- 1Faculty of Health, Social Care and Medicine, Edge Hill University, Ormskirk, United Kingdom
- 2Department of Ear, Nose and Throat, Alder Hey Children's NHS Foundation Trust, Liverpool, United Kingdom
- 3Department of Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, United Kingdom
Introduction: In recent years, there has been an increasing use of otoendoscopy in middle ear surgery. There is also increasing evidence of its usefulness as a diagnostic tool for clinicians. However, there is limited evidence on whether understanding their ear condition is of benefit to patients. This novel study sought to explore the perceptions, perspectives, and satisfaction of parents, children, and young people regarding the use of otoendoscope images in outpatient ENT consultations in relation to their understanding of ear symptoms, disease, and subsequent treatment. The framework for the study is child (and parent) health literacy and how visual images can play in scaffolding understanding, communication, and decision-making.
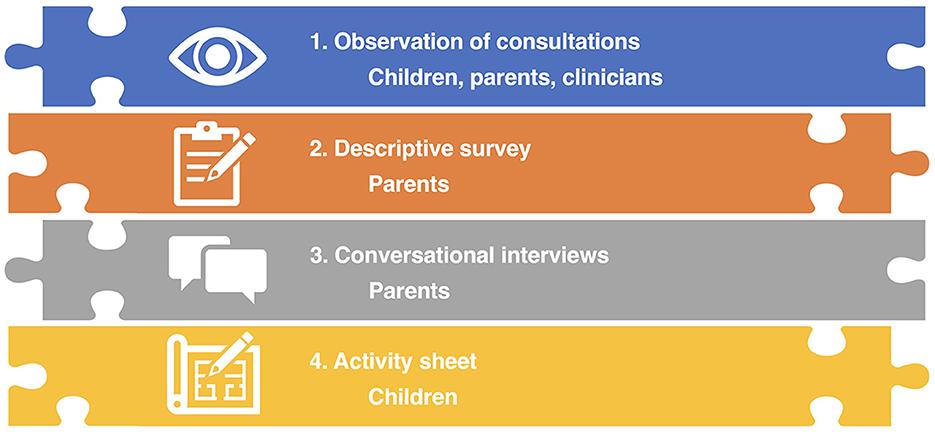
Methods: This qualitative descriptive exploratory study used semi-structured observation, a survey, short conversational interviews, and child activities.
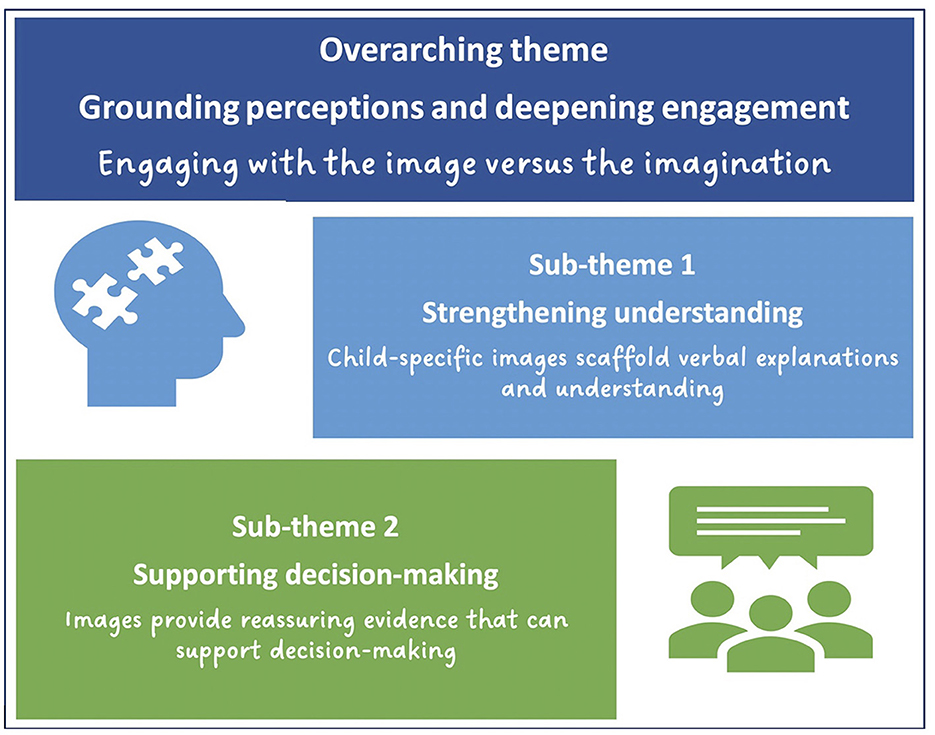
Results: Purposive sampling of 16 children (aged 4–15 yrs, various diagnoses) and parents/carers attending an outpatient ENT clinic at a tertiary pediatric hospital. One overarching theme, “Grounding perceptions and deepening engagement,” and two sub-themes, “Strengthening understanding” and “Supporting decision-making,” were identified. The children and parents valued the opportunity to see the images and gain insight and knowledge of their child's pathology.
Discussion: The images appeared to promote child (and parent) health literacy and interaction between the child-parent-clinician and informed shared decision-making. This study suggests that the use of otoendoscopy in an out-patient setting and sharing of the images with parents, children, and young people have a largely positive impact on understanding, relationship building, and decision making in pediatric ENT consultations.
1. Introduction
1.1. Clinical background
Ear conditions are very common in children and account for a significant proportion of both general practice and Ear, Nose, and Throat (ENT) consultations (Whitburn et al., 2011; Kozin et al., 2015). Globally otitis media is a significant health concern (Harmes et al., 2022). Otitis media with effusion (OME), often called glue ear, is by far the commonest ear condition in children (Simon et al., 2018), particularly in children from lower to middle income countries and disadvantaged populations (Leach et al., 2020). Studies report prevalence figures as high as 36.6% among British children aged 8 months old (Midgley et al., 2000) and 50–80% of children will have experienced at least one episode of acute otitis media before three years of age (Gaddey et al., 2019). In the USA, 2.2 million cases of otitis media are diagnosed yearly (Restuti et al., 2022). Other otological conditions in children that require ENT assessment include recurrent acute otitis media, and chronic otitis media with symptoms including pain, hearing loss, infection with discharge, dizziness.
OME is an important cause of hearing problems in children. Although the hearing loss associated with glue ear is usually transient and self-limiting (NICE, 2008), hearing loss may be persistent and result in language, behavioral and educational problems. Although acute otitis media is usually treated with antibiotic therapy, OME and tympanic membrane perforations sometimes require surgical treatment (NICE, 2008). Cholesteatoma almost always requires surgical treatment (NICE, 2008).
Traditionally, OME and related conditions are primarily diagnosed by examining the appearance of the eardrum using an otoscope with the clinician typically relying on written notes and hand drawn illustrations (Macharia, 2016) to record what has been observed. Many children who have been referred from a primary care setting with a suspected ear condition may, on otoendoscopic examination, be found to have a normal tympanic membrane. However, despite reassurance from a specialist that “all is well” it can be difficult for some parents and children to understand the examination and accept that their child's ear looks normal. Also, for children whose examination reveals problems, it can be difficult for parents and children to visualize what is wrong as they have to rely on the clinician's verbal report and/or illustration of what they have seen. This can be challenging for many parents and children as the anatomy, appearance and workings of the middle ear are both hidden and unknown.
