- Department of Periodontics and Oral Implantology, SRM Dental College and Hospital, Chennai, India
Background: This review examines advancements in oral hygiene aids and their impact on gingival and periodontal health. As periodontal diseases are widespread, effective hygiene is vital. Enhancements in traditional tools and innovations have improved oral hygiene status. Clinical evidence confirms these innovations improve gingival and periodontal health, though proper use and patient adherence are crucial.
Methodology: A comprehensive literature search was conducted using MeSH terms like “Gingivitis/prevention & control*”, “Dental Plaque/prevention & control*”, “Dentifrices”, “Electrical Equipment and Supplies*”, “Toothbrushing”, “Equipment Design”, “Anti-Infective Agents/therapeutic use”, “Oils, Volatile/therapeutic use”, “Dental Devices, Home Care”, “Dentifrices*/therapeutic use”, “Vibration”, “Gingivitis*/drug therapy”, “Gingivitis*/prevention & control”, “Gingival Hemorrhage/prevention & control”, “Anti-Inflammatory Agents/pharmacology”, “Chlorhexidine/pharmacology”, “Mouthwashes/pharmacology”, “Anti-Bacterial Agents/pharmacology”, “Mouthwashes/therapeutic use”, “Anti-Infective Agents, Local*/therapeutic use”, “Mouthwashes/chemistry*”, “Plant Extracts/therapeutic use*”, “Sodium Dodecyl Sulfate/therapeutic use*”, “Treatment Outcome”, “Oral Hygiene/methods”, “Toothpastes/therapeutic use*”, “Hyaluronic Acid/therapeutic use”, “Chronic Periodontitis*/therapy”, “Periodontal Attachment Loss/therapy”, “Probiotics*/therapeutic use”, “Oral Hygiene*”, “Periodontal Index” and so on. This search utilized PubMed and Google Scholar, restricted to English-language publications from 2018 to 2024. The screening process involved reviewing titles, abstracts, and keywords, focusing on randomized clinical trials only. Inclusion criteria focused on novel innovations in conventional oral hygiene methodologies. A total of 86 randomized clinical trial articles met the inclusion criteria.
Results: Recent innovations in traditional oral hygiene tools have markedly enhanced oral hygiene levels and patient compliance. These newer innovations demonstrate substantial efficacy in plaque control and gingival health. Clinical outcomes underscore their pivotal role in improving oral hygiene standards, promoting reduced gingivitis and enhanced patient adherence to oral care regimens.
Conclusion: Advanced oral hygiene aids significantly improve gingival and periodontal health. However, patient adherence and correct usage are crucial for their optimal performance. Incorporating advanced oral hygiene aids into daily practices is essential for achieving optimal periodontal health, and continuous education is necessary to ensure their effective use.
1 Introduction
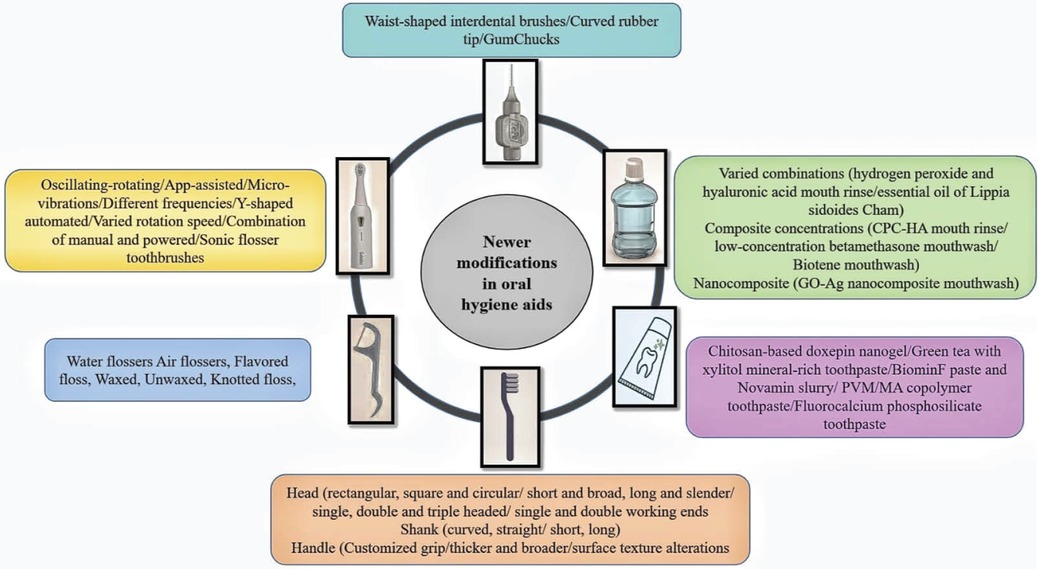
Periodontal diseases are among the most prevalent chronic health conditions worldwide, significantly affecting individuals’ quality of life and overall health. The primary etiology is the accumulation of bacterial biofilm on tooth surfaces, which initiates inflammation. Inadequate removal of dental deposits and neglect of specific areas can precipitate disease progression, leading to the breakdown of the tooth’s supportive structures and further complications (1). Effective oral hygiene practices are crucial for the prevention and management of periodontal diseases (2, 3). Over time, advancements in oral hygiene aids have markedly improved their effectiveness in maintaining optimal oral health. Traditional methods, including manual toothbrushes, dental floss, and mouth rinses, have long been essential components of daily oral care routines. However, these conventional tools often fail to remove plaque from all areas of the mouth, particularly interdental spaces and subgingival regions (4). Recognizing these limitations, more sophisticated tools have been developed to enhance plaque removal and reduce gingival inflammation. These innovations primarily focus on ergonomic designs that enhance precision, particularly in difficult-to-reach areas (5). Modifications in the shank and head sizes of toothbrushes, along with morphological adaptations in interdental brushes, aim to improve accessibility and cleaning efficacy. Electric toothbrushes featuring oscillating-rotating and sonic technologies have demonstrated superior efficacy in plaque removal compared to manual toothbrushes (6, 7). Interdental brushes and water flossers provide more effective cleaning of interdental spaces than traditional flossing techniques (8). Furthermore, antimicrobial mouthwashes, particularly those containing chlorhexidine, offer significant benefits in reducing periodontal pathogens and controlling gingivitis (9). Clinical research consistently demonstrates that the use of these advanced oral hygiene aids results in improved gingival and periodontal health outcomes, including reduced gingivitis, lower plaque indices, and decreased probing pocket depths. Despite these advancements, their effectiveness depends heavily on patient adherence and proper usage techniques. Therefore, continuous education and training on the correct use of these tools are essential to fully realize their benefits.
