- 1Department of Journalism and Communication Research, Hanover University of Music, Drama and Media, Hanover, Germany
- 2Department of Psychiatry and Psychotherapy, University of Leipzig, Leipzig, Germany
- 3Center for Public Mental Health, Wagram, Austria
Introduction: Depression is a globally prevalent mental disorder; however, the stigmatization of individuals experiencing depression remains a significant challenge. The effectiveness of mental health promotion efforts and anti-stigma messages is contingent upon individuals' existing beliefs and the stigmatizing potential of their attitudes. Thus, understanding how individuals perceive mental disorders such as depression, as well as their communicative accessibility, is vital from a strategic health communication standpoint. This study explored the prevailing cognitive frames regarding depression in Germany, and the corresponding affective reactions toward individuals experiencing depression. Differences in communicative accessibility, individuals' social proximity to the topic, as well as socioeconomic characteristics were used to inform stigma-sensitive targeting strategies.
Method: A representative survey of the German adult population (N = 1,530) was conducted, using a vignette describing a person with symptoms of major depression. Factor and cluster analyses identified four distinct cognitive frames of depression, characterized by varying stigmatizing attitudes and attributions of responsibility.
Results: The study has revealed that stigmatizing cognitive frames demonstrate lower receptivity to mental health information. Individuals with stigmatizing perspectives represent a significant portion of the population, have reduced receptivity to mental health information, and are likely to exhibit defensive or even negative affective responses to anti-stigma efforts.
Discussion: The findings underscore the significance of considering cognitive frames as complex but suitable approaches for target group segmentation in mental health communication strategies. The development of tailored and creative low-threshold strategies fitting well within the cognitive frames of individuals with stigmatizing perspectives seems essential.
1 Introduction
Depression is the most prevalent and widely known mental disorder worldwide (Gelenberg, 2010; Richards, 2011; World Health Organization, 2017). Individuals who experience depressive episodes suffer greatly, and symptoms can have substantial consequences that impair their ability to meet requirements at work or school or cope with stressful events and everyday life (Kessler, 2003; McKeever et al., 2017).
Even if there is a perceived normalization of mental health problems from the public perspective (Schomerus et al., 2023), surveys still reveal the existence of remarkably stigmatizing attitudes and stereotypical perceptions (Angermeyer and Dietrich, 2006). Stigmatization implies that socially shared negative stereotypes—that is, devaluing attributes, undesirable characteristics, and negative evaluations—are attributed to individuals, thereby discrediting, labeling, and marking them as different, ultimately leading to social exclusion (Link and Phelan, 2001). Thus, stigmatization is an additional heavy burden for those affected and their relatives, complicating as well as impeding the seeking and obtaining of help; it is a significant barrier to early diagnosis and treatment (Major and O'Brien, 2005; Sickel et al., 2014, 2019).
Studies on attitudes toward individuals with depression have primarily examined specific attitudinal aspects, thereby neglecting the broader perspective and failing to address the complexity of individuals' worldviews. The concept of cognitive framing allows us to cover the complexity of human perceptions. Cognitive frames help us better understand how individuals make sense of the world as a set of deep, implicit, and socially shared pictures in their heads (Lindland and Kendall-Taylor, 2012). From a framing perspective (Goffman, 1974; Entman, 1993), we claim to understand the public perception of depression in terms of socially shared, complex patterns of interpretation; as a bundle of cognitive units forming a network of associations.
Previous research indicates that connecting with affected persons (Couture and Penn, 2003) as well as interest in mental health information (Romer and Bock, 2008; Schomerus et al., 2016) might play a crucial role in mental health communication efforts and anti-stigma campaign effects. Both aspects refer to an individual's receptivity and openness in dealing with mental health-related issues and have been shown to depend upon an individual's existing beliefs (Fransen et al., 2015). Therefore, it is crucial to better understand individuals' cognitive frames of mental disorders and their communicative accessibility to the topic.
2 Background
2.1 Public perception of depression
Studies show a distorted public perception, stereotypical ideas, and stigmatizing attitudes toward individuals experiencing depression (Angermeyer and Dietrich, 2006; Wood et al., 2014). Depression is often viewed as controllable and self-inflicted and is associated with low levels of sympathy and helpfulness (Muschetto and Siegel, 2019). Overall, depression is thought to be caused by acute personal stress, social, marital, or family problems, genes, or brain disease (e.g., Dietrich et al., 2004; Ozmen et al., 2004; Blumner and Marcus, 2009; Schomerus et al., 2014; Lersner et al., 2019), lack of self-control (Hegerl et al., 2003), or an individual's poor or weak character (Jorm et al., 1997; Ozmen et al., 2004; Yokoya et al., 2018). With regard to solutions for depression, many people agree that depression can be treated by a professional and endorse seeing a general physician, a psychiatrist, or a psychotherapist as suitable treatment options (Hegerl et al., 2003; Blumner and Marcus, 2009; Angermeyer et al., 2013a). Yet, the responsibility for adequately dealing with depression is attributed primarily to the affected individuals (Angermeyer and Dietrich, 2006; Wood et al., 2014).
Over the past few decades, attitudes toward individuals living with depression and the anticipated causes of depression have partly changed (Blumner and Marcus, 2009; Pescosolido et al., 2010; Angermeyer et al., 2013a, 2014). While Angermeyer et al. (2013a) investigated an increase in the endorsement of work-related stress as a perceived cause of depression in Germany, a shift toward a biological framework was observed in the U.S., with public beliefs in biological and genetic causes of depression increasing by 10% at the turn of the millennium (Blumner and Marcus, 2009; Pescosolido et al., 2010). The proportion of respondents who endorsed seeking help for depression from a spiritual healer doubled between 1996 and 2006 (Blumner and Marcus, 2009), possibly reflecting how depression is still not taken seriously by a large majority. In line with this, antidepressants continue to be viewed critically and negatively by most people (Hegerl et al., 2003). However, talking to friends or family is still recommended by most people in the U.S. (Blumner and Marcus, 2009). Despite numerous anti-stigma campaigns, individuals experiencing depression are still perceived as dangerous, unpredictable, or weak by a considerable proportion of the population in several countries around the world (Ozmen et al., 2004; Kermode et al., 2009; Peluso and Blay, 2009; Pescosolido et al., 2010; Jorm et al., 2012; Wood et al., 2014; Yang et al., 2020).
In most prior studies, perceptions of causes, solutions, consequences, or affected individuals' characteristics have been assessed and analyzed in an isolated manner. Only a few studies have investigated associations among multiple attitudinal dimensions in bivariate analyses. For example, Phelan et al. (2006) and Lebowitz et al. (2013) found that among both individuals with depressive symptoms and the public, biochemical and genetic attributions for depression are associated with pessimistic prognoses about the course of the disease. In other words, there exist beliefs that depression is a relatively permanent, difficult-to-cure, or difficult-to-treat disorder. In addition to these results, Pescosolido et al. (2010) showed that a neurobiological conception of depression increased the likelihood of support for treatment, but, at the same time, was associated with a higher perception of affected persons as dangerous. Similar findings were obtained by Ozmen et al. (2004), who found that the belief that depression is an illness was associated with both higher perceptions of aggression and higher levels of social distance. Finally, in a study by Schomerus et al. (2013), continuum beliefs were associated with more positive emotional reactions and less desire for social distance from people with depression.
This brief synopsis clearly shows that the problem of stigmatization in general and depression in particular is widely known and has been substantiated in many studies (e.g., Corrigan et al., 2003; Corrigan, 2005, 2014; Angermeyer et al., 2013b; Michaels et al., 2017; Yang et al., 2020). Besides the salience of attributing undesirable characteristics—negative stereotypes (Link and Phelan, 2001)—to people with depression, research has also shown the salience of negative emotional reactions such as anger, irritation, anxiety, pity, or fear, toward people with depression (Peluso and Blay, 2009; Angermeyer et al., 2010) and discussed intergroup emotions as a component (Link et al., 2004), or at least closely related phenomenon of stigmatization processes (Andersen et al., 2022). Against this background, it seems necessary to reflect on emotional reactions toward individuals experiencing depression while examining the stigmatizing potential of individuals' perceptions of depression.
2.2 Cognitive framing approach
From a cognitive framing perspective (Goffman, 1974; Entman, 1993), individuals' general notions and perceptions of (mental) illnesses, and depression in particular, should be reflected as complex cognitive patterns. These ‘pictures in our minds' are referred to as cognitive frames or mental models. They represent bundles of cognitive units of knowledge, attitudes, and thoughts about specific actions, incidents, situations, and objects. These bundles are based on networks of associations that individuals develop and acquire during socialization.
Cognitive frames are socially shared and shaped by both the social environment and cultural factors (Goffman, 1981; van Gorp, 2007). They emerge as individuals experience their environment, recognizing both variance and constancy across events and processes. By abstracting the similarities in these experiences, cognitive frames become more general and more complex. Thus, cognitive frames can be rooted in individuals' own positive or negative experiences, which become increasingly abstract with repetition over time (Johnston, 1996). However, they can also be adapted through observations and vicarious experiences of others; thus, they are also acquired and shaped through social interactions and media use (Wicks, 2005; Ma, 2017).
Sets of deep, implicit, and socially shared cognitive frames constitute idiosyncratic associations creating mental maps of the physical and social worlds and guiding individuals' perceptions and interpretations of the world around them (Shore, 1996; Lindland and Kendall-Taylor, 2012). They enable people “to locate, perceive, identify, and label” occurrences within their life space and the world at large (Goffman, 1974, p. 21) and allow for placing information in context and making sense of events (Wicks, 2005). Thus, cognitive frames help individuals classify and process information, simplify and condense complex issues, and give meaning to events or occurrences. Thereby, they provide a means of organizing experiences and guiding actions (Benford and Snow, 2000). This mechanism of complexity reduction is also inherent in the process of stigmatization (Link and Phelan, 2001). Well-established elements of frames can be derived from the tradition of framing research (Goffman, 1974; Entman, 1993). Entman (1993), for instance, defines framing as a selection of and emphasis upon certain aspects of perceived reality, promoting a particular problem definition, causal interpretation, moral evaluation, or treatment recommendation. In this vein, frames constitute principles of selection, emphasis, and presentation, composed of little tacit theories about “what exists, what happens, and what matters” (Gitlin, 2003, p. 6).
