
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Commun. , 06 December 2023
Sec. Language Communication
Volume 8 - 2023 | https://doi.org/10.3389/fcomm.2023.1221149
This article is part of the Research Topic Digital Participation and Communication Disorders across the Lifespan View all 15 articles
Background: Individuals with chronic traumatic brain injury (TBI) are often affected by communication disorders which might have an impact on their social participation. Due to possible cognitive and communicative disabilities, as well as impairments of social cognitive skills, individuals with TBI have been observed to exhibit difficulties in maintaining and establishing social relationships, resulting in a greater risk of social isolation. This applies to both in-person as well as computer-mediated communication (CMC), which is considered an integral part of everyday life. Research on digital participation in the TBI population has focused on the possible challenges and barriers, but also on the benefits of CMC for social interactions. Guidelines from professional societies recommend questionnaires and checklists for assessing restrictions of communicative participation (e.g., ASHA, INCOG). However, there is no overview of whether the available instruments can capture digital aspects of participation or social media use in TBI.
Aim: In this scoping review, following the PRISMA criteria, we aimed to provide an overview over currently available instruments that help assess CMC use as a measure of digital participation in the TBI population.
Method: The databases Web of Science Core Collection, Ovid, PsycInfo and Psyndex were screened for publications between the years 2013 and 2023 with relevant search terms referring to social participation, assessment tools, CMC and the target group, in order to find suitable tools to assess digital participation in individuals with TBI. In a multistage selection process following the PRISMA criteria, the instruments found were examined in terms of items that assess digital participation. The outcome of the review is an overview of the status quo of potentially available instruments that capture aspects of CMC.
Results: Following a screening on title/abstract and full-text level, a total of 10 studies could be identified that present assessment tools that evaluate CMC use as a measure of digital participation in the TBI population. Said studies were analyzed and compared in terms of content according to the selected parameters.
Conclusion: Digital participation is an important aspect of everyday lives for individuals with TBI. Therefore, CMC should be an integral part of rehabilitation. The existing appropriate questionnaires uncovered in the current study should therefore be applied routinely to detect impairments in CMC and digital participation. Overall, however, there is still a great need for research in the field of CMC, both regarding methods for measuring digital participation disorders as well as resources.
Systematic Review Registration: https://www.germanistik.uni-muenchen.de/forschung/proj_gl/review_participation_tbi.pdf.
Traumatic brain injuries (TBI) are one of the most common neurological causes of disability and limitations in participation and quality of life (QoL) across all ages (McDonald et al., 2014; Anderson et al., 2019). TBIs can be caused by a bump, blow, or jolt to the head or a penetrating injury to the head, disrupting normal brain function (Marr and Coronado, 2004). Based on the affected person's clinically presented neurological symptoms, the severity of a TBI can be classified as mild, moderate, or severe (Centers for Disease Control and Prevention, 2015). Injuries resulting from trauma to the head can include focal lesions as well as diffuse damage such as axonal damage. In particular, areas of the frontal brain and temporal lobe (fronto-temporal regions) are often affected, with damage to various areas and functional circuits relevant to communication (Rosenthal and Hillis, 2012).
Due to the wide-ranging brain areas that can be affected, TBI can have an impact on several cognitive domains which in turn influence communication outcome (MacDonald, 2017). Among the most common consequences are impairments in processing speed, concentration, orientation, memory and working memory, attention, organization, reasoning, problem solving and social cognition (Salmond et al., 2005; Stocchetti and Zanier, 2016; MacDonald, 2017). Changes in cognition and communication have an impact on social participation, with studies reporting correlations between cognitive disturbances and decreased life satisfaction and social and communicative complications (Kilov et al., 2009). Individuals with TBI are reported to have fewer social contacts and difficulties in building or maintaining social relations, and to be at higher risk of experiencing social isolation (Brunner et al., 2015; Stocchetti and Zanier, 2016; Morrow et al., 2021b).
The combination of linguistic and cognitive deficits in TBI was described using the term “cognitive communication disorders (CCD)” (Togher et al., 2014). CCD refers to communication disorders in patients with neurological disorders who show impairments in both cognitive abilities (such as attention, memory, planning ability) and in processing language under various contextual conditions (American Speech-Language-Hearing Association, 2003; Christman Buckingham and Sneed, 2018; Büttner-Kunert et al., 2022). The main impairments in CCD are in the structuring and organization of communication processes, with cognitive, linguistic, and behavioral dysfunctions coinciding (Togher et al., 2014; MacDonald, 2017). Basal linguistic functions, such as phonological, semantic, or grammatical skills at word and sentence level usually appear preserved (McDonald et al., 2014; Togher et al., 2014).
Individuals with CCD have difficulties in understanding and producing conversations as well as written texts (Büttner, 2016; MacDonald, 2017). They find it difficult to understand information that goes beyond the content of individual sentences. They display problems in structuring content according to its relevance (Bootsma et al., 2021), to stay on topic, and to include the perspective of their dialog partners. CCD can be seen in a lack of a common thread, as well as in difficulties in “getting to the point” and “striking the right tone” (Togher et al., 2004; Gindri et al., 2014; Dromer et al., 2021; Büttner-Kunert et al., 2022; Elbourn et al., 2022). This is aggravated by the fact that individuals with CCD do not always fully perceive their communicative limitations and incoherence because they often lack the awareness for it (Büttner and Glindemann, 2019; Büttner-Kunert et al., 2021). Because of the described disturbances in the cognitive-linguistic interaction, CCDs therefore have a clear negative influence on the ability to act appropriately in different communication contexts. Therefore, CCD also constitutes a prototype of acquired “neuropragmatic disorders” (Bambini and Bara, 2012; Cummings, 2014; Bischetti et al., 2022).
After a TBI, heterogeneous changes in discourse behavior can occur, which have in common that people with TBI cannot attend to the communicative needs of their conversational partner. This can manifest itself in a tangential monolog-like discourse behavior or in the tendency to interrupt the interlocutor (e.g., in the presence of an impulse control disorder) or also in a very impoverished conversational behavior with few relevant utterances (Sim et al., 2013; Norman et al., 2022).
The limitations of a TBI affect not only in-person communicative situations, but also digital forms of communication and information processing (Flynn et al., 2019). Therefore, individuals with TBI belong to the population groups that are vulnerable to the “digital divide” (Duplaga, 2017). The term “digital divide” describes the differences in access to and use of information and communication technologies, especially the Internet, between different population groups that result from technical, socioeconomic and individual factors (Rogers, 2001). The digital divide was described on different levels: general access to the necessary technologies (first level), inequalities in actual use (e.g., scope, variety, and type of use) (second level), and inequalities in the utility gained (third level), i.e., how individuals benefit from participating in the digital world (Chuah et al., 2022).
Given the ongoing trend of increased digitalization in society, it may be expected that challenges in the context of digital participation in TBI will gain relevance. Therefore, the need for information regarding methods to measure digital participation will become even more important for speech and language therapy and for neurorehabilitation in general. In this context, it is important to consider that methods for surveying digital participation should also take into account different levels of the digital divide and also take into account the levels of participation as well as the level of activities within the framework of the International Classification of Functioning, Disability and Health (ICF) (WHO, 2021). In this article, we focus primarily on the type of digital divide that manifests itself through differences in the “use” of computers and the internet (van Deursen and van Dijk, 2014). This so-called second-level digital divide (van Deursen and van Dijk, 2014; Cornejo Müller et al., 2020) is operationalized in this review as the use of CMC.
Under the ICF framework, communication disorders in individuals with TBI can be classified as impairment of body functions (b164: higher cognitive performance, b1670-b1679: cognitive linguistic functions), and impairment of participation (e.g., d350-d369: conversation and use of communication devices and techniques) (Rehadat, 2023). In particular, impairments in participation are considered to be pragmatic-communicative impairments at the level of interpersonal relationships and interactions (d730-d799) and significant life domains such as work, employment, or economic life (d810-d899) (Achhammer et al., 2016; Büttner-Kunert et al., 2022). Impairments in communicative abilities affect activity and participation depending on person- and environment-related contextual factors. Based on the rationale of the ICF, diagnostic approaches for the assessment of the level of participation have to be an integral part of the rehabilitation of people with TBI. Knowledge about such procedures is therefore essential to make the barriers and resources for successful communication more visible.
