
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Digit. Health , 27 September 2022
Sec. Health Informatics
Volume 4 - 2022 | https://doi.org/10.3389/fdgth.2022.958539
This article is part of the Research Topic Artificial Intelligence for Human Function and Disability View all 5 articles
 Sunyang Fu1
Sunyang Fu1 Maria Vassilaki2
Maria Vassilaki2 Omar A. Ibrahim1
Omar A. Ibrahim1 Ronald C. Petersen2,3
Ronald C. Petersen2,3 Sandeep Pagali4
Sandeep Pagali4 Jennifer St Sauver2
Jennifer St Sauver2 Sungrim Moon1
Sungrim Moon1 Liwei Wang1
Liwei Wang1 Jungwei W. Fan1,2
Jungwei W. Fan1,2 Hongfang Liu1
Hongfang Liu1 Sunghwan Sohn1*
Sunghwan Sohn1*
The secondary use of electronic health records (EHRs) faces challenges in the form of varying data quality-related issues. To address that, we retrospectively assessed the quality of functional status documentation in EHRs of persons participating in Mayo Clinic Study of Aging (MCSA). We used a convergent parallel design to collect quantitative and qualitative data and independently analyzed the findings. We discovered a heterogeneous documentation process, where the care practice teams, institutions, and EHR systems all play an important role in how text data is documented and organized. Four prevalent instrument-assisted documentation (iDoc) expressions were identified based on three distinct instruments: Epic smart form, questionnaire, and occupational therapy and physical therapy templates. We found strong differences in the usage, information quality (intrinsic and contextual), and naturality of language among different type of iDoc expressions. These variations can be caused by different source instruments, information providers, practice settings, care events and institutions. In addition, iDoc expressions are context specific and thus shall not be viewed and processed uniformly. We recommend conducting data quality assessment of unstructured EHR text prior to using the information.
The rapid adoption of electronic health record (EHR) systems has enabled the secondary use of EHR data for large-scale research discovery, real-time decision support, and data-driven workflow optimization. Unstructured text that represents a large portion of EHR data contains essential information to comprehensively represent a patient's phenotypic profile. Common types of unstructured text include clinical notes (e.g., progress, consultation, admission/discharge summary), radiology reports, pathology reports, and microbiology reports. Since the HITECH Act of 2008, there have been an increasing number of studies that use EHR text to enrich patient information in the areas of incidental findings (1), diseases and conditions with multi-factorial causes (2, 3), diseases and conditions with no singular and conclusive diagnostic tests (4), surgical information(4, 5), and social determinants of health (6). These examples strongly suggest that text information can drastically improve the discovery and detection of conditions that are not routinely coded and/or are underdiagnosed in clinical practice.
A traditional method of utilizing text from EHR systems is manual chart review, a human-assisted process of reviewing, screening, or abstracting textual information. However, this method has been criticized for being labor-intensive and time-consuming (7–10). To facilitate the large-scale secondary use of EHR text, natural language processing (NLP) has been leveraged to automatically retrieve and extract clinical information. Information retrieval for eligibility screening or cohort identification (11, 12) and information extraction for assembling clinical data sets (8, 13–18) have been widely used in EHR-based NLP applications.
Despite the promising potential, the secondary use of EHRs for developing NLP applications faces challenges in the form of varying data quality-related issues. Because EHR systems are primarily designed for patient care, the documentation of text data is affected by numerous contextual factors, including human factors, clinical environment (e.g., in-patient vs. out-patient), and practice guidelines (19–21). On one hand, the EHR system itself has a significant impact on the form and format of clinical text. The unstructured EHR text is comprised of multiple information sources such as progress reports, consultation notes, nursing flowsheets, and patient provided information. Particularly, during the information collection and documentation process, instruments such as questionnaires and templates can have a huge influence on the characteristics of clinical text. On the other hand, Built-in documentation functionality such as SmartForms (i.e., customizable text template for Epic EHR documentation), auto-population, and transcription can affect the EHR-specific syntactic and semantic definition for any data contained therein (22, 23). In our study, we define language derived from unstructured or semi-structured instruments including templates, questionnaires, assessment forms, and smart forms as instrument-assisted documentation (iDoc) expressions.
Existing studies have indicated an increasing occurrence of iDoc expressions in EHRs, which can significantly impact information redundancy and quality (24–26). However, there is a lack of systematic understanding of the data quality of these expressions as well as their downstream impact on the development, evaluation and deployment of NLP applications in single and multi-site EHR environments (19). To further investigate and quantify the text data quality issues caused by iDoc expressions and the heterogeneous EHR environments, we conducted a case study examining the availability of information on functional status focused on activities of daily living (ADL) in the EHRs of persons participating in the Mayo Clinic Study of Aging (MCSA) (27).