In recent years, there has been increasing use of otoendoscopy with an attached camera system in middle ear surgery. There is also increasing evidence of its usefulness as a diagnostic tool for clinicians (Garcia et al., 2021). Otoendoscopy is not widely used within clinic settings due to resource issues, but it does enable image capture onto a screen with subsequent printing of the images and/or storage onto the electronic patient record. Along with clinical history the visual examination of the ear allows the specialist to present a visually supported diagnosis to the child and their parents and to propose what treatment, if any, is needed.
The value of the child and parent being able to see images of the ear canal and eardrum on a screen in real-time during the examination and through captured images (photographs), has not previously been explored.
1.2. Health literacy and child health literacy
Health literacy is a key component of healthcare and has been described as an asset for shared decision-making (Muscat et al., 2021). Core to health literacy is good communication. Low levels of health literacy are linked to numerous negative impacts and improving health literacy can potentially reduce health inequalities (Roberts, 2015). A definition of health literacy based on a recent systematic review proposes that it is the:
ability of an individual to obtain and translate knowledge and information in order to maintain and improve health in a way that is appropriate to the individual and system contexts (Liu et al., 2020, p. 7)
Most work in health literacy has focused on the adult population with less focus on child health literacy. However, the field of child health literacy work is growing. It has extended beyond its original focus on literacy being solely associated with the reading ability or individual agency of a child or young person with a widening of scope to frame child health literacy as being linked to functional, interactive, and critical domains (Nutbeam, 2000, 2008). More recently, work has focused on how contextual, micro, meso, and macro system specific, development-specific, dependency, and power relationships with adults are influential factors (Schulenkorf et al., 2022) that require careful consideration. Although there is no global consensus definition of child health literacy (Bröder et al., 2019, 2020; Schulenkorf et al., 2022), Bröder et al. propose the following definition:
Health literacy of children and young people starts early in life and can be defined as a social and relational construct. It encompasses how health-related, multimodal information from various sources is accessed, understood, appraised, and communicated and used to inform decision-making in different situations in health (care) settings and contexts of everyday life, while taking into account social, cognitive, and legal dependence. (Bröder et al., 2019, p. 11–12)
However, to become be able to exercise health literacy and become literacy agents, children and young people need to have spaces and opportunities created within existing social structures (Bröder et al., 2020). Creating such spaces and opportunities requires health professionals, policy makers, and other stakeholders, including parents, to support the active citizenship and participation of children and young people. Health professionals need to attend to the health literacy needs of the child/young person as well as that of their parent/carer. Skilled and tailored communication between health professionals and the child/young person and their parent/carer is core to enabling children and young people and their parent/carer to be informed, competent and agentic within health care encounters. However, the triadic (professional-child-parent/carer) nature of these healthcare interactions is far from simple to achieve. A recent scoping review of children's participation in triadic (professional-child-parent/carer) medical consultations identified that children's participation in medical consultations was marginal, ranging from 4 to 14% (as determined by measuring speech time, utterances and turns) (van Woerden et al., 2023). In other work, there was clear evidence of the development of “dyadic coalitions between parents and providers such that the child is relegated to the role of passive observer” (Tran et al., 2023, p. 1767).
Verbal communication tends to be the dominant means by which information is shared within the triad and the basis upon which decisions are made. However, verbal communication may also be supplemented or scaffolded by using visual images/visual aids.
1.3. The use of visual images in healthcare
There are many types of visual aids that can be used in healthcare settings to support communication such as photographs, drawings, infographics, and emoticons (Hafner et al., 2022). However, there is, overall, a paucity of research in the area (Williams and Cameron, 2009). Visual aids aim to facilitate attention, comprehension, recall and adherence; this can be most effective for those people with low health literacy (Schubbe et al., 2020) and for conveying complex information (Williams and Cameron, 2009). Visual images in healthcare are most frequently used to support communication related to health messaging and health promotion/education rather than in one-to-one consultations, although there is evidence that consultations can be enriched by using visual aids as they can supplement verbal explanations, and strengthen the clarity of information (Hafner et al., 2022).
Most work on the use and value of visual images in consultations focuses on adult patients; for example, using pain images to strengthen the agency of adult chronic pain patients and increase patient dialogue (Padfield et al., 2018), and using drawings to explain relevant anatomy and proposed surgical interventions to improve communication in adult surgery consultations (Vilallonga et al., 2012). There is less work that addresses the use of patient-specific, medical images (e.g., X-rays and scans) that are generated as part of the diagnostic journey. However, the use of 3-D images alongside a diagnosis have been shown to increase patient understanding, recall and trust in medical information (Phelps et al., 2017, 2021). In other research, 3-D computer images of the patient's ear were used during the consent process to support patient understanding of their condition (cholesteatoma) (Morris and Van Wijhe, 2010).
Research addressing the use of visual images, and more specifically real-time medical images, in clinical consultations with children and young people and their parents is missing.
1.4. Aim of the study
The overall aim of this study was to explore the perceptions, perspectives and satisfaction of parents and children regarding the use of otoendoscope images in outpatient ENT consultations in relation to their understanding of potential ear disease and subsequent treatment.
2. Materials and methods
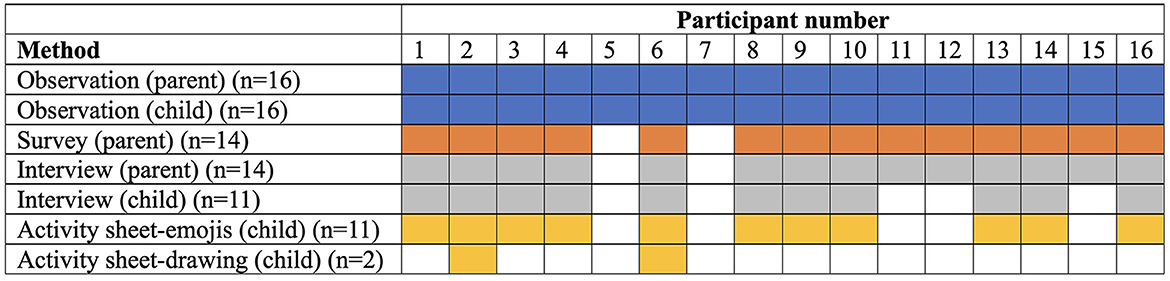
This qualitative descriptive, exploratory study used semi-structured observation, survey, short conversational interviews and a child activity sheet to generate data with children 4–16 years and/or their parents (see Figure 1).
The study was conducted in accordance with Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines (Tong et al., 2007). Ethics approval (London–West London & GTAC Research Ethics Committee REC 20/LO/0186, IRAS ID 264927). This small-scale study was unfunded and undertaken in the months following lockdown when attendance at clinic appointments was starting to return to pre-lockdown conditions.
2.1. Setting
The setting was an ENT clinic (circa 4000+ annual consultations for ear conditions) in a pediatric tertiary hospital in the North-West of England with otoendoscopy being used in <5% of outpatient examinations within this setting. An underpinning rationale for undertaking the study was to provide preliminary evidence on whether increased use of otoendoscope images, as appropriate, would add value to consultations.
