
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Commun., 21 September 2023
Sec. Health Communication
Volume 8 - 2023 | https://doi.org/10.3389/fcomm.2023.1230015
This article is part of the Research TopicIntegrating Digital Health Technologies in Clinical Practice and Everyday Life: Unfolding Innovative Communication PracticesView all 9 articles
Introduction: Increasingly, people are turning toward digital health technologies to support their care management, communication with health professionals, and performing activities of daily living. Digital health technologies may be well implemented in clinical practices in several jurisdictions, but the influence of sociocultural factors may sometimes be neglected. To increase use and sustainability of these innovative solutions in health care, we need to understand acceptability among diverse groups of the population such as linguistically diverse populations. Francophone-speaking populations in Canada, for example, are known to endure challenges with income, health and difficulties associated with living in rural areas which impede on their likelihood to use digital health technologies. As part of the University of Ottawa International Francophonie Research Chair on Digital Health Technologies, this study aimed to understand the conditions that make digital health technologies acceptable among francophone-speaking communities.
Methods: Using a meta-ethnography methodology, this study synthesizes international qualitative research on social acceptability of digital health technology among francophone-speaking communities. We focused on four types of digital health technologies: telemedicine, mobile technologies, wearable technologies, and robotic technologies. Using Noblit and Hare's 7 phase approach to conducting a meta-ethnography, we were able to get a comprehensive synthesis and understanding of the research landscape on the issue. Studies published between 2010 and 2020 were included and synthesized using NVivo, excel and a mind mapping technique.
Results: Our coding revealed that factors of social acceptability for digital health technologies could be grouped into the following categories: care organization, self-care support, communication with care team, relational and technical risks, organizational factors, social and ethical values. Our paper discusses the themes evoked in each category and their relevance for the included digital health technologies.
Discussion: In discussing the results, we present commonalities and differences in the social acceptability factors of the different digital health technologies. In addition, we demonstrate the importance of considering sociocultural diversity in the study of social acceptability for digital health technologies.
Implications: The results of this study have implications for practitioners who are the instigators of digital health technology implementation with healthcare service users. By understanding factors of social acceptability among francophone-speaking communities, practitioners will be better suited to propose and support the implementation of technologies in ways that are suitable for these individuals. For policymakers, this knowledge could be used for developing policy actions based on consideration for diversity.
Technology in all its forms has greatly evolved in the last decade. Technological solutions are being used in many sectors to support and enhance efficacy of operations. In the sphere of healthcare, technologies have revolutionized the delivery of care and even more prominently during the COVID-19 pandemic (Javaid et al., 2022). Digital health technologies specifically have improved many aspects of patient care and healthcare, including care management, communicating with health professionals, and performing activities of daily living (Awad et al., 2021). Areas that have benefitted from advancements in digital health technologies include diagnostics, manufacturing of medicines, treatment, medicine supply, and patient support (Awad et al., 2021). Additionally, the diversity in the types of digital health technologies is continuously growing. They include technologies such as mobile technologies, robot technologies, wearable devices, sensors, telemedicine, among others. Digital health technologies are can be very helpful for healthcare service users and have already been implemented to support a variety of conditions including dementias (Astell, 2019), chronic diseases (Milani et al., 2016), and mental health (Balcombe and Leo, 2021). The World Health Organization, through several resolutions and their Global strategy on digital health 2020–2025, are multiplying efforts urging Member States to develop solutions which consider digital health technologies (World Health Organization, 2023). As mentioned in the global strategy, digital health technologies are changing healthcare and provide opportunities to enhance health (World Health Organization, 2021).
While digital health technologies are widely used and embedded within existing practices, a multiplicity of factors may impact their use and uptake by end-users. In the literature, this concept of use and uptake is often measured and defined as acceptability (Perski and Short, 2021). Technology acceptance, which we also refer to as social acceptability, relates to the attitudes, intentions and perceptions of end-users toward a technology (Nadal et al., 2020). Factors such as digital literacy (Norgaard et al., 2015), technological infrastructure (Anwar and Shamim, 2011; Sharma et al., 2018; Rodriguez et al., 2022), and perceptions of benefits, utility, and effectiveness of a technology (Perski and Short, 2021), all contribute to the success of its implementation and usage. However, sociocultural factors that modulate digital health technology adoption are usually neglected or overseen. Sociocultural factors that are known to have an impact on digital health technology use include culture, ethnicity, geographic location, education, age, and language (Luborsky, 1993; Kontos et al., 2014; Paré et al., 2017; Ashcroft et al., 2021; Perski and Short, 2021). For instance, age is commonly and widely discussed in the literature as a determinant of digital health technology use. In the case of older adults for example, research has found that the combination of intrinsic and extrinsic factors related to age can act both as barriers and facilitators to digital health technology use (Wilson et al., 2021).
In order to increase acceptability and therefore sustained use of digital health technologies by different groups of the population, we need to understand the factors that modulate their acceptability. However, there currently exist limited research that addresses differences in acceptability among diverse groups of end-users, including those with diverse linguistic backgrounds (Nouri et al., 2020; Whitehead et al., 2023). Most studies reflect on the language of the digital health technology and its impact on user acceptance (Whitehead et al., 2023), neglecting the particularities of acceptance from within the linguistically-diverse group. For francophone-speaking populations specifically, previous research has shown that health technologies can sometimes lead to social inequalities in health (Mayères, 2017; Weiss et al., 2018). Additionally, people from culturally and linguistically diverse backgrounds remain underrepresented in digital health research due to the overrepresentation of English-speaking people in the studies (Woodward-Kron et al., 2019). Similarly, linguistic minorities are under-represented in studies on the acceptability of health technologies. Exclusion of these populations from research contributes to health inequalities for linguistic-minority groups or other linguistics groups and also limits the generalizability of research findings (Craig et al., 2021). In response to this gap and findings from previous research focussing on francophone-speaking populations, this project will identify acceptability factors for digital health technologies among francophone-speaking individuals across several French-speaking countries.
As part of the University of Ottawa International Francophonie Research Chair on Digital Health Technologies, this study aimed to understand the conditions that make digital health technologies accessible and acceptable among francophone-speaking communities across the world.
In our study, we used a meta-ethnographic approach using the seven phases identified by Noblit and Hare (1999). A meta-ethnography is an inductive and interpretive approach to synthesize qualitative research (Sattar et al., 2021). Through this approach, we identified and synthesized qualitative studies on the topic of social acceptability of digital health technologies among francophone-speaking communities. Additionally, we interpreted the studies via an analysis and comparison exercise. The phases by Noblit and Hare (1999) were performed as follows:
To get started, Noblit and Hare (1999) point to the importance of carefully delineating the common interest for the meta-ethnography. As such we identified and carefully selected a research question that was of interest to the research team. The guiding question for this research was What conditions make digital health technologies accessible and acceptable among francophone-speaking communities across the world?
Our study is based on an understanding that qualitative studies on the topic of digital health technology can provide significant details on the conditions and determinants that would make them socially acceptable among francophone-speaking communities in Canada and internationally. We believe that capturing the opinions, attitudes and beliefs of francophone individuals can help us identify the decisive factors of social acceptability on digital health technologies for this group of the population.
In the quest for selecting relevant articles, Noblit and Hare (1999) signal the importance of identifying a topic worthy of the efforts. A meta-ethnographic study aims to provide an exhaustive list of all the studies on a particular topic, and for this reason, authors need to make decisions on what is relevant to the inquiry. For our study, we are convinced that francophone-speaking populations could have different motivations or be influenced by diverging factors in their process of accepting to adopt a digital health technology. As such, we have focused our search of qualitative studies in three key areas: social acceptability, digital health technologies and francophone-speaking populations. In our identification and selection of articles, the term digital health technology was used broadly to include various types of health technologies such as telemedicine and mobile applications.
First, we performed a search for relevant articles in scientific databases. With the help from two librarians at the University of Ottawa, we selected scientific databases that were likely to include the articles of interest from the health sciences and social sciences domains. Our detailed search strategy (Supplementary material 1) included a translation of keywords, MeSH terms and limits (dates and article languages) which were applied among 10 different databases. Specifically, articles were included if they were published in English of French, since 2010 and included the views of francophone-speaking populations on the use of digital health technologies. To identify studies that focused on French-speaking populations, we included search terms on the countries with Francophone-speaking communities (i.e., Canada, France, etc.). The database search was performed by two members of the research team (AGB and CS) between June 19, 2020, and June 25, 2020. All members of the research team were bilingual and therefore able to screen and analyze articles in both English and French. For articles that were translated in the interpretation stage of the study, at least two members of the team reviewed the translation and interpretation to ensure accuracy.
The screening of articles was performed in a staged approach using the Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org. Our inclusion criteria specifically focused on identifying studies that were qualitative in nature, included the appropriate concepts of acceptability, and included mention of technologies within the healthcare domain (Table 1). First, we performed title and abstract screening to effectively include or dismiss articles based on their relevance to the three key areas of interest. Subsequently, we performed a full-text screening of the articles to exclude articles that were not relevant to the topic of interest or used methodologies and interventions that diverged from our inclusion criteria. Finally, we also performed citation searching through included articles to identify other articles that were relevant to the topic of interest. If reviewers encountered difficulties or had challenges in making a screening decision, the other reviewer was asked to review the articles and provide their advice. Mutual agreement was obtained on the screening decision for those articles. Details on the screening and article inclusion process can be found in our PRISMA flow diagram (Figure 1).
