
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Commun., 18 July 2023
Sec. Health Communication
Volume 8 - 2023 | https://doi.org/10.3389/fcomm.2023.1110558
Objective: To explore how expressions of uncertainty are used and understood by patients and their health practitioners (HPs) in language-concordant vs. language-discordant consultations and to invoke CAT to identify the use of communication strategies, with a focus on HPs.
Methods: This qualitative study encompassed 15 transcribed video and audio recordings of medical consultations between monolingual and bilingual patients and HPs captured in an Australian Emergency Department (ED). HPs and patients also completed a Language Background Questionnaire (LBQ). The main outcome measures included the number and type of expressions of risk and uncertainty used by patients and HPs and the strategies used by HPs to accommodate their patients' conversational needs.
Results: A total of 15 representative conversations were analyzed, involving two bilingual and two monolingual HPs and 14 patients (of whom five were bilingual). All conversations contained epistemic expressions (e.g., probably), which were used more frequently by patients and more often by bilingual patients. HPs accommodated the patients effectively overall, but some bilingual patients showed difficulties in their understanding.
Conclusion: All interlocutors expressed uncertainty to varying degrees. The greater use of uncertainty expressions by (bilingual) patients suggests that HPs could increase their communicative effectiveness by attending specifically to their patients' uncertainty talk. Such talk may reflect a need for reassurance. For culturally and linguistically diverse patients, it may reflect issues with comprehension.
Uncertainty in healthcare is unavoidable. Health practitioners (HPs) are aware of the uncertainty of diagnosis, treatment options, and treatment outcomes, and they acknowledge and accept its existence. However, they may be less aware of how their communication of uncertainty is understood by patients, who may also perceive uncertainty in communication about their health less favorably (Gala et al., 2021). One of the reasons for that is the nature of uncertainty. Upon reviewing existing theoretical conceptions in healthcare, Han defined uncertainty as a subjective perception of ignorance (Han et al., 2011). This broad definition reflects the complex nature of uncertainty and captures two important meanings: subjectivity and a lack of knowledge or information. In its metacognitive conception, the existence of uncertainty is determined by both the absence of understanding and the presence of conscious awareness. When a person gains understanding or loses their awareness of ignorance, they move to a different epistemic state, i.e., certainty, ignorance, or knowledge (Han, 2021).
The success of health communication depends on how HPs manage to communicate uncertainty to their patients. Communication of uncertainty becomes even more important when it concerns bilingual patients. Language discordance can threaten the quality of care because culturally and linguistically diverse patients are less likely to seek healthcare, participate in medical decisions, adhere to health-promoting behaviors, and attend follow-up appointments (Ferguson and Candib, 2002; Paternotte et al., 2015; Simon et al., 2019; Phillips et al., 2020). These patients may perceive differently the process of decision-making and (un)certainty of the available treatment options due to language barriers and cultural differences (Schinkel et al., 2019).
Miscommunication can also occur when HPs provide healthcare in their non-preferred, other language. International doctors describe language barriers such as grammar, pronunciation, a lack of the relevant subject-area vocabulary, and a lack of the professional biomedical vocabulary (for example, different names of medicines) as threats to the communication with their patients (Gasiorek and Van De Poel, 2012; Skjeggestad et al., 2017). In some regions, where bilingualism or multilingualism is common among HPs, miscommunication can result when HPs need to convey medical knowledge in their less proficient language (Pun et al., 2017). The use of interpreters is not always possible in all healthcare settings. Immigrant patients and HPs frequently use family members (including minors) and gestures to facilitate communication (Fabienne et al., 2019). However, even the use of professional interpreters or another type of language brokering does not guarantee that the messages will be conveyed fully and truthfully (Richardson et al., 2006; Butow et al., 2011), especially when the information provided by practitioners is inconsistent or confusing (Hsieh and Terui, 2015).
Effective communication is critical to ensure high-quality healthcare. However, various existing communication barriers negatively impact on the clarity with which health information is communicated and on how it is understood. Language barriers are one of these obstacles, with HPs admitting that clinical care given to patients with limited English abilities is different to care given to English-speaking patients (White et al., 2018). While verbal expressions of uncertainty are used in more than 70% of clinical visits (Gordon et al., 2000), no research has specifically targeted expressions of uncertainty used in language-concordant versus language-discordant communication between HPs and their patients.
This report is one of the first attempts to analyze expressions of risk and uncertainty used in language-concordant and language-discordant care. We will first look at expressions that were commonly used by HPs and their patients during consultations at an ED of an Australian hospital. We will then apply communication accommodation theory (CAT) to explore how such consultations unfold and which accommodation strategies were used by HPs to communicate risk and uncertainty to their patients. The CAT framework has been successfully applied before to understand practitioner–patient communication (Chevalier et al., 2018, 2020; Jones et al., 2018); however, to the best of our knowledge, this is the first attempt to observe how CAT strategies are used by HPs and patients for communication of risk and uncertainty in EDs. CAT describes five communication strategies, namely interpretability (focusing on speakers' conversational competence), approximation (adjustment of speech patterns), discourse management (management of different environments and contexts), emotional expression (empathy and reassurance demonstrated by speakers), and interpersonal control (use of power and roles by speakers) (Chevalier et al., 2017, 2020). When these strategies are used well, they result in good communication and also reduce communication barriers between speakers (Pines et al., 2021).
Our preliminary findings1 are based on the analyses of 15 consultations with four HPs who performed between three and five consultations each, capturing conversations between (1) monolingual speakers of English; (2) bilingual speakers of English as their second/other language; and (3) a monolingual speaker and a bilingual speaker of English (see Table 1). The HPs included one doctor and three nurses. The 15 conversations analyzed here represent a total of 77.6 min of recorded patient–HP interactions (mean length of consultation = 5.2 min; range = [2.57 min, 11.51 min]; median = 5 min).