2.2. Target population and sampling
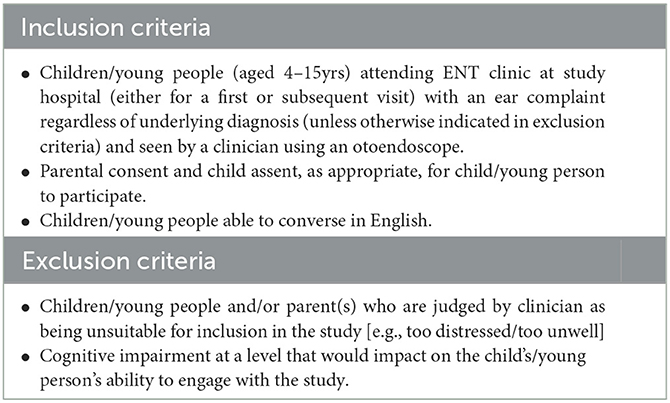
The target population was children and parents/carers attending outpatient ENT clinic at the study hospital (for the key inclusion and exclusion criteria see Table 1). Purposive sampling was used to invite all eligible children (as per inclusion/exclusion criteria) attending 7 ENT outpatient clinics led by two pediatric ENT consultants, and that aligned with researcher availability, during the 5-month recruitment window, to take part in the study. The aim was to recruit a range of children (n = 25) typical of attendance at clinic (e.g., boys and girls, different ages). Invitation packs which included age-appropriate information sheets for the children were sent to parents in advance of clinic attendance, informing them of the study. Recruitment occurred at a routine clinic visit. The researcher approached families once a member of the clinical care team had elicited their interest in the study. Informed consent and assent were undertaken; reasons for declining participation, where possible, were noted. Clinicians undertaking the consultations gave written consent for their participation.
2.3. Methods
All data was collected by one researcher, a female academic children's nurse who was not part of the clinical team. The core data required for each child was demographic and clinical data and observation of their consultation. It was hoped that, subject to availability after the consultation, data could be generated via the other methods.
2.3.1. Clinical data extraction
Basic demographic and clinical data were documented by the child's clinician on a specifically designed clinical data extraction sheet. This included age, gender, reason for referral, duration of problem prompting the referral, other clinicians (primary, secondary, tertiary) involved prior to this referral, and outcome of consultation.
2.3.2. Observation
Observation of the ENT consultations was undertaken with the observer noting the verbal and non-verbal interactions and documenting field notes using a semi-structured template (e.g., what happened, communication, engagement with image during consultation, role the image played in consultation etc.).
The semi-structured template was based on elements of the Pediatric Consultation Assessment Tool (PCAT) (Howells et al., 2010) which was originally designed to measure clinicians' communication behavior with children and their parents/guardian. The PCAT allows scores for observations to be scored 1–7 and although this was initially planned, scoring did not seem to add anything to the observations so was not undertaken. The template in this study aimed to provide structure to the observations and revised to allow documentation of communication specifically relevant to the otoendoscope. The template included prompts for observations focusing on the clinician relating to initial engagement, exploring concerns, preparation for otoendoscope, rapport and explanations during the use of the otoendoscope, feedback about findings and checking understanding, clarification of what happens next. The template also included prompts to document child's responses and behaviors, their apparent understanding, their engagement, and questions about the otoendoscope and images, and engagement in outcome and what happens next. The prompts reflect aspects of communication related to child health literacy such as exploring concerns, checking understanding, clarifying options as well as aspects known to be of importance relating to the use of visual images such as attention and comprehension.
The observer was positioned within the consultation room so that the actions, interactions and behaviors that occurred could be observed whilst ensuring their presence created as minimal disturbance to the consultation as possible.
Following the completion of the consultation and before leaving the clinic, the parents/children could continue to contribute to the study. The following methods were designed in the knowledge that typically children and parents are keen to leave the clinic setting as soon as possible either to go for a promised treat, get home or for the child to return to school or the parent to work. The methods were therefore created to be low burden and quick to complete. The methods were qualitative in design and therefore not validated.
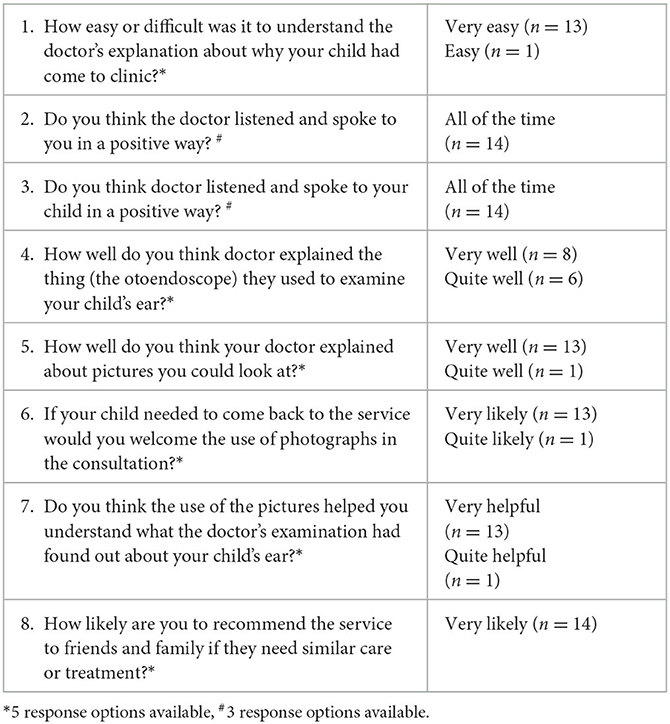
2.3.3. Descriptive survey (parents)
Parents were invited to complete a short paper-based descriptive survey about their experience and perception of the consultation. The survey was composed of eight closed response Likert scale questions. Six questions (questions 1, 4–8) used 5-point scales and the following endpoints were used: question 1 “very difficult” to “very easy”; questions 4 and 5 “very bad” to “very well”; questions 6 and 8 “very unlikely” to “very likely”; question 7 “very unhelpful” to “very helpful”. Questions 2 and 3 used 3-point scales with “none of the time” to “all of the time” as endpoints. Each question had an open response box below each question for any additional comments. Questions focused on the clinician's engagement with parent and child, ease of understanding explanations, and value of the images from the otoendoscope and with the final question being based on the standard “friends and family” evaluation question routinely used by the hospital. For more details about the questions, see Table 2.
2.3.4. Activity sheet (children)
Children were invited to complete an activity sheet consisting of three closed-response questions and a space to create a drawing a picture of their experience. The questions used a 3-option “smiley” face scale (happy-neutral-sad emojis) with the opportunity for the child to create their own emoji if the available emojis did not represent their feelings. The questions asked them about how they felt their appointment had gone, how seeing a picture of their eardrum had made them feel and how interesting they thought it was to see their eardrum.
2.3.5. Conversational interviews (children and parents)
Children and parents could also participate in a short conversational interview (typically around 5–10 min) focusing on the following areas: perspectives of parents/children about the images from the otoendoscope (whether they found them helpful, interesting, reinforced/weakened the consultation), their overall perception of the health professional, and whether their expectations of the consultation were met.
