
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Dent. Med. , 07 March 2022
Sec. Dental Materials
Volume 3 - 2022 | https://doi.org/10.3389/fdmed.2022.768103
This article is part of the Research Topic Advanced Use of Materials in Orthodontics View all 9 articles
Aim: The aim of this study was to measure the transfer accuracy of computer-aided design/computer-aided manufacturing (CAD/CAM) insertion guides using mini-implants. The target value is the virtual planned position (100%). It is also clinically mandatory to use sterilised surgical guides (autoclaved at 137°C). The results obtained using sterilised and non-sterilised insertion guides were compared. In addition, the actual position of the mini-implants, as implemented, was compared with the digitally planned positions.
Materials and Methods: Following CAD/CAM planning and production of 60 insertion guides made from synthetic resins that had been previously tested for suitability, 120 mini-implants were inserted in pairs and in blocks of the bone of the substitute material. Half of the insertion guides were sterilised, while the other half were non-sterilised. Compared with the position of the mini-implants in the digital plans, deviations in the apical and coronal distances between the mini-implants and insertion depth, as well as the included angle of the mini-implants to one another and to the surface of the bone substitute material, were determined.
Results: In post-sterilisation, the dimensional and material changes were observed. When compared, the deviations to the virtual planned position were achieved when the performed insertion using sterilised insertion guides were lower than those achieved when using non-sterilised insertion guides. The heat treatment during the sterilisation process improved the accuracy of the insertion guides. When comparing sterile insertion guides to the digital planned position (100%), the mean coronal deviation was 0.057 mm (0.81%), the apical deviation was 0.428 mm (6.11%), and insertion depth mean deviation at the right side was 0.15 mm (2.15%), while that on the left was 0.073 mm (1.04%).
Conclusion: The CAD/CAM TAD insertion guide could not achieve 100% accuracy in translating the digitally planned position into the real anatomic location. Deviations to the ideal position between 0.81 and 6.11% were observed. Clinically, for appliances that fit post-mini-implant insertion, the coronal distance of the mid-mini-implant head is the most important. At this point, the mean deviation to the planned positions is 0.81%, which is clinically acceptable and most likely reproducible by using CAD/CAM insertion guides.
Mini-implants used in orthodontics have proved themselves over the last few decades as means of achieving maximum anchorage due to high success rates and a wide range of possible applications (1–4). The area of the jaw that is best suited for the insertion of mini-implants is the anterior palate (5–7) due to a large amount of the available bones and the minimal risk of damaging vital anatomical structures (8), such as tooth roots, blood vessels, and nerves. Many studies have shown that this region provides sufficient vertical bone height for secure placement of mini-implants (9). Baumgaertel et al. (10) reported a bone height of 8.68 ± 3.68 mm at the level between the first and second premolars. According to Hourfar et al. (11), the third pair of palatal rugae is considered an anatomical landmark. The precise planning of the position of the mini-implants was, on one hand, carried out using an analysis of an intraoral scan or plaster model and, on the other hand, by means of X-ray (lateral cephalogram or CBCT) (12, 13).
Insertion guides in dental implantology were developed to minimise the risk of damaging the anatomical structures and, at the same time, make ideal use of the available bone material (14). There are a multitude of factors that adversely affect the success of mini-implants. Some of these factors such as an incorrect insertion angle (15), incorrect insertion depth (16), and clinician inexperience (17) can be reduced by precise planning of the position and by the perioperative guidance of the insertion blade using an insertion guide (18). For this study, digitally manufactured CAD/CAM insertion guides that have already been described in the literature were used (14, 18, 19). According to various studies, the insertion depth can be well-controlled by using CAD/CAM-manufactured insertion guides (20, 21).
A central aspect that optimises treatment management is the preoperative preparation of the bone-borne orthodontic appliances (sliders, rapid palatal expanders, etc.) (20). These appliances can be designed and manufactured based on the digitally planned position of the mini-implant and enable a one-visit insertion of the mini-implant and appliance (Figure 1). Therefore, an accurate transfer of the digital planned position to the real anatomic location is essential.