In the third phase of Noblit and Hare (1999) meta-ethnography approach, the authors point to the importance of reading the articles on a repeated basis to really interpret their meaning. For this reason, the research team read the included articles several times and started to identify key characteristics to extract from each.
We began coding each article using the program Nvivo 12. As we were coding, we started producing a coding framework and refined it as more codes were created. As a result, we organized the coding framework using specific categories of factors affecting social acceptability of digital health technologies.
When the studies are well understood and authors are ready to begin the synthesis, Noblit and Hare (1999) refer to this as phase 4 of the meta-ethnography approach. In this phase, researchers must begin synthesizing the information and looking for relationships among the different include studies.
To do this, we decided to start organizing the for each type of digital health technology and identified the perspective from which the study participants provided details on factors of acceptability for the digital health technologies. This was done using a simple excel spreadsheet where we included the codes and article details (Figure 2).
Subsequently, we visually represented the different concepts of acceptability using a concept map, created using the program Xmind.
In phase 5 of Noblit and Hare (1999) meta-ethnography approach, they refer to going beyond the individual articles and comparing their accounts to one another. For our study, we looked at each concept of acceptability for each of the articles and compared them with the other articles within the same technology type and perspective. This allowed us to identify similarities and differences around the factors of social acceptability for each of the digital health technologies.
The results of the synthesis translation exercise will be presented in the results of this article.
In this study, we retrieved 15 articles that met the inclusion criteria (Table 2). The studies were published between 2013 and 2020 and present the perspective of francophone-speaking healthcare service users (n = 8), caregivers (n = 2), healthcare professionals (n = 11), and administrators (n = 4) on social acceptability for four types of digital health technologies. The technologies include telemedicine (n = 7), mobile technologies (n = 4), sensor and wearable technologies (n = 2), and robot technologies (n = 2). The results for each technology will be presented separately. Perceptions of healthcare administrators were combined with that of healthcare professionals.
In the included articles, mobile technologies encompass mobile health apps (Ghandour et al., 2018; Sewitch et al., 2019), technologies such as advanced smartphone features (Lessard et al., 2019), and connected health tools (Cases, 2017).
For mobile technologies, the overall conceptualization of francophone-speaking populations for social acceptability diverged depending on the perspectives that were sought from participants in the studies. From the perspective of healthcare service users, social acceptability for a mobile technology is defined as the technology's ability to meet the needs of end-users on both a personal and technical level. On the personal level, social acceptability was related to the notion of empowerment. For individuals to adopt a digital health technology, they would need to perceive that they are empowered in their care and health management (Cases, 2017). On a technical level, the preferences with regards to the mobile technology itself were described as critical. For example, two studies pointed to the importance for considering the user preferences for the specific content and features of mobile applications (Lessard et al., 2019; Sewitch et al., 2019). From the perspective of healthcare professionals, acceptability is often mentioned in the context of organizational constraints and opportunities. As pointed to Ghandour et al. (2018), social acceptability occurs once a technology has passed through the adoption continuum within an organization.
Social acceptability of mobile technologies is modulated by various factors that differ based on the end-user, whether from the view of the patient (Figure 3) or from the view of a healthcare professional (Figure 4). From the perspective of healthcare service users, a mobile health technology would be accepted if it helps organize care, supports self-care, accounts for technical risks, and has social value. From the perspective of healthcare professionals, the acceptability of a mobile health technology is dependent on its impact toward organization of care, if it supports patient self-care, if it impacts patient/healthcare professional relationships and communication, if it accounts for technical risks, and if it considers organizational factors.
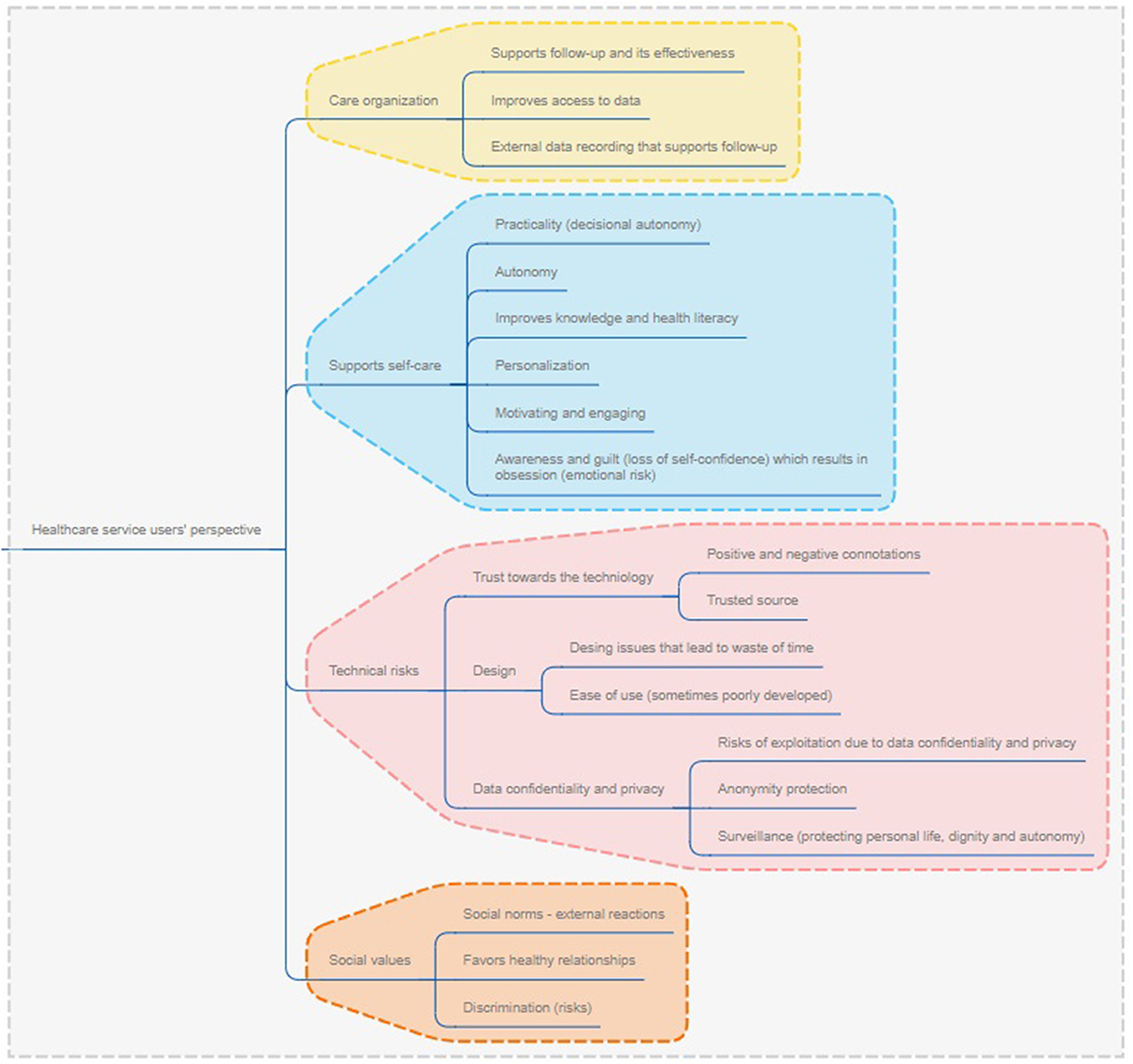
Figure 3. Factors of social acceptability for mobile technologies from the perspective of healthcare service users.
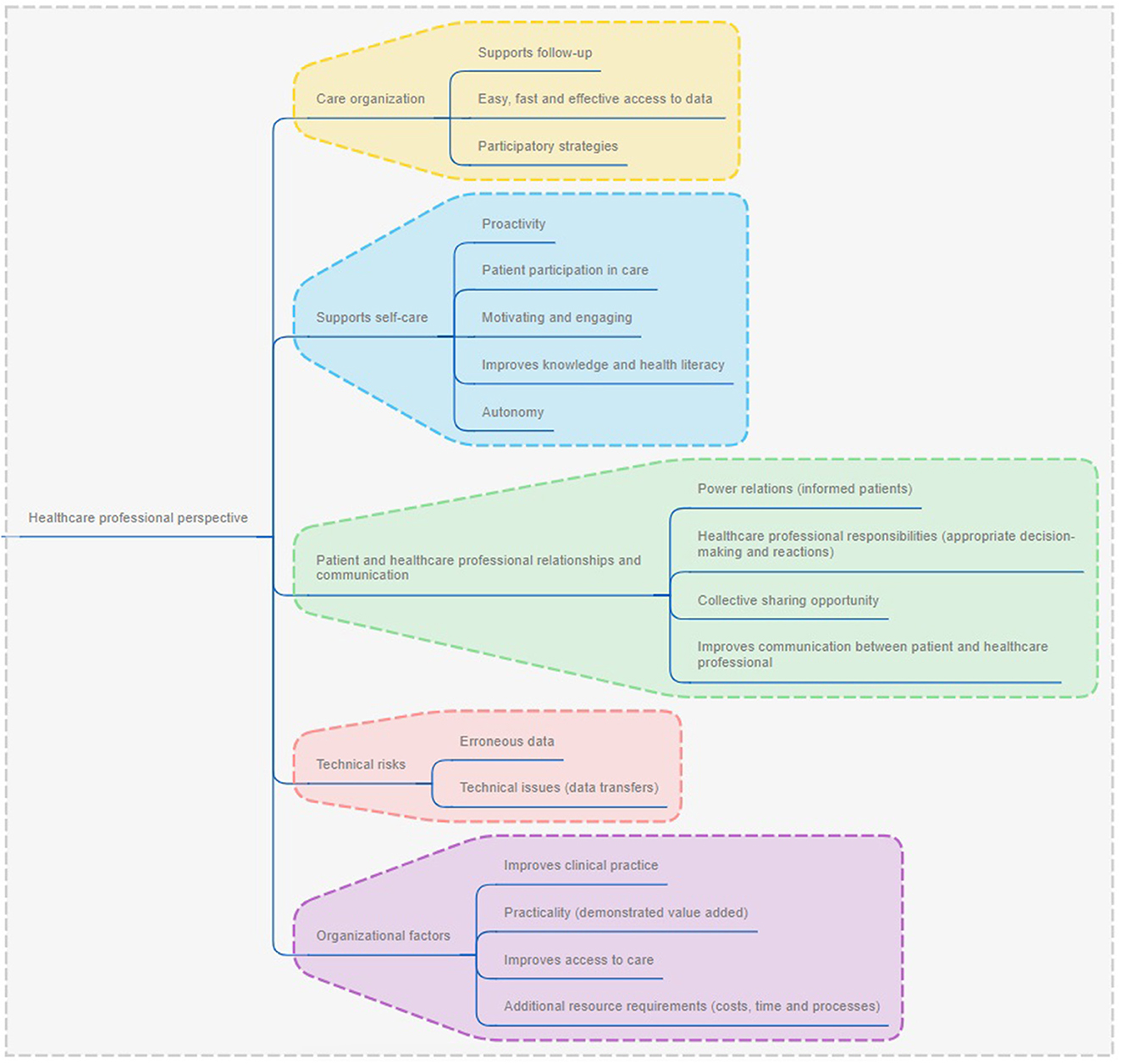
Figure 4. Factors of social acceptability for mobile technologies from the perspective of healthcare providers.