2.4. Analysis and synthesis
All interviews, observational and field notes were transcribed verbatim and analyzed (no software used). Initially each consultation was considered before cross-consultation analysis. The five stages of inductive reflexive thematic analysis were used (familiarization, generating initial codes, searching for themes, reviewing themes and producing report) allowing the shift from descriptive to interpretative analysis (Braun and Clarke, 2021). Survey data were analyzed using basic descriptive statistics for the scale-based data. Initial analysis—coding and development of themes—was conducted by BC (female, PhD, academic children's nurse). The themes and findings were examined and reviewed by the other team members (experienced clinical Ear, Nose, and Throat (ENT) surgeons). The professional backgrounds and personal perspectives of the team members will have informed the study but the adoption of a reflexive approach and transparency about the study (e.g., challenges encountered, limitation of study) aim to allow readers to interpret the findings with appropriate context.
Qualitative data from the observations, interviews, surveys, and activity sheets were synthesized to inform the final set of findings.
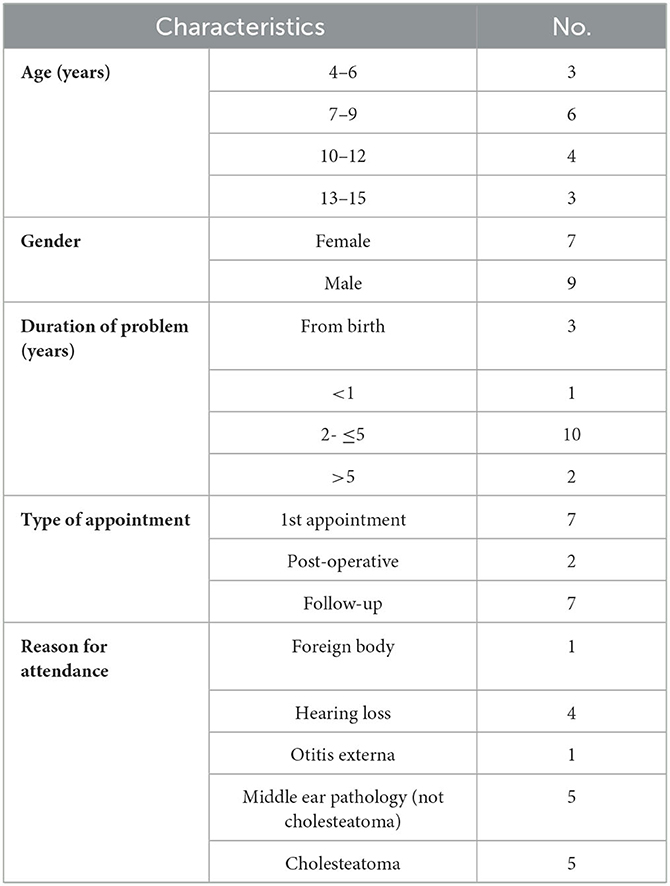
3. Results
Sixteen children (female n = 7, male n = 9, age range 4–15years; mean 9, median 8.5, mode 7 years) and 16 parents (mother n = 13, father n = 3) and three ENT clinicians (consultant n = 2; registrar n = 1) were observed. One boy, aged 7, who attended for post-operative follow-up became distressed at the prospect of wax removal and refused any form of examination with technology so the clinician did not proceed to use the otoendoscope. Duration of problem, type of appointment and reasons for referral are presented in Table 3.
Fourteen parents completed surveys and engaged in a short interview; two parents had to leave clinic immediately after the consultation, so data collection ended after observation. Eleven children completed the activity sheet and engaged in a short interview. Reasons why children did not engage in activity sheets and interview were as follows: left clinic immediately (n = 2), child had limited (n = 1) or no verbal (n = 1) communication, and child declined (n = 1). An overview of participant engagement with the different methods is presented in Figure 2.
3.1. Survey findings
Findings from the 14 parents who completed the survey showed high levels of satisfaction with the various elements of the consultation with most selecting the most positive response option available. Parents found it easy to understand the explanations of why the child had come to clinic and felt that the doctor listened and spoke to them and their child in a positive way “all of the time”. They were positive about the explanations about the otoendoscope and the images and reported they would welcome the use of images in subsequent appointments and said that the use of the images had supported their understanding of the examination. They were all likely to recommend the service to family and friends. The results are reported in Table 2.
3.2. Activity sheet findings
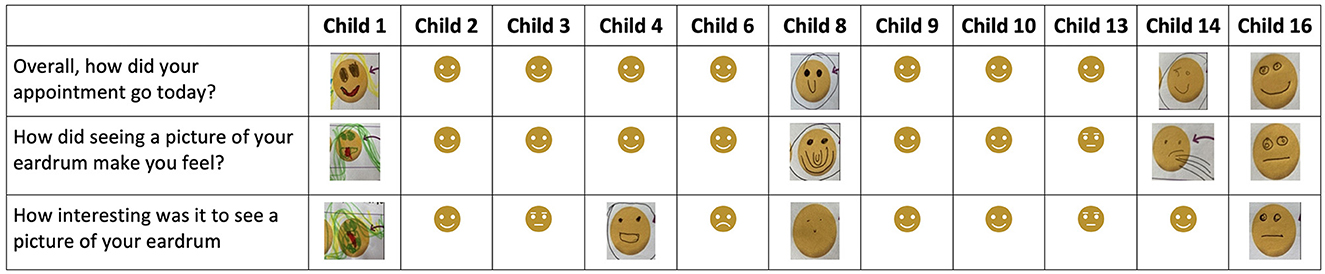
Eleven children completed the emoji component of the activity sheet. Five children drew at least one emoji to represent feelings/responses that they wanted to express that did not fit with the pre-determined response options (see Figure 3) Typically, the responses were positive showing that the children had felt happy or neutral about the three aspects of the appointment. Two children drew emojis representing disgust or reflecting the “yuckiness” of seeing the images. The responses are presented below.
1. Overall, how did your appointment go today? Seven children selected the happy emoji, three drew their own happy emoji, one child chose a neutral emoji.
2. How did seeing a picture of your eardrum make you feel? Six children chose the happy emoji, one child drew a ‘very happy' emoji with lots of smiles, two children drew an emoji representing disgust and vomiting, and one child drew a neutral emoji.
3. How interesting was it to see a picture of your eardrum? Four children selected the happy emoji, and two children drew a happy emoji, two children selected the neutral emoji and one child drew a neutral emoji, one child drew a “yucky” emoji and one child selected the sad emoji.
Three children created additional drawings; one was a scribble picture; one (see Figure 4) showed the child and his mother ready to leave the clinic with big smiles on their faces and the other drawing was of the child's dog who was “waiting for me at home”.
3.3. Qualitative (observation, interview and text-based) findings
In relation to the findings from the observations, interviews, text-based responses from the surveys, one overarching theme and two sub-themes were identified (Figure 5).
Illustrative quotes (from observations, interviews, surveys) are used to support the text linked to participant labels; P1-16, followed by M (mother), F (father), C (child), Clin (clinician). The source of the data is indicated as follows Obs (observation), Int (interview), and Surv (survey).
