- 1School of Health and Welfare, Dalarna University, Falun, Sweden
- 2Institution of Health and Care Sciences, University of Gothenburg, Department of Building Design, Architecture and Civil Engineering, Chalmers University of Technology, Gothenburg, Sweden
- 3Health and Social Care Administration for the Elderly, City of Gothenburg, Gothenburg, Sweden
- 4Department of People and Society, Swedish University of Agricultural Sciences, Alnarp, Sweden
- 5Department of Quality Strategies Sahlgrenska University Hospital, Gothenburg, Sweden
The aim of this discussion paper is to show the way to the outdoors by shedding light on conditions in the physical environment enabling outdoor stays for older adults living in residential care facilities (RCFs). The origin was that outdoor stays is a basic human need and applies to everyone. However, despite extensive research on the health-promoting values of contact with the outdoors, it seems that for older adults in RCFs this is not met because they often have difficulty getting outdoors on their own. Therefore, the access to and the conditions of outdoor environments are discussed and exemplified through two cases based on evidence-based approaches, namely the principal model of four zones of contact with the outdoors, and the Swedish version of the Sheffield Care Environment Assessment Matrix (S-SCEAM). An interdisciplinary team, including both researchers and practitioners highlights future directions by showing the way to the outdoors on a national level with six suggested points. As a reader, you will gain increased knowledge about environmental qualities that support outdoor stays as well as initiatives that are needed to achieve equal conditions related to outdoor stays in RCFs.
Introduction
This discussion paper stems from an identified need of improvement in access and design of outdoor environments for older adults living in residential care facilities (RCFs), so that the basic human need of outdoor stays can be met. We are an interdisciplinary group representing healthcare science, landscape architecture and environmental psychology, as well as practitioners planning RCFs, who have become aware of the challenges of outdoor stays for older adults with frail health. Despite recommendations to spend time outdoors for at least 2 h per week (White et al., 2019), this is seldom the case for older adults in frail health who tend to use the outdoor environment to a limited extent (The Swedish National Board of Health and Welfare, 2012). An identified contributing factor is the design of the physical environment. Therefore, the aim was to show the way to the outdoors by shedding light on conditions in the physical environment enabling outdoor stays for older adults living in RCFs, a group that often faces difficulties in getting outdoors on their own. As the Swedish National Board of Health and Welfare's national survey now also contains items about outdoor environments and activities along with routines for how the outdoor environment should be used, these issues are timely. The goal is that all older adults in RCFs should be offered outdoor stays on a daily basis all year round, therefore, this discussion paper can serve as support for municipalities and authorities in steering toward increased outdoor stays for older adults. In the present study, RCF refers to a special residence offering 24-h health and social care services for older adults in frail health. The care staff mainly consists of licensed practical nurses and nursing assistants, but registered nurses, physiotherapists, and occupational therapists can also be involved in providing care within RCFs (The Swedish National Board of Health Welfare, 2023). Two cases in urban contexts are used to illustrate supportive and hindering conditions related to outdoor stays based on existing evidence- and experienced based knowledge.
Contact with the outdoors and health-related outcomes
Contact with the outdoors such as nature views (Sugiyama et al., 2022; Ulrich, 1984) and outdoor stays are basic human needs (Liljegren et al., 2024a) and applies to everyone, not least older adults in frail health who can benefit the most of having access to outdoor environments (Bengtsson and Lavesson, 2024; Ottosson and Grahn, 2006). One example is a multilevel cross-sectional study involving 290 older adults living in RCFs that showed significant associations between garden visits and self-perceived health (Dahlkvist et al., 2016). This is in accordance with the 2030 Agenda for Sustainable Development stating that accessible, safe, and inclusive green spaces can create opportunities for enriching the lives of the population in general, and older adults with disabilities in particular (United Nations, 2022). For instance, outdoor environments need to be supportive for persons with dementia, which is an essential part in creating dementia-friendly communities (Alzheimer's Society, 2023). A large body of research, including systematic reviews and intervention studies, has shown significant associations between nature and human physical, psychological and social health and wellbeing (Li et al., 2021; White et al., 2019; Yang et al., 2021; Zhang et al., 2017). For instance, outdoor environments can have a positive impact on mobility (Zieris et al., 2023), the immune system (Andersen et al., 2021), stress reduction (Litt et al., 2023), sleep quality (Shin et al., 2020), and reduce the risk of depression, loneliness, and isolation (Astell-Burt et al., 2022; Murroni et al., 2021). Having direct contact with nature also stimulates different senses (Bengtsson, 2015). Studies have also shown that the possibility to have a view from inside the building becomes a springboard that encourages persons to move outdoors (Musselwhite, 2018). Furthermore, spending time outdoors increases the level of physical activity compared to time spent inside and counteracts inactivity such as sedentary behavior and its negative consequences (Akpinar, 2016). Many of the residents spend most of their time indoors in the RCF (Rowles and Bernard, 2013), with a vast majority of waking hours spent in sedentary activities (de Souto Barreto et al., 2016; Parry et al., 2019). For older adults living in RCFs, access to outdoor environments is of particular importance since it can positively impact physical activity, orientation, social contacts, and overall wellbeing (Bengtsson et al., 2015; Brawley, 2001; Joseph, 2006). In dementia care, outdoor stays are linked to lower risk of falls (Detweiler et al., 2009), improved mood and sleep quality (Rappe and Kivelä, 2005), and increased social interactions (Raske, 2010). Moreover, garden activities can improve affective, behavioral, and cognitive factors among persons with dementia (Murroni et al., 2021; van der Velde-van Buuringen et al., 2021).
There is evidence that contact with nature also has positive effects for family members and healthcare staff (Ulrich et al., 1991). For instance, access to gardens have restorative benefits for staff working in healthcare settings (Liljegren et al., 2024a; Ulrich et al., 2008), increase their workplace satisfaction (Ulrich, 1999), and alleviate or prevent burnout among hospital staff (Cordoza et al., 2018; Mihandoust et al., 2021). Mihandoust et al. (2021) found that less exposure to nature views was related to higher burnout levels, especially in terms of emotional exhaustion and depersonalization. During the pandemic, outdoor stays was found to reduce stress and improve mental and physical health among staff (Gola et al., 2021; Iqbal and Abubakar, 2022; Loebach et al., 2022).