For the population of individuals with TBI, participation through digital means has been explored under the term of computer-mediated communication (CMC). This term refers to all types of communicative interactions conveyed by electronic devices such as smartphones, laptops or tablets (Flynn et al., 2019). The mediated information can be based on text, audios or videos, which are often used in order to establish or maintain social relationships or exchange information in personal or professional contexts (Flynn et al., 2019; Morrow et al., 2021b). One of the most predominant forms of CMC is social media, especially social networking sites (e.g., Facebook, Twitter), blogs (e.g., Tumblr) or online content communities (e.g., Youtube) (Baker-Sparr et al., 2018). Social media are characterized by user-generated content, that is to say, content is created by an interactive exchange of users for the purpose of sharing personal or non-personal information and providing feedback on other users' content (Kaplan and Haenlein, 2010; Brunner et al., 2015; Meshi et al., 2015; Baker-Sparr et al., 2018).
Social media use has strongly increased in recent years and can now be considered an “integral part of society” (Brunner et al., 2015). For example, more than 3 billion people world-wide use the most popular social media platforms Facebook, Twitter, and Instagram (Greenwood et al., 2016). The majority of users of social networking sites are adolescents and young adults between 14 and 25 years of age (Gupta and Bashir, 2018), but social networking is common among all age groups (Australian Communications and Media Authority, 2013). According to the most recent statistics of Eurostat (2023), the use of social media is very high among younger people: “Among younger people in the EU aged 16–24 years, almost 9 in every 10 participated in social networks (87%). This share ranged from 79% in Italy to 97% in Denmark” (Eurostat, 2021).
Social media and other forms of CMC have radically influenced the quality and nature of social relationships and communication (Baker-Sparr et al., 2018; Morrow et al., 2021b). As opposed to face-to-face communication, CMC connects communication partners independent of their geographical location, which is especially beneficial for individuals living in areas with low infrastructure or with restricted mobility (e.g., physical disabilities). The computer-mediated exchange can be partly asynchronous, which eliminates time constraints while planning and composing messages (e.g., e-mailing). CMC often provides fewer or no non- and paraverbal information (e.g., text messages), which leads to an emphasis of verbal content (Flynn et al., 2019).
In contrast to CMC and e-services, which mean a broad range of self-served technologies used by the general public, the term assistive technology refers to means that are specifically targeted toward individuals with cognitive or other impairments (Evald, 2015; Eghdam et al., 2016; Chuah et al., 2022). Building on the possibilities and challenges of technology use in patient populations such as the TBI population, there have been considerations about which tools can be utilized for therapy interventions or rehabilitation (Wong et al., 2017). The most common devices explored in this context are smartphones, mobile phones, tablets, computers, and, less commonly, pagers, voice recorders or personal digital assistants (Evald, 2015; Wong et al., 2017). Smartphones in particular, being in the possession of almost two thirds of the inhabitants in developed countries like the UK, have potential as an important kind of assistive technology, including benefits of mobility, portability and widespread use (Wong et al., 2017). The functions of smartphones, such as the use of active visual and auditory reminders, have been used in the context of memory impairment in TBI (Evald, 2015). Assistive technologies have been actively applied in internet-mediated rehabilitation, whose relevance has drastically increased during the pandemic years. According to a definition by Ownsworth et al. (2018), telerehabilitation refers to any kind of rehabilitation method which makes use of communication technologies over distance, such as phone-calls, messaging, or multimodal systems like video-calls and interactive web-platforms. Telerehabilitation comprises online measures (e.g., therapy sessions on a video call) or offline measures (e.g., self-reliant exercises on a web-based platform).
As opposed to in-person communication, CMC has been suggested to alleviate the communicative and social consequences of TBI (Baker-Sparr et al., 2018). A relevant observation here is that regular internet use is almost as common in individuals with TBI than in non-injured peers (Eghdam et al., 2016), and smartphones are used in comparable percentages as in non-injured peers (Baker-Sparr et al., 2018).
An advantageous aspect of CMC for individuals with TBI is that there is a variety of communication forms in synchronous and asynchronous formats available, relying to a different degree on written language, visual or auditory modalities (e.g., posting content on a blog, video-call via Skype). As a possible adaptive skill, users may choose the channel that meets their communicative needs best (Brunner et al., 2015). Consequently, individuals with TBI can “engage in social interactions on their own terms” (Tsaousides et al., 2011).
Certain communicative aspects of CMC may be especially advantageous for individuals with TBI as opposed to face-to-face interactions. For instance, some CMC formats like messaging rely on short written messages with little demand concerning correct spelling and grammar. This might lower the threshold to participate via technology for individuals for whom literacy is challenging. Also, written messages in asynchronous communication formats cause the interaction to be less constrained by time pressure and potentially less dependent on visual social cues (Brunner et al., 2015). The latter aspect might be especially relevant to individuals with TBI who have difficulties in interpreting social signals (Morrow et al., 2021b).
Summarizing the results from 16 studies, Brunner et al. (2015) reported that the social media use of individuals with TBI did not differ qualitatively from non-injured peers concerning the main purpose, which was maintaining social contact with friends and relatives. There is strong evidence that technology-based social media support can reduce both the physical and psychological burdens of loneliness (Morrow et al., 2021b).
However, cognitive communication disorders in TBI might impact CMC use and digital participation beyond already present challenges in real-life social interactions. In particular, participants with moderate and severe forms of TBI have been reported to use the internet or social media less frequently than peers (Brunner et al., 2015; Morrow et al., 2021b). Next to the severity of injury, some demographic factors were held responsible for less frequent use of social media, such as older age, lower income and rural residence (Baker-Sparr et al., 2018).
Additionally, person-related factors such as “low levels of skill, confidence, knowledge, and interest” (Chuah et al., 2022) were discussed to account for lower rates of internet or social media use in TBI. Both cognitive and communicative abilities can have an impact on CMC and digital participation. The successful use of CMC requires the general access and ability to utilize devices, for instance fine-motor skills and high-level cognitive functions like working memory, selective attention and self-regulation (Flynn et al., 2019). On the user level, CMC poses additional requirements as opposed to face-to-face interactions. The accessibility of internet services and websites requires the processing of complex visual stimuli, which might represent a challenge for individuals with visual or text processing impairments (Robertson and Schmitter-Edgecombe, 2017; Ketchum et al., 2020; Brunner et al., 2022). Constantly changing content (especially on social media sites) can be especially demanding in the presence of memory or learning impairments. Attention deficits make it difficult to filter out relevant information (Morrow et al., 2021b). Synchronous formats like live-chatting might pose higher time-constraints on the individuals than asynchronous formats like posting content on a social media site.
CMC in TBI also poses specific demands on social cognitive skills. Many forms of social communication require the abstraction from literal meaning and social inferencing (Morrow et al., 2021b). As opposed to face-to-face interactions, some forms of CMC (f. e. messaging) focus verbal content only, without providing additional paraverbal or non-verbal information. This increases the need of text processing and inferencing skills and might potentially contribute to miscommunications, as reported by participants in the study of Morrow et al. (2021a). Other forms of CMC (f. e. video calls), by contrast, require the ability of processing social signals like gestures or facial expressions, similarly to in-person interactions. As social cognition deficits are a common sequelae of TBI, this makes those formats potentially demanding for individuals concerned (Morrow et al., 2021b).
Overall, CMC has been discussed to have both facilitating and hindering aspects as compared to in-person interactions. It is not yet clear how these factors apply to the heterogeneous population of TBI, with individuals varying in injury-related characteristics and person-related features. Next to more general information about the frequency of use of different devices and internet-based applications, there is a need to evaluate the quality and effectiveness of CMC in the TBI population, and how user profiles change in the presence of cognitive and communicative impairments (Flynn et al., 2019). A deeper understanding on the actual benefits and challenges of CMC, as well as the development and use of adaptive strategies, are beneficial resources to improve digital participation within TBI (Morrow et al., 2021b). Based on this information, adaptive strategies like “how to use social media and how to stay safe” or “using techniques that support recall and retention” (Brunner et al., 2022) could be implemented in rehabilitation in the long-term.
The aim of this scoping review is to provide an overview of currently available instruments that help to assess CMC use in adults with TBI of all degrees of severity. We assume that an increased quantity or quality of CMC use indicates a higher degree of digital participation, that is, individuals make use of CMC to interact and be involved in social interactions via digital means. This could also be associated with a higher real-world participation, but could also compensate for a lack of real-world social interactions (Ketchum et al., 2020). The instruments found in the review process will then be presented in their construction and objectives and evaluated in terms of their potential and limitations. Finally, recommendations for the assessment of CMC will be given and research gaps in this field will be identified.