Due to the need to understand both context (e.g., how does this pattern occur?) and scope (e.g., degree and prevalence of different quality patterns), we used a convergent parallel design, a type of mixed-methods design that emphasizes concurrently collecting qualitative and quantitative data and independently analyzes findings, to assess the textual data quality across institutions. The study design is presented in Figure 1 and summarizes four sequential tasks: (1) contextual understanding of narrative documentation, (2) identification of instrument-assisted documentation, (3) assessment of information quality and (4) examining implications for NLP applications.
This study was approved by the Mayo Clinic and the Olmsted Medical Center Institutional Review Boards. We explored EHRs for participants from the MCSA (27), a population-based cohort study of cognitive aging with comprehensive periodic cognitive assessments, initiated in 2004. The cohort comprises 6,185 unique participants, free of dementia at the study baseline. Among these, 3,070 patients were female (49.6%) and 729 patients (11.6%) have progressed to dementia. The median age of the cohort is 73. The study cohort comprised a total of 673 patients randomly sampled from the MCSA cohort. In the sampled cohort, patients' visit times ranged from December 2004 to February 2020. Three institutions were included in the study: a tertiary care, nonprofit, and academic medical center (institution 1), a network of community-based health systems (institution 2), and a nonprofit community-based hospital (institution 3). Regarding the changes of EHR systems, Institution 1 converted its EHR system from GE Centricity to Epic in 2018, Institution 2's EHR system was converted from Cerner to Epic in 2017, and Institution 3's EHR system was converted from IC chart and Cerner to Epic in 2018.
As EHR system functionality and information documentation patterns are deeply embedded within the clinical workflow and practice, the quality of data needs to be examined for the given context (e.g., clinical setting and information documentation environment). Individual interview sessions were organized to understand the overall documentation process of patient functional status information. Interviews were conducted utilizing the snowball sampling method for recruiting participants from institution 1. Seven participants were enrolled including two geriatricians, one neurologist, three nurses, and one physical therapist. We applied contextual inquiry methods for collecting feedback. Findings were synthesized through thematic analysis.
Four consecutive steps were involved to identify the iDoc patterns: (1) identification of ADL expressions, (2) measuring textual similarity of ADL expressions, (3) manually reviewing iDoc expressions with high similarity scores, and 4) developing symbolic methods to automatically identify iDoc expressions. First, we performed corpus annotation, a task of highlighting descriptive or analytic notations applied to raw language data, to systematically identify functional status-related expressions (i.e., ADL related expressions). We used the definitions based on the International Classification of Functioning, Disability and Health (ICF) (28) to develop an annotation guideline. An iterative consensus development process was conducted involving an experienced nurse abstractor, a neurologist, three epidemiologists, and two informaticians. The annotation was performed on clinical notes. Common note types for clinical notes include visit notes, discharge summaries, physical activity reports, psychiatry reports, PT/OT consultation notes, etc., which were all included in the study. The functional status expressions related to basic activities of daily living (bADL) and instrumental activities of daily living (iADL) were manually extracted from three cohorts (randomly sampled from MCSA participants) from three institutions. Second, to identify iDoc patterns, we examined the language variation of the outputs (i.e., identified ADL expressions) from the previous step using corpus statistics and semantic textual similarity (STS) among the previously annotated ADL expressions. The measurement of STS was based on a string-matching algorithm proposed by Ratcliff and Obershelp, cosine similarity of two-word vector space, and Levenshtein distance (29–31). The method was utilized and evaluated in the 2018 BioCreative/OHNLP clinical semantic textual similarity challenge (30). A high similarity sentence pair is determined when the average score was greater or equal to 0.30. Third, based on the STS results, two trained nurse abstractors manually reviewed expressions with high similarity scores and identified iDoc-related expressions using existing questionnaire instrument forms (e.g., MC PROMIS CAT V2.0-Cognitive Function and MC PROMIS CAT V2.0 - Physical Function) as reference standards. The agreement between the two annotators was 0.907 in f1-score. Lastly, we developed symbolic methods based on manual annotation to automatically identify these iDoc expressions using an open-source information extraction system MedTaggerIE (32, 33). We then ran MedTaggerIE against the entire MCSA cohort with total of 6,185 unique patients across three sites.