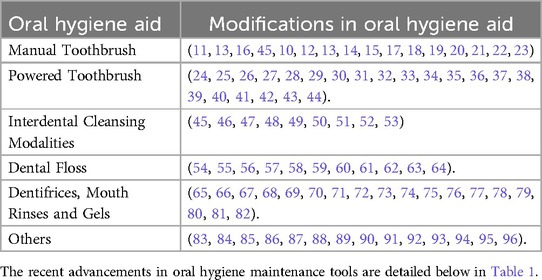
2 Oral hygiene aids
Essential to dental care are maintaining optimal oral health and preventing disorders, facilitated by various oral hygiene tools designed for thorough cleaning and plaque removal. These tools range from basic toothbrushes and floss to advanced electric toothbrushes, water flossers, and interdental brushes, each offering unique benefits. Understanding these oral hygiene maintenance modalities is crucial for effective oral care and dental health maintenance (Figure 1).
2.1 Manual toothbrushes
The efficacy of plaque removal is influenced by several factors including brushing duration, technique, and pressure, which can vary from person to person. Advancements in toothbrush design, aimed at addressing the limitations of traditional methods, have led to the creation of toothbrushes that are more effective at removing plaque compared to the flat-trimmed versions of the early 20th century. These modern toothbrushes feature a variety of bristle configurations, including different quantities, arrangements, lengths, diameters, and head designs. For instance, a 2018 study by Sandhya P. Naik and colleagues investigated the effectiveness of different bristle designs in individuals with fixed orthodontic appliances. Participants were divided into groups using flat, zigzag, and crisscross bristle toothbrushes. After four weeks, the crisscross bristle toothbrush showed the highest mean plaque reduction (10). Similarly, a 2019 study by Clara S. Kim et al. compared a novel bristleless toothbrush to a soft nylon-bristled one in adults undergoing periodontal maintenance, finding equivalent plaque removal and prevention of gingival inflammation, with potential benefits for gingival tissue recovery (11). Additionally, Zhipeng Xu et al. (2019) demonstrated that a manual toothbrush with CrissCross and tapered bristle technology significantly reduced gingivitis and improved plaque removal compared to a traditional flat-trim toothbrush (12). Research by Sara H. Rosenberg in 2018 showed that smooth handle toothbrushes had significantly lower bacterial contamination compared to grooved handle toothbrushes, based on DNA and endotoxin levels (13). A study by Fathima Fazrina Farook et al. in 2023 found that among patients with fixed orthodontic appliances, the Flat Trim (FT) toothbrush was superior in plaque removal after a single use compared to Cross Action (CA) and Orthodontic Type (OT) toothbrushes (14). Additionally, Vineet Kini et al. (2019) revealed that charcoal-infused bristle toothbrushes were more effective in plaque removal and exhibited less wear over time compared to nylon bristle toothbrushes (15). For children with cerebral palsy, custom-handled toothbrushes significantly improved oral hygiene and reduced bad breath over a week (16). In a similar vein, Dr. Lakshmi Krishnan’s team found that modified manual toothbrushes significantly reduced plaque and gingival scores in adolescents with cerebral palsy (17). Trupthi Rai et al. (2018) concluded that personalized toothbrushes notably enhanced oral hygiene and gingival health in cerebral palsy patients (18). Furthermore, Soncini JA and colleagues (1989) showed that individually modified toothbrushes substantially reduced plaque among cerebral palsy patients during clinic visits and at home (19). Tests of the Balene toothbrush in individuals with acquired brain injuries revealed effectiveness comparable to regular toothbrushes, whether used independently or with assistance (20). Studies also found that nanogold-coated toothbrushes significantly reduced microbial contamination and plaque (21) and that short-headed toothbrushes matched conventional ultrasoft ones in plaque removal, with user preference favoring the former due to its higher bristle count (22). Additionally, research highlighted the superior plaque removal of triple-headed and T-shaped toothbrushes compared to ultra-soft single-headed brushes, with variations in plaque scores noted across different toothbrush types and teeth locations (23).
2.2 Powered toothbrushes
Electric toothbrushes, utilizing oscillating-rotating or sonic technologies, outperform manual toothbrushes in plaque removal efficacy. Designed for consistent brushing and reaching difficult areas, they often feature timers and pressure sensors to enhance the user experience. Clinical studies confirm their effectiveness in reducing plaque and gingivitis, thus improving oral health. Gomez-Pereira et al. (2022) evaluated a prototype power toothbrush (PTB) with low rotation speed in “Gumline” and “Interdental” modes, finding that combined modes excelled in plaque removal compared to conventional and commercial PTBs (24). Similarly, Yılmaz Zafer Bilen et al. (2021) studied powered interactive toothbrushes vs. conventional ones during orthodontic treatment, noting improvements in periodontal health, suggesting the viability of powered toothbrushes for maintaining oral health during such treatments (25). An app-assisted interactive powered toothbrush also proved more effective than a manual toothbrush in reducing plaque and gingivitis, as well as preventing gingival abrasion (26). Klonowicz et al. (2018) tested a hybrid toothbrush adaptable for manual, sonic, or combined usage, finding it particularly effective in combined mode for plaque removal after a single use (27). An oscillating-rotating electric toothbrush with a unique round brush head also achieved superior plaque and gingivitis reduction compared to a manual toothbrush (28). Additionally, sonic-flosser toothbrushes with full-size brush heads were significantly better at improving gingival health and reducing plaque compared to manual toothbrushes and dental floss (29). Jing LV et al. (2018) found a novel high-frequency sonic toothbrush more effective at reducing plaque and equally effective at reducing gingivitis over six months compared to an oscillating-rotating toothbrush and a conventional sonic toothbrush (30). For children, a powered toothbrush developed by Mary Francis et al. (2021) showed potential for significant oral hygiene improvements (31). Erden and Camcı (2024) noted superior plaque elimination with an interactive electric toothbrush among orthodontic subjects but found no definitive link between toothbrush type and gingival index or specific salivary bacteria (32). Finally, Ralf Adam et al. (2020) found that the novel O-R toothbrush with micro-vibrations resulted in a significantly greater plaque reduction compared to the manual toothbrush (33). Barallat Lucia et al. (2022) compared an updated sonic toothbrush with a manual one, finding the sonic toothbrush more effective in reducing plaque after a single use (34). In another study, CUdent manual toothbrushes and the GoodAge triple lock toothbrush were equally effective in plaque removal and reducing gingival irritation among the elderly, with CUdent excelling in buccal plaque removal (35). Wang et al. (2022) found a compacted dual-head power toothbrush (DH) superior to a single-head (SH) in plaque removal among university students (36). Milleman et al. (2020) showed the ToothWave radiofrequency (RF) toothbrush significantly reduced plaque, calculus, and gingival inflammation compared to an ADA-approved powered toothbrush (37). Nevins et al. (2021) observed greater improvements in plaque and gingival inflammation with an ionic-sonic electric toothbrush compared to a manual one after one week (38). Takenouchi et al. (2021) highlighted the potential efficacy of high-frequency ultrasound toothbrushes in oral hygiene (39). Koşar et al. (2020) found no significant improvements with xylitol-infused toothbrushes in orthodontic patients (40). Statie et al. (2024) noted a Y-shaped automated electric toothbrush was superior to no brushing but inferior to manual brushing (41). Mylonopoulou et al. (2021) found no significant difference in efficacy between electric 3D and manual toothbrushes in orthodontic patients (42). Adam et al. (2020) and Grender et al. (2020) both demonstrated the superior performance of oscillating-rotating electric toothbrushes with micro-vibrations in reducing plaque and gingivitis compared to manual and sonic toothbrushes (43, 44).
