- Department of Periodontics, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
The goal of this article is to inform dental practitioners and specialists of the benefits of smoking and vaping cessation in relation to COVID-19 transmission. COVID-19 caused by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) has affected more than 31.7 million people globally with infection rates continuing to rise rapidly. Smoking dramatically impairs lung function and gives rise to an increase in susceptibility for infection, allowing for a more difficult recovery due, in part, to the damage SARS-CoV-2 does to the lungs. Tobacco smoking is one of the primary causes of death in the United States (US), however, nearly 40 million adults still smoke cigarettes, with 4.7 million middle and high school students using at least one tobacco product, including electronic cigarettes. COVID-19 is transmitted through salivary droplets, causing severe bilateral pneumonia and significantly reduced lung function, putting smokers and vapers at greater risk through cross-contamination and face touching. So far, data from animal studies suggest that vaping leads to an increased susceptibility to infection, which coincides with evidence of increased rates of chronic bronchitis in vapers. There is yet to be data regarding the benefits of smoking and vaping cessation during the COVID-19 pandemic. However, there is evidence suggesting that 4 weeks or more of smoking cessation intervention reduces the risk of contracting COVID-19 and developing severe complications. Because of these probable connections, dental practitioners should advise their patients to stop smoking and/or vaping via the 5 As Cessation Strategy.
Introduction
The worldwide pandemic otherwise known as Coronavirus Disease 2019 (COVID-19) is caused by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). As of October 6, 2020, more than 35.5 million humans have been infected, and 1.04 million COVID-19 deaths have been reported in more than 213 countries (1). COVID-19 is easily transmissible through salivary droplets and aerosols and heavily impacts pulmonary health in severe cases. Cigarette smoking and electronic cigarette (e-cigarette) vaping damages the lungs, increasing the risk of contracting COVID-19 and developing severe complications (2–5). Nearly 40 million US adults still smoke cigarettes even though it is considered the primary cause of preventable death in the United States (US). Moreover, about 4.7 million middle and high school students use tobacco products, including e-cigarettes (6).
Among various novel tobacco products, e-cigarettes are now the most popular among high school students, surpassing traditional cigarettes (7). In 2020, 4.7% of middle school students and 19.6% of high school students reported current e-cigarette use in the past 30 days (8). New evidence suggests that 1 in 10 young adults who participated in smoking and 1 in 14 who participated in e-cigarette use within the past 30 days were more vulnerable to severe forms of COVID-19 illness. Specifically, 1 in 3 young adults who smoke are vulnerable to severe COVID-19 compared to 1 in 6 young adults who do not (5). The COVID-19 pandemic offers a rare opportunity to support smoking and vaping cessation as a public health intervention. The goal of this article is to inform dental practitioners and specialists of the benefits of smoking and vaping cessation in relation to COVID-19 transmission. To achieve this goal, an extensive PubMed and Google Scholar literature search using a combination of keywords such as COVID-19, smoking, vaping, tobacco, e-cigarettes, risk, transmission, and cessation was performed. This search produced 3,144 publications, governmental and medical websites. After careful review, the publications and websites were narrowed down by title to 182. Abstracts of publications and full papers were reviewed and 40 relevant publications and websites were included.
Increased Risk of Contracting COVID-19 with Increased Risk of Severe Complications
Smoking, vaping, and SARS-CoV-2 all affect the respiratory system. “The virus is highly transmissible by droplets and aerosolization and manifests with severe or critical bilateral pneumonia in 20% of symptomatic cases” (9). However, it is suspected that asymptomatic cases are also contagious based on radiographic imaging features and should be continuously monitored (9). A 2016 systematic review concluded that “smoking among adults is known to increase the risk of chronic obstructive pulmonary disease (Risk Ratio RR 4.01; 95% CI, 3.18–5.05), and asthma (RR 1.61; 95% CI, 1.07–2.42)” (10). In a study examining the Respiratory Syncytial Virus (RSV), a virus like SARS-CoV-2, cigarette smoke caused cell necrosis of airway epithelial cells in conjunction with the viral infection, resulting in inflammation and enhanced viral replication (11).
In 2003, the angiotensin converting enzyme 2 receptor (ACE2R) was identified as a viral binding site, enabling the SARS-CoV (Severe Acute Respiratory Syndrome Coronavirus) entry into human cells for replication. Data reveal that not only does SARS-CoV-2 use ACE2R as its receptor, but it can do so more easily than SARS-CoV. Exposure to tobacco smoke and other products containing nicotine causes changes in ACER2 expression, which can affect a person's susceptibility to SARS-CoV-2 infection (12–14).
