- 1Department of Oral Medicine, School of Dentistry, University of Washington, Seattle, WA, United States
- 2Department of Oral Biology, College of Dentistry, University of Illinois Chicago, Chicago, IL, United States
- 3Department of Pediatric Dentistry, School of Dentistry, University of Washington, Seattle, WA, United States
- 4The Santa Fe Group, New York, NY, United States
- 5Center for Ethics in Healthcare, School of Dentistry, Oregon Health & Science University, Portland, OR, United States
- 6School of Dentistry, Indiana University, Indianapolis, IN, United States
Dentistry and medicine traditionally practice as separate professions despite sharing goals for optimal patient health. Many US residents experience both poor oral and general health, with difficulty accessing care. More efficient collaboration between these professions could enhance health. The COVID-19 pandemic disclosed further disparities while underscoring concerns that physician supply is inadequate for population needs. Hence, enhancing healthcare provider education to better meet the public's health needs is critical. The proposed titles “Oral Physician” or “Oral Health Primary Care Provider” (OP-PCP) acknowledge dentist's capacity to diagnose and manage diseases of the orofacial complex and provide some basic primary healthcare. The US Surgeon General's National Prevention Council and others recommend such models. Medical and dental education already overlap considerably, thus it is plausible that dental graduates could be trained as OP-PCPs to provide primary healthcare such as basic screening and preventive services within existing dental education standards. In 2018, 23 dental and medical educators participated in an expert-opinion elicitation process to review educational competencies for this model. They demonstrated consensus on educational expansion and agreed that the proposed OP-PCP model could work within existing US Commission on Dental Accreditation (CODA) standards for predoctoral education. However, there were broader opinions on scope of practice details. Existing CODA standards could allow interested dental programs to educate OP-PCPs as a highly-skilled workforce assisting with care of medically-complex patients and to helping to reduce health disparities. Next steps include broader stakeholder discussion of OC-PCP competencies and applied studies including patient outcome assessments.
Introduction
Definition of the Problem
Many Americans experience poor health and lack adequate access to care. This is especially true for underserved populations such as low-income and minority groups. Dentistry and medicine practice as separate professions despite their shared missions to optimize their patients' health. Yet more efficient interprofessional collaboration could broaden access to oral and general healthcare, potentially reducing disparities and costs (1–4). Dental team disease screening could save between $42.4 million and $102.6 million in U.S. healthcare costs annually (5). The U.S. Surgeon General's National Prevention Council and others support the use of dentists in primary care roles (6–8). Meanwhile, concerns about lack of an adequate physician supply in the US have only increased during the COVID-19 pandemic.
This paper was submitted in response to a Frontiers in Dental Medicine challenge to “contribute to the development of evidence-based, cost-effective disease prevention and healthcare strategies applicable across diverse populations” on integrating oral and systemic health (9). It evaluates new dental education competency statements for training dentists to provide primary care tasks. To make this curriculum more cost-effective, it proposes to deliver this education during predoctoral education, within existing Commission on Dental Education (CODA) Standards (10). Hence, this educational action step augments recently published aspects of dental and medical integration related to the challenge (3, 4, 11–15).
Oral Health Primary Care Provider
“Oral Physician” or “Oral Health Primary Care Provider" (OP-PCP) are potential titles acknowledging general dentist's prospective expanded roles in basic primary healthcare (16–18). The American Dental Association (ADA) refers to dentists as “doctors who specialize in oral health” (19). The OP-PCP would be an enhanced dental practitioner functioning as part of an interprofessional healthcare team, connected virtually or in-person (20).
When dentists perform a thorough examination of dental patients, they typically assess the patient's blood pressure, and review medical, pharmaceutical, and psychosocial histories. They examine the oral cavity and head and neck, looking for oral diseases ranging from gingivitis to oral cancer. Dentists may detect signs and symptoms of other diseases beyond the oral cavity such as diabetes (21–24), cardiovascular disease (25–27), substance abuse (28, 29), eating disorders (30, 31) and child abuse or intimate partner violence (32–34), among others (35).
At the same time, an increasingly complex patient population requires dentists to become more sophisticated providers with greater knowledge of systemic conditions, and to be familiar with emerging approaches such as precision healthcare, salivary diagnostics, and new medical therapeutics (12). It is within the current legal scope of practice for dentists to diagnose and manage oral manifestations of systemic diseases, and to detect and help prevent systemic manifestations of oral diseases (14, 26, 36).
Appropriately trained dentists could build on these procedures to include some basic primary care in an integrated oral health practice, as described by Myers-Wright and Lamster (1). Expansion of primary screening within dental practice has been shown to be acceptable to the public. For example, random blood glucose testing in the dental office was well accepted by American patients and clinicians (21). Saudi Arabian patients accepted screening for hypertension and diabetes from dentists (37). In response to the pandemic, viral screening and immunizations became part of dentistry's scope of practice in many states (38).
The establishment of OP-PCPs within dentistry could shift dentistry's primary focus from restoring patient's oral health to maintaining their overall health. They could spend more time examining, diagnosing, and counseling patients and less time performing interceptive procedures. As leaders of dental teams, they can selectively delegate care to dental hygienists, expanded function dental assistants, or dental therapists as permitted by law (5, 20) and this could free their time to accommodate this expanded scope. Referral of more complex procedures to specialists makes room for more prevention in their practices an option (20).
Recent Changes and Timelines
The COVID-19 pandemic caused major disruptions in higher education, creating financial and logistical challenges for dental and other health professional schools. As schools struggled to provide adequate patient experiences while maintaining infrastructure and meeting other requirements, challenges led to innovation.
At the University of Washington (UW), the advent of the pandemic coincided with the construction of a new interprofessional health sciences education building, sparking new interprofessional bonds. The Health Sciences deans designed the building together to foster shared education and began planning a merged core curriculum in which dentistry is an equal partner with the other health professions. With the pandemic, scope of dental practice was already changing at the policy level. In Washington, dentists were permitted to prescribe or administer coronavirus screening (39). UW School of Dentistry successfully proposed that the state allow dentists, dental students, and dental hygienists to administer COVID-19 vaccines (40). Subsequently all UW health professions schools attended hands-on vaccination trainings together (with some dentist-trainers).
