- Department of Medical, Oral and Biotechnological Sciences, University G. D'Annunzio, Chieti, Italy
Background: The ponticulus posticus (PP) is an important anomaly of the atlas (C1 vertebra) with a complete or partial bone bridge that transforms the groove of the vertebral artery (VA) into a canal (arcuate foramen). The aim was to retrospectively determine prevalence of PP evaluating morphological features and the possible association with other dentoskeletal anomalies in the midface and neck area such as maxillary canine impaction (MCI), atlas posterior arch deficiency (APAD), and sella turcica bridging (SB).
Methods: This study was conducted in the Department of Medical, Oral and Biotechnological Sciences of the University “G. D'Annunzio” in Chieti. The detection of PP was performed on 500 patients with cone beam CT (CBCT) images (6 to 87 years).
Results: Analysis revealed the presence of uni- and bi-lateral PP in 110 patients (22%): 24 (4.8%) patients with bilateral complete PP, 12 (2.4%) patients with complete PP on the left, 6 (1.2%) patients with complete PP on the right, 8 (1.6%) patients with complete PP on the right and partial PP on the left, 6 (1.2%) patients with complete PP on the left and partial PP on the right, 26 (5.2%) patients with partial bilateral PP, 18 (3.6%) patients with partial left PP, and 10 (2%) patients with partial PP on the right. The Chi-squared statistic confirmed that there are significant associations between MCI and PP (p = 0.020) and between SB and MCI (p <0.00001). No correlation between chronological age and presence of the PP (p = 0.982), between chronological age and morphotypes of the PP (p = 0.779), between APAD and the PP (p = 0.0757), between SB and the PP (p = 0.111), and between APAD and MCI (p = 0.222) were found.
Conclusion: This observational study showed how bilateral partial variant and bilateral complete variant are the most represented morphotypes in all the age groups. The prevalence of MCI is positively associated with PP and with SB.
Introduction
This study aims to improve knowledge regarding age-related prevalence and morphological features of the ponticulus posticus (PP).
The PP is an atlas (C1 vertebra) anatomical variant. It consists of a complete or partial bone bridge in the sulcus located on the first cervical vertebra posterior arch (1).
This sulcus sustains the vertebral artery and suboccipital nerve. In addition to the “PP,” there are many other terms in the literature describing this anomaly: arcuate foramen, atlas bridging, canalis arteriae vertebralis, foramen retroarticular, foramen sagittal, pons ponticus, posterior atlantoid foramen, posterior ponticulus, retroarticular ring (2).
There are different schools of thought regarding the origin of the PP: according to some authors, it is a congenital feature (3); others suggest that it may have a genetic trait (4); however, others assumed that it could be the result of ossification due to aging (5) or a result of external mechanical factors (6) [e.g., carrying heavy objects on the head could play a role in its development (7)]. It has also been suggested that bone arch finally may develop to protect vertebral artery passage during head and neck movements (8).
It should be noted that presence of the PP is considered average in quadrupeds, probably because it aims to provide a further atlas lateral extension for posterior atlanto-occipital membrane attachment. Since in mammals, the head is supported by neck muscles and ligaments and by this membrane. Likely, the adoption of the upright posture in man, transferring vertical head load on the upper articular atlas process led to the progressive disappearance of the PP (9).
There are also conflicting opinions in literature regarding the association between chronological age and presence of the PP. Some authors suggested that this anomaly outcome of senile ossification and, therefore, has a predilection for older subjects (10). It is also possible that over time, progressive mineralisation of the PP occurs. However, other studies have found no statistically significant association between chronological age and presence of the PP (8, 11, 12).
The PP can be radiographically diagnosed by lateral cephalography (6, 13) and CT (7, 14, 15); cone beam CT (CBCT) has recently been used in several studies (11, 16, 17). CBCT allows a shorter scan time and the radiation dose is up to 10 times lower than that of CT scans and costs are significantly reduced (18).
Cone beam CT is considered the gold standard in the radiodiagnosis of the PP; it is possible to carry out correct characterization and classification of the PP, thanks to three-dimensional technology. Bidimensional diagnostic methods do not allow the precise evaluation of morphological characteristics and anomaly symmetry of the PP: this is considered a limitation shared by all the previous radiographic studies performed with lateral cephalography (19). Patients who come to the Orthodontics and Orofacial Pain Department for temporomandibular disorders (TMD) undergo a radiological examination, which consists of a CBCT to plan orthodontic treatment. With the low-dose protocol CBCT, radiation is significantly lower than with the helical CT with higher spatial resolution. A combination of volumetric reconstruction and multiplanar views can provide useful information in orthodontics about skeletal tissue, dentition, and airway status (relevant for sleep apnoea cases). CBCT allows to obtain a complete diagnosis for the patient's general health, instead of a diagnosis limited to the orthodontic field (12).
Identification of the PP is important in orthodontics because this anomaly is implicated in the development of otherwise unexplainable neck pain and headaches, visual disturbances, problems with speech and swallowing, vertigo, and vascular problems (20) (Figure 1).