2.3 Interdental cleansing modalities
Interdental cleaning methods encompass a range of tools crucial for thorough interdental hygiene. From conventional dental floss to modern water flossers and air flossers, each addresses specific needs. Specialized tools like rubber tip stimulators and oral irrigators offer tailored solutions. The choice depends on personal preference, interdental spaces, and dental needs, underscoring the guidance of dental professionals. Research indicates the efficacy of various methods in reducing gingivitis and plaque. Mirza et al. (2024) found the Philips Sonicare Cordless Power Flosser alongside a manual toothbrush notably reduced gingival inflammation (45). Moretti et al. (2020) showed dental floss and curved rubber bristle interdental cleaners to be equally effective (46). Li et al. (2024) highlighted the efficacy of the Philips Sonicare Power Flosser (47). Wehner et al. (2021) observed comparable plaque control between different interdental brushes (48). Graziani et al. (2018) demonstrated the effectiveness of various regimens in reducing plaque and gingival irritation (49). Pune N Paqué et al. (2020) concluded that waist-shaped interdental brushes cleaned proximal tooth surfaces better than cylindrical ones (50). Lastly, Erbe et al. (2023) and Hennequin-Hoenderdos et al. (2018) emphasized the efficacy of specific interdental brushes in reducing plaque and inflammation, respectively (51, 52). Stauff et al. (2018) provided insights into alternative devices for those struggling with traditional flossing methods (53).
2.4 Dental floss
Dental floss, available in various forms such as waxed, unwaxed, and flavored, plays a vital role in removing plaque and food debris between teeth. Waxed floss is ideal for narrow spaces, while unwaxed provides better traction for thorough cleaning. Flavored floss enhances user satisfaction, promoting consistent use. Specialized options, including dental tape and super floss, cater to specific needs like bridgework. Roa López et al. (2021) found knotted floss comparable to conventional floss for plaque removal, especially for beginners (54). Tyler et al. (2023) reported no additional benefits of using a manual toothbrush alongside a WaterPik® for fixed orthodontic appliances (55). Gomes et al. (2022) concluded that knotted flossing is as effective and safe as conventional flossing in reducing plaque and gingival inflammation (56). Muniz et al. (2018) noted that 2% chlorhexidine digluconate-infused floss significantly reduced supragingival interproximal biofilm (57). Studies by Wiesmüller et al. (2023) and Xu et al. (2023) demonstrated the effectiveness of oral irrigators and daily water flossing in managing gingival health (58, 59). Further, Araújo et al. (2020) and Mancinelli-Lyle et al. (2023) highlighted the benefits of text reminders and advanced flossing tools in periodontal health (60, 61). Lin et al. (2020) found GumChucks preferable for children’s plaque removal, and AlMoharib et al. (2024) observed both water and interdental flossing effective during orthodontic treatment (62, 63). Goyal et al. (2018) showed significant improvements in gingival health with combined Waterpik® and manual brushing (64).
2.5 Dentifrices, mouth rinses and gels
Dentifrices, mouthwashes, and gels provide various benefits for oral care, addressing needs like caries prevention, sensitivity relief, and bacterial control, with choices often guided by dental professionals. Kaur et al. (2021) found that a novel dental gel reduced probing depths and inflammation in periodontitis patients without initial scaling and root planing (65). Li et al. (2024) demonstrated a toothpaste’s effectiveness and safety for dentinal hypersensitivity (66). Newman et al. (2022) highlighted a mouth rinse that reduced plaque re-accumulation, though potential adverse effects were noted (67). Samiraninezhad et al. (2023) introduced a chitosan-based doxepin nanogel for oral mucositis, and Boccalari et al. (2022) found a hydrogen peroxide and hyaluronic acid mouth rinse effective for gingivitis (68, 69). Tadakamadla et al. (2020) revealed a CPC-HA mouth rinse was as effective as CHX in preventing plaque and gingivitis without staining (70). Soundarajan and Rajasekar (2023) developed a GO-Ag nanocomposite mouthwash for gingivitis, while Saliasi et al. (2018) and Montesani et al. (2024) tested formulations reducing gum bleeding and plaque (71–73). Research has scrutinized diverse toothpaste formulations, evaluating mouthwashes like “green tea” and “green tea with xylitol,” mineral-rich toothpaste for remineralization, and BiominF paste and Novamin slurry for orthodontically-induced white spot lesions. Studies have also examined toothpaste with PVM/MA copolymer for enamel erosion-rehardening, natural ingredient toothpaste for plaque and gingivitis improvement, and fluorocalcium phosphosilicate toothpaste for dentin hypersensitivity and acid erosion (74–79). Additionally, research has investigated the soft tissue desquamation from toothpaste, a post-foaming dental gel for reducing localized gingival inflammation, and the comparison between a new radiofrequency toothbrush and a sonic vibrating toothbrush for tooth stain reduction and shade improvement (80–82).
2.6 Others
Various combinations of interdental aids with manual or powered toothbrushing have been tested to improve oral hygiene, integrating automatic cleansing devices to enhance Oral Health-Related Quality of Life (OHRQoL). Educational initiatives promote awareness and patient motivation for optimal oral hygiene. Kimberly R. Milleman’s 2023 research found the Fresh Health Inc. system with manual toothbrushing (Fresh + MTB) superior to string floss with manual toothbrushing (floss + MTB) and manual toothbrushing alone (MTB) in reducing gingivitis, plaque, pocket depth, and bleeding on probing (BOP) (83). Keller et al. (2023) reported that while manual brushing reduced more plaque overall, the Y-brush had similar potential with better fit (84). Noraida Mamat (2022) found a T-shaped toothbrush improved children’s gingival health and plaque clearance (85). Padmini Hari’s 2021 study showed the SUN Teeth™ toothbrush was as effective as a conventional ADA toothbrush (86). Other studies (87–90) explored various innovative toothbrushes and incentives, with mixed results on plaque reduction and brushing frequency. Schnabl et al. (2021) compared a “ten seconds” auto-cleaning device to uninstructed manual toothbrushing, finding manual brushing more effective, highlighting the need for improved bristle design (91). Yang et al. (2024) evaluated a tooth-brushing guidance system in preschool children, revealing enhanced plaque removal in difficult areas like the tongue and palate (92). Sabbagh et al. (2020) studied Salvadora persica (miswak) sticks vs. fluoridated toothpaste, finding both effective in reducing plaque scores, with miswak also beneficial for salivary bacteria associated with lower caries risk (93). Saraf et al. (2023) assessed a cartoon-based educational aid vs. a conventional acrylic brushing model for preschoolers, with both methods effectively reducing plaque scores (94). Vouros et al. (2022) evaluated a protocol combining an air-abrasive device with ultrasonic instrumentation (GBT) vs. traditional Scaling and Root Planing (SRP), showing similar effectiveness but with shorter treatment times and better patient perception (95). Weber et al. (2024) investigated antimicrobial chewing gum’s impact on orthodontic patients, finding both experimental and control gums equally effective in reducing plaque and gingival inflammation, and improving OHRQoL (96).