Since the aim of this study was first to obtain an overview of the instruments available that capture CMC, the method chosen was a scoping review. Scoping reviews provide an impression of the state of the research literature on a particular topic. In contrast to systematic reviews, scoping reviews give an overview of existing evidence without assessing the methodological quality of the included studies (Elm et al., 2019). We used the PRISMA extension for scoping reviews (PRISMA-ScR) to report our results (Tricco et al., 2018). The PRISMA-ScR data sheet is provided in the Appendix.
Prior to conducting the scoping review, a search of relevant databases was executed to examine the availability of existing and comparable reviews on the topic. In the Cochrane database and the ClinicalTrials.gov database, no reviews were found that dealt with available instruments and questionnaires for the survey of digital participation in the target TBI population. Reviews that are related in content, e.g., the review by Brunner et al. (2015), emphasize the relevance of CMC for the participation of people with TBI, but do not provide an overview of concrete instruments.
The literature search was conducted in four different databases during the period of 2023-01-16 and 2023-02-03. The databases used were Web of Science Core Collection, Ovid, PsycInfo and Psyndex. The arrangement of the keywords was discussed by the authors and finally combined with the Boolean operators in the following manner: “traumatic brain injury” OR “head injury” OR “brain injury” OR “tbi” AND “chat” OR “social media” OR “digital participation” OR “computer mediated communication” OR “computer-mediated communication” OR “internet use” OR “messenger” AND “assessment” OR “screening” OR “survey” OR “questionnaire”. The search strategy was performed on the title, the publication date of the literature was restricted from 2010-01-31 to 2023-01-31. We chose a time period comparable to a previous scoping review by this group of authors (Falkowska et al., 2021), covering the period from 2010 to 2023. Depending on the database, the results were either filtered by adulthood or filtered manually according to the age group. While we mainly targeted adult participants, we also decided to consider older adolescents. That means we also considered studies that enrolled individuals from 18 to 21 years of age.
The first study selection process was conducted with the Rayyan program (Ouzzani et al., 2016). After deleting the duplicates, the titles and abstracts of 1,558 articles were evaluated for relevance. Each article was screened for eligibility independently by at least two reviewers. 1,545 articles were excluded on the basis of title and abstract, most frequently because of wrong population [no TBI or acquired brain injury (ABI)], wrong outcome (e.g., therapy/intervention study) or wrong study design (e.g., communicative assessment in TBI without relation to internet-based communication or interaction). 13 articles were selected for full text assessment as their content met the inclusion criteria for this review based on the respective title and abstract. Each of them was again screened for eligibility independently by at least two reviewers. From the 13 full texts, two had to be excluded since they did not relate to the target population (TBI). Furthermore, one study was excluded based on the full-text analysis because it was an intervention study. Thus, 10 full texts in total could be included.
In order to fulfill the goal of this review and provide an overview of the currently available instruments to assess CMC use as a measure of digital participation in the TBI population, the 10 included studies were examined as to the assessment tools used in each case. For this, the studies were briefly described in terms of the individual objectives and the individual study design at the outset. Subsequently, they were analyzed and compared in terms of content according to selected parameters: main applied measures, target group, sample size and research question(s)/aim(s) of the study (see Table 1). The main procedures were extracted from the studies and analyzed according to the following parameters: number of items, question types, duration of implementation and availability (see Table 2). In a next step, the procedures uncovered in the studies were examined as to their suitability for the investigation of digital participation in the TBI population. Finally, an overall overview of the potential and the limitations of the methods used in the studies was provided.
The included procedures were analyzed as to whether they examined Internet-based communication tools in the TBI population and were then summarized in tabularized form including some brief information about the respective target group, structure, and content of the items and questions.
The study selection process is depicted in the following PRISMA flow diagram (see Figure 1).
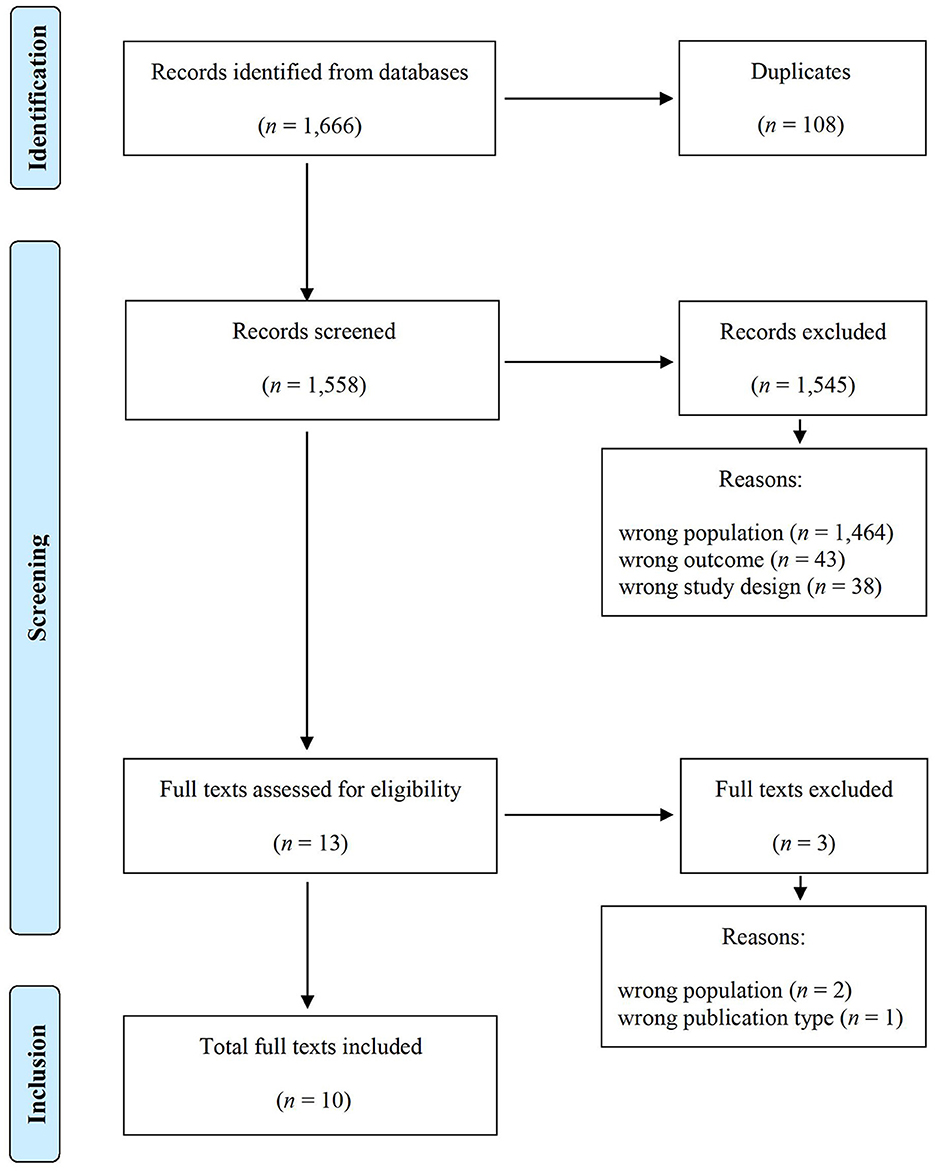
Figure 1. PRISMA flow diagram. From: Page et al. (2021). For more information, visit: http://www.prisma-statement.org/.
Following a screening on title/abstract and full-text level, we were able to identify ten studies which included nine assessment tools that met our inclusion criteria and examined the quantity and the respective objective of Internet-based communication tools in participants with TBI.
The specific objectives of the studies varied in detail (see section 4.3 Study Summaries for further information). Most of the studies had the goal to examine CMC-related aspects in individuals with TBI and compare performance with healthy controls. In (2)1, the questionnaire also served the goal to support the development of an app and coaching program. In (6), the questionnaire supplemented the more central measure of an Actual Reality Task. According to the different goals of the studies, the applied questionnaires and surveys differed in scope and in domains that were addressed.