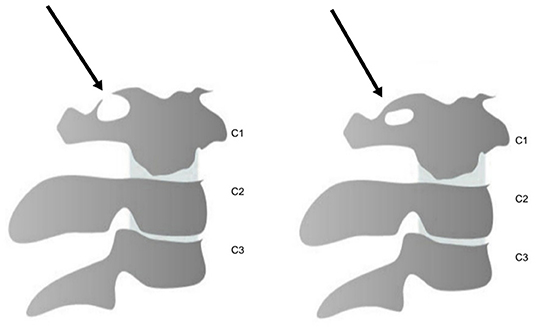
Figure 1. Schematic representation of the partial ponticulus posticus (PP) (left) and the complete PP (right). The image is taken from “G. D'Annunzio” University archives.
It is important to consider that an excessive bone protrusion caused by vertebral artery deep impression should not be confused as the PP. Instead, this refers to a deep sulcus and can often erroneously lead to partial diagnosis of the PP (11).
The PP can be classified as bilateral or unilateral, thus obtaining all the possible variants and being defined as partial and complete.
The PP is generally considered a simple anatomical variant. The clinical significance of this anomaly is still controversial today, as several studies have found a possible association with symptomatologic conditions, although some patients presenting the PP are asymptomatic.
Various authors interpret the etiology of symptoms differently: some believe that the painful symptoms are due to suboccipital nerve compression; others claim that pain is caused by sympathetic periarterial plexus irritation and others suggest that it may instead be related to a vertebral artery direct compression (21).
Compression of nervous and vascular structures passing through this hole (the vertebral artery, sympathetic periarterial plexus, and suboccipital nerve) may involve a combination of symptoms such as headache, neurosensory hearing loss, neck pain, dizziness, vertebrobasilar insufficiency, Barré–Liéou syndrome, shoulder pain, and, in some cases, also postural muscle tone loss and loss of consciousness.
In literature, some recent studies on the PP have evaluated the correlation of craniofacial skeletal anomalies with dental developmental anomalies due to the common embryological origin of the teeth and craniofacial bones, neck, and shoulder. The development of these structures is influenced by neural crest cells (NCCs) (22). So, the various anomalies of this area could be related to each other. The effect of NCCs and homebox and hox genes contributing to the formation of many parts of the cervicovertebral area (including atlas) and the midface (including teeth and sella turcica) seems to explain the relationship between dental and skeletal anomalies following a genetic mutation (23). CBCT allows diagnosing other craniofacial anomalies: maxillary canine impaction (MCI), atlas posterior arch deficiency (APAD), and sella turcica bridging (SB).
After third molars, permanent canines are the most commonly impacted teeth, with an incidence of 0.92 to 3.58% in the general population (24). The incidence of canine inclusion in the maxilla is more than twice that of the mandibular canine inclusion due to genetic factors (25).
Atlas posterior arch deficiency is a rare anomaly of the posterior arch of the atlas. Sella turcica bridge (SB) is a rare phenomenon of ossification of the interclinoid ligament (ICL) between the anterior clinoid process and the posterior clinoid process (26).
Association between dentoskeletal variations has been previously reported in literature, but some results are partially contradictory particularly for APAD (27). The aims of this cross-sectional study were to improve knowledge regarding PP's age-related prevalence and morphological features and verify a correlation between dentoskeletal anomalies in subjects with the PP; the novel aspect of this study is that CBCT conducted the radiographic diagnosis. The first null hypothesis is no association between chronological age and presence of the PP and between chronological age and morphotypes of the PP.
The second null hypothesis is no association between the PP and dentoskeletal variations (MCI, SB, and APAD). The third null hypothesis is no association between the occurrences of dentoskeletal variations (MCI, SB, and APAD).
Materials and Methods
This cross-sectional study used patients with CBCT images obtained from the archives of the Department of Medical, Oral and Biotechnological Sciences of the University “G. D'Annunzio” in Chieti.
Ethical approval (number 23) was obtained from the Independent Ethics Committee of hospital of Chieti. This study protocol was drawn in accordance with the European Union Good Practice Rules and in line with the Helsinki Declaration. Written informed consent was obtained from patients for publication of this report and any accompanying images. The sample included 500 Italian patients (age range: 6–87 years; average age: 27.08 ± 15.12 years) who presented for orthodontic diagnosis and treatment planning (28). This cohort was composed of 202 males (40.4%) and 298 (59.6%) females. Age of the male patients ranged from 6 to 86 years (average age: 23.8 ± 13.3 years), while female patients were aged between 7 and 87 years (average age: 29.3 ±15.9 years).
To eliminate any evaluation error, each CBCT image was separately analyzed and subsequently compared by the authors, detecting in most cases a correspondence between the two control lines. In case of disagreement on presence of the PP, a third observer was consulted. Only images in which all the observers agreed on presence or absence of the PP in any form (complete or partial) were included in prevalence calculation.
To minimize the risk of inaccurate measurements due to fatigue, no more than 50 radiographs were evaluated at a time.
The inclusion criteria were patients aged 6 years or older without any congenital craniofacial region syndromic pathologies and a history of trauma or surgery in the craniofacial and cervical areas. The inclusion criteria were patients aged 14 years or older, since the eruption of the canine usually finishes at 12–13 years of age (all the teeth have usually completely erupted by this time, except the third molar) for the evaluation of the association between MCI and the PP, MCI and SB, MCI and APAD, and SB and APAD (29).
