
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Dent. Med., 01 April 2025
Sec. Aging and Dental Medicine
Volume 6 - 2025 | https://doi.org/10.3389/fdmed.2025.1522892
This article is part of the Research TopicOral Health and Care in the Elderly Population and Aging SocietyView all 3 articles
Oral health is essential for the overall well-being of aging adults, yet significant disparities persist in the United States, contributing to malnutrition, reduced quality of life, and social isolation. Despite advancements in preventive dentistry, older adults continue to face substantial oral health challenges. This study reviewed the current state of oral health among aging adults in the United States, analyzing national health surveys and existing preventive dentistry protocols to assess their effectiveness. National data indicated that a high percentage of older adults experience tooth loss, periodontal disease, and root caries. Results indicated that almost 40% of adults aged 65 and older have lost a significant number of teeth, and a large proportion of the aging adult population has suffered from high rates of caries and periodontal disease. Socioeconomic factors were found to significantly influence access to dental care. Key barriers included low income, inadequate insurance, and low oral health literacy exacerbating disparities. The study proposes a multifaceted approach to improve oral health equity, including policy changes, community-based preventive programs, enhanced geriatric dentistry education, and the integration of oral health into primary care. Addressing these disparities is needed to improve both oral and overall health outcomes for the growing elderly population in the United States.
Oral health is critical for overall health and quality of life, particularly for aging adults who are vulnerable to systemic health issues exacerbated by poor oral conditions. Chronic oral diseases, including tooth loss, periodontal disease, and untreated dental caries, are prevalent among adults aged 65 and older and are correlated with malnutrition, cognitive decline, cardiovascular disease, and other systemic conditions (1, 2). Studies indicate that tooth loss and poor oral health significantly impact dietary intake, limiting the ability to consume nutrient-rich foods such as fruits, vegetables, and lean proteins, which are essential for managing chronic diseases and supporting immune function (3–14). According to the U.S. Census Bureau, the number of adults aged 65 and older is projected to reach 98 million by 2060, underscoring the urgent need for effective interventions to address disparities in access and outcomes in oral healthcare (15).
Despite advancements in preventive dental practices, access remains inequitable. Vulnerable groups – including low-income, minority, and rural populations – face barriers like inadequate insurance, low oral health literacy, and limited local access to care. These disparities contribute to higher rates of caries and edentulism, creating a cycle of health inequity. Previous research has shown that these populations also experience a high prevalence of polypharmacy, leading to side effects such as xerostomia, which can further exacerbate caries risk. Given the interdependence of oral and systemic health, addressing these disparities is essential not only for oral health but also for overall health and well-being in aging adults (3, 4, 6, 7, 12, 16).
This study aims to review the literature and provide a comprehensive discussion on the evidence related to disparities in oral health access and outcomes among adults aged 65 and older in the United States. Additionally, we discuss the role of health literacy in this context and the consequences associated with oral health disorders.
The analysis emphasized the following three main areas: demographic disparities in access to health services and outcomes in oral health, health literacy, and the consequences of disparities in oral health. There was an examination of (i) differences in oral health outcomes by income, race, and insurance status, identifying populations most vulnerable to poor oral health outcomes; (ii) analysis of the role of oral health literacy in shaping preventive care behaviors and health outcomes, drawing on data from health literacy studies specific to older adults; (iii) the consequences of oral diseases, for example on the nutritional intake among adults and the relationship between oral health and chronic diseases, such as diabetes and cardiovascular disease, highlighting the implications of oral health disparities on broader health outcomes.
National Health and Nutrition Examination Survey data indicated that approximately 40% of adults aged 65 and older experience significant tooth loss, with about 13% who have lost all of their teeth (17). These issues were most prevalent among low socioeconomic and minority populations, particularly African American and Hispanic individuals (18). This tooth loss was shown to significantly limit dietary options, reducing intake of key nutrients that are more difficult to consume without functional dentition.
Socioeconomic and geographic factors further compounded these disparities. National data revealed that older adults with household incomes below the federal poverty level had more untreated dental caries compared to those with higher incomes (19). Rural older adults faced a significantly higher prevalence of tooth loss and untreated decay, with the gap pronounced in states that lack adequate dental workforce distribution (20). These systemic barriers contributed to persistent oral health inequities, especially affecting racial and ethnic minority communities who historically faced discrimination in healthcare access.
