- 1School of Public Health, Sefako Makgatho University of Health Sciences, Pretoria, South Africa
- 2Khoury College of Computer Sciences, Northeastern University, Boston, MA, United States
- 3Chobanian & Avedisian School of Medicine, Boston University, Boston, MA, United States
Introduction: Young women from the low-middle-income country of Lesotho in southern Africa frequently report limited knowledge regarding sexual and reproductive health issues and engage in risky sexual behaviors. The purpose of this study is to describe the adaptation of an evidence-based conversational agent system for implementation in Lesotho and provide qualitative data pertaining to the success of the said adaptation.
Methods: An embodied conversational agent system used to provide preconception health advice in the United States was clinically and culturally adapted for use in the rural country of Lesotho in southern Africa. Inputs from potential end users, health leaders, and district nurses guided the adaptations. Focus group discussions with young women aged 18–28 years who had used the newly adapted system renamed “Nthabi” for 3–4 weeks and key informant interviews with Ministry of Health leadership were conducted to explore their views of the acceptability of the said adaptation. Data were analyzed using NVivo software, and a thematic content analysis approach was employed in the study.
Results: A total of 33 women aged 18–28 years used Nthabi for 3–4 weeks; eight (24.2%) of them were able to download and use the app on their mobile phones and 25 (75.8%) of them used the app on a tablet provided to them. Focus group participants (n = 33) reported that adaptations were culturally appropriate and provided relevant clinical information. The participants emphasized that the physical characteristics, personal and non-verbal behaviors, utilization of Sesotho words and idioms, and sensitively delivered clinical content were culturally appropriate for Lesotho. The key informants from the Ministry leadership (n = 10) agreed that the adaptation was successful, and that the system holds great potential to improve the delivery of health education in Lesotho. Both groups suggested modifications, such as using the local language and adapting Nthabi for use by boys and young men.
Conclusions: Clinically tailored, culturally sensitive, and trustworthy content provided by Nthabi has the potential to improve accessibility of sexual and reproductive health information to young women in the low-middle-income country of Lesotho.
1. Introduction
Adolescents face many sexual and reproductive health problems worldwide, including unplanned pregnancy, sexually transmitted infections, and human immunodeficiency virus (HIV) infections (1). Adolescents account for 42% of new HIV infections globally, and four in five young people with HIV live in sub-Saharan Africa (2). Lesotho has the second-highest HIV prevalence in the world, accounting for 22.7%, and one of the highest HIV incidence rates among adolescent girls and young women accounting for 0.33% (3). The maternal mortality rate in Lesotho of 544/100,000 live births is the second highest in Southern African Development Community countries (4).
In Lesotho, adolescent girls and young women frequently report limited knowledge in sexual and reproductive health issues and engage in risky sexual behaviors. They are at increased risk of early sexual debut (14 years), unprotected sex, and multiple sexual partners, exposing them at risk of acquiring sexually transmitted infections, including HIV and unintended pregnancy (5). Providing sexual and reproductive health education to young women is challenging in this rural, mountainous country (6, 7) and where health professionals face constraints related to time and resources.
New tools to deliver health education are needed. In Lesotho, 94% of people aged 18–29 years use smartphones, and 3G data coverage is available in almost 90% of the country (8, 9). The high penetration of mobile technologies provides an opportunity to explore the use of new tools delivered on mobile phones as an alternative to the traditional face-to-face provision of health education (10).
Embodied conversational agents (ECAs) are computer-based animated characters designed to simulate face-to-face human interactions. They are an effective medium to educate patients with limited health or computer literacy, as the human–computer interface relies only minimally on text comprehension and prioritizes conversation making it more accessible to patients with limited literacy skills (11, 12). Non-verbal conversational behaviors, such as hand gestures that convey specific information through pointing, shape, or motion, are channels for conveying information on semantic content that enhances message comprehension (11).