3.3.1. Grounding perceptions and deepening engagement
The overarching theme draws together the parents and children's responses to seeing both the real-time images viewed during the use of otoendoscope and the screenshot images that were then visible on-screen and provided as printouts during the remainder of the consultation.
Typically, the otoendoscope was used about halfway through the appointment when trust and rapport had already been established through a friendly welcome to the clinic room and ongoing communication that involved the child. Children who required wax removal (by suction) prior to the use of the otoendscope, expressed dislike for the “hoover” due to the noise which was described as “sucky” (P3, C-Int). One child explained “I hate the hoover but he's [consultant] not bad at it” (P10, C -Int). None of the children reported that the endoscope hurt them although most were a little dubious about it before it was used.
Careful explanations were provided about what was involved in using the “special camera” and assurances given that it would not hurt but might feel warm, before gaining the child's assent to proceed. All but one child was calm during the use of the otoendoscope with most children remaining still, being quiet and a little anxious but alert to what was happening as they looked at the images.
The clinicians tailored their explanations to each child and their parent(s) both before and during the use of the otoendoscope with a focus on giving information and providing reassurance. Explanations prior to its use explained it was a camera, they would take some images that would be helpful and that the procedure would not hurt but what sensations they might experience:
So, with the little camera we'll be able to see your eardrum, and you should be able to actually see the difference between your ears and see what's happening. We'll get some images and we can look in detail. It won't hurt but might be a bit warm (P13, Clin-Obs).
During the use of the otoendoscope the focus was on reassuring and providing affirmation to the child and simple explanations about what they were seeing
OK, you're doing well. So this side is fine……this is your eardrum, that's your first bone of hearing and this ear looks normal. And on this side–this shows glue ear…..I'll show you on the pictures as well. [Child's response: ‘Ehhhh, oh my god!] …No it's fine, you're doing great, well done (P16, Clin- Obs).
Again, these explanations were tailored to what could be seen using simple language to describe what could be seen and describing the landmarks they were looking at and whether there was anything “out of the ordinary” such as a change to the form of the eardrum:
See here … It looks a bit wet here and rough and the eardrum is pulled in a bit here…. So now I'll take a photo as well and you can keep it…(P9, Clin-Obs)
The images created a natural talking point that helped deepen the engagement with and communication between the clinician and the parent and child.
The otoendoscope was described as “wonderful technology, it was amazing to see the eardrum and down her ears” (P8,M-Int). The images helped to ground their perceptions making things “more real now I can see what's happened” (P11,M-Int).
Parents found the images really useful as the geography of the ear was a mysterious thing:
I've never seen an eardrum before; it's rare to see it. It's nothing like it is in the textbooks. I didn't know it would look like this. It's reassuring to see it (P4,F-Int).
Sometimes, imagined damage was worse than the actual damage shown via the otoendoscope:
The other surgeon at the other hospital said the hole was big but it's not as big as I'd imagined it was - I thought it'd be nearly as big as the whole eardrum and compared to that it's smaller (P12,M-Int).
For other parents being able to see the extent of disease was worrying but important. For one parent and their child being able to witness the responsiveness of the eardrum to pressure changes was valued. During the consultation the child responded saying “Oh that's weird seeing it move like that” (P8,C-Obs) and then later in the interview her mother explained:
I was really impressed by seeing the way the eardrum moved in response to [child's name] pinching and blowing her nose…. It was good, a relief to see the eardrum was working (P8,M-Int).
All parents (n = 14) who completed the survey responded they would welcome seeing images at their next visit.
Most children were interested in seeing the images and thought it was “good” (P2,C), “exciting” (P1,C), and “cool seeing what's wrong with me” (P13,C). One child explained:
I liked to see what the doctor could see. But I wouldn't put the picture on the wall! (P9,C-Int)
And another child who was very fed-up with the blueberry he had put into his ear canal said that he was glad it was “out” and:
I liked to see the blueberry on the picture. It wasn't nice in my ear and it wasn't nice taking it out (P6,C-Int).
Some children wanted to take the images home, as they wanted “to show people the picture” (P4,C-Obs), others could not see the point):
I can't see the point of taking pictures home… I wouldn't show anyone… I wouldn't show people in school …that's way too weird (P8,C-Int).
However, some children “felt a bit grossed out” (P8,C-Int) when they saw the images and others thought they were “yucky and icky” (P1,C-Int) or “disgusting” (P14,C-Obs); often it was seeing the wax that evoked disgust.
3.3.2. Strengthening understanding
The images that were shown on screen and/or printed out created additional evidence that scaffolded the clinician's verbal explanation about the child's pathology. All parents (n = 14) who completed the survey responded that the images had helped them understand. The images were visual proof that provided additional context and clarity for both children “it helped me understand” (P10,C-Int) and “the pictures… helped me understand my ears” (P8,C-Int). This child's mother explained added to this:
It helped me see and think about what was wrong: Things are clearer in a picture than just an explanation…the two together make it easier to understand what's happening in her ear …and reassuring that things are not too bad” (P8,M-Int)
Another mother explained the value in being able to share the image with the child's father:
I want the print-out to show dad–they're a bit ewwwwhhhh. He'll be interested. Everything is really clear… and so weird to see the way her eardrum bulges (P8,M-Int).
Some parents noted they were visual learners, so the images were particularly helpful, “I'm a visual person so the images really helped me and I like learning as much as I can” (P15,M-Obs). In some situations, the images provided reassurance that all was well as “your eardrum is beautiful!” (P2, Clin-Obs) or that healing had occurred:
So, this basically ear canal and eardrum–nicely healed…looks good. No signs of infection…..that's great healing. We can give you a printout…(P10, Clin-Obs)…..
“That's great that healing's good–good to see…. it's reassuring” (P10,M-Obs).
As one mother explained:
It's good to see the images when they were live as the doctor was looking at them–good to see what the doctor could see and have the doctor explain things as she went–made it clearer about the hole and why he needs ear drops (P7,M-Obs).
Greater understanding meant that parents could “explain things to other people better if I understand” (P8,M-Obs) and being able to take the images home would in turn scaffold their explanations and provide hard evidence to other family members, friends or stakeholders such as teachers:
I want the teachers to see the problem with her ear so they can make small adjustments to help her and to help them understand she can't hear as well as other children (P1,M-Obs).
In some consultations, an additional visual aid—an anatomical model of the ear—was used and this reinforced the explanations and the use of the images:
I liked the way the doctor talked about her ear and shared the pictures and used the model (P9,F-Int).
3.3.3. Supporting decision making
Clearer understanding of the child's ear supported decision-making, for example “the pictures help me understand and will help me make a decision about surgery” (P12,M-Obs). Parents talked of how visualizing the extent of the damage was valuable, albeit concerning:
“I feel better now [I've seen images]. I can see where the bones have been eaten away… worrying to see but good that I could see it with my own eyes” (P11,M-Int).
The images also promoted dialogue between the clinician, child and parents. Parents and some of the children better appreciated the need for intervention and it supported their decision-making. One father noted in the consultation, “I can see it's not right, now you've explained. We need a long term solution” (P4,F-Obs). Where appropriate, images were used to compare a healthy and a diseased ear, providing evidence for the need for intervention:
That's a big difference……..is it quite bad? Do I really need to have an operation? (P13,C-Obs)… We can see on the picture, it's pretty sure you do need an operation to stop it progressing (P13, Clin-Obs).