The prevalence of untreated caries and periodontal disease was high across the elderly population, with nearly 96% of older adults experiencing some degree of dental caries (21). Disparities were most pronounced among those with limited financial resources and inadequate insurance coverage. Periodontal disease and root caries presented higher risks for aging adults with chronic illnesses, notably diabetes, underscoring the importance of integrated care approaches.
Oral health literacy levels were notably low among older adults in low-income and minority populations, which limited their understanding of preventive care practices. This was directly correlated with lower utilization rates of dental services, as individuals with limited literacy in oral health were less likely to prioritize preventive care. This lack of preventive care contributes to the observed disparities in oral health outcomes (22).
Public education and health literacy campaigns would be beneficial as well. National public health campaigns to improve oral health literacy among aging adults and caregivers could facilitate better understanding and utilization of preventive practices. Emphasis on accessible information about the importance of regular dental visits, dietary considerations, and proper denture use would empower aging adults to make informed choices regarding their oral health. Programs targeting caregivers, particularly in long-term care settings, could focus on daily oral hygiene practices and the nutritional needs of older adults, thereby reducing preventable oral health issues and supporting systemic health (23).
The analysis revealed that poor oral health directly impacted dietary choices, reducing intake of high-fiber fruits and vegetables, lean proteins, and other nutrient-dense foods. Deficiencies in these essential nutrients may hasten Alzheimer's disease, Parkinson's disease, cognitive function, and systemic health problems such as cardiovascular disease, arterial inflammation, and diabetes, contributing to a downward spiral in both oral and systemic health (24–28). In addition, 88% of persons over the age of 60 are taking one or more medications (29). Additionally, the side effects of common medications taken by older adults, such as dry mouth, compounded these issues by increasing susceptibility to caries and other oral infections as well as difficulty speaking and swallowing (30, 31). Dry mouth, or hyposalivation, is a frequent side-effect of consuming multiple medicines, dehydration, diabetes, Sjögren's Syndrome, radiation, and chemotherapy (32). Periodontal disease causes individuals to decrease fiber intake in their diet, and this phenomenon is similar to those with partial or full dentures, as described in Figures 1–3 (8, 33, 59). Our previous research also indicated an association between clinical attachment level (CAL) and mortality. We found that individuals with increased CAL were more than twice as likely to have mortality due to cardiovascular disease than those with normal CAL, as shown in Figure 4 (10).
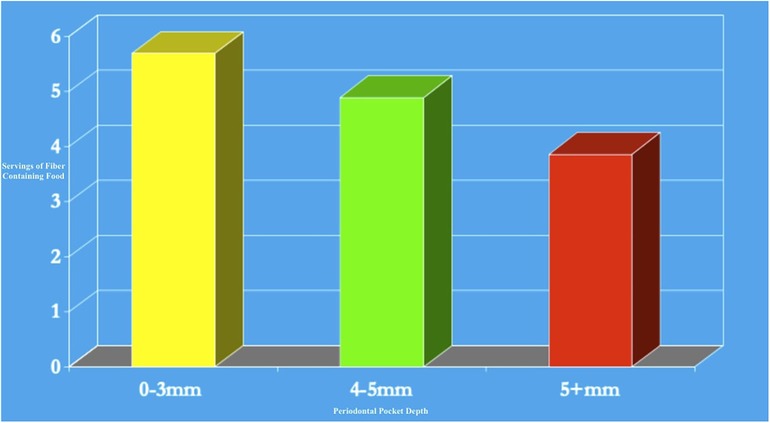
Figure 3. Dairy, green vegetable calories, and protein consumed in denture wearers compared to non-wearers (table adapted from Papas et al., 1998).
Research demonstrates that functional teeth and overall nutritional status are closely interconnected in older Americans (34). Nutritional status impacts oral health, while oral health directly affects one's ability to maintain proper nutrition (35, 36). For aging adults, a lifetime of poor dietary choices, insufficient oral hygiene, and untreated gingivitis can culminate in tooth pain, tooth loss, and inflamed, bleeding gums. These oral health problems create significant barriers to consuming nutritious foods like fresh fruits and vegetables, whole grains, lean meats, and hard cheeses, ultimately compromising both nutrient and caloric intake.