Immunization and disease testing by dentists are not new concepts. In 2005, Illinois Public Act 49-409 gave dentists status as “emergency dental responders” (Illinois Public Act 99-0025 changed this term to “dental responders”) who could provide emergency medical care, triage, and immunizations during a disaster if appropriately certified (41). Illinois dentists were authorized to provide influenza vaccines in 2016 (41) and Oregon has permitted dentists to vaccinate patients since 2019 (42). The US Public Readiness and Emergency Preparedness (PREP) Act extended COVID-19 vaccinator status to all US dentists, dental students, and dental hygienists in 2021 (43). Similarly, the pandemic led to approval and expansion of telehealth services, including certain tele dentistry services.
Beyond vaccination, the broader concept of training pre- and/or postdoctoral students in additional skills for primary care has received national attention within the profession. The American Dental Education Association's (ADEA) 2021 Annual Session featured a Chair of the Board Symposium entitled A Two-way Street: Primary Care and Oral Health Integration Training with speakers from Harvard's Center for Integration of Primary Care and Oral Health. A key takeaway was that “the integration of oral health and primary care won't happen overnight, but it won't happen at all if we do nothing” (44). Previous ADEA panel sessions have examined curricular innovations to foster integrated mastery of biomedical concepts (45).
CODA determines the minimum competency standards that graduating dentists must meet but does not dictate how dental schools teach skills or measure competency (10). Thus, as long as it meets existing CODA Standards, an accredited predoctoral dental education program may require its graduates to demonstrate competency in standards that exceed this national benchmark–such as assuring competency in expanded roles in basic, primary healthcare. The intention of this project was to evaluate the feasibility of developing a new curriculum to provide such training in pre-doctoral dental programs, beginning at the level of expert opinion, the base of the evidence-based pyramid (46).
Purpose
The purpose of this study was to gain expert opinion about whether a pre-doctoral dental program could train its dental graduates as OP-PCP to competently provide primary healthcare in a specific set of proposed professional activities while the program remained in compliance with existing dental competency standards of the Commission on Dental Accreditation (CODA).
Methods
Study Design
This expert opinion elicitation process (47) was a component of an Institutional Action Project for the Executive Leadership in Academic Medicine (ELAM) program at Drexel University by one author (SG). The study was deemed exempt from the institutional review board (IRB) human subject research review at UW.
Participants
The expert opinion elicitation took place between January and May 2018, engaging a convenience sample of educators in healthcare professions. The participant pool was structured to provide diversity by including different academic positions, areas of expertise, sex, and geographic location. Most participants were invited while attending the annual session of ADEA, where the chair-elect of the Section on Academic Affairs/Academic Deans (SG) was able to meet educational leaders face-to-face, explain the project, and request their participation. Some participants were added before and after the meeting to provide more range in expertise and teaching positions. Those who agreed to participate could respond in their preference of format: by email via questionnaire or discussion (SG), or through a verbal discussion (SG) by telephone or in-person.
Questionnaire Development
Sources representing expectations for dental and interprofessional competency were initially examined to create a list of professional skills an OP-PCP would need: Standards of the Commission on Dental Accreditation (10), American Dental Education Association (ADEA) Competencies for the New General Dentist (48), and Interprofessional Education Collaborative (IPEC) Core Competencies for Interprofessional Collaborative Practice (49). The competency statements in these three documents were grouped by content similarities. This revealed skills that an OP-PCP might need, which might not be covered or stressed in current dental education.
Each skill that a dental program could adopt to train OP-PCPs was restated in order to describe the level of competency proposed for new OP-PCP graduates. For some new skills, several alternative competency statements were proposed to determine how far the experts felt scope of practice should extend. All skills were examined to see whether they corresponded to any existing CODA standards. Then they were framed in a questionnaire, reviewed by study collaborators, and adjusted for content and clarity. In the final questionnaire, each respondent indicated whether they agreed with each proposed OP-PCP competency statement and optionally provided comments.
Data Analysis
As the intent was to collect qualitative data for a convenience sample of experts, the data were viewed at response distributions without statistical testing. These response distributions were categorized by two investigators as “agree/yes,” “disagree/no,” or “conditionally agree” (supported by comments). For questions requiring professional knowledge of clinical procedures (correlating with CODA Standard 24), only clinicians' responses were included. The investigators categorized comments into one of three groups: editorial directions for rewording or rewriting the proposal; affirmative statements, in which the respondent expressed enthusiasm; and conceptual/contextual observations or questions. The investigators (LM and SG) discussed any disparate categorizations to finalize this classification.
Results
All proposed OP-PCP competency statements corresponded with existing CODA standards. These statements, grouped with their related CODA Standards, are presented in Tables 1, 2, separating Standard 2-24 from the others. Respondents proposed three additional OP-PCP competency statements that also corresponded with existing CODA standards.

Table 1. CODA Standards (CS) except CODA 2-24, and related Proposed Competency Statements (PCS) for Oral Physician - Oral Health Primary Care Provider (OP-PCP).