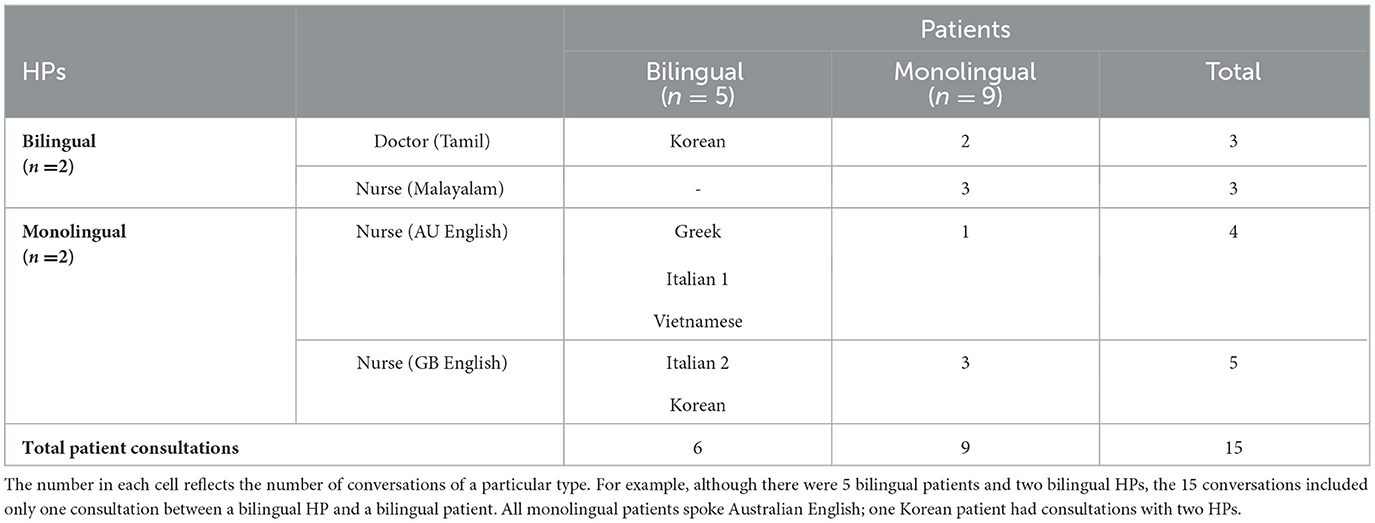
Table 1. Overview of the 15 conversations analyzed herein, the combination of speakers by language background and number of participants (n) per group.
The HPs consisted predominantly of nurses and doctors working at the ED who had learned about the research via notices and through daily scrums. HPs willing to participate provided informed consent. They were also asked to complete a Language Background Questionnaire (LBQ)2. We used the LBQ to establish, in addition to the conversations themselves, how proficient the speakers were in English (if it was their second language). We did that to be able to understand differences in how conversations unfolded that could be associated with (lower) proficiency (particularly speech and comprehension) and with being bilingual. The LBQ consisted of 14 items and included demographic and language background questions (e.g., place of birth, level of education, languages spoken). HPs and patients were further asked to rate their ability to speak, read, understand, and write English, and where English was not their first language, the patients rated their abovementioned abilities in their first language (1 = no ability at all, 2 = very little, 3 = moderate, 4 = very good, and 5 = native-like ability).
All patients who presented to ambulatory care and who were identified in triage as meeting the inclusion criteria (i.e., Australasian Triage Scale 4 or 5). The National Triage Scale (NTS) for Australian Emergency Departments is used by most EDs to identify patient care priorities. Every patient who presents to an ED is assigned a triage category based on the nature of their medical problem and the need for health care. The NTS is a 5-point scale, with category 1 being resuscitation and category 5 being non-urgent (Considine et al., 2000). We worked with a duty nurse to establish which patients would be observed by participating HPs. We approached those patients in the waiting area to explain the research and establish if they wished to participate. Upon obtaining the patient's consent, we alerted the respective HP.
There were 14 patients, of whom five spoke English as their second/other language with different levels of proficiency (see Table 2 for language proficiency details). All monolingual patients were born in Australia, and only one patient was of male sex. In one consultation with a monolingual patient, a family member was present. The bilingual patients spoke Greek, Italian, Korean, and Vietnamese as their first languages; two of the patients were women. None of the consultations with bilingual patients were assisted by interpreters.
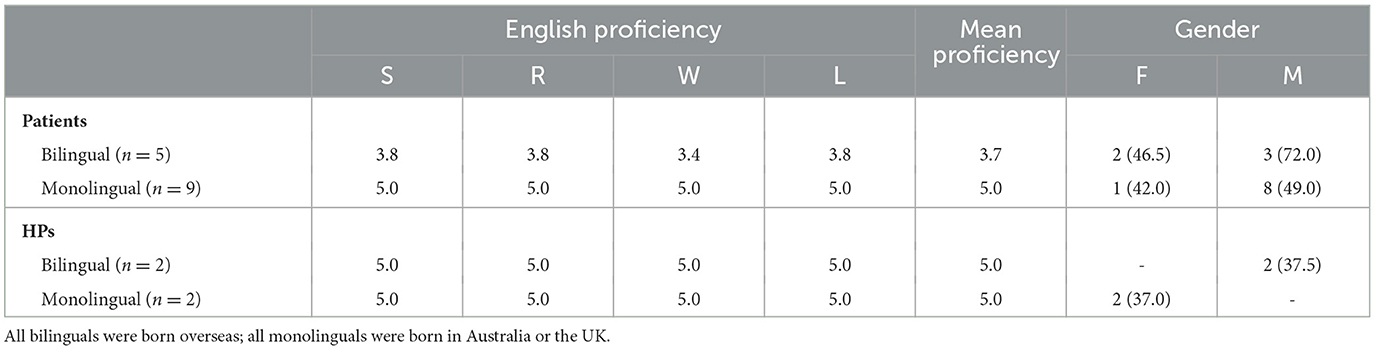
Table 2. Demographics of patients and HPs, including mean self-rated English proficiency in Speaking (S), Reading (R), Writing (W), and Listening (L) (1 = no ability at all; 5 = native-like ability), and Gender (Female (F) and Male (M) (with mean age in brackets)).