Older Americans who struggle with chewing and swallowing frequently show insufficient intake of essential nutrients, including fiber, linoleic acid, and various minerals such as potassium, calcium, magnesium, zinc, and selenium (37). They also often lack adequate levels of vitamins D, E, and K, as well as folate, biotin, and molybdenum (38). Studies have found that older adults without natural teeth or those who rely on dentures consume significantly fewer fruits and vegetables, particularly those rich in carotenoids and vitamin C, compared to those with natural teeth, as seen in Figure 2 (8, 33, 39, 40, 59). Instead, these individuals tend to favor carbohydrate-rich foods that are easier to chew, potentially worsening both their oral health and overall well-being.
Research has revealed that the number of natural teeth is inversely related to several health metrics, including BMI, waist circumference, blood pressure, and fasting blood glucose (41). Those who wear dentures frequently experience involuntary weight loss and frailty, as described in Figure 1 (8, 33, 42, 59). Scientific reviews have documented the complex pathophysiological pathways linking sarcopenia, dysphagia, and oral health, all of which contribute to increased frailty in older adults (43).
Appropriate dietary changes and improved oral hygiene habits can help individuals maintain healthier teeth, support a beneficial oral microbiome, and reverse the common trend toward tooth loss, decay, and gum disease (44). A 2018 systematic review of 26 studies found that well-nourished individuals had significantly more functional tooth units compared to those at risk of malnutrition or who were malnourished (36). This further reinforces the bidirectional connection between diet and oral health.
The frequent presence of fermentable carbohydrates – sugars and starches – in the mouth produces a greater cariogenic effect than the absolute quantity of carbohydrates consumed. Extended oral exposure to carbohydrates enhances the production of bacterial acids and microbial biofilm, does not allow saliva to neutralize the acids, and eventually leads to enamel demineralization (45–47). In periodontitis, the sugars also drive oxidative stress and may trigger a hyper-inflammatory state. To help clean teeth and stimulate saliva after meals and snacks, aging adults should brush their teeth with fluoridated toothpaste, floss and clean between teeth, or chew sugar-free gum (48). Research suggests that chewing sugar-free gum can improve salivary flow rates, reduce new dental caries by 28%, and lower oral biofilm and Streptococcus mutans levels (49, 50). While not a replacement for good dental hygiene, sugar-free gum can have a significant positive impact on dental health.
These nutritional impacts are particularly severe among socioeconomically disadvantaged populations. Among racial and ethnic minorities, the combination of poor oral health and limited access to nutritious foods creates a compound effect – African American and Hispanic older adults with untreated dental disease show lower consumption of fresh fruits and vegetables compared to white counterparts with similar oral health status (51). Rural elderly populations face additional challenges, as both limited dental access and food deserts contribute to poorer nutritional outcomes. In addition, inner-city poor individuals consumed more sugar and refined carbohydrates and had more oral disease. The inability to afford dental care often forces these vulnerable populations to rely on softer, more processed foods, and this phenomenon creates a cycle of declining oral and systemic health (52).
A combined approach of dietary improvements and enhanced oral hygiene can help older adults maintain healthier teeth, support a beneficial oral microbiome, and improve their overall nutritional status. Addressing these interconnected factors is important for promoting healthy aging and preventing the negative spiral of poor oral health leading to inadequate nutrition.
The findings highlight multiple interconnected factors driving oral health disparities among aging adults and underscore the need for targeted policy and healthcare interventions. Key recommendations include policy reforms to expand access. Expanding Medicare coverage to include routine dental services would address a substantial financial barrier for many aging adults, particularly those on fixed incomes. Medicaid expansions in states with limited dental benefits would also reduce disparities in underserved populations. Increased federal funding for oral health programs targeting aging adults, especially in low-income and rural areas, could enhance access to care and preventive services.