The values of the following parameters are important for an optimal fit:
• Coronal distance
• Insertion depth
• Apical distance between the mini-implants
• An angle of the two mini-implants to one another
• An angle of the individual mini-implants to the surface.
This study aimed at measuring the transfer accuracy of CAD/CAM insertion guides using mini-implants. The target value is the virtual planned position (100%). It is also clinically mandatory to use sterilised surgical guides (autoclaved at 137°C). The results obtained using sterilised and non-sterilised insertion guides were compared. The actual position of the mini-implants, as implemented, was compared with the digitally planned positions.
As part of this study, CAD/CAM-planned insertion guides were produced using an STL dataset and a 3D printer (Formlabs, Form 2) (Figure 2).
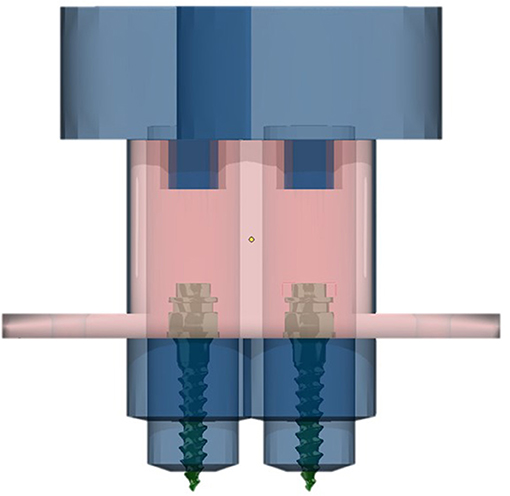
Figure 2. CAD/CAM planning of the insertion guide using Onyxceph (Image Instruments, Chemnitz, Germany).
First, three variants made of three different materials (white resin, dental LT clear resin, and dental SG resin: Formlabs) were printed, cured (Formcure UV, Formlabs, 60°C, 20 min), and autoclaved (Vakuclav 41 B, Melag, 135°C, 18.23 min; Figure 3). Only one material (Dental SG resin) exhibited a suitable behaviour for use in further tests.
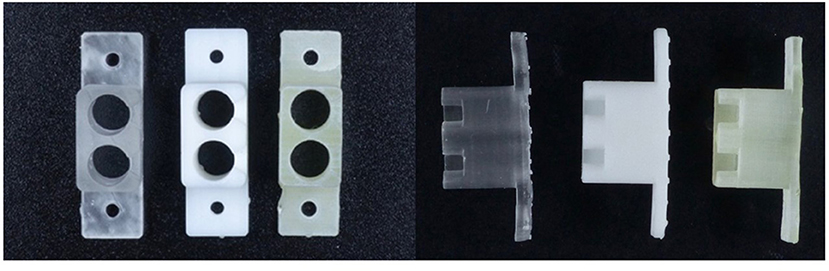
Figure 3. Three different materials (white resin, dental LT clear resin, dental SG resin: Formlabs) were printed, cured (Formcure UV, Formlabs, 60°C, 20 min), and then autoclaved (Vakuclav 41B, Melag, 135°C, 18.23 min).
Sixty identical insertion guides were produced from the above materials (Figure 4). As previously mentioned, they were cured in a curing chamber under UV light and further divided into two groups, with 30 insertion guides each. Random allocation using RandList-software was performed between the non-sterile and sterile groups.
