- 1Endocrinology Department, People's Hospital 115, Ho Chi Minh City, Vietnam
- 2Ho Chi Minh City University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam
- 3Center for Integrated Science and Humanities, Fukushima Medical University, Fukushima, Japan
Objectives: This study aimed to fill the gap between Vietnamese diabetic patients' needs and care through a qualitative study asking about their experiences with diabetes and quality of care.
Methods: Interviews with five diabetic patients were conducted at a tertiary general hospital located in southern Vietnam. The transcribed data were first subjected to quantitative text analysis using KH Coder to identify major categories of frequently used words, followed by a qualitative analysis of selected cases using the Steps for Coding and Theorization (SCAT) method.
Results: The major categories of frequently used words were chronic health conditions, services, facilities, insurance, patient-doctor communication, and medication. SCAT analysis of three selected cases identified six themes: “Disregarding the disease at the early stage,” “Fear of complications,” “Satisfaction with hospital services and medical staff,” “Insurance-related problems,” “Long waiting times,” and “Communication barriers between patients and doctors.” Patients were satisfied with improved hospital facilities and services; however, the overloading of one hospital led to long waiting times and communication difficulties with doctors. Difficulties with health insurance were also observed, and patients were rather passive in disease management and needed to be empowered through improved communication with doctors and other care providers.
Conclusion: These findings from our trial of introducing a qualitative study into service evaluation suggest that listening to patients can help health providers learn their perspectives and be more responsive to their needs.
Introduction
Diabetes mellitus is a global pandemic, with 79% of affected patients living in low- and middle-income countries (International Diabetes Federation, 2019). According to the World Health Organization report in 2016, it is estimated that one in every 20 Vietnamese adults has diabetes. In addition, the number of people with a pre-diabetic condition is estimated to be three times higher than those with diabetes (WHO Representative Office for Vietnam, 2016). Even if patients are diagnosed and seeing doctors, the majority have poor glycemic and metabolic control (Nguyen et al., 2020). Prevention and control of diabetes in the country face various challenges, such as a lack of awareness about diabetes among the population, weak coordination between sectors to create a supportive environment, and poor access to services for diabetes prevention, diagnosis, and treatment (Ngoc et al., 2020). If the patient has to be hospitalized, they are at risk of falling into poverty, especially if they are non-resident, ineligible for insurance, or already struggling financially (Vuong, 2015). Therefore, improvements in the quality of diabetic care and the Vietnamese health care system are still needed.
Moreover, diabetes is a chronic metabolic disorder that impacts not only the physical but also the social and mental wellbeing of people living with it. More attention needs to be paid to patients' emotional responses to illnesses and health providers' responsiveness toward such responses, which influence patients' overall quality of life (Coulter et al., 2014). Although Vietnam has systematized channels to help patients express complaints related to the health system, they do not work effectively in practice (Ha et al., 2015). Further, in the academic field, there are still relatively few studies that aim to explore what diabetic patients think about their disease and quality of care in Vietnam. Therefore, an improved understanding of those patients' experiences is needed. Positive patient experiences have a positive impact on treatment outcomes through improved engagement with and adherence to providers' instructions and treatments.
Numerous studies have explored patient thinking about diseases and satisfaction using self-administered questionnaires (Gadsby et al., 2017; Chiou et al., 2019). There are some studies showing satisfaction among Vietnamese patients (Tran et al., 2019; Tran and Le, 2020). However, patients tend to provide favorable evaluations of the services they receive when assessed by a quantitative research questionnaire (Dambha-Miller et al., 2018). Narrative qualitative methods, such as in-depth interviews or focus groups, can produce more detailed data about patient experiences and the way they are interpreted and explained (Coulter et al., 2014). A recent systematic review that investigated how qualitative methods were used in research on diabetes (Hennink et al., 2017) found comparatively infrequent use over the past 30 years, with the majority being conducted in developed Western countries; only a few studies were conducted in developing countries. In Vietnam, a mixed method of quantitative and qualitative research has been applied for the evaluation of health services since around 2000 (Duong et al., 2004). However, the experiences of Vietnamese patients with diabetes and the challenges they face in the management of chronic conditions have not been reported in detail, other than in one study on patients with gestational diabetes (Hirst et al., 2012) and another on immigrants in the United States (Mull et al., 2001). Therefore, this study aimed to explore the experiences and quality of care of patients with diabetes at a tertiary general hospital in southern Vietnam. To our knowledge, this report represents the very first trial at this study site to apply a qualitative method to service evaluation.