Older adults living in RCFs are characterized by variations in physical and cognitive health conditions (Schweighart et al., 2022). However, in several European countries there is an awareness of the increasing complexity in health conditions, with a growing need for high quality person-centered care and rehabilitation within RCFs (Barker et al., 2021; Spasova et al., 2018). Furthermore, older adults' opportunities to get out tend to decrease after moving into a RCF (Stoneham and Jones, 1997; The Swedish National Board of Health and Welfare, 2012), and outdoor stays has been reported by older adults themselves as the part they miss most after moving to a RCF (Liljegren et al., 2024a). Outdoor environments are of great importance and should be seen as a valuable resource. Unfortunately, there is a lack of incentives for outdoor stays as part of care and rehabilitation in RCFs, which is rooted in physical environmental obstacles as well as obstacles related to organizational challenges (Bengtsson, 2015; Liljegren et al., 2024a,b). Examples of physical obstacles are thresholds and heavy doors (Nordin et al., 2016), inadequate seating, and unsafe walkways (Anderzhon et al., 2007; Rodiek et al., 2014), absence of automatic doors and multi-story buildings (Liljegren et al., 2024b). Some organizational obstacles involve negative attitudes among healthcare staff toward spending time outdoors with the older adults, lack of mandate, and poor planning for outdoor stays as part of care and rehabilitation (Liljegren et al., 2024a).
Theoretical and conceptual frameworks
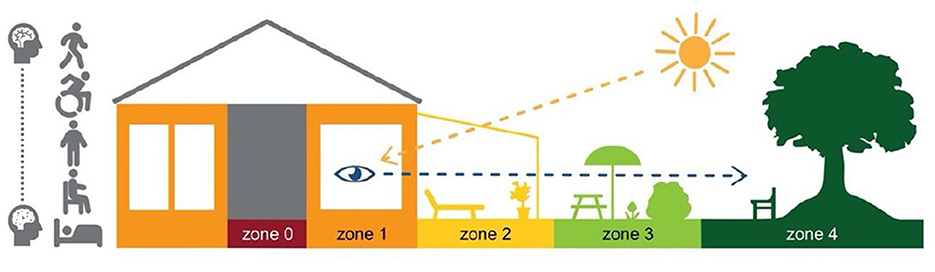
Today, it is well recognized that care and rehabilitation for persons with frail health, including persons with dementia, should be based on a person-centered approach (McCormack et al., 2021; Zidén et al., 2024). Although the physical environment is essential to the opportunities for activities and social interactions, it is not always seen as an integral part of person-centered care and rehabilitation. However, there is an increasing awareness that person-centredness can be supported or hindered by environmental quality (McCormack and McCance, 2021), not least in RCFs (Calkins et al., 2022). To provide outdoor environments useful for older adults with varying physical and cognitive functional status, a conscious design of the environments is therefore required (Bengtsson, 2015; Chaudhury et al., 2018; Ng et al., 2023). For this purpose, a Swedish theoretical principal model of four zones of contact with the outdoors has been developed (Bengtsson, 2015) with each zone having a health-promoting value. The zones range from outdoor contact via windows (zone 1), in transitions between the indoor and outdoor environments (e.g. entrances, patios, balconies) (zone 2), in the garden (zone 3), to the surroundings (zone 4). The model also involves zone 0 which represents the indoor environment without contact with the outside world, i.e., without windows. Furthermore, older adults' opportunities for outdoor stays are related to their physical body positions such as lying, sitting, standing, and in motion with or without aids or personal support. Thus, the model includes a range of body positions. For this article, the model has been further developed to also include a range of cognitive status illustrated by a schematic drawing of a brain with different degrees of change in tissue. For example, a cognitive decline can influence a adults' possibility to express needs and take initiatives for outdoor stays or understand how to move between indoor and outdoor environments (Figure 1).
To ensure supporting aspects of the environments are considered, various assessment instruments can be used. Internationally, instruments that measure the qualities of physical environments in RCFs for older adults with frail health have been identified (Elf et al., 2017; Calkins et al., 2022). Of these, the majority focus on the indoor environment, although some instruments also include aspects on the outdoor environments such as the Quality Evaluation Tool (QET) including 19 design qualities for comfortable and inspiring design of outdoor environments in RCFs (Bengtsson, 2015), the Seniors' Outdoor Survey (SOS) (Rodiek et al., 2016), and the Swedish version of the Sheffield Care Environment Assessment Matrix (S-SCEAM) (Nordin et al., 2015). S-SCEAM have been translated and validated for Swedish RCFs and is based on the idea that a well-functioning RCF can improve the wellbeing of older adults and support them as frailty increases. The instrument assesses the physical environment from a person-centered perspective where the user's needs are represented by domains theorized as central in the occupancy of such environments: Cognitive support, Physical support, Safety, Normalness, Openness and integration, Privacy, Comfort, and Choice. It contains a large number of items, each of which describes environmental aspects that relate to different locations within RCFs, including gardens.
Cases to illustrate quality evaluation by the application of tools
To illuminate varying conditions that support or hinder outdoor stays for older adults in RCFs, two cases from Sweden are presented with the use of the zone model and S-SCEAM. These two cases are chosen based on variations in terms of the prerequisites in the physical environments for contact with the outdoors, and they illustrate different environmental challenges that we have noted in relation to research and to practice, which will be described later. The zone model and S-SCEAM have not previously been used within the same study, however, the combination provided a comprehensive picture in this discussion paper. The RCFs are located in central Gothenburg, which is Sweden's second largest city with about 600,000 inhabitants.
Case A
The RCF is located on a plot of 5,902 m2. The plot contains one building that is shared between the RCF and other type of group housing. The building has five floors with 40 apartments intended for older adults. See Figure 2 for description of case A related to the zone model and S-SCEAM.