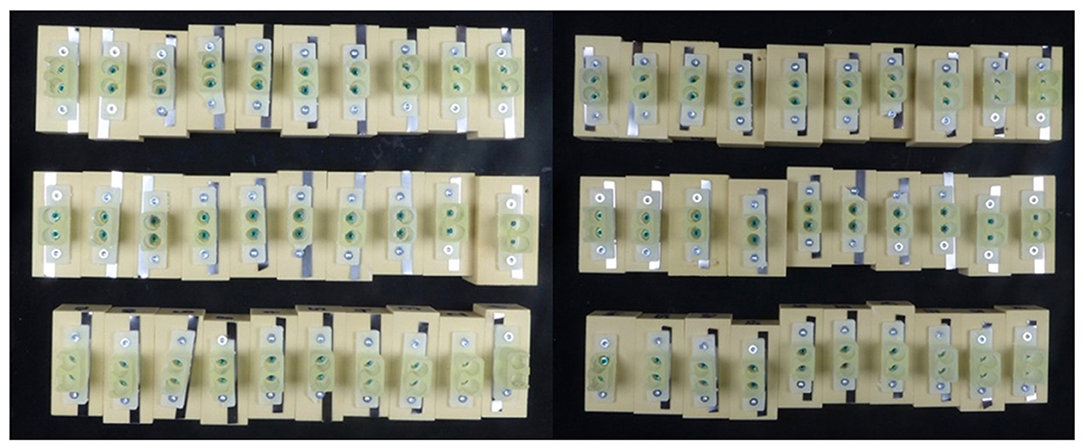
Figure 4. Sixty identical insertion guides were produced and divided into two groups, with 30 insertion guides each.
Group 1: the “non-sterile group” and Group 2: the “sterile group.” Accordingly, only the insertion guides in the second group were sterilised, and those in the first group remained non-sterile.
The insertion guides were fixed at 60 identical solid-rigid-foam bone substitute blocks (SawBones Europe AB, Malmö, Sweden), with a bone density of 40 PCF using screws (Connex, 10 mm). Since these mini-implants (OrthoEasy Pal Pins, Forestadent, 1.7 × 8 mm) were used in pairs, 120 mini-implants were needed.
Since the thread of the OrthoEasy Pal pin is a self-drilling type, no pre-drilling is necessary. Implantation was performed using a standard angled, double-green contra-angle hand piece using a ProFeel+ dental unit (Dentsply Sirona, Germany). The following device settings were defined: no torque limitation and a rotational speed of 60 rotations/min. All 120 insertions were performed by the same clinician. After every 10 mini-implants, a new insertion blade was utilised.
A steel strip was attached between the insertion guides and bone blocks to create a radiopaque layer for subsequent Cone-beam computed tomography (CBCT) images. These X-ray images were obtained using the Orthophos SL 3D X-ray device from Sirona (program VOL 2, 6 mA, 14.4 s). The scans were saved in the DICOM format.
The scans were analysed using the OnyxCeph software (Image Instruments, Chemnitz, Germany). Four measurement points were determined for the tips (points 3 and 4) and heads (points 1 and 2) of the mini-implants in each case. The following angles and distances were partly determined directly in the OnyxCeph program and partly calculated using SPSS for Windows (Statistics 21, SPSS Inc., USA) (Figure 5, Table 1).
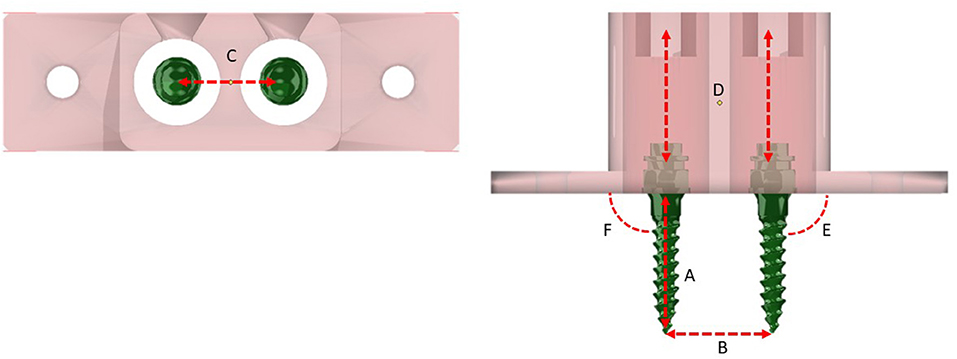
Figure 5. Measurements post insertion. (A) Insertion depth of the mini-implants. (B) Apical distance between the mini-implants. (C) Coronal distance between the mini-implants. (D) An angle of the mini-implants to one another. (E,F) An angle of the mini-implants to the surface of the bone substitute material.