Being able to see the extent of the problem and to ask questions about different aspects of the image helped parents and children gather the information they needed to ground a decision about whether to follow the clinician's advice for their child to be listed for surgery:
I think it would make sense for the operation having seen all that gray stuff, the gunk (P9,F-Obs).
Although less involved than their parents, the children were invited to be part of decisions throughout the consultation from relatively small decisions such as ‘Which ear do you want me to start with?” through to more involved in treatment-related decisions. One of the children expressed a preference to “do nothing” (P8,C-Obs) with regards to having ear drops which they disliked and wanted to wait and see if the grommet “fell out on its own”. Although most children did not get very involved in the detailed explanations of risks associated with their surgery one child directed a series of very pertinent questions to the consultant including “what percentage of children get balance problems?, when will I have the surgery?, Will the cut be there for the rest of my life?, and what do the drops do?” (P13,C-Obs)
Having the visual evidence as well as the expert words from the clinicians helped promote further dialogue about the implications of declining or delaying surgery and coming to their own conclusion that “I can actually see that surgery is best” (P11,M-Int) Another mother who was initially reluctant to have surgery took all the evidence (clinician opinion and the images) into account to conclude surgery was required:
The hole looks really big…what's the white stuff… will the T tube fall out…. how can you mend the hole? It's a big decision to make about surgery… but it's soooo big… it seems it needs to be done (P12,M-Obs).
4. Discussion
This study aimed to explore the perceptions, perspectives and satisfaction of parents and children from their responses regarding the use of otoendoscope images in outpatient ENT consultations in relation to their understanding of potential ear disease and subsequent medical or surgical treatment. The value in supporting engagement in communication, promoting understanding of the child's condition and informing decision-making are inherently linked with child (and parent) health literacy. This study is novel in that it focuses on the contribution of the real-time otoendoscopic imaging and photographs to the consultation.
Health literacy of both parents (Nielsen-Bohlman et al., 2004; Vaillancourt and Cameron, 2021) and children (Broeder et al., 2017; Velardo and Drummond, 2017) is key to understanding, meaning-making and making informed decisions; parents do want more information (Gorodzinsky et al., 2015). It appears that being able to see their child's ear was normal or see the pathological changes that had occurred was important in both allaying fears, deepening understanding, and clarifying understanding. In a related field, a scoping review of health literacy in pediatric otolaryngology showed that parents do not easily recall verbal or written information and that adding visual components improves parental education (Aaronson et al., 2018); this supports the value of engaging children and parents with visual images (Bröder et al., 2019, p11–12, 38).
Children's health literacy was evident in their engagement in dialogue with their parents and with the clinicians during the consultation. To a greater or lesser extent, most of them were able to demonstrate interactive and communicative health literacy by actively participating in the consultation. Some demonstrated this through active information seeking (Massey et al., 2012) by asking what the images were showing and directing questions to the clinician about their treatment and risks associated with surgery. Others were less active and verbally engaged (passive information seekers) (Massey et al., 2012) but were observed to be clearly interested in the images and were listening and taking note of what was being said. Their participation in the consultation was facilitated by the tailored communication skills of the clinicians and the lengths they went to reduce power relationships (e.g., through welcoming the child) and make their consulting room and the furniture (e.g., the big examination chair) and the technology (e.g., the “hoover” and the camera/otoendoscope) feel less intimidating. The clinicians were supported by the parents who used their skills to engage their child or act as an intermediary, as needed. The depth of health literacy that was evident (either through participation in the consultation or discussed in the interview) varied according to the child's age and capabilities. The variance in engagement and contribution to decision-making is in accord with Bröder et al.'s definition of health literacy for children and young people which acknowledges the need to take account of “social, cognitive and legal dependence” (Bröder et al., 2019, p. 11–12). That children could demonstrate core health literacy skills in a relatively short consultation, for the most part with a clinician they had not previously met, in an alien environment and experiencing an investigation, shows that given the opportunity to engage children are interested in doing so. The clinicians created the space and opportunity in the consultation to promote this engagement; Broder notes this as key for chidren to become “health literacy agents” (Bröder et al., 2020, p. 583). However, it is acknowledged that the amount of children's participation was not measured in this study and that more communication occurred between the parent/carer and the clinician. Although other work shows evidence of the prominence of such dyadic coalitions in child-professional-parent/carer triads (van Woerden et al., 2023), the children in this study were for the most part not passive.
The real-time images of the child's ear and the photographs were valued by the parents and to a great extent by the children, although some expressed a sense of disgust (usually about the wax or other debris) that they could see during the use of the otoendoscope. The value of visual images is known to be linked with their capacity to facilitate attention, comprehension, recall and adherence. Within the context of the consultation there was evidence that they facilitated attention and comprehension and contributed to meaning making and decision-making. This is important to note as there is little literature that examines the patients' perspectives on the role of medical imaging within consultations (Carlin et al., 2014; Pinkster et al., 2022) and none could be found addressing the value of the use of medical images in clinical consultations between the triad of clinician-parent-child. Few validated measures exist to measure patient satisfaction with the use of medical imaging modalities in clinical consultations (Pinkster et al., 2022); none exist for use with children.
What literature does exist on the use of medical imaging within consultations, presents various outcomes. Findings show that the use of medical images in adult populations can be perceived as compelling reinforcement of medical expertise with the power to subdue the patient and gain compliance (Mol, 2003), used to support patients' understanding of themselves, their condition and their treatment (Mol, 2003; Carlin et al., 2014), empower the patient (Phelps et al., 2021), or fail to adequately involve the patient (Cox et al., 2020). Although the expectation is that images will bring benefits, this is not always the case, patients may not always be able to relate to or understand the image. In a study where adult patients, in an orthopedic outpatient consultation, were shown 3-D images generated from their own investigations, the outcomes of using these images were categorized as being truthful (evidence they could trust), empowering (supporting sense-making, promoting confidence in decision-making) or unhelpful (distressing or unhelpful) (Phelps et al., 2021). Findings from the parents and children in our study align with the categories of the image as truthful and empowering. The children and one parent who found the images yucky or disgusting still saw the benefit of seeing the images.
However, findings from this study show that understanding was enhanced and this, in turn, supported decision-making and the promoted interaction and detailed dialogue between the child-parent-clinician. This aligns with findings that some adult patients demonstrated better understanding of pain and built a stronger alliance between doctor and patient when shown their X-rays, MRIs or CT images (Carlin et al., 2014).
The otoendoscope images enabled the inner, invisible and unknown geography of the ear to be visualized by the parents and children; they could see what the clinicians could see. This acted as a more robust shared starting point than reliance on verbal explanation alone. A richer, clearer explanation and understanding was co-constructed through their engagement with the images, and for these parents, the actual image was more reassuring than their imagined images.