The definitions of information quality and evaluation methods were adopted from our previous study based on the AIM quality (AIMQ) framework (34, 35). We defined three measurements for assessing intrinsic information quality (accuracy) of iDoc-related expressions of patient functional status (i.e., bADL and iADL): (1) agreement (f1-score) between two iDoc expressions that have similar semantic meaning and occur within the same clinical document (e.g., “Have difficulty dressing: No” vs. “Dressing: Independent”), (2) clinical diagnosis of mild cognitive impairment (MCI) to measure the association between iDoc functional status information and MCI diagnosis, and (3) clinical diagnosis of dementia to measure the association between iDoc functional status information and dementia diagnosis. MCI and dementia diagnoses were ascertained during the MCSA evaluations. MCI was diagnosed according to published criteria (36) and dementia was diagnosed according to DSM-IV criteria (37). For cases (patients with MCI or dementia diagnosis), clinical documents were selected prior to the index diagnosis date of MCI or dementia. For controls, there was no time constraint for document selection. The intrinsic information quality of iDoc expressions (i.e., (2) and (3)) was assessed using positive predicted value (PPV) and negative predicted value (NPV), where true positive is considered to be MCI or dementia patients with positive iDoc expressions (i.e., functional impairment) and false positive is considered to be patients with positive iDoc expressions but no formal diagnosis of MCI or dementia during the study period. Similarly, the NPV was used to examine the quality of negative iDoc expressions such as “no functional impairment”. We further quantified the contextual information (i.e., distribution of iDoc expressions) in different clinical document sections, event types, and hospital services.
To understand the downstream implication of various iDoc expressions in the development, evaluation, and deployment of NLP applications for cohort-based discoveries, we summarized iDoc expressions in three syntactic representations and evaluated their impact. We ran MedTaggerIE to identify ADL-related mentions using the following scenarios: lexicon, context (ConText algorithm 38), pattern (i.e., complex rule), and section-based approach (SecTag algorithm 39). Error analysis was conducted to understand the result of each approach. We then qualitatively evaluated the implications of each iDoc expression for NLP pipelines: preprocessing pipeline, section detector, sentence detector, and context algorithm. False positive and negative cases predicted by the MedTaggerIE were manually reviewed. During the review, we manually annotated the error types including linguistics, logic, and context based on the definition from our previous review study. The process is assisted by two trained nurse abstractors (B.A.L., D.C.O.) and supervised by an informatician (S.F.).
Figure 2 shows the overall functional status (i.e., ADL) documentation process. The qualitative thematic analysis indicates that the primary contributors to functional status documentation in clinical notes are physical and occupational therapists (PT/OT), followed by nurses, speech therapists, and nutritionists. PTs and OTs are trained to use standardized template-based documentation, smart phrases, and dictation. Findings from the PT/OT notes were based on objective measurements of functional goals. However, the documentation patterns may be heavily affected by billing practices. Nursing staff members are advised to perform routine screening to collect functional status information on the day of patients' admission. However, we learned that ADL screening and measurement can vary by care settings and patient characteristics; thus, the information may not be routinely captured. In addition, the information is stored in an independent data source (flowsheet) rather than clinical notes and indicates a need for information integration. The primary care providers (PCPs) and specialists routinely ask about patients' history of ADL information and provide only limited narrative comments. It is probable that there are also different standards and practice variations between specialists and PCPs in the evaluation and diagnosis of ADL-related conditions such as MCI and dementia.
Table 1 provides the overall summary statistics of the cohort across three sites. The distribution of the unique ADL expressions from Figure 3 revealed variant patterns of frequency distribution and language variation (STS score and IQR) across three sites and suggested that institution 2 and institution 1 have more iDoc expressions than institution 3. On the other hand, institution 3 has a more descriptive and cohesive documentation style indicated by the frequency distribution (e.g., less skewed to the left). Based on the chart review, we confirmed that institution 3 had little-to-no instrument-assisted documentation patterns. Four major types of iDoc patterns were identified and presented below. The iDoc expressions i and ii are represented by a standard assertion pattern such as “able to complete” or “unable to complete” follow by inserting a standard list of events (e.g., bathing, feeding, and dressing). iDoc (iii) contains the combination of a question-and-answer format and an ADL item list. iDoc (iv) is represented by a set of standardized value sets.
iDoc (i) Institution 1 - GE Centricity (n = 12,582):
Activities of Daily Living: The patient/caregiver reports being able to complete the following tasks on their own: Preparing meals, feeding themselves, dressing, using the toilet, housekeeping, bathing, walking, using transportation, getting in/out of bed, and managing medications.
iDoc (ii) Institution 1 - GE Centricity (n = 40):
PATIENT NEEDS ASSISTANCE WITH THE FOLLOWING INSTRUMENTAL ACTIVITIES OF DAILY LIVING: meal preparation, medication administration, telephone use, housekeeping, shopping, managing finances, transportation use (drive car/use taxi/bus).