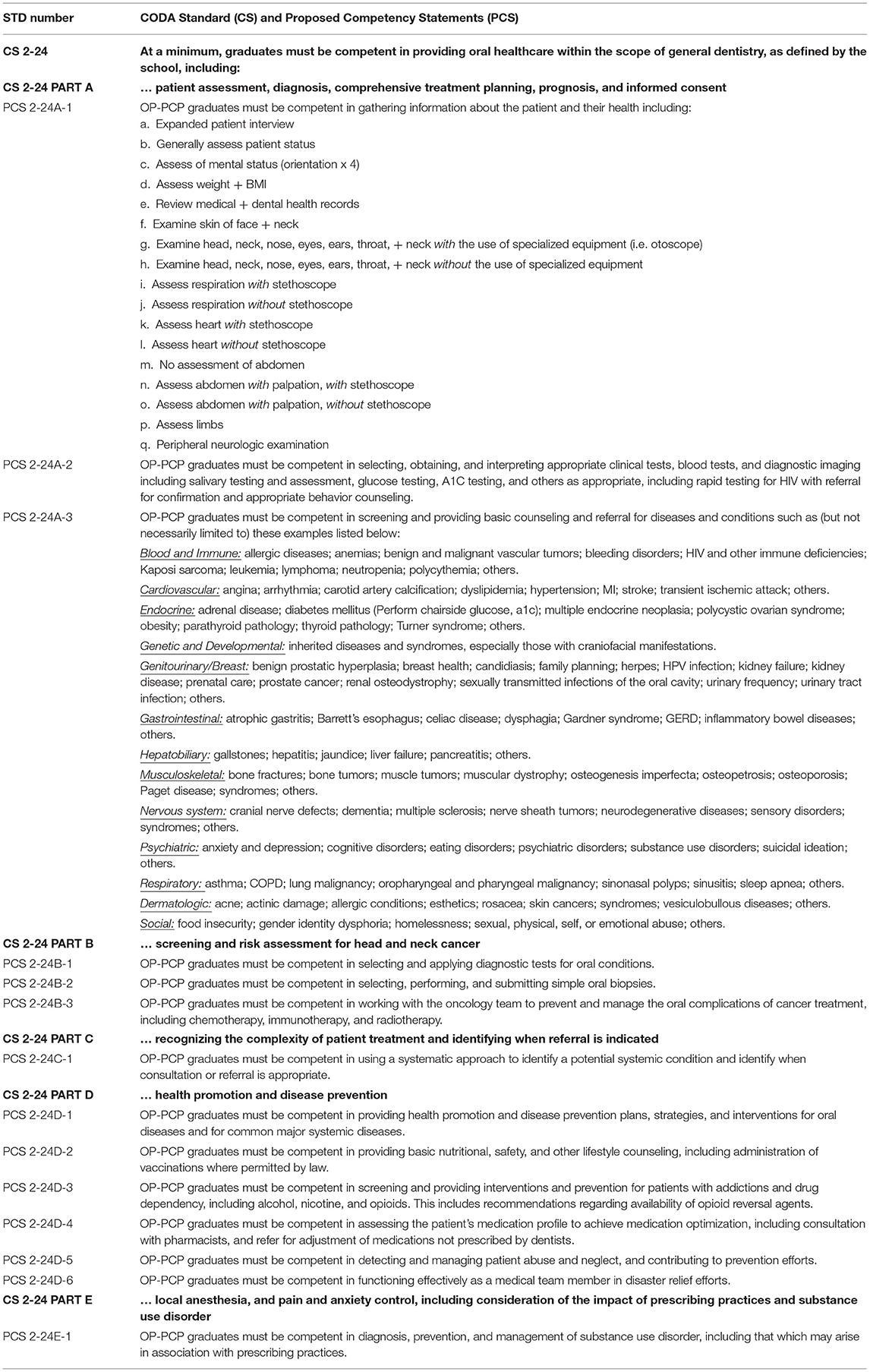
Table 2. CODA Standard (CS) 2-24 only, and related Proposed Competency Statements (PCS) for Oral Physician – Oral Health Primary Care Provider (OP-PCP).
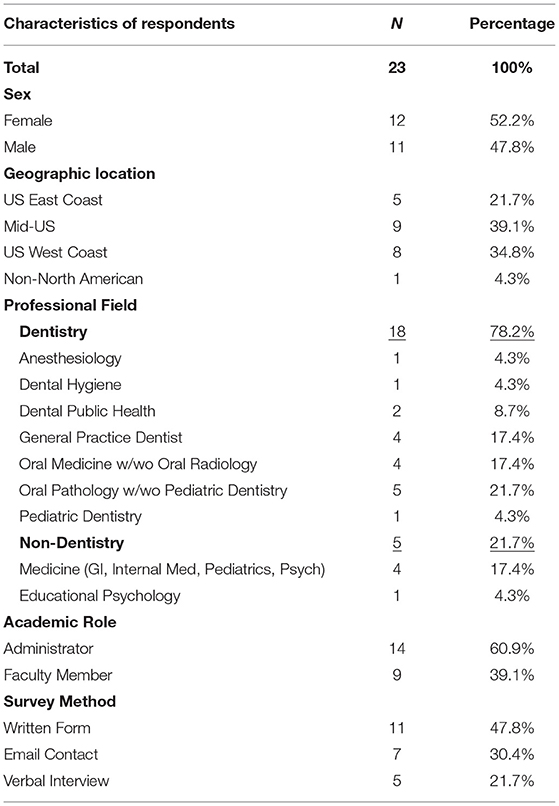
The convenience sample of experts captured distributions by sex, US location, professional field, academic role, and survey method (Table 3). No statistically significant differences were found among the characteristics when assessed by sex, professional field, or academic role (data not shown).
Distribution of support for the proposed OP-PCP competency statements showed general acceptance by the experts (Figure 1). Diversity of opinion occurred in some proposals associated with CODA Standard 2–24. The broadest range of opinion was seen with alternative competency statements proposed within Standard 2-24-A-1. Respondents considered how far they recommended OP-PCPs should develop skills in patient assessment, especially concerning use of an otoscope (2-24-A-1g) or stethoscope (2-24-A-1i, k, and n), assessing the abdomen (2_24-A-1n and o) or limbs (2-24-A-1n), or performing a peripheral neurologic examination (2-24-A-1q).
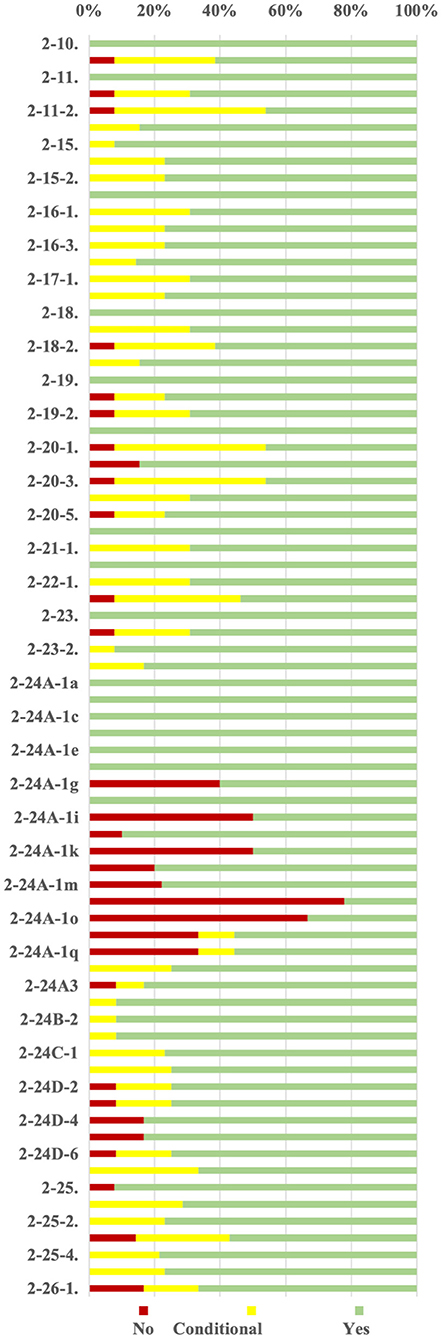
Figure 1. Distribution of support for Proposed Competency Statements (PCS) for OP-PCP related to CODA Predoctoral Standards 2–10 to 2–26 [–separate file].