From both perspectives, acceptability was mediated based on a mobile technology's impact on care management, if they supported self-care and if technical risks were minimal. For care management, studies referred to the potential for mobile technologies to enhance the capacity of healthcare service users to monitor their conditions and symptoms, keep a record of symptoms and support recall for care management purposes. For example, healthcare service users in the study by Cases (2017) mentioned that “parce que des fois, on oublie les choses et que… quand on a quelque chose qui nous rappelle ce qui s'est passé, ça fait un historique. sometimes we forget things and when we have something that helps us remember it, it creates a history” (para. 24). For self-care, both healthcare service users and health-care professionals viewed mobile technologies as a personalized tool to promote autonomy by enhancing health literacy, and being engaging and motivating. For example, in the study by Sewitch et al. (2019), healthcare service users reflected on the mobile technology's benefits for autonomy as a result of personalization: “Although the internet can provide the same information as the smartphone app, the app may be more helpful because (tailored) alerts can remove fear and (make sure) you take the right thing at the right time” (p. 6). For technical risks associated with mobile technologies, healthcare service users and healthcare professionals consistently referred to this type of risk as a limiting factor for technology uptake. Technical risks such as design, operationalization features, and privacy and security of data all stood out as factors that significantly impacted willingness to use and adhere to the technology. For example, in the study by Ghandour et al. (2018), healthcare professionals' mentioned that their decision to adopt mobile technologies were based on the functionalities they offered, if they were operatable in tandem with other existing systems and devices, and if they were easily usable by both healthcare service users and healthcare professionals.
Other relevant factors brought up either by healthcare service users or healthcare providers were the social values associated with a mobile technology, the potential for the mobile technology to support communication between a healthcare team and other relevant organizational factors. With regards to social values, healthcare service users positively viewed mobile technologies when healthcare professionals spoke highly of them (positive connotations) and when the technologies positively enhanced their relationships with others. For example, in the case of a mobile technology where healthcare service users enter their medical information and data prior to a medical consultation, healthcare service users had a tendency to use the technology when it was a recommendation from a medical professional, and was therefore perceived as a valuable tool (Cases, 2017). However, in another example where a mobile technology anonymously disclosed exposures to health risk resulting from close contact with someone presenting a specific disease, participants viewed this as discriminatory and impeding on positive relationships with others, and therefore made them reluctant to use the technology (Lessard et al., 2019). From the perspective of healthcare professionals, mobile technologies presented significant potential to improve communication with their patient. However, healthcare professionals raised concerns with the power relations that would be affected in cases when healthcare service users became more involved and knowledgeable about their situation. For example, in the study by Ghandour et al. (2018), an emerging theme concerned how “les professionnels qui doivent aussi s'habituer à une nouvelle réalité dans leur relation avec des patients de plus en plus informés. The healthcare professionals […] must also adapt to a new reality where patients are more and more informed” (p. 842). Additionally, the studies showed that healthcare professionals had some mixed attitudes with regard to mobile technologies because of several organizational factors. While being open and willing to integrate and use mobile technologies to support care management, healthcare professionals indicated concerns with increased needs for resources and time, capacity to manage change, and disruptions in regular modes of work (Ghandour et al., 2018). However, with appropriate mechanisms in place, such as support from management and training opportunities, healthcare professionals truly see the value and benefits from integrating mobile technologies in care management (Ghandour et al., 2018).
Robot technologies are composed of multiple technologies into one functioning and responsive device. The integration of several technologies into one robot-like device enables developers to create unique technologies that can look like humans, animals or machines (Zsiga et al., 2013).
When analyzing the potential for uptake of robot technologies, Pino et al. (2015) described it as being determined by factors of the Technology Acceptance Model (Davis, 1989). In this model, a person's intention to use and actual use of a technology is determined by several factors of adoption such as social influences, facilitating conditions, trust, privacy concerns, ethical concerns, among others (Pino et al., 2015). Additionally, acceptability is modulated by the perception of stakeholders involved in its implementation including healthcare service users, professionals and caregivers (Zsiga et al., 2013; Pino et al., 2015).
Social acceptability of robot technologies for francophone-speaking populations is determined by factors that are unique to both healthcare service users (Figure 5) and caregivers (Figure 6). From the perspective of healthcare service users, robot technologies are acceptable if they support daily life, align with social values, and meet specific ethical standards. In the case of caregivers, robot technologies need to be embedded within the care continuum and support follow-up, and consider relational aspects within care management as to not remove the human component of care. Healthcare professionals' perspectives on robot technologies were not sought in the identified studies.
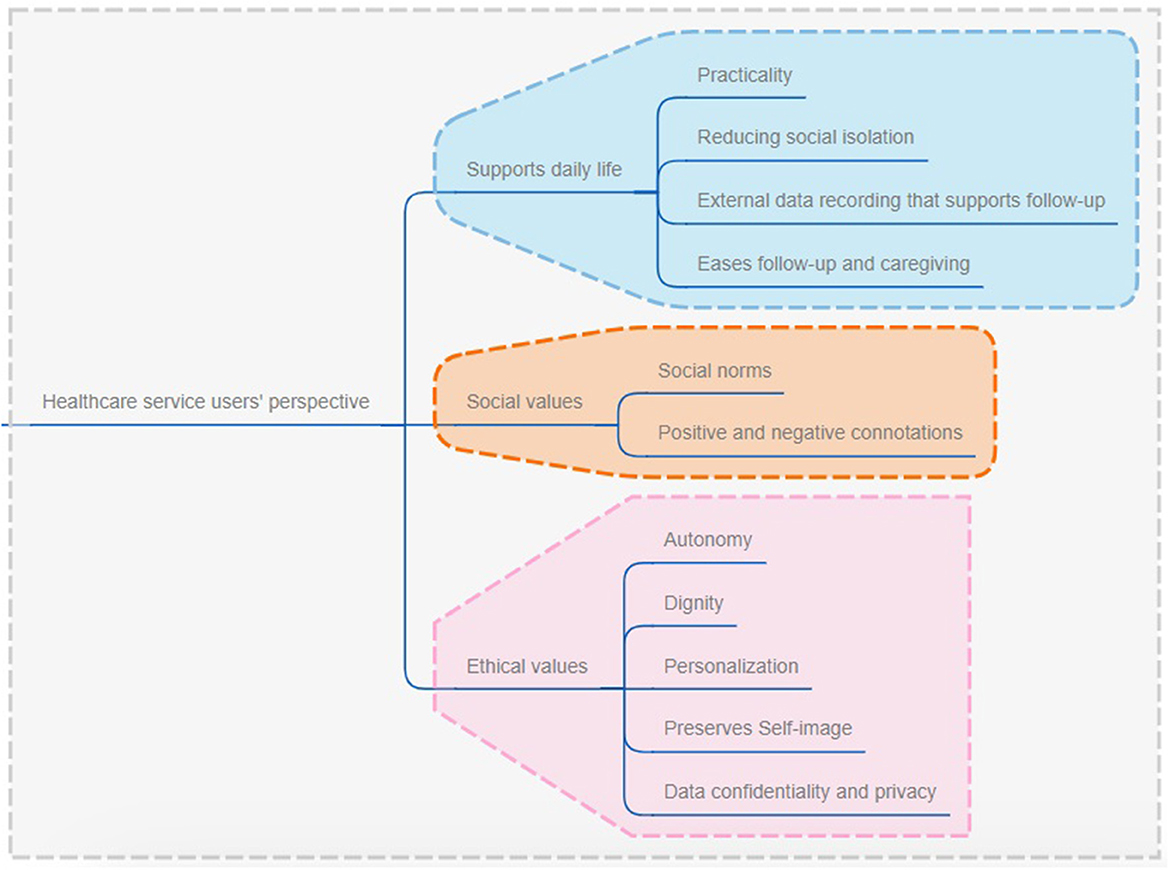
Figure 5. Factors of social acceptability for robot technologies from the perspective of healthcare service users.