iDoc (iii) Institution 1 – Epic (n = 173):
Do you have serious difficulty walking or climbing stairs? Yes 04/25/2022
Do you have difficulty dressing or bathing? No 04/25/2022
• Dressing: Independent
• Bathing: Independent
• Grooming: Independent
• Toileting: Independent
• Feeding: Independent
iDoc (iv) Institution 2 – Cerner (n = 723):
PT Goals:
Bed Mobility Goal: Moderate assistance Time Frame to Reach Bed Mobility Goal: 7-day(s) Bed Mobility Goal Status: Transfer Goal: Maximal assistance Transfer Device: Other: Time Frame to Reach Transfer Goal: 7-day(s) Transfer Goal Status: Ambulation Goal: Ambulation…
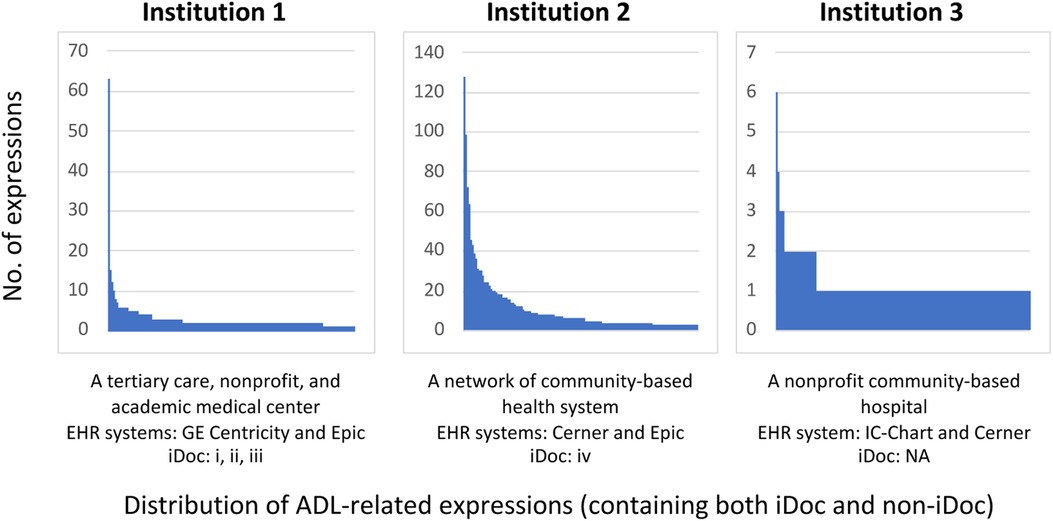
Figure 3. Distribution of ADL expressions in EHR documents across different institutions from the sampled annotation cohorts.
The distinct difference among different iDoc expressions suggests that they should not be uniformly viewed and processed. Some iDoc expressions can be more informative than others depending on the goal of the study. Although iDoc (i) has a high prevalence and is repetitively documented within the MCSA cohort, it can be directly used with high validity to inform patients' functional status. By contrast, iDoc (iv) is less informative without the contextual understanding of PT/OP templates and thus has limited contribution to capturing actual patients' functional status. Among four different types of iDoc expressions, we found three different syntactic representations due to the different sources (e.g., Epic smart form, questionnaire, and PT/OT templates). The question-and-answer format and PT/OT templates have a lower degree of naturality (i.e., closer to semi-structured format) than smart forms. iDoc (iii) and iDoc (iv) expressions were represented by multiple sentence fragments and posed potential challenges for sentence-level NLP models.
Among the 714 patients with iDoc (i) expressions, the PPV for MCI and dementia are 0.735 and 0.874, respectively. Among the 3,244 patients with iDoc (ii) expressions, the NPV for non-MCI and non-dementia are 0.883 and 0.980, respectively. The agreement between two semantically similar iDoc (iii) expressions (“Do you have difficulty dressing? No” and “Dressing Independent” occurred within the same clinical document) is 0.963 in f1-score. The quality of iDoc (iv) was not assessed due to lacking a direct semantic contribution to the overall patient's functional status.
The hospital services present a higher level of heterogeneity among the four iDoc expressions. The unique number of hospital services for iDoc (i) to (iv) were 47, 183, 3, and 3 respectively. Among them, “Primary Care Internal Medicine” and “Family Medicine” were the most frequent visit types across all iDoc expressions. Regarding the event type analysis, we found 21 unique event types for iDoc (i). “Limited exam” (50%) and “Multi-system Evaluation” (38%) were the two primary events. The iDoc (ii) has 11 unique event types. The primary types include “Dismissal Summary” (76%) and “Initial Discharge Planning Assessment” (14%). Two distinct event types were found for iDoc (iii): “Progress” (81%) and “History and Physical Exam” (19%). iDoc (iv) expressions has two event types: Physical therapy progress order text (22%) and Physical therapy daily notes text (78%). The section analysis identified that iDoc (i) expressions were all based on the “System Reviews” (100%) section. We found 10 unique sections for iDoc (ii) expressions including “Instructions for continuing care” (48%), “Ongoing Care Orders” (28%), “System Reviews” (16%), and “Impression/Report/Plan” (6%). Similar to iDoc (i), iDoc (iii) expressions were uniformly based on “Social History” (98%) section. We found no sections to be mapped for iDoc (iv) expressions.
