
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Dent. Med. , 17 October 2022
Sec. Systems Integration
Volume 3 - 2022 | https://doi.org/10.3389/fdmed.2022.1003041
This article is part of the Research Topic Frontiers in Dental Medicine: Highlights in Systems Integration 2021/22 View all 8 articles
 Anjali R. Truitt1
Anjali R. Truitt1 Stephen E. Asche1*
Stephen E. Asche1* Jeanette Y. Ziegenfuss1
Jeanette Y. Ziegenfuss1 Shannon G. Mitchell2
Shannon G. Mitchell2 Jan Gryczynski2
Jan Gryczynski2 Sheryl M. Kane1
Sheryl M. Kane1 Donald C. Worley1
Donald C. Worley1 D. Brad Rindal1*
D. Brad Rindal1*
Introduction: Few studies have assessed the impact of clinical decision support, with or without patient education, on patient-reported outcomes in dentistry. This cross-sectional survey was conducted to understand patients' experience with shared decision-making and pain management associated with a tooth extraction.
Methods: We administered a phone survey to 981 adult patients within a week of having a tooth extraction. The tooth extraction was performed at a large regional dental practice by a dentist participating in a randomized controlled trial of a clinical decision support system to reduce reliance on opioids for tooth extraction-related pain management. The survey compared respondents' answers by study arm: standard practice (SP) or clinical decision support with (CDS-E) or without patient education (CDS).
Results: Of respondents (n = 492, response rate: 52%), 91% reported that their dental provider talked about what to expect for pain in the days following the extraction, 92% stated that their dental provider talked about how to treat post-extraction pain, and 74% expressed they were confident in their ability to manage post-extraction pain at the end of the extraction visit. We found no statistically significant differences in patient responses across study arms for average pain in the 3 days following the extraction (p = 0.65, CDS vs. SP; p = 0.41, CDS-E vs. SP) or in shared decision-making (p = 0.38, CDS vs. SP; p = 0.70, CDS-E vs. SP).
Conclusion: Most patients reported adequate pain management and shared decision-making about pain management related to their tooth extraction. Further research will assess differences in analgesic recommendations across study arms.
Unintentional injury, including drug overdoses, is the leading cause of death in the United States for those aged 1–44 (1). More than half of these drug overdose deaths involve opioids (2). Between 1999 and 2018, this resulted in about half a million opioid-related deaths (3). Unnecessary opioid prescribing has been identified as a contributing factor to this major public health issue.
While the amount of opioids prescribed began to decrease in 2011 (4), some research shows that the number of opioid prescriptions written by dentists has increased between 2011 and 2015 (5, 6). In recognition of the role of dentists in fueling opioid overprescribing, the American Dental Association issued guidelines supporting opioid dose and duration limits, as well as considering nonsteroidal anti-inflammatory analgesics as the first-line therapy (7, 8). Further work shows dentists still have opportunities to align their prescribing behavior with these guidelines (9). Of note, dentists prescribed more opioids to young people (<21 years of age) than any other provider type, including surgeons and emergency medicine physicians (10). This prescribing is likely attributed to third molar extractions occurring in adolescents and young adults. Dentist opioid prescribing to opioid-naïve patients in this age group is associated with subsequent opioid use (11, 12). Current research emphasizes the need for dentist-focused interventions to curb unnecessary opioid prescribing. Clinical decision support (CDS) systems have been one of the strategies used to modify prescribing behavior (13–16). This body of literature largely focuses on primary care providers, while work in dentistry has been more limited.
To address these evidence gaps, we designed a clinical decision support tool targeting dentists' opioid prescribing. The tool was embedded in the electronic health record, providing the dentist with patient-tailored information and messaging. We conducted a 3-arm, cluster-randomized clinical trial (with dentist as the unit of randomization) to assess whether CDS with and without patient education decreases opioid prescribing for tooth extractions compared to standard practice. We expected that if the CDS was effective at providing personalized information to dentists, and they relayed this in their communication with patients about post-extraction pain, patients would report increased shared decision-making. We also expected that if the CDS was effective at changing dentists' medication recommendations, such that dentists substituted non-opioid analgesics for opioids, patients would report similar pain across arms. This paper explores whether an intervention aimed at de-implementing opioid use for post-extraction pain management impacted the patient experience of post-extraction pain management, including shared decision-making, post-extraction pain, and patient-reported self-care strategies to manage post-extraction pain.