Exclusion Criteria
• Insufficient image quality (e.g., because of patient movement)
• Region of interest cut
• Congenital lip and palate anomalies or other craniofacial region syndromic pathologies
• History of trauma or surgery in the cervical spine
• Non-Italian nationality.
Cone beam CT images were obtained by using Pax-Zenith 3D CBCT (Vatech Corporation Ltd., Hwaseong, Korea) with a low-dose acquisition protocol based on the following parameters:
• Field-of-view (FOV) 240 ×190
• Normal resolution quality
• 80 kVp
• 5 mA
• Acquisition time of 15 s.
Patients were positioned at a Frankfurt plane parallel to the floor with the head contained in the portal of the X-ray detector system. A 360° rotation was performed around the head of the patient with a scan time of 15–20 s. Subsequently, the patient left the examination room and the raw data were loaded and reprocessed in multiplanar and three-dimensional images using the Dolphin imaging software.
General prevalence and distribution of the PP were measured considering the different morphotypes compared to the age of the patients.
Patients were divided into three groups to simplify analysis of the obtained results:
• From 6 to 33 years
• From 34 to 60 years
• From 61 to 87 years.
All the data were recorded using the Microsoft Excel version 16.0 for Windows 10.
The PP was classified by authors in all its forms: absent (A), bilateral complete (C), complete left (CL), complete right (CR), complete right and partial left (CRPL), complete left and partial right (CLPR), bilateral partial (P), partial left (PL), and partial right (PR).
Complete PP was defined as a clearly visible bone bridge circumferentially extending from the upper articular process to the posterior arch of the atlas.
Partial PP was defined as a bone spike above the vertebral artery sulcus extending from the upper articular process or from the posterior arch of the atlas. Bone bridges with central discontinuity or discontinuity near their origin have been included in this category (examples of partial PP). However, very accentuated bone angles due to a high depth of vertebral artery sulcus have been discarded and not included in the various forms of PP.
Cone beam CT allows diagnosing other dentoskeletal anomalies such as MCI, APAD, and SB.
Maxillary canine impaction was sought in patients aged 14 years or older and never treated orthodontically before the CBCT images were taken; for this reason, the subsample includes only 256 patients. The diagnosis of MCI was performed on CBCT and confirmed by medical records without distinguishing between unilateral or bilateral impaction of the maxillary canine.
Atlas posterior arch deficiency was diagnosed measuring the sagittal length of the posterior arch of the atlas to define its level of formation: fully formed or deficient (30). SB was diagnosed by measuring the length (from the tip of the dorsum sella to the tuberculum sella) and the diameter (longest distance between the tuberculum and the farthest point on the inner wall of sella). The severity of calcification was classified by using the standardized scoring scale developed by Leonardi:
- No bony bridge: The length of sella turcica was less or equal to three-quarter diameter (type I)
- Partial bony bridge partial calcification: The length of sella turcica was < three-quarter diameter (type II)
- Complete bony bridge: The image showed the diaphragm sella or contact between the tuberculum and dorsum (type III) (31).
Statistical Analysis
All the CBCT images were randomly selected and analyzed to evaluate the reliability of this study. Radiological diagnosis of the PP, MCI, type II SB, type III SB, and APAD was performed on CBCT images.
Data were subjected to statistical analysis using the IBM SPSS 17 software (IBM Corporation, New York, USA) and the Stata 9.0 software (StataCorp LP, College Station, Texas, USA). The chi-squared test was used to analyze the differences between data collected. The level of significance was set at p <0.05 with a 95% CI.
Results
Analysis of 500 CBCT images revealed presence of the PP (uni- or bi-lateral) in 110 patients (22%).
Of these 110 patients:
• 24 patients (4.8%) showed bilateral complete PP
• 12 patients (2.4%) showed complete PP on the left
• 6 patients (1.2%) showed complete PP on the right
• 8 patients (1.6%) showed complete PP on the right and partial on the left
• 6 patients (1.2%) showed complete PP on the left and partial on the right
• 26 patients (5.2%) showed partial bilateral PP
• 18 patients (3.6%) showed partial left PP
• 10 patients (2%) showed partial right PP.
The most represented morphotype of the PP was the bilateral partial form followed by bilateral complete form.
The average age of all the patients recruited in this study was 27.08 years (SD: 15.124 years); among these patients could be classified as:
• Patients with the PP: Average age of 27.2 years (SD: 14.2 years)
• Patients without the PP: Average age of 27.04 years (SD: 15.39 years).
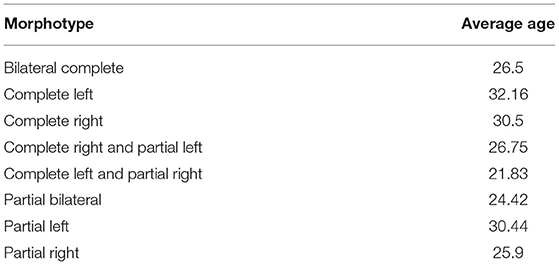
Average ages of the patients are shown in Table 1 and are distributed in various morphotypes of the PP. It was observed that the highest average age refers to the “CL” variant, while the lowest average age refers to the “CLPR” variant.