In ADL expressions, the three instrument types (EHR system Smart form, Questionnaire form, and PT/OT template) showed a decreasing level of naturality of language where the smart form has the highest naturality and the PT/OP template presents a semi-structured format. The overall evaluation results of preprocessing pipeline, section detector, sentence detector, and context algorithm are illustrated in Table 2. Regarding an NLP approach to identity iDoc ADL expressions, the traditional lexicon-based approach (only using keywords) failed to identify all three instrument types. After adding the context component, the out-of-box context algorithm (assertion detection algorithm) failed to correctly determine the certainty (e.g., negated, confirmed) in the questionnaire form because the default information extraction system processes information at the sentence level. Both the questionnaire form and PT/OP template require the linkage of findings across two or more sentences to correctly determine assertion status. In addition, they also have a strong impact on both the sentence detector and context algorithm and thus require a necessary pre-processing step. By contrast, the smart form representation kept a high level of naturality of language and has minimal impact on the existing clinical information extraction pipeline (i.e., no negative impact of the section, sentence, and context algorithms). Overall, it is evident that different representations of iDoc expressions have significant implications for existing clinical information extraction applications.
Our study applied a set of qualitative and quantitative methods to systematically assess the information quality of instrument-assisted documentation (iDoc expressions) across three different institutions. Four prevalent iDoc expressions were identified based on three distinct instruments: Epic smart form, questionnaire, and PT/OT templates. We found significant differences in the usage, information quality (intrinsic and contextual), and naturality of language among the different types of iDoc expressions. These variations are impacted by different source instruments, information providers, practice settings, care events, and institutions. Details in each aspect are as follows:
The contextual inquiry revealed a dynamic, complex, and heterogeneous documentation process. Based on the interview, we discovered that the care practice teams, EHR systems, and institutions all play a significant role in how text data is documented and organized. Patient narratives are comprised of multiple different sources of information such as patients, PTs/OTs, nurses, speech therapists, nutritionists, primary care providers, and specialists. In NLP applications, information documentation and generation processes can affect the development and generalization of the models. Although the use of instruments may enhance documentation standardization, the clinician's reasoning process may be eliminated and resulted in a varying level of contextual knowledge loss. In addition, the highly variable results across three sites strongly indicated that a proper model re-training, refinement, and re-evaluation are needed.
The validity of clinical narratives is crucial for the secondary use of EHR data for the development of robust NLP models. Based on our intrinsic information quality assessment, we discovered a moderate-high validity of iDoc-related expressions. This finding suggests that iDoc expressions can be directly utilized for case ascertainment or common data elements in the context of this case study. However, we were able to identify conflicts amongst iDoc expressions with similar semantic meanings occurring within the same document. For example, the following expressions on the right indicate the patient's both positive and negative statuses of the ability to dress and bath: “Do you have difficulty dressing or bathing? (5 years or older) Yes; Dressing Independent; Bathing Independent.” We believe that such conflict may be introduced during the data collection, particularly from patient-provided questionnaires. This finding affirms that in the context of secondary use, proper data quality assessment needs to be conducted prior to the information use.
The contextual information quality revealed informative contextual information for three out of four iDoc expressions. There was only a little overlap between these identified contexts among different institutions, suggesting the pattern of iDoc documentation is context specific. We also found different practices and frequencies of instrument-assisted documentation patterns across different institutions. Both institution 1 and institution 2 have heavy usage of instrument-assisted documentation for ADL mentions while institution 3 does not have iDoc expression. There is also high heterogeneity in instrument-assisted documentation between institution1 and institution 2. Our finding raises a potential issue regarding NLP algorithm portability (i.e., the ability to successfully deploy an existing NLP solution to a different environment and achieve “similar enough” results after proper system refinement) to extract ADL information from EHR text due to intrinsic documentation differences. The adoption of different instruments for patient data collection can exacerbate challenges of NLP algorithm portability, especially when using instrument-specific symbolic NLP methods. Statistics-based sub-language analysis can be considered to alleviate these challenges.
Because the quality of information is context specific, we recommend applying information quality assessments prior to any practices of information use. Four different information quality (IQ) assessments can be applied in the context of the secondary use of EHRs based on the AIMQ framework (34, 40). The framework summarized four distinct IQ dimensions: accessibility IQ, intrinsic IQ, representational IQ, and contextual IQ. These dimensions can be translated into the context of secondary use of clinical documents. The following types of quality assessment methods can be considered: clinical document accessibility (accessibility IQ), documentation completeness (contextual IQ), documentation accuracy (intrinsic IQ), and syntactic and semantic variability of clinical language (representational IQ). Clinical document accessibility can be evaluated by analyzing the information accessibility and shareability (system and method) based on different EHR settings such as intra-institution or inter-institution. In our previous study, we defined four levels of accessibility to measure the shareability of information resources across different institutions including direct access, adaptive access, partial access, and no access. Documentation completeness measures a record containing all observations made about a patient (41). Examining documentation completeness can be achieved by assessing the availability of clinical notes upon a clinical encounter. If the information is both accessible and complete, researchers can now focus on the validity of the information, which can be evaluated by comparing a particular clinical concept such as iADL with one or more reference sources. For example, the documentation of MCI-related symptoms can be found in clinical notes, nursing flowsheets, and patient-provided information. Lastly, language variability plays a significant role in NLP system portability. The form and format of clinical language can be assessed through corpus statistics and clinical textual similarity measures (35). These information quality assessments are agnostic among healthcare settings and could be applied in other settings.
