- 1Department of Psychology, College of Science, Northeastern University, Boston, MA, United States
- 2Center for Cognitive and Brain Health, Northeastern University, Boston, MA, United States
- 3Department of Medical Sciences, School of Clinical and Rehabilitation Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, MA, United States
- 4Department of Communication Sciences and Disorders, School of Clinical and Rehabilitation Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, MA, United States
- 5Department of Sport Psychology and Human Movement Science, University of Stuttgart, Stuttgart, Germany
- 6Department of Physical Therapy, Movement and Rehabilitation Sciences, School of Clinical and Rehabilitation Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, MA, United States
Introduction: The prevalence of depression and anxiety in children has risen in recent years, while childhood obesity and sedentary behavior continue to be a major public health concern. Existing evidence suggests early motor development and locomotor experiences contribute to psychosocial and physical development. By further understanding the far-reaching effects of early motor development, early life interventions aimed at preventing physical and mental health adversity may benefit from investigating early motor developmental milestones (MDM) attainment. The current study is the first to assess the longitudinal association between parent-reported gross MDM timing with objective measures of mental health, cardiorespiratory fitness (CRF), subcutaneous abdominal (SAAT), and visceral adipose tissue (VAT) outcomes later in childhood.
Method: In total, 131 children aged 8–11 years (46% female) were recruited. The parents of these children reported the age of attainment for five MDMs: holding their head unsupported, rolling over, sitting unsupported, standing, and walking independently. The study encompassed a comprehensive assessment, including measures of mental health, CRF (VO2 max), body–mass index (BMI), SAAT, and VAT. Data were analyzed using multiple stepwise linear regressions, adjusting for demographic and parental factors in Step 1 and including each MDM individually in Step 2.
Results: Our findings indicated earlier rolling over and walking were associated with higher CRF during preadolescence. Earlier rolling over was also linked to healthier BMI and lower levels of VAT, lower levels of trait anxiety, and fewer symptoms of depression.
Conclusion: This study provides further evidence with potential clinical implications that parent-reported MDM age of attainment is related to later preadolescent physical and mental health. The age at which a child first rolls over emerges as a particularly predictive factor for various preadolescent health outcomes, highlighting the multi-finality of MDM timing in understanding developmental trajectories.
1 Introduction
Healthy development during the first few years of life is essential for physical and psychosocial development in childhood and is the cornerstone for lifelong learning (Campbell et al., 2014). Physical development marks the progression from infancy through childhood, following a predictable sequence of developmental milestones wherein subsequent skills build upon earlier ones (Misirliyan et al., 2023). These milestones do not operate in isolation but are closely interconnected with social/emotional, gross and fine motor, language, and cognitive domains; progress in one area can influence and be influenced by others. Understanding typical development helps clinicians detect delayed development. However, limited normative data across early developmental stages hinders a comprehensive understanding of how the timing of motor developmental milestone (MDM) attainment influences subsequent development across the interconnected developmental domains (Sheldrick et al., 2019).
1.1 Motor developmental milestones
Early MDMs encompass fine and gross motor skills that children acquire early in life. Fine motor skills involve the coordination of small muscles, facilitating precise movements such as grasping and object manipulation (Piek et al., 2008). Gross motor skills involve larger muscle groups and coordinate movements essential for proprioception, core stability, and bodily control (Ghassabian et al., 2016). Gross and fine motor skill acquisition improve with age; however, the developmental progression of one is not dependent on the other (Sorgente et al., 2021). The timing of gross MDM attainment is linked to various physical and mental health outcomes in the later stages of childhood and adulthood. For example, research using parent-reported MDMs of their children has shown that the age of walking with support is associated with increased sport participation later in childhood and that earlier standing and walking are linked to higher educational attainment in adulthood (Ridgway et al., 2009a; Taanila et al., 2005).
Distinguishing that MDM attainment represents the endpoint of the process of motor skill acquisition, whereas motor skill acquisition itself is a nuanced and ongoing process that reflects the developmental journey leading to the milestone, is important. This process may offer more insight into the interconnected influences that MDMs have on other developmental domains, highlighting their dynamic role in overall development. While these terms are distinct, they are interrelated as MDM attainment serves as an endpoint of the outcomes of skill acquisition. For example, in the process of learning to walk, a child is unsteady, wobbles, and might only be able to take a few steps with assistance as the gross motor skills are acquired to master walking independently and meet the criteria of MDM attainment.
From the dynamic systems perspective, the maturation of developmental domains (i.e., social, emotional, language, gross motor, fine motor, and cognitive) collectively contributes to the trajectory of other domains and is interrelated within a complex system (Thelen, 1992, 1995). Growth in one domain does not exist in isolation; instead, change in one developmental domain can initiate a cascade of effects in other domains that influence outcomes in other domains not directly related to the initial attainment (Campos et al., 2000). For instance, improvements in fine motor skills can enhance cognitive abilities by facilitating tasks that require precision, such as writing, which, in turn, can boost academic performance. These effects are multidirectional; they can be direct and move in one direction or indirectly through multiple pathways (Thelen and Smith, 1998; Masten and Cicchetti, 2010). Developmental cascades describe the cumulative impacts of multiple interactions and exchanges within developing systems, leading to widespread effects across different levels (Gottlieb, 2007). Importantly, these cascades have lasting influences, fundamentally altering the trajectory of development across levels of neural activity, behavior, and interactions with the physical, social, and cultural environment (Iverson, 2021).
Motor development delays are characterized by motor performance significantly below what is expected for a child's chronological age despite having appropriate opportunities for skill acquisition (Matheis and Estabillo, 2018). These delays can manifest as poor balance, clumsiness, and persistent difficulty acquiring basic motor skills such as catching, throwing, kicking, running, and jumping (Blank, 2012). For infants, motor activities are indicators of early development, and children at risk of developmental delays often face challenges in attaining early MDMs. Understanding how early MDMs are associated with developmental trajectories across domains can help with predicting outcomes, planning services, and monitoring for related developmental and medical disorders (Noritz et al., 2013). Thus, gross MDMs may serve as early-life behavioral markers of a child's physical development, influencing their overall health and wellbeing.
1.2 Physical health
Typically, developing infants achieve several MDMs in the 1st year of life, contributing to fundamental motor skills and physical activity (PA) later in life (Clark and Metcalfe, 2002). Recognizing gross MDMs' influence on later physical health outcomes lays a foundation for exploring specific aspects of physical development on fitness and body composition. Several health organizations have proposed that higher PA levels are associated with short- and long-term benefits for physical, emotional, social, and cognitive health across the lifespan (CDC, 2024a; Association, 2016; HHS, 2023; Liguori et al., 2020; Rock et al., 2020). Regular PA can help children improve cardiorespiratory fitness (CRF), manage weight, and reduce the risk of developing chronic health conditions, such as cardiovascular disease, obesity, and Type 2 diabetes (OASH, 2018). Randomized controlled trials and cross-sectional studies have demonstrated that higher levels of PA improve CRF and prevent excess fat accumulation in children (Khan et al., 2014; Jiménez-Pavón et al., 2011; Ortega et al., 2010). Previous studies have suggested that poor motor competencies, the mastery of physical skills and movement patterns that facilitate engagement in daily activities, is associated with excess body fat during infancy and in preschool-aged children (Castelli and Valley, 2007; Camargos et al., 2016; Morano et al., 2011). Poor gross motor development during infancy also correlates with higher body fat and poor motor skill competency during the first 2 years of development (Andres et al., 2013). In children aged 6–10 years, those who are overweight or obese exhibit significantly lower gross motor skill proficiency and composite scores compared to their healthy-weight peers (Marmeleira et al., 2017). These findings suggest that fine motor skills, particularly those involving stationary object control, are independent of gross motor performance and weight status. Further investigation into the development of early gross motor skills, especially those involving dynamic body movements such as postural control and motor coordination, may enhance our understanding of the factors influencing children's overall fitness levels. Similarly, early attainment of gross MDM is associated with higher PA levels later in childhood and adolescence (Mattocks et al., 2008; Ridgway et al., 2009b). Despite empirical evidence supporting early gross MDMs' role in later physical health outcomes during childhood, the relationship between early MDMs and CRF has not been reported.
1.3 Mental health
Motor skills are often overlooked in discussions about psychosocial maladaptation during childhood. However, research indicates that early locomotor experiences are closely linked to later motor, language, and socio-emotional development (Campos et al., 2000; Iverson, 2021). As an infant attains MDMs, access to physical and social environments is enhanced, allowing the infant to interact with the environment and gather information during exploration while supported in different postures (Iverson, 2021; Elwood et al., 2012). Developmental coordination disorder (DCD), which affects ~6% of school-aged children, provides a notable example (Lino and DPR, 2022). Children with DCD often experience lower self-esteem and reduced participation in playgroups, which can lead to increased anxiety and depression and lower fitness levels, with issues potentially persisting into adulthood (Lingam et al., 2012; Draghi et al., 2021; Schott et al., 2007; Harris et al., 2021). Hua et al. (2022) showed that a 1-month delay in crawling increases overall motor impairment risk by 14%, and a similar delay in independent walking raises the risk by 21%. Variability in the timing of MDM attainment in typical development may obscure the critical importance of how the timing and transition between motor milestones influence other developmental domains. Peik et al. examined the relationship between early gross motor skills assessed by the Ages and Stages Questionnaire (ASQ) and subsequent depression and anxiety as measured by the Child Behavior Checklist (CBCL) in children aged 6–12 years (Piek et al., 2010; Squires et al., 1995; Achenbach and Edelbrock, 1991). They found that variability in gross motor skill attainment from 4 months to 4 years predicted parent-reported depression and anxiety scores. Furthermore, longitudinal data from the Copenhagen Perinatal Cohort demonstrated that this relationship extends into young adulthood, such that the age of gross MDM attainment was associated with neuroticism (a personality trait characterized by emotional instability, anxiety, self-doubt, and depression) 23 years later (Widiger and Oltmanns, 2017; Flensborg-Madsen et al., 2013). Delayed milestone achievement may serve not only as a marker of motor development but also as a potential indicator of the need for early intervention, offering a window into opportunities to address motoric factors that may impact a child's future mental health. By promoting the attainment of early MDMs, such interventions could further support psychological wellbeing and development, potentially reducing or preventing the emergence of mental health issues. Understanding how early MDMs influence mental health factors such as depression and anxiety later in childhood can provide valuable insights and structural support for early interventions aimed at promoting psychological wellbeing.