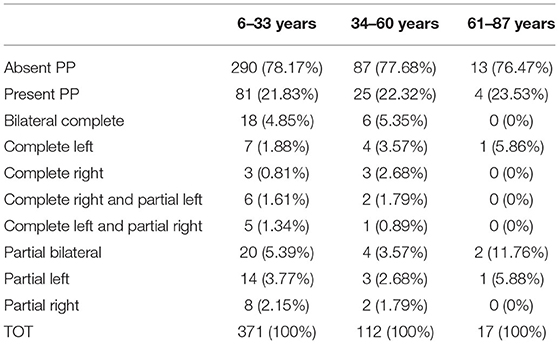
The percentage of patients with PP was estimated in each age group:
• between 6 and 33 years: 21,80% of 371 total patients (81 patients with PP, 290 without PP)
• between 34 and 60 years: 22,30% of 112 total patients (25 patients with PP, 87 without PP)
• between 61 and 87 years: 23,50% of 17 total patients (4 patients with PP, 13 without PP).
The P-value for the comparison of PP prevalences among the age groups was not statistically significant (P = 0.982)
By evaluating the most frequent morphotypes in various age classes, it can be seen that the complete and partial bilateral variants (22 and 25%, respectively) are more represented in the first age bracket (6–33 years).
Subsequently, there is a slight increase in all the complete forms in the second age bracket (34–60 years), primarily bilateral complete form (22 vs. 24%) with a concomitant reduction of partial forms, especially of the bilateral partial (25 vs. 16%); this could be due to complete ossification of adult patients with the PP, transforming partial form to complete bilateral form. The percentages remain almost unchanged in mixed forms (CRPL and CLPR).
Finally, the percentages were completely reversed in the last age group (61–87 years); the bilateral partial form includes half of cases while partial and complete left form represent the other half of patients. This is related to the small number of analyzed patients: 17 total patients and 4 patients with PP.
Table 2 shows the percentages of various morphotypes in different age groups; the chi-squared test showed that the association between chronological age and morphotypes of the PP is not statistically significant (p = 0.779).
Radiological diagnosis of MCI, SB, and APAD was also performed on all the 500 CBCT images.
The percentage, the prevalence, and the chi-squared test of patients with MCI, APAD, and SB were estimated in each case group (with the PP) and control group (without the PP).
Maxillary canine impaction was found in 14 of 256 total patients aged 14 years or older (5.4%) and in 6 of 49 patients with the PP, so the prevalence of MCI in patients with the PP is 12.2%; moreover, the prevalence of MCI in patients without PP is 3.8%.
The chi-squared test showed that MCI is more frequent in the PP group than in the control group (without the PP). There was a significant association of MCI with the PP (p = 0.020).
Atlas posterior arch deficiency was found in 11 of 500 total patients (2.2%) and 2 patients of 110 patients with the PP, so the prevalence of APAD with the PP is 1.8% and the prevalence of APAD in patients without the PP is 2.3%. The chi-squared test showed that the correlation of APAD with the PP is not significant (p = 0.757).
Type II SB (partial form) was found in 17 of 500 total patients (3.4%) and 6 of 110 patients with the PP, so the prevalence of type II SB with the PP is 5.4% and the prevalence of type II SB without the PP is 2.8%.
Type III SB (complete form) was found in 2 of 500 total patients (0.4%) and 9 of 110 patients with the PP, so the prevalence of type III SB with the PP is 0.9% and the prevalence of type III SB without the PP is 0.2%.
The chi-squared test was estimated for both the types of SB (II and III). The chi-squared statistic showed that the correlation between types II SB and type III SB with the PP is insignificant (p = 0.111).
The associations between dentoskeletal variations (MCI-APAD, MCI-SB, and SB-APAD) were sought inside the subsample of 256 patients aged 14 years or older. The APAD was found in 6 patients (2.34%) and SB was found in 15 patients (5.85%).
Atlas posterior arch deficiency was found in 1 patient with MCI (7.14%); SB was found in 5 patients with MCI (35.71%). No patients with SB and APAD were found in the subsample. The chi-squared test showed that the association of MCI with APAD is insignificant (p = 0.222), but the association of MCI with SB is significant (p <0.00001).