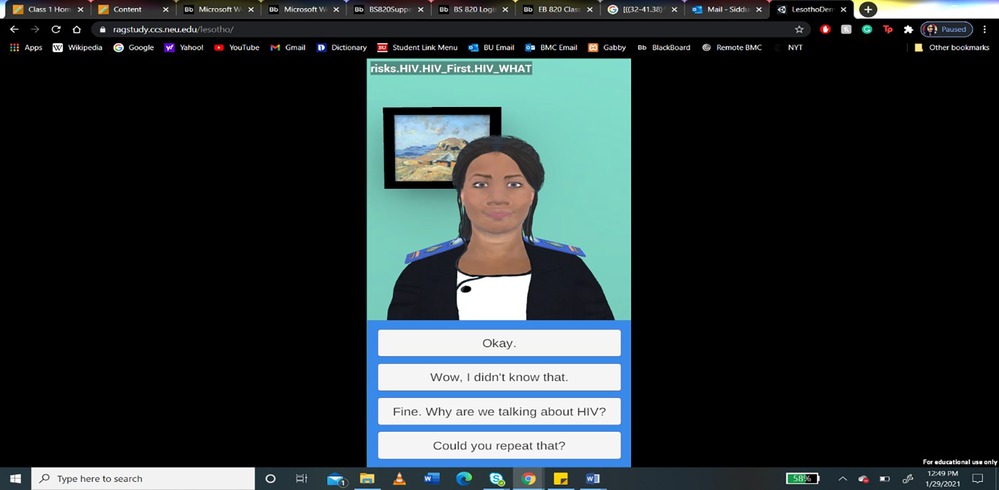
An ECA called Gabby was designed to deliver sexual and reproductive health information to African American women of reproductive age in the United States that demonstrated significant improvement in addressing reproductive health risks (see Figure 1) (13, 14).

Figure 1. Gabby was developed in the United States to deliver health education that women could access on desktop computers.
This paper describes the process used to adapt Gabby for use in Lesotho, and provides qualitative data regarding the success of the adaptation, collected from potential end users and Ministry of Health (MOH) leadership.
2. Methods
2.1. Conceptual model
The PEN-3 cultural utility model guided the adaptations, which provides valuable guidelines for ensuring a culture-specific intervention by identifying and organizing a community's culture in the planning processes (15–17). The model includes the cultural identity domain (person, extended family, and neighborhood), the relationship and expectation domain (perceptions, enablers, and nurturers), and the cultural empowerment domain (positive, existential, and negative) (18–20).
Adaptations were also guided by the heuristic framework for cultural adaptations of Barrera et al. (21), which includes information gathering, preliminary adaptation design, preliminary adaptation tests, adaptation refinement, and cultural adaptation trial.
2.2. Information gathering for adaptation
To understand the adaptations needed, the Northeastern University team leader visited Lesotho in January 2020. Meetings were held with MOH managers for adolescent health, HIV, family planning, and nursing to elicit recommendations with regard to potential adaptations. Meetings were also conducted with district nurses and with young women seeking healthcare services.
The meetings elicited details with regard to how Basotho use their hands, facial gestures, and body language in conversation and ideas regarding the use of Basotho language and cultural references, such as idioms, that could be incorporated into the new system. The persona of the new character was explored to identify those that would lead to greater trust in the health information being delivered. Interviews highlighted the importance of promoting engagement with the new system. Images of Basotho women were used to create the character. Decisions were made regarding the character's appearance (e.g., hair and clothing), behavior (speech pattern), nationality, sex, age, occupation, and name.
The MOH officials were asked to recommend topics that they believed to be critical for improving sexual and reproductive health for adolescents and young women. The topics agreed upon for inclusion in the system were family planning, HIV and AIDS, tuberculosis, healthy eating, and folic acid supplementation. Boston University and the Lesotho team then used the Lesotho national guidelines on these topics to prepare the dialogs to be delivered by Nthabi.
Technical adaptations were required to deploy the prototype Gabby interface (designed to be displayed on a computer screen) to now be displayed on smartphone screens. The new Nthabi system interface was designed to display only the face and response options of the characters.
The development team sourced Lesotho mobile phones to gain information regarding the specifications penetration of devices. To increase the accessibility and use of the system, a decision was made to ensure that the app can be completely downloaded into the user's mobile phone, thereby enabling use even outside of WiFi-enabled environments. Data pertaining to user usage and the content discussed would be downloaded when the user is next in a WiFi-enabled environment.
2.3. Recruitment and enrollment of participants
The participants were recruited to use Nthabi in accordance with predetermined eligibility criteria: aged 18–28, owned a smartphone, spoke English, and lived in the Leribe or Berea districts of Lesotho. A purposive sampling technique was employed to recruit participants when they accessed services at the adolescent and maternal and child services at district hospitals. The Nthabi app was downloaded onto the participants’ mobile phones after they provided informed consent. The participants who were unable to download the app were provided with an internet-accessible tablet device. All participants were asked to use the system daily for 4 weeks.