3 Conclusion and future perspectives
The field of oral hygiene is undergoing rapid transformation, propelled by technological advancements, increased recognition of oral health’s integral role in overall well-being, and a growing demand for more effective and user-friendly products. Contemporary modifications in oral hygiene tools, such as electric toothbrushes with smart technology, water flossers, and interdental cleaners, have markedly improved the efficacy of daily oral care routines. These innovations provide more personalized, efficient, and accessible solutions, catering to diverse dental needs and preferences. These newer modifications play a pivotal role in the orthodontic-perio and prosthodontic-perio relationship, significantly enhancing plaque control and reducing inflammation, which are essential for maintaining oral health. In orthodontics, advanced tools like electric toothbrushes, interdental brushes, and water flossers enable patients with braces to clean hard-to-reach areas effectively, preventing gingivitis and periodontitis. In prosthodontics, antimicrobial mouthwashes and specialized cleaning devices promote the longevity and health of dental prostheses by minimizing bacterial accumulation around implants and prosthetic margins (97, 98). These innovations support the intricate balance between orthodontic and periodontal health, as well as prosthodontic and periodontal health, by fostering healthier gums and reducing the risk of periodontal complications. The incorporation of artificial intelligence and machine learning in oral hygiene devices is particularly promising, offering real-time feedback and tailored recommendations that enhance oral health outcomes. Furthermore, the development of eco-friendly and sustainable oral care products highlights a burgeoning commitment to environmental stewardship. Looking ahead, future advancements are anticipated to further refine these technologies, enhancing user experience, improving accessibility for underserved populations, and mitigating environmental impact. The integration of biotechnology, including probiotics and advanced biomaterials, holds substantial potential to revolutionize preventive care and treatment options, promoting a holistic approach to oral health. Sustained research and interdisciplinary collaboration will be essential in driving these innovations, ensuring that oral hygiene aids not only fulfill the evolving needs of consumers but also contribute to broader health and sustainability objectives. As oral health continues to be increasingly recognized as vital to overall health, the ongoing evolution of oral hygiene aids is poised to play a crucial role in fostering a healthier, more informed, and environmentally conscious society.
Author contributions
SP: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zini A, Mazor S, Timm H, Barker ML, Grender JM, Gerlach RW, et al. Effects of an oral hygiene regimen on progression of gingivitis/early periodontitis: a randomized controlled trial. Can J Dent Hyg. (2021) 55(2):85–94. 34221032
2. Caymaz MG, Buhara O. Association of oral hygiene and periodontal health with third molar pericoronitis: a cross-sectional study. Biomed Res Int. (2021) 2021:6664434. doi: 10.1155/2021/6664434
3. Clarkson J, Ramsay C, Lamont T, Goulao B, Worthington H, Heasman P, et al. Examining the impact of oral hygiene advice and/or scale and polish on periodontal disease: the IQuaD cluster factorial randomised controlled trial. Br Dent J. (2021) 230(4):229–35. doi: 10.1038/s41415-021-2662-3
4. Stenman J, Wennström JL, Abrahamsson KH. A brief motivational interviewing as an adjunct to periodontal therapy-A potential tool to reduce relapse in oral hygiene behaviours. A three-year study. Int J Dent Hyg. (2018) 16(2):298–304. doi: 10.1111/idh.12308
5. Harpenau L, Grill G, Storz M, Zingale J, Lundergan W, Chambers D. Blinded clinical evaluation of a new toothbrush design. J Clin Dent. (2015) 26(4):86–90. 26856013
6. Clerehugh V, Williams P, Shaw WC, Worthington HV, Warren P. A practice-based randomised controlled trial of the efficacy of an electric and a manual toothbrush on gingival health in patients with fixed orthodontic appliances. J Dent. (1998) 26(8):633–9. doi: 10.1016/s0300-5712(97)00065-1
7. Zimmer S, Nezhat V, Bizhang M, Seemann R, Barthel C. Clinical efficacy of a new sonic/ultrasonic toothbrush. J Clin Periodontol. (2002) 29(6):496–500. doi: 10.1034/j.1600-051x.2002.290604.x
8. Lyle DM, Goyal CR, Qaqish JG, Schuller R. Comparison of water flosser and interdental brush on plaque removal: a single-use pilot study. J Clin Dent. (2016) 27(1):23–6. 28390213
9. Ayesha S, Bhargava A, Philip AK, Sam G, Kumari D, George PP. Comparison of the antimicrobial activity of aloevera mouthwash with chlorhexidine mouthwash in fixed orthodontic patients. J Contemp Dent Pract. (2022) 23(7):743–8. doi: 10.5005/jp-journals-10024-3369
10. Naik SP, Punathil S, Shetty P, Jayanti I, Jalaluddin M, Avijeeta A. Effectiveness of different bristle designs of toothbrushes and periodontal status among fixed orthodontic patients: a double-blind crossover design. J Contemp Dent Pract. (2018) 19(2):150–5. doi: 10.5005/jp-journals-10024-2229
11. Kim CS, Chui S, Franc J, Boehm TK. A manual bristleless toothbrush demonstrates slight improvement in gingival recession compared to a conventional soft manual brush. Oral Health Prev Dent. (2019) 17(1):75–82. doi: 10.3290/j.ohpd.a41810
12. Xu Z, Cheng X, Conde E, Zou Y, Grender J, Ccahuana-Vasquez RA. Clinical assessment of a manual toothbrush with CrissCross and tapered bristle technology on gingivitis and plaque reduction. Am J Dent. (2019) 32(3):107–12. 31295390
13. Rosenberg SH, Lee C, Da Silva JD, Chen G, Ishikawa-Nagai S, Nagai M. The effect of a toothbrush handle design in combating microbial contamination. J Clin Dent. (2017) 28(3):62–4. 29211953
14. Farook FF, Alrumi A, Aldalaan K, Ababneh K, Alshammari A, Al-Khamees AA, et al. The efficacy of manual toothbrushes in patients with fixed orthodontic appliances: a randomized clinical trial. BMC Oral Health. (2023) 23(1):315. doi: 10.1186/s12903-023-03035-6
15. Kini V, Yadav S, Rijhwani JA, Farooqui A, Joshi AA, Phad SG. Comparison of plaque removal and wear between charcoal infused bristle and nylon bristle toothbrushes: a randomized clinical crossover study. J Contemp Dent Pract. (2019) 20(3):377–84. doi: 10.5005/jp-journals-10024-2525
16. Pasiga BD. Utilization of special grip toothbrushes for children with cerebral palsy. Syst Rev Pharm. (2020) 11(8):9–16. doi: 10.31838/SRP.2020.8.2
17. Krishnan L, Iyer K, Kumar PM. Effectiveness of two different modifications of manual toothbrush on plaque control -A multiple baseline trial among 12–17 year old children with cerebral palsy. IJDSIR. (2019) 2:462–7. 101738774.