According to our inclusion criteria, the target populations of all studies were individuals with TBI, most commonly in the chronic phase. Study (3) included individuals with ABI, of which TBI was the largest subgroup (40.07%). The severity of TBI of participants was moderate-to-severe (1, 4, 5, 6, 7, 8, 9), with all grades of severity from mild-to-severe (2, 10) or not specified (3). The grade of severity was determined most commonly by duration of loss of consciousness following the trauma, duration of posttraumatic anterograde amnesia, or the Glasgow Coma Scale (GCS) score (Teasdale and Jennett, 1974) (see e.g., 4). The trauma happened at least 6 months (4, 5, 9), or more than one year (1, 2, 6, 7), before the investigation. The period of brain damage was not restricted in (3) and (10), with varying periods from several weeks to more than 10 years post injury. In (8), time since injury was assessed but not reported. The number of participants with TBI ranged from 10 individuals (6) to 337 individuals (1). In more than half of the studies, performance was compared with neurologically healthy controls (2, 4, 5, 6, 8, 9, 10). Six cases (2, 4, 5, 6, 8, 9) involved age- and education-matched control groups and one case (10) involved only an age-matched control group. In two studies (2, 4), caregivers, relatives (e.g., parents), friends or professionals were also interviewed to provide a multiperspective approach to the respective research questions.
In the following section, we provide a short summary of the finally selected studies and their main applied measures. Table 1 provides an overview of the procedures, structured according to the respective authors of the studies and the year of publication, the name of the procedure, the target group, sample size and research question(s)/aim(s) of the study. We included studies from countries worldwide that were published in either English or German.
Baker-Sparr et al. (2018) aimed to characterize the internet and social media use among adults with moderate-to-severe TBI. The participants were 337 individuals who had to meet the inclusion criteria of the Traumatic Brain Injury Model Systems (TBIMS) National Database. The authors developed a tool called Internet Usage Survey in order to assess the participants' internet and social media use. Key domains that were covered by the survey were types of online activity, use of social media as well as size of online community and intensity of use, modes of access, frequency and patterns of usage, barriers to online accessibility, and factors that prevent non-users from engaging in online activity. For the purpose of assessing the extent of social media use, the survey also included the Facebook Intensity Scale (FBI) (Ellison et al., 2007), which is an eight-item questionnaire that depicts an individual's extent of engagement with Facebook including the total number of Facebook Friends, minutes per day spent on Facebook as well as six Likert scale questions assessing emotional connectedness with Facebook. The authors also reported several limitations of the present study that might affect the generalizability of the results, such as a focus on quantity of internet usage and pre-injury level of familiarity with online technology (Baker-Sparr et al., 2018). The survey is supposed to be available via the TBIMS National Database but could unfortunately not be accessed due to technical problems with the Website.
Bedell et al. (2017) conducted a multi-site study with a total of 39 participants from five different participant pools. Information from different target groups (persons who had TBI, relatives, peer groups, professionals) was considered. The study included teenagers and college students with TBI over the age of 18, their parents and also age-matched teenagers and college students without TBI. The objective was to use feedback from questionnaires and interviews as part of an iterative design process to enable the development of a coaching app which was intended to improve social communication. The surveys focused on preferred activities and frequency of participation, barriers and facilitators to social participation, as well as cell phone and app use. Their results showed that individuals with TBI mentioned more barriers to social participation and fewer strategies to overcome those barriers than youth without TBI. A summary of the total 20 questions, which range from single-choice, multiple-choice and yes-no questions to open-ended questions, can be found in the appendix of the article by Bedell et al. (2017).
Eghdam et al. (2016) investigated the use of e-services in a group of brain-injured individuals (n = 282), where TBI was the most common cause (n = 113) of ABI. Given the lack of adequate survey instruments to assess the use and experience with e-services, the authors presented the ICT-CFQ, a self-developed questionnaire, comprising 17 items in the form of single-choice, multiple-choice and opened-ended questions asking about the quality and quantity of the use of e-services in individuals with ABI. The questionnaire was based on and cross-validated with information provided by the ICF, as well as medical experts' and rehabilitative professionals' opinions. Overall, about 89% of the 282 participants with ABI reported regularly using some kind of e-services on their personal computers, mobiles or tablets, of which the most popular types were applications for communication and e-banking, while reading (e-books) and health promotion service apps were the least popular e-services. Additionally, all participants filled out the Cognitive Failure Questionnaire (CFQ) (Broadbent et al., 1982), which the authors conducted to test how participants tackle everyday challenges in the presence of cognitive impairment. The authors found out that ABI participants who complained about strong challenges due to cognitive impairment nevertheless used e-services regularly. In the open answer section, participants reported advantages and personal challenges with e-service use, for example the risk of behavioral influence (e.g., risk of addiction), difficult design (e.g., information overload, unwanted pop-ups and advertisements) or technical issues (e.g., hardware problems, battery life). Eghdam et al. (2016) emphasize the high proportion of individuals with ABI rely on e-services while facing different types of challenges caused by cognitive impairment. They also point to a potential bias in the study, since individuals with strong challenges in the use of e-services may not have even participated in this online study. The ICT-CFQ questionnaire is available in the supplementary material of Eghdam et al. (2016).
Flynn et al. (2018) investigated social participation, friendship quantity and friendship quality of adults with TBI by including a group of uninjured adults. The authors examined 18 adults with moderate-to-severe TBI as well as consulted 16 of their friends. In order to be able to compare the results with those of healthy peers, 18 uninjured adults and 11 of their friends were consulted as well. Measures that were used consisted of the Participation Assessment with Recombined Tools-Objective (PART-O) (Whiteneck et al., 2011), the Social Network Questionnaire (SNQ) (Roberts and Dunbar, 2011), and the McGill Friendship Questionnaire (MFQ) (Mendelson and Aboud, 1999). The PART-O includes 17 items about the number of hours a week spent working or at school, the type and frequency of social activities, and if the individual has any intimate relationships or meaningful friendships. Each item must be scored on a 0–5 point Likert scale. The questionnaire takes approximately 30 min to complete, but the individual questions are however not freely available yet. The PART-O contains an item for Internet use and was therefore included in the search (see Table 3). The latter two assessment tools—SNQ and MFQ—aim to measure friendship quantity and obtain information about friendship quality (Flynn et al., 2018). Since none of the two methods mentioned explicitly measures the digital participation of the participants, they will not be discussed further here.
Flynn et al. (2019) published the results of an investigation with 25 individuals with TBI and 26 healthy individuals. The aim of this study was to characterize the friendship networks and the social participation of people with TBI. Moreover, they analyzed which communication methods, including CMC, are used by adults with TBI. Social participation was measured also with the PART-O (Whiteneck et al., 2011) and the SNQ (Roberts and Dunbar, 2011) was used to measure the friendship quality. The participants additionally had to list the communication method they used when communicating with the listed friends. The authors found out that adults with TBI have smaller social networks and name face-to-face meetings as the preferred communication method (Flynn et al., 2019).
In their study, Goverover and DeLuca (2015) applied an Internet Use Questionnaire to assess prior experience with using a computer of individuals TBI and healthy individuals. To this end, they applied their questionnaire to ten individuals who had sustained a moderate-to-severe TBI at least one year prior to the study and ten healthy individuals. Both groups were demographically matched on age and education. Using seven items, the Internet Use Questionnaire captures one's previous experience with using computers and the Internet as well as one's experience with purchasing gifts and cookies via the Internet. For each item—single-choice or yes-no question—several answer options are available, each of which has a different score. The total score could range from 0 (no Internet experience) to 21 (much Internet experience). The questionnaire is freely available in a previous study by Goverover et al. (2010). Another component of the study by Goverover and DeLuca (2015) was the completion of a so-called Actual Reality task with the following objectives: First, to use the internet to perform an actual everyday life task, and second, to examine possible differences in the performance of individuals with TBI and healthy individuals. Although this task delivers some hints of the everyday use of the internet in the TBI population, it is not addressed in detail in this scoping review, which provides an overview over the currently available measuring instruments for assessing CMC use of individuals with TBI. A detailed description of the AR Task and their results can be found in Goverover and DeLuca (2015).
The objective of the study by Ketchum et al. (2020) was to shed light on the association between social Internet use and real-world societal participation in individuals with TBI. For the study, 331 participants with moderate-to-severe TBI were recruited. The authors assessed the social Internet use based on the items from Baker-Sparr et al. (2018). According to the amount of social Internet use, participants were divided into a group of social Internet users (n = 232) and non-users (n = 99). In a follow-up interview 1 year after the questionnaire assessment, Ketchum et al. (2020) administered the PART-O (Whiteneck et al., 2011), which provides subscales for productivity (e.g., employment), social relations and leisure and community activities. Also, the PART-O includes an item about Internet use in the Social Relations subscale. The authors observed that participants with higher participation scores according to the PART-O also reported higher levels of Internet use. Social media use was therefore interpreted as a supplement instead of a replacement of real-life-participation (Ketchum et al., 2020). The authors interpreted this association in the sense that “similar barriers and facilitators affect both online and real-world social participation” (Ketchum et al., 2020) in TBI cases. For example, impairment in memory, language or executive functions could affect both social media use and the ability to “initiate and maintain social relationships in the real world” (Ketchum et al., 2020).