2.4. Focus groups of participants using Nthabi
Young women who used the Nthabi system were contacted to arrange for their participation in focus groups to elicit their perceptions of the system. Four focus groups were conducted between July and August 2022. The groups were facilitated by the first author using an interview guide with open-ended questions designed to explore the cultural and clinical adaptation, ease of use, problems encountered, willingness to continue use, and possible future use. Focus group participants were provided a stipend of 50 Maloti (∼US $3).
2.5. Key informant interviews with MOH leaders
Purposive sampling was employed to recruit MOH program managers and adolescent health nurses to participate in key informant interviews. They were asked to review the content of a video shared on WhatsApp of the key parts of the Nthabi interactions for 3–5 days. In June and July 2022, interviews to elicit their perceptions were conducted using an interview guide with open-ended questions used to explore cultural and clinical adaptation and perceptions of use to deliver health education in the country. These participants did not receive a stipend.
3. Data analysis
Data analysis was headed by the Sefako Makgatho University team. All interviews and focus groups were approximately 1 h and were audio recorded. The study team members transcribed semi-verbatim all audio recordings into Microsoft® Word and checked for accuracy, and extraneous sounds, remarks, or repetitions were omitted in the transcription. In addition, words were added, as appropriate, for clarity. They were not returned to participants for correction. Before analysis, all identifying data were removed, and Sesotho words were translated into English.
All qualitative data were imported into QSR International's NVIVO v12 software for coding and analysis. We conducted a thematic analysis using a combined inductive and deductive approach to coding, starting with broad codes from the interview guide and allowing room for new codes to emerge. Given the heterogeneity of respondent demographics, we coded all interviews instead of stopping when saturation was researched within particular thematic areas. A coding tree was produced that contained emergent categories of barriers and facilitators and re-coded the data. The core major and minor themes were determined through iterative inputs from authors on the resultant thematic map (22).
The demographic data were collected from the participants at enrollment and were presented as counts, frequencies, and means. All information was stored on encrypted tablets.
4. Results
4.1. Initial consultative meetings
Initial consultative meetings were held with eight MOH directors or program managers, four district nurses who were aged 25–50 years, and nine women aged 18–28 years.
Based on these discussions, it was recommended that the Lesotho version of Gabby would be a young female nurse named “Nthabi”, wearing a Lesotho nurse's uniform and using Sesotho words and idioms. Her hairstyle (braids), complexion (medium, similar to the local population), use of gestures (calm and gentle), and mannerisms (a humble professional with a sense of humor) would be relatable to young women in Lesotho (see Figure 2). English was chosen as the preferred language for Nthabi, since a Sesotho speech synthesizer was unavailable.
To promote engagement, a professional Mosotho woman artist and storyteller was engaged to write 60 daily installments of a serial story, each ending with a cliff-hanger that could motivate users to use the app daily. Such serialized stories are popular in Lesotho.
4.2. Description of participants who used Nthabi
A total of 41 participants who met the eligibility criteria were recruited to use the new app. After giving consent, the participants were assisted to download the Nthabi app onto their mobile phones. Of the 41 eligible participants, 16 (39%) participants were able to download the app onto their phones. If the app could not be downloaded, the participants were loaned a Lenovo© Android 11 OS platform tablet to use. Overall, eight out of 16 (50%) participants who were able to download Nthabi app on their mobile phones used the app consistently. The other eight encountered challenges related to phone memory and freezing of the phone, which leads them to uninstall the app. In total, 25 participants used the Lenovo tablets provided by the research team and eight participants on their phones (total 33).
4.3. Focus group discussions and key informant interviews
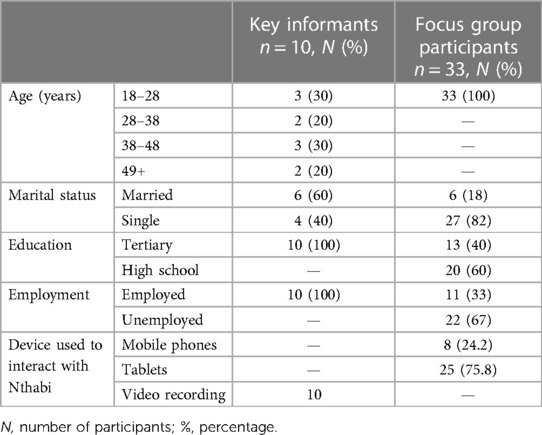
All 33 participants who used Nthabi participated in focus groups. The mean age of the participants was 23 years, and 27 (82%) of them were single. All had completed high school or above, and 22 (76%) were unemployed (Table 1). All the 10 health leaders who participated in the key informant interviews (mean age of 37.5 years) had received tertiary education and were employed (Table 1).