Discussion
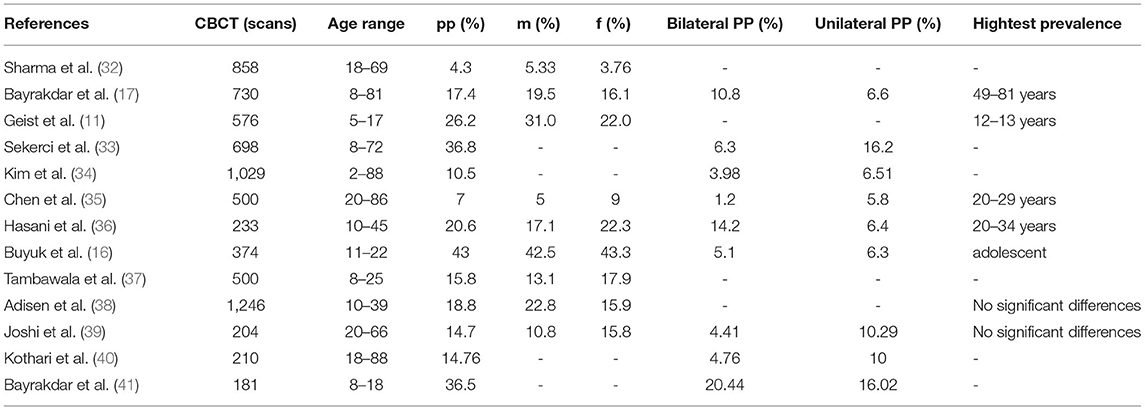
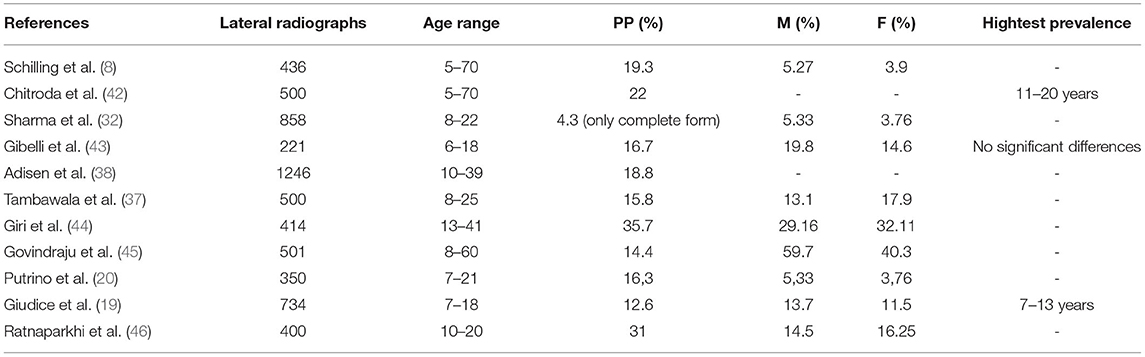
This study evaluated the prevalence of the PP across the general population and examined the association between MCI, APAD, SB, and the PP and between dentoskeletal variations (MCI-APAD, MCI-SB, and SB-APAD). This study also examined the prevalence of MCI, APAD, and SB in patients without the PP. The subjects of this study were patients of Italian nationality (Caucasian race). No formula and parameters were used for sample size estimation. This study showed that the PP has a prevalence of 22% across the general population. This result agrees the previous studies performed on CBCT images as reported in Table 3; only in four studies, authors found a prevalence of the PP higher than our result (11, 16, 17, 33). The result of this study is slightly higher than Elliot and Tanweer revision (performed on cadavers, by lateral radiographs and CT; 2014) in which the reported percentage was 17%. In general, this result is slightly higher than previous studies performed on lateral radiographs as reported in Table 4.
The average age corresponds to 25.87 years in patients with a partial bony bridge and 27.55 years in cases with complete formation of the bony ring. The most represented morphotypes are the bilateral partial form (5.2%) followed by the bilateral complete variant (4.8%) according to the literature (19).
The following study recruited a higher rate of young patients than older patients, because the CBCTs evaluated were performed for orthodontic problems, which are more common in younger patients. The sample size of the age group 61–87 years (17 total patients) is smaller than the sample size of the other age groups due to the low request for orthodontic treatment.
The limitations of this study include the age distribution of the sample, which was not homogeneous.
According to Putrino et al., there is a positive relationship between dental agenesis and the PP. Orthodontists can play a key role in diagnosing the PP. If orthodontists identify the PP during the radiologic examination, it must be documented in medical records of the symptomatic patients and it is necessary to investigate further with specific examinations (20).
The prevalence of the PP is influenced by the quality and resolution of the radiographic image as a diagnostic tool, thus confirming CBCT as the gold standard tool for the diagnosis of the PP compared to plain radiograph (7).
Studies effectuated on CBCT and lateral radiographs obtained different percentages as reported in Tables 3, 4.
The correlation of the PP with the gender of the patients because of the different percentages obtained in the literature can be excluded.
The different percentages are very variable in these studies, because the analyzed range differed according to the age and gender percentages of the patients.
The obtained results confirmed that progressive ossification of the PP with increasing age is the cause of bilateral complete variant increase with the concomitant bilateral partial reduction.
It is incorrect to interpret the results indicating that the percentage of the patients with the PP was slightly higher in the older age, since the p-value for this comparison is not significant. Actually, the age groups were not different (the p-value was not significant).
Maxillary canine impaction and SB were significantly increased in patients with the PP vs. those in the control group (without the PP). The prevalence of MCI with the PP (12.2%) is higher than the prevalence of MCI without the PP (3.8%). The chi-squared statistic confirmed that there is a significant association of MCI and the PP (p > 0.05). In literature, studies sought patients with MCI results have indicated an increased frequency of the PP (26, 47).
The prevalence of type II SB with the PP (5.4%) is higher than the prevalence of type II SB without PP (2.8%). Similarly, the percentage and the prevalence of type III SB in patients with the PP (0.9%) is slightly higher than the control group (0.2%). Type III SB (complete form) was found in only two patients agreeing that it is a rare condition. For this reason, the chi-squared test was estimated for both the types of SB (II and III) due to the irrelevant number of patients with type III SB. The chi-squared statistic confirmed that there is no statistically significant association between the PP and types II and III SB (p > 0.05) as confirmed in literature (23, 47).
