474-9
24. Mental Health Commission of Canada, Nova Scotia Mental Health and Addictions Program. Stepping Together for Digital Mental Health and Addictions Services. Ottawa, Canada: Mental Health Commission of Canada (2022). Available online at: https://mentalhealthcommission.ca/wp-content/uploads/2022/05/Stepping-Together-for-Digital-Mental-Health-and-Addictions-Services.pdf
25. Kontak J, Grant A, Jeffers E, Boulos L, Ricketts J, Davies M, et al. The maritime SPOR SUPPORT unit (MSSU) bridge process: an integrated knowledge translation approach to address priority health issues and increase collaborative research in Nova Scotia, Canada. Int J Health Policy Manag. (2023) 12:6901. doi: 10.34172/ijhpm.2023.6901
26. Hung H, Murray G, Varni G, Lehmann-Willenbrock N, Gerpott FH, Oertel C. Workshop on interdisciplinary insights into group and team dynamics. Proceedings of the 2020 International Conference on Multimodal Interaction. (2020). doi: 10.1145/3382507.3419748
27. Medical Research Council (Canada). Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. Ottawa: Medical Research Council of Canada (2022). Available online at: https://ethics.gc.ca/eng/policy-politique_tcps2-eptc2_2022.html
28. Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open. (2018) 8(10):e019993. doi: 10.1136/bmjopen-2017-019993
29. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:117. doi: 10.1186/1471-2288-13-117
30. Tobin GA, Begley CM. Methodological rigour within a qualitative framework. J Adv Nurs. (2004) 48(4):388–96. doi: 10.1111/j.1365-2648.2004.03207.x
31. Human Resources for Health Global Resource Center. Resource spotlight: gender and health workforce statistics. (2021). Available online at: https://www.hrhresourcecenter.org/gender_stats.html (accessed January 01, 2024).
32. Dodge KA, Prinstein MJ, Evans AC, Ahuvia IL, Alvarez K, Beidas RS, et al. Population mental health science: guiding principles and initial agenda. Am Psychol. (2024) 79(6):805–23. doi: 10.1037/amp0001334
33. Stiles-Shields C, Ramos G, Ortega A, et al. Increasing digital mental health reach and uptake via youth partnerships. Npj Mental Health Res. (2023) 2:9. doi: 10.1038/s44184-023-00030-1
34. Mental Health Commission of Canada. An E-Mental Health Strategy for Canada (2024). Available online at: https://mentalhealthcommission.ca (accessed January 01, 2024).
35. Dimitropoulos G, Bassi EM, Bright KS, Gondziola J, Bradley J, Fersovitch M, et al. Implementation of an electronic mental health platform for youth and young adults in a school context across Alberta, Canada: thematic analysis of the perspectives of stakeholders. JMIR Ment Health. (2024) 11:e49099. doi: 10.2196/49099
36. Abernethy A, Adams L, Barrett M, et al. The promise of digital health: then, now, and the future. NAM Perspect. (2022) 2022. Published June 27, 2022. doi: 10.31478/202206e
37. Wu D, Saint-Hilaire L, Pineda A, Hessler D, Saba G, Salazar R, et al. The efficacy of an anti-oppression curriculum for health professionals. Fam Med. (2019) 51(1):22–30. Published June 2, 2020. doi: 10.22454/fammed.2018.227415
38. Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. (2020) 22(6):e19361. doi: 10.2196/19361
39. Curran JA, Cassidy C, Bishop A, et al. Codesigning discharge communication interventions with healthcare providers, youth and parents for emergency practice settings: eDUCATE study protocol. BMJ Open. (2020) 10:e038314. doi: 10.1136/bmjopen-2020-038314
40. Philippe TJ, Sikder N, Jackson A, Koblanski ME, Liow E, Pilarinos A, et al. Digital health interventions for delivery of mental health care: systematic and comprehensive meta-review. JMIR Ment Health. (2022) 9(5):e35159. doi: 10.2196/35159
Keywords: mental health, technology, diversity, equity and inclusion, interdisciplinary, translational science, knowledge translation
Citation: Adu M, Banire B, Dockrill M, Ilie A, Lappin E, McGrath P, Munro S, Myers K, Obuobi-Donkor G, Orji R, Pillai Riddell R, Wozney L and Yisa V (2024) Centering equity, diversity, and inclusion in youth digital mental health: findings from a research, policy, and practice knowledge exchange workshop. Front. Digit. Health 6:1449129. doi: 10.3389/fdgth.2024.1449129
Received: 14 June 2024; Accepted: 2 October 2024;
Published: 31 October 2024.
Edited by:
Heleen Riper, VU Amsterdam, NetherlandsReviewed by:
Giovanni Ramos, University of California, Irvine, United StatesRicardo Felipe Munoz, Palo Alto University, United States
Copyright: © 2024 Adu, Banire, Dockrill, Ilie, Lappin, McGrath, Munro, Myers, Obuobi-Donkor, Orji, Pillai Riddell, Wozney and Yisa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lori Wozney, bG9yaS53b3puZXlAaXdrLm5zaGVhbHRoLmNh
 Medard Adu1
Medard Adu1 Mya Dockrill
Mya Dockrill Alzena Ilie
Alzena Ilie Elizabeth Lappin
Elizabeth Lappin Patrick McGrath
Patrick McGrath Samantha Munro
Samantha Munro Kady Myers
Kady Myers Gloria Obuobi-Donkor
Gloria Obuobi-Donkor Rita Orji
Rita Orji Rebecca Pillai Riddell
Rebecca Pillai Riddell Lori Wozney
Lori Wozney