Table 2 summarizes the five themes and subthemes that emerged from the key informant interviews and focus group discussions.
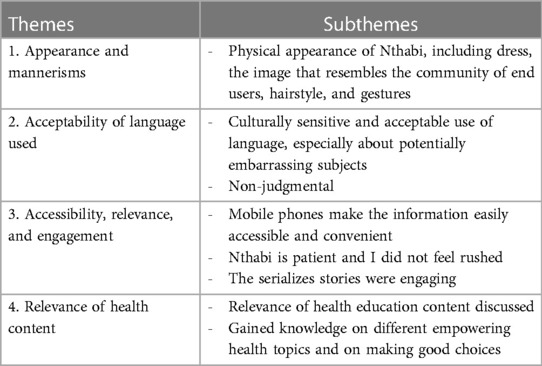
Table 2. Summary of themes and subthemes from data reported by the participants of focus groups and key informant interviews.
5. Theme 1: appearance and mannerisms
The participants described Nthabi as a Mosotho (e.g., singular Basotho) nurse who is friendly, wears her uniform neatly, and provides relevant health education to young women who do not have access to sexual and reproductive health content due to cultural and health provider barriers, such as judgmental attitudes and lack of confidentiality. The participants described Nthabi as relatable to Basotho young women.
5.1. Dress code
Both end users and MOH interview participants approved of the Nthabi character being dressed as a nurse. Wearing a nurse’s uniform implies that the information shared by Nthabi is from a reliable source.
I think she looks good, like the fact that she is a nurse, as this gives young people an assurance that the information that she is providing is credible (Key Informant 7, 43 years).
5.2. Complexion and skin tone
Most participants agreed that Nthabi's skin tone and complexion were relatable to Basotho young women:
The skin tone indeed is relatable to Basotho. Immediately you see her you definitely can say that is a Mosotho woman (Key Informant 10, 49 years).
5.3. Hairstyle
Most participants liked Nthabi's hairstyle and said that it resembled hairstyles of young Basotho women, although there were suggestions to use other styles.
I would prefer that the hair be short African hair … plaited in a way that is common in the country, it can be an essence, just a simple thing just to show that she is an African (Key Informant 8, aged 35 years).
5.4. Gestures
The gestures she used in conversation, such as using her hands, facial expressions, and the humility gesture, were viewed positively. End users and key informants agreed that Nthabi used her hands properly, and her facial expressions and the humble character that she portrayed in conversation were culturally appropriate and relatable to young Basotho women.
I was also surprised with the way the application used gestures, this is a commendable innovation. Truly, she is relatable to Basotho young women (Key Informant 9, 47 years).
6. Theme 2: acceptability of language used
Both end users and key informants appreciated that Nthabi presented information in a tone that is not offensive to the Basotho culture.
Yes, we can listen to Nthabi with our parents because she chooses her words well and that shows she is culturally sensitive. As Basotho girls, there are some words that cannot be used publicly, but Nthabi seems to know that as well (Focus group 3, participant 6, 24 years).
Nthabi is able to provide information about everything even those that a parent or elderly person isn’t comfortable talking about because they are embarrassing (Focus group 4, participant 4, 21 years).
The participants also believed that they would be comfortable sharing their healthcare needs freely with Nthabi, rather than with healthcare providers because Nthabi is non-judgmental, and they often feel judged by nurses.
I found Nthabi to be non-judgemental. For instance, say I am 18 years old and I am pregnant, there are certain things I will be told [about] how much I have been dating, etc. This results is feeling discriminated and being uncomfortable to visit the facility again … Nthabi, on the other hand, is open (Focus group 3, participant 5, 26 years).
7. Theme 3: accessibility, relevance, and engagement
Users applauded the Nthabi app since they could access it at times convenient to them rather than relying on having to go to the health center or the hospital. End users said the information provided was important, and they did not feel rushed when talking to Nthabi.
It was interesting to have a nurse in one's pocket, who is accessible anytime you want to reach out, rather than having to go through long queues at the health facilities to get health information (Focus group 1, participant 7, 22 years).
Nthabi is able to ask whether you would like to continue talking to her or if it is enough for the day, meaning she has time for us, not rushing like Nurses (Focus group 3, participant 5, 26 years).