The various facets of the public perception of depression studied so far (for example, causes and solutions, see above) relate well to the elements of (cognitive) frames as defined by Entman (1993). In the context of mental disorders and from the perspective of stigma research, the attribution of (negative) characteristics to individuals experiencing depression and emotional reactions to them also appear to be particularly relevant considerations for exploring cognitive frames of depression. However, studies on attitudes toward people with depression have so far primarily looked at singular cognitive and affective aspects (e.g., Link et al., 1999; Ozmen et al., 2004; Angermeyer and Dietrich, 2006; Pescosolido et al., 2010; Angermeyer et al., 2013b; Schomerus et al., 2013; Speerforck et al., 2014, 2017; Muschetto and Siegel, 2019). To the best of our knowledge, more complex, multidimensional analyses of the interrelationships between various cognitive and affective facets of the public's perception of depression do not yet exist. Such analyses would help identify and understand varied perceptions of depression in the public as complex cognitive frames, and thereby provide an even better basis for targeting strategies in anti-stigma communication. Therefore, our first research question was:
What are the various cognitive frames of depression that exist among the German population? (RQ 1). Further, to reflect upon the importance of intergroup emotions in the stigmatization of people with mental disorders (Neuberg and Cottrell, 2002; Mackie et al., 2008), we outlined the second research question: How are varied cognitive frames of depression related to individuals' affective reactions toward victims of depression? (RQ 2).
2.3 Communicative accessibility
Being receptive to information regarding mental health-related issues, or actively seeking knowledge about the subject is known to impede stigmatizing attitudes and encourage help-seeking (Griffiths et al., 2008; Romer and Bock, 2008; Lannin et al., 2016; Schomerus et al., 2016). In both the U.S. and Germany, approximately a quarter of adults have already sought information on mental health, often not just for themselves but also for others (Fox and Jones, 2009; Freytag et al., 2023). Initial findings suggest that individuals' proximity to mental health issues, including interactions with individuals affected by a mental disorder or personal experiences with mental health treatment, as well as their educational background and their inclination toward maintaining social distance from affected individuals, are closely linked to mental health information-seeking (Freytag et al., 2023).
The acquisition of mental health information, the perpetuation of mental health stigma, and help-seeking are known to be interrelated (Corrigan, 2014; Clement et al., 2015). Further, empirical evidence has demonstrated that contact with individuals experiencing a mental illness and discussions about the topic can have destigmatizing effects (Couture and Penn, 2003). Both aspects—the interest in or motivation to engage with information about depression and one's social proximity to the issue—underscore the necessity of identifying and gaining a more in-depth understanding of the complex cognitive frames of mental disorders and their stigmatizing aspects. They also foreground the need to consider the communicative accessibility of diverse subpopulations. This represents a significant challenge in the realm of anti-stigma communication (Fransen et al., 2015). Identifying and reflecting upon associations between more or less stigmatizing cognitive frames and individuals' openness to the issue can help guide appropriate communicative ‘pathways' when targeting individuals in anti-stigma communication initiatives. Hence, this study aimed to explore the following questions: To what extent do individuals with varying cognitive frames of depression differ in terms of their social proximity to those affected by depression? (RQ 3a) How do various cognitive frames of depression relate to individuals' information-seeking motivation and their openness to mental health information? (RQ 3b).
3 Materials and methods
3.1 Procedure and sample
A representative, face-to-face population survey was conducted among 3,042 German citizens aged 18 and above, in 2020. The sample was drawn using a random sampling procedure comprising three stages: (1) sample points (electoral wards), (2) households, and (3) individuals within the target households. Target households within the sample points were determined according to the random route procedure; a street was selected randomly as a starting point, from which the interviewer followed a set route through the area. Target individuals within households were selected using random digits. Informed consent was considered to have been given when individuals agreed to complete the interview. The fieldwork was carried out by USUMA (Berlin, Germany), an established market and social research company. All interviews were fully structured, face-to-face, and conducted by interviewers using a paper-and-pencil method. Due to the COVID-19 pandemic, participants had the option to fill out the survey themselves; this option was utilized by 15% of the participants.
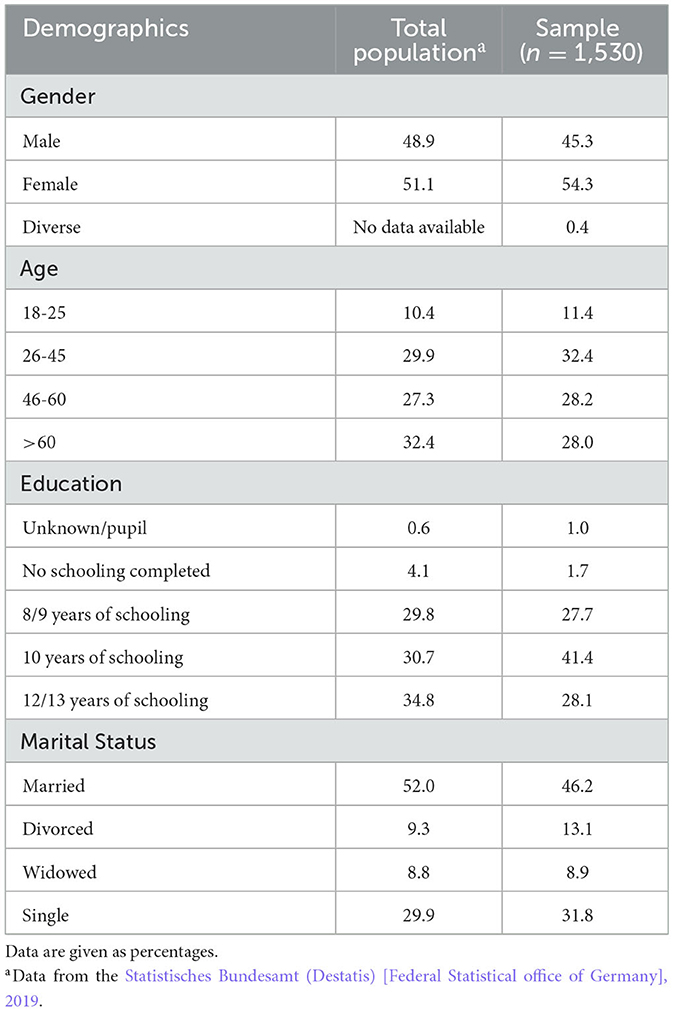
At the beginning of the interview, an unlabeled case vignette of a person experiencing schizophrenia or major depression was presented. The wording of the vignette for depression can be found in the online supplement. Vignettes provide a way to present a mental disorder without using diagnostic terms. They have a long tradition in psychiatric attitude research (e.g., Link et al., 1987) and provide a standardized representation of the various facets of the disorder in large samples. The gender of the person described in the vignette varied randomly. Identical vignettes were used in previous surveys; they had been constructed to match diagnostic criteria for the disorder and had undergone blind validation by experts in psychopathology (Angermeyer and Matschinger, 1997). Half of the total sample (n = 1,530) was confronted with the major depression vignette; it was therefore considered for the following analyses. Table 1 shows the sociodemographic characteristics of our subsample in comparison to the general population.
3.2 Measures
3.2.1 Causal beliefs
As one major component of the conceptualization of a frame, we assessed the respondents' beliefs about the possible causes of the problem described in the major depression vignette using a list of 18 possible causes, each of which had to be rated on a five-point Likert scale anchored with 1 “certainly a cause” and 5 “certainly, not a cause.” Causes were adopted from Schomerus et al. (2014) and enriched based on a qualitative pre-study. Answers to these items were entered into an explorative factor analysis (EFA, principal axis factoring), yielding four factors with an eigenvalue >1. Varimax rotation resulted in four uncorrelated factors. Items loading primarily on the first factor (eigenvalue 3.12) described ‘negative emotions' as causes for the situation in the vignette, for example, stressful life events, conflicts with one's environment, or loneliness. Items loading on the second factor (eigenvalue 2.66) could be grouped under the umbrella term ‘childhood adversities' (for example, childhood sexual abuse). The third factor (eigenvalue 2.02) comprised items describing ‘biogenetic causes', for instance, a brain disease, while ‘lifestyle'-related causes (for example, unhealthy lifestyle) were loading on factor four (eigenvalue 1.15). The four factors accounted for a cumulative variance of 53%. We reversed the rotated factor scores for our analyses, with higher scores indicating higher agreement with the appropriate causes. This yielded z-transformed scores for each factor (mean = 0, standard deviation = 1). An overview of the EFA's results for causal beliefs can be found in Supplementary Table A1.
3.2.2 Proposed solutions
According to frame element ‘treatment recommendations', respondents' suggested solutions to the problem described in the depression vignette were solicited with a list of 21 possible treatments or possible ways to solve the problem. Treatment preferences were adopted from Riedel-Heller et al. (2005) and Speerforck et al. (2017) and were enriched by further items based on a qualitative pre-study. Each solution had to be rated on a five-point Likert scale anchored at 1 “would strongly recommend” and 5 “would strongly advise against.” There was also an option to tick “do not know,” with these responses replaced with the scale mean before further analysis. As for the causal beliefs, answers to the 21 items were entered into an EFA (principal axis factoring). The analysis yielded five uncorrelated factors with an eigenvalue >1.
Items loading on the first factor (eigenvalue 2.68) comprised solutions in the ‘mental health care system' (for example, availing psychotherapy), while items loading primarily on the second factor (eigenvalue 2.46) described ‘alternative medicine', for instance, acupuncture, as a recommendable solution. The third factor (eigenvalue 1.78) encompassed solutions entitled ‘help for self-help' (for example, self-help groups, and advice from friends). Items that described ‘institutions outside the mental health care system', for instance, the church, as a possible solution, were loading on factor four (eigenvalue 1.33), whereas ‘online services' via the Internet or apps represented the fifth factor (eigenvalue 1.23). The five factors accounted for a cumulative variance of 47%. We reversed the rotated factor scores for our analyses, with higher scores indicating higher agreement with the proposed solutions. As for the causal beliefs, this procedure yielded z-transformed scores for each factor. An overview of the EFA's results or proposed solutions can be found in Supplementary Table A2.