1.4 Present study
The relationship between early gross MDM and later physical and mental health outcomes remains under-explored in preadolescent children. Increasing rates of childhood obesity, sedentary behavior, and poor mental health continue to affect developmental trajectories (Stierman et al., 2020; Wilhite et al., 2022; Bitsko et al., 2022). Accordingly, this study aimed to assess parent-reported age of attainment for early gross motor skills (i.e., MDMs) and examine their relationship with CRF, body composition, and mental health outcomes later in childhood as individual MDMs may reflect diverse and discrete differences in later physical and mental health outcomes. Moreover, given that the data set was collected as part of a broader project, leveraging these existing data allowed us to address novel research questions about early MDM attainment. It was predicted that earlier parent-reported attainment of MDMs (e.g., holding the head up, rolling over, sitting, standing, and walking) would be associated with higher CRF, healthier body composition (i.e., decreased fat mass), and fewer symptoms of depression and anxiety.
2 Method
2.1 Participants
The present study was a secondary data analysis of preadolescent children aged 8–11 years engaged in a multiyear National Institutes of Health trial (ClinicalTrials.gov: NCT03592238) from 2019 through 2023 involving CRF testing, body composition assessment, and comprehensive demographic and health history questionnaires at the Center for Cognitive and Brain Health, Northeastern University.
In total, 131 healthy, neurotypical children whose parents retrospectively reported at least one of the five gross MDMs (e.g., holding the head up, rolling over, sitting, standing, and walking) at the time of data collection were included in the present study (Raine et al., 2021). One parent per child completed parental information, of which 85% were mothers and 15% were fathers.
All participants and their legal guardians signed informed assent and consent forms, respectively, in accordance with the Institutional Review Board of Northeastern University under protocol number 17-07-11, before they participated in the study. Study data were collected and managed using REDCap electronic data capture tools (Harris et al., 2009, 2019).
All children participated in a 3-hour assessment session conducted at the Center for Cognitive and Brain Health at Northeastern University. The assessments were administered by trained research staff, including graduate students and professionals with expertise in child development and physiological measurements. Children completed the Child Depression Inventory 2nd Edition Short Form (CDI-2) and the State and Trait Anxiety Inventory for Children (STAIC) questionnaires. Meanwhile, parents completed a demographic questionnaire and provided information on MDM age of attainment for their child. At the completion of the session, children's body composition and CRF were measured using standardized protocols.
2.2 Measures
2.2.1 Demographics
During the child's session, following the consent and assent process, the child's parent was provided with a comprehensive demographic survey through REDCap electronic data capture tools, including developmental, pediatric, and parental health history. Demographic information included age (Agechild), sex, intelligence quotient (IQ, Kaufman Brief Intelligence Test 2nd Edition), body mass index (BMIchild), gestation age in weeks, birth weight in grams, maternal age (Agematernal) in years, maternal BMI at the time of conception (BMIconception; Kaufman and Kaufman, 2004). Socioeconomic status (SES) was estimated using the mother's highest level of education and was assessed on a continuous scale: (1) did not complete high school, (2) high school graduate, (3) some college, (4) bachelor's degree, and (5) advanced degree (Jackson et al., 2017). Parents reported their feelings of anxiety and depression in the past 3 months on a Likert scale: 0 = never, 1 = sometimes, 2 = often, and 3 = almost always.
2.2.2 Motor developmental milestones
The Bayley Scales of Infant Development (BSID) age (mo.) range for gross MDM was used as the criterion to exclude participants' data for a specific MDM if the age of attainment was outside the expected range reported in the BSID (Bayley, 2006, 1936). The child's parent was asked to recall to the best of their ability the age in months at which the child first held their head erect and steady, rolled over from back to side, sat alone steadily, stood alone, and walked independently. Because the sample consisted of a healthy, typically developing sample, we adopted a conservative approach to minimize parental recall bias by removing extreme values. This was particularly important given the reliance on parental reports of MDM attainment, which required recall of events that occurred 8–10 years prior to the laboratory visit.
2.2.3 Body composition assessment
The children had their weight and height measurements taken by trained staff. Body composition was assessed by taking standing height and weight measurements while child participants wore lightweight clothing and no shoes using a Health-O-Meter Professional 500KL digital patient weighing scale with a stadiometer (Health-O-Meter Professional, McCook, IL, USA). BMIchild and maternal BMIconception were calculated using an individual's weight in kilograms divided by their height in meters squared (kg/m2). BMI percentiles were further computed using Centers for Disease Control and Prevention growth charts (Kuczmarski et al., 2002). Whole-body and regional soft tissue of visceral adipose tissue (VAT; mass [grams]) and subcutaneous abdominal adipose tissue (SAAT; mass [grams]) were measured by dual-energy X-ray absorptiometry (DXA; GE Lunar iDXA, Madison, WI, USA) as an accurate and valid measure of body composition in children (Bennett, 2023; Margulies et al., 2005; Ward and Crabtree, 2019).
2.2.4 Cardiorespiratory fitness assessment
Children performed a maximal oxygen consumption test on a motorized treadmill (treadmill: Trackmaster TMX428; metabolic cart: COSMED Quark CPET OMNIA, Concord, CA, USA). The assessment involved monitoring oxygen uptake (VO2) and respiratory exchange ratio (RER) at 20-second intervals. Testing followed a modified Balke protocol using a motor-driven treadmill set at a constant speed, with incremental increases in grade every 2 min by 2.5% until the participant reached volitional exhaustion (Liguori et al., 2020; Ferguson, 2014). Heart rate (HR) was continuously monitored using a Garmin HR monitor (Garmin HRM-Dual, Garmin Ltd., USA), and ratings of perceived exertion (RPE) were recorded every 2 min using the children's OMNI scale (Utter et al., 2002). Relative peak oxygen consumption (VO2 max) was calculated in ml/kg/min based on maximal effort criteria, which included (a) a plateau in oxygen uptake with an increase of <2 mL/kg/min despite increasing workload, (b) a peak HR of ≥185 bpm and a stable HR thereafter, (c) RER ≥ 1.00; and/or (Piek et al., 2008) RPE ratings of ≥8 on the children's OMNI scale (Utter et al., 2002).
2.2.5 CDI-2
The children completed the CDI-2. The CDI was developed as a brief tool for assessing depression symptoms in children. It originated from the Beck Depression Inventory, a widely used measure for depression in adults, and was adapted in 1992 for use with children aged 7–17 years, with a revision in 2011 to reflect improvements to internal and external validity (Beck et al., 1961; Kovacs, 1992, 2011; APA PsycTests, 2019). The CDI-2 short form consists of 12 items, prompting children to choose a phrase that best describes how they feel, such as “I do most things OK,” “I do many things wrong,” or “I do everything wrong.” Each item is scored on a 0–2 Likert-type scale, yielding a total score ranging from 0 to 24, with higher scores indicating more severe symptoms of depression. This version of the CDI-2 has shown good internal consistency, as indicated by Cronbach's alpha values of 0.80 or higher in school-aged children (Allgaier et al., 2012; Caqueo-Urízar et al., 2014).
2.2.6 STAIC
The children answered the STAIC. The STAIC was adapted from its adult counterpart, the State-Trait Anxiety Inventory, to differentiate between two forms of anxiety: state anxiety (STAIC-S) and trait anxiety (STAIC-T; APA PsycTests, 1973; Spielberger, 1983). State anxiety refers to a temporary and situation-specific type of anxiety characterized by feelings of apprehension, tension, nervousness, and worry linked to a particular circumstance or event (Jouvent et al., 1999). In contrast, trait anxiety represents a more enduring and stable personality trait that reflects an individual's predisposition to experience anxiety across various situations and over time (Endler and Kocovski, 2001). Individuals who score higher on the trait anxiety subscale are prone to experiencing anxiety more frequently, even in non-threatening situations, and may exhibit heightened sensitivity to stressors (Elwood et al., 2012). Trait anxiety is believed to have a genetic basis and can be influenced by environmental factors and early life experiences (Garcia et al., 2013). Given our focus on exploring the relationship between early gross MDM and later mental health outcomes, we specifically examined the trait anxiety subscale of the STAIC. The STAIC-T comprises 20 statements, such as “I worry about making mistakes,” that a participant responds to based on their general feelings, such as “hardly ever,” “sometimes,” or “often.” Each item is scored from 1 to 3 for a total score ranging from 20 to 60, with higher scores indicating greater levels of trait anxiety.
2.3 Data analysis
All statistical analyses were performed using IBM SPSS Statistics (version 29.0). The statistical requirements for multivariate procedures were checked, and the hypotheses were tested at a significance level of 0.05. Data were analyzed using multiple stepwise linear regressions to assess the association of early-life gross MDMs with the dependent variables: physical health outcomes (CRF and body composition) and mental health outcomes (symptoms of depression and trait anxiety) later in childhood.