Of importance was the opportunity to take the image(s) home with them meant that partners and other stakeholders could view the actual evidence that had been generated within the consultation. This was expected to help widen understanding of the outcomes of the consultation, by providing evidence to the family and friends that all was well or providing robust evidence of the child's hearing problems. This perhaps enhanced the health literacy of other key stakeholders. This evidence of pathology was considered particularly important to support conversations with teachers who could be asked to make adjustments for the child. No published work was found that explores the wider impact of medical images such as otoendoscopy images in influencing understanding outside of the consultation.
Other research on the value of using pictures to convey health information variously uses pictograms, photographs, cartoons, and illustrations and are used for a variety of purposes (e.g., infographics or booklets to aid preparation for procedures, guidance relating to medications), shows value can be gained particularly for low literacy populations (Schubbe et al., 2020).
Although the methodology was robust, the study has some key limitations. It was conducted in one clinic which may not be typical of other clinics sharing otoendoscope images. The sample size was smaller than the proposed 25 participants; this reflected a higher-than-expected number of non-attendances at the scheduled clinics, perhaps reflecting reluctance of some parents to attend a clinic setting post-lockdown. This may have impacted on the depth of data collected and available for interpretation, although by drawing on data across the different datasets gave us confidence that our themes and findings are sufficiently saturated. Recruitment was further constrained by some clinics being canceled unexpectedly and the non-availability of the researcher to attend some clinics within the study window. Additionally, data collection occurred within the busy clinic environment where robust social distancing requirements were still in place. Useful data that could have generated quantitative information to measure the children's participation (e.g., number of utterance, turn-taking and speech time) was not collected. Future research should be multi-center to increase sample size, account for different communication practices across clinics, could be more clearly informed by a health literacy framework and could collect quantitative measures of child participation. Details such as length of time taken to undertake otoendoscopy could be included.
5. Conclusion
The use of otoendoscope images was welcomed by parents who reported that the images scaffolded understanding and helped inform decision-making about treatment and/or provided assurance that their child's eardrum was normal, healing or required follow-up or intervention. Most of the children found the images interesting and thought they were a helpful part of the consultation. It can be argued that the use of real-time imaging and photographs supported child (and parent) health literacy. However, the use of images, on their own, were not responsible for supporting health literacy and informed decision-making; the clinicians' expertise in tailoring communication and creating the space and place for children and parents to engage, participate, become informed and demonstrate health literacy agency was core to the success of the consultations.
The value of the images is that they grounded perceptions and deepened engagement and provided a boundary to the imagination by showing the reality of the child's condition.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by London–West London and GTAC Research Ethics Committee REC 20/LO/0186, IRAS ID 264927. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants or, for the children, by their legal guardian/next of kin. Children provided assent.
Author contributions
BC, TH, SS, and SD contributed to conception and design of the study. TH drafted submission for NHS ethics. BC undertook data collection and the first drafts of the analysis. TH, SS, and SD supported analysis and corrected and refined the manuscript. BC wrote the first draft of the manuscript. All authors contributed to manuscript revisions, read, and approved the submitted version.
Acknowledgments
Thank you to the children, parents, and clinicians for participating in the study and sharing their experiences.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aaronson, N. L., Joshua, C. L., and Boss, E. F. (2018). Health literacy in pediatric otolaryngology: A scoping review. Int. J. Pediatr. Otorhinolaryngol. 113, 252–259. doi: 10.1016/j.ijporl.2018.08.013
Bröder, J., Okan, O., Bauer, U., Schlupp, S., and Pinheiro, P. (2020). Advancing perspectives on health literacy in childhood and youth. Health Promot. Int. 35, 575–585. doi: 10.1093/heapro/daz041
Bröder, J., Okan, O., Bollweg, T. M., Bruland, D., Pinheiro, P., and Bauer, U. (2019). Child and youth health literacy: a conceptual analysis and proposed target-group-centred definition. Int. J. Environ. Res. Public Health 16 doi: 10.3390/ijerph16183417
Broeder, J., Okan, O., Bauer, U., and Pinheiro, P. (2017). Health literacy in children– towards a child-centered conceptual understanding. Eur. J. Public Health. 27, 3. doi: 10.1093/eurpub/ckx187.138
Carlin, L. E., Smith, H. E., and Henwood, F. (2014). To see or not to see: a qualitative interview study of patients' views on their own diagnostic images. BMJ Open 4, e004999. doi: 10.1136/bmjopen-2014-004999
Cox, W. A. S., Cavenagh, P., and Bello, F. (2020). What are the benefits and risks of sharing patients' diagnostic radiological images with them? A cross-sectional study of the perceptions of patients and clinicians in the UK. BMJ Open 10, e033835. doi: 10.1136/bmjopen-2019-033835
Gaddey, H. L., Wright, M. T., and Nelson, T. N. (2019). Otitis media: rapid evidence review. Am. Fam. Physician 100, 350–356.
Garcia, A., Ridge, S., Garcia, J., Cohen, M., and Lee, D. (2021). New perspectives in office-based otoendoscopy and endoscopic ear surgery. Oper. Tech. Otolayngol. Head Neck Surg. 32, 68–78. doi: 10.1016/j.otot.2021.05.002
Gorodzinsky, A. Y., Hong, P., and Chorney, J. M. (2015). Parental knowledge in pediatric otolaryngology surgical consultations: a qualitative content analysis. Int. J. Pediatr. Otorhinolaryngol. 79, 1135–1139. doi: 10.1016/j.ijporl.2015.05.013
Hafner, C., Schneider, J., Schindler, M., and Braillard, O. (2022). Visual aids in ambulatory clinical practice: Experiences, perceptions and needs of patients and healthcare professionals. PLoS ONE 17, e0263041. doi: 10.1371/journal.pone.0263041
Harmes, K. M., Blackwood, R. A., Burrows, H. L., Cooke, J. M., Harrison, R. V., and Passamani, P. P. (2022). Otitis media. Front. Cell. Infect. Microbiol. 12, 1063153. doi: 10.3389/fcimb.2022.1063153
Howells, R. J., Davies, A., Silverman, J., Archer, J., Mellon, A., et al (2010). Assessment of doctors' consultation skills in the paediatric setting: the Paediatric Consultation Assessment Tool. Arch. Dis. Child. 95, 323–329. doi: 10.1136/adc.2008.146191
Kozin, E. D., Sethi, R. K. V., Remenschneider, A. K., Kaplan, A. B., Portal, D. A. D., Gray, S. T., et al. (2015). Epidemiology of otologic diagnoses in United States emergency departments. Laryngoscope 125, 1926–1933. doi: 10.1002/lary.25197
Leach, A. J., Homøe, P., Chidziva, C., Gunasekera, H., Kong, K., Bhutta, M. F., et al. (2020). Panel 6: Otitis media and associated hearing loss among disadvantaged populations and low to middle-income countries. Int. J. Pediatr. Otorhinolaryngol. 130, 109857. doi: 10.1016/j.ijporl.2019.109857
Liu, C., Wang, D., Liu, C., Jiang, J., Wang, X., Chen, H., et al. (2020). What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam. Med. Community Health 8 doi: 10.1136/fmch-2020-000351
Macharia, I. M. (2016). Common ear conditions underdiagnosed at primary level. Commun. Ear Hear. Health 13, 1–2. doi: 10.56920/cehh.50
Massey, P. M., Prelip, M., Calimlim, B. M., Quiter, E. S., and Glik, D. C. (2012). Contextualizing an expanded definition of health literacy among adolescents in the health care setting. Health Educ. Res. 27, 961–974. doi: 10.1093/her/cys054
Midgley, E. J., Dewey, C., Pryce, K., and Maw, A. R. (2000). The frequency of otitis media with effusion in British pre-school children: a guide for treatment. Clin. Otolaryngol. Allied Sci. 25, 485–491. doi: 10.1046/j.1365-2273.2000.00360.x
Mol, A. (2003). The Body Multiple. Ontology in Medical Practice. Durham, NC.: Duke University Press.