3.2.3 Prognosis—anticipated consequences
Within the causal logic of a (cognitive) frame, anticipated consequences of the problem should be coherently linked to the causal interpretations and the solutions suggested; they should contribute to a holistic perspective of the problem in focus. Anticipated consequences were measured using a list of nine items adapted from Angermeyer and Matschinger (2003) and a five-point Likert scale anchored at 1 “totally agree” and 5 “do not agree at all.” Another EFA (principal axis factoring) produced two uncorrelated factors with an eigenvalue >1. Factor one could be termed ‘negative life trend' (eigenvalue 3.29), with items such as “the person will never recover from that” loading on that factor. The second factor (eigenvalue 1.80), in contrast, gathered all items suggesting that the person with the described problems poses a “risk to the self and social environment.” These two factors explained 57% of the total variance. As before, we reversed the rotated factor scores, with higher scores indicating higher agreement with the consequences, and continued our analyses with z-transformed scores for each factor. An overview of the EFA's results for anticipated consequences can be found in Supplementary Table A3.
3.2.4 Ascribed characteristics
According to the stigma concept, which covers the attribution of negatively stereotyping characteristics to the group (Link and Phelan, 2001; Amodio, 2014; Andersen et al., 2022), we evaluated the respondents' ascription of potential character traits to the person described in the depression vignette. This also corresponded to the frame element “moral evaluations” of the problem, or, in our case, the person showing problematic behavioral symptoms. We used 11 different adjectives adapted from Angermeyer and Matschinger (2003) and a five-point Likert scale anchored at 1 “totally agree” and 5 “do not agree at all.” An EFA (applying principal axis factoring) revealed two factors, of which the first could be described as the perception of the described person as “dangerous” (eigenvalue 2.87) and the second one as “weak” (eigenvalue 1.84). Both factors accounted for 59% of the total variance. Again, we reversed the rotated factor scores, with higher scores indicating higher agreement with the character traits, and saved z-transformed scores for each factor. An overview of this EFA's results can be found in Supplementary Table A4.
3.2.5 Attribution of guilt
The attribution of responsibility, specifically, guilt, was measured with one item based on Angermeyer et al. (2016): “The person is himself/herself to blame for getting his/her condition” on a five-point Likert scale anchored at 1 “totally agree” and 5 “don't agree at all” (M = 3.93, SD = 1.12). This item was included because the attribution of responsibility is fundamental in the context of mental health stigma theory and research. It also contributes to a conceptual enrichment in covering a cognitive frame, by linking causal attributions and negative moral evaluations (Entman, 1993). For unification, the item was reversed and z-transformed as well, before using it in further analyses.
3.2.6 Emotional reactions and sociodemographics
As explained above, the reflection upon emotional reactions toward individuals experiencing depression supplements the patterns of beliefs as covered by the cognitive framing elements. It further adds to a more profound understanding of the potentially stigmatizing cognitive frames. So, we included the emotional reactions to the person described in the depression vignette as well as sociodemographic data of the respondents (sex, age, education level, marital status) in our analyses, to characterize various types of cognitive frames further. The emotional reactions to the vignette were assessed based on an item list used by Schomerus et al. (2013). As in the original study, we confronted respondents with a scale consisting of 10 items describing possible emotional reactions, asking them to indicate how they would react to the person described in the vignette. Answers were given on a five-point Likert-scales anchored at 1 “applies completely” and 5 “does not apply at all.” An exploratory principal-axis analysis revealed three factors, accounting for a cumulative variance of 55%. Reproducing the results from Schomerus et al. (2013), the first factor was termed “fear”, the second “anger”, and the third “prosocial reactions”. Scores were reversed for our analyses, with higher scores indicating stronger emotional reactions. An overview of this EFA's results can be found in Supplementary Table A5.
3.2.7 Social proximity
To operationalize the concept of social proximity to individuals living with mental health disorders, our survey instrument included a series of structured questions. These questions assessed participants' closeness to individuals with mental health concerns along several dimensions. First, we inquired about participants' personal experiences with mental health care, specifically whether they had sought treatment for their own mental health problems, whether on an outpatient basis with a family physician, psychiatrist, psychotherapist, or counseling center, or on an inpatient basis in a clinic (21% of the total sample). Second, we examined the participants' closeness within their close social networks. We asked whether anyone close to them, such as family members or close friends, had received outpatient treatment from mental health professionals or had been admitted to a psychiatric or psychosomatic hospital for inpatient care (29.4% of the total sample). Finally, we examined participants' professional or personal contact with people affected by mental disorders. This included roles such as healthcare professionals, carers, or volunteers in the mental health field (7% of the total sample).
3.2.8 Openness to mental health information
The participants' motivation toward dealing with the issue of depression and acquiring mental health information was assessed via six items developed by Howell and Shepperd (2016), for example, “Even if it will upset me, I want to know anything about mental health and illnesses”. Answers were given on five-point Likert-scales anchored at 1 “applies completely” and 5 “does not apply at all.” Three out of six items were reversed before integrating the items into a mean index, with higher scores indicating more openness, that is, more motivation to obtain mental health information (α = 0.86, M = 2.85, SD = 0.94). Please see Supplementary Table A6 for all items.
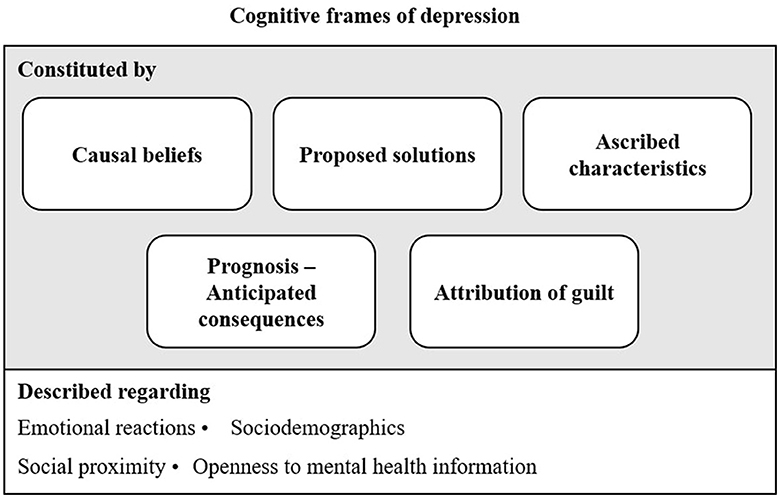
Figure 1 provides an overview of the main dimensions considered in our analyses, either as constituents of the cognitive frames or as relevant descriptive characteristics of the frames.
3.3 Statistical procedure
To answer the research questions and to detect various cognitive frames of depression in the German population, we performed a cluster analysis. Cluster analyses are used to identify patterns in the data and form groups by minimizing within-group variability and maximizing between-group variability (Hair and Black, 2010). It is a commonly used statistical method to investigate media and cognitive frames (David et al., 2011; Stamovlasis et al., 2020).
Using IBM's SPSS Statistics 29 and following recommendations by Hair and Black (2010), we employed a two-step cluster analysis to classify participants based on their varied mental conceptions of depression. The participants' causal beliefs, proposed solutions, and anticipated consequences ascribed characteristics to the person described in the vignette, and their attributions of guilt were entered as the clustering variables. As a first step, we used Ward's linkage to minimize the sum-of-square differences within groups (Ward, 1963). We applied squared Euclidean distance to measure the distance between the individual observations on the clustering variables. To select an optimal number of clusters, we performed a visual analysis of a dendrogram representing the data structure. We investigated the increase in the percentage variance, explained as a function of the number of clusters (“elbow criterion”). A 3- or 4-cluster solution emerged as most suitable at this point.
As a second step, the cluster means (centroids) from the hierarchical 3- and 4-cluster solutions were separately submitted to a non-hierarchical, k-means cluster analysis to refine the initial cluster solution and reduce the risk of cluster misassignment; this is common in hierarchical cluster methods (Blashfield and Aldenderfer, 1988). We found the optimal cluster solution to be comprised of four groups, as it generated the most distinct, meaningful, and coherent interpretation of the groups. To compare group characteristics among clusters, we performed analyses of variance and chi-square testing.
4 Results
4.1 Cognitive frames of depression
We found significant between-group differences for all clustering variables among the four groups (F [14.1430] = 118.722; p ≤ 0.001). The groups accounted for 61% of the variables' between-group-variance. In the following paragraphs, the groups are described in more detail with regard to their most concise properties. An overview of the deviation of the group properties from the overall average can also be found in Table 2.

Table 2. Causal beliefs, proposed solutions, anticipated consequences, ascribed character traits and attribution of guilt by group.
4.1.1 Cognitive frame 1: medical-psychological perspective
The largest cluster (n = 533; 37% of the sample) was characterized by a very rational and relatively low stigmatizing perspective. As can be seen in Table 2, the causes for the problem described in the vignette were considered to be adversities in childhood (0.49) or biogenetic causes (0.29) with above-average frequency, and the lifestyle of the affected person with below-average frequency (-0.14). The mental health system was seen as the main solution (0.56), whereas alternative solutions (-0.18) or online services (-0.19) were recommended significantly less often compared to the other groups. The group assigned below-average responsibility to the person affected (-0.60) and considered them not to be weak (-0.50). Based on these group specifics, we have labeled them as having a “medical-psychological perspective”.
4.1.2 Cognitive frame 2: de-dramatizing alternative perspective
Respondents in the second-largest cluster (n = 405; 28% of the sample) showed the most favorable view of the person described in the vignette. They agreed with negative emotions as a cause slightly above average (0.14); other causes were not attributed as much. Alternative solutions (0.29) and help for self-help (0.12) were most strongly recommended as solutions by this group. Potential negative consequences, as well as negative character traits and the accusation of self-infliction, were rejected significantly more strongly compared to the other groups. As a result of this positive, partly disparaging, small-talking perspective, we have labeled this group as having a “de-dramatizing alternative perspective”.