The participants also reported that the serialized local stories motivated them to use the system every day.
The story about Thabo and Mpho made [me] more excited. I will always want to know what happens next with Mpho (Focus group 3, participant 5, 26 years).
8. Theme 4: relevance of health content
End users and key informants reported that the five health topics covered by Nthabi are relevant in Lesotho.
I learned so much about family planning. I did not know about additional methods that I learned from Nthabi (Focus group 1, participant 3, 21 years).
9. Theme 5: suggested modification
End users and key informants suggested several recommendations for additional content including HIV pre-exposure prophylaxis (PrEP), sexual reproduction, teen pregnancy, cervical cancer, and sexually transmitted infections.
It is very important to actually mention something about cervical cancer, because we know our adolescents actually start to have their sexual debut even before they reach mature age (Key informant 8, 35 years).
The majority of participants suggested that Nthabi should use the local language, Sesotho, so that information can reach the non-English speaking population. There were also suggestions with regard to her accent.
Please consider translating all this information to Sesotho, so that young people can have language options (Key informant 9, 47 years).
Nthabi's accent should also be rectified because she rolls her tongue a lot and one needs headsets in order to hear other words properly. She isn’t audible enough when you play her on speakerphone (Focus group 3, participant 3, 23 years).
Finally, the participants suggested that Nthabi could be adapted further for use by boys and young men.
I also thought the information can be appropriate for boys, please consider an application for boys as well (Key informant 9, 47 years).
10. Discussion
This study found that young women and MOH key informants in the low-middle-income country of Lesotho considered the cultural and clinical adaptation of an evidence-based embodied conversational agent system to have been successful. The clinically tailored, culturally sensitive, and trustworthy content of the Nthabi system has the potential to improve accessibility of sexual and reproductive health information in the rural, mountainous country of Lesotho in southern Africa.
Lesotho faces significant challenges in terms of its healthcare workforce capacity and the effective dissemination of health education (23). There is an urgent need to develop ways to provide trustworthy information regarding sexual and reproductive health, including family planning and condom use to reduce sexually transmitted infections, HIV, unplanned pregnancy, and unsafe abortion in Lesotho.
New technologies are now available to provide evidence-based health education to remote settings with fidelity. Conversational agent technology interactions have been shown to be an effective medium to deliver health education in a variety of topic areas, including to users with limited health literacy (24, 25). Nthabi provides a new opportunity to deliver health education, possibly as an alternative to the traditional face-to-face provision of health education (26, 27).
The study highlights the importance of adaptations of new technologies that represent the unique way of life, behaviors, beliefs, values, and symbols in the Basotho context. Once interactions are defined in relation to appropriate cultural cues, such as language, appearance, gestures, and humility, there is a higher probability of acceptability and usability (28). Substantial testing regarding Nthabi's physical appearance, age, and name was undertaken by the research teams (29).
The study demonstrates that involving stakeholders in the adaptation process can increase the acceptability of systems such as Nthabi. Community participation allowed the system to take on characteristics of the local environment in which it was developed (15, 30). The adaptations considered the language, cultural appropriateness, and context in such a way that is compatible with cultural patterns, meanings, and values of young women (21). This involvement led to incorporation of culturally persuasive features (e.g., physical characteristics, profession, use of Sesotho idioms, storytelling) and addressed issues of potential misfit among the technological, human, and contextual factors. In this way, our findings align with the findings of other studies that utilized the PEN-3 cultural utility model that promoted acceptability (31).
Nthabi's persona as a nurse, as well as the incorporation of storytelling as a persuasive feature to promote engagement, was a new innovation in the Nthabi adaptation. These characteristics were not features of the American Gabby system; however, these were recommended in Lesotho as a way to provide assurance that the health education she delivers is reliable and to promote its utilization. These stories of engagement appear to be important in enhancing user experience and encouraging long-term usage, as indicated by the majority of research findings (32).
The MOH leaders who were involved recognized the potential of this technology to provide widely scalable health education, including in population health efforts at the district or national level. Increased awareness among government officials could lead to further research, development, and facilitation of implementation assistance in the country. Focus group and interview participants expressed that expanding sexual and reproductive health education for boys should be considered in the future.
In an Australian adaptation, Gabby's ability to be sensitive to different cultures and languages seemed to be more important than her physical appearance and accent (33). In Lesotho, the participants had differing views on Nthabi's accent, as some felt it needed to be modified to sound more like the local accent. Furthermore, it was recommended that she uses the local language, which shows the necessity of harnessing local meanings and contextual factors in adapting evidence-based interventions (34).