Respondents provided 261 comments. Fifty percent were editorial directions, including recommendations for wordsmithing or combining the proposal with another or grouping it with a different CODA standard. Twenty six percent were affirmative statements, agreeing with the proposal. Twenty four percent were conceptual/contextual observations or questions. This third group of comments revealed lack of uniformity in current dental education. Some commentators said certain suggested skills are already being taught and assessed at some dental schools, while others commented that those same skills are unrealistic to teach or impossible to assess. Respondents mentioned obstacles such as scope of practice, lack of time in the curriculum, and challenges in achieving appropriate levels of competency.
Illustrative and notable comment examples particularly occurred regarding 2.24. Proposal 2.24A.1 suggests various elements of an expanded physical examination. One expert commented on their agreement with the entire list, “This will be a big part of training.” Another agreed that OP-PCPs should learn to examine the abdomen and commented: “Yes, any relation to having swallowed crown etc.,?” A third's comment on examining the limbs was: “Yes, visual, only if exposed,” meaning that the OP-PCP should not, for example, pull up a patient's sleeves or pant legs to examine their patient's arms or legs for dermatologic features supporting a diagnosis of lichen planus or lupus erythematosus.
Proposal 2.24D.1 is that OP-PCP be competent to provide health promotion and disease prevention plans, strategies, and interventions for oral diseases and for common major systemic diseases. Comments included, “I am not sure about breadth here either,” “I agree with all except interventions for major systemic diseases. This is where referral comes in,” and “As written–implies responsibility to treat primarily major systemic diseases–practicing medicine under current laws.” Similarly, 2.24D.4 proposes that OP-PCP be competent to assess the patient's medication profile to achieve medication optimization, including consultation with pharmacists, and refer for adjustment of medications not prescribed by dentists. One expert's reaction was, “Too far outside scope.” 2.24D.6 proposes that OP-PCP be competent to function effectively as a medical team member in disaster relief efforts. One expert commented, “Already should be doing this.” Another commented “Must define the role. They cannot do emergency amputations, for example,  [sic]. Need to define this carefully.”
[sic]. Need to define this carefully.”
Proposal 2.24B.3 for OP-PCP competency is to work with the oncology team to prevent and manage the oral complications of cancer treatment, including chemotherapy, immunotherapy, and radiotherapy. One comment hinted at potential for antagonism between specialists and those choosing expanded scope of practice for OP-PCPs: “This is now overlapping with the specialty of Oral Medicine.”
Discussion
Expert opinion indicated proposed OP-PCP training is rooted in existing ADEA, CODA, and IPEC competencies, especially interprofessional practice. Experts supported teaching and assessing these skills within the existing framework of pre-doctoral dental education, and felt it was realistic to do so to the “competency” level. They agreed OP-PCPs would require extra education in critical thinking, patient assessment, diagnosis and treatment planning, prevention and health promotion, medical management of conditions already within the scope of dental care, and in certain primary care medical tasks. The respondent's comments, made in 2018, demonstrated a lack of agreement on some details related to scope of practice.
But factors beyond expert opinion are also influencing the practice of dentistry and the shape of dental education. Changes wrought by the pandemic and the evolving recognition of oral-systemic interactions (3, 50) support increased interest in expanding the role of dentists. A growing emphasis on IPE and integration of oral health into primary care is evident in curriculum development, specific funding programs, and other efforts (51–55). Ongoing changes in dentistry and dental education are in keeping with these OP-PCP competency statement proposals: 2.20.2, participate in an interprofessional team approach that integrates oral health for the promotion and maintenance of overall health, and the prevention and treatment of disease; 2.24D.2, perform basic nutritional, safety, and other lifestyle counseling, including administration of vaccinations where permitted by law; and 2.24D.6, function effectively as medical team members in disaster relief efforts.
Barriers to Change: Market Factors
Difficulty obtaining compensation for medical screening and counseling could potentially discourage dentists from primary care despite the obvious benefits to patient's health. Medical insurance coding is different from the claims coding used in dental insurance (56). The range of allowable diagnoses and procedures that can be billed to medical insurance is limited (57). Even if dentists could potentially bill medical insurance for some services, they and their staff are usually not trained to do so. Without compensation, dentists could not feasibly screen for hypertension, diabetes, obesity, missed vaccinations, and other timely primary care tasks. Therefore, Proposal 2-19-2 is that OP-PCP graduates must be competent in describing how to use medical and dental billing to receive compensation for patient care, as allowed by the laws of the state. Medical insurers would also need to be willing to compensate them for these additional services.
Integrated dental and medical systems may provide the ideal setting for the OP-PCP (14, 54, 58–61). Large systems can institute value-based care models that incentivize desired changes; such models already occur in the dental marketplace. The rise of dental service organizations can also facilitate value-based changes, and their acquisition by larger health insurers. Larger health systems can feature interoperable electronic health records (E.H.R.) which improve collaboration and communication, reduce discrepancies and misunderstandings, and facilitate medical billing for dental care (62). Proposals 2-20-1, 2-20-2, 2-20-3, 2-20-4, and 2-20-5 describe competencies an OP-PCP must have to function successfully in such an integrated care setting.
Barriers to Change: Professional Identity
The self-identity of dentists is a barrier to change, whether by a new label or changing dentist's roles without re-branding them (63, 64). The increasing medical complexity of patients and broad calls for action to address systemic conditions such as hypertension (65) and diabetes (66) point to issues in which dentists could play a larger role. Nevertheless, dentistry retains a relative emphasis on technical skills (evident in the lengthy CODA Standard 2-24). Reluctance to cut any traditional skills to make way for new ones is likely.
It may be more difficult to convince dental students of the value of OP-PCPs than it would be to convince their patients (21, 36, 67, 68). Students enter school with expectations about being a dentist that don't include “primary care” tasks. They may say to themselves, “If I wanted to do that, I would have gone to medical school” (63, 64). Over the years, ADEA student surveys have shown that the top reasons students choose dentistry are personal dental experiences (54%), the influence of a family member or friend who is a dentist (38%) and the influence of their family dentist (33%) (69). Current models of dental practice, which have been slow to change, set expectations for students. However, recent events described already could influence a change in public and student expectations.
Barriers to Change: Cost of Dental Education
Given the high costs of dental education (reflected in tuition and high student debt), funding new programs will always be challenging. Dental school clinics operate primarily to train students and require a high faculty-to-student ratio. This model is less fiscally efficient than medical training that is embedded within hospitals and other clinical practice sites.