HPs and patients provided consent prior to their participation. The HPs completed an LBQ on the day or prior. Patients completed the LBQ before or after their consultation. All patients (but not the HPs) also completed a brief post-consultation questionnaire to rate their satisfaction with the communication experience (using a 5-point Likert scale, with 1 = Not at all and 5 = Definitely).
Real-life conversations between patients and their HPs were video- and audio-recorded. Most conversations occurred in private areas of the ED. Some of the conversations occurred in the ambulatory care waiting room when no other patients or staff were present. All participants agreed to both audio- and video-recording, and reassurance of anonymity was provided. The actual names of HPs and patients were not used. The data were collected across a 2-month period in 2021.
The recordings were transcribed verbatim by a professional transcriber and verified by the research team by comparing transcripts with original video recordings to reconcile any discrepancies where applicable. The transcripts formed the basis of the linguistic and qualitative analyses. Transcripts were coded twice, initially for linguistic expressions of uncertainty and then for communication strategies used by HPs. To understand how patients and HPs talked about and negotiated their understanding of uncertainty and risk, we first identified which expressions of risk and certainty (epistemic expressions) were used in practice. Our linguistic analyses focused on the occurrence and use of (1) words reflecting different degrees of certainty (i.e., epistemic adverbs or adverbs which refer to the speaker's knowledge, e.g., probably, possibly, maybe); (2) expressions reflecting different degrees of uncertainty (i.e., epistemic parentheticals, e.g., I think); and (3) verbs that indicate different degrees of certainty (i.e., modal verbs, e.g., can, could). We also noted hedges such as sort of and like; however, they were excluded from our analysis because, consistent with observations by Mulder et al. (2019), hedging captured by sort of was only used by our monolingual Australian English speakers and appeared as a pragmatic marker rather than an uncertainty expression. Additionally, we explored the communication strategies used by HPs using qualitative analyses informed by communication accommodation theory (CAT) (Gallois et al., 2005; Giles, 2016). The transcripts were coded for the occurrence of the CAT strategies using a coding system developed for CAT (Chevalier et al., 2017, 2020). See the Appendix for an overview of the coding scheme.
During their conversations with their HP, collectively our patients used 57 words and phrases that reflected different degrees of certainty (epistemic expressions) (total number of words = 5,003). Six of these were unrelated to their medical problems and therefore excluded from our analysis. The remaining 51 epistemic expressions were used to describe current symptoms and medical history (n = 40), query the likely diagnosis and/or treatment (n = 7), and answer lifestyle questions (n = 4).
Modal verbs (e.g., could, may) were the most common (n = 32), followed by epistemic adverbs (e.g., maybe; n = 10) and epistemic parentheticals (e.g., I think; n = 9). For example, in Excerpt 1, a bilingual patient used “could” when trying to explain her elevated blood count numbers to a nurse.
Excerpt 1—Interaction between patient (woman; age 71; bilingual Italian/English) and nurse (woman; age 41; monolingual British English)
Patient: And when, when I did this blood test…
Nurse: Yeah?
Patient: You know, to see if they were elevated, one of them was doubled. So, it could be, you see, my head is just hurting.
Although bilingual and monolingual patients used approximately the same number of epistemic expressions overall (bilinguals = 25; monolinguals = 26), our HPs had more consultations with monolingual patients (n = 9) compared to consultations with bilingual patients (n = 6). Bilingual patients used more epistemic expressions per conversation (mean = 4.16, SD = 3.54) than monolingual patients (mean = 2.89, SD = 2.95). We calculated the mean frequency per conversation rather than per total number of words because some patients engaged in more small talk. Such shifts to small talk in medical consultations may not always be obvious (Hudak and Maynard, 2011), making it difficult to find clear boundaries between small talk and relevant information.
The somewhat greater use of epistemic expressions in bilingual patients can be explained by the bilinguals' first language and/or their low English proficiency and word-finding difficulties. Interestingly, both monolingual and bilingual patients primarily used probably and maybe to reflect their uncertainty. These adverbs were mainly used for the description of symptoms and in response to lifestyle questions.
In Excerpt 2 below, a doctor asked a bilingual patient about her alcohol intake. The patient used an epistemic adverb maybe because she was not sure when she last had a drink. As the patient had some gastro-related symptoms, it is possible that she felt a need to provide more accurate information about her alcohol consumption and she decided to indicate her uncertainty to the doctor by using the adverb maybe. The doctor further asked about the number of drinks on occasions when the patient consumed alcohol and confirmed that the patient's reply was sufficient by using “Sure.”
Excerpt 2—Interaction between patient (woman; age 22; bilingual Korean/English) and doctor (man; age 29; bilingual Tamil/English)
Doctor: Um, do you drink?
Patient: Like alcohol?
Doctor: Yep.
Patient: Yeah.
Doctor: Every day?
Patient: No, no.
Doctor: When was the last time?
Patient: Like last week.
Doctor: Ok, right.
Patient: 2 weeks, maybe.
Doctor: How much do you drink, when you drink?
Patient: Not much.
Doctor: Not much.
Patient: 1-2 drinks.
Doctor: Sure.
Overall, the HPs used 52 epistemic expressions (total number of words = 4,9863). On average, bilingual and monolingual HPs used approximately the same number of epistemic expressions across their conversations (bilinguals, n = 19, mean = 3.16, SD = 1.83; monolinguals, n = 33, mean = 3.66, SD = 2.40). Six of these were small talk related4 and therefore excluded from our analysis. As was the case for our patients, modal verbs were also the most common for HPs (n = 27).
Excerpt 3—Interaction between patient (woman; age 22; bilingual Korean/English) and doctor (man; age 29; bilingual Tamil/English)
Patient: Yeah, that hurts.
Doctor: That's fine?
Patient: Yeah [grunts in pain]
Doctor: Right here?
Patient: Ah, yeah.
Doctor: Deep breath in. Good. And again. I think you might have gallstones. No burning when you urinate?