4.1.3 Cognitive frame 3: pessimistic perspective of guilt and danger
The third group (n = 396; 27% of the sample) differed considerably from the first two. Individuals with this cognitive frame agreed with all causes above average; that is, they saw several possible triggers for the situation described in the vignette. In group-wise comparison, they agreed most strongly with biogenetic causes (0.40). With regard to possible solutions, this perspective was characterized by an above-average recommendation of institutions, such as the church, the emergency doctor, or the health department as possible solutions (0.51). Online services were also recommended as being above average (0.30). This group was, vis-à-vis group-wise comparison, most remarkably characterized by their strong agreement with an unfavorable life prognosis for those affected (0.82) and the assumption that these individuals are both dangerous (0.80) and weak (0.78). Similarly, their agreement with the statement that it is the described individual's fault (0.67) was stronger than in groups 1 and 2. On account of this pessimistic perspective, we have named members of this group as ones with a “pessimistic perspective of guilt and danger”.
4.1.4 Cognitive frame 4: superficial guilt perspective
Members of the smallest cluster (n = 113; 8% of the sample) reported the most dismissive attitudes. They offered a below-average agreement to all the causes presented, as if, for them, there seemed to be no real cause for the problem described in the vignette. Likewise, they saw the proposed solutions as being below average in recommendation; in particular, the mental health care system did not seem to be an adequate solution for this group (-1.70). They agreed less with the negative consequences compared to the other groups (-0.38 and−0.29), and among all groups, they saw those affected as being the least dangerous (-0.95). On the other hand, they agreed most strongly that individuals as described in the vignette were weak (0.92) and that they were to be blamed for the condition described (1.75). Across the variables, the impression emerges that this group did not take the situation described in the vignette seriously and blamed the affected individuals. We have therefore labeled this perspective as a “superficial guilt perspective”.
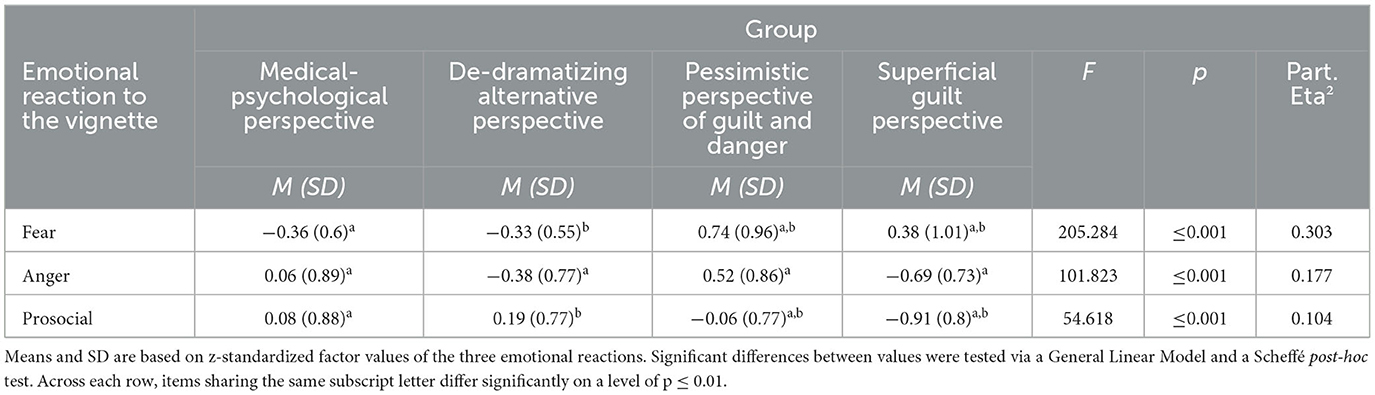
4.2 Comparison of emotional reactions toward the vignette among groups
We compared the emotional reactions toward the person described in the vignette among the identified groups to answer RQ 2. As can be seen in Table 3, respondents with a de-dramatizing alternative perspective showed the most prosocial emotions (M = 0.19, SD = 0.77), whereas anger (M = −0.38 SD = 0.77) and fear (M = −0.33, SD = 0.55) were clearly below average. Among respondents with a medical-psychological perspective, prosocial emotions were found to be at an average level (M = 0.08, SD = 0.88), as was their anger (M = 0.06, SD = 0.89). However, their fear was the lowest among the four groups (M = −0.36, SD = 0.60). People taking a superficial guilt perspective with regard to depression showed above-average degrees of fear (M = 0.38, SD = 1.01), accompanied by below-average prosocial emotions (M = −0.91, SD = 0.80), and interestingly, the lowest degree of anger (M = −0.69, SD = 0.73). Remarkably, individuals with a pessimistic perspective of guilt and danger showed most anger (M = 0.52, SD = 0.86) and most fear (M = 0.74, SD = 0.96), but still exhibited an average degree of prosocial emotions toward the person described in the vignette (M = −0.06, SD = 0.77).
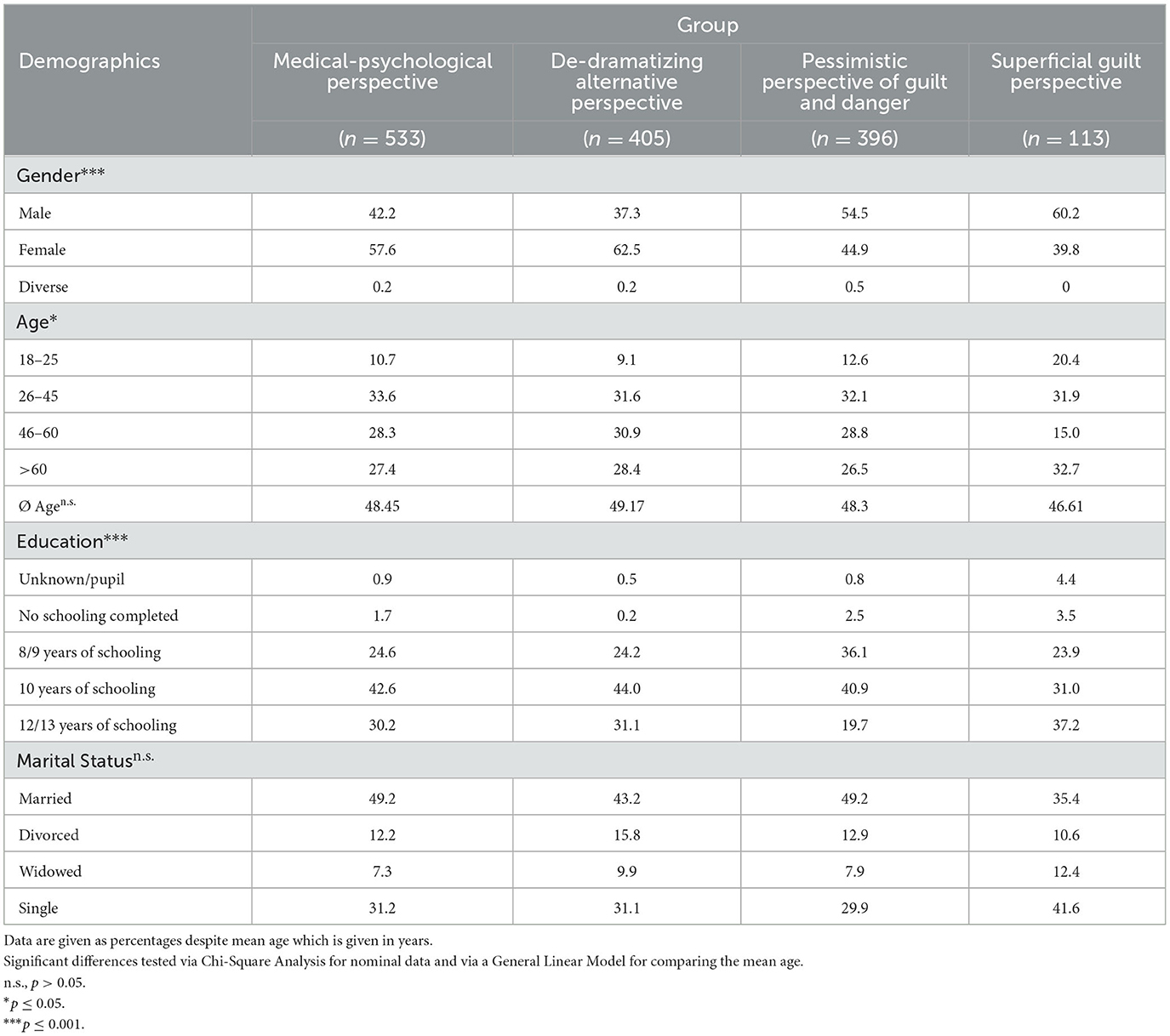
4.3 Comparison of sociodemographic characteristics among the groups
The groups differed significantly, but only slightly, in terms of gender, age, and education. As can be seen in Table 4, the group with a medical-psychological perspective was slightly better educated, and a slightly larger proportion of the group was female. The age groups were distributed similarly across the overall population. In comparison, individuals with a de-dramatizing alternative perspective on depression were mostly women (62.5%). On average, they tended to be older than the other groups and somewhat better educated. The most striking characteristic of respondents showing a pessimistic perspective of guilt and danger was that they had mostly attended only 8/9 years or 10 years of schooling, thus being the less educated group. Otherwise, their characteristics did not differ particularly from those of the overall sample and the population, so they represented a group of typical Germans in terms of sociodemographic characteristics. In contrast, the group with a superficial guilt perspective was 60% male. Besides, they were the youngest group, with a high proportion being in the age group of 18–25 years. This group was also characterized by the highest proportion of highly educated respondents. In summary, they were mostly young men with high levels of education.