Dental schools are also typically safety net providers. While Medicaid covers pediatric dental care, adult dental benefits under Medicaid vary substantially between states, some states lacking them entirely. When money is tight, states often discontinue adult dental benefits. Traditional Medicare has no general dental benefit and Medicare Advantage Plans vary in coverage. Dental residencies with significant hospital-based training such as oral surgery or pediatric dentistry receive Graduate Medical Education (GME) funding but that money goes primarily to the hospitals, not the hospitals (70).
Students may be reluctant to participate in OP-PCP training if it would require additional time in dental school because 83% of dental students graduate with educational debt, averaging $304,824 in 2020 (71). Therefore, this proposal adapts predoctoral education within existing length of training. IPE could also advance this goal. If medical, dental, and nursing students all learned blood pressure measurement together, they would have greater confidence in each other's skills as future health professionals. Among others, Proposal 2-11-2, educate others about health, including clinicians from other health professions, using critical thinking and feedback techniques promotes this collaboration.
Barriers to Change: Scope of Practice
State laws govern the scope of practice of dentistry and other health professions. Changes in law allow healthcare practitioners, including faculty and students under their supervision, to perform tasks such as vaccinations and point of care diagnostic testing and counseling for systemic diseases (19).
For an expanded scope of dental practice to be successfully implemented, the profession would need to clearly define the desired scope of practice for the OP-PCP and achieve consensus on that definition. As Mathews [(72) Mathews 2010] mentions, this requires buy-in from all specialties. It would also be more likely to succeed if the change were supported by medical colleagues and those in other health professions. Such a conversation needs to begin somewhere, and the proposals presented to the experts in this project were aimed to begin such a discussion. Standard 2–24, the group of competency statements that lists specific clinical procedures, sparked the greatest diversity of opinion among the experts, as it was designed to do. Examples of comments provided by the experts, shared in the results, illustrate the need for further discussion and consensus on the scope of practice. Issues to be addressed include boundaries with dental specialties and other healthcare professions. Graduates would need to be cognizant of those limits, hence Proposal 2-18-1 is that OP-PCP graduates must be competent in describing the boundaries between dental and medical licensure.
Of relevance, historical changes that allowed advanced practice registered nurses (APRNs) and nurse practitioners (NP) in several states to be recognized as primary care providers are instructive. Such changes occurred in Massachusetts through legislation that recognized NPs as primary care providers (73). In Hawai'i, APRNs successfully introduced legislation to remove “barriers to full utilization of APRNs as primary healthcare providers with global signature authority and with prescriptive authority for controlled substances, medical equipment and therapeutic regimens in accordance with their scope of practice” (72). Key factors for a successful collaborative initiative were a comprehensive approach including all APRN specialties; key political champions who grasped the healthcare issues; the excellent reputation of APRNs; continuous communication and willingness to compromise on issues; and the support of nursing educators (72).
Limitations
This assessment is limited in its very nature, by design. Baseline expert opinion is challenging to acquire, especially using a grassroots, unfunded mechanism, yet it is valid to elicit opinions from a group of experts at the beginning of a bold new educational endeavor. The convenience sample is not generalizable to “population” but represents a valuable range of opinions. The expert opinion participant group had representation from females, males, deans, faculty members, and experts with geographic dispersion. The group included various ADA recognized dental specialty areas (74) whose definitions emphasize focus on patients or populations as opposed to procedures or specific anatomy.
Limitations of expert opinion are multifold. Foremost is the reliance on opinion versus synthesis of peer-reviewed scientific evidence. A high level of consensus was achieved in this one-round process, lending prima facie credibility to the findings. Nevertheless, this expert opinion assessment's function is simply to provide a starting point from which to define competencies for the OP-PCP, as demonstrated in similar processes in other professions (75). Further independent work based on this study is needed to progress toward finalizing OP-PCP educational competencies.
Next Steps
To become competent OP-PCPs, dental students would need authentic clinical experiences (76). Thus IPE must extend beyond didactic, simulation, and project-based learning, to include immersion in authentic collaborative clinical care settings where dentists function as OP-PCP (76–78).
Dental educators would need appropriate knowledge, skills, and attitudes to teach potential OP-PCPs. Many dental specialists in oral medicine, oral pathology, and oral surgery already have this expertise. Collaboration with other health professions education programs could help meet this need. Video teleconferencing could allow for more efficient faculty development across sites (76, 77).
Pilot projects could tackle key questions related to the modified curriculum's effectiveness and financial viability. Endpoints should include outcome measures that are student-centered (i.e., pass rates on national licensure examinations or alumni surveys), patient-centered (i.e., satisfaction of patients treated by these students), clinic-centered (i.e., satisfaction of health professionals who work with these students), finance-centered (i.e., differences in their clinical productivity as well as added training costs), and eventually community-centered (for example, improved healthcare outcomes in populations treated by these students and graduates).
Conclusions
No previous efforts have defined additional spheres of competency that should be required for dentists to function as OP-PCPs. These initial findings by 23 experts provide a platform for further discussion and action among dental and medical educators, policymakers, funders, health systems, patient groups and others. The healthcare system could gain high-quality capacity by using dentists as primary care providers within the scope of dental licensure to improve oral and overall health outcomes and achieve health equity.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
SG conceived and designed the study and wrote the first draft of the competency statements and questionnaire. JB and WM reviewed the study design. LK, WM, PB, and CM-K reviewed the competency statements and questionnaire. SG recruited participants and collected comments. LK organized the database and analysis. SG and LK wrote the introduction, methods, results, and conclusions. SG, LK, and WM wrote the abstract. WM, PB, JB, and CM-K wrote sections of the discussion. LK, WM, and SG contributed to manuscript revision. All authors read and approved the submitted version.
Funding
The University of Washington School of Dentistry provided funds for Sara Gordon to attend the Executive Leadership in Academic Medicine fellowship program.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Myers-Wright N, Lamster IB. A new practice approach for oral health professionals. J Evid Based Dent Pract. (2016) (Suppl. 16):43–51. doi: 10.1016/j.jebdp.2016.01.027
2. Nasseh K, Vujicic M, Glick M. The relationship between periodontal interventions and healthcare costs and utilization. Evidence from an integrated dental, medical, and pharmacy commercial claims database. Health Econ. (2017) 26:519–27. doi: 10.1002/hec.3316
3. Borgnakke WS, Poudel P. Diabetes and oral health: summary of current scientific evidence for why transdisciplinary collaboration is needed. Front Dent Med. (2021) 2:709831. doi: 10.3389/fdmed.2021.709831
4. Kleinman DV, Horowitz AM, Atchison KA. A framework to foster oral health literacy and oral/general health integration. Front Dent Med. (2021) 2:723021. doi: 10.3389/fdmed.2021.723021
5. Nasseh K, Greenberg B, Vujicic M, Glick M. The effect of chairside chronic disease screenings by oral health professionals on healthcare costs. Am J Public Health. (2014) 104:744–50. doi: 10.2105/AJPH.2013.301644
6. National Prevention, Health Promotion and Public Health Council. National Prevention Strategy. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General (2011). Available online at: https://www.hhs.gov/sites/default/files/disease-prevention-wellness-report.pdf (accessed April 27, 2021).