Materials and Methods
This qualitative study involved semi-structured interviews conducted at a tertiary general hospital in Ho Chi Minh City as a part of the Japan International Cooperation Agency's Partnership Program. All researchers received training in qualitative research and analysis in the program's research methodology training course (Le et al., 2014).
Patients were recruited from the outpatient unit of the endocrinology department. The investigators identified five patients who met the following inclusion criteria: diagnosis of diabetes mellitus, aged 18 years or older, and able to give informed consent. Each participant was interviewed individually by one of the coauthors, who is an experienced physician but was not involved in the patients' diagnosis or treatment. The interviews took place in a quiet room outside the clinic. The interview guide included information on basic characteristics (e.g., sex, age, disease duration, current treatment) and the following main questions by referring to previous qualitative research on the topic of shared decision-making between physicians and patients: “How do you feel about your disease?” “What do you expect from your doctor?” “Were you able to express your expectations to your doctor? If not, why?” “What makes you feel most comfortable/uncomfortable during your hospitalization?” and “What do you think about the services at this hospital?”
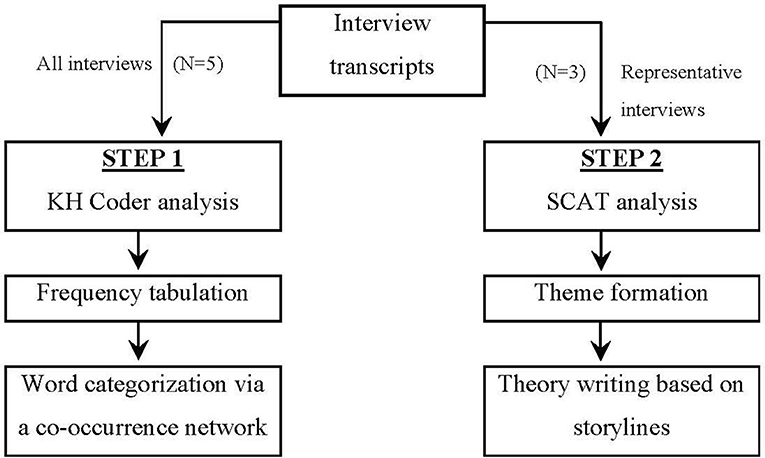
All interviews were recorded, transcribed in Vietnamese, and translated into English by a bilingual translator. Following the method used in a previous study (Goto et al., 2014), a quantitative analysis of the text data was conducted, followed by a qualitative analysis (Figure 1). In the first step of the analysis, the translated English text data were analyzed by the text mining software KH Coder (version 3) (Higuchi, 2021). KH Coder segments sentences, lists frequently used words, and develops a co-occurrence network diagram showing relationships between words and their corresponding frequencies. We first focused on the most frequently used words, excluding pronouns, and then categorized these words using the sub-graph analysis of the co-occurrence network. Sentences using the words included in each category were placed closely in the diagrams and labeled with different colors. These major categories in the co-occurrence network served as a visual aid to capture the overall conversations.
In the second step of the analysis, three cases with rich data on the topics extracted from the text analysis were selected and analyzed qualitatively using the Steps for Coding and Theorization (SCAT) method (Otani, 2008), which consists of the following four steps: (1) capture noteworthy words or phrases from the text; (2) paraphrase the words or phrases extracted in the previous step; (3) create the concepts that account for the words listed in the previous steps; and (4) form the themes in consideration of the context from the concepts in the third step. In the following re-contextualization process, we developed a “storyline” from the emerging themes in the fourth step, and summarized the main points in the “theory writing”. Theories from three patients were summarized and discussed. Two authors analyzed the data using KH Coder and SCAT independently. The results were then compared and combined after being reviewed by another coauthor.
Consent was obtained from all participants after they had been given a thorough explanation of the research aims and protocol. This study was approved by the Medical Ethics Committee of People's Hospital 115 (Approval No. CS/15/19/20).
Results
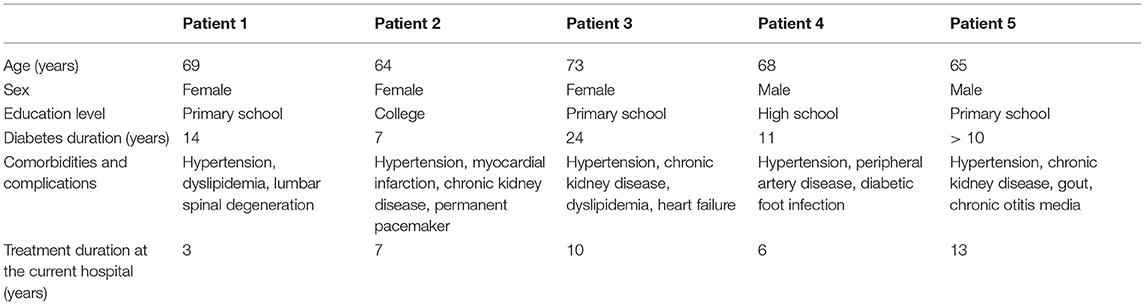
The basic characteristics of the five participants are presented in Table 1. Most patients had a long duration of diabetes (four of five patients had a disease duration longer than a decade) accompanied by multiple comorbidities and diabetic complications. Accordingly, these patients had been visiting the study site for a long time. Two participants had a relatively high-level educational background (high school and university graduates), whereas the others had a lower education level.