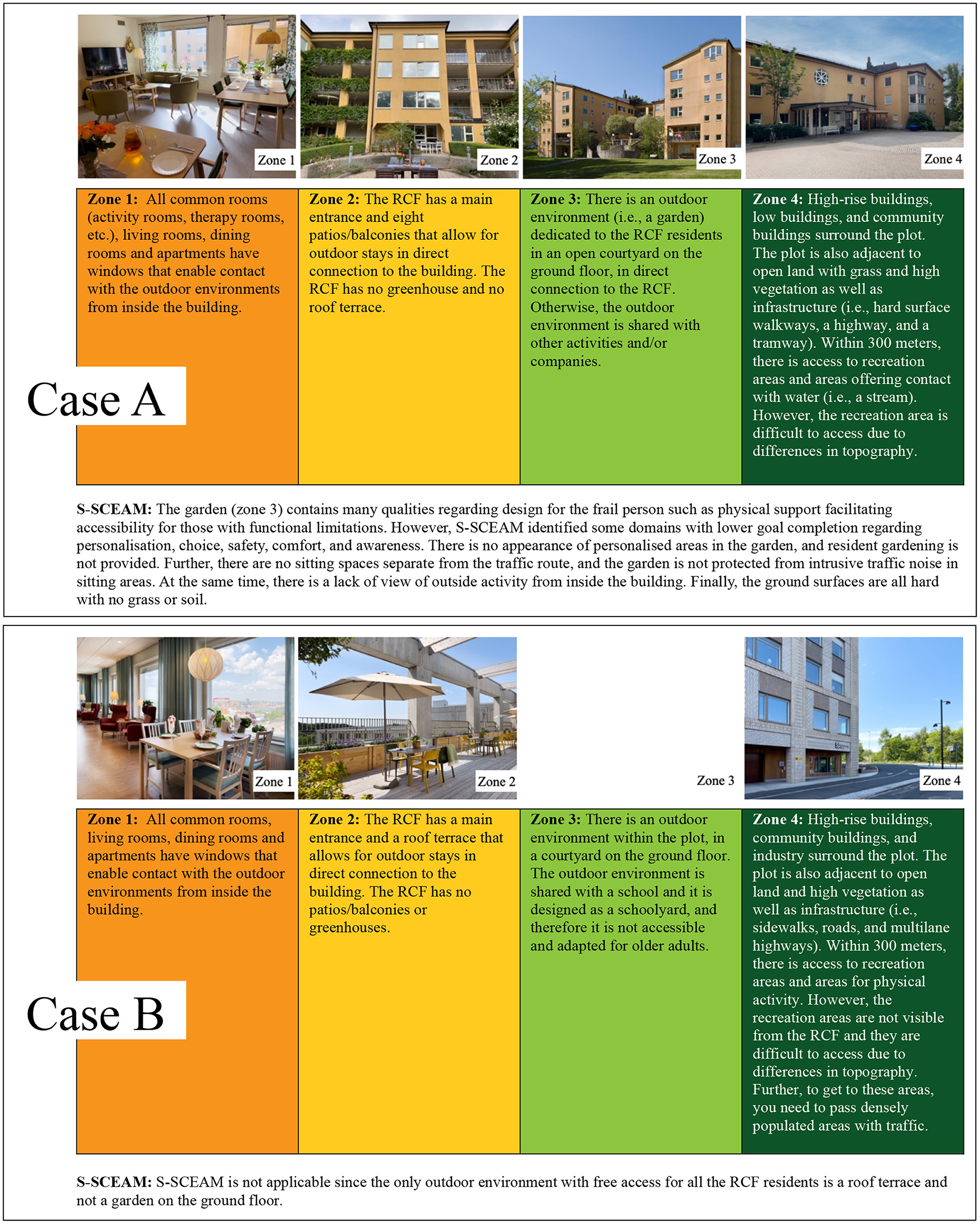
Figure 2. Description of Case A and Case B related to the zone model and S-SCEAM. Photo: Cordovan communication and P. Svensson, city of Gothenburg. Illustrated by M. Liljegren.
Case B
The RCF is located on a plot of 9571 m2. The plot contains one building that is shared between the RCF and a school. The building has seven floors with 100 apartments intended for older adults. See Figure 2 for description of case B related to the zone model and S-SCEAM.
The two cases presented in this discussion paper, showed interesting differences related to the varying conditions of the environments. These differences concerned both supportive and hindering aspects of the outdoor environments. In the following section, practical and theoretical aspects are discussed in relation to these two cases.
Getting outdoors in practice
Zone 1
Regarding zone 1, all common areas within the RCFs have outdoor contact via windows which is supported by recommendations stating that views of the outdoors from the interior should be maximized and distributed across multiple locations within the building (van den Berg et al., 2020). Although both cases have access to windows, there is a difference in what can be seen through the windows. In Case A, there are views toward greenery from all parts of the building, and the garden can be viewed from the indoor environment, whereas Case B have limited greenery views from the windows. Although the Case B have a panoramic view overlooking the harbor entrance and city center from some of the common rooms, the majority of the private rooms only have views toward the schoolyard and the facades of nearby buildings. Further, the roof terrace, i.e., the only outdoor environment with free access for all the RCF residents, cannot be seen through the windows. As previously mentioned, research has shown the importance of windows facing natural views. This aspect concerns from the older adults' private rooms and communal spaces. Previous research also shown that view of gardens and vegetation was a highly valued aspect when older adults themselves were asked what they preferred to look at through windows (Kearney and Winterbottom, 2006). Moreover, outdoor views from inside the building can be a springboard to get outdoors (Musselwhite, 2018). Considering that many older adults have frail health resulting in difficulties getting outside, access to zone 1 in terms of views through windows means a valuable contact with the outdoors, which therefore should be considered early in the process of building or renovation of RCFs.
Zone 2
Case A have access to shared balconies for all older adults and visitors. Compared to private balconies, shared balconies are usually larger and provide better accessibility, but do not offer the same opportunity for integrity. In Case A, all balconies have thresholds for water drainage purposes, which is also the case for the roof terrace in Case B. However, thresholds are problematic as they pose obstacles for persons to reach the outdoors, not least for those using a wheelchair or a walker, something that has been highlighted in several studies (Bengtsson and Carlsson, 2006; Liljegren et al., 2024a,b; Nordin et al., 2016; Rodiek et al., 2014). In Case B, the only outdoor space with free access for all is a roof terrace, and internal signage is used to find its way there.