HPs also used epistemic adverbs (e.g., maybe; n = 13) and epistemic parentheticals (e.g., I think; n = 6). We found no uses of hedges and, importantly, HPs often directly acknowledged certainty and uncertainty, including in some instances their own uncertainty (e.g., about the cause of a medical condition). One of the possible explanations is that HPs may have been trained in how to discuss diagnostic uncertainty with their patients. Although there are no standard instructions and approaches to discussing uncertainty for patients discharged from the ED with diagnostic uncertainty (McCarthy et al., 2020), recent studies have reported on the inclusion of training in how to discuss diagnostic uncertainty with patients in medical degree programs (McCarthy et al., 2020; Poluch et al., 2022). Specifically, medical students are instructed to explicitly tell patients that there is no confirmed explanation (diagnosis) for what the patient has been experiencing (McCarthy et al., 2020; Poluch et al., 2022). In the recorded data, some HPs directly acknowledged uncertainty by saying: “I don't know,” which may explain why they used epistemic adverbs less frequently than their patients.
The HPs' use of CAT strategies, either to address uncertainty expressed by their patients or when they themselves were uncertain of their knowledge, was evident in all conversations. Our HPs often adopted appropriate communication strategies to try to reduce uncertainty for their patients. It was supported by self-report measures, which showed that our patients were highly satisfied with the standard of communication with HPs. Although there is some evidence that the results of self-report measures may not be sufficient to identify whether HPs demonstrated accommodative communication or not (Fossli Jensen et al., 2011), these results were supported by our analysis of video-recorded consultations.
To ensure clarity, some HPs admitted to a lack of knowledge about a health issue. Doing so may help to reduce ambiguity and make the conversation clearer (i.e., helps with interpretability). We also noticed evidence of this “ownership” of lack of expertise when, in one consultation, the multilingual HP repeatedly said “I don't know,” also clearly stating that the particular health problem was outside his expertise (“We'll have to talk to Orthopedics”). His monolingual patient appeared to accept this but did express initial disappointment using the colloquial “Cool-o.”
The conversations showed that the patient's level of English proficiency changed the way their HP talked: HPs adjusted their talk to increase clarity for patients with limited English proficiency (interpretability). Interpretability refers to an ability to explain things in a clear and concise way and check the understanding of the other party. For example, in Excerpt 3, a nurse changed “How is your vision?” to a simpler question: “Can you see out of your eye?.” However, after receiving a minimal response (“Yeah”), she double-checked with an even simpler question: “You can see?.” The modal verb can was used here to reduce uncertainty. The fact that the patient had limited English prompted the nurse to use simpler phrasing and reduce uncertainty progressively. The nurse also successfully maintained conversation by back-channeling: “No. OK” (discourse management). Discourse management includes different ways of managing a conversation by, for example, taking the lead or sharing topic selection, (not) allowing turn taking, etc. (Hehl and McDonald, 2014).
Excerpt 4—Interaction between patient (man; age 68; bilingual Vietnamese/English) and nurse (woman; age 33; monolingual Australian English)
Patient: Yes. I called my, my… eh… you know they have, with the [unclear]
Nurse: Ambulance?
Patient: He go “What are you?” I don't know.
Nurse: It didn't help.
Patient: Ohh, eye was sore
Nurse: Did it help your eye, or no?
Patient: No.
Nurse: No. Ok.
Patient: Oh, [crosstalk]
Nurse: Um, ok, but how's your vision? Can you see out of your eye?
Patient: Yeah.
NU: You can see?
In Excerpt 5, the same nurse correctly interpreted another bilingual patient who forgot the word “CT,” while talking about potential procedures for his leg (interpretability). The patient forgot this word twice. The second time, he also used an epistemic adverb maybe along with an uncertainty gesture, which helped the nurse to identify the problem. In her reply, the nurse confirmed that it was CT and backchanneled by using “yeah” and “yep.” Although the patient had problems with remembering the word “CT,” the nurse did not use elderspeak, which is sometimes mistakenly viewed as an approximation strategy, but rather demonstrated approximation by watching and listening to the patient's verbal and non-verbal expressions to indicate that she was following/hearing.
Excerpt 5—Interaction between patient (man; age 72; bilingual Italian/English) and nurse (woman; age 33; monolingual Australian English)
Nurse: It's easy, isn't it? I don't mind at all. Well, I'll [unclear] the room, and the doctor will see you for your leg, and hopefully he can sort it out for you today.
Patient: Well, maybe he does, what is it, what do they call this [gestures]?
Nurse: CT potentially, yeah. Yeah, we'll see what they say.
Approximation refers to the ways in which the speaker adjusts their style in response to the other person. These adjustments can be manifested in the rate of speech, accents, pauses, or non-verbal behaviors (Hehl and McDonald, 2014). In the analyzed conversations, HPs were comfortable with changing the way they spoke, more formally or casually, to match their patient's manner of speech or what they believed their patient's preferred speech register to be. For example, in Excerpt 6, in a language-discordant consultation, a bilingual doctor used a colloquial form of address “mate,” which was accepted by his monolingual patient who reciprocated. The patient also used an epistemic adverb probably to show his uncertainty about the exact time of the lump's appearance.
Excerpt 6—Interaction between patient (man; age 37; monolingual Australian English) and doctor (man; age 29; bilingual Tamil/English)
Doctor: What can I do for you, mate?
Patient: Mate, looks lumpy. It's popped up probably in the past 24 hours.
Doctor: Yep. Ok.
In the colloquial form of address used in Excerpt 6, “mate” is considered to be truly Australian and encapsulates everything it means to be Australian (Rendle-Short, 2009). It is worth noting that, although the doctor was overseas born, he had a pronounced Australian accent and had completed his education in Australia. His successful approach to his Australian patient, and the effective approximation strategy involving something as simple as the use of 'mate', enabled him to build trust with his patient almost within one turn.
HPs also used epistemic expressions to validate patients' concerns and provide reassurance (emotional expression). In Excerpt 7, the nurse provided reassurance to the patient. She used the adverb of course to validate her patient's concerns regarding some water in the lungs. After acknowledging the patient's concerns, the nurse regained control over the conversation (discourse management). The use of the epistemic adverb in this conversation helped to provide reassurance to the patient.
Excerpt 7—Interaction between patient (woman; age 71; bilingual Italian/English) and nurse [woman; age 41; monolingual English (UK)]
Nurse: Yeah. Oh, we'll get you checked out by the doctor.