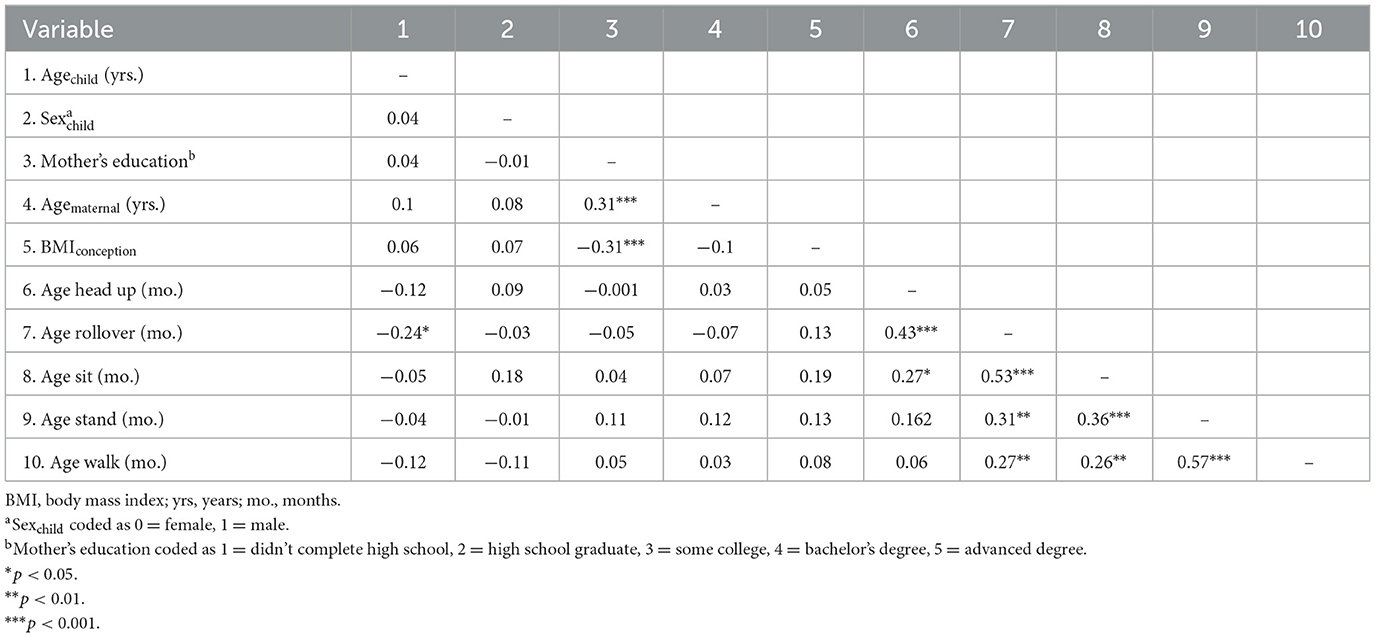
Previous research has highlighted the significance of several biological and social factors such as age, sex, mother's education, maternal age and BMI at conception, and parental mental health in influencing motor developmental outcomes (Flensborg-Madsen and Mortensen, 2017; Lung et al., 2009; Mota et al., 2002; Freitas et al., 2007; D'Ascenzi et al., 2021; Mannino et al., 2022; Savage et al., 2013; Fergusson and Woodward, 1999; Van Santvoort et al., 2015; Pierce et al., 2020). Accordingly, these biological and social factors were included as independent variables to control for their potential effects on later health outcomes. In Step 1, demographic factors (e.g., Agechild, sex of the child, and mother's education), maternal factors (e.g., Agematernal and maternal BMIconception), and parental factors (e.g., parent self-reported feelings of anxiety and parent self-reported feelings of depression) were included as covariates and entered in the regression analysis. In Step 2, the five MDMs were individually introduced as independent variables to assess their specific associations with later developmental health outcomes. See the main variables' correlation coefficient in Table 1.
2.3.1 Physical health
To assess the association between MDM parent-reported age (months) of attainment and CRF (e.g., relative VO2 max score) later in childhood, we performed five stepwise linear regressions for each MDM (e.g., holding the head up, rolling over, sitting, standing, and walking) in Step 2.
To assess the association between MDM parent-reported age (months) of attainment and body composition (e.g., BMI, SAAT, and VAT) later in childhood, we performed five stepwise linear regressions for each MDM (e.g., holding the head up, rolling over, sitting, standing, and walking) in Step 2.
2.3.2 Mental health
To assess the association between MDM parent-reported age (months) of attainment and symptoms of depression (e.g., CDI-2) later in childhood, we performed five stepwise linear regression for each MDM (e.g., holding the head up, rolling over, sitting, standing, and walking) in Step 2.
To assess the association between MDM To assess the association between MDM parent-reported age (months) of attainment and trait level anxiety (e.g., STAIC-T) later in childhood, we performed five stepwise linear regression for each MDM (e.g., holding the head up, rolling over, sitting, standing, and walking) in Step 2.
3 Results
3.1 Demographics
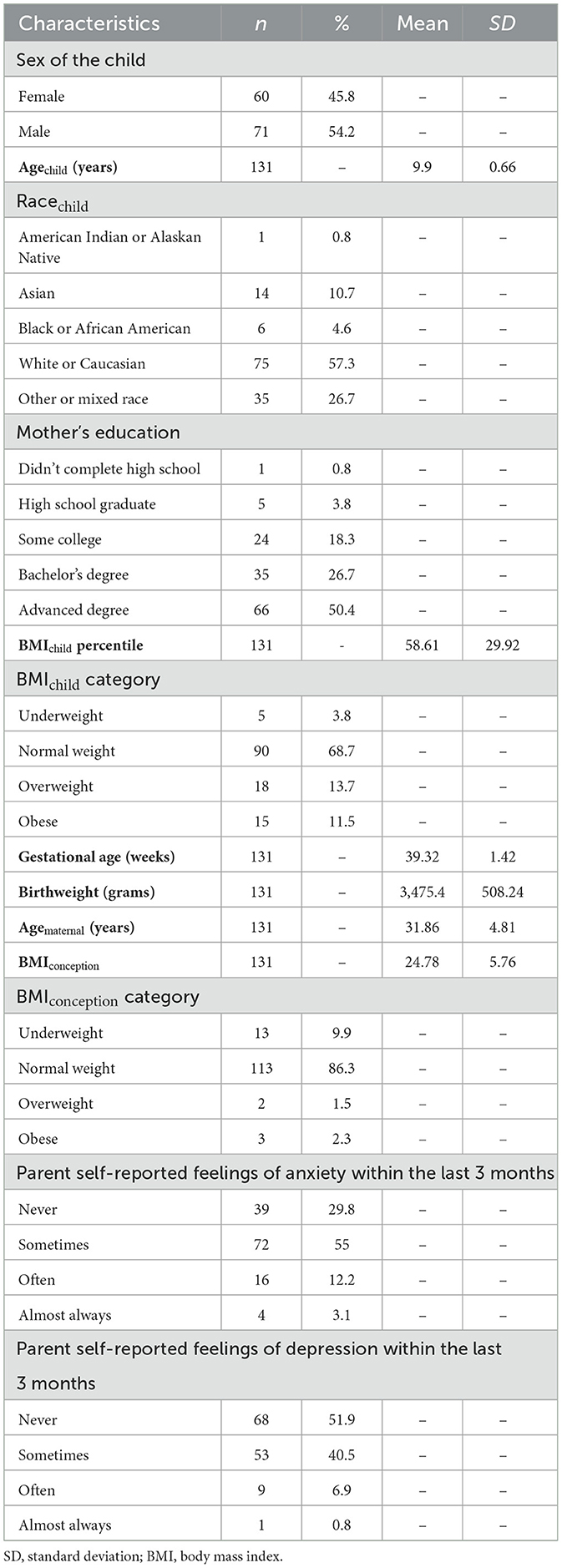
The study included children with a sex distribution of 45.8% female and an average age of 9.9 years (±0.66). The cohort was predominantly of Caucasian descent (57.3%) and had a healthy BMI range (68.7%). Notably, all children were born full-term and within a normal range for birth weight (≥2,500 g; CDC, 2024b). Regarding maternal demographics, approximately half of the children's mothers held an advanced degree (50.4%), were within a healthy BMI range at conception with 86.3%, with a BMI between 18.5 and 24.9 (Maring et al., 2015), and were, on average, 31.9 (± 4.81) years old at the time of their child's birth. In terms of parental (85% mothers, 15% fathers) mental health, a significant proportion of parents self-reported experiencing anxiety sometimes (55%) and depressive symptoms sometimes (40.5%) in the 3 months preceding data collection. See Table 2 for a comprehensive breakdown of participant demographics.
3.2 Motor developmental milestones
For the parent-reported age of MDM attainment, the children first held their head erect and steady at 2.3 (±1) months, rolled over back to side at 3.7 (±1.1) months, sat alone steadily at 6.2 (±1.1) months, stood alone at 10.5 (±1.3) months, and walked independently at 11.9 (±1.6) months. See Table 3 for MDM inclusion criteria and characteristics.
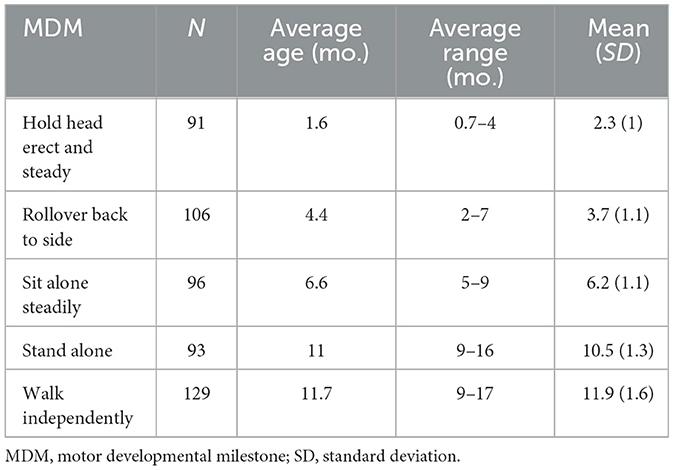
Table 3. Motor developmental milestones (months) sample descriptive data meeting the Bayley scales of infant development age of attainment.