4.4 Comparison of openness to mental health information among the groups
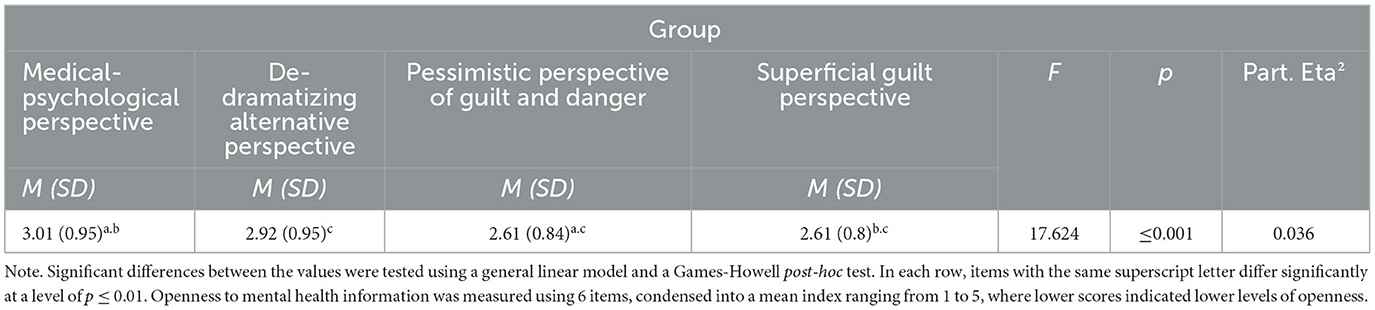
To answer RQ 3a, we compared the identified groups' motivation toward obtaining mental health information. Among the four groups, respondents with a pessimistic perspective of guilt and danger (M = 2.61, SD = 0.84) or with a superficial guilt perspective (M = 2.61, SD = 0.80) showed less information-related motivation, implying that they also reported the highest tendency to avoid information about mental health and illness (see Table 5). These two groups differed significantly with regard to their mental health information motivation in comparison to the other two groups. People with a medical-psychological perspective showed the greatest openness to mental health information (M = 3.01, SD = 0.95), closely followed by people with a de-dramatizing alternative perspective (M = 2.92, SD = 0.95).
4.5 Comparison of social proximity among the groups
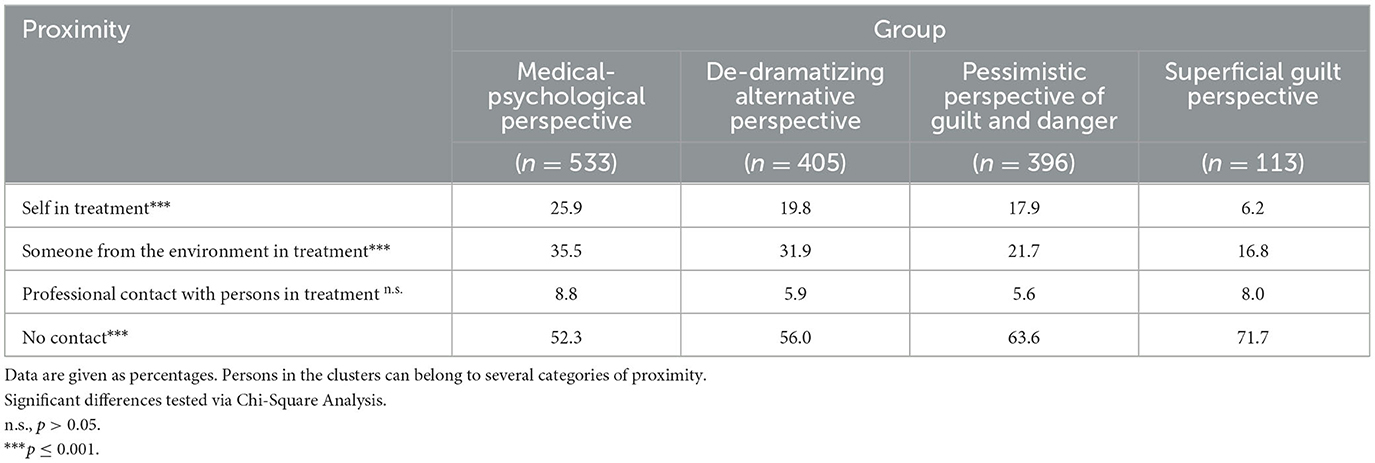
Finally, the groups also differed significantly regarding their personal proximity to those affected by a mental illness, that is, regarding the proportion of individuals undergoing psychological treatment themselves, and the proportion of people in the social environment undergoing psychological treatment. As can be seen in Table 6, the group with a medical-psychological perspective had in group-wise comparison the highest shares of individuals with personal proximity: More than a quarter of the individuals in this group had been or were undergoing any psychological or psychiatric treatment themselves (25.9%) and 35.5% knew someone in their personal surrounding undergoing treatment. Among group members with a de-dramatizing alternative perspective, a good one-third knew someone in their environment who was undergoing psychological treatment (31.9%), and almost 20% had received or were receiving treatment themselves. In contrast, those with a pessimistic perspective of guilt and danger had less personal contact with those affected by a mental illness; only 17.9% had been undergoing any psychological or psychiatric treatment themselves, and 21.7% knew someone in treatment. The lowest personal proximity was associated with those having a superficial guilt perspective: only 6.2% had been or were undergoing any psychological treatment themselves, and the proportion of those with someone in their surroundings undergoing treatment was comparatively the lowest among all clusters (16.8%). With regard to the proportion of people with professional contact to affected individuals, the groups, however, did not differ significantly.
5 Discussion
This study aimed to explore individuals' perceptions of depression and the complex cognitive patterns they have developed and employed to understand their social environments, cope with problems, or distinguish themselves from those who might seem different, or “abnormal,” or even frightening to them. Such cognitive frames help them simplify and condense complex issues and guide information acquisition and processing (Benford and Snow, 2000). In doing so, we particularly aimed to identify and describe facets pointing to the stigmatizing potential of various perceptions of depression (Griffiths et al., 2008).
Our exploratory analysis revealed the existence of four distinct cognitive frames among the German adult population, each characterized by distinctive yet coherent patterns of causal interpretations and beliefs in solutions when confronted with the description of a person showing symptoms of major depression. These patterns—the cognitive frames—prove that there is a diversity in how individuals think and feel about individuals experiencing depression. The results further highlight that these perspectives vary in their stigmatizing potential, including attributions of negative characteristics and responsibility and varied emotional reactions toward those affected. Revealing clear interrelations between cognitive frames on the one hand and communicative accessibility on the other, this analysis provides initial evidence for the value of a more holistic view. Therefore, a multidimensional approach to mental health stigma communication is suggested instead of looking at single attributions, as has been researched so far. It is the idea of a coherent causal cognitive structure that, together with attributions and evaluations, provides a mental framework guiding social interaction, observation, and interpretation of others (Goffman, 1974; Entman, 1993; Benford and Snow, 2000). It can act as a breeding ground as well as a protective wall against stigmatization and calls for tailored, stigma-sensitive communication strategies that also reflect individuals' information motivation and proximity to the topic.
Individuals with a medical-psychological perspective—representing the largest group—exhibited a rather factual-distant, rational, and less stigmatizing view of depression, emphasizing both childhood adversities and biogenetic causes as the main contributors—two factors that are also considered by current psychiatric research to be important causes of depression (Schotte et al., 2006). Individuals with this cognitive frame tend to omit the social facets of depression slightly. They viewed the mental health system as a viable solution, which, unsurprisingly, is accompanied by the fact that a larger proportion of this group has already had experience with the mental health system themselves or has someone in their environment undergoing professional treatment. It can be expected that these people are able and willing to process factual, more complex mental health information to further deepen their knowledge and understanding. To foster a more balanced perspective based upon the biopsychosocial model of (mental) health (Suls and Rothman, 2004), the social determinants and responsibilities as supportive opportunities supplementary to professional healthcare could be emphasized.
Conversely, those with a pessimistic perspective of guilt and danger demonstrated a more pessimistic view, attributing depression to multiple causes and harboring a strong belief in the threat from and weakness of those affected. The high levels of anger and guilt that those with this perspective reported toward the person in the vignette demonstrate the high levels of threat they perceive from those with depressive symptoms (Neuberg and Cottrell, 2002). These findings highlight the importance of addressing such individuals very carefully in mental health communication efforts. Fear appeals would be counterproductive here because the likelihood of reactivating only adverse emotions and attitudes without processing the actual message and the risk of triggering reactance and undesired effects is relatively high among this group (Witte and Allen, 2000). However, this might not be easy, as this group is seen to be less receptive to mental health information, and may require specialized approaches to reduce stigma. The goal would be to reduce fear, explain and illustrate the continuum character of depression (Schomerus et al., 2016; Corrigan et al., 2017), and establish proximity to people affected, for instance, by narrating stories of recovery that depict sympathetic individuals sharing insights into their feelings and thoughts during the disease (Corrigan et al., 2013). Perhaps social media influencers or celebrities might also help to bridge the gap (Eaton, 2009; Betton et al., 2015; Sampogna et al., 2017; Gronholm and Thornicroft, 2022).
Those with a de-dramatizing alternative perspective, at first glance, held a favorable view, rejecting negative character traits and self-infliction. Their relatively high prosocial dispositions and openness to the topic suggest that they are easier to reach as a target group and could also be mobilized as advocates in anti-stigma initiatives. On closer inspection, however, this group is also found to be problematic because they do not seem to consider the described symptoms as a serious illness deserving professional treatment. Therefore, this group should be addressed with stigma-sensitive but more pronounced risk-and-danger messages to raise awareness about the prevalence and severity of the disease.
Finally, the group with a superficial guilt perspective exhibited a dismissive attitude, showing the least agreement with any causes or solutions presented. They placed a higher degree of blame on affected individuals and were less likely to take the situation seriously, making them a relevant but challenging target for stigma reduction efforts, especially due to their low levels of openness to mental health information. In any case, the communication approach should have a very low threshold in its content and message design. Establishing proximity by occasionally getting in touch with individuals living with depression and having positive experiences might offer the biggest chance to make a difference and change attitudes. Influencer communication (via preferred influencers of these people) or entertainment education approaches could also be tested to offer a possible pathway (Ritterfeld and Jin, 2006; Chan et al., 2009).