Overall, 2,489 words in English (2,022 words in Vietnamese before translation) and 280 sentences were entered into the KH Coder analysis, and 55 words (nouns, adjectives, adverbs, and verbs) used five times or more were entered to be analyzed in the co-occurrence network (Figure 2). The major topics of the interviews included issues related to chronic disease conditions (sub-graph group numbers 3, 4, and 8), services (services, facilities, insurance, and medication) (1, 2, 5, and 7), and patient-doctor communication (Coulter et al., 2014). We then selected three patients whose interviews were rich in these topics.
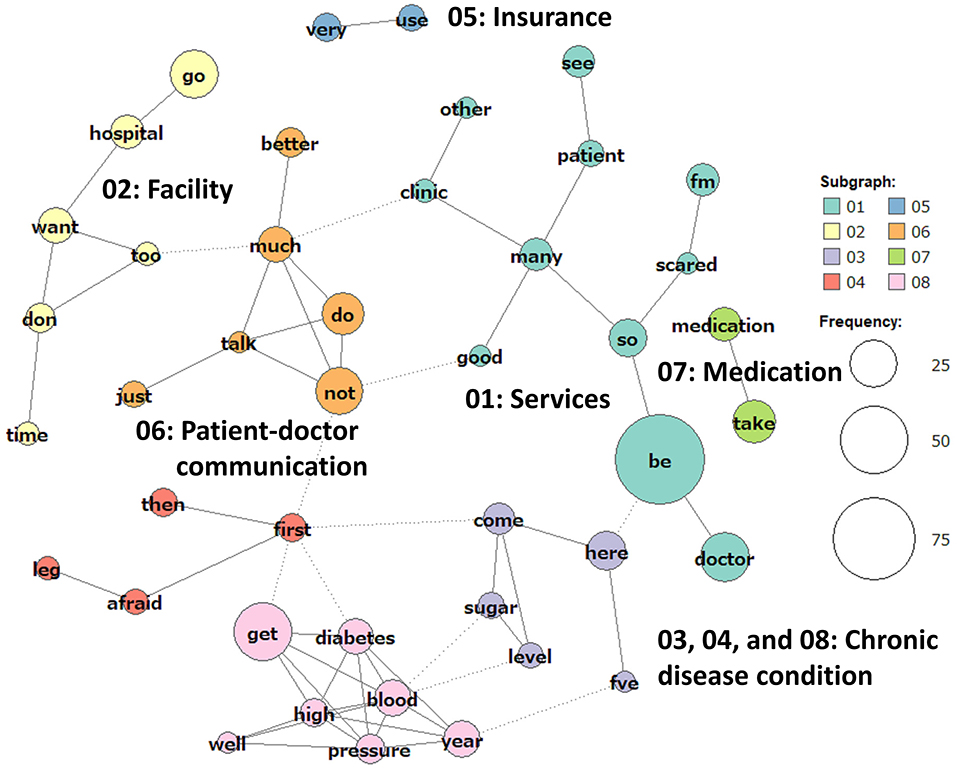
Figure 2. Co-occurrence network of frequently used words. A total of 280 sentences were entered into the KH Coder analysis and 55 words used five times or more were analyzed in the co-occurrence network.