3.3 Cardiorespiratory fitness
For VO2 max scores and the age rolling over was achieved, the Step 1 regression analysis indicated a significant overall effect, adjusted R2 = 0.08, F(1, 100) = 9.45, p = 0.001. There was a significant effect for the mother's education, pr (partial correlation) = 0.28, t(101) = 3.07, p = 0.003, β = 0.293, such that a higher mother's education was associated with higher VO2 max. With the addition of age of rolling over, Step 2 was also significant, ΔR2 = 0.06, F(2, 100) = 8.15, p < 0.001, such that an earlier age of rolling over was associated with greater VO2 max, pr = −0.3, t(100) = −2.52, p = 0.013, β = – 0.23.
In addition, VO2 max scores and the age of attainment for walking indicated a significant overall effect in Step 1 of the regression analysis, adjusted R2 = 0.15, F(2, 122) = 8.18, p < 0.001. There were significant effects for both mother's education, pr = 0.3, t(122) = 3.47, p < 0.001, β = 0.3, and sex, pr = 0.19, t(122) = 2.13, p = 0.04, β = 0.18), such that a higher level of mother's education and male sex were associated with higher VO2 max. With the addition of age of walking, Step 2 was also significant, ΔR2 = 0.04, F(3, 121) = 7.3, p < 0.001, such that earlier age of walking was associated with greater VO2 max, pr = −0.2, t(121) = −2.24, p = 0.027, β = −0.19. Parent-reported age for when their child held their head up, sat, and stood was not significantly associated (ps ≥ 0.05) with CRF as a physical health outcome (see Table 4).
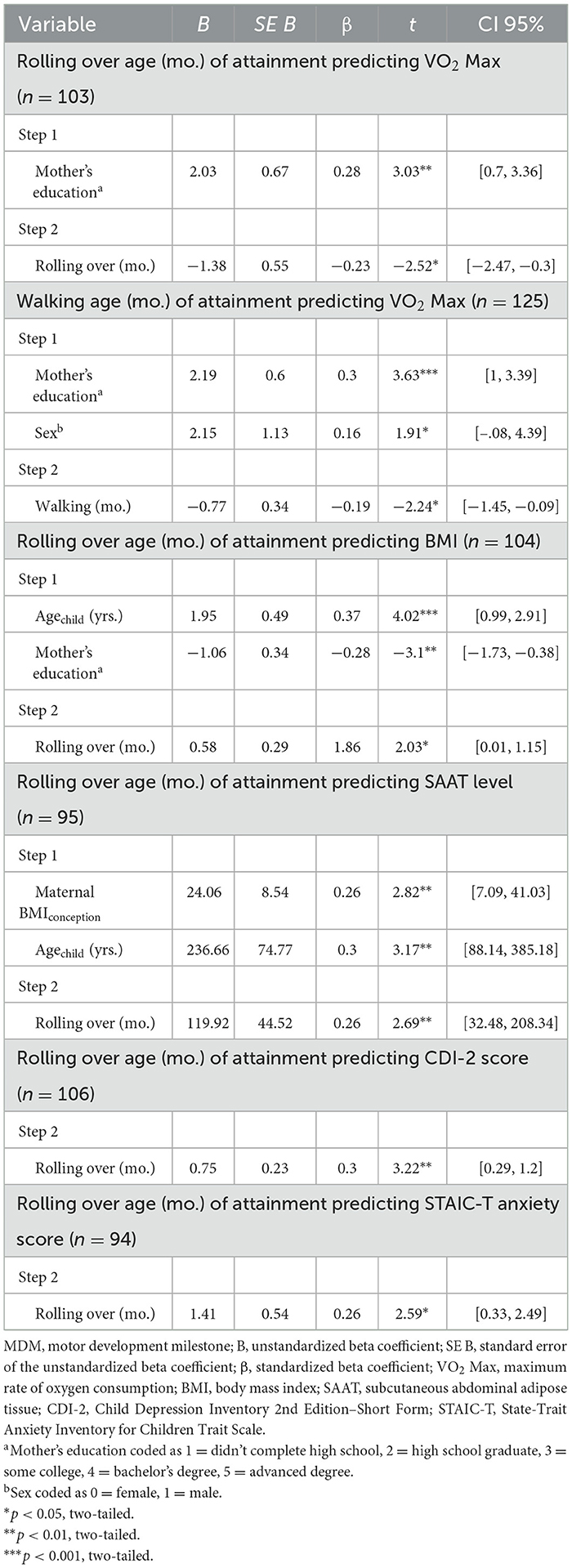
Table 4. Stepwise linear regression final model for significant MDM age (months) of attainment predicting each health outcome.
3.4 Body composition
For BMI and age rolling over was achieved, the Step 1 regression analysis indicated a significant overall effect, adjusted R2 = 0.19, F(2, 101) = 8.87, p = 0.045. There were significant effects for both Agechild, pr = 0.32, t(101) = 2.59, p < 0.001, β = 0.32, and mother's education, pr = −0.28, t(101) = −3.13, p = 0.002, β = −0.28, such that younger age and higher maternal education are associated with a lower BMI. With the addition of age of rolling over, Step 2 was also significant, ΔR2 = 0.03, F(3, 100) = 8.52, p < 0.001, such that earlier age of rolling over was associated with lower BMI, pr = 0.2, t(100) = 2.03, p = 0.045, β = 0.19. For SAAT levels and the age rolling over was achieved, the Step 1 regression analysis indicated a significant overall effect, adjusted R2 = 0.16, F(2, 92) = 8.58, p < 0.001. There were significant effects for both maternal BMIconception, pr = 0.31, t(92) = 3.14, p = 0.002, β = 0.3, and Agechild, pr = 0.25, t(92) = 2.5, p = 0.01, β = 0.24, such that mothers with a higher BMI at the time of conception and older age of the child were associated with greater levels of SAAT. With the addition of age of rolling over, Step 2 was also significant, ΔR2 = 0.06, F(3, 91) = 8.52, p < 0.001, such that earlier age of rolling over was associated with lower levels of SAAT, pr = 0.27, t(91) = 2.69, p = 0.008, β = 0.26. The stepwise regression analysis with VAT as the outcome was not significantly associated with any of the MDMs. Parent-reported age for when their child held their head up, sat, stood, and walked was not significantly associated (ps ≥ 0.05) with preadolescent levels of SAAT as a physical health outcome (see Table 4).
3.5 Symptoms of depression
For CDI-2 scores and the age rolling over was achieved, the Step 1 regression analysis did not indicate child, maternal, or parental factors were significant. With the addition of age of rolling over, Step 2 regression analysis was significant, ΔR2 = 0.06, F(1, 104) = 10.36, p = 0.002, indicating earlier rolling over was associated with fewer symptoms of depression during preadolescence, pr = 0.3, t(104) = 3.22, p = 0.002, β = 0.3. Parent-reported age for when their child held their head up, sat, stood, and walked was not significantly associated (ps ≥ 0.05) with preadolescent depression as a mental health outcome (see Table 4).
3.6 Trait-level anxiety
For STAIC-T and age rolling over was achieved, the Step 1 regression analysis on STAIC-T scores did not indicate child, maternal, or parental factors were significant. With the addition of age of rolling over, Step 2 regression analysis was significant, ΔR2 = 0.08, F(1, 92) = 6.73, p = 0.011, indicating earlier rolling over was associated with lower levels of trait anxiety during preadolescence, pr = 0.26, t(92) = 2.59, p = 0.011, β = 0.26. Parent-reported age for when their child held their head up, sat, stood, and walked was not significantly associated (ps ≥ 0.05) with preadolescent trait anxiety levels as a mental health outcome (see Table 4).
4 Discussion
This study investigated the association between the timing of parent-reported MDM attainment and physical and mental health outcomes in later childhood. Our findings demonstrated that the timing of specific gross MDM attainment (rolling over and walking) is significantly associated with both physical and mental health outcomes 7–10 years later. Specifically, earlier parent-reported rolling over and walking were associated with healthier CRF, as measured via higher relative VO2 max scores. Additionally, earlier rolling over was associated with healthier body composition, as reflected in DXA-derived lower SAAT levels. This relationship with rolling over extended to self-reported lower levels of trait anxiety and fewer symptoms of depression during preadolescence.
4.1 Physical health
Physical fitness is an important indicator of health and is associated with PA and CRF (Lamb et al., 1988; Warburton et al., 2006; Ribeiro et al., 2003). Gross motor development and mastery of fundamental movement skills (FMS) provide the foundation for an active lifestyle (Cairney et al., 2019; Lubans et al., 2010). Earlier mastery of MDM has been associated with greater FMS competence, increased PA engagement, and sport participation later in childhood and into adulthood (Ridgway et al., 2009b; Cattuzzo et al., 2016; Cliff et al., 2009; Aaltonen et al., 2015). The relationship between MDMs and aspects of physical fitness illustrates the importance of evaluating MDM timing when investigating the nature of developmental trajectories. To our knowledge, the association between early gross MDM attainment and later CRF via VO2 max has not been previously reported. The American Heart Association has listed CRF as a critical measure, as children in the lowest quartile for CRF have ~5 times greater risk of cardiovascular disease (Raghuveer et al., 2020; Dencker et al., 2012). Our study indicated that earlier parent-reported rolling over and walking are significantly associated with higher relative VO2 max scores, indicating healthier CRF later in development. These associations remained even after controlling for other critical features, including the age and sex of the child, the mother's education, maternal age, and BMI at the time of conception. This relationship is important as maximal oxygen consumption (VO2 max) is the gold standard for indicating CRF and is a strong predictor of all-cause mortality and future disease, such as cardiovascular disease, Alzheimer's disease, and other diseases after adjusting for risk factors including hypertension, smoking, and obesity (Armstrong, 2019; Hawkins et al., 2007; Shephard et al., 1968; Ross et al., 2016).