Morris, D. P., and Van Wijhe, R. G. (2010). Cholesteatoma in three dimensions: a teaching tool and an aid to improved pre-operative consent. J. Laryngol. Otol. 124, 126–131. doi: 10.1017/S0022215109991216
Muscat, D. M., Shepherd, H. L., Nutbeam, D., Trevena, L., and McCaffery, K. J. (2021). Health literacy and shared decision-making: exploring the relationship to enable meaningful patient engagement in healthcare. J. Gen. Intern. Med. 36, 521–524. doi: 10.1007/s11606-020-05912-0
NICE (2008). “Otitis media with effusion in under 12s: surgery,” in Clinical Guideline [CG60]. London: National Institute for Health and Care Excellence. Available online at: www.nice.org.uk/guidance/cg60
Nielsen-Bohlman, L., Panzer, A. M., and Kinding, D. (2004). Health Literacy: a Prescription to End Confusion. Washington, D.C.: National Academies Press.
Nutbeam, D. (2000). Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 15, 259–267. doi: 10.1093/heapro/15.3.259
Nutbeam, D. (2008). The evolving concept of health literacy. Soc. Sci. Med. 67, 2072–2078. doi: 10.1016/j.socscimed.2008.09.050
Padfield, D., Omand, H., Semino, E., Williams, A. C., and Zakrzewska, J. M. (2018). Images as catalysts for meaning-making in medical pain encounters: a multidisciplinary analysis. Med. Humanit. 44, 74–81. doi: 10.1136/medhum-2017-011415
Phelps, E. E., Wellings, R., Griffiths, F., Hutchinson, C., and Kunar, M. (2017). Do medical images aid understanding and recall of medical information? An experimental study comparing the experience of viewing no image, a 2D medical image and a 3D medical image alongside a diagnosis. Patient Educ. Couns. 100, 1120–1127. doi: 10.1016/j.pec.2016.12.034
Phelps, E. E., Wellings, R., Kunar, M., Hutchinson, C., and Griffiths, F. (2021). A qualitative study exploring the experience of viewing three-dimensional medical images during an orthopaedic outpatient consultation from the perspective of patients, health care professionals, lay representatives. J. Eval. Clin. Pract. 27, 333–343. doi: 10.1111/jep.13417
Pinkster, H., Meester, A., Ijpma, F., Taal, E., Kraeima, J., and Klooster, P. (2022). Developing a patient satisfaction measure for imaging-based patient information during clinical consultations. Patient Exp. J. 9, 3. doi: 10.35680/2372-0247.1668
Restuti, R. D., Tamin, S., Nugroho, D., Hutauruk, S., and Mansyur, M. (2022). Factors affecting the occurrence of otitis media with effusion in preschool and elementary school children: a comparative cross-sectional study. BMJ Open 12, e065291. doi: 10.1136/bmjopen-2022-065291
Roberts, J. (2015). Local Action on Health Inequalities: Improving Health Literacy to Reduce Health Inequalities (PHE publications gateway number: 2015329). London. Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/460709/4a_Health_Literacy-Full.pdf
Schubbe, D., Scalia, P., Yen, R. W., Saunders, C. H., Cohen, S., Elwyn, G., et al. (2020). Using pictures to convey health information: a systematic review and meta-analysis of the effects on patient and consumer health behaviors and outcomes. Patient Educ. Couns. 103, 1935–1960. doi: 10.1016/j.pec.2020.04.010
Schulenkorf, T., Sørensen, K., and Okan, O. (2022). International understandings of health literacy in childhood and adolescence-a qualitative-explorative analysis of global expert interviews. Int. J. Environ. Res. Public Health 19 doi: 10.3390/ijerph19031591
Simon, F., Haggard, M., Rosenfeld, R. M., Jia, H., Peer, S., Calmels, M-N., et al. (2018). International consensus (ICON) on management of otitis media with effusion in children. Eur. Ann. Otorhinolaryngol Head Neck Dis. 135., S33–S39. doi: 10.1016/j.anorl.2017.11.009
Tong, A., Sainsbury, P., and Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 19, 349–357. doi: 10.1093/intqhc/mzm042
Tran, B. Q., Mendoza, M. M., Saini, S. K., and Sweeny, K. (2023). Let the Kid Speak: Dynamics of Triadic Medical Interactions Involving Pediatric Patients. Health Commun. 38, 1762–1769. doi: 10.1080/10410236.2022.2031450
Vaillancourt, R., and Cameron, J. D. (2021). Health literacy for children and families. Br. J. Clin. Pharmacol. 88, 4328–4336. doi: 10.22541/au.160029850.03204485
van Woerden, C. S., Vroman, H., and Brand, P. L. P. (2023). Child participation in triadic medical consultations: a scoping review and summary of promotive interventions. Patient Educ. Couns. 113, 107749. doi: 10.1016/j.pec.2023.107749
Velardo, S., and Drummond, M. (2017). Emphasizing the child in child health literacy research. J. Child Health Care. 21, 5–13. doi: 10.1177/1367493516643423
Vilallonga, R., Fort, J. M., Iordache, N., Armengol, M., Clèries, X., and Solà, M. (2012). Use of images in a surgery consultation. Will it improve the communication? Chirurgia (Bucur) 107, 213–217.
Whitburn, S., Costelloe, C., Montgomery, A. A., Redmond, N. M., Fletcher, M., Peters, T. J., et al. (2011). The frequency distribution of presenting symptoms in children aged six months to six years to primary care. Prim Health Care Res. Dev. 12, 123–134. doi: 10.1017/S146342361000040X
Keywords: otoendoscopy, medical imaging, consultation, child (and parent) health literacy, decision-making, Ear, Nose, Throat (ENT)
Citation: Carter B, Hampton T, Sharma S and De S (2023) Grounding perceptions: the value of otoendoscopy images in strengthening parents and children's understanding and decision making in a pediatric ENT clinic. Front. Commun. 8:1215262. doi: 10.3389/fcomm.2023.1215262
Received: 01 May 2023; Accepted: 15 August 2023;
Published: 04 September 2023.
Edited by:
Parul Jain, Ohio University, United StatesReviewed by:
Mary Hughes, Trinity College Dublin, IrelandUttara Manohar, Eastern Michigan University, United States
Copyright © 2023 Carter, Hampton, Sharma and De. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernie Carter, YmVybmllLmNhcnRlckBlZGdlaGlsbC5hYy51aw==
 Bernie Carter
Bernie Carter Thomas Hampton
Thomas Hampton Sunil Sharma2
Sunil Sharma2