In addition, preventive and community-based programs would be advantageous. Community-based mobile dental clinics could improve access to care in rural areas, providing preventive services and screenings to older adults who otherwise lack access to routine dental care (41, 53). This is particularly valuable for those with mobility issues or transportation limitations. Expanding fluoride access in rural areas could prevent caries, reducing dental disease by approximately 25% among those exposed (54). A fluoridation program at this scale could result in significant cost savings, with an estimated $20 return on investment per $1 spent on water fluoridation, benefiting entire communities (55). Medical and dental curricula should emphasize geriatric dentistry, with a focus on preventive care, management of polypharmacy effects, and treatment of age-specific conditions. Provider training should also cover the nutritional impacts of oral health and the specific needs of elderly patients, particularly in underserved communities.
Given the link between oral health and systemic conditions, routine primary care visits for aging adults should include an oral health assessment. Primary care providers should receive training in basic oral health screening and counseling to reinforce preventive behaviors and facilitate timely referrals to dental professionals.
The inclusion of oral health-related dietary guidelines in the 2025–2030 Dietary Guidelines for Americans could further emphasize the importance of nutrient-dense, easy-to-chew foods, helping to mitigate the impact of poor oral health on diet and nutrition (3, 10, 56, 57). Recommendations would focus on foods high in fiber, vitamins, and minerals, critical for older adults' health. Efforts to promote soft-textured, nutrient-dense options could improve dietary intake among those with compromised oral function.
Initiatives have been implemented to address oral health inequalities in the United States. The Health Resources and Services Administration's Grants to States to Support Oral Health Workforce Activities program showed promise in expanding access to care in underserved areas, with greater access to oral healthcare in the Midwest and West (58). Initiatives like this one highlight both the potential for successful interventions and the ongoing challenges in addressing oral health inequalities systematically. More sustainable funding and broader policy support remain critical barriers to achieving comprehensive improvements in oral health equity.
This study underscores the substantial oral health challenges facing aging adults in the United States, particularly those in socioeconomically disadvantaged groups. The proposed recommendations – ranging from policy and insurance reforms to community-based programs and health literacy improvements – offer a framework to reduce disparities and improve outcomes for aging adults. An integrated approach addressing both preventive and therapeutic needs can enhance oral health and, consequently, overall health and quality of life for older adults. These strategies, if implemented, could foster a more equitable healthcare system, ensuring that all aging adults have access to essential oral health services and nutrition support.
AL: Writing – original draft, Writing – review & editing. MS: Writing – original draft, Writing – review & editing. AP: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Tsakos G, Watt RG, Rouxel PL, de Oliveira C, Demakakos P. Tooth loss associated with physical and cognitive decline in older adults. J Am Geriatr Soc. (2015) 63(1):91–9. doi: 10.1111/jgs.13190
2. Shen T, Lv J, Wang L, Wang W, Zhang D. Association between tooth loss and dementia among older people: a meta-analysis. Int J Geriatr Psychiatry. (2016) 31(8):953–5. doi: 10.1002/gps.4396