Since we only interviewed clinicians from institution 1 due to the recruitment challenges, identified documentation practices and workflow may not be fully representative of the broader healthcare setting. In addition, since the study was conducted on three sites with a single case scenario, the generalizability of the finding is limited by the designed scope. Specifically, an institution that does not have standard guidelines and routine practices for research-level data abstraction may find it difficult to establish reference standards. In the future study, we aim to collaborate with national data consortiums such as National COVID Cohort Collaborative (N3C) and Observational Health Data Sciences and Informatics (ODHSI) to share established standard operating procedures and best practices for quality assessment. We would also like to broaden the study scope by involving more institutions and case studies.
Our study applied a set of quality assessment methods to systematically examine the information quality of instrument-assisted documentation across three different institutions. We discovered a varying level of textual information documentation patterns across three institutions, the presence of semantic conflict within clinical text, and the context-specific iDoc presentations. Our study demonstrated that the quality of EHR data is closely related to the documentation workflow, stakeholders, and the functionality of individual EHR systems and thus needs to be viewed from the context of data being generated and documented. The finding affirms that data quality assessment needs to be conducted prior to the information use. These variant iDoc expressions have strong implications for NLP models. Therefore, proper model re-training, refinement, and re-evaluation are needed for a multi-institutional environment. We also discussed our recommendations for applying quality assessment methods (e.g., statistics-based sub-language analysis) for the secondary use of EHR text data. These efforts can be considered to develop and implement robust downstream applications using functional status.
The datasets presented in this article are not readily available because they contain protected health information. Requests to access the datasets should be directed to the corresponding author.
This study was approved by the Mayo Clinic and the Olmsted Medical Center Institutional Review Boards.
All co-authors are justifiably credited with authorship, according to the authorship criteria. All authors read and approved the final manuscript. In detail: SS and SF- design, development, data collection, analysis of data, interpretation of results, drafting and revision of the manuscript; All authors- critical revision of the manuscript; SS and SF - conception, design, analysis of data, interpretation of results, critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
The study was supported by National Institution of Aging (R01 AG068007 and R01 AG072799). The Mayo Clinic Study of Aging was supported by the NIH (U01 AG006786, P30 AG062677, R37 AG011378, R01 AG041851), the Alexander Family Alzheimer's Disease Research Professorship of the Mayo Clinic, GHR, Mayo Foundation for Medical Education and Research, the Liston Award, the Schuler Foundation and was made possible by the Rochester Epidemiology Project (R01AG034676).
The authors would like to gratefully acknowledge Brenda A Lee and Deborah C Olson for annotation.
Maria Vassilaki has received research funding from F. Hoffmann-La Roche Ltd and Biogen in the past and consults for F. Hoffmann-La Roche Ltd; she receives research funding from NIH and has equity ownership in Abbott Laboratories, Johnson and Johnson, Medtronic, AbbVie and Amgen. RCP is a consultant for Roche, Inc., Biogen, Inc., Merck, Inc., Eisai, Inc., Genentech, Inc. and Nestle, Inc.; receives publishing royalties from Mild Cognitive Impairment (Oxford University Press, 2003), UpToDate and receives research support from the National Institute of Health.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Fu S, Leung LY, Wang Y, Raulli A-O, Kallmes DF, Kinsman KA, et al. Natural language processing for the identification of silent brain infarcts from neuroimaging reports. JMIR Med Inform. (2019) 7(2):e12109. doi: 10.2196/12109