The study by Kilov et al. (2015) examined the reliability of a computer and Internet survey (Computer User Profile, CUP) which was originally developed by Todis et al. (2005). With the CUP it is possible to assess the nature and frequency of social communication and computer and Internet activities. The CUP includes 62 items in four domains: (1) demographic data, (2) social communication and activity engagement, (3) injury-related information, and (4) computer use. Answer types varied from checking boxes on 7-point Likert scales to checking boxes on nominal yes-no or categorical questions. Likert scaled items asked how often participants engaged in social communication and leisure activities and how often they participated in computer/Internet activities (e.g., writing emails, using chat rooms, downloading music). Kilov et al. (2015) analyzed the responses to the CUP in individuals with moderate-to-severe TBI (n =16) and in an age- and education-level-matched control group (n = 40). For the control group, an adapted version of the CUP without injury-related items was applied. Kilov et al. (2015) showed that the CUP and the adapted version for non-injured participants have satisfactory test-retest reliability measures. Intra-class correlation coefficients and kappa coefficients were conducted to measure reliability of individual CUP items. The CUP questionnaire is freely available in the appendix of the study by Kilov et al. (2015).
As part of their study about CMC in adults with and without TBI, Morrow et al. (2021b) conducted a web-based Survey of 53 individuals with a chronic history of moderate-to-severe TBI (TBI group) and of 51 non injured peers (NC group). Both groups were demographically matched according to age and education. With the aforementioned survey the authors pursued three objectives: characterizing how and why adults with TBI use social media and CMC platforms, evaluating changes in CMC after TBI, and eliciting suggestions from individuals with TBI for improving access to social media after injury. In general, the survey consisted of up to 280 items, but in the context of the present study, the authors considered only 15 items that were relevant to social media usage and changes in usage related to TBI. These 15 items differ in their question types. Thus, in addition to multiple-choice questions, yes-no and open-ended questions also occur. The implementation took 60 min for the TBI group, divided into two times 30 min, and 30–45 min for the NC group. The short version of the Web-based Survey with its 15 items is freely available in the appendix of the study by Morrow et al. (2021b).
With their Smartphone Survey, Wong et al. (2017) aimed to analyze patterns of smartphone use amongst people with TBI, explore potential barriers to use, and examine relationships between smartphone use and daily functioning. The participants were 29 people with TBI in the chronic phase and 33 non-injured participants. The severity of the initial injury in the TBI group ranged from very severe to mild. The items were based on an earlier work by Hart et al. (2004), which included questions relating to self-reported needs for improvement and interest in portable technology. Additional items were derived from a pilot study with two participants with TBI, using their feedback to optimize the content of the Smartphone Survey. The resulting survey consisted of 309 items, using both multiple-choice and open-ended formats. Question topics covered duration and frequency of smartphone use and different app types (n = 24), perceived utility of different apps and features, and smartphone use in rehabilitation services. Barriers to smartphone use and factors contributing to difficulties in using the technology were also evaluated. The questionnaire was used in different ways, as an online survey, on the phone and in person. The individual questions of the survey have not yet been published.
Seven questionnaires applied in the studies were freely available, one questionnaire was not yet published (Smartphone Survey, Wong et al., 2017), and one was not made available by the authors after request (Internet Usage Survey, Baker-Sparr et al., 2018, with similar items used by Ketchum et al., 2020). All information concerning the questionnaires that were not available were second-hand, based on the information provided in the studies.
Within the studies analyzed, we found nine tools that met our inclusion criteria of assessing aspects of digital participation in TBI (see inclusion criteria in sections 3.1 and Supplementary material). All of the tools were self-administration questionnaires that can be filled out by individuals with TBI either online or in a printed version. All tools served to assess the frequency, quality and purpose of internet and/or social media use in TBI. Most tools aimed at the general internet use (f. e., Internet Use Questionnaire, Internet Usage Survey, Adapted Computer User Profile) or e-service use (see: E-Services Questionnaire). Other tools focused on social media (survey by Morrow et al., 2021b), or a specific social media platform [see: Facebook Intensity Scale (1)]. The Smartphone Survey by Wong et al. (2017) and also parts of the survey by Bedell et al. (2017) placed an emphasis on the general purpose, frequency and barriers of smartphone use. The PART-O aims primarily to assess general productivity and social relations and includes only one item related to digital participation. Typical questions within the questionnaires concern:
• frequency of internet or social media use (f. e., “In a typical week, how many times do you use the Internet for communication, such as for e-mail, visiting chat rooms, or instant messaging?”, PART-O, Whiteneck et al., 2011);
• quality of internet or social media use [f. e., “Are you able to participate in Internet chatrooms?”, Adapted Computer User Profile, (8)];
• purpose of internet or social media use [f. e., “I use social media for … (example: keeping in touch with friends and family)”, survey by (9)];
• quality of social relations via internet or social media [f. e., “Do you use the Internet to connect with other people with similar cognitive problems?”, E-Services Questionnaire, (3)];
• barriers or challenges of internet or social media use [f. e., “If you are not using a computer, why not? (example: visual problems)”, Adapted Computer User Profile, (8)];
• benefits or potential of internet or social media use [f. e., “Do you use any Internet service that helps you with your forgetfulness, difficulty concentrating, or other cognitive problems?”, E-Services Questionnaire, (3)].
The instruments applied had a number of items ranging from rather few items [seven items in the Internet Use Questionnaire (6)] to extensive questionnaires like the Smartphone Survey with 309 items (10). The questionnaires included different question formats such as Likert scales (4, 5, 8) or a mixture of single- and multiple-choice, yes-no and open-ended questions (2, 3, 6, 8, 9, 10). Frequently, Likert scales were used to elicit frequency of use or satisfaction with use [e.g., Adapted Computer Use Profile (8)].
While some questionnaires used items from existing questionnaires on social or digital participation (PART-O, survey by Morrow et al., 2021b, Smartphone Survey), other questionnaires were designed for the purpose of the specific study based on previous knowledge from existing research (f. e., Internet Usage Survey) or on the experience of rehabilitation professionals and medical experts (f. e., E-Services Questionnaire). Kilov et al. (2015) adapted the Computer User Profile for both the TBI and general population, as it was originally designed for a broader target group of individuals with cognitive impairments. The survey by Bedell et al. (2017) served the specific cause of assessing the perspective of both individuals with TBI and their relatives concerning social participation and smartphone use in the context of the development of a smartphone app and coaching program. As for the Internet Use Questionnaire (6), the development of the items was not further described. The internal consistency of the questionnaires (f. e., split half-analysis) was not reported in any of the studies. For the Adapted Computer User Profile (Kilov et al., 2015) and the Smartphone Study (Wong et al., 2017), the assessment was repeated 1–2 weeks after the first trial. Both author groups reported sufficient test-retest reliability. Interestingly, Kilov et al. (2015) found higher reliability coefficients for adults without TBI than for adults with TBI.
For external validation, additional measures like demographic variables and injury characteristics have been taken into consideration to varying degrees by all studies reported. In seven of ten studies, performance was compared with a healthy control group in order to reveal characteristics of CMC in individuals with TBI. In four studies, additional cognitive, emotional and social measures were applied. Next to the Smartphone Study, Wong et al. (2017) performed the Cognitive Failures Questionnaire (CFQ) in order to test verbal learning, emotional functioning, everyday functioning and self-reported cognitive performance. The authors reported more frequent use of memory and organization apps in TBI individuals who indicated poorer cognitive performance in the CFQ. Also, they found that TBI individuals who used communication apps more often reported themselves to be better socially integrated according to the Community Integration Questionnaire (CIQ). Goverover and DeLuca (2015) conducted an actual reality task and examined information processing speed, episodic learning and memory, visual spatial memory, executive functions, emotional functioning, daily functioning and quality of life; however, no correlations between internet use experience and these measures were reported. Eghdam et al. (2016) assessed subjective cognitive performance with the CFQ and found TBI individuals who reported fewer cognitive complaints to use more e-services as indicated by their questionnaire. In order to evaluate the PART-O, Flynn et al. (2018) assessed quality and quantity of friendship relations with two additional questionnaires, but did not report interactions between PART-O and these measures.