E-cigarette use should also be regarded as a risk factor for enhancing respiratory symptoms caused by SARS-CoV-2. The Centers for Disease Control (CDC) identified E-cigarette or Vaping product use-Associated Lung Injury (EVALI) in August 2019, after serious lung infections unexpectedly occurred in healthy individuals. Various case studies reported diffuse basilar opacities and nodular lesions in the lungs (9). As more details emerged, it was found that e-cigarettes that contain tetrahydrocannabinol (THC), a chemical derived from marijuana and vitamin E acetate additive, were strongly linked to the outbreak (15). Recent findings demonstrate increased prevalence of marijuana vaping in middle and high school students. According to recent 2019 data, “past 30-day prevalence of marijuana vaping was reported by 3.9% (95% CI, 3.3%–4.7%) of middle school students and 14.0% (95% CI, 12.6%–15.5%) of high school students” (16).
A recent clinical trial concluded that short-term vaping of glycerol aerosol at high wattages causes airway epithelial injury and constant reduction in transcutaneous oxygen tension (indirect measurement of arterial blood gas tension) in young e-cigarette smokers (17). Animal studies with mice demonstrated that a two-week exposure to e-cigarette aerosols decreased survival rates and increased pathogen load with Streptococcus pneumoniae and influenza, two sources of human pneumoniae (18). A recent study concluded that the “risk of bronchitic symptoms increased by almost two-fold among past e-cigarette users (Odds Ratio (OR), 1.85; 95% [CI], 1.37–2.49), compared with never-users, and by 2.02-fold (95% CI, 1.42–2.88) among current users.” “Risk increased with frequency of current use (OR, 1.66; 95% CI, 1.02–2.68) for 1–2 days and 2.52 (95% CI, 1.56–4.08) for 3 or more days in past 30 days compared with those who had never used prior” (3). Thus, the data suggesting that vaping leads to an increased susceptibility to infection, which coincides with evidence of increased rates of chronic bronchitis in vapers (19).
Smokers infected with SARS-CoV-2 also have an increased risk of developing severe complications (20). A recent systematic review examined five studies in China that included positive COVID-19 patients with a smoking status. The review concluded that “smokers (compared to non-smokers) were 1.4 (RR = 1.4 95% CI: 0.98–2.00) times more likely to suffer from severe symptoms of COVID-19. They were also 2.4 times (RR = 2.4, 95% CI: 1.43–4.04) more likely to be placed in the intensive care unit (ICU), require mechanical ventilation, or die” (20). A recent meta-analysis by Zhao Qianwen, Meng Meng, and Kumar Rahul investigated the risk of developing severe COVID-19 in 2,002 chronic obstructive pulmonary disease (COPD) patients and current smokers. The results demonstrated a “relationship between current smoking and development of severe COVID-19 (OR 1.98; 95% CI: 1.29–3.05)” (21). An updated version of this meta-analysis, showed a “stronger association between current smoking and severe disease (OR 2.16; 95% CI: 1.45–3.22), and a reduction in study heterogeneity (I2 = 39%)” (22).
Similarly, in a meta-analysis where 11,590 positive COVID-19 patients with smoking history were examined, 29.8% of patients reported increased disease progression, compared with 17.6% of non-smoking patients. The results displayed a “significant association between smoking and COVID-19 progression (OR 1.91, 95% confidence interval [CI] 1.42–2.59, p = 0.001)” (23). Although further research is needed, it is reasonable to suggest that smokers and vapers may be more vulnerable to contracting COVID-19. This is due to an increase in hand-to-mouth motion involved in smoking, which poses the possibility of an increased chance of viral transmission from touch. Similarly, people who vape often do it socially by sharing spaces and equipment, thus increasing the risk of viral transmission.
The Benefits of Cessation in Relation to COVID-19 Transmission
Smoking and vaping causes harm to the lungs, leaving lungs more vulnerable to infection. Long-term cessation provides an opportunity for the body to recover from the damaging effects. Immune function improves as inflammation caused by smoking decreases and the white blood cell count returns to normal, thereby decreasing the rate of respiratory infections in former smokers (24). Research has also shown that the risk of heart disease begins to decline by 50% after 1 year of smoking cessation (25).