18. Rai T, Ym K, Rao A, Anupama Nayak P, Natarajan S, Joseph RM. Evaluation of the effectiveness of a custom-made toothbrush in maintaining oral hygiene and gingival health in cerebral palsy patients. Spec Care Dentist. (2018) 38(6):367–72. doi: 10.1111/scd.12334
19. Soncini JA, Tsamtsouris A. Individually modified toothbrushes and improvement of oral hygiene and gingival health in cerebral palsy children. J Pedod. (1989) 13(4):331–4. 2534698
20. Mato EG, López LS, Freitas MD, Pazos MTA, Posse JL, Dios PD, et al. Plaque removal efficacy of a new toothbrush with a double-sided head and rotating handle-a pilot randomized control trial in acquired brain injury patients. Clin Oral Investig. (2023) 27(8):4855–60. doi: 10.1007/s00784-023-05106-y
21. Durgesh P, Sridharan S, Prabhu SK, Rao R, Rudresh V, Bangalore DH. Microbial contamination and plaque scores of nanogold-coated toothbrush. Int J Dent Hyg. (2020) 18(3):278–84. doi: 10.1111/idh.12433
22. Nair UP, Ravindra S, Reddy RN. Assessment of plaque control efficacy using two types of toothbrushes in young adults: an interventional crossover study. Int J Dent Hyg. (2023) 21(2):365–70. doi: 10.1111/idh.12621
23. Wu JH, Li JY, Du JK, Lee CY. Comparison of the plaque-removal efficacy of ultra-soft single-headed, triple-headed, and T-shaped toothbrushes and the subjective perceptions of users. J Oral Sci. (2023) 65(2):102–6. doi: 10.2334/josnusd.22-0307
24. Gomez-Pereira P, Axe A, Butler A, Qaqish J, Goyal CR. Plaque removal by a novel prototype power toothbrush versus a manual toothbrush: a randomized, exploratory clinical study. Clin Exp Dent Res. (2022) 8(4):849–57. doi: 10.1002/cre2.556
25. Bilen YZ, Çokakoğlu S, Öztürk F. The short-term effects of manual and interactive powered toothbrushes on the periodontal status of orthodontic patients: a randomized clinical trial. J World Fed Orthod. (2021) 10(1):14–9. doi: 10.1016/j.ejwf.2020.11.003
26. Gürbüz S, Çankaya ZT, Cinal E, Koçyiğit EG, Bodur A. Effects of interactive power toothbrush with or without application assistance on the plaque, gingivitis, and gingival abrasion among dental students: a randomized controlled clinical trial. Clin Oral Investig. (2022) 26(9):5931–41. doi: 10.1007/s00784-022-04553-3
27. Klonowicz D, Czerwinska M, Sirvent A, Gatignol JP. A new tooth brushing approach supported by an innovative hybrid toothbrush-compared reduction of dental plaque after a single use versus an oscillating-rotating powered toothbrush. BMC Oral Health. (2018) 18(1):185. doi: 10.1186/s12903-018-0647-7
28. Ccahuana-Vasquez RA, Adam R, Conde E, Grender JM, Cunningham P, Goyal CR, et al. A 5-week randomized clinical evaluation of a novel electric toothbrush head with regular and tapered bristles versus a manual toothbrush for reduction of gingivitis and plaque. Int J Dent Hyg. (2019) 17(2):153–60. doi: 10.1111/idh.12372
29. Mancinelli-Lyle D, Qaqish JG, Goyal CR, Schuller R. Effectiveness of a sonic-flosser toothbrush with different size brush heads and manual toothbrush plus dental floss on plaque, gingival bleeding and inflammation in adults with naturally occurring gingivitis: a 4-week randomized controlled trial. Int J Dent Hyg. (2023) 21(3):624–33. doi: 10.1111/idh.12675
30. Lv J, Guo B, Ling J. A 6-month clinical evaluation of a high frequency sonic toothbrush in comparison with an oscillating-rotating power toothbrush and a traditional sonic toothbrush in reducing gingivitis and plaque. Am J Dent. (2018) 31(4):171–6. 30106531
31. Francis M, Hooper WJ, Worob D, Huy G, Santos S, Goyal CR, et al. Comparative plaque removal efficacy of a new children’s powered toothbrush and a manual toothbrush: randomized, single use clinical study. Am J Dent. (2021) 34(6):338–44. 35051323
32. Erden T, Camcı H. Manual vs. interactive power toothbrush on plaque removal and salivary Streptococcus mutans and Lactobacillus casei levels: single-center, examiner-blinded, randomized clinical trial in orthodontic patients. J Orofac Orthop. (2024) 85(Suppl 1):41–51. doi: 10.1007/s00056-023-00470-6
33. Adam R, Erb J, Grender J. Randomized controlled trial assessing plaque removal of an oscillating-rotating electric toothbrush with micro-vibrations. Int Dent J. (2020) 70:S22–7. doi: 10.1111/idj.12568
34. Lucía B, Léna BK, Xavi C, Paniagua B, Pascual-La Rocca A. Efficacy of a new sonic powered toothbrush versus a manual toothbrush in a young population. A randomized cross-over clinical trial. Int J Dent Hyg. (2023) 21(2):382–8. doi: 10.1111/idh.12656
35. Nitipong V, Laiteerapong A, Lochaiwatana Y, Arunyanak SP. Clinical evaluation of toothbrushes for elderly patients: a crossover study. Int Dent J. (2023) 73(1):93–100. doi: 10.1016/j.identj.2022.10.001
36. Wang M, Zhao J, Zhang R, Li L, Shao J, Zheng Y, et al. Plaque removal efficacy of a compacted dual-head power toothbrush: a split-mouth randomized clinical trial. Am J Dent. (2022) 35(2):146–51. 35798710
37. Milleman KR, Levi L, Grahovac TL, Milleman JL. Safety and efficacy of a novel toothbrush utilizing RF energy for the reduction of plaque, calculus and gingivitis. Am J Dent. (2020) 33(3):151–6. 32470241
38. Nevins M, Chen CY, Kerr E, Mendoza-Azpur G, Isola G, Soto CP, et al. Comparison of a novel sonic toothbrush to manual brushing on plaque control and gingival inflammation: a multicenter, randomized, controlled clinical trial. Int J Periodontics Restorative Dent. (2021) 41(1):99–104. doi: 10.11607/prd.5363
39. Takenouchi A, Otani E, Satoho Y, Kakegawa Y, Arai H, Matsukubo T. Comparison of the effects of ultrasound toothbrushes with different frequencies on oral hygiene: a randomized-controlled clinical trial. Int J Dent Hyg. (2021) 19(4):376–81. doi: 10.1111/idh.12496