The prevalence of APAD with the PP (1.8%) is slightly inferior to the prevalence of APAD without the PP (2.3%), and the chi-squared statistic confirmed that there is no statistically significant association (p > 0.05) between APAD and PP. In literature, no other studies have sought to determine the presence of APAD in patients with the PP.
The prevalence of APAD with MCI (7.14%) is inferior than the prevalence of SB with MCI (35.71%). No patients with SB and APAD were found in the subsample. No other studies have sought to determine the presence of APAD in patients with SB. The chi-squared test showed that the association of APAD with MCI is not significant (p = 0.222), but the association of MCI with SB is significant (p <0.00001). In literature, are conflicting opinions concerning the association between APAD and MCI and between SB and MCI. Some authors found significant associations between SB and MCI [30, 33.]. A significant association between APAD and MCI was found by Pasini et al. (30). This study result agrees with the study of Ghadimi et al. (26) where the association between APAD and MCI was not significant.
Conclusion
The first null hypothesis was not rejected because there is no association between chronological age and presence of the PP and between chronological age and morphotypes of the PP.
The second null hypothesis of the study was partially rejected because the presence of MCI is positively associated with the PP, but the presences of APAD and types II and III SB are not associated with the PP. The third null hypothesis was partially rejected because only the presence of SB is positively associated with MCI, but the presence of APAD is not associated with the MCI.
Dentists can consider maxillary canine impaction for a precocious diagnosis of the PP, since it is visible in radiographic images. It is also important that the dentists detect these anomalies in asymptomatic patients, reporting them in the medical record, as they may be related to some medically relevant symptoms.
There may be other dentoskeletal anomalies that deserve further studies.
Although limited by the small sample size of the last age group, this observational study showed that partial bilateral variant and complete bilateral variant subsequently are the most represented morphotypes in all the age groups.
Moreover, this study shows that partial variants decrease with a concomitant complete variant increase with rising registry age. Our future goal will be to understand whether a certain variant of the PP could be closely related to a specific symptomatic picture or to the complete absence of symptoms in order to set up therapy and treat each individual patient.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by ethics approval (number 23) was obtained by the Hospital's Independent Ethics Committee of Chieti. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
FF and MM documented the cases. GP and MM conducted a review of literature and drafted the manuscript. FR and MM analyzed the data. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Simsek S, Yigitkanli K, Comert A, Acar HI, Seckin H, Er U, et al. Posterior osseous bridging of C1. J Clin Neurosci. (2008) 15:686–8. doi: 10.1016/j.jocn.2007.06.004
2. Tassoker M, Kok H, Ozcan S. Investigation of the relationship between “Sella Turcica Bridge” and “Ponticulus Posticus”: a lateral cephalometric study. Int J Morphol. (2017) 35:337–44. doi: 10.4067/S0717-95022017000100053
3. Allen W. The varieties of the atlas in the human subject, and the homologies of its transverse processes. J Anat Physiol. (1879) 14:18–27.
4. Selby S, Garn SM, Kanareff V. The incidence and familial nature of a bony bridge on the first cervical vertebra. Am J Phys Anthropol. (1955) 13:129–14. doi: 10.1002/ajpa.1330130110
5. White AA, Panjabi MM. Clinical Biomechanics of the Spine. Philadelphia, PA: Lippincott Williams & Wilkins (1978).
6. Taitz C, Nathan H. Some observations on the posterior and lateral bridge of the atlas. Acta Anat (Basel). (1986) 127:212–7. doi: 10.1159/000146284
7. Cho YJ. Radiological analysis of ponticulus posticus in Koreans. Yonsei Med J. (2009) 50:45–9. doi: 10.3349/ymj.2009.50.1.45
8. Schilling J, Schilling A, Galdames IS. Ponticulus posticus on the posterior arch of atlas, prevalence analysis in asymptomatic patients. Int J Morphol. (2010) 28:317–22. doi: 10.4067/S0717-95022010000100046
9. Lambarty BGH, Zivanovic S. The retroarticular vertebral artery ring of the atlas and its significance. Acta Anat. (1973) 85:113–22. doi: 10.1159/000143987