Consistent with our findings, Ridgway and colleagues demonstrated that the age of walking with support predicted sport participation at 14 years (Ridgway et al., 2009b). Although the current study did not examine PA, investigating MDM's relationship to a child's history of PA engagement and sport participation may further elucidate the mechanisms involved in promoting CRF. Ridgway and colleagues also found that earlier age of standing unaided and walking independently predicted healthier aerobic fitness in adults aged 31 years, estimated by post-exercise heart rate following a 4-minute submaximal step test (Ridgway et al., 2009a). Based on their findings, infant growth during the 1st year may be important to consider in future studies as this may influence MDM attainment. Furthermore, MDM timing may depend on external factors such as early life environment, social and cultural variations related to physical health factors (Adolph and Hoch, 2019). Of the five MDMs examined, rolling over and walking involve crossing the midline and bilateral coordinated movements involving the whole body, whereas holding the head up, sitting, and standing are stationary positions marking postural control. The ability to roll over and walk facilitates more locomotor behaviors and exploration. As infants progress into childhood, locomotion enables more opportunities to explore, play, and engage in PA, possibly contributing to cardiovascular development and later CRF (Barnett et al., 2016).
A synergistic association exists between an individual's motor skill level, PA engagement, CRF level, and body composition, all of which influence developmental trajectories (Kolunsarka et al., 2021). Research has indicated that poor gross motor skills development is associated with overweight and obesity in children aged 3–6 years, particularly for dynamic gross motor movements compared to fine motor skills like stationary object control (Morano et al., 2011; Marmeleira et al., 2017). This relationship extends into later childhood, where longitudinal research in children aged 6–10 has shown that motor coordination, muscular strength, and aerobic endurance decrease as SAAT levels increase (Lopes et al., 2012). During late childhood and adolescence, changes in BMI are associated with SAAT levels, whereas changes in BMI are associated with VAT levels in adulthood (Kindblom et al., 2009). After controlling for demographic and maternal health factors, our study indicated that earlier attainment of rolling over was associated with lower levels of SAAT mass and healthier BMI 10–12 years later, further supporting the importance of early locomotion experience during development for healthier body composition.
Interestingly, the age of MDM attainment was not associated with preadolescent VAT mass. While this finding was a bit surprising, the current study included only 15 (11.5%) children with obesity. This suggests that there may have been little variation in VAT levels in normal-weight children, and future studies should include more children across a more extensive weight range.
Rolling over, compared to other motor milestones, is a coordinated and dynamic movement that facilitates transitioning into and out of stationary positions and progressing into bipedal movements. Moreover, rolling over benefits the learning of more complex movements later in development, i.e., movements requiring crossing the midline and shifting positions to regain stability and control, such as recovering from a fall (Hoogenboom et al., 2009). Competence in balance, coordination, and proprioception early in life boosts motor skill acquisition and PA engagement which may contribute to healthier SAAT levels (Lopes et al., 2012). The timing of rolling over attainment may have a bidirectional exponential effect where earlier attainment encourages a more active lifestyle, and later attainment may influence factors contributing to an increased risk of developing health complications later in life. The non-significant relationship between early MDM and preadolescent VAT levels could reflect the relatively low-risk nature of this study's sample. Similar studies investigating early life influences on the accumulation of VAT and SAAT mass later in development may benefit from including MDM timing of attainment in future analyses to further understand the synergistic effects of motor behavior throughout development.
4.2 Mental health
Early attainment of MDMs may contribute to locomotor experiences associated with psychosocial development (Campos et al., 2000). Many longitudinal studies have identified the relationship between gross MDMs and later mental health outcomes; however, more robust evidence of a causal relationship with differing developmental trajectories is needed. Siggurdson et al. examined 6,850 participants from the 1958 U.K. Birth Cohort and the National Child Development Study, demonstrating that delays in locomotor milestones, such as walking after 18 months, are associated with the development of anxiety problems between the ages of 7 and 16 years (Sigurdsson et al., 2002). Another study of 4,627 participants from the British 1946 birth cohort that measured anxiety and depression symptoms at ages 13, 15, 36, 43, and 53 years found that earlier standing and walking were associated with a reduced likelihood of symptoms later in life (Colman et al., 2007). This suggests that early life behavioral markers, such as MDM, are important to consider when determining contributing factors in the later development of mental health outcomes, including anxiety and depression.
The ability to competently move with age-appropriate accuracy and coordination enables opportunities for the optimal development of psychosocial wellbeing (Mancini et al., 2016). Learning to roll over involves using the entire body to coordinate the head, arms, torso, and legs to move from the stomach (prone) to the back (supine) position and vice versa. During the learning process of this movement and eventual mastery of rolling over, the amount and type of learning experiences increase, allowing an infant to adapt and enhance motor independence and confidence (Adolph and Franchak, 2017). Our findings suggest earlier rolling over is associated with self-reported lower levels of trait anxiety (STAIC-T) and fewer symptoms of depression (CDI-2) 9–11 years later. These associations were independent of demographic and maternal health factors. Attainment of rolling over contributes to vestibular development for balance, muscle development for coordination and postural control, and proprioception or bodily awareness (Piek et al., 2010; Adolph and Robinson, 2015). Developing balance, coordination, and bodily awareness facilitates learning experiences through exploration, leading to maturation and attaining subsequent milestones (Cech and Martin, 2011; Sangkarit and Tapanya, 2024). This dynamic relationship is important for play, where an infant's self-discovery is enriched through interacting with their environment, thereby contributing to other developmental domains such as language, cognition, and socio-emotional development (Adolph and Hoch, 2019; Schott et al., 2023; Thelen et al., 2001; Aguilera-Alcala et al., 2020; Valadi and Gabbard, 2020; Venetsanou and Kambas, 2010). Successive gross MDM attainment builds on this spatial exploration and may foster peer-to-peer interactions and familial bonding (Sangkarit and Tapanya, 2024; Thurman and Corbetta, 2017; Rocha et al., 2019). Earlier MDM attainment may afford more motor learning experiences, aiding positive social interactions that, in return, build motor confidence and self-confidence, contributing to overall wellbeing later in development.
4.3 Limitations
There are important limitations of this study to note. First, this secondary data analysis of a multiyear randomized controlled crossover trial provided multiple metrics to assess early MDM association with later outcomes. Due to some parents being unable to recall all their child's MDMs, many participants did not have complete data for all five MDMs, leading to varying sample sizes per analysis that may impact consistency across analyses. Second, MDM age of attainment data was obtained through retrospective recall from the participants' parent for each milestone, which introduces a risk of recall bias. Future research can improve this approach by confirming or retrieving MDM attainment data from the child's pediatrician or being in closer proximity to the occurrence of each MDM. Third, the sample population was primarily low-risk, typically developing preadolescent children, which may not be representative of children who fall into the extremes of mental and physical health status. That is, 69% of the sample was within a normal weight range, all participants were born full term at a healthy birthweight and had no neuropsychological disorder during childhood, and all gross MDM ages of attainment were within the expected age range as described by the BSID (Bayley, 2006, 1936). Fourth, only five gross MDMs up to 18 months postpartum were included in the analysis, excluding the development of transitional gross motor skills. Collecting data on gross MDM from birth to 4 years may offer more insight into early life behavioral changes influencing the relationship with later health outcomes. Fifth, our sample primarily consisted of mostly White, well-educated families, which may limit the generalizability of our findings to more diverse populations. Families with different socioeconomic, cultural, and educational backgrounds may have varying access to resources and developmental opportunities that could influence MDM attainment and related outcomes. Future studies should aim to include more heterogeneous samples to better capture the variability across broader populations. Sixth, perinatal maternal health, parent–infant interaction, affordances in the home environment, infant feeding, sleeping patterns, growth, and milestone attainment across developmental domains were not included and remain areas for further investigation. Finally, other confounding factors, such as parental mental and physical health history, parental PA engagement, maternal alcohol consumption, smoking, number of siblings, and parenting practices, may have long-lasting influences on developmental trajectories. Accordingly, these findings should be taken with caution, as children develop rapidly, and data between infancy and preadolescence may further inform interpretations of the role MDMs serve in understanding developmental trajectories and later health outcomes.
5 Conclusion
Even with the limitations and all the other factors that might affect physical and mental health in preadolescence, the results of this study provide further evidence that parent-reported MDM age of attainment is related to later preadolescent physical and psychological health. This study provides further evidence that parent-reported MDM age of achievement is related to later preadolescent physical and mental health. These findings are among the first to assess the relation of early MDMs with objective measures of CRF and body composition in preadolescent children and have potential clinical implications, with early MDMs serving as a marker for later physical and mental health. Earlier attainment of rolling over within the expected range was associated with healthier body composition (SAAT), lower levels of trait anxiety, and fewer symptoms of depression. Additionally, earlier walking and rolling over were associated with healthier CRF (VO2 max). By further understanding the far-reaching effects of early motor development, early life interventions aimed at preventing physical and mental health adversity may benefit from investigating early MDM attainment. Similar studies following children and their families from infancy through adolescence while tracking all early gross MDM may help distinguish whether such links between early gross MDM and preadolescent health outcomes might be attributed to early life environmental influences across developmental stages. These findings support theories advocating that early locomotor experiences are essential for understanding developmental health trajectories.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Northeastern University under protocol number 17-07-11. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
MC: Conceptualization, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. LR: Data curation, Project administration, Writing – review & editing. EZ: Writing – review & editing. NS: Writing – review & editing. CH: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This material was based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-1938052 and National Institute of Health NICHD Grant No. HD094054. Funding sources were not involved in study design, collection, analysis, data interpretation, report writing, or the decision to submit the article for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors(s) and do not necessarily reflect the views of the National Science Foundation.