40. Koşar S, Çokakoğlu S, Kaleli İ. Effects of xylitol impregnated toothbrushes on periodontal status and microbial flora in orthodontic patients. Angle Orthod. (2020) 90(6):837–43. doi: 10.2319/022420-125.1
41. Statie MD, Lomonaco I, Nieri M, Giuntini V, Franceschi D, Franchi L. Efficacy of an automatic electric toothbrush with nylon bristles in dental plaque removal: a cross-over randomized controlled trial. Clin Oral Investig. (2024) 28(4):211. doi: 10.1007/s00784-024-05601-w
42. Mylonopoulou IM, Pepelassi E, Madianos P, Halazonetis DJ. A randomized, 3-month, parallel-group clinical trial to compare the efficacy of electric 3-dimensional toothbrushes vs manual toothbrushes in maintaining oral health in patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. (2021) 160(5):648–58. doi: 10.1016/j.ajodo.2021.02.016
43. Adam R, Ram Goyal C, Qaqish J, Grender J. Evaluation of an oscillating-rotating toothbrush with micro-vibrations versus a sonic toothbrush for the reduction of plaque and gingivitis: results from a randomized controlled trial. Int Dent J. (2020) 70:S16–21. doi: 10.1111/idj.12569
44. Grender J, Ram Goyal C, Qaqish J, Adam R. An 8-week randomized controlled trial comparing the effect of a novel oscillating-rotating toothbrush versus a manual toothbrush on plaque and gingivitis. Int Dent J. (2020) 70:S7–15. doi: 10.1111/idj.12571
45. Mirza F, Nelson M, Ambers J, Milleman K, Milleman J, Ward M. A randomized, parallel design study to compare the effects of different interdental cleaning modalities on gingivitis and plaque after a 6-week period of home use. Compend Contin Educ Dent. (2024) 45(Suppl 1):14–7. 38781412
46. Moretti AJ, Zhang S, Phillips ST, Williams K, Moss KL, Offenbacher S. Evaluation of a curved design rubber bristle interdental cleaner on patients with gingivitis. J Dent Hyg. (2020) 94(1):6–13. 32127424
47. Li J, Mirza F, Nelson M, Foster J, Amini P, Imtiaz U, et al. A randomized, parallel design study to compare the effects of two different interdental cleaning modalities on gingivitis and plaque after a 4-week period of home use. Compend Contin Educ Dent. (2024) 45(Suppl 1):10–3. 38781411
48. Wehner C, Husejnagic S, Laky B, Rausch-Fan X, Moritz A, Haririan H. Effect of interdental brush design on plaque during nonsurgical periodontal therapy. Clin Oral Investig. (2021) 25(1):87–94. doi: 10.1007/s00784-020-03337-x
49. Graziani F, Palazzolo A, Gennai S, Karapetsa D, Giuca MR, Cei S, et al. Interdental plaque reduction after use of different devices in young subjects with intact papilla: a randomized clinical trial. Int J Dent Hyg. (2018) 16(3):389–96. doi: 10.1111/idh.12318
50. Paqué PN, Attin T, Ender A, Al-Majid A, Wegehaupt F, Sener B, et al. Impact of interdental brush shape on interpapillary cleaning efficacy—a clinical trial. Sci Rep. (2020) 10(1):7922. doi: 10.1038/s41598-020-64816-5
51. Erbe C, Zanders-Grote L, Wagner Y, Schmidtmann I, Lang NP, Wehrbein H. Randomized multicenter study on the plaque removal efficacy of 2 interdental brushes around the base of orthodontic brackets. Am J Orthod Dentofacial Orthop. (2023) 164(4):466–75. doi: 10.1016/j.ajodo.2023.06.017
52. Hennequin-Hoenderdos NL, van der Sluijs E, van der Weijden GA, Slot DE. Efficacy of a rubber bristles interdental cleaner compared to an interdental brush on dental plaque, gingival bleeding and gingival abrasion: a randomized clinical trial. Int J Dent Hyg. (2018) 16(3):380–8. doi: 10.1111/idh.12316
53. Stauff I, Derman S, Barbe AG, Hoefer KC, Bizhang M, Zimmer S, et al. Efficacy and acceptance of a high-velocity microdroplet device for interdental cleaning in gingivitis patients-A monitored, randomized controlled trial. Int J Dent Hyg. (2018) 16(2):e31–7. doi: 10.1111/idh.12292
54. Roa López A, Moreu Burgos G, Aguilar Salvatierra A, Fernández Delgado J, Bravo M, González Jaranay M. Efficacy of dental floss with ellipsoidal knots vs conventional dental floss for plaque removal: a split-mouth randomized trial. Int J Dent Hyg. (2021) 19(2):209–14. doi: 10.1111/idh.12473
55. Tyler D, Kang J, Goh HH. Effectiveness of Waterpik® for oral hygiene maintenance in orthodontic fixed appliance patients: a randomised controlled trial. J Orthod. (2023) 50(4):367–77. doi: 10.1177/14653125231173708
56. Gomes AF, Rekhi A, Meru S, Divakar P. Efficacy, safety and patient preference of knotted floss technique in type II gingival embrasures. J Dent Hyg. (2022) 96(1):64–75. 35190495
57. Muniz FWMG, da Silva Lima H, Rösing CK, Martins RS, Moreira MMSM, Carvalho RdS. Efficacy of an unwaxed dental floss impregnated with 2% chlorhexidine on control of supragingival biofilm: a randomized, clinical trial. J Investig Clin Dent. (2018) 9(1):e12280. doi: 10.1111/jicd.12280
58. Wiesmüller V, Kasslatter M, Zengin B, Zotz D, Offermanns V, Steiner R, et al. Cleansing efficacy of an oral irrigator with microburst technology in orthodontic patients-a randomized-controlled crossover study. Clin Oral Investig. (2023) 27(5):2089–95. doi: 10.1007/s00784-023-05003-4
59. Xu X, Zhou Y, Liu C, Zhao L, Zhang L, Li H, et al. Effects of water flossing on gingival inflammation and supragingival plaque microbiota: a 12-week randomized controlled trial. Clin Oral Investig. (2023) 27(8):4567–77. doi: 10.1007/s00784-023-05081-4
60. Araújo MR, Alvarez MJ, Godinho CA. The effect of mobile text messages and a novel floss holder on gingival health: a randomized control trial. J Dent Hyg. (2020) 94(4):29–38. 32753522.