This project was conducted in a large integrated healthcare system in the Greater Minneapolis-St. Paul metropolitan with more than 60 dentists practicing at 20 sites. Dentists were eligible for the trial if they performed permanent tooth extractions within the healthcare system on a regular basis in the year before the intervention period. Eligible dentists were randomized to standard practice (SP), clinical decision support (CDS), or CDS enhanced with patient education (CDS-E). Randomization was stratified by provider type (dentist vs. oral surgeon) and volume of opioid prescribing during the baseline period.
The CDS offered guidance about pain management recommendations personalized to the patient, including potential medication interactions between the patient's current medication list and commonly recommended analgesics, a summary of potentially relevant health conditions that may impact pain management approaches, and automated access to the state's Prescription Drug Monitoring Program. If the dentist performing the extraction was randomized to the CDS-E arm, their patients would also receive supplemental patient education, including information about the effectiveness and side effects of different pain medications, pain management strategies post-extraction, and pain expectations following an extraction. The patient education was either automatically printed when a patient checked in for a scheduled extraction or was printed by the dentist at the point of care. Further details about the trial are described elsewhere (17). The survey results presented here are an exploratory analysis in the context of this larger project.
Adult patients who had an index visit for which they were eligible for the trial, who had a phone number documented in the electronic health record, and who had not opted out of research were eligible to complete the survey. To balance responses by study group and provider type (i.e., dentist vs. oral surgeons), we applied a systematic sampling approach (every Nth patient per dentist) with a variable sampling ratio by dentist. The study statistician provided this sampling ratio based on prior extraction counts by dentist. Patients were randomly selected based on this sampling ratio, such that all patients were selected from dentists with a low volume of extractions, and a subset of patients were selected from dentists with a high volume of extractions. These weights were adjusted periodically during the study recruitment period to best reflect current extraction volumes.
The HealthPartners Institutional Review Board reviewed in advance, approved, and monitored the project. All methods were performed in accordance with local and federal regulations. Study participants provided verbal consent at the time of survey administration.
The HealthPartners Institute Center for Evaluation and Survey Research (CESR) conducted the survey from October 2020 through May 2021. Selected patients were called, consented, and administered the survey by phone. The initial call occurred 3 days post-extraction and additional follow-up calls continued until 6 days post-extraction visit. CESR staff documented survey outreach, recruitment, and survey responses in real time in REDCap (18).
The survey included questions about patient demographics, including gender, race, ethnicity, education, income, and opioid history. The survey also addressed post-extraction pain using a 10-point numerical rating scale (0 = “no pain at all,” 10 = “worst imaginable pain”) and asked patients what was the average pain they experienced in the first 3 days following their extraction. Shared decision-making was assessed using the 3-item collaboRATE scale, which asked patients to report their experience at the extraction encounter on a 5-point scale, with higher scores indicating more shared decision-making occurred (19). Finally, the survey included questions about pain management actions made by the patient, confidence in managing pain, patient reports of whether the provider talked with the patient about pain expectations following the extraction, and a general rating of the visit. The survey was designed to take 10 min to complete. Respondents were offered a $10 gift card as a thank you for completing the survey.
For the analysis of patient rating of pain and shared decision-making, general linear mixed models tested pre-specified contrasts in means (CDS vs. SP, CDS-E vs. SP) and report model-derived means and 95% confidence intervals. Each model included fixed effects for study arm, baseline prescribing strata (a four-category variable indicating the extent of opioid prescribing conducted by providers prior to the study intervention), extraction complexity, patient sex, and patient age and included a random provider intercept to acknowledge the cluster-randomized design. Mean pain ratings for those prescribed opioids and not prescribed opioids, stratified by complex extraction status, were tested with independent samples t-tests. Other survey items were summarized with frequencies, percentages, unadjusted means, and standard deviation. Analyses were conducted with SAS 9.4.
Contact was attempted with 981 patients eligible for this survey. A total of 16 patients had incorrect phone numbers, and 7 were found to be ineligible (language barrier, physical or mental inability to complete the survey). Among the 958 remaining, 495 were reached to complete the survey (52% response rate). An additional three patients did not complete key shared decision-making or pain items, resulting in a final analytic sample size of 492 completed surveys. Figure 1 shows the overall survey flow. Of those who completed the survey, 59% were female, 68% were White, and 32% had a college degree. Overall, 47% had taken opioids previously. Table 1 shows patient characteristics by study arm.