3. Papas A, Herman J, Palmer C, Rounds M, Russell R, McGandy R, et al. Oral health status of the elderly, with dietary and nutritional considerations. Gerodontology. (1984) 3(2):147–55. doi: 10.1111/j.1741-2358.1984.tb00366.x
4. Papas AS, Hefferren JH. Nutrition and preventive needs of older adults. Spec Care Dentist. (1987) 7(1):13–4. doi: 10.1111/j.1754-4505.1987.tb01558.x
5. Papas AS, Palmer CA, Rounds MC, Herman J, McGandy RB, Hartz SC, et al. Longitudinal relationships between nutrition and oral health. Ann N Y Acad Sci. (1989) 561:124–42. doi: 10.1111/j.1749-6632.1989.tb20976.x
6. Palmer CA, Papas A. Nutrition and the oral health of the elderly. World Rev Nutr Diet. (1989) 59:71–94. doi: 10.1159/000417075
7. Krall EA, Dawson-Hughes B, Papas A, Garcia RI. Tooth loss and skeletal bone density in healthy postmenopausal women. Osteoporos Int. (1994) 4(2):104–9. doi: 10.1007/bf01623233
8. Papas AS, Joshi A, Giunta JL, Palmer CA. Relationships among education, dentate status, and diet in adults. Spec Care Dentist. (1998) 18(1):26–32. doi: 10.1111/j.1754-4505.1998.tb01355.x
9. Papas AS, Palmer CA, Rounds MC, Russell RM. The effects of denture status on nutrition. Spec Care Dentist. (1998) 18(1):17–25. doi: 10.1111/j.1754-4505.1998.tb01354.x
10. Natto ZS, Aladmawy M, Alasqah M, Papas A. Is there a relationship between periodontal disease and causes of death? A cross sectional study. Braz Dent J. (2015) 26(1):33–8. doi: 10.1590/0103-6440201300117
11. Papas A, Hefferren J. Nutrition and preventive needs of older adults. Spec Care Dentist. (2008) 7:13–4. doi: 10.1111/j.1754-4505.1987.tb01558.x
12. Natto ZS, Aladmawy M, Alasqah M, Papas A. Factors contributing to tooth loss among the elderly: a cross sectional study. Singapore Dent J. (2014) 35:17–22. doi: 10.1016/j.sdj.2014.11.002
13. The National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Food and Nutrition Board, Food Forum. The national academies collection: reports funded by national institutes of health. Nutrition Across the Lifespan for Healthy Aging: Proceedings of a Workshop. Washington (DC): National Academies Press (US)
14. Qi X, Li Y, Fang C, Jia Y, Chen M, Chen X, et al. The associations between dietary fibers intake and systemic immune and inflammatory biomarkers, a multi-cycle study of NHANES 2015–2020. Front Nutr. (2023) 10:1216445. doi: 10.3389/fnut.2023.1242115
15. Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014–2060. Census.gov, editor. (2021). Available at: https://www.census.gov/library/publications/2015/demo/p25-1143.html (Accessed October 30, 2024).
16. Papas AS, Palmer CA, McGandy RB, Hartz SC, Russell RM. Dietary and nutritional factors in relation to dental caries in elderly subjects. Gerodontics. (1987) 3(1):30–7.3471616
17. CDC. Adults Aged 65+ who Have Lost all of Their Natural Teeth due to Tooth Decay or Gum Disease. Atlanta, GA: Centers for Disease Control and Prevention (2020).
18. Brennan DS, Singh KA. Dietary, self-reported oral health and socio-demographic predictors of general health status among older adults. J Nutr Health Aging. (2012) 16(5):437–41. doi: 10.1007/s12603-012-0006-3
19. Junger ML, Griffin SO, Lesaja S, Espinoza L. Awareness among US adults of dental sealants for caries prevention. Prev Chronic Dis. (2019) 16:E29. doi: 10.5888/pcd16.180398
20. Tiwari T, Scarbro S, Bryant LL, Puma J. Factors associated with tooth loss in older adults in rural Colorado. J Community Health. (2016) 41(3):476–81. doi: 10.1007/s10900-015-0117-y
21. CDC. Dental Caries Among Adults and Older Adults. Atlanta, GA: Centers for Disease Control and Prevention (2019).