61. Mancinelli-Lyle D, Qaqish JG, Goyal CR, Schuller R. Efficacy of water flossing on clinical parameters of inflammation and plaque: a 4-week randomized controlled trial. Int J Dent Hyg. (2023 Nov) 21(4):659–68. doi: 10.1111/idh.12770
62. Lin J, Dinis M, Tseng CH, Agnello M, He X, Silva DR, et al. Effectiveness of the GumChucks flossing system compared to string floss for interdental plaque removal in children: a randomized clinical trial. Sci Rep. (2020 Feb 20) 10(1):3052. doi: 10.1038/s41598-020-59705-w
63. AlMoharib HS, Alqasem A, Almusfer G, Aldosari MA, Almadhoon HW. The effectiveness of water jet flossing and interdental flossing for oral hygiene in orthodontic patients with fixed appliances: a randomized clinical trial. BMC Oral Health. (2024) 24(1):498. doi: 10.1186/s12903-024-04166-0
64. Goyal CR, Qaqish JG, Schuller R, Lyle DM. Evaluation of the addition of a water flosser to manual brushing on gingival health. J Clin Dent. (2018) 29(4):81–6. 30942963
65. Kaur M, Geurs NC, Cobb CM, Otomo-Corgel J, Takesh T, Lee JH, et al. Evaluating efficacy of a novel dentifrice in reducing probing depths in stage I and II periodontitis maintenance patients: a randomized, double-blind, positive controlled clinical trial. J Periodontol. (2021) 92(9):1286–94. doi: 10.1002/JPER.20-0721
66. Li J, Han Q, Zhang L, Zhang J, Yin W, Zhong Y. Efficacy of a novel dentifrice containing bioactive glass-ceramic for dentinal hypersensitivity: a double-blind randomized controlled trial in Chinese adults. J Dent. (2024) 144:104898. doi: 10.1016/j.jdent.2024.104898
67. Newman BA, Rosebrough CN, Tamashiro RA, Dias Ribeiro AP, Whitlock JA, Sidhu G, et al. A randomized controlled trial to evaluate the effectiveness of a novel mouth rinse in patients with gingivitis. BMC Oral Health. (2022) 22(1):461. doi: 10.1186/s12903-022-02518-2
68. Samiraninezhad N, Rezaee M, Gholami A, Amanati A, Mardani M. A novel chitosan-based doxepin nano-formulation for chemotherapy-induced oral mucositis: a randomized, double-blinded, placebo-controlled clinical trial. Inflammopharmacology. (2023) 31(5):2411–20. doi: 10.1007/s10787-023-01325-7
69. Boccalari E, Tadakamadla SK, Occhipinti C, Lanteri V, Maspero C. Evaluation of the effectiveness of a novel mouth rinse containing hyaluronic acid and hydrogen peroxide on gingivitis: a randomized pilot controlled trial. Clin Exp Dent Res. (2022) 8(3):673–9. doi: 10.1002/cre2.498
70. Tadakamadla SK, Bharathwaj VV, Duraiswamy P, Sforza C, Tartaglia GM. Clinical efficacy of a new cetylpyridinium chloride-hyaluronic acid-based mouthrinse compared to chlorhexidine and placebo mouthrinses-A 21-day randomized clinical trial. Int J Dent Hyg. (2020) 18(1):116–23. doi: 10.1111/idh.12413
71. Soundarajan S, Rajasekar A. Antibacterial and anti-inflammatory effects of a novel herb-mediated nanocomposite mouthwash in plaque-induced gingivitis: a randomized controlled trial. Dent Med Probl. (2023) 60(3):445–51. doi: 10.17219/dmp/150728
72. Saliasi I, Llodra JC, Bravo M, Tramini P, Dussart C, Viennot S, et al. Effect of a toothpaste/mouthwash containing carica papaya leaf extract on interdental gingival bleeding: a randomized controlled trial. Int J Environ Res Public Health. (2018) 15(12):1–16. doi: 10.3390/ijerph15122660
73. Montesani L, Montesani L, Mateo L, Daep C, Huber N, Isapour G, et al. Antibacterial and clinical effectiveness of a mouthwash with a novel active system of amine+zinc lactate+fluoride: a randomized controlled trial. Clin Oral Investig. (2024) 28(1):90. doi: 10.1007/s00784-023-05487-0
74. Hajiahmadi M, Yegdaneh A, Homayoni A, Parishani H, Moshkelgosha H, Salari-Moghaddam R. Comparative evaluation of efficacy of “green tea” and “green tea with xylitol” mouthwashes on the salivary Streptococcus mutans and Lactobacillus colony count in children: a randomized clinical trial. J Contemp Dent Pract. (2019) 20(10):1190–4. . doi: 10.5005/jp-journals-10024-2652
75. Yilmaz MA, Gokkaya B, Yildiz PK, Bilsel SO, Kargul B. The effect of a novel toothpaste in children with white spot lesions. J Pak Med Assoc. (2022) 72(11):2170–4. doi: 10.47391/JPMA.2409
76. Salah R, Afifi RR, Kehela HA, Aly NM, Rashwan M, Hill RG. Efficacy of novel bioactive glass in the treatment of enamel white spot lesions: a randomized controlled trial✰. J Evid Based Dent Pract. (2022) 22(4):101725. doi: 10.1016/j.jebdp.2022.101725
77. Creeth JE, Burnett GR, Souverain A, Gomez-Pereira P, Zero DT, Lippert F, et al. In situ efficacy of an experimental toothpaste on enamel rehardening and prevention of demineralisation: a randomised, controlled trial. BMC Oral Health. (2020) 20(1):118. doi: 10.1186/s12903-020-01081-y
78. Nandlal B, Sreenivasan PK, Shashikumar P, Devishree G, Bettahalli Shivamallu A. A randomized clinical study to examine the oral hygiene efficacy of a novel herbal toothpaste with zinc over a 6-month period. Int J Dent Hyg. (2021) 19(4):440–9. doi: 10.1111/idh.12505
79. Patel VR, Shettar L, Thakur S, Gillam D, Kamala DN. A randomised clinical trial on the efficacy of 5% fluorocalcium phosphosilicate-containing novel bioactive glass toothpaste. J Oral Rehabil. (2019) 46(12):1121–6. doi: 10.1111/joor.12847
80. Green A, Crichard S, Ling-Mountford N, Milward M, Hubber N, Platten S, et al. A randomised clinical study comparing the effect of Steareth 30 and SLS containing toothpastes on oral epithelial integrity (desquamation). J Dent. (2019) 80(Suppl 1):S33–9. doi: 10.1016/j.jdent.2018.11.005