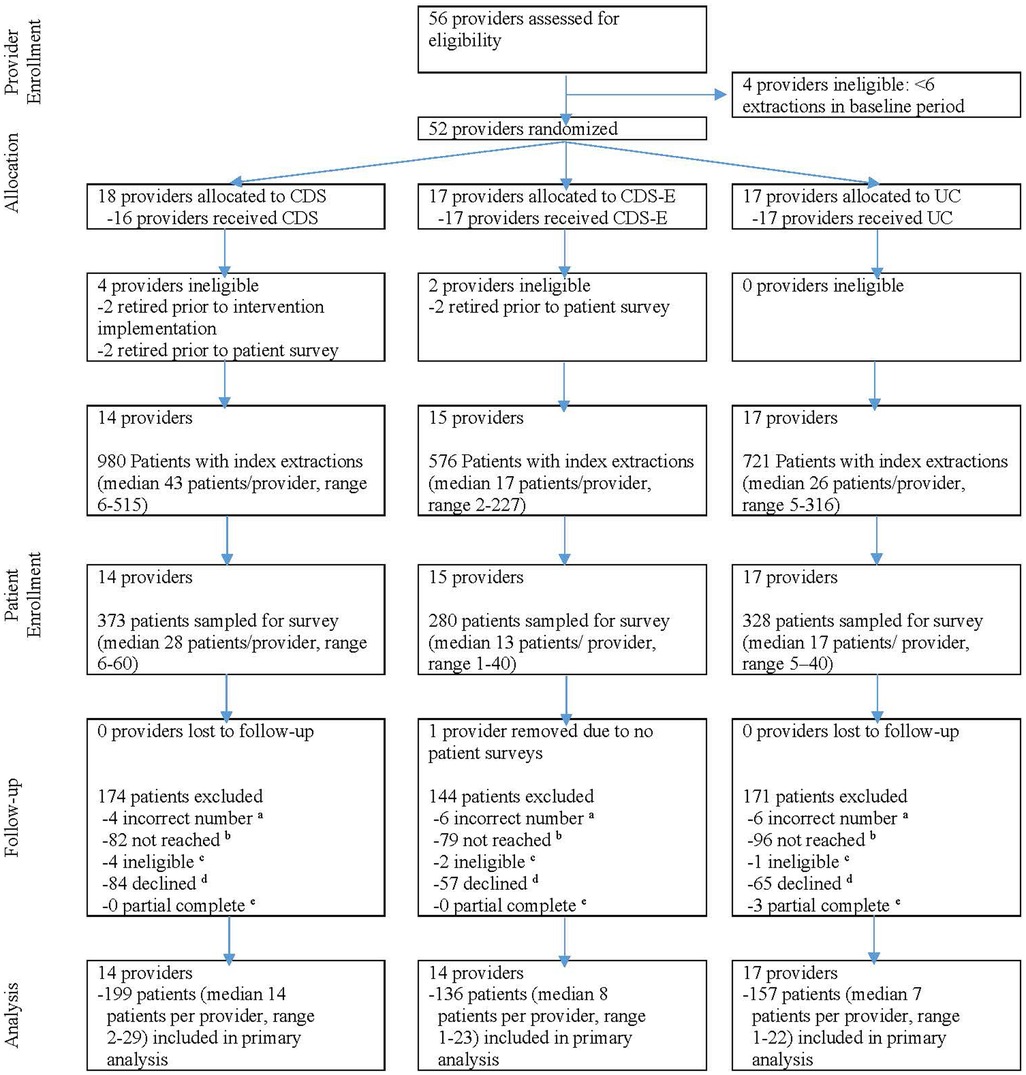
Figure 1 Patient survey CONSORT diagram. aIncorrect phone number (n = 16). bNot reached (n = 257) includes not reached during call window. cIneligible (n = 7) includes language barriers, physical/mental inability to take survey. dDeclined (n = 206) includes declined the survey after being reached. eDid not complete key shared decision-making and pain rating items (n = 3).
Pooling across all three study arms, the unadjusted mean pain rating (3.66, SD = 2.75) was low in the 3 days following the extraction (0 = no pain at all, 10 = worst imaginable pain). We found no statistically significant differences in patient responses across study arms for average pain in the 3 days following the extraction (p = 0.65, CDS vs. SP; p = 0.41, CDS-E vs. SP). Table 2 shows the model-derived estimates and mean differences by study arm. Among patients with a complex extraction (n = 151), mean pain ratings in the 3 days following the extraction were higher for patients prescribed opioids compared to those not prescribed opioids (mean = 5.1 (SD = 2.2, n = 41) vs. mean = 4.2 (SD = 2.9, n = 110), p = 0.05). Similarly, among patients with a simple extraction (n = 341), mean pain ratings in the 3 days following the extraction were higher for patients prescribed opioids compared to those not prescribed opioids (mean = 5.2 (SD = 1.8, n = 14) vs. mean = 3.2 (SD = 2.7, n = 327), p = 0.007).