On the roof terrace, there is limited greenery, and a lack of weather and climate protection features. Overall, it is a challenge to choose suitable plants on roof terraces as they are exposed to different conditions such as sun, wind, rain and drought. For example, trees can provide natural shade, but these are difficult to establish in such outdoor environments. This was recently highlighted in an Australian study of urban apartment buildings showing that roof terraces had poor access to green space in terms of trees and vegetated landscapes (Bolleter et al., 2024). Regardless of which plants are chosen, roof terraces need to provide protection in various weather conditions (Chao et al., 2014; Cioffi et al., 2007; Heath and Gifford, 2001). Weather protection is essential to meet the needs of older adults in RCFs (Bengtsson and Carlsson, 2006). Moreover, since the roof terrace is situated high up in the building, it can pose challenges for older adults with both physical and cognitive disabilities to get there, and previous research has shown that proximity to outdoor spaces is important, especially for persons with dementia (van den Berg et al., 2020). Based on insights from these two cases, we argue that environments in zone 2 such as balconies and roof terraces require well-founded solutions and should not form the primary outdoor environment within RCFs. In other studies, it has been suggested that contact with the outdoors can be facilitated if there are several access points to reach the outdoors, instead of only one that may be located far from the older adults' apartments (Kearney and Winterbottom, 2006).
Zone 3
In Case A, the S-SCEAM assessments identified environmental qualities in terms of physical support which is essential for accessing the outdoors for older adults with varying levels of functioning. The study by Potter et al. (2018) found that aspects related to both the physical environmental support, and the care staff influenced access to outdoor spaces for older adults in RCFs. For example, outdoor stays were restricted due to insufficient seating, uneven surfaces, or the need for assistance or permission from staff, which had a negative impact on their mood. Further, the S-SCEAM assessments showed that the garden was not protected from ambient environmental aspects such as traffic noise. This might be problematic for persons with cognitive disabilities as disturbing noise levels can be especially stressful (Joosse, 2012).
In case B, the ground floor outdoor environment was shared with children attending preschool and primary school. There may be benefits for older adults to share space with others such as cognitive stimulation and feelings of participation (Bengtsson, 2015), but it can also pose challenges as different groups have different needs. In addition, sufficient space is required both for school activities and for care and rehabilitation provided in RCFs. However, for schools in Sweden there are recommendations in terms of key figures of ~30–40 m2 for outdoor environment per child (The Swedish National Board of Housing, Building and Planning, 2024), something that does not exist for RCFs. Consequently, the school's outdoor environment is prioritized resulting in limited opportunities for outdoor stays for older adults' which can impinge on their choice and control. This is particularly relevant for case B, where the plot is divided between the RCF and a school. Since, at the time of construction, there were key figures for the school's outdoor environment but not for the RCF, it resulted in the outdoor environment at ground level being designed as a schoolyard and not in relation to the needs and preferences of the RCF tenants. In the city of Gothenburg, this problem has led to a local solution. A guideline with key figures for dedicated outdoor areas (within the plot) have recently been formulated for RCFs (Gothenburg City, 2024). However, the problem persists in other parts of Sweden, as well as in other European countries (Artmann et al., 2017).
Zone 4
Regarding zone 4, there are level differences in terms of steep slopes in both cases. Case A has a staircase from the garden in zone 3 to the public recreation areas in zone 4, as well as sloping ground outside the entrance. In case B, there is a longer distance to recreation areas in zone 4, and it is not visible from the RCF. Further, the RCF is located in a dense area with traffic. Although older adults do not spend much of their time in public green areas beyond RCFs, they value access to these environments (Kearney and Winterbottom, 2006). For older adults with frail health, both sloping ground and long distances are obstacles making it difficult to reach public areas in zone 4. This have been reported in previous research as aspects that restricted the use of outdoor spaces, not least for those who are using wheelchairs or walkers (van den Berg et al., 2020), and even small grade changes seemed to limit outdoor stays (Kearney and Winterbottom, 2006).
Theoretical perspectives on outdoor stays
Despite all the evidence of the importance of outdoor stays, it is still not considered a necessary activity at Swedish RCFs. Examples of hindering factors are staff being occupied with other tasks and have insufficient time to accompany the person, as well as their perception of safety risks in connection with outdoor stays (van den Berg et al., 2020). Consequently, systematic evaluations of outdoor access are given low priority. However, as researchers and practitioners, we believe that it is necessary to use evidence-based tools as part of ensuring and increasing the quality of outdoor environments in RCFs, which in turn can improve the living conditions of those living in such facilities. Furthermore, the importance of adopting a holistic and person-centered care approach is increasingly emphasized (Phelan et al., 2020). In this context, organizational factors such as leadership are essential for the care provided (Backman, 2018), which in turn will affect older adults' opportunities to access the outdoor environment.
With this paper, we want to highlight that the physical environment should be an integral part of care and rehabilitation, as environmental aspects have great potential to support or hinder the person-centered processes (McCormack et al., 2021). Because of this, and the fact that the construction and renovation of RCF involves large societal costs, we find it necessary to consider environmental qualities of the outdoor environment early in the planning process. The zone model provides a holistic perspective of contact with the outdoors where each of the four zones contributes to unique qualities. By using this model, environmental qualities can be related to the preferences, needs and prerequisites of older adults, and thus provide valuable knowledge about qualities that should be prioritized within the different zones (Bengtsson, 2015; Liljegren et al., 2024a,b). The S-SCEAM reflects core values of person-centredness such as opportunities for choice, comfort, integrity, and support for physical and cognitive frailty (Calkins et al., 2022; Nordin et al., 2015). The instrument can be used for detailed environmental assessments and identify specific aspects of the environment in need of improvement. For instance, environmental aspects that provide support for older adults with cognitive disabilities can be emphasized.