The participants in Lesotho emphasized the importance of physical characteristics, character, hand gestures, Sesotho name, and using Sesotho words and idioms. This finding complements the findings of the study conducted by Fendt-Newlin et al. (30), which emphasized that it must be acknowledged that straightforward extrapolation of the existing evidence base is not always appropriate.
Despite the high penetration of smartphones among young women in Lesotho, only eight of the 33 participants succeeded in downloading the app onto their mobile phones, primarily due to limited memory on many phones and the unavailability of the app in the Google Play Store, especially for the latest Huawei phones, such as the P50 Pro. The research team opted to offer full downloadability of the app onto mobile phones, thereby allowing its use in non-WiFi environments in order to increase the accessibility and use of the system. The results showed that possible improved accessibility is balanced by the size of the app (particularly the speech synthesizer), which limits the downloading of the app to phones. The app could be accessed more easily if it were on the Cloud, and the participants were able to access the Internet; however, this would limit accessibility. Balancing offline accessibility and wide usage of mobile phones needs to be addressed and should be an important consideration in future developments.
This study is limited in that it was an exploratory qualitative study of users’ perceptions. The findings should be confirmed using quantitative methods, such as a survey instrument and improved knowledge acquisition. While the results reflect successful adaptation, it is not known whether the adapted Nthabi system will improve users’ health knowledge or change attitudes and behaviors. Ultimately, systems such as Nthabi will need to be tested to measure impact on important clinical outcomes.
11. Conclusion
The culturally adapted Nthabi character and trustworthy relevant content has the potential in enhancing the accessibility of sexual and reproductive health information for young women in Lesotho. Furthermore, this approach has the potential to serve as an alternative to traditional face-to-face health education methods. Suggested modifications include adopting the local language and accent and adapting Nthabi for use by boys and young men. Balancing the size of the app and accessibility in non-WiFi-enabled environments is needed in future deployments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical clearance was obtained from the Boston University Institutional Review Board (H-40268), Sefako Makgatho University Health Sciences Ethics Review Committee (H/343/2021), and the Lesotho Ministry of Health Research Ethics Committee (145-2021).
Author contributions
EN-N conceptualized the research, led cultural adaptation, conducted interviews, analyzed data, and wrote the first draft of the manuscript. MM supervised the adaptation, data collection, and analysis and contributed to manuscript writing. TB conceptualized the research, assisted with funding acquisition, led adaptation efforts, assisted with evaluation and analysis, and contributed to manuscript writing. CJ assisted with the adaptation and evaluation methodology and contributed to manuscript writing. BJ led the funding acquisition, assisted with the adaptation and analysis and contributed to manuscript writing. All authors contributed to the article and approved the submitted version.
Funding
The project was funded by the US National Institutes of Health (NIH) R21 from the Fogarty Institute; BJ (PI) 7/1/19–6/30/21, Grant Number: 1R21TW011361-01. The funder did not contribute to the research or the submission of the manuscript.
Acknowledgments
This research would not have been possible without funding from NIH R21-Forgarty Institute, involvement of the Lesotho Ministry of Health leadership, young women who participated in this study, research assistants: Paballo Lethunya and Moleboheng Mofolo, the Boston Medical Center, and the Lesotho Boston Health Alliance teams involved in this study. The authors are grateful for their participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Melesse DY, Mutua MK, Choudhury A, Wado YD, Faye CM, Neal S, et al. Adolescent sexual and reproductive health in sub-Saharan Africa: who is left behind? BMJ Glob Health. (2020) 5:e002231. doi: 10.1136/bmjgh-2019-002231
2. Rokicki S, Fink G. Assessing the reach and effectiveness of mHealth: evidence from a reproductive health program for adolescent girls in Ghana. BMC Public Health. (2017) 17:969. doi: 10.1186/s12889-017-4939-7
3. Lesotho Ministry of Health. Lesotho population-based HIV impact assessment 2020 (LePHIA 2020): Final report. Maseru: MOH (2022).
4. World Bank. Lesotho’s number of maternal deaths 1990–2015. Available at: https://www.ceicdata.com/en/lesotho/health-statistics/ls-number-of-maternal-death (Accessed April 3, 2023).
5. Ministry of Health and ICF International. Lesotho demographic and health survey 2014. Maseru: Ministry of Health and ICF International (2016).