Although there are limited data available, a meta-analysis of 25 studies published in the Canadian Journal of Anesthesia in 2012 concluded that “at least 4 weeks of smoking cessation lowers the risk of respiratory complications compared to current smokers (RR 0.77; 95% CI 0.61 to 0.96 and RR 0.53; 95% CI 0.37 to 0.76)” (26). In another surgical study, “current smokers had a higher likelihood of 30-day mortality (RR 1.38; 95% CI, 1.11–1.72) and a higher incidence of postoperative complications such as pneumonia (OR 2.09; 95% CI, 1.80–2.43), unplanned intubation (OR 1.87; 95% CI, 1.58–2.21), and mechanical ventilation (OR, 1.53; 95% CI, 1.31–1.79)” (27). Thus, based on research data, there is reason to conclude that smoking cessation could reduce the risk of developing severe complications from COVID-19.
Equally imperative, populations at higher risk for many chronic diseases are similar to those at higher risk for developing oral diseases. Research has shown time and time again that tobacco use is a risk factor for oral cancer, oral mucosal lesions, periodontal disease, gingival recession, impaired wound healing, and coronal and root caries (28). A recent meta-analysis showed that “patients who had never smoked and former smokers presented no increased risk of tooth loss (RR 1.15; 95% CI = 0.98 to 1.35, I2 = 76%), while current smokers presented an increased risk of tooth loss (RR 2.60; 95% CI = 2.29 to 2.96, I2 = 61%)” (29). A 2018 systematic review concluded that 9 different oral mucosal lesions (OML) were detected in 65.4% (n = 36/55) e-cigarettes cases with greater prevalence of nicotinic stomatitis, hairy tongue, and angular cheilitis (30). While there is no strong evidence suggesting a direct association to the pathogenesis of oral disorders or cancers, there is in-vitro data indicating that vapor causes oxidative stress resulting in damage to gingival tissue (31).
Role of Dental Practitioner in Cessation Interventions
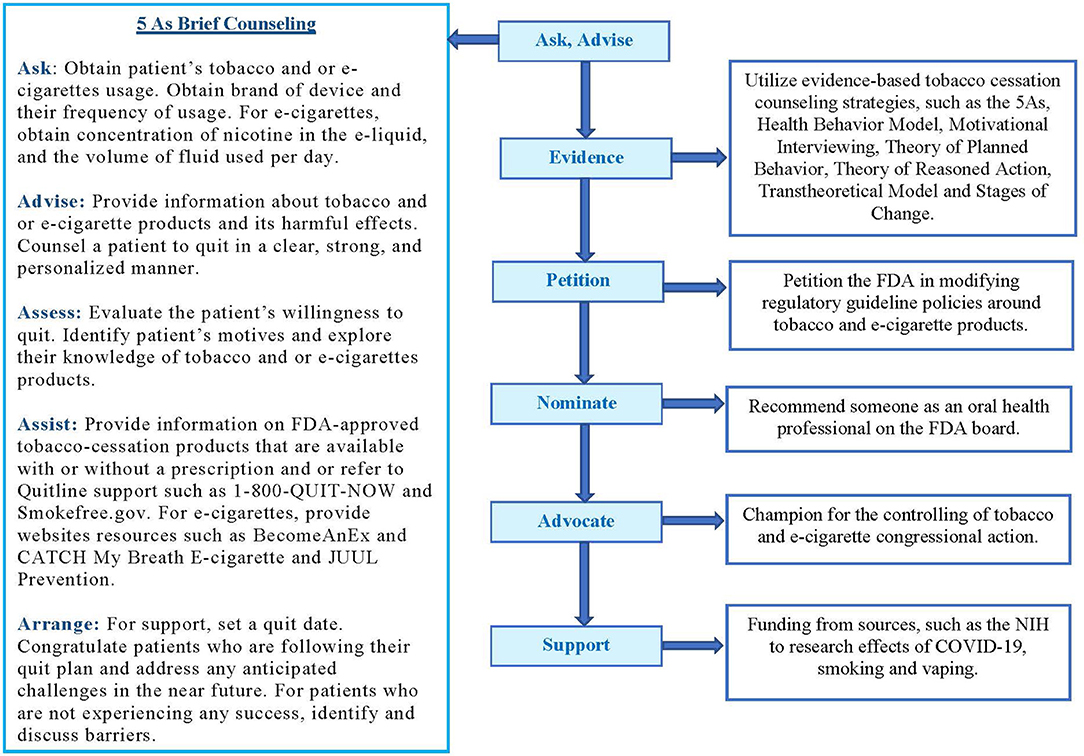
Given that people visit their dental practitioners more routinely than other healthcare providers, dental practitioners are uniquely positioned to screen and provide cessation intervention during the COVID-19 pandemic (32). Research has shown that a brief counseling session is one of the most cost-effective and useful means of smoking cessation in patients with established smoking-related oral disease (33). Furthermore, it was found that the dental team approach, reinforced repeatedly over a long period of time (pooled OR 1.71; 95% CI 1.44 to 2.03), was ideal for providing brief, office-based smoking cessation interventions (34). A recent study demonstrated that “patients who were satisfied with the brief counseling intervention 5As (Ask, Advise, Assess, Assist, and Arrange) were 5 times more likely to intend to quit using tobacco and 4 times more likely to recommend counseling to other tobacco users” (35).