10. Paraskevas G, Papaziogas B, Tsonidis C, Kapetanos G. Gross morphology of the bridges over the vertebral artery groove on the atlas. Surg Radiol Anat. (2005) 27:129–36. doi: 10.1007/s00276-004-0300-9
11. Geist JR, Geist SM, Lin LM A. cone beam CT investigation of ponticulus posticus and lateralis in children and adolescents. Dentomaxillofac Radiol. (2014) 43:2013045. doi: 10.1259/dmfr.20130451
12. Feragalli B, Rampado O, Abate C, Macrì M, Festa F, Stromei F, et al. Cone beam computed tomography for dental and maxillofacial imaging: technique improvement and low-dose protocols. Radiol Med. (2017) 122:581–8. doi: 10.1007/s11547-017-0758-2
13. Young JP, Young PH, Ackermann MJ, Anderson PA, Riew KD. The ponticulus posticus: implications for screw insertion into the first cervical lateral mass. J Bone Joint Surg Am. (2005) 87:2495–8. doi: 10.2106/00004623-200511000-00017
14. Kim KH, Park KW, Manh TH, Yeom JS, Chang BS, Lee CK. Prevalence and morphologic features of ponticulus posticus in Koreans: analysis of 312 radiographs and 225 three-dimensional CT scans. Asian Spine J. (2007) 1:27–31. doi: 10.4184/asj.2007.1.1.27
15. Hong JT, Lee SW, Son BC. Analysis of anatomical variations of bone and vascular structures around the posterior atlantal arch using three-dimensional computed tomography angiographyet. J Neurosurg Spine. (2008) 8:230–6. doi: 10.3171/SPI/2008/8/3/230
16. Buyuk SK, Sekerci AE, Benkli YA, Ekizer A. A survey of ponticulus posticus: radiological analysis of atlas in an orthodontic population based on cone-beam computed tomography. Niger J Clin Pract. (2017) 20:106–10. doi: 10.4103/1119-3077.178916
17. Bayrakdar IS, Miloglu O, Altun O, Gumussoy I, Durna D, Yilmaz AB. Cone beam computed tomography imaging of ponticulus posticus: prevalence, characteristics, and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. (2014) 118:e210–9. doi: 10.1016/j.oooo.2014.09.014
18. Cohnen M, Kemper J, Mobes O, Pawelzik J, Modder U. Radiation dose in dental radiology. Eur Radiol. (2002) 12:634–7. doi: 10.1007/s003300100928
19. Giudice AL, Caccianiga G, Crimi S, Cavallini C, Leonardi R. Frequency and type of ponticulus posticus in a longitudinal sample of non-orthodontically treated patients: Relationship with gender, age, skeletal maturity, and skeletal malocclusion. Oral Surg Oral Med Oral Pathol Oral Radiol. (2018) 126:291–7. doi: 10.1016/j.oooo.2018.05.001
20. Putrino A, Leonardi RM, Barbato E, Galluccio G. The association between ponticulus posticus and dental agenesis: a retrospective study. Open Dent J. (2018) 12:510. doi: 10.2174/1874210601812010510
21. Sabir H, Kumbhare S, Rout P. Evaluation of ponticulus posticus on digital lateral cephalograms and cone beam computed tomography in patients with migraine and healthy individuals: a comparative study. Oral Surg Oral Med Oral Pathol Oral Radiol. (2014) 118:348–54. doi: 10.1016/j.oooo.2014.04.016
22. Matsuoka T, Ahlberg PE, Kessaris N, Iannarelli P, Dennehy U, Richardson WD, et al. Neural crest origins of the neck and shoulder. Nature. (2005) 436:347–55. doi: 10.1038/nature03837
23. Leonardi R, Barbato E, Vichi M, Caltabiano M. Skeletal anomalies and normal variants in patients with palatally displaced canines. Angle Orthod. (2009) 79:727–32. doi: 10.2319/082408-448.1
24. Al-Zoubi H, Alharbi AA, Ferguson DJ, Zafar MS. Frequency of impacted teeth and categorization of impacted canines: a retrospective radiographic study using orthopantomograms. Eur J Dent. (2017) 11:117–21. doi: 10.4103/ejd.ejd_308_16
25. Manne R, Gandikota C, Juvvadi SR, Rama HR, Anche S. Impacted canines: etiology, diagnosis, and orthodontic management. J Pharm Bioallied Sci. 2012 4(Suppl. 2):S234. doi: 10.4103/0975-7406.100216
26. Ghadimi MH, Amini F, Hamedi S, Rakhshan V. Associations among sella turcica bridging, atlas arcuate foramen (ponticulus posticus) development, atlas posterior arch deficiency, and the occurrence of palatally displaced canine impaction. Am J Orthod Dent Orthop. (2017) 151:513–20. doi: 10.1016/j.ajodo.2016.08.024
27. Kaya Y, Öztaş E, Goymen M, Keskin S. Sella turcica bridging and ponticulus posticus calcification in subjects with different dental anomalies. Am J Orthod Dent Orthop. (2021) 159:627–34. doi: 10.1016/j.ajodo.2019.11.024
28. Festa F, Rotelli C, Scarano A, Navarra R, Caulo M, Macrì M. Functional magnetic resonance connectivity in patients with temporomadibular joint disorders. Front Neurol. (2021) 12:629211. doi: 10.3389/fneur.2021.629211
29. Amelinda VP, Ismaniati NA, Purbiati M. Association of Sella Turcica bridge and ponticulus posticus with palatally impacted canine and hypodontia. J Int Dent Medical Res. (2019) 12:1090–4.