Patient: Yeah, it would be good. I'm a little bit worried about the water in the lungs.
Nurse: Yes. At Exact Radiology.
Patient: Yeah, of course. So the X-ray's about 6 weeks ago, hey?
Overall, the results of our preliminary analysis showed that HPs attempted to accommodate to their patients. Both communication parties (HPs and patients) were striving to accommodate to each other, and the more the HPs accommodated to their patients, the more collaborative the patients were. The use of epistemic expressions was mostly justified and clear; however, on some occasions HPs should reconsider their use of expressions of (un)certainty if they do not add clarity to the conversation.
Our preliminary findings showed that, while the communication of risk and uncertainty we observed was mostly clear and successful, there were instances where the patient's understanding was in doubt (e.g., when the HP re-checked their patient's ability to see) and where it was unclear whether the HP's use of an expression carried the same meaning for the patient (e.g., communicating and understanding the likelihood of gallstones between non-native English speakers). While these examples of possible (if slight) misunderstandings may not have had a significant impact on the patient, there would be situations resulting in unfortunate patient outcomes, affecting both patients' trust in doctors and their intention to seek a second opinion (see also, for example, Blanch-Hartigan et al., 2019).
As previous research shows, even native English speakers from different speech communities (e.g., Canada and Australia) may have a slightly different understanding of words of risk and certainty such as probably and possibly in a healthcare context (Segalowitz et al., 2016). Differences in how these words are understood are more pronounced in bilingual speakers. For example, a UK study on the use of may and might in educational and legal contexts showed that non-native English speakers rated expressions involving may as events that were much more likely to have happened than those expressed with might (Filipović, 2016). This difference in understanding of may and might could have had relevance in at least one of the conversations between a multilingual HP and a bilingual patient. The HP used “might” to indicate a certain likelihood of gallstones: “I think you might have gallstones.” Whether might was used intentionally to suggest a smaller chance of gallstones was unclear from the context, but it is conceivable, given that the HP was a non-native English speaker who, possibly, makes a different likelihood distinction between may and might. Unfortunately, the patient's interpretation of the diagnosis is unknown because of their minimal response. However, given that they were also a non-native English speaker, the pronouncement may have been reassuring if they similarly interpreted might as a lower possibility of gallstones (compared to the use of may). Our example shows not only that there is a greater likelihood of miscommunication when expressions of uncertainty and risk are used but also that such miscommunication may be more likely when speakers do not share and/or use the same language (in this case English) or when they share the same native language but not the same culture.
Even direct and explicit expression “I don't know” may express different degrees of uncertainty in health communication (Menichetti et al., 2021). Therefore, to ensure that the patients fully understand what they are told, we recommend paying particular attention to the clarity of messages that contain expressions of uncertainty and risk, not only with bilingual patients but also with native English speakers from culturally diverse backgrounds (e.g., Singapore, South Africa). HPs should also pay particular attention to expressions of uncertainty used by their patients, because these may reflect an unspoken request for reassurance or, in the case of culturally and linguistically diverse patients, insufficient knowledge of English or uncertainty regarding cultural norms and expectations in healthcare, eventually resulting in a poorer healthcare experience (Burt et al., 2016).
Where the HPs are themselves bilingual, or native English speakers from a different cultural background, we recommend that they reflect on their use of risk and uncertainty expressions and the meaning they intend in relation to their knowledge of their patients' background. This recommendation is supported by findings of the study on communication at Hong Kong emergency departments, which found that nearly half of the doctors thought that the information was changed when they had to switch between the Cantonese and English languages (Pun et al., 2017).
Reassuringly, the HPs mostly demonstrated positive accommodative behaviors. Although we targeted only those parts of the talk that involved (un)certainty regarding the patient's health or diagnosis, the full conversations showed that HPs consistently and appropriately used CAT strategies throughout their talk. Their use of multiple strategies created communication patterns such as “small talk-providing diagnosis” sandwiches. The HPs' skilled approach ensured that their patients felt safe and relaxed. The patients rated the quality of the interactions they had with their HP highly (mean = 4.9; 5 = Definitely), confirming that they were happy.
We acknowledge that, because this study was conducted in one ED of a single public hospital in Queensland, it was not possible to recruit a wide range of, and more, bilingual patients and HPs. Data collection was entirely dependent on who presented and which HPs were rostered on. The ED context also generated a variety of health presentations and therefore different degrees of uncertainty. It would be of interest to explore how conversations about uncertainty differ in more acute settings.
No interpreters were used in the analyzed conversations. However, patients differed in their proficiency in English, as evident from the recordings and their self-assessed proficiency ratings. Existing research shows that patients from diverse cultural and linguistic backgrounds may have low health literacy (Mantwill and Schulz, 2017; Guttman et al., 2018). Low health literacy is associated with limited second language proficiency (Becerra et al., 2017; Mantwill and Schulz, 2017), but could also reflect a lack of experience with or understanding of the medical environment in the host country (e.g., Hyatt et al., 2017). A lack of proficiency in the language used in health consultations is an important barrier to understanding healthcare advice and may exacerbate difficulties in understanding the healthcare context [see, for example, Zamor et al. (2022)]. Further research should consider a systematic exploration of second language skills and health literacy, specifically targeting proficiency in speaking and understanding. Given the differences in the use and understanding of epistemic expressions, and the importance of such expressions in healthcare conversations, a better understanding of the interaction between language proficiency and health literacy and their impact on how uncertainty expressions are understood and used will enable more targeted advice for HPs to mitigate against miscommunication.
HPs and patients used a variety of words and expressions to communicate uncertainty and risk. Overall, both bilingual and monolingual HPs communicated effectively with their patients when there was uncertainty. However, there were instances when it was unclear whether expressions of uncertainty used by HPs were understood by their bilingual patients as intended. This is concerning because the misunderstandings that can result may put patients at risk and contribute to poorer patient outcomes. To ensure clarity of their messages to patients, HPs should reflect on their use of expressions of (un)certainty and risk and how these are variably understood depending on their patient's cultural and linguistic background.