The aim of the present scoping review was to identify measurement tools that contribute to the assessment of CMC in individuals with TBI. In our study, CMC was considered as a means to assess digital participation in people with TBI. How little the field of CMC has been studied so far was evident from our review revealing only very few standardized assessments which can actually be used as questionnaires with precise instructions and which are characterized by test quality criteria. Many of the studies had a rather exploratory character with very high sample sizes and/or many items (e.g., Wong et al., 2017; Ketchum et al., 2020). These surveys served rather to identify suitable questions and items and can be seen as precursors for the development of questionnaires. These surveys are not suitable for routine use, as they are not standardized, use a lot of open-ended questions and are very time-consuming (sometimes between 60 and 90 min).
In relation to our research questions mentioned at the beginning, we can summarize that we found a total of 9 tools for the measurement of CMC in the specified search period. Of these, 7 are available for practical use (see Table 2). The majority of the methods can map the opportunities and barriers of CMC to varying degrees (see Table 3).
Concerning the target group, all questionnaires were applied to individuals with TBI. As for the examined populations, it should be noted with criticism that some of the studies conducted web-based surveys. This implies that only individuals with internet access and the ability to use technology were able to participate. Overall, this leads to a selection bias in the studies presented here by excluding severe cases of TBI or individuals with specific CMC complaints, which also means that the examined tools might be not suitable for the whole population of TBI (Baker-Sparr et al., 2018; Morrow et al., 2021b).
As for the validity of the tools, some of the studies have carried out further measurements in regards to criterion validity. Only Kilov et al. (2015) and Wong et al. (2017) provided test-retest-reliability measures for their questionnaires. Our examination revealed a need for studies that examine the validity, reliability, and objectivity of the surveys and questionnaires and that also take into account secondary criteria such as acceptance, fairness, economy, and robustness to social desirability. In general, a lack of standardized instruments, especially ones accompanied by normative data, can be identified. In the following, a brief overview of the opportunities and barriers of CMC which could be obtained from the selected studies will be given.
The use of CMC devices can present a challenge for individuals with TBI who suffer from cognitive impairments like memory changes, social cognitive impairments or communicative impairments. Adults with TBI report using social media less frequently than non-injured controls and being faced with challenges in social media access and use (Morrow et al., 2021b). At the same time, some studies report a high level of individuals with ABI regularly using Internet technologies, and depending on these every day (Eghdam et al., 2016).
Brunner et al. (2015) also addressed certain risks in the social media use for individuals with TBI. One important point is Internet safety: individuals with TBI are possibly at a higher risk of encountering online miscommunications, cyber-bullying, online scams, web-based manipulation or fraud. Another aspect is the risk of over-use and addictive behavior concerning internet or social media use, as possibly enhanced by changes in inhibition and self-regulation (Eghdam et al., 2016; Morrow et al., 2021b). In the social media context, TBI individuals have been reported to publish inaccurate or inappropriate content or violate confidentiality of information more often (Brunner et al., 2015).
Individuals with TBI may have a greater risk of encountering difficulties in CMC use due to linguistic or cognitive impairment, and of therefore becoming affected by the digital divide. At the same time, technology provides the potential to overcome barriers and constraints (Chuah et al., 2022). The benefits of availability, mobility, flexibility, and rapidity not only apply to users overall, but also to the use of CMC in TBI (Eghdam et al., 2016). Individuals can use communication technologies at a comparably low financial expense and can interact independently of their geographic location. Content-wise, communication technologies allow individuals with TBI to interact with online communities and groups of interest according to their needs, which allows them to get information or (peer) support in stigma-free environments (Brunner et al., 2015; Morrow et al., 2021b; Chuah et al., 2022). Especially younger individuals who engage in social networks rely on the use of CMC technologies (Bedell et al., 2017).
CMC can be actively used to provide an environment to generalize therapy skills. Technology-based interactions can be used as an additional, cost-effective means of training or monitoring communicative or cognitive skills addressed in therapy (Chuah et al., 2022). Therapy goals could both address the domain of activity (e.g., handling applications on a smartphone), as well as the level of participation (e.g., formulating messages in an online forum). For instance, smartphone functions like calendars and reminders can be used to improve organizational or memory skills (Wong et al., 2017). Telerehabilitation allows for remote therapy opportunities from home (Chuah et al., 2022). Integrating the safe and effective use of CMC into rehabilitation as a therapy goal could possibly even serve as a means of increasing social participation for individuals with TBI (Morrow et al., 2021b).
Generally, the use of communication technologies is an integral part of life for individuals with TBI, allowing them to connect with family and friends. Eghdam et al. (2016) reported that the use of internet-based tools is not diminished, but equally important for people with TBI. Research points to higher satisfaction and lower grades of social isolation for individuals with TBI who use social media (Brunner et al., 2015).
One limitation of our study concerns our search strategy. Our specific criteria led to the generation of fewer but more relevant results. However, it must be mentioned that some measurement tools were not picked up by the applied search terms (see Appendix). While we did not explicitly assess the study quality of the articles we found, we do provide some information on the study design and content of the tools. The assessment of study quality could be the aim of a future systematic review. In contrast to systematic reviews, scoping reviews do not necessarily have to be registered (or cannot be registered at all, e.g., in PROSPERO). However, in order to improve transparency, future reviews should be registered in advance, e.g., in BMJ Open, which also publishes study protocols.
Our systematic data research revealed that there is a great need for research in the field of CMC in general, including methods for measuring digital participation disorders and resources. Based on our findings we recommend that the existing questionnaires should be applied routinely to detect impairments in CMC and digital participation. CMC should be an integral part of rehabilitation in TBI, as digital methods of communication are of great importance in society in general and also for teenagers and adults with TBI. In this context it is important to consider the benefits and risks of CMC use in TBI. Although this issue was partially addressed in the present study, a more in-depth investigation of the risks and benefits needs to be conducted in further studies. Individuals with TBI encounter similar risks in using CMC as the general population, as well additional challenges caused by linguistic or cognitive impairment. Generally, the same challenges apply for both computer-mediated, as well as face-to-face communication interactions. For example, impairments in memory, language or executive functions could affect both CMC and real-live relationships (Ketchum et al., 2020).
Next to possible challenges in CMC use in TBI, the use of communication technologies is equally relevant and also satisfactory for this population. Professionals should be aware of the relevance of communication technologies and also the possible need for assistance to ensure a safe and effective use for individuals with TBI. CMC goals “should be included in formal rehabilitation plans for people with TBI, both to improve peer interaction and to show patients how to minimize the risks of online activity” (Ketchum et al., 2020). The possible challenges and individual needs of individuals with TBI should be addressed and targeted in rehabilitation for both natural as well as technology-mediated communicative interactions.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
JB-K contributed to funding, conception, and design of the study. JB-K, JR, KR, NH, and ZF conducted the study retrieval and selection and wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research publication was supported by LMUexcellent, funded by the Federal Ministry of Education and Research (BMBF) and the Free State of Bavaria under the Excellence Strategy of the Federal Government and the Länder.
We thank Katja Viebahn for proofreading the article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2023.1221149/full#supplementary-material
Achhammer, B., Büttner, J., Sallat, S., and Spreer, M. (2016). Pragmatische Störungen im Kindes- und Erwachsenenalter. 1st ed. Stuttgart: Thieme.
American Speech-Language-Hearing Association (2003). Evaluating and Treating Communication and Cognitive Disorders: Approaches to Referral and Collaboration for Speech-Language Pathology and Clinical Neuropsychology [Technical Report]. Available online at: www.asha.org/policy (accessed August 31, 2023).
Anderson, V., Northam, E., and Wrennall, J. (2019). Developmental Neuropsychology: A Clinical Approach. 2nd ed. Milton Park, Abingdon, Oxon, New York, NY: Routledge.
Australian Communications Media Authority (2013). Like, Post, Share: Young Australians' Experience of Social Media. Quantitative research report. Australian Communications and Media Authority. Available online at: www.acma.gov.au/theACMA/Library/researchacma/Research-reports/young-australians-and-social-media (accessed August 31, 2023).