30. Pasini M, Giuca MR, Ligori S, Mummolo S, Fiasca F, Marzo G, et al. Association between anatomical variations and maxillary canine impaction: a retrospective study in orthodontics. Appl Sci. (2020) 10:5638. doi: 10.3390/app10165638
31. Leonardi R, Barbato E, Vichi M, Caltabiano M A. sella turcica bridge in subjects with dental anomalies. Eur J Orthod. (2006) 28:580–5. doi: 10.1093/ejo/cjl032
32. Sharma V, Chaudhary D, Mitra R. Prevalence of ponticulus posticus in Indian orthodontic patients. Dentomaxillofac Radiol. (2010) 39:277–83. doi: 10.1259/dmfr/16271087
33. Sekerci AE, Soylu E, Arikan MP, Ozcan G, Amuk M, Kocoglu F. Prevalence and morphologic characteristics of ponticulus posticus: analysis using cone-beam computed tomography. J Chiropr Med. (2015) 14:153–61. doi: 10.1016/j.jcm.2015.06.003
34. Kim MS. Anatomical variant of atlas: arcuate foramen, occpitalization of atlas, and defect of posterior arch of atlas. J Korean Neurosurg Soc. (2015) 58:528–33. doi: 10.3340/jkns.2015.58.6.528
35. Chen CH, Chen YK, Wang CK. Prevalence of ponticuli posticus among patients referred for dental examinations by cone-beam CT. Spine J. (2015) 15:1270–6. doi: 10.1016/j.spinee.2015.02.031
36. Hasani M, Shahidi S, Rashedi V, Hasani M, Hajiyan K. Cone Beam CT study of Ponticulus Posticus: Prevalence, Characterictics. Biomed Pharmacol J. (2016) 9:1067–72. doi: 10.13005/bpj/1050
37. Tambawala SS, Karjodkar FR, Sansare K, Motghare D, Mishra I, Gaikwad S, et al. Prevalence of ponticulus posticus on lateral cephalometric radiographs, its association with cervicogenic headache and a review of literature. World Neurosurg. (2017) 103:566–75. doi: 10.1016/j.wneu.2017.04.030
38. Adisen MZ, Misirlioglu M. Prevalence of ponticulus posticus among patients with different dental malocclusions by digital lateral cephalogram: a comparative study. Surg Radiol Anat. (2017) 39:293–7. doi: 10.1007/s00276-016-1728-4
39. Joshi V, Matsuda Y, Kimura Y, Araki K, Ishida H. Evaluation of prevalence and characteristics of ponticulus posticus among Japanese adults: a comparative study between CBCT imaging and lateral cephalogram. Orthod Waves. (2018) 77:134–41. doi: 10.1016/j.odw.2018.04.001
40. Kothari MK, Dalvie SS, Gupta S, Tikoo A, Singh DK. The C2 pedicle width, pars length, and laminar thickness in concurrent ipsilateral ponticulus posticus and high-riding vertebral artery: a radiological computed tomography scan-based study. Asian Spine J. (2019) 13:290–5. doi: 10.31616/asj.2018.0057
41. Bayrakdar İŞ, Miloğlu Ö, Yeşiltepe S, Yilmaz AB. Ponticulus posticus in a cohort of orthodontic children and adolescent patients with different sagittal skeletal anomalies: a comparative cone beam computed tomography investigation. Folia Morphol. (2018) 77:65–71. doi: 10.5603/FM.a2017.0075
42. Chitroda PK, Katti G, Baba IA, Najmudin M, Ghali SR, Kalmath B. Ponticulus posticus on the posterior arch of atlas, prevalence analysis in symptomatic and asymptomatic patients of gulbarga population. J Clin Diagn Res. (2013) 7:3044–7. doi: 10.7860/JCDR/2013/6795.3847
43. Gibelli D, Cappella A, Cerutti E, Spagnoli L, Dolci C, Sforza C. Prevalence of ponticulus posticus in a Northern Italian orthodontic population: a lateral cephalometric study. Surg Radiol Anat. (2016) 38:309–12. doi: 10.1007/s00276-015-1554-0
44. Giri J, Pokharel PR, Gyawali R. How common is ponticulus posticus on lateral cephalograms? BMC Res Notes. (2017) 10:1–5.
45. Govindraju P, Kumar TS. Prevalence of ponticulus posticus of the first cervical vertebra: a digital radiographic study. J Indian Acad Oral Med Radiol. (2017) 29:95–9. doi: 10.4103/jiaomr.JIAOMR_148_16
46. Ratnaparkhi MM, Pokharkar PM, Mhapuskar A, Hiremutt DR, Jain R, Telrandhe NV. Co-relation between presence of ponticulus posticus on the lateral cephalogram with cervical pain and vertigo. Eur J Mol Clin Med. (2021) 7:4047–53.
Keywords: ponticulus posticus, cervical vertebra, lateral cephalogram, CBCT, orthodontics, atlas posterior arch deficiency, maxillary canine impaction, sella turcica bridging
Citation: Macrì M, Perrella G, Varvara G, Murmura G, Traini T, Rendina F and Festa F (2021) Assessments of Prevalence of Ponticulus Posticus, Atlas Posterior Arch Deficiency, Sella Turcica Bridging, Maxillary Canine Impaction, and Associations Among Them in 500 CBCTs of Italian Orthodontic Patients. Front. Dent. Med. 2:708169. doi: 10.3389/fdmed.2021.708169
Received: 14 July 2021; Accepted: 25 October 2021;
Published: 10 December 2021.
Edited by:
Vahid Rakhshan, Institute for Cognitive Science Studies, IranReviewed by:
Cristina Grippaudo, Catholic University of the Sacred Heart, ItalyFarhad Sobouti, Mazandaran University of Medical Sciences, Iran
Copyright © 2021 Macrì, Perrella, Varvara, Murmura, Traini, Rendina and Festa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Monica Macrì, bS5tYWNyaUB1bmljaC5pdA==
 Monica Macrì
Monica Macrì Giada Perrella
Giada Perrella Giuseppe Varvara
Giuseppe Varvara Fabiola Rendina
Fabiola Rendina Felice Festa
Felice Festa