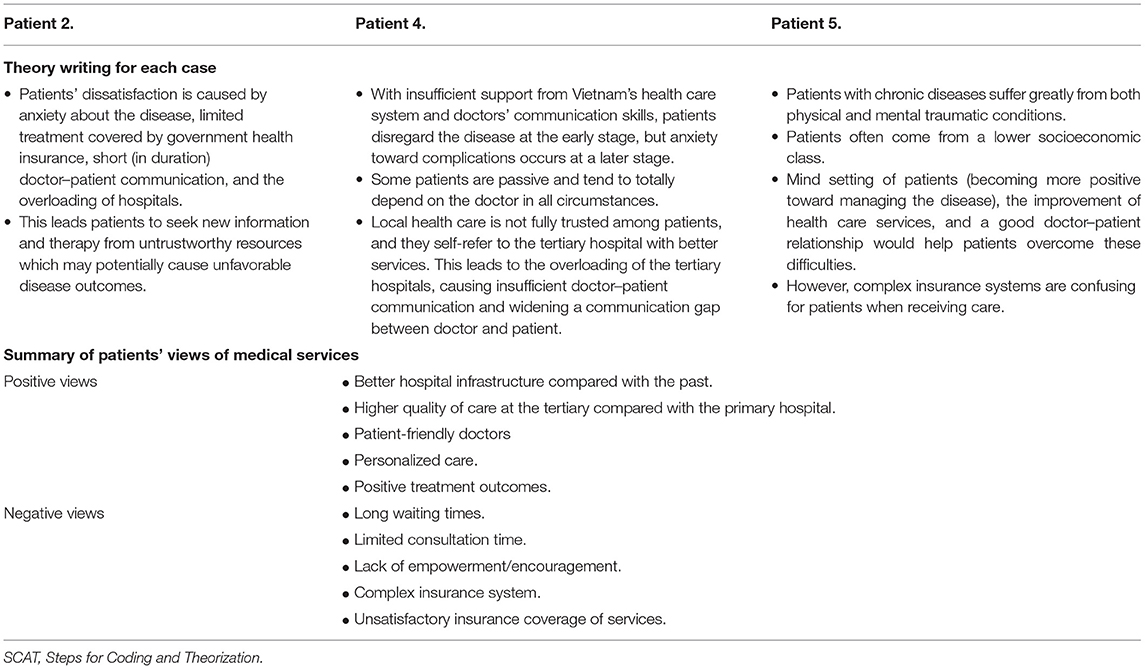
Following the results of the KH Coder analysis, we focused on patients' perceptions of their disease condition and patient-doctor communication in the subsequent SCAT analysis. The main points listed in the theory writing are presented in Table 2. The six themes that emerged are listed below.
“Disregarding the Disease at the Early Stage” and “Fear of Complications”
Patients often disregarded diabetes at the early stage of the disease, but were subsequently terrified, especially when faced with complications. Patients stated, “I was not afraid when I first got diabetes”; “It is getting worse”; and “I'm so scared now.” They realized that diabetes is a chronic and invisible disease that can cause a variety of severe complications leading to physical disability and mental trauma that they have to suffer throughout their lifetime. One patient said, “Got my medication and take it every day. We Vietnamese often don't take medication during Tet (Vietnamese New Year), but I have to take it every day.”
“Satisfaction With Hospital Services and Medical Staff”, “Insurance-Related Problems”, and “Long Waiting Times”
Positive and negative views about services are also shown in Table 2. Patients gave high evaluations of the hospital facilities and services. They mentioned that the services were better now than in the past. One patient emphasized, “I've been here many, many times. There have been many changes here. The services and facilities are much better.” Another patient mentioned the staff by saying, “Everyone is very nice, the doctors and nurses.” However, many clinical encounters, including those about insurance, long waiting times, and short conversations between doctors and patients, made them feel uncomfortable. Insurance-related issues seemed to be a major concern for the patients. One patient said, “I don't want to use my health insurance too much,” and another said, “I was told my health insurance is still valid, but I feel uncomfortable.” Long waiting times were another major concern among the patients because this led to short conversations between doctors and patients. One participant complained, “Waiting...waiting… and waiting. We have no choice but to wait because the hospital is so crowded.”
“Communication Barriers Between Doctors and Patients”
Despite these complaints, patients still felt comfortable talking with a doctor or expressing their demands. One patient stated, “I tell my doctor everything.” The patients also expressed trust in the doctors. One patient said, “I only take what the doctor tells me. If I took anything else, I would tell the doctor. Or I would ask for the doctor's advice.” Others remarked, “I just follow the doctor's instructions, I will take whatever the doctor prescribes.” However, a lack of time was causing a communication barrier between doctors and patients. One patient stated, “The doctor does not talk much. I don't want to ask him too much. He has so many patients.”
Discussion
Diabetes mellitus is a chronic silent disease that people do not recognize as a serious problem because its consequences do not manifest immediately (Ramachandran, 2014). Our patients tended to disregard the disease at an early stage but became terrified of the consequences once they began to experience comorbidities and complications. This might be caused by the lack of patient education and empowerment strategies in the current Vietnamese health system. One study from southern Vietnam showed a low level of disease knowledge among the general population aged 40–64 years (Binh et al., 2015), indicating the need for careful communication and education about diabetes around the time of diagnosis.