Baker-Sparr, C., Hart, T., Bergquist, T., Bogner, J., Dreer, L., Juengst, S., et al. (2018). Internet and social media use after traumatic brain injury. A traumatic brain injury model systems study. J Head Trauma Rehabil. 33, E9–E17. doi: 10.1097/HTR.0000000000000305
Bambini, V., and Bara, B. G. (2012). “Neuropragmatics,” in Handbook of Pragmatics, eds. J.-O. Östman, and J. Verschueren (Amsterdam: John Benjamins Publishing Company), 1–21.
Bedell, G. M., Wade, S. L., Turkstra, L. S., Haarbauer-Krupa, J., and King, J. A. (2017). Informing design of an app-based coaching intervention to promote social participation of teenagers with traumatic brain injury. Dev. Neurorehabil. 20, 408–417. doi: 10.1080/17518423.2016.1237584
Bischetti, L., Frau, F., and Bambini, V. (2022). “Neuropragmatics. Book chapter to be included,” in The Handbook of Clinical Linguistics, 2nd ed, eds. M. J. Ball, N. Müller, and L. Spencer (Hoboken, NJ: Wiley).
Bootsma, J. N., Turkstra, L. S., and Gorter, J. W. (2021). Expression of propositional attitudes in conversation by adults with traumatic brain injury: a relevance theoretic approach. Int. J. Lang. Commun. Dis. 56, 346–359. doi: 10.1111/1460-6984.12608
Broadbent, D. E., Cooper, P. F., FitzGerald, P., and Parkes, K. R. (1982). The cognitive failures questionnaire (CFQ) and its correlates. Br. J. Clin. Psychol. 21, 1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x
Brunner, M., Hemsley, B., Palmer, S., Dann, S., and Togher, L. (2015). Review of the literature on the use of social media by people with traumatic brain injury (TBI). Disabil. Rehabil. 37, 1511–1521. doi: 10.3109/09638288.2015.1045992
Brunner, M., Rietdijk, R., and Togher, L. (2022). Training resources targeting social media skills to inform rehabilitation for people who have an acquired brain injury: scoping review. J. Med. Int. Res. 24, e35595. doi: 10.2196/35595
Büttner, J. (2016). Kognitive Kommunikationsstörungen: Aktuelle Ansätze für Diagnostik und Therapie. Forum Logopädie 6, 6–16.
Büttner, J., and Glindemann, R. (2019). Kognitive Kommunikationsstörungen. 1st ed. Göttingen: Hogrefe.
Büttner-Kunert, J., Falkowska, Z., and Blöchinger, S. (2021). Is there an impact of theory of mind on narrative discourse production and social-communicative participation in people with Traumatic Brain Injury and healthy individuals? Neurol. Rehabil. S1, 11–12.
Büttner-Kunert, J., Jonas, K., Rosenkranz, A., and Thöne-Otto, A. (2022). Kognitive Kommunikationsstörungen: Wenn die Zusammenarbeit von Sprache und geistigen Fähigkeiten durch eine neurologische Erkrankung beeinträchtigt ist. 1st ed. Idstein: Schulz-Kirchner.
Centers for Disease Control and Prevention (2015). Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. Atlanta, GA: National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention.
Christman Buckingham, S. S., and Sneed, K. E. (2018). “Cognitive-communication disorder,” in Encyclopedia of Clinical Neuropsychology, eds. J. Kreutzer, J. DeLuca, and B. Caplan (Cham: Springer International Publishing), 1–8.
Chuah, S. L., Whiting, D. L., and Simpson, G. K. (2022). Digital divide among individuals with acquired brain injury. A scoping review protocol. JBI Evid. Synth. 20, 3009–3016. doi: 10.11124/JBIES-21-00423
Cornejo Müller, A., Wachtler, B., and Lampert, T. (2020). Digital Divide – Soziale Unterschiede in der Nutzung digitaler Gesundheitsangebote. Bundesgesundheitsblatt 63, 185–191. doi: 10.1007/s00103-019-03081-y
Dromer, E., Kheloufi, L., and Azouvi, P. (2021). Impaired self-awareness after traumatic brain injury: A systematic review. Part 2. Consequences and predictors of poor self-awareness. Ann. Phy. Rehabil. Med. 64, 101542. doi: 10.1016/j.rehab.2021.101542
Duplaga, M. (2017). Digital divide among people with disabilities. Analysis of data from a nationwide study for Determinants of Internet use and activities performed online. PLoS ONE 12, e0179825. doi: 10.1371/journal.pone.0179825
Eghdam, A., Bartfai, A., Oldenburg, C., and Koch, S. (2016). How do persons with mild acquired cognitive impairment use information and communication technology and e-services? Results from a Swedish National Survey. PLoS ONE 11, e0159362. doi: 10.1371/journal.pone.0159362
Elbourn, E., Brassel, S., Steel, J., and Togher, L. (2022). Perceptions of communication recovery following traumatic brain injury: a qualitative investigation across 2 years. Int. J. Lang. Commun. Disord. doi: 10.1111/1460-6984.12795 [Epub ahead of print].
Ellison, N. B., Steinfield, C., and Lampe, C. (2007). The benefits of facebook “Friends:” social capital and college students' use of online social network sites. J. Comp. Med. Commun. 12, 1143–1168. doi: 10.1111/j.1083-6101.2007.00367.x
Elm, E., von Schreiber, G., and Haupt, C. C. (2019). Methodische Anleitung für Scoping Reviews (JBI-Methodologie). Zeitschrift für Evidenz, Fortbildung und Qualitat im Gesundheitswesen 143, 1–7. doi: 10.1016/j.zefq.2019.05.004
Eurostat (2021). Do you participate in social networks? Newsarticle. Available online at: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210630-1 (accessed November 4, 2023).
Eurostat (2023). Table: Individual Internet Activities. Available online at: https://ec.europa.eu/eurostat/databrowser/view/ISOC_CI_AC_I__custom_1058781/bookmark/table?lang=enandbookmarkId=0dd5535e-a7e5-4ff8-a2a4-134d5b56718dandpage=time:2020 (accessed November 4, 2023).
Evald, L. (2015). Prospective memory rehabilitation using smartphones in patients with TBI. What do participants report? Neuropsychol. Rehabil. 25, 283–297. doi: 10.1080/09602011.2014.970557
Falkowska, Z., Heider, N., Resch, K., Royko, J., and Büttner-Kunert, J. (2021). Die Erhebung von kommunikativ-pragmatischen Fähigkeiten und Lebensqualität nach Schädel-Hirn-Trauma. Zeitschrift für Neuropsychologie 32, 181–193. doi: 10.1024/1016-264X/a000336
Flynn, M. A., Mutlu, B., Duff, M. C., and Turkstra, L. S. (2018). Friendship quality, friendship quantity, and social participation in adults with traumatic brain injury. Semin. Speech Lang. 39, 416–426. doi: 10.1055/s-0038-1670672
Flynn, M. A., Rigon, A., Kornfield, R., Mutlu, B., Duff, M. C., and Turkstra, L. S. (2019). Characterizing computer-mediated communication, friendship, and social participation in adults with traumatic brain injury. Brain Injury 33, 1097–1104. doi: 10.1080/02699052.2019.1616112
Gindri, G., Pagliarin, K. C., Casarin, F. S., Branco, L. D., Ferré, P., Joanette, Y., et al. (2014). Rehabilitation of discourse impairments after acquired brain injury. Dement. Neuropsychol. 8, 58–65. doi: 10.1590/S1980-57642014DN81000009
Goverover, Y., and DeLuca, J. (2015). Actual reality. Using the Internet to assess everyday functioning after traumatic brain injury. Brain injury 29, 715–721. doi: 10.3109/02699052.2015.1004744
Goverover, Y., O'Brien, A. R., Moore, N. B., and DeLuca, J. (2010). Actual reality. A new approach to functional assessment in persons with multiple sclerosis. Arch. Phy. Med. Rehabil. 91, 252–260. doi: 10.1016/j.apmr.2009.09.022
Greenwood, S., Perrin, A., and Duggan, M. (2016). Social Media Update 2016. Pew Research Center. Available online at: www.pewresearch.org/internet/2016/11/11/social-media-update-2016/ (accessed July 7, 2023).