81. Levine JB, Goncalves J, Nguyen D, Nguyen O, Hasturk H. Efficacy of a novel post-foaming dental gel on gingival inflammation: a randomized controlled clinical trial. J Periodontol. (2020 Dec) 91(12):1569–83. doi: 10.1002/JPER.19-0594
82. Amaechi BT, Levi L, Silman Z, Evans V, Shehata MAS, Alonso-Ryan JR, et al. Clinical efficacy of a novel radiofrequency toothbrush for tooth stain reduction and tooth whitening: a randomized controlled trial. J Am Dent Assoc. (2022 Apr) 153(4):342–53. doi: 10.1016/j.adaj.2021.09.006
83. Milleman KR, Milleman JL, Gaff M, Cook K, Mateo L. Clinical efficacy of the oral health system by fresh health inc. In adults on gingivitis and plaque in a 3-arm, 30-day study as compared to string floss and manual brushing. Compend Contin Educ Dent. (2023) 44(Suppl 1):2–13. 38781418
84. Keller M, Keller G, Eller T, Sigwart L, Wiesmüller V, Steiner R, et al. Cleansing efficacy of an auto-cleaning toothbrushing device with nylon bristles: a randomized-controlled pilot study. Clin Oral Investig. (2023) 27(2):603–11. doi: 10.1007/s00784-022-04755-9
85. Mamat N, Mani SA, Danaee M. T-shaped toothbrush for plaque removal and gingival health in children: a randomized controlled trial. BMC Oral Health. (2022) 22(1):113. doi: 10.1186/s12903-022-02137-x
86. Hari P, Dutta S, Hanapi NSBM, Ali TBT, Thomas B, Tang TH, et al. Evaluation of the isosceles-configured SUN TeethTMtoothbrush in dental plaque removal and gingival health. Can J Dent Hyg. (2021) 55(2):101–9. 34221034
87. White JS, Ramos-Gomez F, Liu JX, Jue B, Finlayson TL, Garza JR, et al. Monetary incentives for improving smartphone-measured oral hygiene behaviors in young children: a randomized pilot trial. PLoS One. (2020) 15(7):e0236692. doi: 10.1371/journal.pone.0236692
88. Subburaman N, Madan Kumar PD, Iyer K. Effectiveness of musical toothbrush on oral debris and gingival bleeding among 6–10-year-old children: a randomized controlled trial. Indian J Dent Res. (2019) 30(2):196–9. doi: 10.4103/ijdr.IJDR_128_17
89. Nieri M, Giuntini V, Pagliaro U, Giani M, Franchi L, Franceschi D. Efficacy of a U-shaped automatic electric toothbrush in dental plaque removal: a cross-over randomized controlled trial. Int J Environ Res Public Health. (2020) 17(13):4649. doi: 10.3390/ijerph17134649
90. Jeong JS, Kim KS, Lee JW, Kim KD, Park W. Efficacy of tooth brushing via a three-dimensional motion tracking system for dental plaque control in school children: a randomized controlled clinical trial. BMC Oral Health. (2022) 22(1):626. doi: 10.1186/s12903-022-02665-6
91. Schnabl D, Wiesmüller V, Hönlinger V, Wimmer S, Bruckmoser E, Kapferer-Seebacher I. Cleansing efficacy of an auto-cleaning electronic toothbrushing device: a randomized-controlled crossover pilot study. Clin Oral Investig. (2021) 25(1):247–53. doi: 10.1007/s00784-020-03359-5
92. Yang M, Yang J, Zhao Y, Wei H, Shang Y. Enhancement plaque control in preschool children by an intelligent brushing guide device. J Clin Pediatr Dent. (2024) 48(2):121–8. doi: 10.22514/jocpd.2024.041
93. Sabbagh HJ, AlGhamdi KS, Mujalled HT, Bagher SM. The effect of brushing with Salvadora persica (miswak) sticks on salivary Streptococcus mutans and plaque levels in children: a clinical trial. BMC Complement Med Ther. (2020) 20(1):53. doi: 10.1186/s12906-020-2847-3
94. Saraf T, Hegde R, Shah P. A comparative evaluation of the learning outcome of toothbrushing in preschoolers by a novel cartoon-based education aid with conventional toothbrushing model education technique: a randomized controlled trial. J Indian Soc Pedod Prev Dent. (2023) 41(4):302–8. doi: 10.4103/jisppd.jisppd_496_23
95. Vouros I, Antonoglou GN, Anoixiadou S, Kalfas S. A novel biofilm removal approach (guided biofilm therapy) utilizing erythritol air-polishing and ultrasonic piezo instrumentation: a randomized controlled trial. Int J Dent Hyg. (2022) 20(2):381–90. doi: 10.1111/idh.12533
96. Weber J, Scholz KJ, Schenke IM, Pfab F, Cieplik F, Hiller KA, et al. Randomized controlled clinical trial on the efficacy of a novel antimicrobial chewing gum in reducing plaque and gingivitis in adolescent orthodontic patients. Clin Oral Investig. (2024) 28(5):272. doi: 10.1007/s00784-024-05669-4
97. Srimaneepong V, Heboyan A, Zafar MS, Khurshid Z, Marya A, Fernandes GVO, et al. Fixed prosthetic restorations and periodontal health: a narrative review. J Funct Biomater. (2022) 13(1):1–21. doi: 10.3390/jfb13010015
98. Scheerman JFM, van Meijel B, van Empelen P, Kramer GJC, Verrips GHW, Pakpour AH, et al. Study protocol of a randomized controlled trial to test the effect of a smartphone application on oral-health behavior and oral hygiene in adolescents with fixed orthodontic appliances. BMC Oral Health. (2018) 18(1):19. doi: 10.1186/s12903-018-0475-9
Keywords: toothbrush modifications, newer oral hygiene strategies, oral health technology, dental hygiene innovations, smart oral care devices
Citation: Palanisamy S (2024) Innovations in oral hygiene tools: a mini review on recent developments. Front. Dent. Med. 5:1442887. doi: 10.3389/fdmed.2024.1442887
Received: 3 June 2024; Accepted: 31 July 2024;
Published: 14 August 2024.
Edited by:
Davide Pietropaoli, University of L'Aquila, ItalyReviewed by:
Dinesh Rokaya, Walailak University International College of Dentistry, ThailandSara Di Nicolantonio, University of L'Aquila, Italy
Copyright: © 2024 Palanisamy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sucharitha Palanisamy, c3VjaGlwYWxhbmkxMjNAZ21haWwuY29t
 Sucharitha Palanisamy
Sucharitha Palanisamy