Our study participants accepted diabetes as a part of their life and followed their treatment instructions. Collins and colleagues classified diabetes patients into three types based on qualitative interviews: (1) “proactive managers,” who are self-motivated in disease control, (2) “passive followers,” who simply follow a prescribed regime, and (3) “non-conformists,” who do not follow a prescribed regimen closely (Collins et al., 2009). The attitudes of our study participants fit the description of “passive followers,” possibly in part because of their inadequate knowledge and self-management skills. Our patients were inactive or showed a strong dependence on their doctors without understanding the importance of disease self-management.
Major factors that have been reported to affect patients' choices of a doctor or hospital are geographical and administrative access, the cleanliness and modernity of the facilities, and equipment, reputation, medical costs, staff kindness, and waiting times (Burge et al., 2004; Yoon et al., 2004; Kim et al., 2017). All of the participants in this study stated that they selected the tertiary hospital because of its positive reputation and were satisfied with the hospital infrastructure and staff kindness. However, they experienced distress caused by the insurance system and long waiting times. Vietnam has made significant progress toward achieving universal health coverage, and 87% of the population is currently covered by national insurance (WHO Representative Office for Vietnam, 2016). Unfortunately, patient evaluations of hospital services have been lower among those using insurance compared with those paying out of pocket (Hwang et al., 2020), which might be associated with patients' hesitation to use insurance. Such differences in service quality depending on the payment method require further investigation. Moreover, improvements in insurance coverage have led to an increase in health service utilization, resulting in occasional overloads of the public health system (Matsushima et al., 2019). Likewise, other studies conducted at tertiary hospitals in Vietnam have highlighted long waiting times as a serious matter (Tran et al., 2017; Nguyen et al., 2018).
Overloads of a public health care system not only cause long waiting times but also represent a barrier to sufficient doctor-patient communication. The patients in our study voiced their concerns that their doctor did not talk with them very much or that they hesitated to talk to a busy doctor. Such hesitation is possibly augmented by several other underlying factors in Vietnam. First, older patients lived through a very difficult socioeconomic period after a series of long wars. Their past experiences with a severely deficient health system might make them feel more comfortable with current services, despite the need for improvement. Second, patients perceive the role of doctors to cure (not care for) their disease, and open conversations between doctors and patients may not be a part of the culture. This very first qualitative study in Viet Nam aimed to discover the experiences of long-term diabetic patients provided the information about lacking patient-doctor communication in Viet Nam which is the same in some developing countries. Previous research in the Southeast Asia region has reported paternalistic communication among doctors, although they were aware that participatory communication was desirable (Duong et al., 2004; Claramita et al., 2011, 2013). Such focus on preventing miscommunication or poor communication between patients and healthcare providers might help improve treatment outcomes and mitigate the cost of treatment which has been already an economic burden at both the individual and country levels (Vuong, 2015, 2018). It is noteworthy that the patients in our study mentioned that they were satisfied with hospital “staff” that might include doctors and nurses. This may provide a clue for promoting more communication between patients and health professionals in overloaded public hospitals in Vietnam. One study on diabetes care among Vietnamese nurses revealed that they recognized the role of nurses in creating a positive relationship with patients and supporting them to take part in disease management within a social context (Pham and Ziegert, 2016). Interprofessional efforts are therefore needed to improve communication with patients effectively in the overloaded public service setting in Vietnam.
There might be important country-specific issues underpinning the patients' perceptions of the services that they receive. First, the low socioeconomic starting point of Vietnam after long wars may have made it easier for patients to accept their current circumstances. Second, the low level of health literacy among the general public (regardless of educational background) may have accelerated the difficulty communicating with doctors. On the provider side, especially with regard to the above-mentioned collaboration with nurses, Kanno's work on Japanese nurses' experiences of supporting patients' decision-making used the same analysis methods as in our study and revealed that they faced a “difficult environment for supporting decision-making” and a need for “collaborating at the organizational level,” which required organizational changes including improving staff allocation, providing times and spaces for interviews, and skills training for nurses in decision-making support (Kanno et al., 2019). Health policy attention toward the need for organizational efforts to facilitate such a mind shift in both patients and providers is required in Vietnam. Vuong and Napier (2015) proposed the “mindsponge mechanism,” which explains knowledge processing as a series of steps involving filtering information, trusting and accepting the information, and entering it into one's mindset. They have shown that the theory is applicable to process large amount of complex information including COVID-19 vaccination (Vuong et al., 2022). Understanding and application of such theory in clinical practice would help health providers to improve their methods of communication at the individual and organizational levels. Vuong (2018) states that “communication of science and scientists' efforts to better serve the public with their research, directly or indirectly, will become the next challenge if Vietnam is to move forward in a more competitive world.”