2. Fu S, Lopes GS, Pagali SR, Thorsteinsdottir B, LeBrasseur NK, Wen A, et al. Ascertainment of delirium status using natural language processing from electronic health records. J Gerontol: Series A. (2020) 77(3):524–30. doi: 10.1093/gerona/glaa275
3. Inouye SK, Westendorp RG, Saczynski JS, Kimchi EY, Cleinman AA. Delirium in elderly people–Authors’ reply. The Lancet. (2014) 383(9934):2045. doi: 10.1016/S0140-6736(14)60994-6
4. Fu S, Wyles CC, Osmon DR, Carvour ML, Sagheb E, Ramazanian T, et al. Automated detection of periprosthetic joint infections and data elements using natural language processing. J Arthroplasty. (2021) 36(2):688–92. doi: 10.1016/j.arth.2020.07.076
5. Tibbo ME, Wyles CC, Fu S, Sohn S, Lewallen DG, Berry DJ, et al. Use o natural language processing tools to identify and classify periprosthetic femur fractures. J Arthroplasty. (2019) 34(10):2216–9. doi: 10.1016/j.arth.2019.07.025
6. Bennett LM, Gadlin H. Collaboration and team science: from theory to practice. J Invest Med. (2012) 60(5):768–75. doi: 10.2310/JIM.0b013e318250871d
7. Kaur H, Sohn S, Wi CI, Ryu E, Park MA, Bachman K, et al. Automated chart review utilizing natural language processing algorithm for asthma predictive index. BMC Pulm Med. (2018) 18(1):34. doi: 10.1186/s12890-018-0593-9
8. Wang Y, Wang L, Rastegar-Mojarad M, Moon S, Shen F, Afzal N, et al. Clinical information extraction applications: a literature review. J Biomed Inform. (2018) 77:34–49. doi: 10.1016/j.jbi.2017.11.011
9. Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. (1996) 27(3):305–8. doi: 10.1016/S0196-0644(96)70264-0
10. Fu S, Carlson LA, Peterson KJ, Wang N, Zhou X, Peng S, et al. Natural language processing for the evaluation of methodological standards and best practices of EHR-based clinical research. AMIA Summits Transl Sci Proc. (2020) 2020:171–80. PMID: 32477636; PMCID: PMC7233049
11. Chute CG, editor. The horizontal and vertical nature of patient phenotype retrieval: new directions for clinical text processing. Proceedings of the AMIA symposium; American Medical Informatics Association (2002).
12. Kaggal VC, Elayavilli RK, Mehrabi S, Pankratz JJ, Sohn S, Wang Y, et al. Toward a learning health-care system–knowledge delivery at the point of care empowered by big data and NLP. Biomed Inform Insights. (2016) 8:BII. S37977. doi: 10.4137/BII.S37977
14. Nadeau D, Sekine S. A survey of named entity recognition and classification. Lingvisticae Investigationes. (2007) 30(1):3–26. doi: 10.1075/li.30.1.03nad
15. Marsh E, Perzanowski D. Seventh message understanding conference (MUC-7): proceedings of a conference held in fairfax. MUC-7 evaluation of IE technology: overview of results; April 29-May 1, 1998; Virginia (1998).
16. Torii M, Wagholikar K, Liu HF. Using machine learning for concept extraction on clinical documents from multiple data sources. J Am Med Inform Assoc. (2011) 18(5):580–7. doi: 10.1136/amiajnl-2011-000155
17. Si Y, Wang J, Xu H, Roberts K. Enhancing clinical concept extraction with contextual embeddings. J Am Med Inform Assoc. (2019) 26(11):1297–304. doi: 10.1093/jamia/ocz096
18. Fu S, Chen D, He H, Liu S, Moon S, Peterson KJ, et al. Clinical concept extraction: a methodology review. J Biomed Inform. (2020) 109:103526. doi: 10.1016/j.jbi.2020.103526
19. Fu S, Leung LY, Raulli A-O, Kallmes DF, Kinsman KA, Nelson KB, et al. Assessment of the impact of EHR heterogeneity for clinical research through a case study of silent brain infarction. BMC Med Inform Decis Mak. (2020) 20(1):1–12. doi: 10.1186/s12911-019-1002-x
20. Sohn S, Wang Y, Wi C-I, Krusemark EA, Ryu E, Ali MH, et al. Clinical documentation variations and NLP system portability: a case study in asthma birth cohorts across institutions. J Am Med Inform Assoc. (2018) 25(3):353–9. doi: 10.1093/jamia/ocx138
21. Cohen GR, Friedman CP, Ryan AM, Richardson CR, Adler-Milstein J. Variation in physicians’ electronic health record documentation and potential patient harm from that variation. J Gen Intern Med. (2019) 34(11):2355–67. doi: 10.1007/s11606-019-05025-3
22. Zhang R, Pakhomov S, McInnes BT, Melton GB, editors. Evaluating measures of redundancy in clinical texts. AMIA Annual symposium proceedings; American Medical Informatics Association (2011).