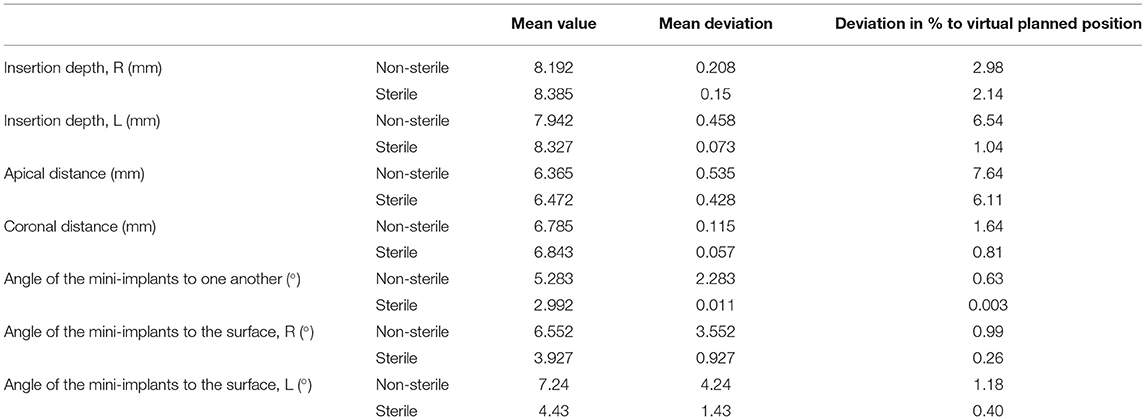
Table 1. Results of the analysis of post insertion position of the mini-implants and deviation in % to the virtually planned position.
The determined values were then compared with the target value (CAD/CAM planned position), and the associated deviations were ascertained.
Preliminary tests showed that only the Dental SG resin was suitable for further use in this study. In case of the other two materials, post-sterilisation dimensional imbalances and material changes occurred, rendering them unsuitable for further use. The results of this analysis are summarised in Table 1. Post-sterilisation, dimensional, and material changes were observed. When compared, the achieved deviations to the virtually planned position when performing the insertion using sterilised insertion guides were lower than those achieved when using non-sterilised insertion guides. Heat treatment during the sterilisation process improved the accuracy of the insertion guides. When comparing sterile insertion guides to the digitally planned position (100%), the mean coronal deviation was 0.057 mm (0.81%), the apical deviation was 0.428 mm (6.11%), and insertion depth mean deviation at the right side was 0.15 mm (2.15%), while that at the left was 0.073 mm (1.04%) (Table 1, Figure 6).
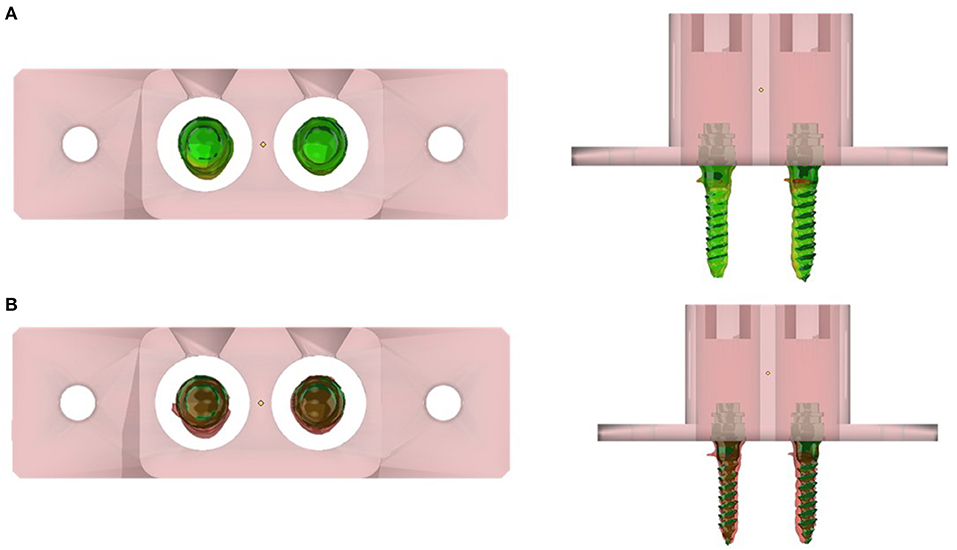
Figure 6. 3D colour-coded matching/superimposition of inserted mini-implants and digitally planned position: (A) at 0.1-mm deviation, and (B) 0.5-mm deviation.