Gupta, S., and Bashir, L. (2018). Social networking usage questionnaire. Development and validation in an indian higher education context. Turk. Onl. J. Dist. Educ. 19, 214–227. doi: 10.17718/tojde.471918
Hart, T., Buchhofer, R., and Vaccaro, M. (2004). Portable electronic devices as memory and organizational aids after traumatic brain injury: a consumer survey study. J. Head Trauma Rehabil. 19, 351–365. doi: 10.1097/00001199-200409000-00001
Kaplan, A. M., and Haenlein, M. (2010). Users of the world, unite! The challenges and opportunities of social media. Bus Horiz 53, 59–68. doi: 10.1016/j.bushor.2009.09.003
Ketchum, J. M., Sevigny, M., Hart, T., O'Neil-Pirozzi, T. M., Sander, A. M., Juengst, S. B., et al. (2020). The association between community participation and social internet use among adults with traumatic brain injury. J. Head Trauma Rehabil. 35, 254–261. doi: 10.1097/HTR.0000000000000566
Kilov, A. M., Togher, L., and Grant, S. (2009). Problem solving with friends: discourse participation and performance of individuals with and without traumatic brain injury. Aphasiology 23, 584–605. doi: 10.1080/02687030701855382
Kilov, A. M., Togher, L., and Power, E. (2015). Reliability of a computer and Internet survey (Computer User Profile) used by adults with and without traumatic brain injury (TBI). Brain Injury 29, 1273–1291. doi: 10.3109/02699052.2015.1042052
MacDonald, S. (2017). Introducing the model of cognitive-communication competence: A model to guide evidence-based communication interventions after brain injury. Brain Injury 31, 1760–1780. doi: 10.1080/02699052.2017.1379613
Manago, A. M., Taylor, T., and Greenfield, P. M. (2012). Me and my 400 friends: the anatomy of college students' Facebook networks, their communication patterns, and well-being. Dev. Psychol. 48, 369–380. doi: 10.1037/a0026338
Marr, A. L., and Coronado, V. G. (2004). Central Nervous System Injury Surveillance Data Submission Standards−2002. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control.
McDonald, S., Togher, L., and Code, C. (2014). “Traumatic brain injury: basic features,” in Social and Communication Disorders Following Traumatic Brain Injury, 2nd ed. eds. S. McDonald, L. Togher, and C. Code (London: Psychology Press), 26–47.
Mendelson, M. J., and Aboud, F. E. (1999). Measuring friendship quality in late adolescents and young adults. McGill Friendship Questionnaires. Can. J. Behav. Sci. 31, 130–132. doi: 10.1037/h0087080
Meshi, D., Tamir, D. I., and Heekeren, H. R. (2015). The emerging neuroscience of social media. Trends Cogn. Sci. 19, 771–782. doi: 10.1016/j.tics.2015.09.004
Morrow, E. L., Patel, N. N., and Duff, M. C. (2021a). Disability and the COVID-19 pandemic: a survey of individuals with traumatic brain injury. Arch. Phy. Med. Rehabil. 102, 1075–1083. doi: 10.1016/j.apmr.2021.01.064
Morrow, E. L., Zhao, F., Turkstra, L., Toma, C., Mutlu, B., and Duff, M. C. (2021b). Computer-mediated communication in adults with and without moderate-to-severe traumatic brain injury. Survey of social media use. JMIR Rehabil. Assist. Technol. 8, e26586. doi: 10.2196/26586
Norman, R. S., Mueller, K. D., Huerta, P., Shah, M. N., Turkstra, L. S., and Power, E. (2022). Discourse performance in adults with mild traumatic brain injury, orthopedic injuries, and moderate to severe traumatic brain injury, and healthy controls. Am. J. Speech Lang. Pathol. 31, 67–83. doi: 10.1044/2021_AJSLP-20-00299
Ouzzani, M., Hammady, H., Fedorowicz, Z., and Elmagarmid, A. (2016). Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 5, 210. doi: 10.1186/s13643-016-0384-4
Ownsworth, T., Arnautovska, U., Beadle, E., Shum, D. H. K., and Moyle, W. (2018). Efficacy of telerehabilitation for adults with traumatic brain injury. A systematic review. J. Head Trauma Rehabil. 33, E33–E46. doi: 10.1097/HTR.0000000000000350
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71. doi: 10.1136/bmj.n71
Rehadat (2023). ICF-Guide. Available online at: www.rehadat-icf.de/en/klassifikation/aktivitaeten-partizipation/d3/ (accessed July 10, 2023).
Roberts, S. G., and Dunbar, R. I. (2011). The costs of family and friends. An 18-month longitudinal study of relationship maintenance and decay. Evol. Hum. Behav. 32, 186–197. doi: 10.1016/j.evolhumbehav.2010.08.005
Robertson, K., and Schmitter-Edgecombe, M. (2017). Focused and divided attention abilities in the acute phase of recovery from moderate to severe traumatic brain injury. Brain Inj. 31, 1069–1076. doi: 10.1080/02699052.2017.1296192
Rosenthal, L. S., and Hillis, A. E. (2012). “Neuropathologies underlying acquired language disorders,” in Cognition and Acquired Language Disorders: An Information Processing Approach, eds. R.K. Peach, and L. P. Shapiro (Amsterdam: Elsevier), 37–60.
Salmond, C. H., Chatfield, D. A., Menon, D. K., Pickard, J. D., and Sahakian, B. J. (2005). Cognitive sequelae of head injury. Involvement of basal forebrain and associated structures. Brain J. Neurol. 128, 189–200. doi: 10.1093/brain/awh352
Sim, P., Power, E., and Togher, L. (2013). Describing conversations between individuals with traumatic brain injury (TBI) and communication partners following communication partner training: using exchange structure analysis. Brain Inj. 27, 717–742. doi: 10.3109/02699052.2013.775485
Stocchetti, N., and Zanier, E. R. (2016). Chronic impact of traumatic brain injury on outcome and quality of life. A narrative review. Crit. Care 20, 148. doi: 10.1186/s13054-016-1318-1
Teasdale, G., and Jennett, B. (1974). Assessment of coma and impaired consciousness. Lancet 304, 81–84. doi: 10.1016/S0140-6736(74)91639-0
Todis, B., Sohlberg, M. M., Hood, D., and Fickas, S. (2005). Making electronic mail accessible. Perspectives of people with acquired cognitive impairments, caregivers and professionals. Brain Inj. 19, 389–401. doi: 10.1080/02699050400003957
Togher, L., McDonald, S., Code, C., and Grant, S. (2004). Training communication partners of people with traumatic brain injury: a randomised controlled trial. Aphasiology 18, 313–335. doi: 10.1080/02687030344000535
Togher, L., McDonald, S., Coelho, C. A., and Byom, L. (2014). “Cognitive communication disability following TBI,” in Social and Communication Disorders Following Traumatic Brain Injury, eds. S. McDonald, L. Togher, and C. Code, 2nd ed., (London: Psychology Press), 89–118.
Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Int. Med. 169, 467–473. doi: 10.7326/M18-0850
Tsaousides, T., Matsuzawa, Y., and Lebowitz, M. (2011). Familiarity and prevalence of Facebook use for social networking among individuals with traumatic brain injury. Brain Inj. 25, 1155–1162. doi: 10.3109/02699052.2011.613086
van Deursen, A. J., and van Dijk, J. A. (2014). The digital divide shifts to differences in usage. New Media Soc. 16, 507–526. doi: 10.1177/1461444813487959
Whiteneck, G. G., Dijkers, M. P., Heinemann, A. W., Bogner, J. A., Bushnik, T., Cicerone, K. D., et al. (2011). Development of the participation assessment with recombined tools-objective for use after traumatic brain injury. Arch. Phy. Med. Rehabil. 92, 542–551. doi: 10.1016/j.apmr.2010.08.002
WHO (2021). Internationale Klassifikation der Funktionsfähigkeit, Behinderung und Gesundheit (ICF). Inhaltlich unveränderter Nachdruck. Bonn: Bundesinstitut für Arzneimittel und Medizinprodukte.
Keywords: digital participation, computer-mediated communication, traumatic brain injury, cognitive communication disorders, assessment tools
Citation: Büttner-Kunert J, Royko J, Resch K, Heider N and Falkowska Z (2023) Digital participation in traumatic brain injury: scoping review about assessment tools for computer-mediated communication. Front. Commun. 8:1221149. doi: 10.3389/fcomm.2023.1221149
Received: 11 May 2023; Accepted: 13 November 2023;
Published: 06 December 2023.
Edited by:
Petra Jaecks, Bielefeld University, GermanyReviewed by:
Emma Power, University of Technology Sydney, AustraliaCopyright © 2023 Büttner-Kunert, Royko, Resch, Heider and Falkowska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julia Büttner-Kunert, anVsaWEuYnVldHRuZXJAbG11LmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.