Across all study arms the unadjusted mean shared decision-making score (3.29, SD = 0.80) indicated that respondents reported that a lot of effort was made by the dental care team to manage post-extraction pain (0 = no effort was made, 4 = every effort was made). We found no statistically significant differences in patient responses across study arms for average shared decision-making (p = 0.38, CDS vs. SP; p = 0.70, CDS-E vs. SP).
Respondents described their dental care team as taking actions to address their post-extraction pain. Many respondents (72%) rated their dental extraction visit as excellent. In total, 91% reported that their dental care team talked about pain expectations post-extraction; 92% reported that their dental care team discussed how to treat post-extraction pain; 74% reported feeling confident at the end of their extraction visit about their ability to manage their post-extraction pain. Respondents described taking a variety of self-care actions to manage their post-extraction pain (more than one activity could be selected): avoiding straw use (93%), avoiding vigorous rinsing (90%), avoiding solid foods (87%), applying cold (38%), and applying warm (15%). Table 3 shows the responses by study arm.
This study illuminates the patient experience of pain management following a tooth extraction. No notable differences were seen across study arms. This suggests that the clinical decision support had no added benefit in terms of reducing patient-reported pain or improving patient-reported shared decision-making. This may be in part because of the overall high ratings patients gave about their pain management experience, in that they thought their dental care team made a lot of effort to manage post-extraction, expressed confidence in their ability to manage their post-extraction pain, and were able to implement pain mitigation strategies to manage their post-extraction pain.
Across all arms, survey respondents reported relatively low pain in the 3 days following their extraction and high general rating of their visit. Consistent with other work (20), patients prescribed opioids reported higher pain than those who were not prescribed opioids regardless of whether they had a simple or complex extraction. This may suggest dentists are accurately targeting opioid prescriptions to patients who experience greater post-operative pain. High satisfaction with extraction-related care is also consistent with other studies (20, 21). Our results may suggest shared decision-making as a potential mechanism for both high satisfaction and low pain rating, in that survey respondents expressed that their dental care team communicated about post-extraction pain expectations and how to manage it. Adolescents described a similar experience in terms of pain and shared decision-making with their dentist following third molar extractions (22). Awareness about pain expectations and knowledge about strategies may have led survey respondents to express confidence in their ability to manage their post-extraction pain and to use self-care strategies to manage it.
Other research has shown that the modality of post-extraction pain management instructions (verbal vs. written vs. verbal plus written) leads to different pain experience following extractions, with higher reported pain in those with verbal instructions compared to those with written or with written plus verbal (23). Other research has shown higher opioid prescribing with less patient education or less Prescription Drug Monitoring Program use (24). While our results show no statistically significant differences in patient responses across study arms for average pain, this may be in part because standard practice at the participating healthcare organization includes providing written instructions and prompted access to the Prescription Drug Monitoring Program. The overall low pain scores may further support the value of written instructions for patients' post-extraction pain management.
This study has several limitations worth noting. First, survey administration took place after the emergence of COVID-19. The survey period was coincident with enhanced respiratory precautions for the care team and patients, and poor clinic access because of recent clinic closures associated with the pandemic. It is unclear how these issues impacted patient responses. The extraction volumes were lower, and the patient mix may have differed due to changes in care-seeking behaviors during the pandemic. However, the 3-arm study design mitigates this limitation in that it allows for meaningful comparisons that would not have been possible without a control. Second, shared decision-making measures are based on patient self-report, which can be subject to social desirability bias, particularly in interviewer-administered data collection. This mode was necessary because of the short window to capture extraction-related pain outcomes without contamination by other extraction sequalae that can cause pain (e.g., dry socket, infection). We minimized the potential for social desirability by ensuring confidentiality and independence from clinicians. Specifically, interviewers were trained to elicit positive and negative experiences, and standardized tools were used to measure shared decision-making. Third, this study was conducted in a large, multi-clinic, dental practice with an integrated electronic health and dental record system. As such, providers may have more access to patient health history, best practice alerts, and patient education materials than a typical private practice group. This may account partly for why our results show no statistically significant differences.