The aim of this study was to evaluate the level of accuracy when implementing a digitally planned mini-implant position using sterilised and non-sterilised CAD/CAM insertion guides. For this purpose, mini-implants were inserted into a bone-substitute material, and their positioning was examined three-dimensionally and compared with the associated target tolerance values.
The results showed that all mean values were outliers to the target values. On comparing the mean deviations achieved, the studies revealed similar results. Möhlhenrich et al. (14), for example, compared the transfer accuracy of gingiva-borne (GBG) and tooth-borne (TBG) surgical guides made of silicone. He examined the parameters of lateral and vertical deviations as well as deviations in angulations. The values he determined were 0.8, 2.34 mm, and 3.6° for the lateral deviation, vertical deviation (TGB), and angulation (TGB), respectively. Compared with these results, smaller deviations were observed in the present study. Unlike Möhlhenrich et al., Cassetta et al. used CAD/CAM insertion guides (18) and examined the accuracy of the positioning of palatal mini-implants. They documented a deviation of 1.38, 1.73 mm, and 4.60° (1) for the coronal position, apical position, and angulation, respectively.
The deviations between the non-sterile and sterile groups recorded for each examined parameter showed that the sterilisation process had an impact on the material properties of the insertion guides. The accuracy is increased when sterilised insertion guides are used. To date, the material behaviour of synthetic resin insertion guides in the sterilisation process has not been examined in any comparative study. Most Class 1 and Class 2 resins need a temperature elevation during post-curing to fully achieve final polymerisation and ideal mechanical properties. The sterilisation process at 137°C seems to improve the polymerisation according to Bayarsaikhan et al. (22).
The use of insertion guides, made from a wide variety of materials, has been extensively described in literature (18–21, 23, 24). There are various options for materials, such as silicone, synthetic resin, or thermoforming films. Möhlhenrich et al. (14) believed that the elastic properties of silicone can lead to inaccuracies in the achieved insertion depth. There are no consistent results in the literature that shows that one system is superior to the other. In this study, CAD/CAM insertion guides made of a synthetic resin were used. According to the manufacturer (Formlabs), the material used is approved for use in dentistry and is also suitable for sterilisation. Similar results were documented with conventional dental implants in an in vitro study by Soares et al. (25). The angular deviation was 2.16 ± 0.92°. Overall, the authors rated the positions as promisingly precise. Similar results were observed in a meta-analysis by Van Assche et al. (26) who also evaluated the positional accuracy of dental implants. In that study, mean deviations of 0.99 mm in the coronal direction and 1.24 mm in the apical direction were documented. The angular deviation was 3.81°. These values were consistent with the results of our study.
Tatakis et al. (27) addressed the possible sources of errors that cause inaccuracies in the final implant position. They cited the gap between the guide unit of the insertion guides and the blade of the system in question as a possible cause. Their study showed that the effects on accuracy are proportional to the difference between the inner diameter of the guide sleeve and the outer diameter of the blade. However, Laederach et al. (28) noted that one cannot refrain from using a minimal gap as large mechanical frictional forces may arise. Another cause cited by Tatakis et al. (27) is the experience of the clinician, because, despite a guided insertion, it is possible to improve the implant positioning when the implantation is performed by an experienced clinician. These potential sources of error may be considered similar for dental implants as well as for orthodontic mini-implants.