The implications of our findings for HPs are threefold. First, HPs should be especially mindful when using risk and uncertainty expressions in their consultations. For HPs who practice in their other language (i.e., not their first language), such mindful practice is vital, given that their own use and understanding of uncertainty expressions may differ from that of their patients. Second, when communicating with patients, especially when it is evident that the patient speaks another language as their first language and when the health information that is conveyed to them must be clearly understood by the patient (e.g., treatment options, medication instructions), HPs are advised to carefully check their patients' understanding, repeat important messages, and/or avoid using epistemic expressions where possible. Finally, the recommendations above should not be confined to linguistically or culturally discordant healthcare contexts. When we speak the same language, perhaps especially when we are native or fluent speakers, we tend to assume that the words we use are understood, as intended, by others. They may not be, and it is important for HPs to be mindful of nuances in meaning, especially when communicating uncertainty, in all healthcare interactions, even when both HP and patients share the same first language.
The datasets presented in this article are not readily available because the participants did not agree for this to occur. Please contact the first author (djIubmlzc2VuQHF1dC5lZHUuYXU=) directly for data requests.
The studies involving human participants were reviewed and approved by Metro South Human Research Ethics Committee and the Human Research Ethics Committee at Queensland University of Technology (Ethics approval number HREC/2021/QMS/73181). The patients/participants provided their written informed consent to participate in this study.
VN was responsible for the data collection and original analyses and led the development of the manuscript. RM provided research supervision. Both authors contributed to the conceptualization of the project and its methodology.
The study was funded by the PA Research Foundation through a Rethinking Emergency Medicine Grant (2021) and supported by the Princess Alexandra Hospital (PAH) Emergency Medicine Department.
We thank the staff of the Princess Alexandra (PA) Hospital Emergency Department and the patients who contributed to the study, as well as Dr. Rob Eley for his feedback and support and Ass. Prof. Michelle Riedlinger for her feedback.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^Our larger dataset includes 53 conversations between both monolingual and bilingual HPs (n = 37) and patients (n = 43).
2. ^We recognize that there are limitations with any questionnaires that involve self-rated language proficiency, including the fact that it is unclear whether the person compares their proficiency in the second language against their first language skills or against the skills of a monolingual speaker of the other language. However, it gives an indication of how the individual perceives their own skills and that perception is likely to impact how confidently they engage in their health consultations. Also, it is common practice in bilingual research to administer language questionnaires that involve self-ratings of proficiency (see, for example, Hatzidaki and Potnos, 2008). In our study, it was not practicable to do anything other than obtain self-ratings of proficiency.
3. ^We excluded interjections (e.g., “um”), unclear words, and words intended for people other than patients and HPs (e.g., other HPs or companions) and that were not part of the direct communication between the patient and their HP.
4. ^For the purposes of this article, we understand small talk in healthcare settings as sequences of sentences that involve a topic shift or change, initiated by either the HP or patient at any point in the visit, to talk that both participants treat as a new line of talk that is referentially independent from their institutional identities as patients or HPs (Hudak and Maynard, 2011). Small talk is essential in building rapport with the patient, but the use of these words in rapport building was not the focus of our analysis.
Becerra, B. J., Arias, D., and Becerra, M. B. (2017). Low health literacy among immigrant Hispanics. J. Racial Ethn. Health Disparities. 4, 480–483. doi: 10.1007/s40615-016-0249-5
Blanch-Hartigan, D., Van Eeden, M., Verdam, M. G. E., Han, P. K. J., Smets, E. M. A., and Hillen, M. A. (2019). Effects of communication about uncertainty and oncologist gender on the physician-patient relationship. Patient Educ. Couns. 102, 1613–1620. doi: 10.1016/j.pec.2019.05.002
Burt, J., Lloyd, C., Campbell, J., Roland, M., and Abel, G. (2016). Variations in GP-patient communication by ethnicity, age, and gender: evidence from a national primary care patient survey. Br. J. Gen. Pract. 66, e47–e52. doi: 10.3399/bjgp15X687637
Butow, P., Sze, M., Dugal-Beri, P., Mikhail, M., Eisenbruch, M., Jefford, M., et al. (2011). From inside the bubble: migrants' perceptions of communication with the cancer team. Supportive Care in Cancer. 19, 281–290. doi: 10.1007/s00520-010-0817-x
Chevalier, B. A. M., Watson, B. M., Barras, M. A., and Cottrell, W. N. (2017). Investigating strategies used by hospital pharmacists to effectively communicate with patients during medication counselling. Health Expect. 20, 1121–1132. doi: 10.1111/hex.12558
Chevalier, B. A. M., Watson, B. M., Barras, M. A., and Cottrell, W. N. (2018). Hospital pharmacists' and patients' views about what constitutes effective communication between pharmacists and patients. Int. J. Pharm. Pract. 26, 450–457. doi: 10.1111/ijpp.12423
Chevalier, B. A. M., Watson, B. M., Barras, M. A., and Cottrell, W. N. (2020). Assessing communication behaviours of hospital pharmacists: How well do the perspectives of pharmacists, patients, and an independent observer align? J. Lang. Soc. Psychol. 39, 626–652. doi: 10.1177/0261927X20909867
Considine, J., Ung, L., and Thomas, S. (2000). Triage nurses' decisions using the National Triage Scale for Australian emergency departments. Accident and Emergency Nursing. 8, 201–209. doi: 10.1054/aaen.2000.0166
Fabienne, N. J., Nicole, P., Bénédicte, L., and Pierre, K. (2019). The migration-related language barrier and professional interpreter use in primary health care in Switzerland. BMC Health Serv. Res. 19, 1–10. doi: 10.1186/s12913-019-4164-4
Ferguson, W. J., and Candib, L. M. (2002). Culture, language, and the doctor-patient relationship. Fam. Med. 34, 353–361.