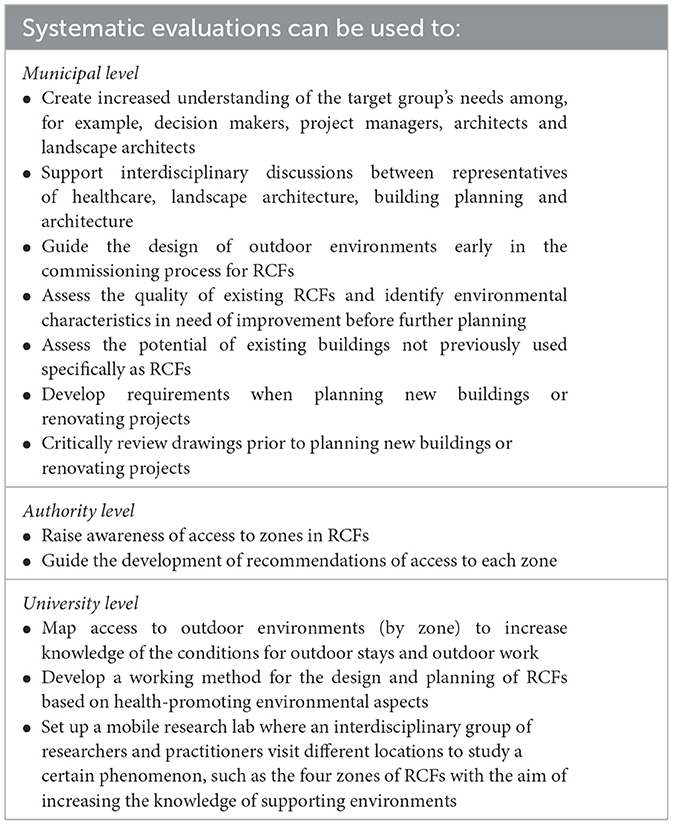
In sum, we argue that systematic evaluations are critical to the development of high-quality outdoor environments in RCFs, both the access to and the design of (see Table 1). The development can also lead to ground-level actions to change the working practices as part of overcoming the challenges of delivering outdoor care and rehabilitation. Today, there is already a shortage of healthcare staff in RCFs and the situation is expected to get worse. Hence, it is reasonable to assume that RCFs that invest in outdoor environments have a better chance of attracting new staff members.
Future directions
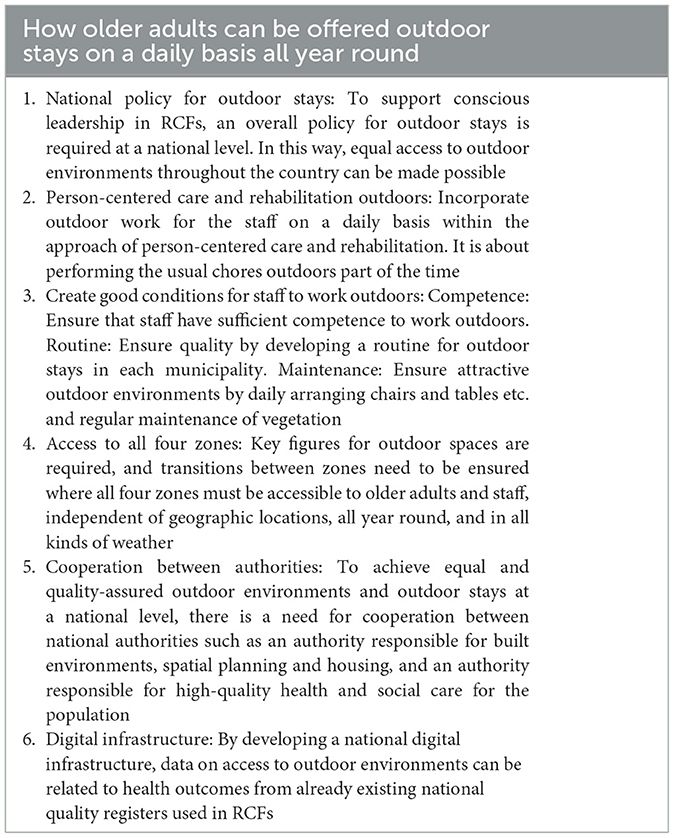
To show the way to the outdoors, we need to know where we come from. There is extensive and robust research on the health-promoting potential of the outdoors for older adults with frail health as well as for healthcare staff. Furthermore, there is research on supporting and hindering aspects in RCF environments, along with tools to support the planning of these environments. The importance of working from a person-centered approach has also previously been researched. The next step is therefore about the application of existing knowledge. See Table 2 for a presentation of conditions for how older adults can be offered outdoor stays on a daily basis.
Conclusion
In response to the opening title question: yes, outdoor stays is a basic human need even for older adults in RCFs, including persons with cognitive disabilities. This discussion paper highlights how older adults' needs of the outdoors in RCFs can be met by applying previous research on the health-promoting values of the outdoor environment in combination with six identified points. These points include the development of a national policy for outdoor stays, the promotion of person-centered care and rehabilitation outdoors as well as to create good conditions for healthcare staff to work outdoors. The points also include ensuring access to all four zones, cooperation between authorities, and the development of digital infrastructure.
The opportunities for outdoor stays for older adults in frail health is a matter of equality where such opportunities must be offered regardless of which municipality or RCF the older adult is living in. In this article, the researcher-practitioner interaction has crossed zones and showed the way to the outdoors. Now, municipalities and authorities need to join the discussion in Sweden and in other countries with similar challenges.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions. The data is not available until later. Requests to access these datasets should be directed to: Susanna Nordin, c25yQGR1LnNl.
Author contributions
SN: Writing – review & editing, Writing – original draft, Visualization, Validation, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. ML: Writing – review & editing, Writing – original draft, Visualization, Validation, Resources, Methodology, Investigation, Formal analysis, Conceptualization. MN: Writing – review & editing, Writing – original draft, Visualization, Validation, Resources, Methodology, Investigation, Formal analysis, Conceptualization. AB: Writing – review & editing, Writing – original draft, Visualization, Validation, Resources, Methodology, Investigation, Formal analysis, Conceptualization. HW: Writing – review & editing, Writing – original draft, Visualization, Validation, Resources, Methodology, Investigation, Formal analysis, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was part of the OUTFIT project funded by the Swedish Research Council for Health, Working Life and Welfare (2021-00212), Formas (2020-01959), and the Kamprad Family Foundation for Entrepreneurship, Research and Charity (20210117).
Acknowledgments
We gratefully acknowledge Dalarna University for the support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akpinar, A. (2016). How is quality of urban green spaces associated with physical activity and health? Urban For. Urban Green. 16, 76–83. doi: 10.1016/j.ufug.2016.01.011
Alzheimer's Society (2023). What is a dementia-friendly community? Available at: https://www.alzheimers.org.uk/get-involved/dementia-friendly-communities/what-dementia-friendly-community#:~:text=A%20dementia%2Dfriendly%20community%20is,are%20understood%2C%20respected%20and%20supported (accessed July 20, 2024).