23. Thaker VV, Lee F, Bottino CJ, Perry CL, Holm IA, Hirschhorn JN, et al. Impact of an electronic template on documentation of obesity in a primary care clinic. Clin Pediatr (Phila). (2016) 55(12):1152–9. doi: 10.1177/0009922815621331
24. Searle T, Ibrahim Z, Teo J, Dobson R. Estimating redundancy in clinical text. J Biomed Inform. (2021) 124:103938. doi: 10.1016/j.jbi.2021.103938
25. Cohen R, Elhadad M, Elhadad N. Redundancy in electronic health record corpora: analysis, impact on text mining performance and mitigation strategies. BMC Bioinformatics. (2013) 14(1):1–15. doi: 10.1186/1471-2105-14-10
26. Wrenn JO, Stein DM, Bakken S, Stetson PD. Quantifying clinical narrative redundancy in an electronic health record. J Am Med Inform Assoc. (2010) 17(1):49–53. doi: 10.1197/jamia.M3390
27. Roberts RO, Geda YE, Knopman DS, Cha RH, Pankratz VS, Boeve BF, et al. The mayo clinic study of aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. (2008) 30(1):58–69. doi: 10.1159/000115751
28. Üstün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The international classification of functioning, disability and health: a new tool for understanding disability and health. Disabil Rehabil. (2003) 25(11-12):565–71. doi: 10.1080/0963828031000137063
30. Wang Y, Afzal N, Fu S, Wang L, Shen F, Rastegar-Mojarad M, et al. MedSTS: a resource for clinical semantic textual similarity. Lang Resour Eval. (2020) 54(1):57–72. doi: 10.1007/s10579-018-9431-1
31. Singhal A. Modern information retrieval: a brief overview. IEEE Data Eng Bull. (2001) 24(4):35–43.
32. Wen A, Fu S, Moon S, El Wazir M, Rosenbaum A, Kaggal VC, et al. Desiderata for delivering NLP to accelerate healthcare AI advancement and a Mayo Clinic NLP-as-a-service implementation. NPJ Digit Med. (2019) 2(1):1–7. doi: 10.1038/s41746-018-0076-7
33. Liu H, Bielinski SJ, Sohn S, Murphy S, Wagholikar KB, Jonnalagadda SR, et al. An information extraction framework for cohort identification using electronic health records. AMIA Summits Transl Sci Proc. (2013) 2013:149.24303255
34. Lee YW, Strong DM, Kahn BK, Wang RY. AIMQ: a methodology for information quality assessment. Info Manage. (2002) 40(2):133–46. doi: 10.1016/S0378-7206(02)00043-5
35. Fu S, Wen A, Schaeferle GM, Wilson PM, Demuth G, Ruan X, et al., editors. Assessment of data quality variability across two EHR systems through a case study of post-surgical complications. AMIA Annual symposium proceedings; American Medical Informatics Association (2022).
36. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. (2004) 256(3):183–94. doi: 10.1111/j.1365-2796.2004.01388.x
37. Association AP. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association (1994).
38. Chapman WW, Bridewell W, Hanbury P, Cooper GF, Buchanan BG. A simple algorithm for identifying negated findings and diseases in discharge summaries. J Biomed Inform. (2001) 34(5):301–10. doi: 10.1006/jbin.2001.1029
39. Denny JC, Spickard A III, Johnson KB, Peterson NB, Peterson JF, Miller RA. Evaluation of a method to identify and categorize section headers in clinical documents. J Am Med Inform Assoc. (2009) 16(6):806–15. doi: 10.1197/jamia.M3037
40. Fu S, Wen A, Pagali S, Zong N, St Sauver J, Sohn S, et al. The implication of latent information quality to the reproducibility of secondary use of electronic health records. Stud Health Technol Inform. (2022) 290:173–7.35672994
Keywords: information quality, electronic health records, natural language processing, functional status (activity levels), aging
Citation: Fu S, Vassilaki M, Ibrahim OA, Petersen RC, Pagali S, St Sauver J, Moon S, Wang L, Fan JW, Liu H and Sohn S (2022) Quality assessment of functional status documentation in EHRs across different healthcare institutions. Front. Digit. Health 4:958539. doi: 10.3389/fdgth.2022.958539
Received: 31 May 2022; Accepted: 5 September 2022;
Published: 27 September 2022.
Edited by:
Suzanne Roberta Tamang, Stanford University, United StatesReviewed by:
Sergey Blok, Booz Allen Hamilton (United States), United States© 2022 Fu, Vassilaki, Ibrahim, Petersen, Pagali, St Sauver, Moon, Wang, Fan, Liu and Sohn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sunghwan Sohn c29obi5zdW5naHdhbkBtYXlvLmVkdQ==
Specialty Section: This article was submitted to Health Informatics, a section of the journal Frontiers in Digital Health
Abbreviations EHR, Electronic Health Record; MCSA, Mayo Clinic Study of Aging; iDoc, instrument-assisted Documentation; NLP, Natural Language Processing; ADL, Activities of Daily Living; bADL, basic Activities of Daily Living; iADL, instrumental Activities of Daily Living; STS, semantic textual similarity; MCI, mild cognitive impairment; PPV, positive predicted value; NPV, negative predicted value; PT/OT, physical and occupational therapists; PCPs, primary care providers; IQR, interquartile range
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.