Recently, a study documented the development of a dental practitioner-based e-cigarette cessation program called RAKE (ReACH Assessment of Knowledge for E-cigarette), consisting of an intervention that combines education with the 5A's– adapted for vaping cessation (36). Whilst research is ongoing, current evidence suggests that e-cigarettes are known to contain harmful ingredients such as ultrafine particles, flavoring chemicals such as diacetyl, volatile organic compounds, and heavy metals (24).
Dentists can use in-office or virtual visits to counsel their patients regarding smoking and vaping cessation, recommend prescription or over the counter pharmacotherapy, or nicotine replacement therapies. A recent study of 8,144 patients showed that “Varenicline had better abstinence rates compared with those on placebo (OR 3.61; 95% CI 3.07 to 4.24), those using the nicotine patch (OR 1.68; 95% CI 1.46 to 1.93), and those using bupropion (OR 1.75; 95% CI 1.52 to 2.01)” (37). Finally, practitioners should also make their patients aware of state and national Quitlines (1-800-QUIT-NOW) with counselors who are trained specifically to help smokers quit. Thus, research suggests that for smoking cessation assistance to be successful, a culture change is necessary in which health professionals become more proactive and better accepting of their increasing role in health promotion and prevention, especially during this time of the COVID-19 pandemic (38).
Conclusion
Smoking has long been the primary cause of preventable death and disability in the US. Many adult Americans smoke and have developed health issues related to tobacco usage. E-cigarettes, the popular alternative tobacco product, have also been linked to medical complications. Cigarette smoking and e-cigarette vaping dramatically damages the respiratory system, increasing the risk of contracting COVID-19 and developing severe complications. Smoking and vaping cessation can reduce those risks. For this reason, dental practitioners and specialists should advise their patients to stop smoking and vaping as well as provide the necessary tools and support for cessation success (Figure 1). Furthermore, dental practitioners and specialists should be motivated to advocate for tobacco and e-cigarette policy changes and funding around COVID-19, smoking and vaping research (Figure 1) (39, 40).
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author's Note
COVID-19, caused by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), has affected more than 31.7 million people worldwide with infection rates continuing to rise rapidly. Smoking dramatically impairs lung function and gives rise to an increase in susceptibility for infection allowing for a more difficult recovery due, in part, to the damage SARS-CoV-2 does to the lungs. COVID-19 is transmitted through salivary droplets, causing severe bilateral pneumonia and significantly reduced lung function, putting smokers and vapers at greater risk through cross-contamination and face touching. Because of these probable connections, dental practitioners should advise their patients to stop smoking and/or vaping via the 5 As cessation program. Awareness of this information is key, so that dental practitioners take this topic seriously and provide cessation services to their patients.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed October 1, 2020).
2. Wills TA, Pagano I, Williams RJ, and Tam EK. E-cigarette use and respiratory disorder in an adult sample. Drug Alcohol Depend. (2019) 194:363–70. doi: 10.1016/j.drugalcdep.2018.10.004
3. McConnell R, Barrington-Trimis JL, Wang K, Urman R, Hong H, Unger J, et al. Electronic cigarette use and respiratory symptoms in adolescents. Am J Respir Crit Care Med. (2017) 195:1043–9. doi: 10.1164/rccm.201604-0804OC
4. Ghosh A, Coakley RD, Ghio AJ, Muhlebach MS, Esther CRJr, Alexis NE, et al. Chronic e-cigarette use increases neutrophil elastase and matrix metalloprotease levels in the lung. Am J Respir Crit Care Med. (2019) 200:1392–401. doi: 10.1164/rccm.201903-0615OC
5. Adams SH, Park MJ, Schaub JP, Brindis CD, Irwin, and CE Jr. Medical vulnerability of young adults to severe COVID-19 illness-Data from the National Health Interview Survey. J Adolesc Health. (2020) 67:362–8. doi: 10.1016/j.jadohealth.2020.06.025
6. Center for Disease Control and Prevention. Data and Statistics. (2020). Available online at: https://www.cdc.gov/tobacco/data_statistics/index.htm (accessed October 1, 2020).