Filipović, L. (2016). May vs. might in native vs. non-native English: Implications for inference and judgement in legal and educational contexts. Appl. Linguist. 181–201. doi: 10.1515/applirev-2016-0008
Fossli Jensen, B., Dahl, F. A., Safran, D. G., Garratt, A. M., Krupat, E., Finset, A., et al. (2011). The ability of a behaviour-specific patient questionnaire to identify poorly performing doctors. BMJ Qual. Saf. 20, 885–893. doi: 10.1136/bmjqs-2011-000021
Gala, P., Sriram, V., Kotian, C., Ballala, K., Vedanthan, R., Perish, E., et al. (2021). Perceptions of the doctor-patient relationship among patients in a private, secondary-level hospital in Southern India. Front. Public Health. 9, 768705–768705. doi: 10.3389/fpubh.2021.768705
Gallois, C., Ogay, T., and Giles, H. (2005). “Communication accommodation theory: a look back and a look ahead.” in: Theorizing About Intercultural Communication, Ed W. B. Gudykunst (Thousand Oaks, CA: Sage).
Gasiorek, J., and Van De Poel, K. (2012). Divergent perspectives on language-discordant mobile medical professionals' communication with colleagues: an exploratory study. J. Appl. Commun Res. 40, 368–383. doi: 10.1080/00909882.2012.712708
Giles, H. (2016). Communication Accommodation Theory: Negotiating Personal Relationships and Social Identities Across Contexts. Cambridge, Cambridge University Press. doi: 10.1017/CBO9781316226537
Gordon, G. H., Joos, S. K., and Byrne, J. (2000). Physician expressions of uncertainty during patient encounters. Patient Educ. Couns. 40, 59–65. doi: 10.1016/S0738-3991(99)00069-5
Guttman, N., Lev, E., Segev, E., Ayecheh, S., Ziv, L., Gadamo, F., et al. (2018). “I never thought I could get health information from the Internet!”: Unexpected uses of an Internet website designed to enable Ethiopian immigrants with low/no literacy skills to browse health information. New Media Soc. 20, 2272–2295. doi: 10.1177/1461444817712937
Han, P. K. J. (2021). Uncertainty in Medicine: A Framework For Tolerance. Oxford, Oxford University Press, Incorporated. doi: 10.1093/oso/9780190270582.001.0001
Han, P. K. J., Klein, W. M. P., and Arora, N. K. (2011). Varieties of uncertainty in health care: a conceptual taxonomy. Med. Decis. Making. 31, 828–838. doi: 10.1177/0272989X10393976
Hehl, J., and McDonald, D. D. (2014). Older adults' pain communication during ambulatory medical visits: An exploration of communication accommodation theory. Pain Manag. Nurs. 15, 466–473. doi: 10.1016/j.pmn.2012.03.007
Hsieh, E., and Terui, S. (2015). Inherent tensions and challenges of oncologist-patient communication: implications for interpreter training in health-care settings. J. Appl. Commun. 43, 141–162. doi: 10.1080/00909882.2015.1019542
Hudak, P. L., and Maynard, D. W. (2011). An interactional approach to conceptualising small talk in medical interactions. Sociol Health Illn. 33, 634–653. doi: 10.1111/j.1467-9566.2011.01343.x
Hyatt, A., Lipson-Smith, R., Schofield, P., Gough, K., Sze, M., Aldridge, L., et al. (2017). Communication challenges experienced by migrants with cancer: A comparison of migrant and English-speaking Australian-born cancer patients. Health Expectations: An International Journal of Public Participation in Health Care and Health Policy. 20, 886–895. doi: 10.1111/hex.12529
Jones, L., Sheeran, N., Lanyon, H., Evans, K., and Martincovic, T. (2018). Nurses' perceptions of communicating with minority parents in a neonatal nursery: a communication accommodation theory approach. J. Healthc. Commun. 11, 175–185. doi: 10.1080/17538068.2018.1460959
Mantwill, S., and Schulz, P. J. (2017). Low health literacy and healthcare utilization among immigrants and non-immigrants in Switzerland. Patient Educ. Couns. 100, 2020–2027. doi: 10.1016/j.pec.2017.05.023
McCarthy, D., Powell, R. E., Cameron, K. A., Salzman, D. H., Papanagnou, D., Doty, A. M., et al. (2020). Simulation-based mastery learning compared to standard education for discussing diagnostic uncertainty with patients in the emergency department: a randomized controlled trial. BMC Med. Educ. 20, 49. doi: 10.1186/s12909-020-1926-y
Menichetti, J., Gerwing, J., Borghi, L., Gulbrandsen, P., and Vegni, E. (2021). Saying “I Don't Know”: a video-based study on physicians' claims of no-knowledge in assisted reproductive technology consultations. Front. Psychol. 11, 611074–611074. doi: 10.3389/fpsyg.2020.611074