Sociodemographic information often serves as a set of criteria for target group segmentation and a media planning resource for the targeted dissemination of (health) campaign messages to specific audiences (Schultz and Block, 2018). While we did observe some sociodemographic differences among individuals with distinct cognitive frames of depression, these distinctions remained relatively modest and did not always align with common assumptions. Notably, age appears to play no role in adopting particular cognitive frames, and gender only marginally distinguishes among groups with varied cognitive perspectives. There is merely a slight tendency for men to constitute a larger portion of groups with more stigmatizing viewpoints, consistent with prior stigma research (Holzinger et al., 2012). The level of education does vary among the identified groups with differing cognitive frames, but does not consistently emerge as an explanatory factor for a distant attitude with a high potential for stigmatization. Both individuals with a medical-psychological perspective and those with a superficial guilt perspective encompass an above-average proportion of highly educated individuals. Consequently, anti-stigma communication should not exclusively target presumably less-educated demographics. In conclusion, sociodemographic characteristics alone appear inadequate as targeting tools in anti-stigma interventions. The limited explanatory power of sociodemographic and socioeconomic characteristics, compared to cognitive and proximity factors, has also been demonstrated in multivariate analyses of determinants of health information seeking in general (Link et al., 2021) and of self- and surrogate seeking of mental health information in particular (Freytag et al., 2023). In line with these prior findings, our study also suggested that conventional socioeconomic target group characteristics would offer only limited utility in effectively addressing individuals with mental health promotion efforts. Thus, they should be seen as complementary and used as a bridge to target group segmentation characteristics alongside auxiliary constructs such as media consumption patterns or political attitudes derived from interfacing with other media and opinion research studies.
As illustrated above in the discussion of the individual cognitive frames, our findings have several implications for stigma-sensitive mental health communication approaches. Of course, the few targeting approaches derived above are by no means exhaustive. They only serve as examples and would need to be worked out in detail and evaluated formatively. Nevertheless, we are convinced that a more holistic approach, as described in our study, is capable of guiding better-targeted, more effective, and stigma-sensitive mental health communication strategies. As the cognitive frames are associated with significant differences in motivation for mental health information and with different levels of closeness to people with a mental disorder, this approach allows for a significant improvement in targeting strategies for mental health promotion and anti-stigma communication. Our findings underline that groups with stigmatizing attitudes are challenging to reach and cannot be addressed by a communicative “shotgun approach”.
As expected, we found that the communicative accessibility and information motivation are lowest among those with a superficial guilt perspective and a pessimistic perspective of guilt and danger; in both groups, reactance to “educational attempts” is to be expected, and there is a risk of even reinforcing existing negative attitudes or creating other unintended effects (Corrigan, 2016; Röhm et al., 2018).
Comparing social proximity among the groups also turned out to be very conclusive and helped to better understand varied perceptions of depression. On one hand, social proximity might result from a specific cognitive frame (that is, “if I perceive people in a depressive mode as aggressive, I will keep my distance and not work with them”). On the other hand, a specific cognitive frame might also result from very little or much contact with those affected. Without encountering people in their environment or having any personal experience of depression, individuals are more likely to draw on media sources or generally existing stereotypes for their image of depression. Research has further found that the more familiar we are with a person and the better we know an individual, the less we apply (negative) stereotypes to the person, even if we assign them to a particular social category, such as individuals with depression (Hugenberg and Sacco, 2008). A lack of this social proximity might finally lead to cognitive frames, such as those found with the pessimistic perspective of guilt and danger and the superficial guilt perspective. These perceptions are particularly shaped by negative emotional reactions toward members of this “outgroup” that one wishes to keep as far away as possible from oneself, which may ultimately be mainly due to insecurities. As mentioned, for these two “problematic groups”, creating social proximity might offer an opening window (for example, everyday interventions that create encounters among those affected and those not affected, or celebrities as advocates and social media influencers to address those with superficial guilt perspectives, or recovery stories for the pessimists).
To summarize, as information processing always depends on the interplay between the characteristics of the message and the characteristics of the recipient (Früh, 1994), an anti-stigma message is not only more likely to be selected if it matches a cognitive frame, but the activated cognitive frame also guides further information processing (Scheufele, 2003). Thus, the likelihood that an anti-stigma message will have the desired effect (that is, be perceived, processed, understood, and accepted) is likely to be higher if the message frame matches the recipients' cognitive frame because the message will then be seen as more plausible and processed more fluently (Meyer et al., 2020; Hoeken et al., 2022). It is, therefore, of utmost importance to consider in an anti-stigma campaign, what the target audience thinks and feels about mental health and illness. In addition, it seems necessary to consider if there are misperceptions that need to be “corrected” (for example, for those with a pessimistic perspective of guilt and danger or a superficial guilt perspective), and which messages might evoke reactions or even activate existing stigmatizing attitudes instead of changing them. However, to achieve this, we need to understand the dominant cognitive frames of the target audiences of our anti-stigma communication efforts.
5.1 Limitations
Our study and its findings must be interpreted within the context of several limitations. Our data was collected in Germany, and cultural differences may influence cognitive frames. Future research should explore the cognitive frames of varied mental disorders across different cultural contexts. Additionally, longitudinal research could provide insights into the stability of cognitive frames over time and the effectiveness of long-term anti-stigma interventions. Further, our study relies on cross-sectional data, which does not allow us to establish causality. While it is reasonable to infer that pre-existing perceptions of depression and specific cognitive frames may predict openness to mental health information, it is equally plausible that avoidance of mental health information could lead to more stigmatizing views of mental disorders such as depression. Therefore, a conclusive causal relationship cannot be established based on our data set, and experimental research or longitudinal designs are needed for further clarification.
Furthermore, we must acknowledge that our data relies on self-reports, and it is important to recognize the potential biases associated with social desirability. Finally, it is noteworthy that our assessment of motivation and openness to mental health information was relatively broad, as we did not ask about specific channels or topics. Participants' responses referred to their openness to information related to both mental health and illness in general. To build upon the findings of this study, future research could take a more nuanced approach and explore variations related to specific channels and topics to better understand the communicative behavior of individuals with varied cognitive frames of depression.
6 Conclusion
The German population has internalized varied cognitive frames for those exhibiting depressive symptoms. Considering these cognitive frames while developing stigma-sensitive mental health communication strategies seems promising. In particular, individuals with a pessimistic perspective of guilt and danger, as well as a superficial guilt perspective are to be regarded as critical. They constitute more than one-third of the respondents and particularly agree with placing the personal responsibility of depression on the affected individuals. Nevertheless, reaching out to such individuals using anti-stigma communication strategies and bringing them into contact with people affected seems challenging, as openness to information about the topic is rather low.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Greifswald University Medical Center (affiliation of project initiator at the beginning of the project, BB 195/18). The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AF: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. EB: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. SS: Data curation, Formal analysis, Methodology, Project administration, Writing – review & editing. MA: Conceptualization, Funding acquisition, Project administration, Writing – review & editing. GS: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Fritz-Thyssen-Foundation, Grant number Az. 10.18.2.009SO.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2023.1308281/full#supplementary-material
References
Amodio, D. M. (2014). The neuroscience of prejudice and stereotyping. Nat. Rev. Neurosci. 15, 670–682. doi: 10.1038/nrn3800
Andersen, M. M., Varga, S., and Folker, A. P. (2022). On the definition of stigma. J. Eval. Clin. Pract. 28, 847–853. doi: 10.1111/jep.13684
Angermeyer, M. C., Carta, M. G., Matschinger, H., Millier, A., Refaï, T., Schomerus, G., et al. (2016). Cultural differences in stigma surrounding schizophrenia: comparison between Central Europe and North Africa. Br. J. Psychiatry J. Ment. Sci. 208, 389–397. doi: 10.1192/bjp.bp.114.154260
Angermeyer, M. C., and Dietrich, S. (2006). Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatrica Scandinavica 113, 163–179. doi: 10.1111/j.1600-0447.2005.00699.x
Angermeyer, M. C., Holzinger, A., and Matschinger, H. (2010). Emotional reactions to people with mental illness. Epidemiol. Psichiatr. Soc. 19, 26–32. doi: 10.1017/S1121189X00001573
Angermeyer, M. C., and Matschinger, H. (1997). Social distance towards the mentally ill: results of representative surveys in the Federal Republic of Germany. Psychol. Med. 27, 131–141. doi: 10.1017/S0033291796004205
Angermeyer, M. C., and Matschinger, H. (2003). Public beliefs about schizophrenia and depression: similarities and differences. Soc. Psychiat. Epidemiol. 38, 526–534. doi: 10.1007/s00127-003-0676-6
Angermeyer, M. C., Matschinger, H., Carta, M. G., and Schomerus, G. (2014). Changes in the perception of mental illness stigma in Germany over the last two decades. Eur. Psychiatry J. Assoc. Eur. Psych. 29, 390–395. doi: 10.1016/j.eurpsy.2013.10.004
Angermeyer, M. C., Matschinger, H., and Schomerus, G. (2013a). Attitudes Towards Psychiatric treatment and people with mental illness: changes over two decades. Br. J. Psych. J. Ment. Sci. 203, 146–151. doi: 10.1192/bjp.bp.112.122978
Angermeyer, M. C., Matschinger, H., and Schomerus, G. (2013b). Public attitudes towards people with depression in times of uncertainty: results from three population surveys in Germany. Soc. Psychiatry Psychiatric Epidemiol. 48, 1513–1518. doi: 10.1007/s00127-012-0618-2
Benford, R. D., and Snow, D. A. (2000). Framing processes and social movements: an overview and assessment. Annu. Rev. Sociol. 26, 611–639. doi: 10.1146/annurev.soc.26.1.611
Betton, V., Borschmann, R., Docherty, M., Coleman, S., Brown, M., and Henderson, C. (2015). The role of social media in reducing stigma and discrimination. Br. J. Psychiatry 206, 443–444. doi: 10.1192/bjp.bp.114.152835
Blashfield, R. K., and Aldenderfer, M. S. (1988). “The methods and problems of cluster analysis” in Handbook of Multivariate Experimental Psychology, ed. J. R. Nesselroade, R. B. Cattell (New York, NY: Springer), 447–73.