• The CAD/CAM insertion guides were unable to implement a digitally planned position with 100% accuracy.
• Clinically, for appliances that fit post-mini-implant insertion, the coronal distance of the mid-mini-implant head is the most important. At this point, the mean deviation to the planned positions is 0.81%, which is clinically acceptable and most likely reproducible by using CAD/CAM insertion guides.
• The results obtained showed a similar level of accuracy compared with studies on dental implants.
• Heat treatment for mandatory clinical sterilisation improved the accuracy of the CAD/CAM insertion guide.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
LK conceived the project, gathered and processed the data, created the material presented (tables, electronic images, references, et cetera), and drafted the manuscript. BL translated and critically revised the manuscript. AV reviewed the process and critically revised the manuscript. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sherman AJ. Bone reaction to orthodontic forces on vitreous carbon dental implants. Am J Orthod. (1978) 74:79–87. doi: 10.1016/0002-9416(78)90047-7
2. Hourfar J, Bister D, Kanavakis G, Lisson JA, Ludwig B. Influence of interradicular and palatal placement of orthodontic mini-implants on the success (survival) rate. Head Face Med. (2017) 13:14. doi: 10.1186/s13005-017-0147-z
3. Leung MT, Lee TC, Rabie AB, Wong RW. Use of miniscrews and miniplates in orthodontics. J Oral Maxillofac Surg. (2008) 66:1461–6. doi: 10.1016/j.joms.2007.12.029
4. Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. (2009) 135:486–94. doi: 10.1016/j.ajodo.2007.05.019
5. Ludwig B, Glasl B, Bowman SJ, Wilmes B, Kinzinger GS, Lisson JA. Anatomical guidelines for miniscrew insertion: palatal sites. J Clin Orthod. (2011) 45:433–41; quiz: 467.
6. Hourfar J, Bister D, Lisson JA, Ludwig B. Incidence of pulp sensibility loss of anterior teeth after paramedian insertion of orthodontic mini-implants in the anterior maxilla (acccepted). Head Face Med. (2016) 13:1. doi: 10.1186/s13005-016-0134-9
7. Ludwig B, Baumgaertel S, Bowman JS. Mini-Implants in Orthodontics. Innovative Anchorage Concepts. London: Quintessence Publishing Co Ltd. (2008).
8. Hourfar J, Ludwig B, Bister D, Braun A, Kanavakis G. The most distal palatal ruga for placement of orthodontic mini-implants. Eur J Orthod. (2015) 37:373–8. doi: 10.1093/ejo/cju056
9. Winsauer H, Vlachojannis C, Bumann A, Vlachojannis J, Chrubasik S. Paramedian vertical palatal bone height for mini-implant insertion: a systematic review. Eur J Orthod. (2014) 36:541–9. doi: 10.1093/ejo/cjs068
10. Baumgaertel S. Quantitative investigation of palatal bone depth and cortical bone thickness for mini-implant placement in adults. Am J Orthod Dentofacial Orthop. (2009) 136:104–8. doi: 10.1016/j.ajodo.2008.11.020
11. Hourfar J, Kanavakis G, Bister D, Schatzle M, Awad L, Nienkemper M, et al. Three dimensional anatomical exploration of the anterior hard palate at the level of the third ruga for the placement of mini-implants–a cone-beam CT study. Eur J Orthod. (2015) 37:589–95. doi: 10.1093/ejo/cju093
12. Jung BA, Wehrbein H, Wagner W, Kunkel M. Preoperative diagnostic for palatal implants: is CT or CBCT necessary? Clin Implant Dent Relat Res. (2012) 14:400–5. doi: 10.1111/j.1708-8208.2009.00259.x
13. Baumgaertel S, Palomo JM, Palomo L, Hans MG. Reliability and accuracy of cone-beam computed tomography dental measurements. Am J Orthod Dentofacial Orthop. (2009) 136:19–25; discussion: 25–8. doi: 10.1016/j.ajodo.2007.09.016