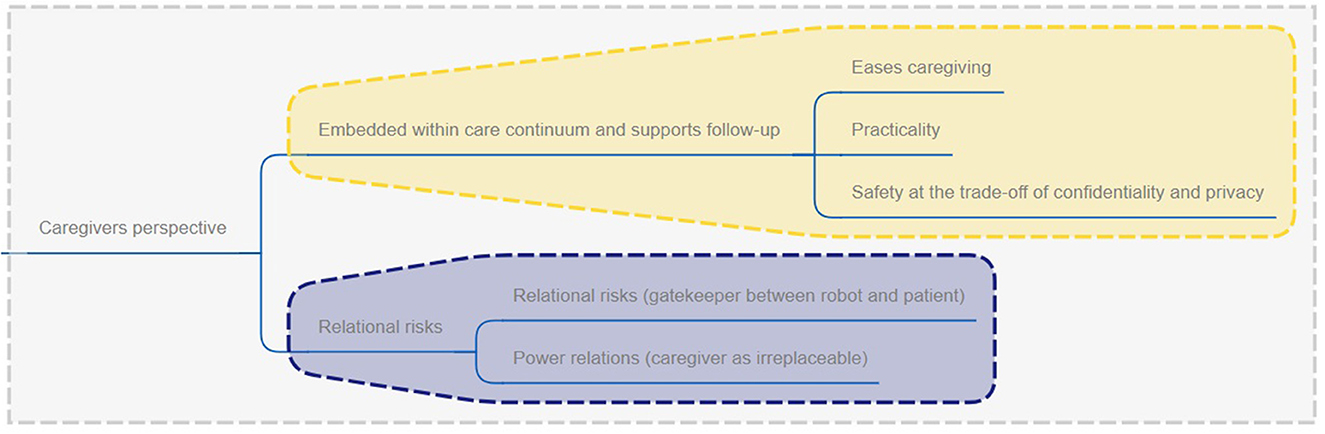
Figure 6. Factors of social acceptability for robot technologies from the perspective of caregivers.
For both healthcare service users and caregivers, robots should support a person in performing activities of daily living. For instance, robots should help fil a gap for healthcare service users (i.e., individuals with cognitive impairment) and also for their caregivers to increase the likelihood that it would be accepted (Zsiga et al., 2013; Pino et al., 2015). For users, such as older adults with cognitive impairment, the value of robots remains not only in its potential to be helpful, such as for remembering things, providing companionship, supporting safety at home and in emergency situations, but the technology must also respond and communicate back with the end-user (Zsiga et al., 2013; Pino et al., 2015). For caregivers, robots should ease their role as a caregiver by decreasing the caregiving burden through taking over simple tasks that would otherwise have to be accomplished by a caregiver (Pino et al., 2015). However, caregivers believe that their role as a human caregiver should not be overlooked or neglected even if a robot takes over certain functions (Zsiga et al., 2013).
The ethical factors associated with robots were mentioned in the articles as a point of contention for their use in healthcare. Privacy issues were raised by both healthcare service users and caregivers in the case when robots have the capacity to film (Zsiga et al., 2013) and when the robots have surveillance capacities (Pino et al., 2015). The studies reported that filming and surveillance capacities were viewed as infringing on the users' privacy. One article noted, however, that caregivers value safety of the person they cared for as a necessary trade-off to confidentiality and privacy (Pino et al., 2015). In regard to the appearance of the robot, healthcare service users viewed them as potentially stigmatizing. As pointed out by a participant with mild cognitive impairment in Pino et al. (2015), “some work has to be done if you don't want people to think that if they are given a robot it's because they are not worth a human company” (p. 10). Generally, animal-like or machine-like robots were preferred by both healthcare service users and caregivers because human-like appearances may be viewed as infantilizing and even confuse older adults with cognitive impairment (Pino et al., 2015).
Telemedicine is a practical medical tool that encompasses various forms of consultation, diagnostic, and therapeutic modes of engagement between healthcare service users and healthcare professionals (Durupt et al., 2016). It is an effective remote tool that allows the integration, communication and sharing of data between a care team, caregivers and healthcare service users, and allows improvements to medical processes (Lamothe et al., 2013; Habib et al., 2019).
In the literature the social acceptability of telemedicine for francophone-speaking populations is mainly described in terms of its organizational impacts and requirements (Lamothe et al., 2013; Mathieu-Fritz and Esterle, 2013; Meyer et al., 2014; Durupt et al., 2016; Odnoletkova et al., 2016; Mathieu-Fritz, 2018; Habib et al., 2019). The nature of telemedicine, which involves healthcare professionals, aligns with the social acceptability construct focussed on organizational factors. As described in Mathieu-Fritz and Esterle (2013), telemedicine usage is dependent on the benefits it has on improving professional practice. Telemedicine's acceptability is also defined for its benefits toward healthcare service users. As described by Odnoletkova et al. (2016), healthcare service users can benefit from telemedicine as it is an effective form of communication with the care team, it enhances health literacy, provides useful and timely information, and leads to satisfaction with overall care management.
In the articles retrieved, factors of social acceptability for telemedicine for healthcare service users and healthcare professionals were similar except for organizational factors (Figures 7, 8). For both groups, telemedicine was accepted if it allowed for better care coordination, supported patient self-care, enabled better communication between the patient and the care team, and effectively considered and mitigated technical risks.
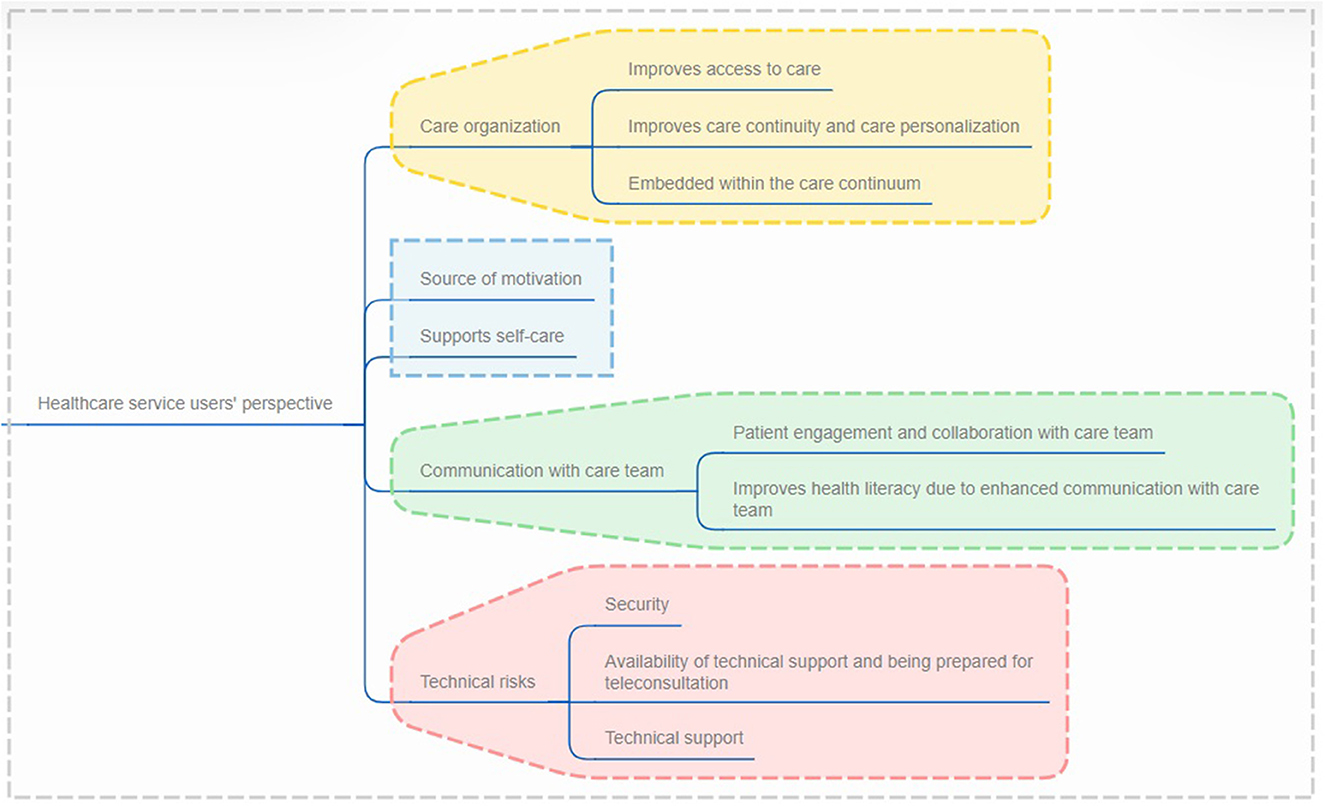
Figure 7. Factors of social acceptability for telemedicine from the perspective of healthcare service users.