Andersen, L., Corazon, S. S., and Stigsdotter, U. K. (2021). Nature exposure and its effects on immune system functioning: a systematic review. Int. J. Environ. Res. Public Health 18:1416. doi: 10.3390/ijerph18041416
Anderzhon, J. W., Fraley, I. L., Green, M., and Calkins, M. (2007). Design for aging post occupancy evaluations: lessons learned from senior living environments featured in the AIA's Design for Aging Review. Hoboken, NJ: John Wiley and Sons.
Artmann, M., Chen, X., Ioja, C., Hof, A., Onose, D., Ponizy, L., et al. (2017). The role of urban green spaces in care facilities for elderly people across European cities. Urban For. Urban Green. 27, 203–213. doi: 10.1016/j.ufug.2017.08.007
Astell-Burt, T., Hartig, T., Eckermann, S., Nieuwenhuisen, M., McMunn, A., Frumkin, H., et al. (2022). More green, less lonely? A longitudinal cohort study. Int. J. Epidemiol. 51, 99–110. doi: 10.1093/ije/dyab089
Backman, A. (2018). Leadership: Person-Centred Care and the Work Situation of Staff in Swedish Nursing Homes. Umeå: Umeå Universitet. doi: 10.1093/geroni/igy023.686
Barker, R. O., Hanratty, B., Kingston, A., Ramsay, S. E., and Matthews, F. E. (2021). Changes in health and functioning of care home residents over two decades: what can we learn from population-based studies? Age Ageing 50, 921–927. doi: 10.1093/ageing/afaa227
Bengtsson, A. (2015). From experiences of the outdoors to the design of healthcare environments. Acta Univ. Agric. Suec. 66, 1652–6880. doi: 10.13140/RG.2.1.2666.8964
Bengtsson, A., and Carlsson, G. (2006). Outdoor environments at three nursing homes: focus group interviews with staff. J. Hous. Elderly 19, 49–69. doi: 10.1300/J081v19n03_04
Bengtsson, A., Häagerhäll, C., Englund, J.-E., and Grahn, P. (2015). Outdoor environments at three nursing homes: semantic environmental descriptions. J. Hous. Elderly 29, 53–76. doi: 10.1080/02763893.2014.987863
Bengtsson, A., and Lavesson, L. (2024). “To promote contact with nature and greenery in healthcare environments,” in ARCH24 The 6th International Conference on Architecture, Research, Health, and Care (Espoo Aalto University ).
Bolleter, J., Hooper, P., Kleeman, A., Edwards, N., and Foster, S. (2024). A typological study of the provision and use of communal outdoor space in Australian apartment developments. Landsc. Urban Plan. 246:105040. doi: 10.1016/j.landurbplan.2024.105040
Brawley, E. C. (2001). Environmental design for Alzheimer's disease: a quality of life issue. Aging Mental Health 5, 79–83. doi: 10.1080/713650005
Calkins, M. P., Kaup, M. L., and Abushouseheh, A. M. (2022). Evaluation of environmental assessment tools for settings for individuals living with dementia. Alzheimers Dement. 8:e12353. doi: 10.1002/trc2.12353
Chao, T. W., Chai, C. W., and Juan, Y. K. (2014). Landscape design for outdoor leisure spaces at nursing homes: a case study of Taiwan Suang-Lien Elderly Centre. J. Food Agric. Environ. 12, 1036–1044.
Chaudhury, H., Cooke, H. A., Cowie, H., and Razaghi, L. (2018). The influence of the physical environment on residents with dementia in long-term care settings: a review of the empirical literature. Gerontologist 58, e325–e337. doi: 10.1093/geront/gnw259
Cioffi, J. M., Fleming, A., Wilkes, L., Sinfield, M., and Le Miere, J. (2007). The effect of environmental change on residents with dementia: the perceptions of relatives and staff. Dementia 6, 215–231. doi: 10.1177/1471301207080364
Cordoza, M., Ulrich, R. S., Manulik, B. J., Gardiner, S. K., Fitzpatrick, P. S., Hazen, T. M., et al. (2018). Impact of nurses taking daily work breaks in a hospital garden on burnout. Am. J. Crit. Care 27, 508–512. doi: 10.4037/ajcc2018131
Dahlkvist, E., Hartig, T., Nilsson, A., Högberg, H., Skovdahl, K., Engström, M., et al. (2016). Garden greenery and the health of older people in residential care facilities: a multi-level cross-sectional study. J. Adv. Nurs. 72, 2065–2076. doi: 10.1111/jan.12968
de Souto Barreto, P., Morley, J. E., Chodzko-Zajko, W., Pitkala, K. H., Weening-Djiksterhuis, E., Rodriguez-Manas, E., et al. (2016). Recommendations on physical activity and exercise for older adults living in long-term care facilities: a taskforce report. J. Am. Med. Dir. Assoc. 17, 381–392. doi: 10.1016/j.jamda.2016.01.021
Detweiler, M. B., Murphy, P. F., Kim, K. Y., Myers, L. C., and Ashai, A. (2009). Scheduled medications and falls in dementia patients utilizing a wander garden. Am. J. Alzheimers Dis. Other Dement. 24, 322–332. doi: 10.1177/1533317509334036
Elf, M., Nordin, S., Wijk, H., and McKee, K. (2017). A systematic review of the psychometric properties of instruments for assessing the quality of the physical environment in healthcare. J. Adv. Nurs. 73, 2796–2816. doi: 10.1111/jan.13281
Gola, M., Botta, M., Daniello, A. L., and Capolongo, S. (2021). Influence of nature at the time of the pandemic: an experience-based survey at the time of SARS-CoV-2 to demonstrate how even a short break in nature can reduce stress for healthcare staff. HERD 14, 49–65. doi: 10.1177/1937586721991113
Gothenburg City (2024). Göteborgs Stads riktlinje för styrande nyckeltal samt inriktning för samnyttjan och samlokalisering avseende kommunala verksamhetslokaler. Diarienummer: SLK-2021-00581, 2024-02-01 § 27. Gothenburg: City of Gothenburg.