6. Milne-Ives M, de Cock C, Lim E, Shehadeh MH, de Pennington N, Mole G, et al. The effectiveness of artificial intelligence conversational agents in health care: systematic review. J Med Internet Res. (2020) 22:e20346. doi: 10.2196/20346
7. Dingler T, Kwasnicka D, Wei J, Gong E, Oldenburg B. The use and promise of conversational agents in digital health. Yearb Med Inform. (2021) 30:191–99. doi: 10.1055/s-0041-1726510
8. Pule N. The state of ICT in Lesotho. Commissioned by the Lesotho communications authority and the International Telecommunication Union, Research ICT Africa (2016). CID: 20.500.12592/hjdh28. Available at: https://policycommons.net/artifacts/2282108/the-state-of-ict-in-lesotho-2016/3042180/ (Accessed April 3, 2023).
9. StatCounter Global Stats. Mobile operating system market share Lesotho (2020). Available at: https://gs.statcounter.com/os-market-share/mobile/lesotho/2020 (Accessed April 3, 2023).
10. Provoost S, Lau HM, Ruwaard J, Riper H. Embodied conversational agents in clinical psychology: a scoping review. J Med Internet Res. (2017) 19:e151. doi: 10.2196/jmir.6553
11. Sebastian J, Richards D. Changing stigmatizing attitudes to mental health via education and contact with embodied conversational agents. Comput Hum Behav. (2017) 73:479–88. doi: 10.1016/j.chb.2017.03.071
12. Bickmore TW, Pfeifer LM, Byron D, Forsythe S, Henault LE, Jack BW, et al. Usability of conversational agents by patients with inadequate health literacy: evidence from two clinical trials. J Health Commun. (2010) 15:197–210. doi: 10.1080/10810730.2010.499991
13. Jack B, Bickmore T, Hempstead M, Yinusa-Nyahkoon L, Sadikova E, Mitchell S, et al. Reducing preconception risks among African American women with conversational agent technology. J Am Board Fam Med. (2015) 28:441–51. doi: 10.3122/jabfm.2015.04.140327
14. Jack BW, Bickmore T, Yinusa-Nyahkoon L, Reichert M, Julce C, Sidduri N, et al. Using the Gabby health information technology system to improve the health of young African American women: a randomized controlled trial. Lancet Digit Health. (2020) 2:e475–85. doi: 10.1016/S2589-7500(20)30189-8
15. Moeini B, Rezapur-Shahkolai F, Jahanfar S, Naghdi A. Utilizing the PEN-3 model to identify socio-cultural factors affecting intimate partner violence against pregnant women in Suburban Hamadan. Health Care Women Int. (2019) 40:1212–28. doi: 10.1080/07399332.2019.1578777
16. Olufowote J, Aranda J. The PEN-3 cultural model: a critical review of health communication for Africans and African immigrants. In: Mao Y, Ahmed R, editors. Culture, migration, and health communication in a global context. New York, NY: Routledge (2018). p. 177–90.
17. Iwelunmor J, Ezeanolue EE, Airhihenbuwa CO, Obiefune MC, Ezeanolue CO, Ogedegbe GG. Socio-cultural factors influencing the prevention of mother-to-child transmission of HIV in Nigeria: a synthesis of the literature. BMC Public Health. (2014) 14:771. doi: 10.1186/1471-2458-14-771
18. Mason S, Ezechi OC, Obiezu-Umeh C, Nwaozuru U, Belue R, Airhihenbuwa C, et al. Understanding factors that promote uptake of HIV self-testing among young people in Nigeria: framing youth narratives using the PEN-3 cultural model. PLoS One. (2022) 17:e0268945. doi: 10.1371/journal.pone.0268945
19. Scarinci I, Bandura L, Hidalgo B, Cherrington A. Development of a theory-based (PEN-3 and health belief model), culturally relevant intervention on cervical cancer prevention among Latina immigrants using intervention mapping. Health Promot Pract. (2012) 13:29–40. doi: 10.1177/1524839910366416
20. Airhihenbuwa C, Okoror T, Shefer T, Brown D, Iwelunmor J, Smith E, et al. Stigma, culture, and HIV and AIDS in the Western Cape, South Africa: an application of the PEN-3 cultural model for community-based research. J Black Psychol. (2009) 35:407–32. doi: 10.1177/0095798408329941
21. Barrera M, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol. (2013) 81:196–205. doi: 10.1037/a0027085
22. Tolley EE, Ulin PR, Mack N, Robinson ET, Succop SM. Qualitative methods in public health: a field guide for applied research. Hoboken, NY: John Wiley & Sons (2016).