14. Möhlhenrich SC, Brandt M, Kniha K, Prescher A, Hölzle F, Modabber A, et al. Accuracy of orthodontic mini-implants placed at the anterior palate by tooth-borne or gingiva-borne guide support: a cadaveric study. Clin Oral Invest. (2019) 23:4425–31. doi: 10.1007/s00784-019-02885-1
15. Kuroda S, Tanaka E. Risks and complications of miniscrew anchorage in clinical orthodontics. Jpn Dent Sci Rev. (2014) 50:79–85. doi: 10.1016/j.jdsr.2014.05.001
16. Tsaousidis G, Bauss O. Einfluss der insertionsstelle auf die misserfolgsraten kieferorthopädischer verankerungsschrauben. J Orofac Orthop. (2008) 69:349–56. doi: 10.1007/s00056-008-0809-3
17. Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. (2006) 130:18–25. doi: 10.1016/j.ajodo.2004.11.032
18. Cassetta M, Altieri F R., Di Giorgio, Barbato E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: description of a technique. Int J Oral Maxillofac Surg. (2018) 47:1195–8. doi: 10.1016/j.ijom.2018.03.018
19. Liu H, Liu DX, Wang G, Wang CL, Zhao Z. Accuracy of surgical positioning of orthodontic miniscrews with a computer-aided design and manufacturing template. Am J Orthod Dentofacial Orthop. (2010) 137:728.e1–10; discussion: 728–9. doi: 10.1016/j.ajodo.2009.12.025
20. Gabriele O, Dallatana G, Riva R, Vasudavan S, Wilmes B. The easy driver for placement of palatal mini-implants and a maxillary expander in a single appointment. J Clin Orthodont. (2017) 51:728–37.
21. Maino BG, Paoletto E, Lombardo L III, Siciliani G. A Three-dimensional digital insertion guide for palatal miniscrew placement. J Clin Orthod. (2016) 50:12–22.
22. Bayarsaikhan E, Lim J-H, Shin S-H, Park K-H, Park Y-B, Lee J-H, et al. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers. (2021) 13:1180. doi: 10.3390/polym13081180
23. Tosun T, Keles A, Erverdi N. Method for the placement of palatal implants. Int J Oral Maxillofac Implants. (2002) 17:95–100.
24. Morea C, Hayek JE, Oleskovicz C, Dominguez GC, Chilvarquer I. Precise insertion of orthodontic miniscrews with a stereolithographic surgical guide based on cone beam computed tomography data: a pilot study. Int J Oral Maxillofac Implants. (2011) 26:860–5.
25. Soares MM, Harari ND, Cardoso ES, Manso MC, Conz MB, Vidigal GM Jr. An in vitro model to evaluate the accuracy of guided surgery systems. Int J Oral Maxillofac Implants. (2012) 27:824–31.
26. Van Assche N, Vercruyssen M, Coucke W, Teughels W, Jacobs R, Quirynen M. Accuracy of computer-aided implant placement. Clin Oral Implants Res. (2012) 23(Suppl 6):112–23. doi: 10.1111/j.1600-0501.2012.02552.x
27. Tatakis DN, Chien HH, Parashis AO. Guided implant surgery risks and their prevention. Periodontol 2000. (2019) 811:194–208. doi: 10.1111/prd.12292
Keywords: CAD/CAM, TAD, 3D printing, mini-implants, palate, insertion guides
Citation: Ludwig B, Krause L and Venugopal A (2022) Accuracy of Sterile and Non-Sterile CAD/CAM Insertion Guides for Orthodontic Mini-Implants. Front. Dent. Med. 3:768103. doi: 10.3389/fdmed.2022.768103
Received: 31 August 2021; Accepted: 24 January 2022;
Published: 07 March 2022.
Edited by:
Paolo M. Cattaneo, University of Melbourne, AustraliaReviewed by:
Satoshi Yamaguchi, Osaka University, JapanCopyright © 2022 Ludwig, Krause and Venugopal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Björn Ludwig, Ymx1ZHdpZ0BraWVmZXJvcnRob3BhZWRpZS1tb3NlbC5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.