7. Creamer MR, Everett Jones S, Gentzke AS, Jamal A, and King BA. Tobacco product use among high school students - youth risk behavior survey, United States, 2019. MMWR Suppl. (2020) 69:56–63. doi: 10.15585/mmwr.su6901a7
8. Wang TW, Linda JN, Eunice PL, Chunfeng R, Karen AC, and Brian AK. E-Cigarette Use Among Middle and High School Students - United States, 2020. Centers for Disease Control and Prevention (2020). Available online at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6937e1.htm?s_cid=mm6937e1_w (accessed September 17, 2020).
9. Javelle E. Electronic cigarette and vaping should be discouraged during the new coronavirus SARS-CoV-2 pandemic. Arch Toxicol. (2020) 94:2261–2. doi: 10.1007/s00204-020-02744-z
10. Jayes L, Haslam PL, Gratziou CG, Powell P, Britton J, Vardavas C, et al. SmokeHaz: systematic reviews and meta-analyses of the effects of smoking on respiratory health. Chest. (2016) 150:164–79. doi: 10.1016/j.chest.2016.03.060
11. Arcavi L, and Benowitz NL. Cigarette smoking and infection. Arch Intern Med. (2004) 164:2206–16. doi: 10.1001/archinte.164.20.2206
12. Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. (2005) 11:875–9. doi: 10.1038/nm1267
13. Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS, and Sohal SS. Smoking upregulates angiotensin-converting enzyme-2 receptor: a potential adhesion site for novel Coronavirus SARS-CoV-2 (Covid-19). J Clin Med. (2020) 9:841. doi: 10.3390/jcm9030841
14. National Institutes of Health. Novel Coronavirus Structure Reveals Targets for Vaccines and Treatments. (2020). Available online at: https://www.nih.gov/news-events/nih-research-matters/novel-coronavirus-structure-reveals-targets-vaccines-treatments (accessed October 1, 2020).
15. Yale Medicine. E-cigarette or Vaping Product Use-Associated Lung Injury (EVALI). (2020). Available online at: https://www.yalemedicine.org/conditions/evali/ (accessed October 1, 2020).
16. Miech AR, Patrick EM, O'Malley PM, Johnston DL, and Bachman GJ. Trends in reported marijuana vaping among US adolescents, 2017-2019. JAMA. (2019) 323:475–6. doi: 10.1001/jama.2019.20185
17. Chaumont M, van de Borne P, Bernard A, Van Muylem A, Deprez G, Ullmo J, et al. Fourth generation e-cigarette vaping induces transient lung inflammation and gas exchange disturbances: results from two randomized clinical trials. Am J Physiol Lung Cell Mol Physiol. (2019) 316:L705–19. doi: 10.1152/ajplung.00492.2018
18. Thomas ES, Sachin G, Rajesh KT, Jinfang M, Jung-Hyun K, Kuladeep S, et al. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. US Natl Libr Med. (2015) 10:e0116861. doi: 10.1371/journal.pone.0116861
19. Gotts JE, Jordt SE, McConnell R, and Tarran R. What are the respiratory effects of e-cigarettes? BMJ. (2019) 366:l5275. doi: 10.1136/bmj.l5275
20. Vardavas CI, and Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. (2020) 18:20. doi: 10.18332/tid/119324
21. Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J Med Virol. (2020). doi: 10.1002/jmv.25889. [Epub ahead of print].
22. Guo FR. Smoking links to the severity of COVID-19: An update of a meta-analysis. J Med Virol. (2020) 92:2304–5. doi: 10.1002/jmv.25967
23. Patanavanich R, and Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res. (2020) 22:1653–6. doi: 10.1093/ntr/ntaa082
24. U.S. Department of Health and Human Services. The Health Consequences of Smoking-−50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health (2014). Available online at: https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf (accessed April 20, 2017).