22. Badran A, Keraa K, Farghaly MM. The impact of oral health literacy on dental anxiety and utilization of oral health services among dental patients: a cross sectional study. BMC Oral Health. (2023) 23(1):146. doi: 10.1186/s12903-023-02840-3
23. Kohli R, Nelson S, Ulrich S, Finch T, Hall K, Schwarz E. Dental care practices and oral health training for professional caregivers in long-term care facilities: an interdisciplinary approach to address oral health disparities. Geriatr Nurs. (2017) 38(4):296–301. doi: 10.1016/j.gerinurse.2016.11.008
24. Dioguardi M, Crincoli V, Laino L, Alovisi M, Sovereto D, Mastrangelo F, et al. The role of periodontitis and periodontal Bacteria in the onset and progression of Alzheimer’s disease: a systematic review. J Clin Med. (2020) 9(2):495–510. doi: 10.3390/jcm9020495
25. Chen CK, Wu YT, Chang YC. Periodontal inflammatory disease is associated with the risk of Parkinson’s disease: a population-based retrospective matched-cohort study. PeerJ. (2017) 5:e3647. doi: 10.7717/peerj.3647
26. Nilsson H, Berglund JS, Renvert S. Periodontitis, tooth loss and cognitive functions among older adults. Clin Oral Investig. (2018) 22(5):2103–9. doi: 10.1007/s00784-017-2307-8
27. Van Dyke TE, Kholy KE, Ishai A, Takx RAP, Mezue K, Abohashem SM, et al. Inflammation of the periodontium associates with risk of future cardiovascular events. J Periodontol. (2021) 92(3):348–58. doi: 10.1002/jper.19-0441
28. Luo H, Wu B, Kamer AR, Adhikari S, Sloan F, Plassman BL, et al. Oral health, diabetes, and inflammation: effects of oral hygiene behaviour. Int Dent J. (2022) 72(4):484–90. doi: 10.1016/j.identj.2021.10.001
29. Gu Q, Dillon CF, Burt VL. Prescription drug use continues to increase: U.S. Prescription drug data for 2007–2008. NCHS Data Brief. (2010) 29(42):1–8.20854747
30. Soto AP, Meyer SL. Oral implications of polypharmacy in older adults. Dent Clin North Am. (2021) 65(2):323–43. doi: 10.1016/j.cden.2020.11.007
31. Soto AP, Meyer SL. Oral implications of polypharmacy in older Adults. Clin Geriatr Med. (2023) 39(2):273–93. doi: 10.1016/j.cger.2023.01.008
33. Hartz SC, Russell RM, Rosenberg IH, Boston Nutritional Status S and Aging UHNRCo. Nutrition in the Elderly: The Boston Nutritional Status Survey. London, UK: Smith-Gordon; Niigata-shi, Japan: Nishimura; Herndon, VA, USA: Books International (1992).
34. Sahyoun NR, Lin C-L, Krall E. Nutritional status of the older adult is associated with dentition status. J Am Diet Assoc. (2003) 103(1):61–6. doi: 10.1053/jada.2003.50003
35. Marshall TA, Warren JJ, Hand JS, Xie X-J, Stumbo PJ. Oral health, nutrient intake and dietary quality in the very old. J Am Dent Assoc. (2002) 133(10):1369–79. doi: 10.14219/jada.archive.2002.0052
36. Toniazzo MP, Amorim P, Muniz FWMG, Weidlich P. Relationship of nutritional status and oral health in elderly: systematic review with meta-analysis. Clin Nutr. (2018) 37(3):824–30. doi: 10.1016/j.clnu.2017.03.014
37. Teixeira FB, Pereira Fernandes Lde M, Noronha PA, dos Santos MA, Gomes-Leal W, Ferraz Maia Cdo S, et al. Masticatory deficiency as a risk factor for cognitive dysfunction. Int J Med Sci. (2014) 11(2):209–14. doi: 10.7150/ijms.6801
38. Lieu PK, Chong MS, Seshadri R. The impact of swallowing disorders in the elderly. Ann Acad Med Singap. (2001) 30(2):148–54.11379412
39. Ervin RB, Dye BA. The effect of functional dentition on healthy eating index scores and nutrient intakes in a nationally representative sample of older adults. J Public Health Dent. (2009) 69(4):207–16. doi: 10.1111/j.1752-7325.2009.00124.x
40. Savoca MR, Arcury TA, Leng X, Chen H, Bell RA, Anderson AM, et al. Impact of denture usage patterns on dietary quality and food avoidance among older adults. J Nutr Gerontol Geriatr. (2011) 30(1):86–102. doi: 10.1080/01639366.2011.545043