7. Joskow CR. Integrating oral health and primary care: federal initiatives to drive systems change. Dent Clin North Am. (2016) 60:951–68. doi: 10.1016/j.cden.2016.05.010
8. American State and Territorial Dental Directors (ASTDD). White Paper: Opportunities to Improving Oral Health and Chronic Disease Program Collaboration and Medical-Dental Integration. (2018). Available online at: https://www.astdd.org/docs/opportunities-for-improving-oh-and-cd-integration-white-paper.pdf (accessed September 23, 2021).
9. Somerman M, Mouradian WE. Field grand challenge: integrating oral and systemic health: innovations in transdisciplinary science, healthcare and policy. Front Dent Med. (2020) 1:15. doi: 10.3389/fdmed.2020.599214
10. Commission on Dental Accreditation (CODA). Accreditation standards for dental education programs. Chicago: American Dental Association 2018. Available online at: https://www.ada.org/~/media/CODA/Files/predoc_standards.pdf?la=en
11. Glurich I, Berg R, Panny A, Shimpi N, Steinmetz A, Nycz G, et al. Longitudinal observation or outcomes and patient access to integrated care following point-of-care glycemic screening in community health center dental safety net clinics. Front Oral Health. (2021) 2:670355. doi: 10.3389/froh.2021.670355
12. MacNeil RL, Hilario H. Input from practice: reshaping dental education for integrated patient care. Front Oral Health. (2021) 2:659030. doi: 10.3389/froh.2021.659030
13. Mays KA. Designing oral health curriculum that facilitates greater integration of oral health into overall health. Front Dent Med. (2021) 2:680520. doi: 10.3389/fdmed.2021.680520
14. Mosen DM, Banegas MP, Dickerson JF, Fellows JL, Pihlostrom DJ, Kershah HM, et al. Evaluating the effectiveness of medical-dental integration to close preventive and disease management care gaps. Front Dent Med. (2021) 2:670012. doi: 10.3389/fdmed.2021.670012
15. Mouradian W, Lee J, Wilentz J, Somerman M A perspective: integrating dental and medical research improved overall health. Front Dent Med. (2021) 2:699575. doi: 10.3389/fdmed.2021.699575
16. Nash DA. The oral physician. creating a new oral health professional for a new century. J Dent Educ. (1995) 59:587–97. doi: 10.1002/j.0022-0337.1995.59.5.tb02949.x
17. Giddon DB, Swann B, Donoff RB, Hertzman-Miller R. Dentists as oral physicians: the overlooked primary healthcare resource. J Prim Prev. (2013) 34:279–91. doi: 10.1007/s10935-013-0310-7
18. Kaste LM, Wilder JR, Halpern LR. Emerging topics for dentists as primary care providers. Dent Clin North Am. (2013) 57:371–6. doi: 10.1016/j.cden.2013.02.002
19. American Dental Association. Dentists: Doctors of Oral Health. Available online at: https://www.ada.org/en/about-the-ada/dentists-doctors-of-oral-health (accessed April 27, 2021).
20. Gordon SC, Beemsterboer P, Berg J, Kaste LM, Murdoch-Kinch CA, Mouradian W. The Other Doctors: Dentists in Primary Care. Philadelphia, PA: Executive Leadership in Academic Medicine 2018 Leadership Forum (2018).
21. Barasch A, Safford MM, Qvist V, Palmore R, Gesko D, Gilbert GH. Random blood glucose testing in dental practice: a community-based feasibility study from the dental practice-based research network. J Am Dent Assoc. (2012) 143:262–9. doi: 10.14219/jada.archive.2012.0151
22. Herman WH, Taylor GW, Jacobson JJ, Burke R, Brown MB. Screening for prediabetes and type 2 diabetes in dental offices. J Public Health Dent. (2015) 75:175–82. doi: 10.1111/jphd.12082
23. Glurich I, Bartkowiak B, Berg RL, Acharya A. Screening for dysglycaemia in dental primary care practice settings: systematic review of the evidence. Int Dent J. (2018) 68:369–77. doi: 10.1111/idj.12405
24. Grigoriadis A, Räisänen IT, Pärnänen P, Tervahartiala T, Sorsa T, Sakellari D. Prediabetes/diabetes screening strategy at the periodontal clinic. Clin Exp Dent Res. (2021) 7:85–92. doi: 10.1002/cre2.338
25. Glick M, Greenberg BL. The potential role of dentists in identifying patients' risk of experiencing coronary heart disease events. J Am Dent Assoc. (2005) 136:1541–6. doi: 10.14219/jada.archive.2005.0084
26. Jontell M, Glick M. Oral healthcare professionals' identification of cardiovascular disease risk among patients in private practice in Sweden. J Am Dent Assoc. (2009) 140:385–91. doi: 10.14219/jada.archive.2009.0075
27. Singer RH, Feaster DJ, Stoutenberg M, Hlaing WM, Pereyra M, Abel S, et al. Dentist's willingness to screen for cardiovascular disease in the dental care setting: Findings from a nationally representative survey. Community Dent Oral Epidemiol. (2019) 47:299–308. doi: 10.1111/cdoe.12457
28. Parish CL, Pereyra MR, Pollack HA, Cardenas G, Castellon PC, Abel SN, et al. Screening for substance misuse in the dental care setting: findings from a nationally representative survey of dentists. Addiction. (2015) 110:1516–23. doi: 10.1111/add.13004
29. Davis JM, Arnett MR, Loewen J, Romito L, Gordon SC. Tobacco dependence education: A survey of US and Canadian dental schools. J Am Dent Assoc. (2016) 147:405–12. doi: 10.1016/j.adaj.2015.12.012
30. Faine MP. Recognition and management of eating disorders in the dental office. Dent Clin North Am. (2003) 47:395–410. doi: 10.1016/S0011-8532(02)00108-8
31. Debate RD, Tedesco LA. Increasing dentists' capacity for secondary prevention of eating disorders: identification of training, network, and professional contingencies. J Dent Educ. (2006) 70:1066–75. doi: 10.1002/j.0022-0337.2006.70.10.tb04179.x
32. Bhandari M, Dosanjh S, Tornetta P. 3rd, Matthews D. Violence Against Women Health Research Collaborative Musculoskeletal manifestations of physical abuse after intimate partner violence. J Trauma. (2006) 61:1473–9. doi: 10.1097/01.ta.0000196419.36019.5a
33. Tam S, Joyce D, Gerber MR, Tan A. Head and neck injuries in adult victims of intimate-partner violence. J Otolaryngol Head Neck Surg. (2010) 39:737–43.