Blumner, K. H., and Marcus, S. C. (2009). Changing perceptions of depression: ten-year trends from the general social survey. Psychiatric Serv. 60, 306–312. doi: 10.1176/ps.2009.60.3.306
Chan, J. Y. N., Mak, W. W. S., and Law, L. S. C. (2009). Combining education and video-based contact to reduce stigma of mental illness: the same or not the same anti-stigma program for secondary schools in Hong Kong. Soc. Sci. Med. 68, 1521–1526. doi: 10.1016/j.socscimed.2009.02.016
Clement, S., Schauman, O., Graham, T., Maggioni, F., Evans-Lacko, S., Bezborodovs, N., et al. (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 45, 11–27. doi: 10.1017/S0033291714000129
Corrigan, P. W. (2005). On the Stigma of Mental Illness: Practical Strategies for Research and Social Change. 1st ed. Washington, DC: American Psychological Association.
Corrigan, P. W. (2014). The Stigma of Disease and Disability. Understanding Causes and Overcoming Injustices. Washington, DC: American Psychological Association.
Corrigan, P. W. (2016). Lessons learned from unintended consequences about erasing the stigma of mental illness. World Psychiatry 15, 67–73. doi: 10.1002/wps.20295
Corrigan, P. W., Markowitz, F. E., Watson, A. C., Rowan, D., and Kubiak, M. A. (2003). An attribution model of public discrimination towards persons with mental illness. J. Health Soc. Behav. 44, 162. doi: 10.2307/1519806
Corrigan, P. W., Powell, K. J., and Michaels, P. J. (2013). The effects of news stories on the stigma of mental illness. J. Nerv. Ment. Dis. 201, 179–182. doi: 10.1097/NMD.0b013e3182848c24
Corrigan, P. W., Schmidt, A., Bink, A. B., Nieweglowski, K., Al-Khouja, M. A., Qin, S., et al. (2017). Changing public stigma with continuum beliefs. J. Ment. Health 26, 411–418. doi: 10.1080/09638237.2016.1207224
Couture, S., and Penn, D. L. (2003). Interpersonal contact and the stigma of mental illness: a review of the literature. J. Mental Health 12, 291–305. doi: 10.1080/09638231000118276
David, C. C., Atun, J. M., Fille, E., and Monterola, C. (2011). Finding frames: comparing two methods of frame analysis. Communication Methods and Measures 5, 329–351. doi: 10.1080/19312458.2011.624873
Dietrich, S., Beck, M., Bujantugs, B., Kenzine, D., Matschinger, H., and Angermeyer, M. C. (2004). The relationship between public causal beliefs and social distance toward mentally ill people. Aust. N. Z. J. Psych. 38, 348–354; discussion 355–357. doi: 10.1080/j.1440-1614.2004.01363.x
Eaton, L. (2009). Celebrities help promote campaign to destigmatise mental illness. BMJ 338. doi: 10.1136/bmj.b309
Entman, R. M. (1993). Framing: toward clarification of a fractured paradigm. J. Commun. 43, 51–58. doi: 10.1111/j.1460-2466.1993.tb01304.x
Fox, S., and Jones, S. (2009). The Social Life of Health Information. Available online at: https://www.pewresearch.org/internet/2009/06/11/the-social-life-of-health-information/ (accessed February 8, 2022).
Fransen, M. L., Smit, E. G., and Verlegh, P. W. J. (2015). Strategies and motives for resistance to persuasion: an integrative framework. Front. Psychol. 6, 1201. doi: 10.3389/fpsyg.2015.01201
Freytag, A., Baumann, E., Angermeyer, M. C., and Schomerus, G. (2023). Self- and surrogate-seeking of information about mental health and illness in Germany. BMC Public Health 23, 65. doi: 10.1186/s12889-023-14998-0
Früh, W. (1994). Realitätsvermittlung durch Massenmedien: Die permanente Transformation der Wirklichkeit [Communication of Reality Through Mass Media: The Permanent Transformation of Reality]. Opladen: Westdt. Verl.
Gelenberg, A. J. (2010). The prevalence and impact of depression. J. Clin. Psychiatry 71, e06. doi: 10.4088/JCP.8001tx17c
Gitlin, T. (2003). The Whole World Is Watching: Mass Media in the Making and Unmaking of the New Left. Berkeley, CA: University of California Press.
Goffman, E. (1974). Frame Analysis: An Essay on the Organization of Experience. Frame Analysis: An Essay on the Organization of Experience. Cambridge, MA: Harvard University Press.
Griffiths, K. M., Christensen, H., and Jorm, A. F. (2008). Predictors of depression stigma. BMC Psychiatry 8, 25. doi: 10.1186/1471-244X-8-25
Gronholm, P. C., and Thornicroft, G. (2022). Impact of celebrity disclosure on mental health-related stigma. Epidemiol. Psych. Sci. 31, e62. doi: 10.1017/S2045796022000488
Hair, J. F., and Black, W. C. (2010). “Cluster analysis,” in Reading and Understanding More Multivariate Statistics, ed. L. G. Grimm, P. R. Yarnold (Washington, DC: American Psychological Association), 147–206.
Hegerl, U., Althaus, D., and Stefanek, J. (2003). Public attitudes towards treatment of depression: effects of an information campaign. Pharmacopsychiatry 36, 288–291. doi: 10.1055/s-2003-45115
Hoeken, H., Fikkers, K., Eerland, A., Holleman, B., van Berkum, J., and Maat, H. P. (2022). The perceived convincingness model: why and under what conditions processing fluency and emotions are valid indicators of a message's perceived convincingness. Commun. Theory 32, 488–496. doi: 10.1093/ct/qtac019
Holzinger, A., Floris, F., Schomerus, G., Carta, M. G., and Angermeyer, M. C. (2012). Gender differences in public beliefs and attitudes about mental disorder in Western Countries: a systematic review of population studies. Epidemiol. Psychiatric Sci. 21, 73–85. doi: 10.1017/S2045796011000552
Howell, J., and Shepperd, J. A. (2016). Establishing an information avoidance scale. Psychol. Asses. 28, 1695–1708. doi: 10.1037/pas0000315
Hugenberg, K., and Sacco, D. F. (2008). Social categorization and stereotyping: how social categorization biases person perception and face memory. Soc. Person. Psychol. Comp. 2, 1052–1072. doi: 10.1111/j.1751-9004.2008.00090.x
Johnston, H. (1996). “A methodology for frame analysis: from discourse to cognitive schemata,” in Social Movements and Culture, ed. H. Johnston, B. Klandermans (London: Routledge), 217–46.
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rodgers, B., and Pollitt, P. (1997). Mental health literacy: a survey of the public's ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med. J. Aust. 166, 182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x
Jorm, A. F., Reavley, N. J., and Ross, A. M. (2012). Belief in the dangerousness of people with mental disorders: a review. Aust. N. Z. J. Psychiatry 46, 1029–1045. doi: 10.1177/0004867412442406
Kermode, M., Bowen, K., Arole, S., Pathare, S., and Jorm, A. F. (2009). Attitudes to people with mental disorders: a mental health literacy survey in a rural area of Maharashtra, India. Soc. Psychiat. Epidemiol. 44, 1087–1096. doi: 10.1007/s00127-009-0031-7
Kessler, R. C. (2003). Epidemiology of women and depression. J. Affect. Dis. 74, 5–13. doi: 10.1016/S0165-0327(02)00426-3
Lannin, D. G., Vogel, D. L., Brenner, R. E., Abraham, W. T., and Heath, P. J. (2016). Does self-stigma reduce the probability of seeking mental health information? Health Soc. Work 63, 351–358. doi: 10.1037/cou0000108
Lebowitz, M. S., Ahn, W.-K., and Nolen-Hoeksema, S. (2013). Fixable or fate? Perceptions of the biology of depression. J. Consult. Clin. Psychol. 81, 518–527. doi: 10.1037/a0031730
Lersner, U.v, Gerb, J., Hizli, S., Waldhuber, D., Wallerand, A. F., Bajbouj, M., Schomerus, G., et al. (2019). Stigma of mental illness in Germans and Turkish immigrants in Germany: the effect of causal beliefs. Front. Psychiatry 10, 46. doi: 10.3389/fpsyt.2019.00046
Lindland, E. H., and Kendall-Taylor, N. (2012). Sensical translations: three case studies in applied cognitive communications. Annals Anthropol. Pract. 36, 45–67. doi: 10.1111/j.2153-9588.2012.01092.x
Link, B. G., Cullen, F. T., Frank, J., and Wozniak, J. F. (1987). The social rejection of former mental patients: understanding why labels matter. Am. J. Sociol. 92, 1461–1500. doi: 10.1086/228672
Link, B. G., and Phelan, J. C. (2001). Conceptualizing stigma. Annual Rev. Sociol. 27, 363–385. doi: 10.1146/annurev.soc.27.1.363
Link, B. G., Phelan, J. C., Bresnahan, M., Stueve, A., and Pescosolido, B. A. (1999). Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am. J. Public Health 89, 1328–1333. doi: 10.2105/AJPH.89.9.1328
Link, B. G., Yang, L. H., Phelan, J. C., and Collins, P. Y. (2004). Measuring mental illness stigma. Schizophrenia Bul. 30, 511–541. doi: 10.1093/oxfordjournals.schbul.a007098
Link, E., Baumann, E., Linn, A. J., Fahr, A., Schulz, P. J., and Abuzahra, A. E. (2021). Influencing factors of online health information seeking in selected European countries. EJHC 2, 29–55. doi: 10.47368/ejhc.2021.002
Ma, Z. (2017). How the media cover mental illnesses: a review. Health Educ. 117, 90–109. doi: 10.1108/HE-01-2016-0004
Mackie, D. M., Smith, E. R., and Ray, D. G. (2008). Intergroup emotions and intergroup relations. Soc. Person. Psychol. Comp. 2, 1866–1880. doi: 10.1111/j.1751-9004.2008.00130.x
Major, B., and O'Brien, L. T. (2005). The Social Psychology of Stigma. Annual review of psychology 56, 393–421. doi: 10.1146/annurev.psych.56.091103.070137
McKeever, A., Agius, M., and Mohr, P. (2017). A review of the epidemiology of major depressive disorder and of its consequences for society and the individual. Psychiatria Danubina 29, 222–231.