This study had two major methodological limitations. First, the data collected from the interviews were not exhaustive. The sample size was small, with only three patients being interviewed, and the length of the interviews was <30 min given the busy clinical setting and the fact that some participants were hurrying to return home to faraway provinces. In addition, we lacked expertise in holding qualitative interviews because this was the first trial introducing this method to review clinical practice. Second, our study participants were limited to outpatients with a long disease duration; the inclusion of inpatients and those with a shorter disease duration might have revealed different viewpoints about the disease and quality of care. Despite these limitations, this pilot trial could serve as a basis for promoting such research requiring active listening to patients' voices and improved participatory communication between doctors and patients. Further study is needed to repeat the interviews to confirm the theoretical saturation of our obtained data (Dworkin, 2012), and to deepen analysis by applying a psychological theory such as the above-mentioned “mindsponge mechanism.”
Conclusion
The findings of this study indicate that patients with diabetes visiting a general hospital in southern Vietnam were dependent on doctors and not fully empowered to manage their disease on their own. They complained about the insurance system and long waiting times, which led to short consultation times. Although small in scale, the results of this qualitative research trial highlight the need for patient education and empowerment strategies, improved accessibility and insurance system quality, and increased interprofessional efforts to create more space for patients to communicate with doctors and other health professionals openly. Assessing health services by carefully listening to patients could provide health care providers with opportunities to learn patients' perspectives and be more responsive to their needs.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of People's Hospital 115. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MT was responsible for collecting data, analyzing data, and writing the manuscript. NK was responsible for collecting data and writing the manuscript. VK was responsible for conceiving and designing the analysis and collecting the data. AG was responsible for conceiving and designing the analysis and writing the manuscript. All authors read and approved the final manuscript.
Funding
This project was supported by the Japan International Cooperation Agency Partnership Program Promoting Evidence-based Patient-centered Health Services in Southern Vietnam: University and Medical Association Partnership Initiative (PI: AG) and in part by the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (No. 20K10539) (Co-PI: AG, PI: Hirohide Yokokawa at Juntendo University).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Oliver Stanyon for editing a draft of this manuscript and reviewers for insightful comments to improve and finalize the manuscript.
References
Binh, T. Q., Phuong, P. T., and Nhung, B. T. (2015). Knowledge and associated factors towards type 2 diabetes among a rural population in the Red River Delta region, Vietnam. Rural Remote Health 15, 3275. doi: 10.22605/rrh3275
Burge, P., Devlin, N., Appleby, J., Rohr, C., and Grant, J. (2004). Do patients always prefer quicker treatment? Appl. Health Econ. Health Policy 3, 183–194. doi: 10.2165/00148365-200403040-00002
Chiou, S.-J., Lee, P.-C., Chang, Y.-H., Huang, P.-S., Lee, L.-H., and Lin, K.-C. (2019). Assessment of patient experience profiles and satisfaction with expectations of treatment effects by using latent class analysis based on a national patient experience survey in Taiwan. BMJ Open 9, e023045. doi: 10.1136/bmjopen-2018-023045
Claramita, M., Dalen, J. V., and Van Der Vleuten, C. P. (2011). Doctors in a Southeast Asian country communicate sub-optimally regardless of patients' educational background. Patient Educ. Couns. 85, e169–174. doi: 10.1016/j.pec.2011.02.002
Claramita, M., Nugraheni, M. D. F., van Dalen, J., and van der Vleuten, C. (2013). Doctor-patient communication in Southeast Asia: a different culture? Adv. Health Sci. Educ. Theory Pract. 18, 15–31. doi: 10.1007/s10459-012-9352-5
Collins, M. M., Bradley, C. P., O'Sullivan, T., and Perry, I. J. (2009). Self-care coping strategies in people with diabetes: a qualitative exploratory study. BMC Endocr. Disord. 9, 6. doi: 10.1186/1472-6823-9-6
Coulter, A., Locock, L., Ziebland, S., and Calabrese, J. (2014). Collecting data on patient experience is not enough: they must be used to improve care. BMJ 348, g2225. doi: 10.1136/bmj.g2225