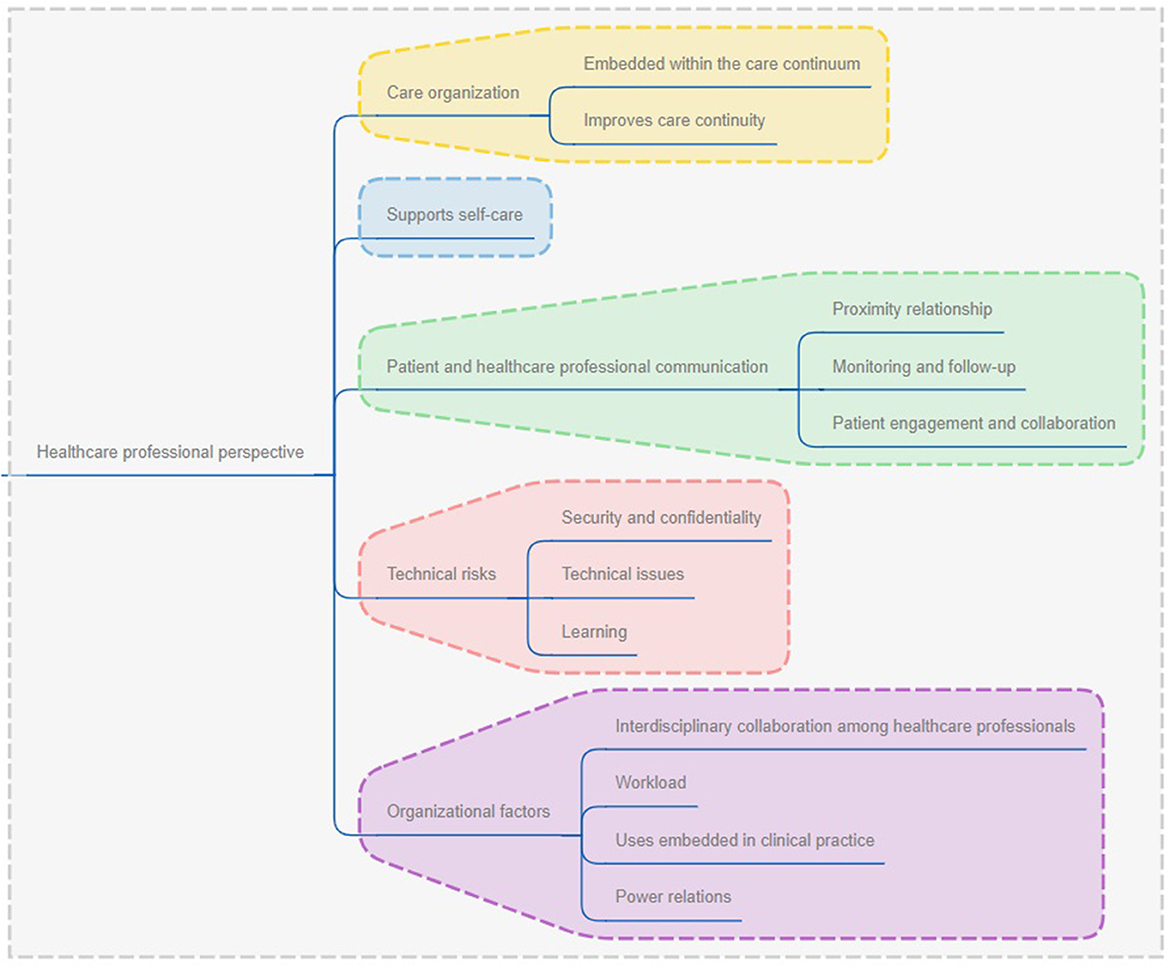
Figure 8. Factors of social acceptability for telemedicine from the perspective of healthcare providers.
Telemedicine, which is composed of diverse modes of virtual consultation through which healthcare service users can receive medical advice and treatment, is a powerful tool for better organization of care and mitigating challenges with care management. From all perspectives, one critical component that makes telemedicine acceptable is the necessity for it to improving access to care (Lamothe et al., 2013; Mathieu-Fritz and Esterle, 2013; Meyer et al., 2014; Durupt et al., 2016; Odnoletkova et al., 2016; Mathieu-Fritz, 2018; Habib et al., 2019). Its potential to connect healthcare service users that live far from care specialists (Durupt et al., 2016; Habib et al., 2019) and those who are unable to travel to a healthcare professional due to medical reasons (Mathieu-Fritz and Esterle, 2013; Odnoletkova et al., 2016), make it an attractive tool overall. Additionally, telemedicine also presents opportunities for mitigating shortages in medical professionals by allowing healthcare service users to consult with healthcare professionals that they would otherwise not be able to receive due to geographical constraints (Durupt et al., 2016).
One of the unique factors associated with telemedicine, which was viewed as a critical factor of acceptability, is its potential to connect healthcare service users and the care team along with healthcare professionals within the care team. The highly collaborative nature of the technology was viewed by healthcare service users and healthcare providers as an avenue for personalized knowledge exchange and even building health literacy of healthcare service users. For example, the results from Habib et al. (2019) demonstrate that telemedicine enable more efficient referral processes since different parts of the healthcare system can more easily connect, collaborate and exchange on care management options of healthcare service users.
While telemedicine presented as a positive solution, the studies revealed that factors associated with technical risks of the technology also influenced the choice to use it. Issues with the technological infrastructure and the unnatural aspects of telemedicine pose challenges to healthcare providers which may decide against using the technology. For example, healthcare professionals have noted issues with the sound and video quality (Mathieu-Fritz, 2018), challenges associated with getting used to new software and ways of working (Odnoletkova et al., 2016), and technology failures (Meyer et al., 2014) as all decreasing their willingness and commitment toward using the technology.
Finally, and unique to healthcare providers, are considerations for organizational effects of telemedicine. While being able to connect with members of the care team presented as an attractive organizational benefit of telemedicine (Habib et al., 2019), the associated increase in workload and procedural changes may also hinder its uptake. For example, Durupt et al. (2016) discussed how healthcare professionals needed significant amounts of time to learn and implement telemedicine, which, in turn, augmented workload. Procedurally, telemedicine also presented as a challenge since it requires that system administrators rethink diagnostic and patient intake mechanisms due to the virtual nature of consultations (Habib et al., 2019). For telemedicine to be attractive and implemented by healthcare professionals, organizational challenges should be mitigated to decrease the burden and difficulties that would otherwise fall on healthcare professionals and administrators.
Sensor-based and wearable technologies are technologies that offer the possibility for healthcare service users to monitor and record specific health metrics (Delbreil and Zvobgo, 2013; Houle et al., 2020).
Social acceptability of sensor and wearable technologies for francophone-speaking populations relies heavily on the capacity of the technology to monitor and detect a predetermined event or activity (Delbreil and Zvobgo, 2013; Houle et al., 2020). Specifically, when the technology demonstrated potential improvements to health and security, stakeholders were more likely to engage with them.
Social acceptability factors impacting use of sensor and wearable technologies are similar to all the previous technologies and dependent of the patient or healthcare professional perspective. From the patient perspective, sensor and wearable technologies are accepted if they enable more effective care organization, supports self-care, have limited technical risks and are accessible in terms of their cost (Figure 9). Similarly, for healthcare professionals, sensor and wearable technologies are accepted if they support care organization, supports patient self-care, account for technical challenges, and consider organizational factors (Figure 10).
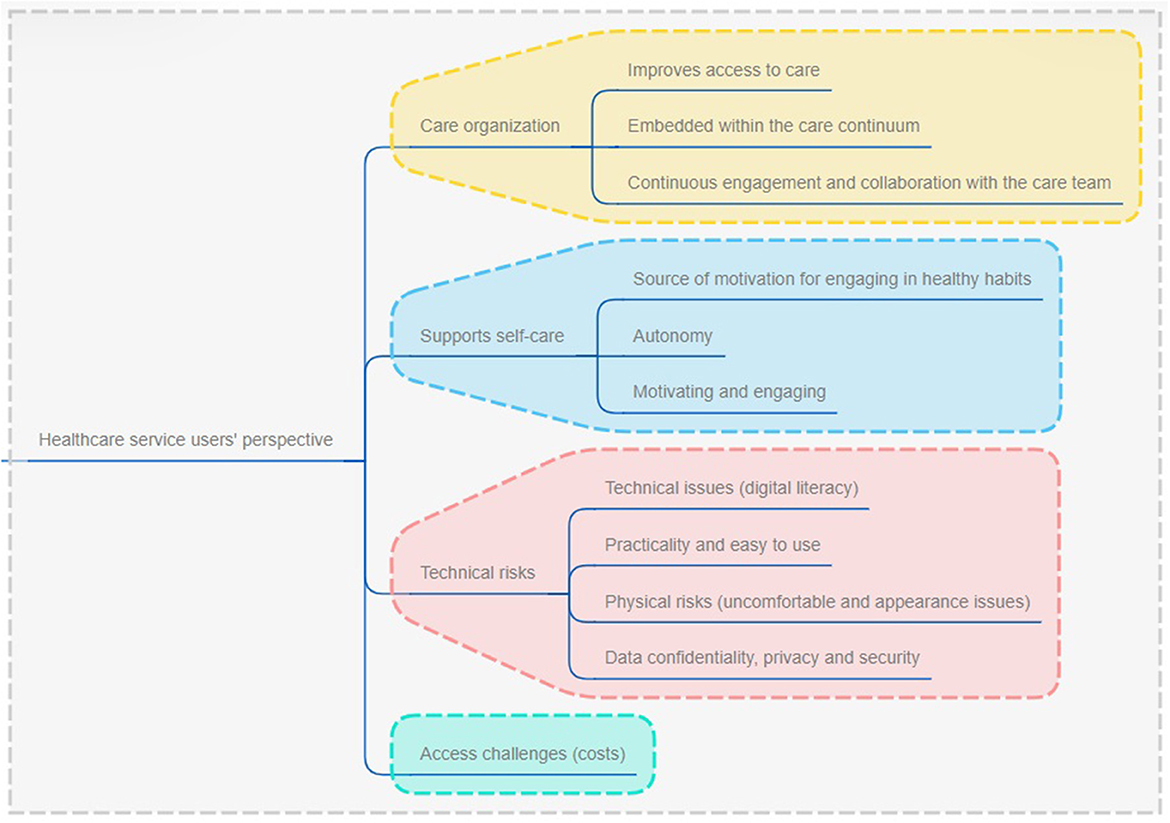
Figure 9. Factors of social acceptability for sensors and wearable technologies from the perspective of healthcare service users.