References
Aaltonen, S., Latvala, A., Rose, R. J., Pulkkinen, L., Kujala, U. M., Kaprio, J., et al. (2015). Motor development and physical activity: a longitudinal discordant twin-pair study. Med. Sci. Sports Exer. 47:2111. doi: 10.1249/MSS.0000000000000650
Adolph, K. E., and Franchak, J. M. (2017). The development of motor behavior. Wiley Interdiscipl. Rev. 8:e1430. doi: 10.1002/wcs.1430
Adolph, K. E., and Hoch, J. E. (2019). Motor development: embodied, embedded, enculturated, and enabling. Ann. Rev. Psychol. 70, 141–164. doi: 10.1146/annurev-psych-010418-102836
Adolph, K. E., and Robinson, S. R. (2015). Motor development. Handb. Child Psychol. Dev. Sci. 2015, 1–45. doi: 10.1002/9781118963418.childpsy204
Aguilera-Alcala, N., Morales-Reyes, Z., Martin-Lopez, B., Moleon, M., and Sanchez-Zapata, J. A. (2020). Role of scavengers in providing non-material contributions to people. Ecol. Indic. 117:11. doi: 10.1016/j.ecolind.2020.106643
Allgaier, A.-K., Frühe, B., Pietsch, K., Saravo, B., Baethmann, M., and Schulte-Körne, G. (2012). Is the Children's Depression Inventory Short version a valid screening tool in pediatric care? a comparison to its full-length version. J. Psychosomat. Res. 73, 369–374. doi: 10.1016/j.jpsychores.2012.08.016
Andres, A., Casey, P. H., Bellando, J., Cleves, M. A., and Badger, T. M. (2013). Effects of fat mass on motor development during the first 2 years of life. Infant Child Adolesc. Nutr. 5, 248–254. doi: 10.1177/1941406413489728
Armstrong, N. (2019). Youth aerobic fitness. Pediatr. Exer. Sci. 31, 137–143. doi: 10.1123/pes.2019-0039
Association, A. H. (2016). What's the Link Between Physical Activity and Health? Available at: https://www.heart.org/en/health-topics/cardiac-rehab/getting-physically-active/whats-the-link-between-physical-activity-and-health (accessed June 10, 2024).
Barnett, L. M., Salmon, J., and Hesketh, K. D. (2016). More active pre-school children have better motor competence at school starting age: an observational cohort study. BMC Publ. Health 16:1068. doi: 10.1186/s12889-016-3742-1
Bayley, N. (1936). The development of motor abilities during the first three years: a study of sixty-one infants tested repeatedly. Monogr. Soc. Res. Child Dev. 1, 1–26. doi: 10.2307/1165480
Bayley, N. (2006). Bayley scales of infant and toddler development. Pearson Educ. 2006:t14978. doi: 10.1037/t14978-000
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., and Erbaugh, J. (1961). An inventory for measuring depression. Archiv. Gen. Psychiat. 4, 561–571. doi: 10.1001/archpsyc.1961.01710120031004
Bennett, J. P. (2023). Emerging Applications in the Measurement of Body Composition and Their Relationships to Disease Risk. Manoa: University of Hawai'i at Manoa.
Bitsko, R., Claussen, A., Lichtstein, J., Black, L., Everett Jones, S., Danielson, M., et al. (2022). Surveillance of children's mental health-United States, 2013–2019. MMWR 71, 1–42. doi: 10.15585/mmwr.su7102a1
Blank, R. (2012). European Academy of Childhood Disability (EACD): Recommendations on the definition, diagnosis and intervention of developmental coordination disorder (pocket version) German-Swiss interdisciplinary clinical practice guideline S3-standard according to the Association of the Scientific Medical Societies in Germany* European Academy of Childhood Disability (EACD): Recommendations on the definition, diagnosis and intervention of developmental coordination disorder (pocket version) German-Swiss interdisciplinary clinical practice guideline S3-standard according to the Association of the Scientific Medical Societies in Germany. Dev. Med. Child Neurol. 54:4175. doi: 10.1111/j.1469-8749.2011.04175.x
Cairney, J., Dudley, D., Kwan, M., Bulten, R., and Kriellaars, D. (2019). Physical literacy, physical activity and health: toward an evidence-informed conceptual model. Sports Med. 49, 371–383. doi: 10.1007/s40279-019-01063-3
Camargos, A. C. R., Mendonca, V. A., de Andrade, C. A., Oliveira, K. S. C., and Lacerda, A. C. R. (2016). Overweight and obese infants present lower cognitive and motor development scores than normal-weight peers. Res. Dev. Disabil. 59, 410–416. doi: 10.1016/j.ridd.2016.10.001
Campbell, F., Conti, G., Heckman, J. J., Moon, S. H., Pinto, R., Pungello, E., et al. (2014). Early childhood investments substantially boost adult health. Science 343, 1478–1485. doi: 10.1126/science.1248429
Campos, J. J., Anderson, D. I., Barbu-Roth, M. A., Hubbard, E. M., Hertenstein, M. J., Witherington, D., et al. (2000). Travel broadens the mind. Infancy 1, 149–219. doi: 10.1207/S15327078IN0102_1
Caqueo-Urízar, A., Urzúa, A., and De Munter, K. (2014). Mental health of indigenous school children in Northern Chile. BMC Psychiat. 14, 1–7. doi: 10.1186/1471-244X.-14-11
Castelli, D. M., and Valley, J. A. (2007). The relationship of physical fitness and motor competence to physical activity. J. Teach. Phys. Educ. 26:358. doi: 10.1123/jtpe.26.4.358
Cattuzzo, M. T., dos Santos Henrique, R., Ré, A. H. N., de Oliveira, I. S., Melo, B. M., de Sousa Moura, M., et al. (2016). Motor competence and health related physical fitness in youth: a systematic review. J. Sci. Med. Sport 19, 123–129. doi: 10.1016/j.jsams.2014.12.004
CDC (2024b). FastStats—birthweight: Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/nchs/fastats/birthweight.htm (accessed July 27, 2024).
Cech, D. J., and Martin, S. T. (2011). Functional movement development across the life span. Elsev. Health Sci. 4:3. doi: 10.1016/B978-1-4160-4978-4.00003-X
Clark, J. E., and Metcalfe, J. S. (2002). “The mountain of motor development: a metaphor,” in Motor Development: Research and Reviews, eds. J. E. Clark, and J. Humphrey (Reston, VA: NASPE Publications), 163–190.
Cliff, D. P., Okely, A. D., Smith, L. M., and McKeen, K. (2009). Relationships between fundamental movement skills and objectively measured physical activity in preschool children. Pediatr. Exer. Sci. 21, 436–449. doi: 10.1123/pes.21.4.436
Colman, I., Ploubidis, G. B., Wadsworth, M. E., Jones, P. B., and Croudace, T. J. A. (2007). longitudinal typology of symptoms of depression and anxiety over the life course. Biol. Psychiat. 62, 1265–1271. doi: 10.1016/j.biopsych.2007.05.012
D'Ascenzi, F., Sciaccaluga, C., Cameli, M., Cecere, A., Ciccone, M. M., Di Francesco, S., et al. (2021). When should cardiovascular prevention begin? the importance of antenatal, perinatal and primordial prevention. Eur. J. Prev. Cardiol. 28, 361–369. doi: 10.1177/2047487319893832
Dencker, M., Thorsson, O., Karlsson, M. K., Lindén, C., Wollmer, P., Andersen, L. B., et al. (2012). Aerobic fitness related to cardiovascular risk factors in young children. Eur. J. Pediatr. 171, 705–710. doi: 10.1007/s00431-011-1617-0
Draghi, T. T. G., Cavalcante Neto, J. L., and Tudella, E. (2021). Symptoms of anxiety and depression in schoolchildren with and without developmental coordination disorder. J. Health Psychol. 26, 1519–1527. doi: 10.1177/1359105319878253
Elwood, L. S., Wolitzky-Taylor, K., and Olatunji, B. O. (2012). Measurement of anxious traits: a contemporary review and synthesis. Anxiety Stress Cop. 25, 647–666. doi: 10.1080/10615806.2011.582949
Endler, N. S., and Kocovski, N. L. (2001). State and trait anxiety revisited. J. Anxiety Disord. 15, 231–245. doi: 10.1016/S0887-6185(01)00060-3
Ferguson, B. (2014). ACSM's guidelines for exercise testing and prescription 9th Ed. J. Can. Chiropract. Assoc. 58:328.
Fergusson, D. M., and Woodward, L. J. (1999). Maternal age and educational and psychosocial outcomes in early adulthood. J. Child Psychol. Psychiat. Allied Discipl. 40, 479–489. doi: 10.1111/1469-7610.00464
Flensborg-Madsen, T., and Mortensen, E. L. (2017). Predictors of motor developmental milestones during the first year of life. Eur. J. Pediatr. 176, 109–119. doi: 10.1007/s00431-016-2817-4
Flensborg-Madsen, T., Sorensen, H. J., Revsbech, R., and Mortensen, E. L. (2013). Early motor developmental milestones and level of neuroticism in young adulthood: a 23-year follow-up study of the Copenhagen Perinatal Cohort. Psychol. Med. 43, 1293–1301. doi: 10.1017/S0033291712001997
Freitas, D., Maia, J., Beunen, G., Claessens, A., Thomis, M., Marques, A., et al. (2007). Socio-economic status, growth, physical activity and fitness: the Madeira Growth Study. Ann. Hum. Biol. 34, 107–122. doi: 10.1080/03014460601080983
Garcia, S. E., Tully, E. C., Tarantino, N., South, S., Iacono, W. G., McGue, M., et al. (2013). Changes in genetic and environmental influences on trait anxiety from middle adolescence to early adulthood. J. Affect. Disord. 151, 46–53. doi: 10.1016/j.jad.2013.05.046
Ghassabian, A., Sundaram, R., Bell, E., Bello, S. C., Kus, C., Yeung, E., et al. (2016). Gross motor milestones and subsequent development. Pediatrics 138:4372. doi: 10.1542/peds.2015-4372
Gottlieb, G. (2007). Probabilistic epigenesis. Dev. Sci. 10, 1–11. doi: 10.1111/j.1467-7687.2007.00556.x
Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O'Neal, L., et al. (2019). The REDCap consortium: building an international community of software platform partners. J. Biomed. Informat. 95:103208. doi: 10.1016/j.jbi.2019.103208
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., Conde, J. G., et al. (2009). Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Informat. 42, 377–381. doi: 10.1016/j.jbi.2008.08.010
Harris, S., Wilmut, K., and Rathbone, C. (2021). Anxiety, confidence and self-concept in adults with and without developmental coordination disorder. Res. Dev. Disabil. 119:104119. doi: 10.1016/j.ridd.2021.104119
Hawkins, M. N., Raven, P. B., Snell, P. G., Stray-Gundersen, J., and Levine, B. D. (2007). Maximal oxygen uptake as a parametric measure of cardiorespiratory capacity. Med. Sci. Sports Exer. 39, 103–107. doi: 10.1249/01.mss.0000241641.75101.64
HHS (2023). Releases Physical Activity Guidelines for Americans Midcourse Report: Implementation Strategies for Older Adults. Washington, DC.