Heath, Y., and Gifford, R. (2001). Post-occupancy evaluation of therapeutic gardens in a multi-level care facility for the aged. Activ. Adapt. Aging. 25, 21–43. doi: 10.1300/J016v25n02_02
Iqbal, S. A., and Abubakar, I. R. (2022). Hospital outdoor spaces as respite areas for healthcare staff during the COVID-19 pandemic. HERD 15, 343–353. doi: 10.1177/19375867221111530
Joosse, L. L. (2012). Do sound levels and space contribute to agitation in nursing home residents with dementia? Res. Gerontol. Nurs. 5, 174–184. doi: 10.3928/19404921-20120605-02
Joseph, A. (2006). Health Promotion by Design in Long-term Care Settings. Concord, CA: Center for Health Design.
Kearney, A. R., and Winterbottom, D. (2006). Nearby nature and long-term care facility residents: benefits and design recommendations. J. Hous. Elderly 19, 7–28. doi: 10.1300/Jo81v19n03_02
Li, D., Menotti, T., Ding, Y., and Wells, N. M. (2021). Life course nature exposure and mental health outcomes: a systematic review and future directions. Int. J. Environ. Res. Public Health 18:5146. doi: 10.3390/ijerph18105146
Liljegren, M., Bengtsson, A., Lindahl, G., and Wijk, H. (2024a). Introducing the Outdoor Environment as an Arena for Person-centred Care and Rehabilitation at Residential Care Facilities for Older Adults—a Care Worker's Perspective. Manuscript submitted for publication.
Liljegren, M., Bengtsson, A., Lindahl, G., and Wijk, H. (2024b). Older adults' needs and wishes for contact with the outdoors at residential care facilities: implications for theory and practice. HERD 1–18. doi: 10.1177/19375867241276296
Litt, J. S., Alaimo, K., Harrall, K. K., Hamman, R. F., Hébert, J. R., Hurley, T. G., et al. (2023). Effects of a community gardening intervention on diet, physical activity, and anthropometry outcomes in the USA (CAPS): an observer-blind, randomised controlled trial. Lancet Planet. Health 7, e23–e32. doi: 10.1016/S2542-5196(22)00303-5
Loebach, J., Rakow, D. A., Meredith, G., and Shepley, M.M. (2022). Time outdoors in nature to improve staff well-being: examining changes in behaviors and motivations among university staff in the use of natural outdoor environments since the emergence of the COVID-19 pandemic. Front. Psychol. 13:869122. doi: 10.3389/fpsyg.2022.869122
McCormack, B., McCance, T., Bulley, C., Brown, D., McMillan, A., Martin, S., et al. (2021). Fundamentals of Person-centred Healthcare Practice. Hoboken, NJ: Wiley Blackwell.
McCormack, B., and McCance, T. V. (2021). Development of a framework for person-centred nursing. J. Adv. Nurs. 56, 472–479. doi: 10.1111/j.1365-2648.2006.04042.x
Mihandoust, S., Pati, D., Lee, J., and Roney, J. (2021). Exploring the relationship between perceived visual access to nature and nurse burnout. HERD 14, 258–273. doi: 10.1177/1937586721996302
Murroni, V., Cavalli, R., Basso, A., Borella, E., Meneghetti, C., Melendugno, A., et al. (2021). Effectiveness of therapeutic gardens for people with dementia: a systematic review. Int. J. Environ. Res. Public Health 18:9595. doi: 10.3390/ijerph18189595
Musselwhite, C. (2018). The importance of a room with a view for older people with limited mobility. Qual. Ageing Older Adults 19, 273–285. doi: 10.1108/QAOA-01-2018-0003
Ng, L., Oliver, E., and Laver, K. (2023). Beyond garden design: a review of outdoor occupation in hospital and residential care settings for people with dementia. Aust. Occup. Ther. J., 70, 97–118. doi: 10.1111/1440-1630.12826
Nordin, S., Elf, M., McKee, K., and Wijk, H. (2015). Assessing the physical environment of older people's residential care facilities: development of the Swedish version of the Sheffield Care Environment Assessment Matrix (S-SCEAM). BMC Geriatr. 15:3. doi: 10.1186/1471-2318-15-3
Nordin, S., McKee, K., Wallinder, M., von Koch, L., Wijk, H., Elf, M., et al. (2016). The physical environment, activity and interaction in residential care facilities for older people: a comparative case study. Scand. J. Caring Sci. 31, 727–738. doi: 10.1111/scs.12391
Ottosson, J., and Grahn, P. (2006). Measures of restoration in geriatric care residences: the influence of nature on elderly people's power of concentration, blood pressure and pulse rate. J. Hous. Elderly 19, 227–256. doi: 10.1300/J081v19n03_12
Parry, S., Chow, M., Batchelor, F., and Fary, R. E. (2019). Physical activity and sedentary behaviour in a residential aged care facility. Australas. J. Ageing 38, E12–E18. doi: 10.1111/ajag.12589
Phelan, A., McCormack, B., Dewing, J., Brown, D., Cardiff, S., Cook, N. F., et al. (2020). Review of developments in person-centred healthcare. Int. Pract. Dev. J. 10, 1–29. doi: 10.19043/ipdj.10Suppl2.003
Potter, R., Sheehan, B., Cain, R., Griffin, J., and Jennings, P. A. (2018). The impact of the physical environment on depressive symptoms of older residents living in care homes: a mixed methods study. Gerontologist 58, 438–447. doi: 10.1093/geront/gnx041
Rappe, E., and Kivelä, S. L. (2005). Effects of garden visits on long-term care residents as related to depression. Horttechnology 15, 298–303. doi: 10.21273/HORTTECH.15.2.0298
Raske, M. (2010). Nursing home quality of life: study of an enabling garden. J. Gerontol. Soc. Work 53, 336–351. doi: 10.1080/01634371003741482
Rodiek, S., Lee, C., and Nejati, A. (2014). You can't get there from here: reaching the outdoors in senior housing. J. Hous. Elderly 28, 63–84. doi: 10.1080/02763893.2013.858093
Rodiek, S., Nejati, A., Bardenhagen, E., Lee, C., and Senes, G. (2016). The seniors' outdoor survey: an observational tool for assessing outdoor environments at long-term care settings. Gerontologist 56, 222–233. doi: 10.1093/geront/gnu050
Rowles, G. D., and Bernard, M. A. (2013). Environmental Gerontology: Making Meaningful Places in Old Age. Cham: Springer Publishing Company.