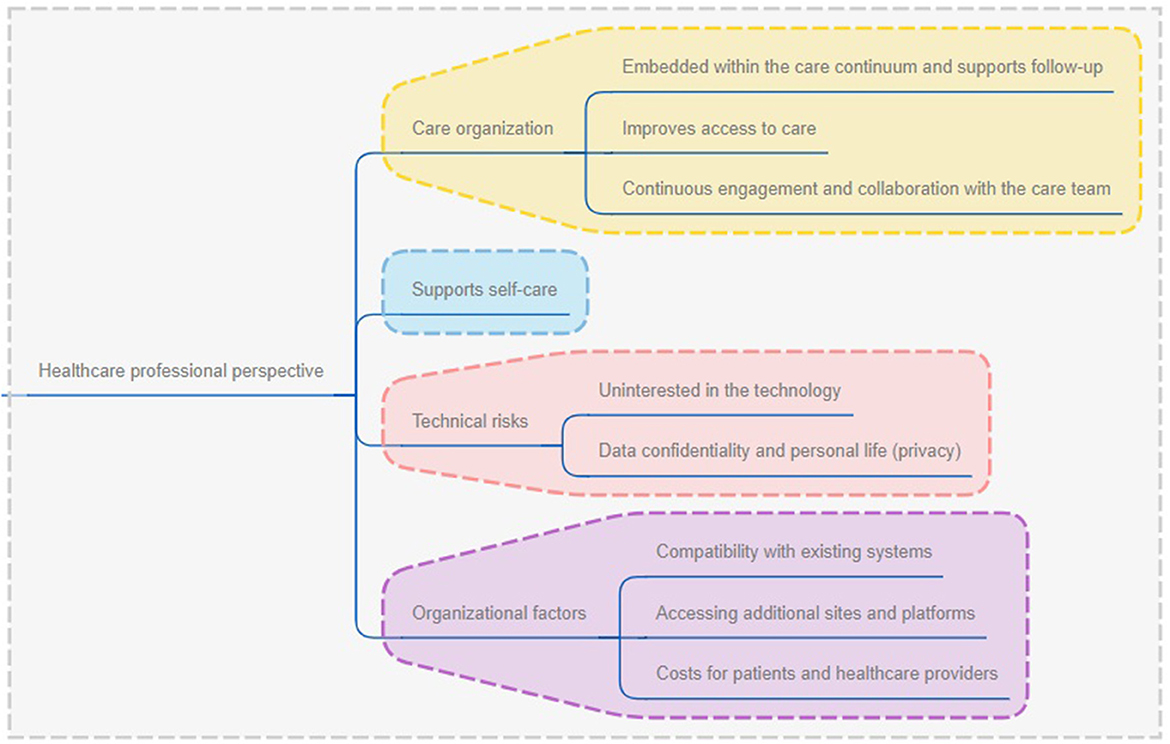
Figure 10. Factors of social acceptability for sensors and wearable technologies from the perspective of healthcare providers.
Improvements to care through better access and connectedness to healthcare professionals is a common factor of acceptability. As described in the study by Houle et al. (2020) wearing a technology facilitates easy and direct access to a healthcare professional, who can act as a source of motivation and take on an instructor role for the patient. Additionally, self-care is a common theme for both healthcare service users and healthcare professionals as both technologies allow the end users to remain autonomous, monitor their habits and motivate them to continue or enhance their efforts. As discussed in Delbreil and Zvobgo (2013), sensor technology supports autonomy and can enable the reduction of medication intake which are both seen to lead to positive health outcomes such as improved quality of life.
While the care organization and self-care are facilitating factors to the adoption of sensor and wearable technology, the technical risks were mentioned throughout as a major concern. For healthcare service users, dissatisfaction with the physical appearance and comfort of the technology, and issues with digital literacy were both barriers to using the technology. In the case of physical appearance and comfort for example, healthcare service users in Houle et al. (2020) pointed to challenges with wearing pedometers with different outfits such as dresses. Additionally, both healthcare professionals and healthcare service users in the study by Houle et al. (2020) mentioned some barriers with the use of the technology because “we (healthcare providers) have to think about teaching healthcare service users to use the technology, obviously, but sometimes we think it's easy for some of our staff, when in fact it can be a huge problem” (Houle et al., 2020, p. 8). Additionally, another major barrier for both healthcare service users and healthcare professionals is the concern for data confidentiality and privacy. The data gathered through the sensor and wearable technologies can easily be shared and may sometimes reveal confidential and sensitive data that healthcare service users may not want to share. As pointed out in the study by Houle et al. (2020), it is the online transmission of data by healthcare professionals that can lead to breaches in confidentiality. However, the results from Delbreil and Zvobgo (2013) point to a certain level of acceptance from end users on losing some privacy to the benefit of enhanced autonomy.
Healthcare professionals raised organizational barriers and opportunities as critical factors of sensor and wearable technology implementation and adoption. In the case of pedometers, these wearable devices are easy-to-use and highly compatible with existing systems (Houle et al., 2020). The compatibility of sensors, however, was not discussed. Often, sensor and wearable technologies must be used in conjunction with other platforms, such as an online web-based platforms, which can enhance the complexity if the platform isn't accessible or designed to meet accessibility standards for end-users. Additionally, having to conjoin technologies and platform can also complicate data exchange in instances where healthcare professionals need to access platforms that are secured or blocked. For example, a participant in the study by Houle et al. (2020) mentioned that “trying to access information, the websites can't be accessed, they're secure, so this complicates things too” (p. 8). Finally, another important barrier for both groups is the cost of sensor and wearable technologies. For healthcare service users, the cost of purchasing these technologies can represent significant amounts that are not realistic and within reach for many (Houle et al., 2020). Another cost-related issue concerns the necessary training and cost of training for healthcare professionals that need to become familiar and acquainted with the technology to integrate it within existing services (Houle et al., 2020).
The results of this study point to major factors of acceptability for francophone-speaking populations that are common across multiple digital health technologies. For both healthcare service users, caregivers and healthcare professionals/administrators, there is a common appreciation for technologies that can support care organization, enhance patient self-care, and mitigate and account for technical risks. For healthcare professionals and administrators specifically, acceptance of digital health technologies is also impacted by organizational factors whereby issues with compatibility, increased workload, resource requirement can deter their willingness to use digital health technologies while enhanced productivity, and collaboration and engagement opportunities will enhance willingness to implement them.
As was demonstrated in the results, healthcare professionals are usually wiling to implement and adhere to digital health technologies. However, considerations to the broader care environment, processes and systems in place can discourage them from engaging with them. The results pointed to significant differences between several types of digital health technologies in terms of organizational factors of acceptability. For mobile technologies, healthcare professionals valued their use for enhancing care management and facilitating the collection of data. However, for sensor and wearable technologies, there seem to be more concerns over their integration within the existing system. The difference in acceptability can be explained by looking at Roger's Diffusion of Innovation theory (Rogers, 2010). This theory clearly illustrates that a technology must pass through different phases of adoption until its use becomes widespread. While wearable technologies have been around for many years, their uptake may have been slower compared to that of mobile technologies, which can explain differences in acceptability. As noted in an article by Sultan (2015), wearable technologies present significant advantages for monitoring and the collection of data, but their implementation relies heavily on the uptake by end-users. With the results of this study pointing to concerns of healthcare providers in integrating wearable technologies within clinical practice, it can help to explain their slower uptake compared to mobile technologies. Telemedicine was also quite similar to mobile technologies in that healthcare professionals seemed to have less concerns over the organizational requirements for its implementation and use in clinical practice. The rapid adoption of telemedicine can likely be explained by its significant advantage and benefit for organizations, including on a clinical level. Telemedicine is attractive because it is known to improve access to care, decrease care costs, allow healthcare service users to be seen by the right healthcare professional more quickly, and even have positive impacts on patient satisfaction with care (Waller and Stotler, 2018). Contrarily, the studies focussed on robot technologies had very limited considerations for the organizational requirements associated with their use in healthcare. This could likely be explained by the technology's limited implementation in current environments and how its application to the healthcare context is newer. In this line of thought, we have confidence that the acceptability of digital health technologies is highly influenced by the stage at which the technology stands in the diffusion of innovation model, and also depends on the advantages it presents to the system, healthcare professionals, administrators, caregivers and francophone-speaking healthcare service users overall.