In summary, most respondents reported adequate post-extraction pain management. To achieve low pain, they implemented a variety of self-care activities to mitigate their pain. This may be attributed in part to the dental care team's effort to manage post-extraction pain. Overall, this work suggests that both dental care teams and patients are open to self-care approaches to post-extraction pain management. Future research will assess the effects of both interventions on opioid prescribing and non-opioid analgesic recommendations for post-extraction pain management.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Methodist Hospital IRB affiliated to HealthPartners Institute. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
SQM and DBR conceived of the study and obtained funding. All authors were involved in the protocol development. SMK and SEA conceptualized and implemented the sampling. SEA conducted the statistical analysis. JYZ conceptualized the survey and managed the staff involved with administering the survey. ART wrote the early drafts of the manuscript. All authors contributed to the article and approved the submitted version.
Research reported in this publication was supported by the National Institute of Dental & Craniofacial Research of the National Institutes of Health under Award Number U01DE027441. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
We would like to acknowledge the HealthPartners Institute Center for Evaluation and Survey Research staff involved with administering this survey and the patients who contributed to this work.
Unrelated to the present study, Gryczynski is an investigator on an NIH-funded study that has received free medication from Indivior and Alkermes, has received research funding from Indivior (paid to his institution and including project-related salary support), and is part of owner of COG Analytics. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Web-Based Injury Statistics Query and Reporting System [Internet]. Centers for Disease Control and Prevention (2020) [cited 30 May 2022].
2. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. Morb Mortal Wkly Rep. (2016) 64(50):1378–82. doi: 10.15585/mmwr.mm6450a3
3. Wilson N, Kariisa M, Seth P, Ht S, Davis NL. Drug and opioid-involved overdose deaths—United States, 2017–2018. MMWR Morb Mortal Wkly Rep. (2020) 69(11):290–7. doi: 10.15585/mmwr.mm6911a4 Epub 2020/03/20.32191688
4. Schieber LZ, Guy GP Jr, Seth P, Young R, Mattson CL, Mikosz CA, et al. Trends and patterns of geographic variation in opioid prescribing practices by state, United States, 2006–2017. JAMA Network Open. (2019) 2(3):e190665. doi: 10.1001/jamanetworkopen.2019.0665
5. Gupta N, Vujicic M, Blatz A. Opioid prescribing practices from 2010 through 2015 among dentists in the United States: What do claims data tell us? J Am Dent Assoc. (2018) 149(4):237–45.e6. doi: 10.1016/j.adaj.2018.01.005 Epub 2018/03/31.29599017
6. Steinmetz CN, Zheng C, Okunseri E, Szabo A, Okunseri C. Opioid analgesic prescribing practices of dental professionals in the United States. JDR Clin Trans Res. (2017) 2(3):241–8. doi: 10.1177/2380084417693826 Epub 2017/09/08.28879246
7. Association AD. Policy on opioid prescribing. Substance use disorder (opioid crisis). Chicago: American Dental Association (2018).
8. Association AD. Policy on the use of opioids in the treatment of dental pain. Substance use disorder (opioid crisis). Chicago: American Dental Association (2018).
9. Suda KJ, Zhou J, Rowan SA, McGregor JC, Perez RI, Evans CT, et al. Overprescribing of opioids to adults by dentists in the U.S., 2011–2015. Am J Prev Med. (2020) 58(4):473–86. doi: 10.1016/j.amepre.2019.11.006 Epub 2020/02/09.32033856
10. Chua KP, Brummett CM, Conti RM, Bohnert AS. Opioid prescribing to us children and young adults in 2019. Pediatrics. (2021) 148(3):e1360–8. doi: 10.1542/peds.2021-051539 Epub 2021/08/18.