Dambha-Miller, H., Silarova, B., Irving, G., Kinmonth, A. L., and Griffin, S. J. (2018). Patients' views on interactions with practitioners for type 2 diabetes: a longitudinal qualitative study in primary care over 10 years. Br. J. Gen. Pract. 68, e36. doi: 10.3399/bjgp17X693917
Duong, D. V., Binns, C. W., and Lee, A. H. (2004). Utilization of delivery services at the primary health care level in rural Vietnam. Soc. Sci. Med. 59, 2585–2595. doi: 10.1016/j.socscimed.2004.04.007
Dworkin, S. L. (2012). Sample size policy for qualitative studies using in-depth interviews. Arch. Sex. Behav. 41, 1319–1320. doi: 10.1007/s10508-012-0016-6
Gadsby, R., Fargher, L., Dunn, L., and Young, B. (2017). Measuring patient experience in diabetes care in England and Wales: proof of concept from the Patient Experience of Diabetes Services (PEDS) pilot. Br. J. Diabetes 17, 11–13. doi: 10.15277/bjd.2017.118
Goto, A., Rudd, R. E., Lai, A. Y., Yoshida, K., Suzuki, Y., Halstead, D. D., et al. (2014). Leveraging public health nurses for disaster risk communication in Fukushima City: a qualitative analysis of nurses' written records of parenting counseling and peer discussions. BMC Health Serv. Res. 14, 129. doi: 10.1186/1472-6963-14-129
Ha, B. T. T., Mirzoev, T., and Morgan, R. (2015). Patient complaints in healthcare services in Vietnam's health system. SAGE Open Med. 3, 2050312115610127. doi: 10.1177/2050312115610127
Hennink, M. M., Kaiser, B. N., Sekar, S., Griswold, E. P., and Ali, M. K. (2017). How are qualitative methods used in diabetes research? A 30-year systematic review. Glob. Public Health 12, 200–219. doi: 10.1080/17441692.2015.1120337
Higuchi, K. (2021). KH Coder Version 3.0. Available online at: https://khcoder.net/en/ (accessed July 17, 2021).
Hirst, J. E., Tran, T. S., Do, M. A., Rowena, F., Morris, J. M., and Jeffery, H. E. (2012). Women with gestational diabetes in Vietnam: a qualitative study to determine attitudes and health behaviours. BMC Pregnancy Childbirth 12, 81. doi: 10.1186/1471-2393-12-81
Hwang, J., Vu, G. T., Tran, B. X., Nguyen, T. H. T., Nguyen, B. V., Nguyen, L. H., et al. (2020). Measuring satisfaction with health care services for Vietnamese patients with cardiovascular diseases. PLoS ONE 15, e0235333. doi: 10.1371/journal.pone.0235333
International Diabetes Federation (2019). IDF Diabetes Atlas 9th ed. Brussels: International Diabetes Federation.
Kanno, N., Goto, A., Sato, K., Kawahara, R., and Hatakeyama, T. (2019). Outpatient nurses' awareness of their support for the decision-making of cancer patients undergoing surgical therapy. J. Jpn. Primary Care Assoc. 2019, 78–84. doi: 10.14442/generalist.42.78
Kim, Y.-Y., Bae, J., and Lee, J.-S. (2017). Effects of patients' motives in choosing a provider on determining the type of medical institution. Patient Prefer. Adherence 11, 1933–1938. doi: 10.2147/PPA.S148530
Le, T. Q. N., Goto, A., Tran, T. T., Nguyen, Q. V., and Nguyen, T. K. (2014). Capacity building toward evidence-based medicine among healthcare professionals at the university of medicine and pharmacy, Ho Chi Minh City, and its related institutes. JMAJ. 57, 49–55. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4130096 (accessed January 01, 2020).
Matsushima, M., Yamada, H., and Shimamura, Y. (2019). Analysis on demand and supply side responses during the expansion of health insurance coverage in Vietnam: challenges and policy implications toward universal health coverage. Rev. Dev. Econ. 24, 144–166. doi: 10.1111/rode.12627
Mull, D. S., Nguyen, N., and Mull, J. D. (2001). Vietnamese diabetic patients and their physicians: what ethnography can teach us. West. J. Med. 175, 307–311. doi: 10.1136/ewjm.175.5.307
Ngoc, N. B., Lin, Z. L., and Ahmed, W. (2020). Diabetes: what challenges lie ahead for Vietnam? Ann. Glob. Health 86, 1. doi: 10.5334/aogh.2526
Nguyen, S. T. T., Yamamoto, E., Nguyen, M. T. N., Le, H. B., Kariya, T., Saw, Y. M., et al. (2018). Waiting time in the outpatient clinic at a national hospital in Vietnam. Nagoya J. Med. Sci. 80, 227–239. doi: 10.18999/nagjms.80.2.227
Nguyen, T. K., Diep, B. T. T., Nguyen, V. D. K., Van Lam, H., Tran, K. Q., and Tran, N. Q. (2020). A cross-sectional study to evaluate diabetes management, control and complications in 1631 patients with type 2 diabetes mellitus in Vietnam. Int. J. Diabetes Dev. Ctries. 40, 70–79. doi: 10.1007/s13410-019-00755-w
Otani, T. (2008). SCAT, a qualitative data analysis method by four-step coding: easy startable and small scale data-applicable process of theorization. Bull. Gradu. School Educ. Hum. Develop. 54, 27–44. Availalble online at: https://www.educa.nagoya-u.ac.jp/~otani/scat/index-e.html (accessed January 01, 2020).