The technical risks associated with digital technologies is another major point of contention for technology acceptance. This consideration was found to be quite similar across all types of digital health technologies and from the perspective of healthcare service users and healthcare providers. Issues with accessibility and design, digital literacy, and data confidentiality and privacy are all well documented in the literature as being critical in technology adoption. Accessibility and design of health technologies can enhance the end-user's experience and likelihood to use a digital health technology. Common approaches to the design process include co-design and co-creation where the anticipated user of a technology becomes a critical player in the collective creation of the technology (Sanders and Stappers, 2008). As an expert on their own lived experiences, end-users can offer valuable insight to developers and therefore participate in the co-creation and co-design approach (Sanders and Stappers, 2008). Technology acceptability is also influenced by digital competence of end-users. Studies have shown that end-users, which include healthcare service users and healthcare providers, who build digital competence will be more likely to accept and use the technology for health and healthcare management purposes (Bosch et al., 2022; Le et al., 2023). Finally, data confidentiality and privacy concerns with regard to the implementation of digital health technologies were extremely important as an acceptability factor. Technologies that have the power to collect and share patient data to others may represent a threat to privacy. As discussed in a recent article, privacy concerns associated with the use of digital health technologies are cross cutting across several domains of data collection and dissemination (Grande et al., 2020). The unawareness and inaccurate data collection or unethical dissemination, which may compromise anonymity, are critical factors of privacy which may severely dimmish the willingness to use digital health technologies (Grande et al., 2020). These results, however, cannot be generalized to all groups since our results portray the willingness of caregivers to give up the privacy of their loved one if the use of digital health technologies ensured greater safety.
While this study allowed to discover factors influencing social acceptability of francophone-speaking populations for digital health technologies, we must consider these as intersecting with broader social determinants of health. For example, lower income, poor health status, and living in rural areas are few characteristics of francophones living in minority communities which research has shown to influence and reduce the likelihood for uptake of digital health technologies (Paré et al., 2017). A wider consideration for the context in which digital health technologies are used is critical in the analysis of their uptake and implementation (Terrade et al., 2009). Nonetheless, our results are transferable in the understanding of social acceptability among linguistically-diverse and culturally-diverse groups of the population because it sheds light on specific factors of social acceptability which may replicate among other groups of the population. If implemented appropriately and with consideration sociocultural factors and health equity, digital health technologies can go as far as improving care and reducing health disparities (Lawrence, 2022).
Several studies focus on digital health access and utilization among linguistically diverse populations living in minority contexts. In a recent qualitative systematic review on digital health for culturally and linguistically-diverse populations, the results align with the findings of this study pointing to the wide range of social acceptability factors modulating their use (Whitehead et al., 2023). For example, design components of digital health technologies were found to be extremely important in decisions to use them and reflect the need to include users in the development of such technologies (Whitehead et al., 2023). Additionally, specific research focussed on one group of the population and a single technology are not uncommon. In a study by Frey and Kerkemeyer (2022), the authors looked at the acceptance of therapists toward digital health applications. Findings of this study are aligned with our findings which consider the organizational requirements for deciding to use and implement a digital health technology. For example, if a technology is not implemented at the organization level and that there are uncertainties with risks and liability of its use, then there is a decreased likelihood for therapists to adhere and implement these tools in their practice (Frey and Kerkemeyer, 2022). Our study is unique from existing literature as it includes the perspectives of healthcare service users, healthcare professionals/administrators and caregivers, and it covers a wide range of digital health technologies.
This study has limitations that relate to the meta-ethnographic approach. First, our study had a sample size of 15 included articles. The literature points to diverging perspective in the number of studies that should compose a meta-ethnography, ranging between 2 and 77 articles (Soundy and Heneghan, 2022). While we were only able to retrieve 15 articles, this amount aligns with current trends in meta-ethnographies which an average of 17 studies (Soundy and Heneghan, 2022). Additionally, similar to qualitative studies, meta-ethnographies have been critiqued as being subjective in the synthesis phases (Sattar et al., 2021). To account for this, our approach followed the systematic approach described by Noblit and Hare (1999). Additionally, data analysis and interpretation stages were reviewed, discussed and validated among two members of the research team.
To conclude, factors of acceptability for francophone-speaking users of digital health technology cross multiple areas, mainly care organization, supporting patient self-care, enhancing communication with the care team, perceived technical and relational risks, organizational factors, and social and ethical values. Factors of acceptability can present as barriers or facilitators to use, and highly depend on the type of technology and whether the end-user is a patient or healthcare provider. This present work is critical to understand unique factors that would impact francophone-speaking communities in their decision to use digital health technologies. These findings can be applied in the design of digital health technologies and in their implementation among countries with francophone-speaking communities. In the future, it will be important for the healthcare professionals and decision-makers to consider the factors of social acceptability that are particular to linguistically diverse communities, such as francophones, to ensure implementation interventions with digital health technologies are effective in reaching those within these communities and generate better health outcomes and decreasing health disparities. Further research should expand on their value across diverse groups of francophone-speaking communities and within diverse cultural contexts to identify nuances that can be present within and across several types of technologies.
AG-B and SG contributed to conception and design of the study, analyzed the data, and wrote sections of the manuscript. AG-B conducted the searches, collected the data, screened the articles, and wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This study was funded under the International Francophonie Research Chair on Digital Health Technologies. The Chair aims to foster a better understanding of issues related to the use and design of digital health technologies, in light of the specific challenges that Francophones face.
We would like to acknowledge the support of the librarians from the University of Ottawa who contributed to the design of the search strategy for the identification of relevant articles. We would also like to thank Catarina Silva who supported preliminary stages of data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2023.1230015/full#supplementary-material
Anwar, F., and Shamim, A. (2011). Barriers in adoption of health information technology in developing societies. Int. J. Adv. Comput. Sci. Applic. 2, 8. doi: 10.14569/IJACSA.2011.020808
Ashcroft, R., Dahrouge, S., Lam, S., and Saluja, K. (2021). Patient's Experiences with Telephone and Video Appointments in Primary Care during COVID-19 Pandemic. Univeristy of Toronto and Bruyère 32. Available online at: https://tspace.library.utoronto.ca/bitstream/1807/126226/1/OH%20Report_Ashcroft_Dahrouge%20%282021-Nov-29%29_FINAL.pdf (accessed September 11, 2023).
Astell, A. J. (2019). Technology and dementia: the future is now. Dementia Geriatr. Cogn. Disor. 47, 131–139. doi: 10.1159/000497800
Awad, A., Trenfield, S. J., Pollard, T. D., Ong, J. J., Elbadawi, M., McCoubrey, L. E., et al. (2021). Connected healthcare: Improving patient care using digital health technologies. Adv. Drug Deliv. Rev. 178, 113958. doi: 10.1016/j.addr.2021.113958
Balcombe, L., and Leo, D. D. (2021). Digital mental health challenges and the horizon ahead for solutions. JMIR Mental Health 8, e26811. doi: 10.2196/26811
Bosch, J., Ludwig, C., Fluch-Niebuhr, J., and Stoevesandt, D. (2022). Empowerment for the Digital Transformation: Results of a Structured Blended-Learning On-the-Job Training for Practicing Physicians in Germany. Int. J. Environ. Res. Public Health 19, 12991. doi: 10.3390/ijerph192012991
Cases, A.-S. (2017). L'e-santé: l'empowerment du patient connecté. J. de gestion et d'économie Méd. 35, 137–158. doi: 10.3917/jgem.174.0137
Craig, S., Shen, A., Wallis, K., Ortiz, P., Pak-Gorestein, S., Yun, K., et al (2021). Addressing Language Barriers to Digital Health Equity. Penn LDI, 27 May. Available online at: https://ldi.upenn.edu/our-work/research-updates/how-health-systems-can-help-address-language-barriers-to-achieve-digital-health-equity/ (accessed July 25, 2023).
Davis, F. D. (1989). Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Quart. 13, 319–340. doi: 10.2307/249008
Delbreil, E., and Zvobgo, G. (2013). Wireless sensor technology in dementia care: Caregiver perceptions, technology take-up and business model innovation. EuroMed J. Bus. 8, 79–97. doi: 10.1108/EMJB-05-2013-0019
Durupt, M., Bouchy, O., Christophe, S., Kivits, J., and Boivin, J.-M. (2016). La télémédecine en zones rurales : représentations et expériences de médecins généralistes'. Santé Publique 28, 487–497. doi: 10.3917/spub.164.0487
Frey, S., and Kerkemeyer, L. (2022). Acceptance of digital health applications in non-pharmacological therapies in German statutory healthcare system: Results of an online survey. Digital Health 8, 20552076221131144. doi: 10.1177/20552076221131142
Ghandour, E. K., Gagnon, M.-P., and Fortin, J.-P. (2018). Conditions d'adoption du dossier de santé électronique personnel par les professionnels de la première ligne au Québec : perspectives professionnelle et organisationnelle:. Santé Publique 29, 837–850. doi: 10.3917/spub.176.0837
Grande, D., Marti, X. L., Feuerstein-Simon, R., Merchant, R. M., Asch, D. A., Lewson, A., et al. (2020). Health policy and privacy challenges associated with digital technology. JAMA Netw. Open, 3, e208285. doi: 10.1001/jamanetworkopen.2020.8285
Habib, J., Yatim, F., and Sebai, J. (2019). Analyse des facteurs influençant l'émergence des pratiques de télémédecine : le cas des Maisons de Santé en France. Syst. d'inform. Manag. 24, 47–85. doi: 10.3917/sim.191.0047
Houle, J., Gallani, M.-C., Pettigrew, M., Laflamme, G., Mathieu, L., Boudreau, F., et al. (2020). Acceptability of a computer-tailored and pedometer-based socio-cognitive intervention in a secondary coronary heart disease prevention program: A qualitative study. Digital Health 6, 205520761989984. doi: 10.1177/2055207619899840
Javaid, M., Haleem, A., Singh, R. P., and Suman, R. (2022). “Health care digital revolution during COVID-19,” in R. Anandan et al. (eds) How COVID-19 is Accelerating the Digital Revolution: Challenges and Opportunities (Cham: Springer International Publishing) 17–30. doi: 10.1007/978-3-030-98167-9_2
Kontos, E., Blake, K. D., Chou, W.-Y. S., and Prestin, A. (2014). Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J. Med. Internet Res. 16, e3117. doi: 10.2196/jmir.3117
Lamothe, L., Paquette, M.-A., Fortin, J.-P., Labbé, F., Messikhs, D., and Duplantie, J. (2013). L'utilisation des télésoins à domicile pour un meilleur suivi des maladies chroniques. Santé Publique 25, 203. doi: 10.3917/spub.132.0203
Lawrence, K. (2022). “Digital Health Equity,” in S. L. Linwood (ed.) Digital Health. Brisbane (AU): Exon Publications. Available online at: http://www.ncbi.nlm.nih.gov/books/NBK580635/ (accessed July 20, 2023).