Mulder, J., Williams, C. P., and Moore, E. (2019). Sort of in Australian English: the elasticity of a pragmatic marker. J. Asian Pac. Commun. 29, 9–32. doi: 10.1075/japc.00019.mul
Paternotte, E., Van Dulmen, S., Van Der Lee, N., Scherpbier, A. J. J. A., and Scheele, F. (2015). Factors influencing intercultural doctor–patient communication: a realist review. Patient Educ. Couns. 98, 420–445. doi: 10.1016/j.pec.2014.11.018
Phillips, S., Wyatt, L. C., Turner, M. M., Trinh-Shevrin, C., and Kwon, S. C. (2020). Patient-provider communication patterns among Asian American immigrant subgroups in New York City. Patient Educ. Couns. 1049–1058. doi: 10.1016/j.pec.2020.10.002
Pines, R., Giles, H., and Watson, B. (2021). Managing patient aggression in healthcare: initial testing of a communication accommodation theory intervention. Psychol. Lang. Commun. 25, 62–81. doi: 10.2478/plc-2021-0004
Poluch, M., Feingold-Link, J., Ankam, N., Kilpatrick, J., Cameron, K., Chandra, S., et al. (2022). I don't have a diagnosis for you: preparing medical students to communicate diagnostic uncertainty in the emergency department. MedEdPORTAL. 18, 11218. doi: 10.15766/mep_2374-8265.11218
Pun, J. K. H., Chan, E. A., Murray, K. A., Slade, D., and Matthiessen, C. M. I. M. (2017). Complexities of emergency communication: clinicians' perceptions of communication challenges in a trilingual emergency department. J. Clin. Nurs. 26, 3396–3407. doi: 10.1111/jocn.13699
Rendle-Short, J. (2009). The address term mate in Australian English: is it still a masculine term? Aust. J. Linguist. 29, 245–268. doi: 10.1080/07268600902823110
Richardson, A., Thomas, V. N., and Richardson, A. (2006). “Reduced to nods and smiles”: Experiences of professionals caring for people with cancer from black and ethnic minority groups. Eur. J. Oncol. Nurs. 10, 93–101. doi: 10.1016/j.ejon.2005.05.002
Schinkel, S., Schouten, B. C., Kerpiclik, F., Van Den Putte, B., and Van Weert, J. C. M. (2019). Perceptions of barriers to patient participation: are they due to language, culture, or discrimination? Health Commun. 34, 1469–1481. doi: 10.1080/10410236.2018.1500431
Segalowitz, N. S., Doucerain, M. M., Meuter, R. F. I., Zhao, Y., Hocking, J., and Ryder, A. G. (2016). Comprehending adverbs of doubt and certainty in health communication: a multidimensional scaling approach. Front. Psychol. 7, 558. doi: 10.3389/fpsyg.2016.00558
Simon, M. A., Tom, L. S., Taylor, S., Leung, I., and Vicencio, D. (2019). ‘There's nothing you can do … it's like that in Chinatown': chinese immigrant women's perceptions of experiences in Chicago Chinatown healthcare settings. Ethn. Health. 26, 1–18. doi: 10.1080/13557858.2019.1573973
Skjeggestad, E., Gerwing, J., and Gulbrandsen, P. (2017). Language barriers and professional identity: a qualitative interview study of newly employed international medical doctors and Norwegian colleagues. Patient Educ. Couns. 100, 1466–1472. doi: 10.1016/j.pec.2017.03.007
White, J., Plompen, T., Osadnik, C., Tao, L., Micallef, E., and Haines, T. (2018). The experience of interpreter access and language discordant clinical encounters in Australian health care: a mixed methods exploration. Int. J. Equity Health. 17, 151. doi: 10.1186/s12939-018-0865-2
Zamor, R. L. L., Vaughn, L. M. M., Mccann, E., Sanchez, L., Page, E. M. M., and Mahabee-Gittens, E. M. (2022). Perceptions and experiences of Latinx parents with language barriers in a pediatric emergency department: a qualitative study. BMC Health Serv. Res. 22, 1–1463. doi: 10.1186/s12913-022-08839-w
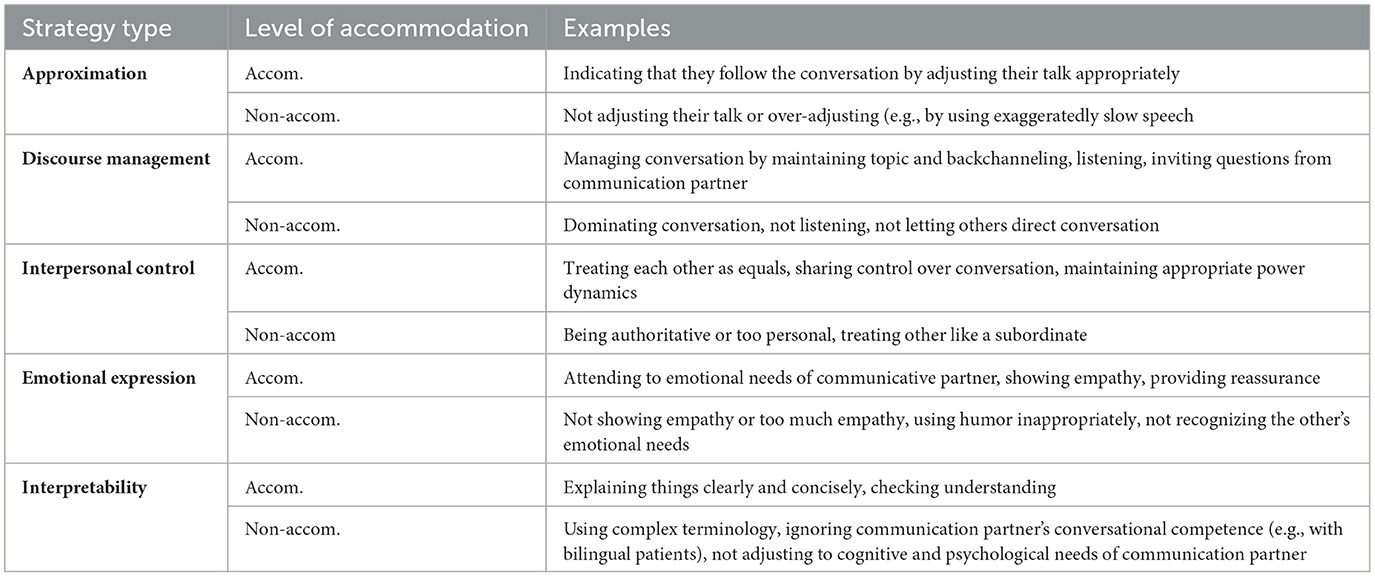
Table A1. Communication strategies coding scheme used in the current study (see Jones et al. (2018) and Chevalier et al. (2020) for Examples).
Keywords: health communication, bilingual patients, health practitioner, emergency department, communication accommodation theory (CAT)
Citation: Nissen V and Meuter RFI (2023) Language and culture in health communication in an emergency context: do health practitioners and patients talk differently about uncertainty and risk? Front. Commun. 8:1110558. doi: 10.3389/fcomm.2023.1110558
Received: 29 November 2022; Accepted: 22 June 2023;
Published: 18 July 2023.
Edited by:
Christiane Stock, Institute of Health and Nursing Science, Berlin, GermanyReviewed by:
Pål Gulbrandsen, University of Oslo, NorwayCopyright © 2023 Nissen and Meuter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vanda Nissen, djIubmlzc2VuQHF1dC5lZHUuYXU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.