Pham, L., and Ziegert, K. (2016). Ways of promoting health to patients with diabetes and chronic kidney disease from a nursing perspective in Vietnam: a phenomenographic study. Int. J. Qual. Stud. Health Wellbeing 11, 30722. doi: 10.3402/qhw.v11.30722
Ramachandran, A. (2014). Know the signs and symptoms of diabetes. Indian J. Med. Res. 140, 579–581. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4311308 (accessed January 01, 2020).
Tran, B. X., Dang, A. K., Vu, G. T., Tran, T. T., Latkin, C. A., Ho, C. S. H., et al. (2019). Patient satisfaction with HIV services in Vietnam: Status, service models and association with treatment outcome. PLoS ONE 14, e0223723. doi: 10.1371/journal.pone.0223723
Tran, T. D., Nguyen, U. V., Nong, V. M., and Tran, B. X. (2017). The patient waiting time in the outpatient clinic at a central surgical hospital of Vietnam: Implications for resource allocation. F1000Research 6, 454. doi: 10.12688/f1000research.11045.3
Tran, T. H. G., and Le, Q. T. (2020). Inpatient satisfaction survey with the communication and behavior of medical staffs in 7A Military Hospital, Ho Chi Minh City, Vietnam. Int. J. Community Med. Public Health 7, 480–483. doi: 10.18203/2394-6040.ijcmph20200050
Vuong, Q. H. (2015). Be rich or don't be sick: estimating Vietnamese patients' risk of falling into destitution. Springerplus 4, 529. doi: 10.1186/s40064-015-1279-x
Vuong, Q. H. (2018). The (Ir)Rational consideration of the cost of science in transition economies. Nat. Hum. Behav. 2, 5. doi: 10.1038/s41562-017-0281-4
Vuong, Q. H., Le, T. T., La, V. P., Nguyen, H. T. T., Ho, M. T., Van Khuc, Q., et al. (2022). Covid-19 vaccines production and societal immunization under the serendipity-mindsponge-3D knowledge management theory and conceptual framework. Humanit. Soc. Sci. Commun. 9, 22. doi: 10.1057/s41599-022-01034-6
Vuong, Q. H., and Napier, N. K. (2015). Acculturation and global mindsponge: an emerging market perspective. Int. J. Intercult. Relat. 49, 354–367. doi: 10.1016/j.ijintrel.2015.06.003
WHO Representative Office for Vietnam (2016). The Growing Burden of Diabetes in Vietnam. Available online at: https://www.who.int/vietnam/news/feature-stories/detail/the-growing-burden-of-diabetes-in-viet-nam?msclkid=39abb0a6b5a211ec984e6b8eced44297 (accessed January 1, 2020).
Yoon, S. J., Yu, S. H., Kim, Y. H., and Lee, J. J. (2004). A study for the factors on choosing hospitals and patients satisfaction between geriatric hospitals and general hospitals. Korea J. Hosp. Manag. 9, 46–75. Available online at: https://www.koreascience.or.kr/article/JAKO200420149327909.page (accessed January 01, 2020).
Keywords: qualitative study, diabetes, Vietnam, quality of life, quality of care
Citation: Tri MT, Khue NT, Khoa VT and Goto A (2022) Patient Views on Quality of Life and Hospital Care: Results From a Qualitative Study Among Vietnamese Patients With Diabetes. Front. Commun. 7:894435. doi: 10.3389/fcomm.2022.894435
Received: 11 March 2022; Accepted: 19 April 2022;
Published: 06 May 2022.
Edited by:
Quan-Hoang Vuong, Phenikaa University, VietnamReviewed by:
Minh-Hoang Nguyen, Ritsumeikan Asia Pacific University, JapanTam-Tri Le, Phenikaa University, Vietnam
Copyright © 2022 Tri, Khue, Khoa and Goto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mai Trong Tri, ZHJtdHRyaUBnbWFpbC5jb20=
 Mai Trong Tri
Mai Trong Tri Nguyen Thy Khue2
Nguyen Thy Khue2 Aya Goto
Aya Goto