Le, T. V., Galperin, H., and Traube, D. (2023). The impact of digital competence on telehealth utilization. Health Policy Technol. 12, 100724. doi: 10.1016/j.hlpt.2023.100724
Lessard, D., Aslan, A., Zeggagh, J., Morel, S., Michels, D., and Lebouché, B. (2019). Acceptability of a digital patient notification and linkage-to-care tool for French PrEPers (WeFLASH ©): Key stakeholders' perspectives. Int. J. STD AIDS 30, 1397–1407. doi: 10.1177/0956462419878043
Luborsky, M. R. (1993). Sociocultural factors shaping technology usage. Technol. Disab. 2, 71–78. doi: 10.3233/TAD-1993-2110
Mathieu-Fritz, A. (2018). Les téléconsultations en santé mentale: Ou comment établir la relation psychothérapeutique à distance. Réseaux 207, 123–164. doi: 10.3917/res.207.0123
Mathieu-Fritz, A., and Esterle, L. (2013). Les transformations des pratiques professionnelles lors des téléconsultations médicales: Coopération interprofessionnelle et délégation des tâches. Rev. française de Sociol. 54, 303–329. doi: 10.3917/rfs.542.0303
Mayères, A. (2017). “L'e-santé et la question des inégalités sociales de santé,” in Les inégalités sociales de santé: Actes du séminaire de recherche de la DREES 2015-2016, 294. Available online at: https://drees.solidarites-sante.gouv.fr/sites/default/files/2021-01/ouvrage_actes_seminaire_iss_pour_bat_cabinet_-_web.pdf (accessed September 11, 2023).
Meyer, J., Paré, G., Trudel, M., and Têtu, B. (2014). Télémédecine et accessibilité aux soins de santé spécialisés en régions éloignées'. Gestion. 39, 29–37. doi: 10.3917/riges.393.0029
Milani, R. V., Bober, R. M., and Lavie, C. J. (2016). The role of technology in chronic disease care. Progr. Cardiov. Dis. 58, 579–583. doi: 10.1016/j.pcad.2016.01.001
Nadal, C., Sas, C., and Doherty, G. (2020). Technology acceptance in mobile health: scoping review of definitions, models, and measurement. J. Med. Internet Res. 22, e17256. doi: 10.2196/17256
Noblit, G. W., and Hare, R. D. (1999). Chapter 5: meta-ethnography: synthesizing qualitative studies. Counterpoints 44, 93–123.
Norgaard, O., Furstrand, D., Klokker, L., Karnoe, A., Batterham, R., Kayser, L., et al. (2015). The e-health literacy framework: A conceptual framework for characterizing e-health users and their interaction with e-health systems. Knowl. Manage. E-Learn, 7, 522–540. doi: 10.34105/j.kmel.2015.07.035
Nouri, S. S., Adler-Milstein, J., Thao, C., Acharya, P., Barr-Walker, J., Sarkar, U., et al. (2020). Patient characteristics associated with objective measures of digital health tool use in the United States: A literature review. J. Am. Med. Inf. Assoc. 27, 834–841. doi: 10.1093/jamia/ocaa024
Odnoletkova, I., Buysse, H., Nobels, F., Goderis, G., Aertgeerts, B., Annemans, L., et al. (2016). Patient and provider acceptance of telecoaching in type 2 diabetes: a mixed-method study embedded in a randomised clinical trial. BMC Med. Inf. Decis. Mak. 16, 142. doi: 10.1186/s12911-016-0383-3
Paré, G., Leaver, C., and Bourget, C. (2017). Diffusion of smart devices for health in Canada. J. Med. Internet Res. 20, e177. doi: 10.2196/jmir.9388
Perski, O., and Short, C. E. (2021). Acceptability of digital health interventions: embracing the complexity. Transl. Behav. Med. 11, 1473–1480. doi: 10.1093/tbm/ibab048
Pino, M., Boulay, M., Jouen, F., and Rigaud, A.-S. (2015). “Are we ready for robots that care for us?” Attitudes and opinions of older adults toward socially assistive robots. Front. Aging Neurosci. 7, 141. doi: 10.3389/fnagi.2015.00141
Rodriguez, J. A., Shachar, C., and Bates, D. W. (2022). Digital inclusion as health care — supporting health care equity with digital-infrastructure initiatives. New Engl. J. Med. 386, 1101–1103. doi: 10.1056/NEJMp2115646
Sanders, E. B.-N., and Stappers, P. J. (2008). Co-creation and the new landscapes of design. CoDesign 4, 5–18. doi: 10.1080/15710880701875068
Sattar, R., Lawton, R., Panagioti, M., and Johnson, J. (2021). Meta-ethnography in healthcare research: a guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv. Res. 21, 50. doi: 10.1186/s12913-020-06049-w
Sewitch, M. J., Fallone, C. A., Ghali, P., and Lee, G. E. (2019). What patients want in a smartphone app that supports colonoscopy preparation: qualitative study to inform a user-centered smartphone A JMIR mHealth uHealth, 7, e12242. doi: 10.2196/12242
Sharma, A., Harrington, R. A., McClellan, M. B., Turakhia, M. P., Eapen, Z. J., Steinhubl, S., et al. (2018). Using digital health technology to better generate evidence and deliver evidence-based care. J. Am. College Cardiol. 71, 2680–2690. doi: 10.1016/j.jacc.2018.03.523
Soundy, A., and Heneghan, N. R. (2022). Meta-ethnography. Int. Rev. Sport Exerc. Psychol. 15, 266–286. doi: 10.1080/1750984X.2021.1966822
Sultan, N. (2015). Reflective thoughts on the potential and challenges of wearable technology for healthcare provision and medical education. Int. J. Inf. Manag. 35, 521–526. doi: 10.1016/j.ijinfomgt.2015.04.010
Terrade, F., Pasquier, H., Juliette, R., and Guingouain, G. (2009). L'acceptabilité sociale: la prise en compte des déterminants sociaux dans l'analyse de l'acceptabilité des systèmes technologiques. Le Travail Humain 72, 383–395. doi: 10.3917/th.724.0383
Waller, M., and Stotler, C. (2018). Telemedicine: a primer. Curr. Aller. Asthma Rep. 18, 54. doi: 10.1007/s11882-018-0808-4
Weiss, D., Rydland, H. T., Øversveen, E., Jensen, M. R., Solhaug, S., and Krokstad, S. (2018). Innovative technologies and social inequalities in health: A scoping review of the literature. PLoS ONE 13, e0195447. doi: 10.1371/journal.pone.0195447
Whitehead, L., Talevski, J., Fatehi, F., and Beauchamp, A. (2023). Barriers to and facilitators of digital health among culturally and linguistically diverse populations: qualitative systematic review. J. Med. Internet Res. 25, e42719. doi: 10.2196/42719
Wilson, J., Heinsch, M., Betts, D., Booth, D., and Kay-Lambkin, F. (2021). Barriers and facilitators to the use of e-health by older adults: a scoping review. BMC Public Health 21, 1556. doi: 10.1186/s12889-021-11623-w
Woodward-Kron, R., Bresin, A., Hajek, J., Parker, A., Phan, T. D., Hughson, J., et al. (2019). “Improving access to and participation in medical research for culturally and linguistically diverse background patients: A bilingual, digital communication approach,” in Cross-Cultural Health Translation, ed. M., Ji (London: Routledge) 117–130. doi: 10.4324/9780429054402-8
World Health Organization (2021). Global strategy on digital health 2020-2025. Geneva: WHO. Available online at: https://apps.who.int/iris/bitstream/handle/10665/344249/9789240020924-eng.pdf (accessed July 20, 2023).
World Health Organization (2023). Digital health. Available online at: https://www.who.int/health-topics/digital-health (accessed September 11, 2023).
Keywords: digital health technologies, social acceptability, francophone, meta-ethnography, sociocultural diversity
Citation: Gauthier-Beaupré A and Grosjean S (2023) Understanding acceptability of digital health technologies among francophone-speaking communities across the world: a meta-ethnographic study. Front. Commun. 8:1230015. doi: 10.3389/fcomm.2023.1230015
Received: 27 May 2023; Accepted: 31 August 2023;
Published: 21 September 2023.
Edited by:
Ashok Kumbamu, Mayo Clinic, United StatesReviewed by:
Rachael Dix, Centro de innovación social y urbana del municipio de Valencia - Las Naves, SpainCopyright © 2023 Gauthier-Beaupré and Grosjean. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sylvie Grosjean, c3lsdmllLmdyb3NqZWFuQHVvdHRhd2EuY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.