25. World Health Organization (2020). Available online at: https://www.who.int/news/item/22-09-2020-tobacco-responsible-for-20-of-deaths-from-coronary-heart-disease (accessed October 15, 2020).
26. Wong J, Lam DP, Abrishami A, Chan MT, and Chung F. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth. (2012) 59:268–79. doi: 10.1007/s12630-011-9652-x
27. Turan A, Mascha EJ, Roberman D, Turner PL, You J, Kurz A, et al. Smoking and perioperative outcomes. Anesthesiology. (2011) 114:837–46. doi: 10.1097/ALN.0b013e318210f560
28. Winn DM. Tobacco use and oral disease. J Dent Educ. (2001) 65:306–12. doi: 10.1002/j.0022-0337.2001.65.4.tb03400.x
29. Souto MLS, Rovai ES, Villar CC, Braga MM, and Pannuti CM. Effect of smoking cessation on tooth loss: a systematic review with meta-analysis. BMC Oral Health. (2019) 19:245. doi: 10.1186/s12903-019-0930-2
30. Bardellini E, Amadori F, Conti G, and Majorana A. Oral mucosal lesions in electronic cigarettes consumers versus former smokers. Acta Odontol Scand. (2017) 76:226–8. doi: 10.1080/00016357.2017.1406613
31. Andrikopoulos GI, Farsalinos K, and Poulas K. Electronic nicotine delivery systems (ENDS) and their relevance in oral health. Toxics MDPI Open Access J. (2019) 7:61. doi: 10.3390/toxics7040061
32. Smith HA, and Smith ML. The role of dentists and primary care physicians in the care of patients with sleep-related breathing disorders. Front Public Health. (2017) 5:137. doi: 10.3389/fpubh.2017.00137
33. Coleman T. ABC of smoking cessation. Use of simple advice and behavioural support. BMJ. (2004) 328:397–9. doi: 10.1136/bmj.328.7436.397
34. Carr AB, and Ebbert J. Interventions for tobacco cessation in the dental setting. Cochrane Database Syst Rev. (2012) 2012:CD005084. doi: 10.1002/14651858.CD005084.pub3
35. Persai D, Panda R, Venkatesan S, Arora M, and Ahluwalia JS. Does receipt of 5As services have implications for patients' satisfaction in India? BMC Fam Pract. (2014) 15:209. doi: 10.1186/s12875-014-0209-2
36. Mungia R, Case K, Valerio M, Mendoza M, Taverna M, de la Rosa EM, et al. Development of an e-cigarette education and cessation program: a South Texas oral health network study. Health Promot Pract. (2020) 1–3. doi: 10.1177/1524839920914870
37. Anthenelli RM, Benowitz NL, West R, St Aubin L, McRae T, Lawrence D, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. (2016) 387:2507–20. doi: 10.1016/S0140-6736(16)30272-0
38. Van Rossem C, Spigt MG, Kleijsen JR, Hendricx M, van Schayck CP, and Kotz D. Smoking cessation in primary care: exploration of barriers and solutions in current daily practice from the perspective of smokers and healthcare professionals. Eur J Gen Pract. (2015) 21:111–7. doi: 10.3109/13814788.2014.990881
39. Prochnow JA. E-cigarettes: a practical, evidence-based guide for advanced practice nurses. J Nurse Pract. (2017) 13:449–55. doi: 10.1016/j.nurpra.2017.03.015
Keywords: COVID-19, smoking, vaping, risk, transmission, cessation, tobacco, e-cigarettes
Citation: Mungia R and Valdez DN (2020) Smoking, Vaping, and the Benefits Cessation in Times of COVID-19: A Public Health Perspective. Front. Dent. Med. 1:618364. doi: 10.3389/fdmed.2020.618364
Received: 16 October 2020; Accepted: 26 November 2020;
Published: 17 December 2020.
Edited by:
Henry Fergus Duncan, Trinity College Dublin, IrelandReviewed by:
Richard L. Gregory, Indiana University, Purdue University Indianapolis, United StatesCristiane Miranda Franca, Oregon Health and Science University, United States
Copyright © 2020 Mungia and Valdez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rahma Mungia, bXVuZ2lhQHV0aHNjc2EuZWR1
 Rahma Mungia
Rahma Mungia Danielle Nicole Valdez
Danielle Nicole Valdez