34. Femi-Ajao O. Perception of women with lived experience of domestic violence and abuse on the involvement of the dental team in supporting adult patients with lived experience of domestic abuse in England: a pilot study. Int J Environ Res Public Health. (2021) 18:2024. doi: 10.3390/ijerph18042024
35. Greenberg BL, Glick M, Frantsve-Hawley J, Kantor ML. Dentist's attitudes toward chairside screening for medical conditions. J Am Dent Assoc. (2010) 141:52–62. doi: 10.14219/jada.archive.2010.0021
36. Andrews EA. The future of interprofessional education and practice for dentists and dental education. J Dent Educ. (2017) 81:eS186–92. doi: 10.21815/JDE.017.026
37. Bin Mubayrik A, Al Dosary S, Alshawaf R, Alduweesh R, Alfurayh S, Alojaymi T, et al. Public attitudes toward chairside screening for medical conditions in dental settings. Patient Prefer Adherence. (2021) 15:187–95. doi: 10.2147/PPA.S297882
38. Burger D. Dentists Administering Vaccines Gaining Acceptance in States. ADA News (2021). Available online at: https://www.ada.org/en/publications/ada-news/2021-archive/february/dentists-administering-vaccines-gaining-acceptance-in-states (accessed September 30, 2021).
39. Dental Quality Assurance Commission. Coronavirus Screening in Dental Offices. State of Washington Department of Health. (2020). Available online at: https://www.doh.wa.gov/Portals/1/Documents/2300/2020/COVID-DentalCommScreening.pdf (accessed April 23, 2021).
40. Dental Quality Assurance Commission. Novel Coronavirus Disease 2019 (COVID-19) Vaccine Ordering and Administration. (2021). Available online at: https://www.doh.wa.gov/Portals/1/Documents/2300/CovidVaccineIS.pdf (accessed April 23, 2021).
41. Colvard MD, Vesper BJ, Kaste LM, Hirst JL, Peters DE, James J, et al. 3rd. The evolving role of dental responders on interprofessional emergency response teams. Dent Clin North Am. (2016) 60:907–20. doi: 10.1016/j.cden.2016.05.008
42. Oregon Immunization Program. Immunization Information for Dentists. Available online at: https://www.oregon.gov/oha/PH/PREVENTIONWELLNESS/VACCINESIMMUNIZATION/IMMUNIZATIONPROVIDERRESOURCES/Pages/Dentists.aspx (accessed April 25, 2021).
43. White House. Fact Sheet: President Biden Expands Efforts to Recruit More Vaccinators. (2021). Available online at: https://www.whitehouse.gov/briefing-room/statements-releases/2021/03/12/fact-sheet-president-biden-expands-efforts-to-recruit-more-vaccinators (accessed April 23, 2021).
44. American Dental Education Association. Key Takeaways from the 2021 Annual Session and Exhibit. (2021). Available online at: https://www.adea.org/uploadedFiles/ADEA/Content_Conversion/2021Annual_Session/AS21_KeyTakeaways_FINAL.pdf (accessed April 21, 2021).
45. American Dental Education Association. ADEA Chair of the Board of Directors Symposia. (2017). Available online at: https://www.adea.org/2016/program/chair-symposia.aspx/ (accessed April 21, 2021).
46. Hujoel PH. Grading the evidence: The core of EBD. J Evid Base Dent Pract. (2009) 9:122–4. doi: 10.1016/j.jebdp.2009.06.007
47. Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: characteristics and guidelines for use. Am J Public Health. (1984) 74:979–83. doi: 10.2105/AJPH.74.9.979
48. American Dental Education Association. Competencies for the new general dentist (as approved by the 2008 ADEA House of Delegates). J Dent Educ. (2008) 72: 823– 6. doi: 10.1002/j.0022-0337.2008.72.7.tb04552.x
49. Interprofessional Education Collaborative (IPEC). Core competencies for interprofessional Collaborative practice: 2016 Update. Washington, DC: Interprofessional Education Collaborative (2016). Available online at: https://ipec.memberclicks.net/assets/2016-Update.pdf (accessed September 30, 2021).
50. Kleinstein S, Nelson K, Freire M. Inflammatory networks linking oral microbiome with systemic health and disease. J Dent Res. (2020) 99:1131–9. doi: 10.1177/0022034520926126
51. Institute of Medicine (IOM). Advancing Oral Health in America. Washington, DC: The National Academies Press (2011). Available online at: https://www.hrsa.gov/sites/default/files/publichealth/clinical/oralhealth/advancingoralhealth.pdf (accessed April 27, 2021).
52. Clark M, Quinonez R, Bowser J, Silk H. Curriculum influence on interdisciplinary oral health education and practice. J Public Health Dent. (2017) 77:272–82. doi: 10.1111/jphd.12215
53. Park SE, Saldana F, Donoff RB, A. New integrated oral health and primary care education program in the dental student clinic. J Mass Dent Soc. (2016) 64:26–30.
54. Atchison KA, Rozier RG, Weintraub, JA. Integration of oral health and primary care: communication, coordination and referral. In: NAM Perspectives. Washington, DC: Discussion Paper, National Academy of Medicine (2018). doi: 10.31478/201810e
55. Health Resources and Services Administration (HRSA). Primary Care Dental Faculty Development Program. (2021). Available online at: https://www.hrsa.gov/grants/find-funding/hrsa-21-018
56. Napier RH, Bruelheide LS, Demann ET, Haug RH. Insurance billing and coding. Dent Clin North Am. (2008) 52:507–27. doi: 10.1016/j.cden.2008.02.008
57. California Dental Association. Dental Benefit Plans News. Billing Medical Plans for Dental Treatment. (2016). Available online at: https://www.cda.org/Home/News-and-Events/Newsroom/Article-Details/billing-medical-plans-for-dental-treatment-1 (accessed September 30, 2021).