Meyer, J.-H., de Ruyter, K., Grewal, D., Cleeren, K., Keeling, D. I., and Motyka, S. (2020). Categorical versus dimensional thinking: improving anti-stigma campaigns by matching health message frames and implicit worldviews. J. Acad. Mark. Sci. 48, 222–245. doi: 10.1007/s11747-019-00673-7
Michaels, P. J., López, M., Rüsch, N., and Corrigan, P. W. (2017). Constructs and concepts comprising the stigma of mental illness. PSYE 4, 183. doi: 10.25115/psye.v4i2.490
Muschetto, T., and Siegel, J. T. (2019). Attribution theory and support for individuals with depression: the impact of controllability, stability, and interpersonal relationship. Stigma Health 4, 126–135. doi: 10.1037/sah0000131
Neuberg, S. L., and Cottrell, C. A. (2002). “Intergroup emotions: a sociofunctional approach,” in From Prejudice to Intergroup Emotions: Differentiated Reactions to Social Groups, ed. D. M. Mackie, E. R. Smith (London: Psychology Press), 265–83.
Ozmen, E., Ogel, K., Aker, T., Sagduyu, A., Tamar, D., and Boratav, C. (2004). Public Attitudes to depression in Urban Turkey - the influence of perceptions and causal attributions on social distance towards individuals suffering from depression. Soc. Psychiat. Epidemiol. 39, 1010–1016. doi: 10.1007/s00127-004-0843-4
Peluso, E. T. P., and Blay, S. L. (2009). Public stigma in relation to individuals with depression. J. Affect. Dis. 115, 201–206. doi: 10.1016/j.jad.2008.08.013
Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., and Link, B. G. (2010). A disease like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am. J. Psychiatry 167, 1321–1330. doi: 10.1176/appi.ajp.2010.09121743
Phelan, J. C., Yang, L. H., and Cruz-Rojas, R. (2006). Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatric Serv. 57, 382–7. doi: 10.1176/appi.ps.57.3.382
Richards, D. (2011). Prevalence and clinical course of depression: a review. Clin. Psychol. Rev. 31, 1117–1125. doi: 10.1016/j.cpr.2011.07.004
Riedel-Heller, S. G., Matschinger, H., and Angermeyer, M. C. (2005). Mental disorders–who and what might help? Help-seeking and treatment preferences of the lay public. Soc. Psychiat. Epidemiol. 40, 167–174. doi: 10.1007/s00127-005-0863-8
Ritterfeld, U., and Jin, S.-A. (2006). Addressing media stigma for people experiencing mental illness using an entertainment-education strategy. J. Health Psychol. 11, 247–267. doi: 10.1177/1359105306061185
Röhm, A., Hastall, M. R., and Ritterfeld, U. (2018). “Stigmatisierende und destigmatisierende prozesse in der gesundheitskommunikation,” in Handbuch Gesundheitskommunikation: Kommunikationswissenschaftliche Perspektiven, ed. C. Rossmann, M. R. Hastall (Wiesbaden: Springer Fachmedien Wiesbaden), 1–11.
Romer, D., and Bock, M. (2008). Reducing the stigma of mental illness among adolescents and young adults: the effects of treatment information. J. Health Commun. 13, 742–758. doi: 10.1080/10810730802487406
Sampogna, G., Bakolis, I., Evans-Lacko, S., Robinson, E., Thornicroft, G., and Henderson, C. (2017). The impact of social marketing campaigns on reducing mental health stigma: results from the 2009-2014 time to change programme. Eur. Psychiatry J. Assoc. Eur. Psychiat. 40, 116–122. doi: 10.1016/j.eurpsy.2016.08.008
Scheufele, B. (2003). Frames - Framing - Framing-Effekte [Frames - Framing - Framing Effects]. Wiesbaden: VS Verlag für Sozialwissenschaften.
Schomerus, G., Angermeyer, M. C., Baumeister, S. E., Stolzenburg, S., Link, B. G., and Phelan, J. C. (2016). An online intervention using information on the mental health-mental illness continuum to reduce stigma. Eur. Psychiatry J. Assoc. Eur. Psychiat. 32, 21–27. doi: 10.1016/j.eurpsy.2015.11.006
Schomerus, G., Matschinger, H., and Angermeyer, M. C. (2013). Continuum beliefs and stigmatizing attitudes towards persons with schizophrenia, depression and alcohol dependence. Psychiatry Res. 209, 665–669. doi: 10.1016/j.psychres.2013.02.006
Schomerus, G., Matschinger, H., and Angermeyer, M. C. (2014). Causal beliefs of the public and social acceptance of persons with mental illness: a comparative analysis of schizophrenia, depression and alcohol dependence. Psychol. Med. 44, 303–314. doi: 10.1017/S003329171300072X
Schomerus, G., Schindler, S., Baumann, E., and Angermeyer, M. C. (2023). Changes in continuum beliefs for depression and schizophrenia in the general population 2011-2020: a widening gap. Soc. Psychiat. Epidemiol. 58, 17–23. doi: 10.1007/s00127-022-02272-4
Schotte, C. K. W., van den Bossche, B., de Doncker, D., Claes, S., and Cosyns, P. (2006). A biopsychosocial model as a guide for psychoeducation and treatment of depression. Depression Anxiety 23, 312–324. doi: 10.1002/da.20177
Schultz, D. E., and Block, M. P. (2018). “Beyond demographics: enhancing media planning with emotional variables,” in Power to Consumers, ed. V. Cauberghe, L. Hudders, M. Eisend (Wiesbaden, Heidelberg: Springer Gabler), 177–90.
Shore, B. (1996). Culture in Mind: Cognition, Culture, and the Problem of Meaning. 1st ed. as an Oxford Univ. Press paperback. New York, NY: Oxford Univ. Press.
Sickel, A. E., Seacat, J. D., and Nabors, N. A. (2014). Mental health stigma update: a review of consequences. Adv. Mental Health 12, 202–215. doi: 10.1080/18374905.2014.11081898
Sickel, A. E., Seacat, J. D., and Nabors, N. A. (2019). Mental health stigma: impact on mental health treatment attitudes and physical health. J. Health Psychol. 24, 586–599. doi: 10.1177/1359105316681430
Speerforck, S., Schomerus, G., Matschinger, H., and Angermeyer, M. C. (2017). Treatment recommendations for schizophrenia, major depression and alcohol dependence and stigmatizing attitudes of the public: results from a german population survey. Eur. Arch. Psychiatry Clin. Neurosci. 267, 341–350. doi: 10.1007/s00406-016-0755-9
Speerforck, S., Schomerus, G., Pruess, S., and Angermeyer, M. C. (2014). Different biogenetic causal explanations and attitudes towards persons with major depression, schizophrenia and alcohol dependence: is the concept of a chemical imbalance beneficial? J. Affect. Dis. 168, 224–228. doi: 10.1016/j.jad.2014.06.013
Stamovlasis, D., Vaiopoulou, J., and Papageorgiou, G. (2020). A comparative evaluation of dissimilarity-based and model-based clustering in science education research: the case of children's mental models of the earth. IJDATS 12, 247. doi: 10.1504/IJDATS.2020.108080
Statistisches Bundesamt (Destatis) [Federal Statistical office of Germany] (2019). Bevölkerung in Deutschland [Population of Germany]. Available online at: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/_inhalt.html
Suls, J., and Rothman, A. (2004). Evolution of the biopsychosocial model: prospects and challenges for health psychology. Health Psychol. Official J. Div. Health Psychol. Am. Psychol. Assoc. 23, 119–125. doi: 10.1037/0278-6133.23.2.119
van Gorp, B. (2007). The constructionist approach to framing: bringing culture back in. J. Commun. 57, 60–78. doi: 10.1111/j.1460-2466.2006.00329_5.x
Ward, J. H. Jr. (1963). Hierarchical grouping to optimize an objective function. J. Am. Stat. Assoc. 58, 236–244. doi: 10.1080/01621459.1963.10500845
Wicks, R. H. (2005). Message framing and constructing meaning: an emerging paradigm in mass communication research. Annals Int. Commun. Assoc. 29, 335–362. doi: 10.1080/23808985.2005.11679052
Witte, K., and Allen, M. (2000). A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ. Behav. 27, 591–615. doi: 10.1177/109019810002700506
Wood, L., Birtel, M. D., Alsawy, S., Pyle, M., and Morrison, A. P. (2014). Public perceptions of stigma towards people with schizophrenia, depression, and anxiety. Psychiatry Res. 220, 604–608. doi: 10.1016/j.psychres.2014.07.012
World Health Organization (2017). Depression and Other Common Mental Disorders: Global Health Estimates. Unpublished manuscript. Available online at: https://apps.who.int/iris/handle/10665/254610 (accessed July 19, 2022).
Yang, F., Yang, B. X., Stone, T. E., Wang, X. Q., Zhou, Y., Zhang, J., et al. (2020). Stigma towards depression in a community-based sample in China. Comprehen. Psychiatry 97, 152152. doi: 10.1016/j.comppsych.2019.152152
Keywords: anti-stigma communication, cluster analysis, cognitive framing, depression, health communication, stigma
Citation: Freytag A, Baumann E, Schindler S, Angermeyer MC and Schomerus G (2024) Cognitive frames of depression and their association with accessibility to mental health communication: a cluster analysis for developing stigma-sensitive targeting strategies. Front. Commun. 8:1308281. doi: 10.3389/fcomm.2023.1308281
Received: 06 October 2023; Accepted: 29 November 2023;
Published: 08 January 2024.
Edited by:
Sergio Villanueva Baselga, University of Barcelona, SpainReviewed by:
Alexander Ort, University of Lucerne, SwitzerlandGrant Corser, Southern Utah University, United States
Copyright © 2024 Freytag, Baumann, Schindler, Angermeyer and Schomerus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Freytag, YW5uYS5mcmV5dGFnQGlqay5obXRtLWhhbm5vdmVyLmRl
 Anna Freytag
Anna Freytag Eva Baumann
Eva Baumann Stephanie Schindler
Stephanie Schindler Matthias C. Angermeyer3
Matthias C. Angermeyer3