Schweighart, R., O'Sullivan, J. L., Klemmt, M., Teti, A., and Neuderth, S. (2022). Wishes and needs of nursing home residents: a scoping review. Healthcare 854. doi: 10.3390/healthcare10050854
Shin, J. C., Parab, K. V., An, R., and Grigsby-Toussaint, D. S. (2020). Greenspace exposure and sleep: a systematic review. Environ. Res. 182:109081. doi: 10.1016/j.envres.2019.109081
Spasova, S., Baeten, R., and Vanhercke, B. (2018). Challenges in long-term care in Europe. Eurohealth 24, 7–12.
Stoneham, J., and Jones, R. (1997). Residential landscapes: their contribution to the quality of older people's lives. Activ. Adapt. Aging 22, 17–26. doi: 10.1300/J016v22n01_03
Sugiyama, T., Carver, A., Sugiyama, M., Lorenzon, A., and Davison, T. E. (2022). Views of greenery and psychological well-being in residential aged care facilities: longitudinal associations. HERD 15, 219–232. doi: 10.1177/19375867211059757
The Swedish National Board of Health and Welfare (2012). Vad tycker de äldre om äldreomsorgen?: en rikstäckande undersökning av äldres uppfattning om kvaliteten i hemtjänst och äldreboenden 2012 (in Swedish) [What do older people think about elderly care?: a national survey on older person's views on the quality of home services and residential care facilities 2012]. Stockholm: Socialstyrelsen.
The Swedish National Board of Health and Welfare (2023). Öppna jämförelser 2023. Resultat från undersökningen ”Vad tycker de äldre om äldreomsorgen?” (Open comparisons in 2023. Results from the survey “What do the elderly think of elderly care?”). Available at: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2023-10-8759.pdf (accessed July 17, 2024).
The Swedish National Board of Housing Building and Planning. (2024). Boverkets allmänna råd (2015:1) om friyta för lek och utevistelse vid fritidshem, förskolor, skolor eller liknande verksamhet. (in Swedish) [The Housing Agency's general advice (2015:1) on open space for play and outdoor activities at leisure centers, preschools, schools or similar activities] BFS 2015:1. Available at: https://forfattningssamling.boverket.se/detaljer/BFS2015-1Accessed~2024-07-17.Boverket (accessed July 17, 2024).
Ulrich, R. (1984). View from a window may influence recovery from surgery. Science 224, 420–421. doi: 10.1126/science.6143402
Ulrich, R. S. (1999). “Effects of gardens on health outcomes: theory and research,” in Healing Gardens: Therapeutic Benefits and Design Recommendations, eds. C. Cooper-Marcus and M. Barnes (New York, NY: John Wiley), 27–86.
Ulrich, R. S., Simons, R. F., Losito, B. D., Fiorito, E., Miles, M. A., and Zelson, M. (1991). Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 11, 201–230. doi: 10.1016/S0272-4944(05)80184-7
Ulrich, R. S., Zimring, C., Zhu, X., DuBose, J., Seo, H., Choi, Y. S., et al. (2008). A review of the research literature on evidence-based healthcare design. HERD 1, 61–125. doi: 10.1177/193758670800100306
United Nations (2022). The 17 goals. Available at: https://sdgs.un.org/goals (accessed July 20, 2024)
van den Berg, M., Winsall, M., Dyer, S. M., Breen, F., Gresham, M., and Crotty, M. (2020). Understanding the barriers and enablers to using outdoor spaces in nursing homes: a systematic review. Gerontologist 60, e254–e269. doi: 10.1093/geront/gnz055
van der Velde-van Buuringen, M., Achterberg, W. P., and Caljouw, M. A. (2021). Daily garden use and quality of life in persons with advanced dementia living in a nursing home: a feasibility study. Nurs. Open 8, 1243–1253. doi: 10.1002/nop2.740
White, M. P., Alcock, I., Grellier, J., Wheeler, B. W., Hartig, T., Warber, S. L., et al. (2019). Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Sci. Rep. 9, 1–11. doi: 10.1038/s41598-019-44097-3
Yang, B.-Y., Zhao, T., Hu, L.-X., Browning, M. H., Heinrich, J., Dharmage, S. C., et al. (2021). Greenspace and human health: an umbrella review. Innovation 2:100164. doi: 10.1016/j.xinn.2021.100164
Zhang, G., Poulssen, D. V., Lygum, V. L., Corazon, S., Gramkow, M. C., and Stigsdotter, U. K. (2017). Health-promoting nature access for people with mobility impairments: a systematic review. Int. J. Environ. Res. Public Health 14:703. doi: 10.3390/ijerph14070703
Zidén, L., Erhag, H. F., and Wijk, H. (2024). Person-centred care as a tool to reduce behavioral and psychological symptoms in older adults with dementia living in residential care facilities. Geriatr. Nurs. 57, 51–57. doi: 10.1016/j.gerinurse.2024.03.003
Keywords: dementia, environmental evaluation tools, older adults, outdoor environment, outdoor stay, person-centered care and rehabilitation outdoors, researcher-practitioner interaction, residential care facility
Citation: Nordin S, Liljegren M, Nilsson M, Bengtsson A and Wijk H (2024) Outdoor stays—A basic human need except for older adults in residential care facilities? Researcher-practitioner interaction crosses zones and shows the way out. Front. Dement. 3:1470691. doi: 10.3389/frdem.2024.1470691
Received: 25 July 2024; Accepted: 08 October 2024;
Published: 29 October 2024.
Edited by:
Habib Chaudhury, Simon Fraser University, CanadaReviewed by:
Irina Anna Skylar-Scott, Stanford University, United StatesCopyright © 2024 Nordin, Liljegren, Nilsson, Bengtsson and Wijk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanna Nordin, c25yQGR1LnNl
†ORCID: Madeleine Liljegren orcid.org/0000-0003-4656-9019
Martin Nilsson orcid.org/0000-0002-8634-735X
Anna Bengtsson orcid.org/0000-0003-1312-9711
Helle Wijk orcid.org/0000-0003-2396-6505
 Susanna Nordin
Susanna Nordin Madeleine Liljegren2†
Madeleine Liljegren2†