Hoogenboom, B. J., Voight, M. L., Cook, G., and Gill, L. (2009). Using rolling to develop neuromuscular control and coordination of the core and extremities of athletes. N. Am. J. Sports Phys. Ther. 4, 70–82.
Hua, J., Williams, G. J., Jin, H., Chen, J., Xu, M., Zhou, Y., et al. (2022). Early motor milestones in infancy and later motor impairments: a population-based data linkage study. Front. Psychiat. 13:809181. doi: 10.3389/fpsyt.2022.809181
Iverson, J. M. (2021). Developmental variability and developmental cascades: lessons from motor and language development in infancy. Curr. Dir. Psychol. 30, 228–235. doi: 10.1177/0963721421993822
Jackson, M. I., Kiernan, K., and McLanahan, S. (2017). Maternal education, changing family circumstances, and children's skill development in the United States and UK. Ann. Am. Acad. Polit. Soc. Sci. 674, 59–84. doi: 10.1177/0002716217729471
Jiménez-Pavón, D., Ruiz, J. R., Ortega, F. B., Artero, E. G., España-Romero, V., Castro-Piñero, J., et al. (2011). “Physical activity, fitness and fatness in children and adolescents,” in Epidemiology of Obesity in Children and Adolescents: Prevalence and Etiology, eds. L. A. Moreno, I. Pigeot, and W. Ahrens (New York, NY: Springer New York), 347–366.
Jouvent, R., Bungener, C., Morand, P., Millet, V., Lancrenon, S., Ferreri, M., et al. (1999). Distinction trait/état et anxiété en médecine générale: Étude descriptive. [The distinction between state/trait-anxiety in a medical survey: A descriptive study.]. L'Encéphale: Revue de psychiatrie clinique biologique et thérapeutique 25, 44–49.
Kaufman, A. S., and Kaufman, N. L. (2004). Kaufman Brief Intelligence Test, 2nd Edn. Circle Pines, MN: American Guidance.
Khan, N. A., Raine, L. B., Drollette, E. S., Scudder, M. R., Pontifex, M. B., Castelli, D. M., et al. (2014). Impact of the FITKids physical activity intervention on adiposity in prepubertal children. Pediatrics 133, e875–e883. doi: 10.1542/peds.2013-2246
Kindblom, J. M., Lorentzon, M., Hellqvist, Å., Lönn, L., Brandberg, J., Nilsson, S., et al. (2009). BMI changes during childhood and adolescence as predictors of amount of adult subcutaneous and visceral adipose tissue in men: the GOOD study. Diabetes 58, 867–874. doi: 10.2337/db08-0606
Kolunsarka, I., Gråsten, A., Huhtineimi, M., and Jaakkola, T. (2021). Development of children's actual and perceived motor competence, cardiorespiratory fitness, physical activity, and BMI. Med. Sci. Sports Exer. 53, 2653–2660. doi: 10.1249/MSS.0000000000002749
Kovacs, M. (1992). Manual for the Children's Depression Inventory. North Tonawanda NJ: Multi-Health Systems.
Kovacs, M. (2011). Children's Depression Inventory 2nd Edition Technical Manual; Multi-Health Systems. Ontario, ON: Inc.
Kuczmarski, R. J., Statistics, N. C. f. H., Health, N., and Survey, N. E. (2002). 2000 CDC Growth Charts for the United States: Methods and Development: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Hyattsville.
Lamb, K. L., Brodie, D. A., and Roberts, K. (1988). Physical fitness and health-related fitness as indicators of a positive health state. Health Promot. Int. 3, 171–182. doi: 10.1093/heapro/3.2.171
Liguori, G., and Medicine, A. C. o. S. (2020). ACSM's Guidelines for Exercise Testing and Prescription. Philadelphia, PA: Lippincott Williams & Wilkins.
Lingam, R., Jongmans, M. J., Ellis, M., Hunt, L. P., Golding, J., Emond, A., et al. (2012). Mental health difficulties in children with developmental coordination disorder. Pediatrics 129, e882–e891. doi: 10.1542/peds.2011-1556
Lino, F., and DPR, C. (2022). Developmental coordination disorder and most prevalent comorbidities: a narrative review. Children 9:1095. doi: 10.3390/children9071095
Lopes, V. P., Maia, J. A. R., Rodrigues, L. P., and Malina, R. (2012). Motor coordination, physical activity and fitness as predictors of longitudinal change in adiposity during childhood. Eur. J. Sport Sci. 12, 384–391. doi: 10.1080/17461391.2011.566368
Lubans, D. R., Morgan, P. J., Cliff, D. P., Barnett, L. M., and Okely, A. D. (2010). Fundamental movement skills in children and adolescents. Sports Med. 40, 1019–1035. doi: 10.2165/11536850-000000000-00000
Lung, F.-W., Shu, B.-C., Chiang, T.-L., and Lin, S.-J. (2009). Parental mental health, education, age at childbirth and child development from six to 18 months. Acta Paediatr. 98, 834–841. doi: 10.1111/j.1651-2227.2008.01166.x
Mancini, V. O., Rigoli, D., Cairney, J., Roberts, L. D., and Piek, J. P. (2016). The elaborated environmental stress hypothesis as a framework for understanding the association between motor skills and internalizing problems: a mini-review. Front. Psychol. 7:239. doi: 10.3389/fpsyg.2016.00239
Mannino, A., Sarapis, K., and Moschonis, G. (2022). The effect of maternal overweight and obesity pre-pregnancy and during childhood in the development of obesity in children and adolescents: a systematic literature review. Nutrients 13:5125. doi: 10.3390/nu14235125
Margulies, L., Horlick, M., Thornton, J. C., Wang, J., Ioannidou, E., Heymsfield, S. B., et al. (2005). Reproducibility of pediatric whole body bone and body composition measures by dual-energy x-ray absorptiometry using the GE Lunar Prodigy. J. Clin. Densitomet. 8, 298–304. doi: 10.1385/JCD:8:3:298
Maring, B., Greenspan, L. C., Chandra, M., Daniels, S. R., Sinaiko, A., Prineas, R. J., et al. (2015). Comparing US paediatric and adult weight classification at the transition from late teenage to young adulthood. Pediatr. Obes. 10, 371–379. doi: 10.1111/ijpo.274
Marmeleira, J., Veiga, G., Cansado, H., and Raimundo, A. (2017). Relationship between motor proficiency and body composition in 6- to 10-year-old children. J. Paediatr. Child Health 53, 348–353. doi: 10.1111/jpc.13446
Masten, A. S., and Cicchetti, D. (2010). Developmental cascades. Dev. Psychopathol. 22, 491–495. doi: 10.1017/S0954579410000222
Matheis, M., and Estabillo, J. A. (2018). “Assessment of fine and gross motor skills in children,” in Handbook of Childhood Psychopathology and Developmental Disabilities Assessment, ed. J. L. Matson (Cham: Springer International Publishing), 467–484.
Mattocks, C., Ness, A., Deere, K., Tilling, K., Leary, S., Blair, S. N., et al. (2008). Early life determinants of physical activity in 11 to 12 year olds: cohort study. Br. Med. J. 336, 26–29. doi: 10.1136/bmj.39385.443565.BE
Misirliyan, S., Boehning, A., and Shah, M. (2023). Development Milestones. [Updated 2023 Mar 16]. New York, NY: StatPearls.