23. Asamani JA, Zurn P, Pitso P, Mothebe M, Moalosi N, Malieane T, et al. Health workforce supply, needs and financial feasibility in Lesotho: a labour market analysis. BMJ Glob Health. (2022) 7:e008420. doi: 10.1136/bmjgh-2021-008420
24. Sawad A B, Narayan B, Alnefaie A, Maqbool A, Mckie I, Smith J, et al. A systematic review on healthcare artificial intelligent conversational agents for chronic conditions. Sensors (Basel). (2022) 22(7):2625. doi: 10.3390/s22072625
25. Dhinagaran DA, Sathish T, Soong A, Theng Y-L, Best J, Tudor Car L. Conversational agent for healthy lifestyle behavior change: web-based feasibility study. JMIR Form Res. (2021) 5:e27956. doi: 10.2196/27956
26. Martinengo L, Jabir AI, Goh WWT, Lo NYW, Ho M-HR, Kowatsch T, et al. Conversational agents in health care: scoping review of their behavior change techniques and underpinning theory. J Med Internet Res. (2022) 24(10):e39243. doi: 10.2196/39243
27. ter Stal S, Kramer LL, Tabak M, op den Akker H, Hermens H. Design features of embodied conversational agents in eHealth: a literature review. Int J Hum Comput. (2020) 138:102409.
28. Garabiles MR, Harper Shehadeh M, Hall BJ. Cultural adaptation of a scalable World Health Organization e-mental health program for overseas Filipino workers. J Med Internet Res Form Res. (2019) 3:e11600.
29. Gardiner P, Hempstead MB, Ring L, Bickmore T, Yinusa-Nyahkoon L, Tran H, et al. Reaching women through health information technology: the gabby preconception care system. Am J Health Promot. (2013) 27:eS11–20.14. doi: 10.4278/ajhp.1200113-QUAN-18
30. Fendt-Newlin M, Jagannathan A, Webber M. Cultural adaptation framework of social interventions in mental health: evidence-based case studies from low- and middle-income countries. Int J Soc Psychiatry. (2020) 66:41–8. doi: 10.1177/0020764019879943
31. Abuwalla Z, Kadhem Z, Gladstone T, Mikhael E, Bishay A, Van Voorhees BW. Proposed model for the cultural adaptation of an Internet-based depression prevention intervention (CATCH-IT) for Arab adolescents. Int J Adolesc Med Health. (2017) 31:1–24. doi: 10.1515/ijamh-2016-0147
32. Kocaballi AB, Sezgin E, Clark L, Carroll JM, Huang Y, Huh-Yoo J, et al. Design and evaluation challenges of conversational agents in health care and well-being: selective review study. J Med Internet Res. (2022) 24(11):e38525. doi: 10.2196/38525
33. Walker R, Drakeley S, Julce C, Sidduri N, Bickmore T, Skouteris H, et al. Assessing the potential of a virtual patient advocate to provide preconception care and health advice to women living in Australia. J Dev Orig Health Dis. (2021) 12(2):300–8. doi: 10.1017/S2040174420000264
Keywords: preconception care, conversational agent technology, women’s health education, mHealth adaptation, health education in global health
Citation: Nkabane-Nkholongo E, Mokgatle M, Bickmore T, Julce C and Jack BW (2023) Adaptation of the Gabby conversational agent system to improve the sexual and reproductive health of young women in Lesotho. Front. Digit. Health 5:1224429. doi: 10.3389/fdgth.2023.1224429
Received: 17 May 2023; Accepted: 18 September 2023;
Published: 4 October 2023.
Edited by:
Maurizio Caon, University of Applied Sciences and Arts of Western Switzerland, SwitzerlandReviewed by:
Ahmet Fatih Durmusoglu, Istanbul Medipol University, TürkiyeIvan Miguel Pires, Universidade da Beira Interior, Portugal
© 2023 Nkabane-Nkholongo, Mokgatle, Bickmore, Julce and Jack. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth Nkabane-Nkholongo ZWxpemFiZXRoLm5raG9sb25nb0BnbWFpbC5jb20=
 Elizabeth Nkabane-Nkholongo
Elizabeth Nkabane-Nkholongo Mathildah Mokgatle1
Mathildah Mokgatle1