11. Harbaugh CM, Nalliah RP, Hu HM, Englesbe MJ, Waljee JF, Brummett CM. Persistent opioid use after wisdom tooth extraction. Jama. (2018) 320(5):504–6. doi: 10.1001/jama.2018.9023
12. Schroeder AR, Dehghan M, Newman TB, Bentley JP, Park KT. Association of opioid prescriptions from dental clinicians for us adolescents and young adults with subsequent opioid use and abuse. JAMA Intern Med. (2019) 179(2):145–52. doi: 10.1001/jamainternmed.2018.5419
13. Robertson J, Walkom E, Pearson SA, Hains I, Williamsone M, Newby D. The impact of pharmacy computerised clinical decision support on prescribing, clinical and patient outcomes: a systematic review of the literature. Int J Pharm Pract. (2010) 18(2):69–87. Epub 2010/05/06. doi: 10.1211/ijpp.18.02.0002
14. Holstiege J, Mathes T, Pieper D. Effects of computer-aided clinical decision support systems in improving antibiotic prescribing by primary care providers: a systematic review. J Am Med Inform Assoc. (2015) 22(1):236–42. doi: 10.1136/amiajnl-2014-002886 Epub 2014/08/16.25125688
15. Hemens BJ, Holbrook A, Tonkin M, Mackay JA, Weise-Kelly L, Navarro T, et al. Computerized clinical decision support systems for drug prescribing and management: a decision-maker-researcher partnership systematic review. Implement Sci. (2011) 6(1):89. doi: 10.1186/1748-5908-6-89
16. Pearson S-A, Moxey A, Robertson J, Hains I, Williamson M, Reeve J, et al. Do computerised clinical decision support systems for prescribing change practice? A systematic review of the literature (1990–2007). BMC Health Serv Res. (2009) 9(1):154. doi: 10.1186/1472-6963-9-154
17. Rindal DB, Asche SE, Gryczynski J, Kane SM, Truitt AR, Shea TL, et al. De-Implementing opioid use and implementing optimal pain management following dental extractions (Diode): protocol for a cluster randomized trial. JMIR Res Protoc. (2021) 10(4):e24342. doi: 10.2196/24342 Epub 2021/04/13.33843594
18. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The redcap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
19. Barr PJ, Thompson R, Walsh T, Grande SW, Ozanne EM, Elwyn G. The psychometric properties of collaborate: a fast and frugal patient-reported measure of the shared decision-making process. J Med Internet Res. (2014) 16(1):e2. doi: 10.2196/jmir.3085 Epub 2014/01/07.24389354
20. Nalliah RP, Sloss KR, Kenney BC, Bettag SK, Thomas S, Dubois K, et al. Association of opioid use with pain and satisfaction after dental extraction. JAMA Network Open. (2020) 3(3):e200901. doi: 10.1001/jamanetworkopen.2020.0901
21. Al-Khateeb TH, Alnahar A. Pain experience after simple tooth extraction. J Oral Maxillofac Surg. (2008) 66(5):911–7. doi: 10.1016/j.joms.2007.12.008 Epub 2008/04/22.18423280
22. Mitchell SG, Truitt AR, Davin LM, Rindal DB. Pain management after third molar extractions in adolescents: a qualitative study. BMC Pediatr. (2022) 22(1):184. doi: 10.1186/s12887-022-03261-x
23. Gheisari R, Resalati F, Mahmoudi S, Golkari A, Mosaddad SA. Do different modes of delivering postoperative instructions to patients help reduce the side effects of tooth extraction? A randomized clinical trial. J Oral Maxillofac Surg. (2018) 76(8):1652.e1–.e7. doi: 10.1016/j.joms.2018.04.019 Epub 2018/05/15.29758175
24. McCauley JL, Leite RS, Gordan VV, Fillingim RB, Gilbert GH, Meyerowitz C, et al. Opioid prescribing and risk mitigation implementation in the management of acute pain: results from the national dental practice-based research network. J Am Dent Assoc. (2018) 149(5):353–62. doi: 10.1016/j.adaj.2017.11.031 Epub 2018/03/20.29550022
Keywords: tooth extraction, analgesics, pain management (MeSH), dentistry (MeSH), shared decision-making
Citation: Truitt AR, Asche SE, Ziegenfuss JY, Mitchell SG, Gryczynski J, Kane SM, Worley Donald C. and Rindal D.B (2022) Patient experience of post-extraction pain management. Front. Dent. Med 3: 1003041. doi: 10.3389/fdmed.2022.1003041
Received: 25 July 2022; Accepted: 29 September 2022;
Published: 17 October 2022.
Edited by:
Man-Kyo Chung, University of Maryland, United StatesReviewed by:
Douglas Oyler, University of Kentucky, United States© 2022 Truitt, Asche, Ziegenfuss, Mitchell, Gryczynski, Kane, Worley and Rindal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: D. Brad Rindal, RG9uYWxkLkIuUmluZGFsQEhlYWx0aFBhcnRuZXJzLmNvbQ==
Specialty Section: This article was submitted to Systems Integration, a section of the journal Frontiers in Dental Medicine
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.