Morano, M., Colella, D., and Caroli, M. (2011). Gross motor skill performance in a sample of overweight and non-overweight preschool children. Int. J. Pediatr. Obes. 6, 42–46. doi: 10.3109/17477166.2011.613665
Mota, J., Guerra, S., Leandro, C., Pinto, A., Ribeiro, J. C., Duarte, J. A., et al. (2002). Association of maturation, sex, and body fat in cardiorespiratory fitness. Am. J. Hum. Biol. 14, 707–712. doi: 10.1002/ajhb.10086
Noritz, G. H., Murphy, N. A., Panel, N. S. E., Murphy, N. A., Hagan, J. F. Jr., Lipkin, P. H., et al. (2013). Motor delays: early identification and evaluation. Pediatrics 131, e2016–e2027. doi: 10.1542/peds.2013-1056
Ortega, F. B., Ruiz, J. R., Hurtig-Wennlöf, A., Vicente-Rodríguez, G., Rizzo, N. S., Castillo, M. J., et al. (2010). Cardiovascular fitness modifies the associations between physical activity and abdominal adiposity in children and adolescents: the European Youth Heart Study. Br. J. Sports Med. 44, 256–262. doi: 10.1136/bjsm.2008.046391
Piek, J. P., Barrett, N. C., Smith, L. M., Rigoli, D., and Gasson, N. (2010). Do motor skills in infancy and early childhood predict anxious and depressive symptomatology at school age? Hum. Mov. Sci. 29, 777–786. doi: 10.1016/j.humov.2010.03.006
Piek, J. P., Dawson, L., Smith, L. M., and Gasson, N. (2008). The role of early fine and gross motor development on later motor and cognitive ability. Human Movement Science. 27, 668–681. doi: 10.1016/j.humov.2007.11.002
Pierce, M., Hope, H. F., Kolade, A., Gellatly, J., Osam, C. S., Perchard, R., et al. (2020). Effects of parental mental illness on children's physical health: systematic review and meta-analysis. Br. J. Psychiat. 217, 354–363. doi: 10.1192/bjp.2019.216
Raghuveer, G., Hartz, J., Lubans, D. R., Takken, T., Wiltz, J. L., Mietus-Snyder, M., et al. (2020). Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American Heart Association. Circulation 142, e101–e118. doi: 10.1161/CIR.0000000000000866
Raine, L. B., McDonald, K., Shigeta, T. T., Hsieh, S. S., Hunt, J., Chiarlitti, N. A., et al. (2021). Sympathetic nervous system and exercise affects cognition in youth (SNEACY): study protocol for a randomized crossover trial. Trials 22:154. doi: 10.1186/s13063-021-05096-w
Ribeiro, J., Leandro, C., Guerra, S., Oliveira, J., Duarte, J. A., Mota, J., et al. (2003). Cardiorespiratory fitness level and cardiovascular risk factors in school-aged girls. J. Hum. Mov. Stud. 45, 257–272.
Ridgway, C. L., Ong, K. K., Tammelin, T., Sharp, S. J., Ekelund, U., Jarvelin, M.-R., et al. (2009a). Birth size, infant weight gain, and motor development influence adult physical performance. Med. Sci. Sports Exer. 41, 1212–1221. doi: 10.1249/MSS.0b013e31819794ab
Ridgway, C. L., Ong, K. K., Tammelin, T. H., Sharp, S., Ekelund, U., Jarvelin, M.-., et al. (2009b). Infant motor development predicts sports participation at age 14 years: northern Finland birth cohort of 1966. PLoS ONE 4:e6837. doi: 10.1371/journal.pone.0006837
Rocha, N. A. C. F., dos Santos Silva, F. P., dos Santos, M. M., and Dusing, S. C. (2019). Impact of mother-infant interaction on development during the first year of life: a systematic review. J. Child Health Care 24, 365–385. doi: 10.1177/1367493519864742
Rock, C. L., Thomson, C., Gansler, T., Gapstur, S. M., McCullough, M. L., Patel, A. V., et al. (2020). American Cancer Society guideline for diet and physical activity for cancer prevention. Cancer J. Clin. 70, 245–271. doi: 10.3322/caac.21591
Ross, R., Blair, S. N., Arena, R., Church, T. S., Després, J.-P., Franklin, B. A., et al. (2016). Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation 134, e653–e699. doi: 10.1161/CIR.0000000000000461
Sangkarit, N., and Tapanya, W. (2024). Factors influencing on gross motor skills in infants: implications for walking development. Early Hum. Dev. 195:106076. doi: 10.1016/j.earlhumdev.2024.106076
Savage, T., Derraik, J. G., Miles, H. L., Mouat, F., Hofman, P. L., Cutfield, W. S., et al. (2013). Increasing maternal age is associated with taller stature and reduced abdominal fat in their children. PLoS ONE 8:e58869. doi: 10.1371/journal.pone.0058869
Schott, N., Alof, V., Hultsch, D., and Meermann, D. (2007). Physical fitness in children with developmental coordination disorder. Res. Quart. Exer. Sport 78, 438–450. doi: 10.1080/02701367.2007.10599444
Schott, N., Mündörfer, A., and Holfelder, B. (2023). Neighborhood socio-economic status influences motor performance and inhibitory control in kindergarten children-findings from the Cross-Sectional Kitafit Study. Children 10:1332. doi: 10.3390/children10081332
Sheldrick, R. C., Schlichting, L. E., Berger, B., Clyne, A., Ni, P., Perrin, E. C., et al. (2019). Establishing new norms for developmental milestones. Pediatrics 144:374. doi: 10.1542/peds.2019-0374
Shephard, R. J., Allen, C., Benade, A. J., Davies, C. T., Di Prampero, P. E., Hedman, R., et al. (1968). The maximum oxygen intake. An international reference standard of cardiorespiratory fitness. Bull. World Health Organ. 38, 757–764.
Sigurdsson, E., Os, J. V., and Fombonne, E. (2002). Are impaired childhood motor skills a risk factor for adolescent anxiety? results from the 1958 U.K. Birth Cohort and the National Child Development Study. Am. J. Psychiat. 159, 1044–1046. doi: 10.1176/appi.ajp.159.6.1044
Sorgente, V., Cohen, E. J., Bravi, R., and Minciacchi, D. (2021). Crosstalk between gross and fine motor domains during late childhood: the influence of gross motor training on fine motor performances in primary school children. Int. J. Environ. Res. Publ. Health 18:11387. doi: 10.3390/ijerph182111387
Spielberger, C. D. (1983). Manual for the State-Trait Anxiety Inventory. STAI Manual. Palo Alto, CA: Psychologist Press.
Squires, J., Potter, L., and Bricker, D. (1995). The ASQ User's Guide for the Ages & Stages Questionnaires: A Parent-Completed, Child-Monitoring System (Baltimore, MD: Paul H Brookes Publishing), 156-xvi.
Stierman, B., Afful, J., Carroll, M. D., Chen, T. C., Davy, O., Fink, S., et al. (2020). National Health and Nutrition Examination Survey 2017-March 2020 Prepandemic Data Files—Development of Files and Prevalence Estimates for Selected Health Outcomes, Report. Hyattsville, MD: NHS.
Taanila, A., Murray, G. K., Jokelainen, J., Isohanni, M., and Rantakallio, P. (2005). Infant developmental milestones: a 31-year follow-up. Dev. Med. Child Neurol. 47, 581–586. doi: 10.1111/j.1469-8749.2005.tb01207.x
Thelen, E. (1992). Development as a dynamic system. Curr. Dir. Psychol. 1, 189–193. doi: 10.1111/1467-8721.ep10770402
Thelen, E. (1995). Motor development: a new synthesis. Am. Psychol. 50, 79. doi: 10.1037/0003-066X.50.2.79
Thelen, E., Schöner, G., Scheier, C., and Smith, L. B. (2001). The dynamics of embodiment: a field theory of infant perseverative reaching. Behav. Brain Sci. 24, 1–34. doi: 10.1017/S0140525X01003910
Thelen, E., and Smith, L. (1998). “Dynamic systems theories,” in Handbook of Child Psychology, eds. W. Damon and R. Lerner (New York, NY: Wiley), 563–634.
Thurman, S. L., and Corbetta, D. (2017). Spatial exploration and changes in infant-mother dyads around transitions in infant locomotion. Dev. Psychol. 53:1207. doi: 10.1037/dev0000328
Utter, A. C., Robertson, R. J., Nieman, D. C., and Kang, J. (2002). Children's OMNI scale of perceived exertion: walking/running evaluation. Med. Sci. Sports Exer. 34, 139–144. doi: 10.1097/00005768-200201000-00021
Valadi, S., and Gabbard, C. (2020). The effect of affordances in the home environment on children's fine- and gross motor skills. Early Child Dev. Care 190, 1225–1232. doi: 10.1080/03004430.2018.1526791
Van Santvoort, F., Hosman, C. M., Janssens, J. M., Van Doesum, K. T., Reupert, A., Van Loon, L. M., et al. (2015). The impact of various parental mental disorders on children's diagnoses: a systematic review. Clin. Child Fam. Psychol. Rev. 18, 281–299. doi: 10.1007/s10567-015-0191-9
Venetsanou, F., and Kambas, A. (2010). Environmental factors affecting preschoolers' motor development. Early Childh. Educ. J. 37, 319–327. doi: 10.1007/s10643-009-0350-z
Warburton, D. E. R., Nicol, C. W., and Bredin, S. S. D. (2006). Health benefits of physical activity: the evidence. Can. Med. Assoc. J. 174, 801–809. doi: 10.1503/cmaj.051351
Ward, K. A., and Crabtree, N. J. (2019). Optimal Clinical Use of DXA in Children and Adolescents. Zaventum: Hologic BV.
Widiger, T. A., and Oltmanns, J. R. (2017). Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiat. 16, 144–145. doi: 10.1002/wps.20411
Wilhite, K., Booker, B., Huang, B. H., Antczak, D., Corbett, L., Parker, P., et al. (2022). Combinations of physical activity, sedentary behavior, and sleep duration and their associations with physical, psychological, and educational outcomes in children and adolescents: a systematic review. Am. J. Epidemiol. 192, 665–679. doi: 10.1093/aje/kwac212
Keywords: cardiorespiratory fitness, body composition, anxiety, depression, motor development, childhood
Citation: Card MR, Raine L, Zimmerman E, Schott N and Hillman CH (2024) Early motor developmental milestones and health outcomes in preadolescent children. Front. Dev. Psychol. 2:1509327. doi: 10.3389/fdpys.2024.1509327
Received: 10 October 2024; Accepted: 30 November 2024;
Published: 18 December 2024.
Edited by:
Jordan Ashton Booker, University of Missouri, United StatesReviewed by:
Anna Pouplier, Rigshospitalet, DenmarkValentina Stefanica, Polytechnic University of Bucharest, Romania
Copyright © 2024 Card, Raine, Zimmerman, Schott and Hillman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madison R. Card, Y2FyZC5tQG5vcnRoZWFzdGVybi5lZHU=
 Madison R. Card
Madison R. Card Lauren Raine
Lauren Raine Emily Zimmerman
Emily Zimmerman Nadja Schott
Nadja Schott Charles H. Hillman
Charles H. Hillman