58. Patel J, Mowery D, Krishnan A, Thyvalikakath T. Assessing information congruence of documented cardiovascular disease between electronic dental and medical records. AMIA Ann Symp Proc. (2018) 18:1442–50. Available online at: https://europepmc.org/article/med/30815189
59. MacNeil RL, Hilario H. The case for integrated oral and primary medical healthcare delivery: An introduction to an examination of three engaged healthcare entities. J Dent Educ. (2020) 84:917–9. doi: 10.1002/jdd.12286
60. Gesko DS, Worley D, Rindal BD. Creating systems aligned with the triple-aim and value-based care. J Public Health Dent. (2020) 80:S109–13. doi: 10.1111/jphd.12409
61. Santa Fe Group Webinar, Hinde W, Irving K, Baenen B; Murphy EA, Stenzel C. Learning from the Convergence of Medical and Dental Insurance: Who's Driving the Change. (2021). Available online at: https://santafegroup.org/webinars/learning-from-the-convergence-of-medical-and-dental-insurance-whos-driving-the-change/ (accessed June 30, 2024).
62. Feldman SS, Buchalter S, Hayes LW. Health information technology in healthcare quality and patient safety: literature review. JMIR Med Inform. (2018) 6:e10264. Erratum in: JMIR Med Inform. (2019) 7:e11320. doi: 10.2196/10264
63. Giddon DB. Should dentists become oral physicians? Yes, dentists should become oral physicians. J Am Dent Assoc. (2004) 135:438–49. doi: 10.14219/jada.archive.2004.0208
64. Giddon DB, Donoff RB, Edwards PC, Goldblatt LI. Should dental schools train dentists to routinely provide limited preventive primary medical care? two viewpoints viewpoint 1: dentists should be trained to routinely provide limited preventive primary care viewpoint 2: dentists should be trained in primary care medicine to enable comprehensive patient management within their scope of practice. J Dent Educ. (2017) 81:561–70. doi: 10.21815/JDE.016.023
65. Bakris G, Hill M, Mancia G, Steyn K, Black HR, Pickering T, et al. Achieving blood pressure goals globally: five core actions for health-care professionals. A worldwide call to action. J Hum Hypertens. (2008) 22:63–70. doi: 10.1038/sj.jhh.1002284
66. Reusch JEB. The Diabetes story: a call to action: 2018 presidential address. Diabetes Care. (2019) 42:713–7. doi: 10.2337/dci18-0050
67. Beazoglou TJ, Chen L, Lazar VF, Brown LJ, Ray SC, Heffley DR, et al. Expanded function allied dental personnel and dental practice productivity and efficiency. J Dent Educ. (2012) 76:1054–60. doi: 10.1002/j.0022-0337.2012.76.8.tb05358.x
68. Blue CM, Funkhouser DE, Riggs S, Rindal DB, Worley D, Pihlstrom DJ, et al. National Dental PBRN Collaborative Group. Utilization of non-dentist providers and attitudes toward new provider models: findings from the national dental practice-based research network. J Public Health Dent. (2013) 73:237–44. doi: 10.1111/jphd.12020
69. Istrate EC, Slapar FJ, Mallarapu M, Stewart DCL, West KP. Dentists of tomorrow 2020: an analysis of the results of the 2020 ADEA survey of U.S. dental school seniors. J Dent Educ. (2021) 85:427–40. doi: 10.1002/jdd.12568
70. Committee on the Governance and Financing of Graduate Medical Education. Board on Healthcare Services. Institute of Medicine. In: Eden J, Berwick D, Wilensky G, editors. Graduate Medical Education That Meets the Nation's Health Needs. Washington, DC: National Academies Press (US) (2014). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK248024/ (accessed September 30, 2021).
71. American Dental Education Association. Trends in Dental Education 2020-21. (2020). Available online at: https://www.adea.org/DentEdTrends (accessed April 24, 2021).
72. Mathews BP, Boland MG, Kim Stanton B. Removing barriers to APRN practice in the state of Hawai'i. Policy Polit Nursing Pract. (2010) 11:260–5. doi: 10.1177/1527154410383158
73. The Medical News. New Legislation Addresses Massachusetts Primary Crisis. (2008). Available online at: http://www.news-medical.net/news/2008/11/10/42685.aspx (accessed September 27, 2021).
74. American Dental Association. Specialty Definitions: Approved and Adopted by the National Commission on Recognition of Dental Specialties and Certifying Boards. Available online at: https://www.ada.org/en/ncrdscb/dental-specialties/specialty-definitions
75. Janke KK, Kelley KA, Sweet BV, Kuba SE. A modified Delphi process to define competencies for assessment leads supporting a doctor of pharmacy program. Am J Pharm Educ. (2016) 80:167. doi: 10.5688/ajpe8010167
76. Donoff RB, Daley GQ. Oral healthcare in the 21st century: It is time for the integration of dental and medical education. J Dent Educ. (2020) 84:999–1002. doi: 10.1002/jdd.12191
77. Giddon DB, Seymour BA, Swann B, Anderson NK, Jayaratne YS, Outlaw J, et al. Innovative primary care training: the Cambridge Health Alliance Oral Physician Program. Am J Public Health. (2012) 102:e48–9. doi: 10.2105/AJPH.2012.300954
Keywords: oral physician, primary care dentist, dental student, oral health primary care provider (OP-PCP), oral-systemic, interprofessional education/care (IPE/IPC), dental education, dentistry
Citation: Gordon SC, Kaste LM, Mouradian WE, Beemsterboer PL, Berg JH and Murdoch-Kinch CA (2021) Dentists as Primary Care Providers: Expert Opinion on Predoctoral Competencies. Front. Dent. Med. 2:703958. doi: 10.3389/fdmed.2021.703958
Received: 01 May 2021; Accepted: 08 October 2021;
Published: 11 November 2021.
Edited by:
Francisco Nociti, Universidade Estadual de Campinas, BrazilReviewed by:
Adolfo Contreras, University of Valle, ColombiaAlvin Gerard Wee, University of Minnesota Twin Cities, United States
Copyright © 2021 Gordon, Kaste, Mouradian, Beemsterboer, Berg and Murdoch-Kinch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara C. Gordon, Z29yZG9uc0B1dy5lZHU=
†These authors have contributed equally to this work and share first authorship
 Sara C. Gordon
Sara C. Gordon Linda M. Kaste
Linda M. Kaste Wendy E. Mouradian
Wendy E. Mouradian Phyllis L. Beemsterboer5
Phyllis L. Beemsterboer5 Joel H. Berg
Joel H. Berg Carol Anne Murdoch-Kinch
Carol Anne Murdoch-Kinch