41. CDC. 2020 Water Fluoridation Statistics. Atlanta, GA: Centers for Disease Control and Prevention (2020).
42. Kamdem B, Seematter-Bagnoud L, Botrugno F, Santos-Eggimann B. Relationship between oral health and Fried’s frailty criteria in community-dwelling older persons. BMC Geriatr. (2017) 17(1):174. doi: 10.1186/s12877-017-0568-3
43. de Sire A, Ferrillo M, Lippi L, Agostini F, de Sire R, Ferrara PE, et al. Sarcopenic dysphagia, malnutrition, and oral frailty in elderly: a comprehensive review. Nutrients. (2022) 14(5):982–98. doi: 10.3390/nu14050982
44. Nowjack-Raymer RE, Sheiham A. Association of edentulism and diet and nutrition in US adults. J Dent Res. (2003) 82(2):123–6. doi: 10.1177/154405910308200209
45. Atkinson FS, Khan JH, Brand-Miller JC, Eberhard J. The impact of carbohydrate quality on dental plaque pH: does the glycemic index of starchy foods matter for dental health? Nutrients. (2021) 13(8):2711–23. doi: 10.3390/nu13082711
46. Paes Leme AF, Koo H, Bellato CM, Bedi G, Cury JA. The role of sucrose in cariogenic dental biofilm formation–new insight. J Dent Res. (2006) 85(10):878–87. doi: 10.1177/154405910608501002
47. Suarez-Durall P, Mulligan R, Enciso R. Oral health for baby boomers: past, present, and future. Spec Care Dentist. (2023) 43(3):346–58. doi: 10.1111/scd.12829
48. Marchesan JT, Byrd KM, Moss K, Preisser JS, Morelli T, Zandona AF, et al. Flossing is associated with improved oral health in older adults. J Dent Res. (2020) 99(9):1047–53. doi: 10.1177/0022034520916151
49. Newton JT, Awojobi O, Nasseripour M, Warburton F, Di Giorgio S, Gallagher JE, et al. A systematic review and meta-analysis of the role of sugar-free chewing gum in dental caries. JDR Clin Trans Res. (2020) 5(3):214–23. doi: 10.1177/2380084419887178
50. Nasseripour M, Newton JT, Warburton F, Awojobi O, Di Giorgio S, Gallagher JE, et al. A systematic review and meta-analysis of the role of sugar-free chewing gum on plaque quantity in the oral cavity. Front Oral Health. (2022) 3:845921. doi: 10.3389/froh.2022.845921
51. Kibe LW, Bazargan M. Fruit and vegetable intake among older African American and Hispanic adults with cardiovascular risk factors. Gerontol Geriatr Med. (2022) 8:23337214211057730. doi: 10.1177/23337214211057730
52. Naavaal S, Griffin SO, Jones JA. Impact of making dental care affordable on quality of life in adults aged 45 years and older. J Aging Health. (2020) 32(7–8):861–70. doi: 10.1177/0898264319857967
53. Iheozor-Ejiofor Z, Worthington HV, Walsh T, O'Malley L, Clarkson JE, Macey R, et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. (2015) 75(6):Cd010856. doi: 10.1002/14651858.CD010856.pub2
54. CDC. Health and Economic Benefits of Oral Disease Interventions. Atlanta, GA: Centers for Disease Control and Prevention (2024).
55. O'Connell J, Rockell J, Ouellet J, Tomar SL, Maas W. Costs and savings associated with community water fluoridation in the United States. Health Aff (Millwood). (2016) 35(12):2224–32. doi: 10.1377/hlthaff.2016.0881
56. Moynihan PJ. The relationship between nutrition and systemic and oral well-being in older people. J Am Dent Assoc. (2007) 138(4):493–7. doi: 10.14219/jada.archive.2007.0201
57. Papas A. Nutrition and Oral Health in Aging in Nutrition Across the Lifespan for Healthy Aging: Proceedings of a Workshop of the National Academy of Science. Washington, DC: National Academies Press (2017).
58. Chou CF, Vallin T, Rogers S, Streeter RA, Worede I, Washko MM, et al. Impact of the health resources and services administration’s state oral health workforce grant program on dental workforce density and access to oral health care. Eval Program Plann. (2019) 75:43–53. doi: 10.1016/j.evalprogplan.2019.04.004
Keywords: aged, oral health, healthcare disparities, dental care for aged, health literacy, socioeconomic factors, periodontal diseases, dental caries
Citation: Lowenstein A, Singh ML and Papas AS (2025) Addressing disparities in oral health access and outcomes for aging adults in the United States. Front. Dent. Med. 6:1522892. doi: 10.3389/fdmed.2025.1522892
Received: 5 November 2024; Accepted: 10 March 2025;
Published: 1 April 2025.
Edited by:
Sherry Shiqian Gao, Xiamen University, ChinaReviewed by:
Francine Costa, International Center for Equity in Health, BrazilCopyright: © 2025 Lowenstein, Singh and Papas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Athena S. Papas, YXRoZW5hLnBhcGFzQHR1ZnRzLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.